Abstract
Background
Identifying the key determinants of vaccine uptake in the context of coronavirus disease 2019 (COVID-19) is critical to increasing vaccination rates, especially for Medicare beneficiaries.
Objective
We examined how the source of COVID-19 information shapes perceptions of COVID-19 severity and the likelihood of COVID-19 vaccine uptake among Medicare beneficiaries.
Design, Setting, and Participants
We included 6478 Medicare beneficiaries from the Fall 2020 Medicare Current Beneficiary Survey COVID-19 Supplement.
Main Measures
Our dependent variables were perception of COVID-19 severity and the likelihood of getting a COVID-19 vaccine. Our key independent variable was the beneficiaries’ primary source of information about COVID-19 and included six mutually exclusive categories: traditional news sources, guidance from government officials, social media, other webpages/Internet, friends or family members, or health care providers.
Key Results
Compared to those relying on traditional news sources or guidance from governmental officials, those relying on other sources had lower perceptions of COVID-19 severity and lower likelihood of getting a COVID-19 vaccine. Those relying on social media had the lowest levels in all measures (65.5% for those who agreed that COVID-19 is more contagious than the flu, 62.1% for those who agreed that COVID-19 is more deadly than the flu, 87.8% for those who agreed that all should take COVID-19 precautions, and 43.3% for those who answered that they would get a COVID-19 vaccine). The likelihood of COVID-19 vaccine uptake was also low among those relying on health care providers (55.5%). These findings remained similar even after adjusting for perceptions of COVID-19 severity in the relationship between the source of COVID-19 information and the likelihood of COVID-19 vaccine uptake.
Conclusions
The primary source of information that Medicare beneficiaries used to learn about COVID-19 may play a critical role in shaping perceptions of COVID-19 severity and attitudes toward getting a COVID-19 vaccine.
KEY WORDS: COVID-19, vaccine uptake, risk perception, source of information, Medicare
A vaccine for coronavirus disease 2019 (COVID-19) has been developed and distributed at an unprecedented rate, but there are concerns about vaccine hesitancy and its impact on vaccine uptake. According to a survey of US adults conducted in November 2020, about 63% said they would get a COVID-19 vaccine if one were available today.1 This rate is close to an actual uptake rate of COVID-19 vaccines. As of June 2021, a majority of the total US adult population have been fully vaccinated and two-thirds have received at least one dose of a vaccine.2 However, evidence suggests that COVID-19 vaccination rates have started to level off. The 7-day average of newly administered doses of COVID-19 vaccines peaked in early April at more than three million COVID-19 doses per day, but has fallen below one million per day for the first time since January 2021.3
Identifying the key determinants of vaccine uptake in the context of COVID-19 is critical to increasing vaccination rates. Prior research has investigated predictors of COVID-19 vaccine uptake among US adults and found that several demographic and socioeconomic factors were associated with the likelihood of COVID-19 vaccine uptake.4–7 In addition, where people get their information from has been shown to be a key determinant of vaccine attitudes and uptake more broadly.8 This suggests that access to credible information sources may play a role in influencing risk perceptions, which may in turn shape attitudes toward COVID-19 vaccination. Recent research from an Internet survey panel found that the likelihood of COVID-19 vaccine uptake was lower among those who relied on social media for virus information compared to those who did not, as well as among those who watched Fox News for virus information compared to those who watched CNN/MSNBC.4
However, existing evidence is limited in a number of ways. First, prior studies have examined the association of the source of information and vaccine uptake—there is a limited understanding of the underlying mechanism and the interplay between the source of information, risk perceptions, and vaccine uptake. Second, few population-based samples in recent studies limit the generalizability of findings. Third, when population-based samples were examined, the focus was on the entire US adult population. Our study adds to this research by focusing on Medicare beneficiaries those who are of high policy relevance as many of them are the most susceptive to COVID-19 mortality. Indeed, evidence suggests that the risk and severity of COVID-19 illness increases with age and/or baseline health status, leading to high case-fatality rates.9
Using newly released nationally representative data from Medicare beneficiaries, we examined the role of the source of COVID-19 information in shaping perceptions of COVID-19 severity and the likelihood of COVID-19 vaccine uptake. Specifically, we investigated whether the primary source of information about COVID-19 was associated with perception of COVID-19 severity and the likelihood of COVID-19 vaccine uptake (if available). Furthermore, we examined whether the primary source of COVID-19 information was associated with the likelihood of COVID-19 vaccine uptake, independent of perception of COVID-19 severity. We also examined whether perceived COVID-19 severity was associated with the likelihood of getting a COVID-19 vaccine.
