Abstract
We present the case of a 55-year-old man who had a diagnosis of an acute anterior ST-segment elevation myocardial infarction. Emergency angiography demonstrated that both coronary systems originated from the right coronary sinus with a culprit proximal left anterior descending artery lesion, which was stented. This is a rare presentation, with only 1 similar case found in published reports. (Level of Difficulty: Intermediate.)
Key Words: acute coronary syndrome, anomalous origination of a coronary artery from the opposite sinus, coronary artery anomaly, single coronary artery, sudden cardiac death
Abbreviations and Acronyms: CAA, coronary artery anomaly; CTA, computed tomography angiography; LAD, left anterior descending (artery); PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-segment elevation myocardial infarction
Central Illustration
History of Presentation
A 55-year-old man presented with a 2-week history of a burning sensation in his throat after 25 min of cycling. This sensation eased with rest initially, but on the day of his hospital admission, it did not. He was taken to his local hospital by paramedics.
On examination, his cardiovascular examination was normal.
Learning Objectives
-
•
To be able to differentiate between normal and anomalous coronary artery anatomy.
-
•
To appreciate that an anomalous coronary artery can complicate the diagnosis and treatment of STEMI.
-
•
To understand the role of coronary CTA in differentiating between benign and malignant CAAs.
Past Medical History
He had hypercholesterolemia and was taking 40 mg of atorvastatin, and he was a smoker with 30-pack-year history. He had no other risk factors for ischemic heart disease.
Differential Diagnosis
The combination of cardiac risk factors and the acute onset of exertional chest pain raised the possibility of an acute coronary syndrome.
Investigations
His initial electrocardiogram showed anterior ST-segment elevation with reciprocal inferior ST-segment depression. His high-sensitivity troponin I level was 61 ng/l (normal range 0 to 35 ng/l).
Management
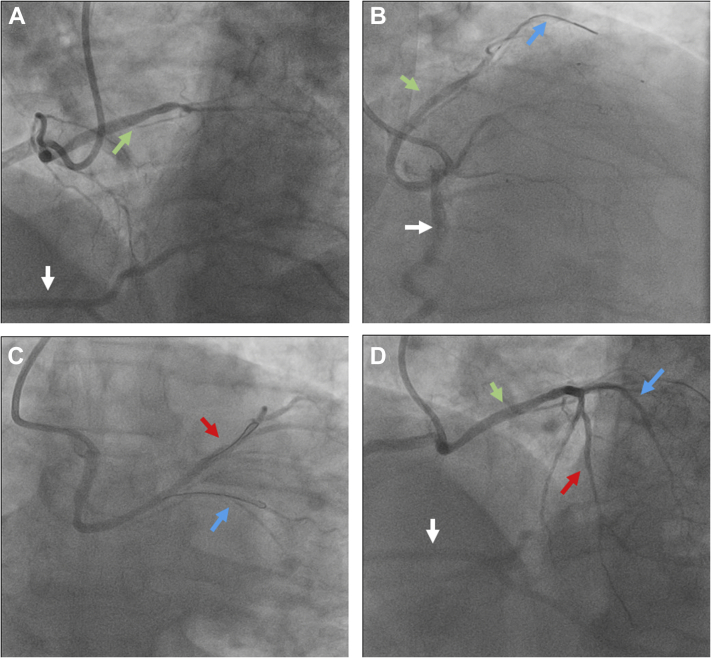
