Health care systems in industrialized countries are built around acute health problems (Etzwiler, 1997). This approach is successful when the goal is to improve or overcome pathologies that result in severe health issues or death. With the recent tremendous improvement of the treatments of life-threatening conditions, the clinical focus has moved from short term results to the overall expected quality of life and long-term outcomes. Unfortunately, the new objectives imply to consider a multitude of interacting processes and variables. In fact, a complex interplay of biological systems (nervous, immune, and endocrine) works together in an integrated and synergistic way to deal with a constantly evolving environment, determining our physical, behavioral, and psychological/subjective conditions. This interplay is the mechanism that allows us to adapt promptly and appropriately to circumstances, the key feature for successful living.
It can happen that the balance among these operating systems breaks. At that time, we can no longer function properly, and this condition could manifest itself as a physical illness, psychiatric disorder, or cognitive impairment. The symptomatology may be specific to a system, but the underlying causes are often multiple and interconnected. For example, stressful events may exacerbate a chronic inflammatory systemic disease, demonstrating the role of stress hormones and neurotransmitters in these diseases (Cutolo et al., 2006). In a striking manifestation of the overlap of contributions between systems, hemiplegia spares the paretic side from inflammatory signs and symptoms, supporting an important role of the nervous system in propagating inflammation (Miller et al., 1999). Insights are also offered by the interaction and overlap between different levels of functioning. Cognitive performances may significantly be affected by psychological state, but also by physical activity and nutrition (Reginato et al., 2000). Psychiatric disorders reflect biological and neurological vulnerabilities. Finally, psychological dysfunctions may exacerbate a physical illness, and temperamental attitudes may determine the course and the prognosis of the disease. In this scenario, the former model of treatment based on symptoms is no longer optimal because it lacks a global view of these dynamical interactions and the underlying mechanisms.
Even if the urge of a synergistic approach is evident and promoted in multiple medical disciplines, its application is strongly dependent on the local and ultra-local (i.e., each department of the same hospital) medical environment. The result is that still today, health professionals communicate poorly with each other. The majority of them work alone in their specialistic field; even those who usually adopt a multidisciplinary approach often just aggregate several disciplines rather than facilitate reciprocal enrichment. So it often happens that advances in a field go ahead without communicating with related fields, thus precluding the possibility of sharing useful scientific discoveries in favor of over-specialization (Figure 1).
Figure 1.
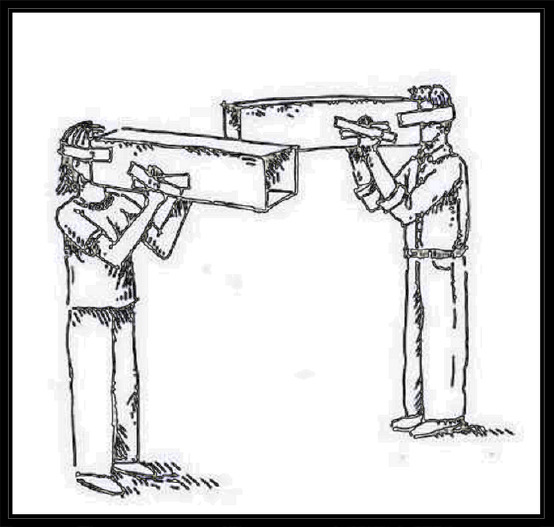
Tunnel vision.
A subtle side effect of poor communication and over-specialization is that some fields can be neglected in favor of “trendy” domains, and neuroscience is not spared. Studies on high-order cognitive functions have historically focused on the cerebral cortex. This phenomenon has been called “corticocentric myopia” because scarce attention was given to other cerebral structures such as white matter. However, it is well known that white matter is critical in the organization of the distributed neural networks. Researchers have thus underestimated the extent to which structural connectivity determines the properties of functional connectivity. It also exhibits plasticity, the capacity to induce brain modifications by experience. White matter’s plasticity properties have been reported, but studies investigating the effect of interventions and rehabilitation are still rare. In our experience with neonates and children, we tried a transversal approach to describe how very different diseases (e.g., prematurity and congenital heart diseases) could be crossed by a fil rouge of white matter instability that leads to common neurodevelopmental deficits (Cainelli et al., 2020). Despite their cross-disease peculiarity, every patient group can benefit from what is more broadly known about white matter. The great challenge is to understand how to use identified mechanisms in intervention programs to provide therapeutic benefits beyond a specific target to everyday life. Preterm birth patients can benefit from constant, gentle, pre-birth, and early post-natal care; the congenital heart disease’s perioperative window requires careful and rapidly adaptive management, and asphyxiated patients could likely benefit from the development of more effective drugs. A combination of biomarkers and constant, non-invasive monitoring can help in disease assessment, staging, and evaluation of a therapy’s effectiveness. A close neurodevelopmental follow-up would provide an objective tool to assess the injury and the stage of recovery of every child. All these aspects are a burden that requires the tight collaboration of professionals in different fields, psychologists, neuro-radiologists, and biologists, to try to have a global view at the problem and ultimately to look for common solutions. With this perspective, integrated approaches and efforts between several professionals can contribute to improving the management of patients (Suppiej et al., 2015; Vedovelli et al., 2019; Vaccaro et al., 2020). From an individual point of view, it allows scholars to avoid focusing only on a partial manifestation of the problem, which would bring to distorting fragments instead of the overall picture, allowing misconceptions to emerge.