METHODS
Data
We used data from the Fall 2020 Medicare Current Beneficiary Survey (MCBS) COVID-19 Supplement, which were collected via a telephone survey between October and November 2020.4 The MCBS is a nationally representative, longitudinal survey of Medicare beneficiaries and has been collecting data on Medicare beneficiaries for over 25 years. The data combine information from Medicare claims and administrative data with an interview survey. The MCBS COVID-19 Supplement collect additional information to better understand how Medicare beneficiaries experienced with the COVID-19 pandemic (e.g., beneficiaries’ perceptions of COVID-19 and vaccine uptake) (see the data user’s guide for more details). The MCBS COVID-19 Supplement have been used in multiple studies.10–12
Using the data, we identified all Medicare beneficiaries who were continuously enrolled in Medicare from the beginning of 2020 and living in the community in Fall 2020 and had complete information.
This study was exempted from review and informed consent by the institutional review board of Drexel University because the data were deidentified and publicly available. Reporting followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Variables
We examined four dependent variables—three measured perceived severity and one the likelihood of getting the vaccine. The three measures of perceived COVID-19 severity, all with response categories using a 5-point scale ranging from strongly agree to strongly disagree, included “Coronavirus is more contagious than the flu,” “Coronavirus is more deadly than the flu,” and “it is important for everyone to take precautions to prevent the spread of the Coronavirus, even if they are not in a high-risk group.” These measures were sources from the University of California Irvine’s COVID-19 Outbreak Study.13 We categorized responses as agreed (strongly agree or agree) or not (neither agree nor disagree, disagree, or strongly disagree). Since these variables may influence the likelihood of COVID-19 vaccine uptake while being influenced by the primary source of the COVD-19 information, we also used these variables as a mediator. Second, we included the likelihood of COVID-19 vaccine uptake if available. Beneficiaries were asked to rate the following statement using a 5-point scale: “If a vaccine that protected you from coronavirus was available to everyone who wanted it, would you get it?” We categorized into two levels: yes (definitely or probably) or no (not sure, probably not, or definitely not).
Our key independent variable was the beneficiaries’ primary source of information about COVID-19. Beneficiaries were asked the following question: “which of these sources (do you/does he/does she) rely on most for information about the coronavirus?” The following six mutually exclusive categories were given: traditional news sources (television, radio, news websites, and/or newspapers), guidance from government officials, social media, other webpages/Internet (excluding news websites), friends or family members, or health care providers. This variable was sourced from the March 2020 Associated Press-NORC Center Poll.13
We also included the following individual-level demographic, socioeconomic, and health-related characteristics: age (< 65, 65–74, or 75+ years), gender (male or female), race/ethnicity (non-Hispanic white, Hispanic, non-Hispanic black, or other), income (≥ $25,000 or < $25,000), rural residence (rural or urban), census region of residence (Northeast, Midwest, South, or West), insurance (enrollment in both Medicare and Medicaid or enrollment in privately run Medicare known as Medicare Advantage), use of other language at home other than English (yes or no), having a particular place for medical care (yes or no), self-reported health conditions (hypertension, myocardial infarction, congestive heart failure, stroke, high cholesterol, cancer, Alzheimer’s disease/dementia, depression, osteoporosis, broken hip, emphysema/asthma/chronic obstructive pulmonary disease, diabetes, or weak immune system), smoking status (current smoker, former smoker, or never smoked), and the date of interview (week of October 4, 2020; week of October 11, 2020; week of October 18, 2020; week of October 25, 2020; week of November 1, 2020; or November 8 to 15, 2020). We included these variables as control variables because they are determinants of perception of COVID-19 severity and/or the likelihood of COVID-19 vaccine uptake.4–7,10–12 These variables were determined based on survey as well as administrative data.
Statistical Analysis
We first calculated descriptive statistics for dependent and independent variables. We also stratified dependent variables by primary source of COVID-19 information.
To examine whether the primary source of COVID-19 information was a determinant of perception of COVID-19 severity and the likelihood of COVID-19 vaccine uptake, we performed logistic regression while controlling for individual-level demographic, socioeconomic, and health-related variables described above. We then estimated the adjusted mean values of the dependent variable while holding the values of other variables at the same levels except the key independent variable. This allows for comparison of the dependent variable across groups that are similar across the set of control variables.