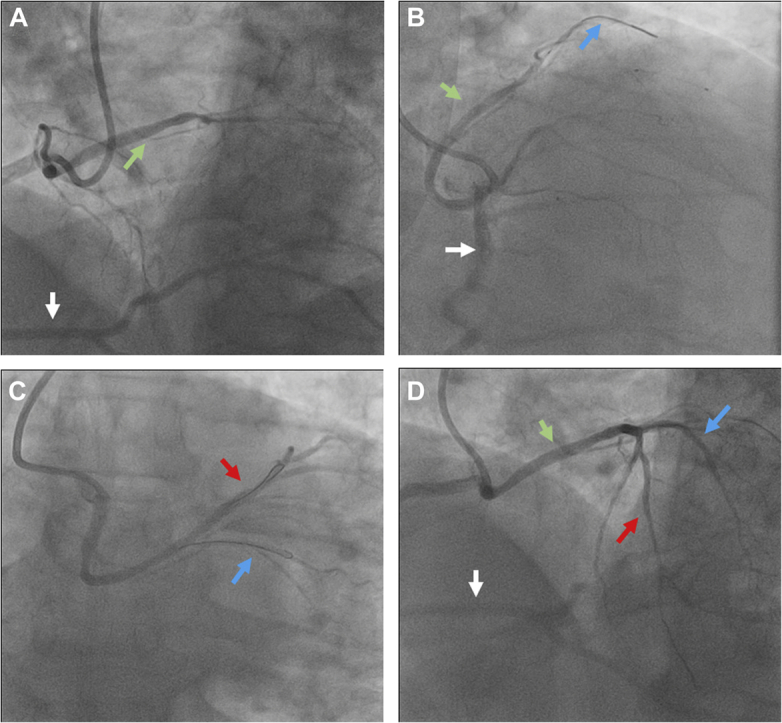
The patient was transferred to our center (Harefield Hospital, Uxbridge, United Kingdom) for consideration of primary percutaneous coronary intervention (PCI). On arrival, he was still in pain. A bedside echocardiogram showed good left ventricular function with anterior hypokinesia. Emergency left-sided heart catheterization was performed using right radial artery access. This showed that both the left coronary arteries and the right coronary artery (RCA) had a common origin from the right coronary sinus (Figure 1A, Video 1A). The culprit lesion was in the proximal left anterior descending artery (LAD), with a Thrombolysis in Myocardial Infarction score of 2 (Figure 1B, Video 1B). The other arteries were unobstructed. Initially, it was challenging to identify the coronary arteries in the context of the anomaly. We proceeded to pre-dilate the LAD lesion (Figure 1C, Video 1C) with 2.0 × 20 mm and 2.5 × 20 mm semicompliant balloons at 16 atm and then stent with a 2.75 × 23 mm Xience Sierra (Abbott Laboratories, Abbott Park, Illinois) at 18 atm, with a good angiographic result (Figure 1D, Video 1D).
Figure 1.
Invasive Coronary Angiography Images Pre-, During, and Post-LAD Stent
Images in the (A and D) cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery (green arrows) originating from the right coronary artery (white arrows) where it bifurcates into the left anterior descending (LAD) (red arrows) and left circumflex (blue arrows) arteries. (C and D) The left anterior descending artery after stent insertion.
Post-procedure, he was prescribed dual antiplatelet therapy with ticagrelor for 1 year and aspirin for life, as well as other secondary prevention medications, including bisoprolol and ramipril. He was given smoking cessation advice. His peak high-sensitivity troponin I level was 10,644 ng/l (normal range <19.8 ng/l). A departmental echocardiogram showed a left ventricular ejection fraction of 49%, with hypokinesia of the lateral, apical, anteroseptal, and anterior wall. He was discharged after 48 h in the hospital.