Furthermore, if current knowledge determines professionals’ choices rather than guides their diagnostic and inferential process, patients with poorly explored conditions may lack provision. An illustrative example is the autonomic nervous system. Since the 1990s, the autonomic nervous system’s role in health and people’s psychological functioning has been postulated (Porges, 1995). In Polyvagal Theory, Porges (1995) theorized that through stages of phylogeny (immobilization, mobilization, and communication), the autonomic nervous system has evolved to support social behavior through the myelinated branch of the vagus cranial nerve, the more recently developed of the nerve’s two main branches. In confirmation, the autonomic nervous system is intricately connected to higher brain systems involved in emotional and psychological aspects. Therefore, the early disruption of autonomic development may significantly influence the autonomic system’s developmental trajectory, limiting its capacity to respond to physiologic changes and environment and determining a vulnerability to later neuropsychiatric disorders (Mulkey and du Plessis, 2019). Although a striking amount of data have confirmed this first theory, it is actually neglected in clinical practice. From a physical perspective, the autonomic nervous system is implicated in a wide range of conditions, from bone density, healing rates, gastrointestinal control, immunity, growth, behavior, and psychological dysfunctions (Rees, 2014). Since the autonomic nervous system is transversal to numerous specialties, patients may fit nowhere.
The complexity characterizing the symptomatology and the interactions of this system could be, in part, responsible for the insufficient attention put to it.
Given that dysfunctions in the autonomic nervous system can take different forms, the risk is to manage each symptom as isolated. Early insults in infancy, such as perinatal asphyxia or a traumatic experience, deeply impact multiple systems’ development and cannot merely be based on specific interventions targeted on the primary condition’s manifestation. For example, neural plasticity requests prompt cognitive intervention, but also a modulation of stress responses upregulated by targeted interventions on the autonomic nervous system. The familial context cannot be neglected: infants depend on parents, and they influence all aspects of child development and personality. Since young people rely on others’ feedback in building self-perception, misattribution matters. Furthermore, the protection of the early attachment is important because it mediates the link.
In the absence of these cautions, the immature system of, for example, a premature infant influenced by antenatal stress or unpredictable pain and hyper-stimulation under neonatal intensive care may develop autonomic dysregulation. This could transform adaptive responses to dangers and then into inflexible and counterproductive behaviors. Without a comprehensive intervention, also targeted to regulate stress responses, a noisy school or supermarket may determine huge stress as this vulnerable child grows up, determining disorganized behavioral reactions. Without specific attention to adult counseling, parents can ignore the child’s needs and choose the environments that suit their regulatory capacity. In this context, what is usually provided is an intervention target to contain exaggerated behavioral reactions, both with medication and behavioral treatments. It should come as no surprise if the results are often suboptimal or simply switch into another problem.
This perspective is crucial in understanding the factors that drive training-induced changes, particularly in the early stages of development, when the maturing brain exhibits maximal learning potential. Plasticity is a transversal property of different systems, exploiting in the embryological, fetal, and perinatal periods. During these phases, the orchestrated interplay of the nervous, endocrine, and immune systems become imprinted for a lifetime. In determining the quality of life and long-term health status, proper neurodevelopment is a cornerstone. Although this has been recognized in animal research, studies in humans are still rare and mainly epidemiological.
An integrated approach should encourage greater communication between professionals dealing with different life phases. Abnormal neurodevelopment has a clear relapse even in adulthood and elderly, but patients are not accompanied in the transition, and services dealing with transition programs are still rare. In our vision, the global approach should be organized with clear and realistic medical and developmental objectives, executed in synergy by different health specialists, targeted and tailored for each population of interests identified on achievable goals, regardless of the condition that generated the impairment. Probably our vision is biased by our background, but we think that since optimal neurodevelopment is crucial to a satisfactory and independent life, a well and widely trained neuropsychiatrist or psychologist could be the organizer and keystone of all the approaches. Given their education, these professionals have broad training that allows them to embrace a global overview of the different levels of human functioning - physical, behavioral, and psychological/subjective. Child neuropsychiatry and psychology are complex health disciplines because they reflect the multiple and multiform aspects of child’s development. The founding element is the impossibility of distinguishing, both in normal and pathological development, one function from another, the “mens” from the body, always considering the great influence of environmental and contextual elements. Separate these aspects, considering them as fields of intervention of different specialties, would lead to serious distortions in the diagnosis, treatment, and rehabilitation of individuals in their developmental age. Hence the need for their organizer role of the integrated network of health and social services preventing the transformation of discomfort into disorder and disorder and disabilities into handicaps.