To examine whether the primary source of COVID-19 information was associated with the likelihood of COVID-19 vaccine uptake, independent of perception of COVID-19 severity, we conducted the analysis described above while additionally controlling for the three measures of perceptions of COVID-19 severity. Then, we calculated the adjusted mean values of the dependent variable by primary source of COVID-19 information. This may help us understand the mechanism that underlies an observed relationship between the primary source of COVID-19 information and the likelihood of COVID-19 vaccine uptake via perceptions of COVID-19 severity. Exploring a mediator is important because interventions can target treatment to address the mediator to help improve outcomes.
To examine the magnitude of the association between the likelihood of COVID-19 vaccine uptake and perception of COVID-19 severity, we estimated correlations. As the correlation coefficient measures the strength of the relationship between two variables, this enables us to straightforwardly understand how strongly the likelihood of COVID-19 vaccine uptake is associated with each measure of perceptions of COVID-19 severity without being influenced by other relevant variables.
For all analyses, we accounted for complex sample design with sampling weights provided by the MCBS to generate nationally representative estimates. For all analysis, STATA software version 11.0 (Stata Corp., College Station, TX, USA) was used and the statistical significance level was set at 0.05.
RESULTS
Our final sample included 6478 Medicare beneficiaries (weighted N = 39,591,268) (Table 1). While perceptions of COVID-19 severity were high across all three measures (85.6% to 97.3%), the likelihood of COVID-19 vaccine uptake was relatively low (61.6%). Traditional news sources were the most common source of COVID-19 information (53.6%), followed by health care providers (21.0%), guidance from governmental officials (8.6%), friends or family member (8.1%), other webpages/Internet (6.9%), and social media (1.8%).
Table 1.
Descriptive Statistics for Medicare Beneficiaries from the Fall 2020 Medicare Current Beneficiary Survey (MCBS) COVID-19 Supplement
| Variables |
N (%), N = 6478 and weighted N = 39,591,268 |
|---|---|
| Agree that COVID-19 is more contagious than flu | 5547 (85.6) |
| Agree that COVID-19 is more deadly than flu | 5544 (85.6) |
| Agree that all should take COVID-19 precautions | 6302 (97.3) |
| Would get a COVID-19 vaccine if available | 3989 (61.6) |
| Primary sources of COVID-19 information | |
| Traditional news sources | 3471 (53.6) |
| Guidance from governmental officials | 558 (8.6) |
| Social media | 115 (1.8) |
| Other webpages/Internet | 447 (6.9) |
| Friends or family members | 525 (8.1) |
| Health care providers | 1362 (21.0) |
| Age | |
| < 65 years | 1295 (20.0) |
| 65–74 years | 2437 (37.6) |
| 75+ years | 2746 (42.4) |
| Female | 3624 (55.9) |
| Race/ethnicity | |
| Non-Hispanic white | 4945 (76.3) |
| Hispanic | 625 (9.6) |
| Non-Hispanic black | 579 (8.9) |
| Other | 329 (5.1) |
| Income | |
| $25,000 or more | 2215 (34.2) |
| Less than $25,000 | 4263 (65.8) |
| Residence of rural areas | 5004 (77.2) |
| US census regions | |
| Northeast | 1197 (18.5) |
| Midwest | 1522 (23.5) |
| South | 2444 (37.7) |
| West | 1315 (20.3) |
| Insurance | |
| Enrollment in Medicare and Medicaid | 1131 (17.5) |
| Enrollment in Medicare Advantage | 2782 (42.9) |
| Use of other language at home other than English | 697 (10.8) |
| Having a particular place for medical care | 5941 (91.7) |
| Self-reported health conditions | |
| Hypertension | 4172 (64.4) |
| Myocardial infarction | 626 (9.7) |
| Congestive heart failure | 406 (6.3) |
| Stroke | 584 (9.0) |
| High cholesterol | 4285 (66.1) |
| Cancer | 1378 (21.3) |
| Alzheimer’s disease/dementia | 101 (1.6) |
| Depression | 1756 (27.1) |
| Osteoporosis | 1234 (19.0) |
| Broken hip | 211 (3.3) |
| Emphysema/asthma/COPD | 1250 (19.3) |
| Diabetes | 2142 (33.1) |
| Weak immune system | 1162 (17.9) |
| Smoking status | |
| Current smoker | 746 (11.5) |
| Former smoker | 3014 (46.5) |
| Never smoked | 2718 (42.0) |
| Interview date | |
| Week of October 4, 2020 | 1217 (18.8) |
| Week of October 11, 2020 | 1630 (25.2) |
| Week of October 18, 2020 | 1217 (18.8) |
| Week of October 25, 2020 | 1106 (17.1) |
| Week of November 1, 2020 | 835 (12.9) |
| November 8 to 15, 2020 | 473 (7.3) |
Abbreviations: COVID-19, coronavirus disease 2019; COPD, chronic obstructive pulmonary disease
Unadjusted descriptive statistics showed that compared to those relying on traditional news sources or guidance from governmental officials as a primary source of COVID-19 information, those relying on other sources had lower perceptions of COVID-19 severity and lower likelihood of COVID-19 vaccine uptake (Table 2). Those relying on social media were of particular interest because they had the lowest levels in all measures.