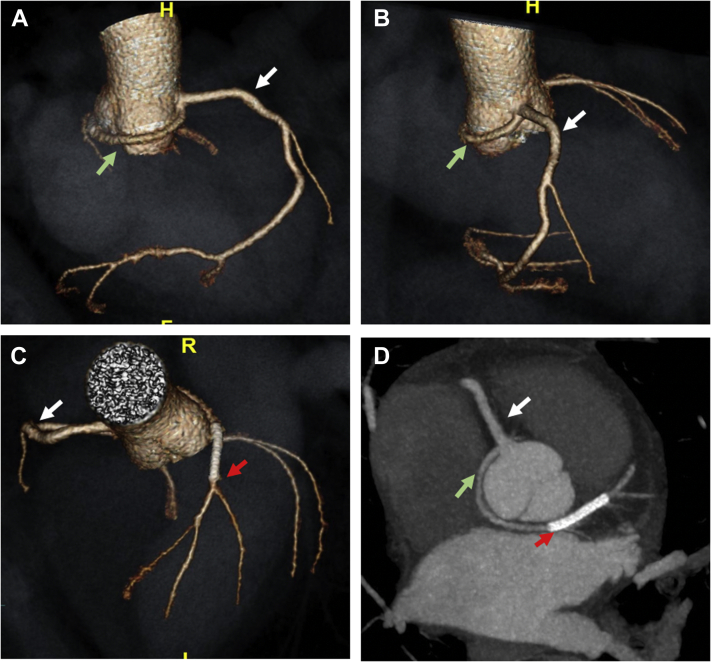
Given the anomalous anatomy of the coronary arteries, coronary computed tomography angiography (CTA) was performed as an outpatient procedure. This showed that the RCA arose from the right coronary sinus and was dominant (Figures 2A and 2B). The left main coronary artery arose from the inferior aspect of the RCA ostium (Figure 2B). It went posterior and inferior to the aortic root, thus suggesting a benign course. The left main coronary artery subsequently emerged on the left side of the aortic root and divided into the LAD and circumflex arteries with a normal course (Figure 2C). The recent stent was noted in the distal part of the long left main coronary artery extending into the proximal segment of the LAD (Figure 2D). The aortic root, parts of thoracic aorta, and aortic and mitral valves appeared morphologically normal.
Figure 2.
Coronary CTA 3D Volume-Rendered Images of Coronary Anatomy Course
Coronary computed tomography angiography (CTA) images in the (A) right anterior oblique projection, (B) posterior view, and (C) cranial view demonstrating the anomalous origin of the left main coronary artery (green arrow in B) from the inferior aspect of the right coronary artery ostium, taking a course posterior to the aortic root (green arrow in A) and emerging in the anterior interventricular groove (red arrow in C). The dominant right coronary artery is shown (white arrows in A to D). (D) Multiplanar image also demonstrating the same features. 3D = 3-dimensional; H = head; R = right.
Discussion
Coronary artery anomalies (CAAs) have been described extensively in published reports (1). Several groups have tried to clarify various fundamental issues in the study of CAAs, including definitions, classification, incidence, pathophysiological mechanisms, and clinical relevance of each anomaly (2). This information is crucial because CAA is the second most common cause of sudden cardiac death in young competitive athletes (3).
To define a CAA, it is vital to have definite morphological criteria to describe normal coronary arteries (3). Angelini (1,2) suggested such criteria using numerous morphological features, including number of ostia, location, course, and branches. Every “normal” feature, including normal anatomic variants, has >1% of frequency in an unselected population (2). By definition, a CAA is defined as a morphological feature found in <1% of the population (1,2).
According to published reports, CAA affects approximately 1% of the general population and 0.3% to 5.6% in studies of patients undergoing coronary angiography (2,4). This variability in incidence is likely a reflection of referral bias and the definition specificity of abnormal and normal (2).
The most detailed and accurate classification was proposed by Angelini (1,2) and is based on anatomic features. This classification can be categorized as follows: 1) anomalies of origination and course of coronary arteries; 2) anomalies of intrinsic coronary anatomy; 3) anomalies of coronary artery termination; and 4) anomalous collateral vessels (1,2).
Our case can be described as anomalous origination of a coronary artery from the opposite sinus constituting a single coronary artery; this CAA has an incidence of approximately 0.1% (1, 2, 3, 4, 5). An anomalous left coronary artery arising from the right coronary sinus is very rare, with a reported prevalence of 0.02% to 0.05% on angiographic studies (4). Although the origin of the artery is ectopic, it is the course that the abnormal coronary artery takes to its perfusion territory that is problematic (5).