In this way, she will help ease the burden of all the other professionals, making collaboration and exchange efficient. A well-organized integrated approach, after the first period of settlement, was demonstrated to be efficient and effective in the management of patients with chronic conditions. Thus, the initial investment would repay itself in the mid-long period. For example, Cumming (2011) described the real possibility of transforming highly fragmented, poorly coordinated services in an integrated continuum of care. They point out that policies are only the first step of integration that could facilitate the adoption of integrated services, but they are not enough unless changes on how services are actually delivered take places. In summary, the pipeline of integration should smoothly follow the policy/managers/providers axis where each one step should facilitate the other with reciprocal feedback. Moreover, more than 20 years ago, Leutz (1999) outlined what is the path to follow to obtain results from integrated care: integration is not for all and it costs before it pays. We think that neuroscience is probably one of the best examples where professionals’ integration would produce a tangible improvement in patient outcomes and satisfaction, also considering that today the integration is facilitated by the development of informatic tools able to ease the burden of data sharing and updating among providers.
Footnotes
Copyright license agreement:The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
C-Editors: Zhao M, Song LP; T-Editor: Jia Y
References
- 1.Cainelli E, Arrigoni F, Vedovelli L. White matter injury and neurodevelopmental disabilities: a cross-disease (dis)connection. Prog Neurobiol. 2020;193:101845. doi: 10.1016/j.pneurobio.2020.101845. [DOI] [PubMed] [Google Scholar]
- 2.Cumming J. Integrated care in New Zealand. Int J Integr Care. 2011;11:e138. doi: 10.5334/ijic.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cutolo M, Straub RH, Chrousos GP. Stress and autoimmunity. Neuroimmunomodulation. 2006;13:5–6. doi: 10.1159/000104855. [DOI] [PubMed] [Google Scholar]
- 4.Etzwiler DD. Chronic care: a need in search of a system. Diabetes Educ. 1997;23:569–573. doi: 10.1177/014572179702300509. [DOI] [PubMed] [Google Scholar]
- 5.Leutz WN. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Q. 1999;77:77–110, iv-v. doi: 10.1111/1468-0009.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller LE, Wessinghage D, Müller-Ladner U, Schölmerich J, Falk W, Kerner T, Straub RH. In vitro superfusion method to study nerve-immune cell interactions in human synovial membrane in long-standing rheumatoid arthritis or osteoarthritis. Ann N Y Acad Sci. 1999;876:266–275. doi: 10.1111/j.1749-6632.1999.tb07649.x. [DOI] [PubMed] [Google Scholar]
- 7.Mulkey SB, du Plessis AJ. Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatr Res. 2019;85:120–126. doi: 10.1038/s41390-018-0155-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Porges SW. Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology. 1995;32:301–318. doi: 10.1111/j.1469-8986.1995.tb01213.x. [DOI] [PubMed] [Google Scholar]
- 9.Rees CA. Lost among the trees? The autonomic nervous system and paediatrics. Arch Dis Child. 2014;99:552–562. doi: 10.1136/archdischild-2012-301863. [DOI] [PubMed] [Google Scholar]
- 10.Reginato E, Azzolina D, Folino F, Valentini R, Bendinelli C, Gafare CE, Cainelli E, Vedovelli L, Iliceto S, Gregori D, Lorenzoni G. Dietary and lifestyle patterns are associated with heart rate variability. J Clin Med. 2020;9:1121. doi: 10.3390/jcm9041121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suppiej A, Cainelli E, Cappellari A, Ermani M, Sartori S, Bisiacchi PS. Neonatal cortical auditory evoked potentials are affected by clinical conditions occurring in early prematurity. J Clin Neurophysiol. 2015;32(5):419–423. doi: 10.1097/WNP.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 12.Vaccaro MG, Sarica A, Quattrone A, Chiriaco C, Salsone M, Morelli M, Quattrone A. Neuropsychological assessment could distinguish among different clinical phenotypes of progressive supranuclear palsy: A Machine Learning approach. J Neuropsychol. 2020 doi: 10.1111/jnp.12232. doi: 101111/jnp12232. [DOI] [PubMed] [Google Scholar]
- 13.Vedovelli L, Cogo P, Cainelli E, Suppiej A, Padalino M, Tassini M, Simonato M, Stellin G, Carnielli VP, Buonocore G, Longini M. Pre-surgery urine metabolomics may predict late neurodevelopmental outcome in children with congenital heart disease. Heliyon. 2019;5:e02547. doi: 10.1016/j.heliyon.2019.e02547. [DOI] [PMC free article] [PubMed] [Google Scholar]