Table 2.
Unadjusted Descriptive Statistics for Dependent Variables by Primary Source of COVID-19 Information
| Primary sources of COVID-19 information, N (% of those with each primary source of COVID-19 information that agree each statement) | ||||||
|---|---|---|---|---|---|---|
| Dependent variables | Traditional news sources (N = 3471) | Guidance from governmental officials (N = 558) | Social media (N = 115) | Other webpages/Internet (N = 447) | Friends or family members (N = 525) | Health care providers (N = 1362) |
| Agree that COVID-19 is more contagious than flu | 3079 (88.7) | 487 (87.3) | 76 (66.1) | 335 (74.9) | 412 (78.5) | 1158 (85.0) |
| Agree that COVID-19 is more deadly than flu | 3084 (88.9) | 488 (87.5) | 78 (67.8) | 332 (74.3) | 406 (77.3) | 1156 (84.9) |
| Agree that all should take COVID-19 precautions | 3398 (97.9) | 548 (98.2) | 104 (90.4) | 413 (92.4) | 503 (95.8) | 1336 (98.1) |
| Would get a COVID-19 vaccine if available | 2254 (64.9) | 358 (64.2) | 49 (42.6) | 262 (58.6) | 289 (55.0) | 777 (57.0) |
Abbreviations: COVID-19, coronavirus disease 2019
Our logistic regression analysis showed that the primary source of COVID-19 information was a determinant of perception of COVID-19 severity and the likelihood of COVID-19 vaccine uptake (Table 3). Compared to those relying on traditional news sources as their primary source of COVID-19 information, those relying on social media, other webpages/Internet, friends or family member, or health care providers were significantly less likely to have high perception of COVID-19 severity (odds ratios [ORs] ranging from 0.22 [95% CI: 0.14–0.36] to 0.71 [95% CI: 0.57–0.88] for those who agreed that COVID-19 is more contagious than the flu (model 1), ORs ranging from 0.19 [95% CI: 0.11–0.32] to 0.66 [95% CI: 0.53–0.83] for those who agreed that COVID-19 is more deadly than the flu (model 2), and ORs ranging from 0.16 [95% CI: 0.07–0.37] to 0.42 [95% CI: 0.24–0.73] for those who agreed that all should take COVID-19 precautions (model 3)). In model 4, compared to those relying on traditional news sources as their primary source of COVID-19 information, the likelihood of COVID-19 vaccine uptake was significantly lower among those relying on social media (OR = 0.40 [95% CI: 0.25–0.65]), other webpages/Internet (OR = 0.69 [95% CI: 0.53–0.88]), friends or family member (OR = 0.75 [95% CI: 0.59–0.95]), or health care providers (OR = 0.68 [95% CI: 0.58–0.80]). However, no significant associations were found among those relying on guidance from governmental officials in all outcomes.
Table 3.