The 5 potential paths taken by the abnormal coronary artery can be described as follows: pre-pulmonic, anterior to the right ventricular outflow tract; retroaortic, posterior to the aortic root; transseptal, through the proximal interventricular septum, analogous to a right superior septal perforator; interarterial, between the aorta and the pulmonary artery; or retrocardiac, behind the mitral and tricuspid valves in the posterior atrioventricular grove (2,5).
Pre-pulmonic and retroaortic (our case) courses are categorized as benign CAAs, with little risk associated with the condition (5). An interarterial course, however, is associated with up to a 30% risk of sudden cardiac death, for unclear reasons (5). A retrocardiac course is thought to make the individual more prone to atherosclerosis (2).
Unless patients have presented in early life with angina, the discovery of the CAA in patients with acute coronary syndrome is incidental (2). To date, there is only 1 other reported case of a patient presenting with 1) an anterior ST-segment elevation myocardial infarction (STEMI) from 2) a culprit lesion in the LAD that is anomalous with the 3) left coronary artery arising from the right coronary sinus (6). Performing PCI in patients with CAAs is challenging and carries an increased risk of ostial dissection (6).
Coronary CTA is currently regarded as the diagnostic standard. In fact, the prevalence of CAAs noted on coronary CTA is substantially higher than with coronary angiography, a finding suggesting possible underdiagnosis if only invasive angiography is used (7).
Follow-Up
The patient was symptom free at his 6-week post–primary PCI appointment and was discharged.
Conclusions
CAAs are rare anatomic variants. We presented the second case of an incidental finding of an anomalous left coronary artery originating from the right coronary sinus in the setting of an anterior STEMI. Coronary CTA is a standard diagnostic tool to differentiate between a benign and a malignant course.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For a supplemental video, please see the online version of this article.
Contributor Information
Prina Rajani, Email: prina.rajani@nhs.net.
Wala Mattar, Email: w.mattar@rbht.nhs.uk.
Appendix
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
References
- 1.Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007;115:1296–1305. doi: 10.1161/CIRCULATIONAHA.106.618082. [DOI] [PubMed] [Google Scholar]
- 2.Angelini P. Coronary artery anomalies – current clinical issues: definitions, classification, incidence, clinical relevance, treatment guidelines. Tex Heart Inst J. 2002;29:271–278. [PMC free article] [PubMed] [Google Scholar]
- 3.Kastellanos S., Aznaouridis K., Vlachopoulos C. Overview of coronary artery variants, aberrations and anomalies. World J Cardiol. 2018;10:127–140. doi: 10.4330/wjc.v10.i10.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villa A.D., Sammut E., Nair A. Coronary artery anomalies overview: the normal and the abnormal. World J Radiol. 2016;8:537–555. doi: 10.4329/wjr.v8.i6.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young P.M., Gerber T.C., Williamson E.E. Cardiac imaging: part 2, normal, variant, and anomalous configurations of the coronary vasculature. AJR Am J Roentgenol. 2011;197:816–826. doi: 10.2214/AJR.10.7249. [DOI] [PubMed] [Google Scholar]
- 6.Tyczyński P., Kukula K., Pietrasik A. Anomalous origin of culprit coronary arteries in acute coronary syndromes. Cardiol J. 2018;25:683–690. doi: 10.5603/CJ.a2017.0142. [DOI] [PubMed] [Google Scholar]
- 7.Ghadri J.R., Kazakauskaite E., Braunschweig S. Congenital coronary anomalies detected by coronary computed tomography compared to invasive coronary angiography. BMC Cardiovasc Disord. 2014;14:81. doi: 10.1186/1471-2261-14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.
Invasive Coronary Angiogram Videos Pre-, During-, and Post-LAD Stent, Coronary angiography in (A and D) the cranial right anterior oblique projection, (B) the cranial left anterior oblique projection, and (C) the caudal right anterior oblique projection demonstrating the left main coronary artery originating from the right coronary artery where it bifurcates into left anterior descending (LAD) and left circumflex arteries. (C and D) The left anterior descending artery after stent insertion.