Odds Ratio Estimates for Perception of COVID-19 Severity and Likelihood of Getting a COVID-19 Vaccine
| Odds ratio (95% confidence interval)* | |||||
|---|---|---|---|---|---|
| Variables | Model 1: Agree that COVID-19 is more contagious than flu† |
Model 2: Agree that COVID-19 is more deadly than flu† |
Model 3: Agree that all should take COVID-19 precautions† |
Model 4: Would get a COVID-19 vaccine if available‡ |
Model 5: Would get a COVID-19 vaccine if available‡ |
| Primary sources of COVID-19 information | |||||
| Traditional news sources§ | Ref | Ref | Ref | Ref | Ref |
| Guidance from governmental officials | 0.83 (0.59 to 1.16) | 0.85 (0.61 to 1.19) | 1.70 (0.74 to 3.92) | 0.90 (0.71 to 1.14) | 0.91 (0.72 to 1.15) |
| Social media | 0.22 (0.14 to 0.36) | 0.19 (0.11 to 0.32) | 0.16 (0.07 to 0.37) | 0.40 (0.25 to 0.65) | 0.52 (0.33 to 0.81) |
| Other webpages/Internet | 0.41 (0.30 to 0.56) | 0.40 (0.29 to 0.55) | 0.33 (0.19 to 0.57) | 0.69 (0.53 to 0.88) | 0.78 (0.60 to 1.00) |
| Friends or family members | 0.46 (0.34 to 0.63) | 0.39 (0.30 to 0.52) | 0.42 (0.24 to 0.73) | 0.75 (0.59 to 0.95) | 0.84 (0.66 to 1.07) |
| Health care providers | 0.71 (0.57 to 0.88) | 0.66 (0.53 to 0.83) | 1.24 (0.73 to 2.11) | 0.68 (0.58 to 0.80) | 0.70 (0.60 to 0.82) |
| Perception of COVID-19 severity | |||||
| Agree that COVID-19 is more contagious than flu | - | - | - | - | 1.39 (1.14 to 1.71) |
| Agree that COVID-19 is more deadly than flu | - | - | - | - | 1.71 (1.39 to 2.10) |
| Agree that all should take COVID-19 precautions | - | - | - | - | 1.59 (1.05 to 2.40) |
| Age | |||||
| <65 years | Ref | Ref | Ref | Ref | Ref |
| 65–74 years | 1.33 (1.02 to 1.72) | 1.25 (0.96 to 1.62) | 1.70 (0.96 to 3.01) | 1.36 (1.12 to 1.64) | 1.33 (1.10 to 1.61) |
| 75+ years | 1.37 (1.05 to 1.79) | 1.34 (1.02 to 1.76) | 1.75 (0.99 to 3.07) | 1.59 (1.31 to 1.93) | 1.54 (1.27 to 1.88) |
| Female | 1.35 (1.12 to 1.63) | 1.07 (0.89 to 1.30) | 1.49 (0.99 to 2.24) | 0.56 (0.48 to 0.64) | 0.54 (0.46 to 0.62) |
| Race/ethnicity | |||||
| Non-Hispanic white | Ref | Ref | Ref | Ref | Ref |
| Hispanic | 3.88 (2.09 to 7.22) | 4.84 (2.47 to 9.46) | 2.55 (0.71 to 9.18) | 0.45 (0.36 to 0.57) | 0.40 (0.31 to 0.50) |
| Non-Hispanic black | 2.29 (1.41 to 3.70) | 1.94 (1.00 to 3.76) | 4.56 (1.67 to 12.46) | 0.72 (0.53 to 0.99) | 0.67 (0.49 to 0.92) |
| Other | 1.39 (0.91 to 2.13) | 1.51 (0.98 to 2.32) | 1.96 (0.70 to 5.49) | 0.95 (0.70 to 1.28) | 0.90 (0.66 to 1.23) |
| Income | |||||
| $25,000 or more | Ref | Ref | Ref | Ref | Ref |
| Less than $25,000 | 0.82 (0.65 to 1.03) | 1.08 (0.85 to 1.36) | 0.80 (0.47 to 1.37) | 0.64 (0.54 to 0.75) | 0.64 (0.54 to 0.75) |
| Residence of rural areas | 0.70 (0.57 to 0.86) | 0.67 (0.55 to 0.82) | 1.23 (0.74 to 2.06) | 0.82 (0.70 to 0.96) | 0.85 (0.73 to 1.00) |
| US census regions | |||||
| Northeast | Ref | Ref | Ref | Ref | Ref |
| Midwest | 0.70 (0.53 to 0.93) | 0.65 (0.49 to 0.86) | 1.03 (0.56 to 1.88) | 1.03 (0.84 to 1.25) | 1.07 (0.87 to 1.31) |
| South | 0.62 (0.48 to 0.81) | 0.59 (0.45 to 0.77) | 0.69 (0.40 to 1.19) | 0.91 (0.76 to 1.10) | 0.96 (0.80 to 1.16) |
| West | 0.78 (0.57 to 1.06) | 0.72 (0.52 to 0.98) | 0.62 (0.34 to 1.15) | 1.11 (0.91 to 1.37) | 1.15 (0.93 to 1.42) |
| Insurance | |||||
| Medicaid | 1.18 (0.86 to 1.63) | 1.14 (0.81 to 1.60) | 1.61 (0.77 to 3.40) | 1.36 (1.09 to 1.70) | 1.35 (1.08 to 1.69) |
| Medicare Advantage | 1.05 (0.88 to 1.26) | 1.07 (0.89 to 1.29) | 1.51 (1.02 to 2.23) | 0.95 (0.84 to 1.08) | 0.94 (0.83 to 1.07) |
| Use of other language at home other than English | 0.97 (0.60 to 1.58) | 1.27 (0.71 to 2.28) | 0.84 (0.34 to 2.10) | 0.81 (0.61 to 1.07) | 0.80 (0.60 to 1.06) |
| Having a particular place for medical care | 1.02 (0.75 to 1.40) | 0.91 (0.68 to 1.24) | 0.70 (0.35 to 1.40) | 0.87 (0.70 to 1.08) | 0.87 (0.70 to 1.09) |
| Self-reported health conditions | |||||
| Hypertension | 1.30 (1.08 to 1.57) | 1.29 (1.07 to 1.54) | 1.56 (1.06 to 2.31) | 1.02 (0.88 to 1.17) | 0.98 (0.85 to 1.13) |
| Myocardial infarction | 1.03 (0.76 to 1.40) | 0.88 (0.65 to 1.19) | 0.81 (0.47 to 1.40) | 0.94 (0.75 to 1.17) | 0.95 (0.76 to 1.18) |
| Congestive heart failure | 1.02 (0.71 to 1.45) | 1.46 (1.02 to 2.09) | 2.79 (1.13 to 6.85) | 0.90 (0.70 to 1.17) | 0.87 (0.67 to 1.13) |
| Stroke | 0.89 (0.66 to 1.21) | 0.88 (0.64 to 1.22) | 0.86 (0.48 to 1.57) | 1.03 (0.82 to 1.28) | 1.04 (0.83 to 1.31) |
| High cholesterol | 0.98 (0.81 to 1.19) | 1.08 (0.90 to 1.31) | 0.74 (0.48 to 1.14) | 1.10 (0.95 to 1.26) | 1.10 (0.96 to 1.27) |
| Cancer | 1.03 (0.83 to 1.28) | 1.15 (0.93 to 1.42) | 0.78 (0.50 to 1.22) | 0.99 (0.85 to 1.16) | 0.98 (0.84 to 1.15) |
| Alzheimer’s disease/dementia | 0.87 (0.47 to 1.61) | 1.24 (0.64 to 2.38) | 0.54 (0.17 to 1.70) | 1.36 (0.82 to 2.24) | 1.37 (0.84 to 2.23) |
| Depression | 1.08 (0.87 to 1.34) | 1.09 (0.88 to 1.34) | 1.90 (1.12 to 3.22) | 1.14 (0.99 to 1.33) | 1.13 (0.97 to 1.31) |
| Osteoporosis | 1.12 (0.87 to 1.45) | 1.20 (0.94 to 1.53) | 1.19 (0.68 to 2.08) | 0.99 (0.84 to 1.17) | 0.98 (0.83 to 1.15) |
| Broken hip | 1.09 (0.69 to 1.74) | 1.58 (0.93 to 2.67) | 1.05 (0.41 to 2.67) | 0.91 (0.64 to 1.31) | 0.89 (0.61 to 1.29) |
| Emphysema/asthma/COPD | 0.86 (0.68 to 1.09) | 0.98 (0.77 to 1.23) | 0.61 (0.38 to 0.97) | 0.91 (0.77 to 1.07) | 0.92 (0.78 to 1.09) |
| Diabetes | 0.92 (0.76 to 1.11) | 0.90 (0.74 to 1.10) | 0.98 (0.66 to 1.47) | 0.85 (0.74 to 0.98) | 0.86 (0.75 to 0.99) |
| Weak immune system | 0.93 (0.74 to 1.19) | 0.86 (0.69 to 1.08) | 0.97 (0.58 to 1.63) | 1.09 (0.92 to 1.29) | 1.10 (0.93 to 1.31) |
| Smoking status | |||||
| Current smoker | Ref | Ref | Ref | Ref | Ref |
| Former smoker | 1.25 (0.95 to 1.65) | 1.24 (0.93 to 1.64) | 2.20 (1.28 to 3.79) | 1.30 (1.05 to 1.61) | 1.26 (1.02 to 1.57) |
| Never smoked | 1.16 (0.88 to 1.54) | 1.27 (0.95 to 1.70) | 2.21 (1.27 to 3.85) | 1.35 (1.08 to 1.69) | 1.31 (1.05 to 1.64) |
| Interview date | |||||
| Week of October 4, 2020 | Ref | Ref | Ref | Ref | Ref |
| Week of October 11, 2020 | 0.81 (0.61 to 1.07) | 0.92 (0.70 to 1.21) | 0.90 (0.50 to 1.61) | 0.98 (0.81 to 1.19) | 0.99 (0.82 to 1.20) |
| Week of October 18, 2020 | 0.80 (0.60 to 1.08) | 0.90 (0.67 to 1.21) | 1.43 (0.70 to 2.91) | 1.07 (0.87 to 1.31) | 1.08 (0.88 to 1.33) |
| Week of October 25, 2020 | 0.69 (0.51 to 0.94) | 0.81 (0.60 to 1.09) | 1.16 (0.59 to 2.26) | 1.00 (0.81 to 1.24) | 1.03 (0.83 to 1.28) |
| Week of November 1, 2020 | 0.70 (0.50 to 0.99) | 0.75 (0.53 to 1.05) | 0.73 (0.38 to 1.38) | 0.97 (0.77 to 1.22) | 1.01 (0.80 to 1.27) |
| November 8 to 15, 2020 | 0.67 (0.46 to 0.98) | 0.93 (0.63 to 1.37) | 0.95 (0.45 to 1.99) | 0.86 (0.65 to 1.13) | 0.87 (0.66 to 1.16) |
Abbreviations: COVID-19, coronavirus disease 2019; COPD, chronic obstructive pulmonary disease
*We accounted for complex sample design with sampling weights provided by the MCBS to generate nationally representative estimates
†Beneficiaries were asked to rate the following statements using a 5-point scale: “Coronavirus is more contagious than the flu,” “Coronavirus is more deadly than the flu,” and “it is important for everyone to take precautions to prevent the spread of the Coronavirus, even if they are not in a high-risk group.” We categorized responses as agreed (strongly agree or agree) or not (neither agree nor disagree, disagree, or strongly disagree)
‡Beneficiaries were asked to rate their answers on a 5-point scale, which we categorized into two levels: yes (definitely or probably) or no (not sure, probably not, or definitely not)
§Includes television, radio, websites, and/or newspapers
Boldface indicates statistical significance
In model 5, higher perceptions of COVID-19 severity were associated with higher likelihood of COVID-19 vaccine uptake (OR = 1.39 [95% CI: 1.14–1.71] for those who agreed that COVID-19 is more contagious than the flu, OR = 1.71 [95% CI: 1.39–2.10] for those who agreed that COVID-19 is more deadly than the flu, OR = 1.59 [95% CI: 1.05–2.40] for those who agreed that all should take COVID-19 precautions) (Table 3). Findings in model 5 remained substantively similar to those in model 4, even after adjusting for perceptions of COVID-19 severity. However, in model 5, significant associations were no longer observed among those relying on webpages/Internet or friends or family member as a primary source of COVID-19 information.
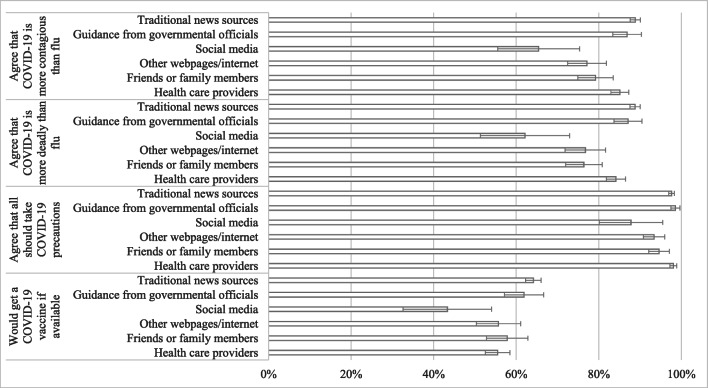
Our adjusted analysis showed that compared to those relying on traditional news sources or guidance from governmental officials as a primary source of COVID-19 information, those relying on other sources had lower perceptions of COVID-19 severity and lower likelihood of COVID-19 vaccine uptake (Fig. 1). Those relying on social media had the lowest levels in all measures (65.5% [95% CI: 55.5–75.4] for those who agreed that COVID-19 is more contagious than the flu, 62.1% [95% CI: 51.3–72.9] for those who agreed that COVID-19 is more deadly than the flu, 87.8% [95% CI: 80.1–95.5] for those who agreed that all should take COVID-19 precautions, and 43.3% [95% CI: 32.6–54.1] for those who answered that they would get a COVID-19 vaccine). Another notable finding was that the likelihood of COVID-19 vaccine uptake was also low among those relying on health care providers (55.5% [95% CI: 52.5–58.8]).
Figure 1.
Adjusted probabilities for perception of COVID-19 severity and likelihood of getting a COVID-19 vaccine if available by primary source of COVID-19 information. Adjusted rates and 95% confidence intervals (represented by the whiskers) were estimated using a logistic regression model while controlling for age, gender, race/ethnicity, income, rural residence, census region of residence, insurance, use of other language at home other than English, presence of a particular place for medical care, self-reported health conditions, smoking status, and interview date as well as the primary source of COVID-19 information. Using coefficients from the logistic regression model, we estimated the adjusted mean values of the outcome, holding the values of other covariates at the same levels. We accounted for complex sample design with sampling weights provided by the MCBS to generate nationally representative estimates.
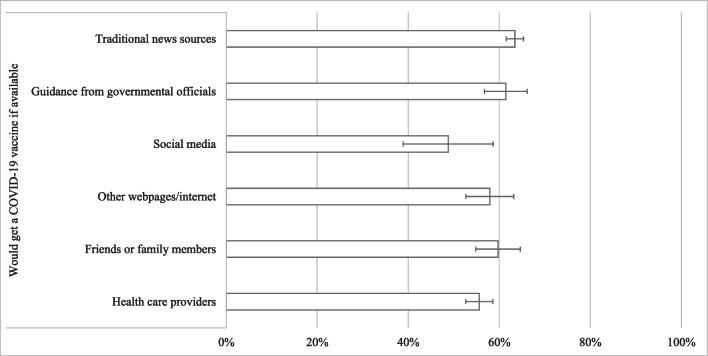
These findings remained similar in terms of sign and significance even after adjusting for perceptions of COVID-19 severity (Fig. 2). However, significant associations were no longer observed among those relying on webpages/Internet or friends or family member as a primary source of COVID-19 information (Table 3).
Figure 2.
Adjusted likelihood of getting a COVID-19 vaccine if available by primary source of COVID-19 information (after adjusting for perception of COVID-19 severity). Adjusted rates and 95% confidence intervals (represented by the whiskers) were estimated using a logistic regression model while controlling for age, gender, race/ethnicity, income, rural residence, census region of residence, insurance, use of other language at home other than English, presence of a particular place for medical care, self-reported health conditions, smoking status, interview date, the primary source of COVID-19 information, as well as three measures of perception of COVID-19 severity. Using coefficients from the logistic regression model, we estimated the adjusted mean values of the outcome, holding the values of other covariates at the same levels. We accounted for complex sample design with sampling weights provided by the MCBS to generate nationally representative estimates.
The correlations of the likelihood of COVID-19 vaccine uptake with perceptions of COVID-19 severity were weak but statistically significant (0.088 to 0.116; P < 0.001) (Table 4). However, the correlations among the measures of perception of COVID-19 severity were relatively high (0.283 to 0.586; P < 0.001).
Table 4.
Correlation of Perceptions of COVID-19 Severity with the Likelihood of COVID-19 Vaccine Uptake
| Agree that COVID-19 is more contagious than flu | Agree that COVID-19 is more deadly than flu | Agree that all should take COVID-19 precautions | Would get a COVID-19 vaccine if available | |
|---|---|---|---|---|
| Agree that COVID-19 is more contagious than flu | 1.000 | |||
| Agree that COVID-19 is more deadly than flu | 0.586 | 1.000 | ||
| Agree that all should take COVID-19 precautions | 0.283 | 0.286 | 1.000 | |
| Would get a COVID-19 vaccine if available | 0.116 | 0.127 | 0.088 | 1.000 |
Boldface indicates statistical significance
DISCUSSION
We found that the primary source of information that Medicare beneficiaries use to learn about COVID-19 was a key determinant of perceptions of COVID-19 severity as well as the likelihood of COVID-19 vaccine uptake. Among the primary source of COVID-19 information, social media or health care providers were notable due to relatively lower likelihood of COVID-19 vaccine uptake. Our findings suggest that the primary source of COVID-19 information may play a critical role in shaping perception of COVID-19 severity and intentions to get a COVID-19 vaccine among Medicare beneficiaries.
We showed that Medicare beneficiaries who relied on social media for COVID-19 information had the lowest levels of perceptions of COVID-19 severity and lowest likelihood of getting a COVID-19 vaccine. Although only 2% of Medicare beneficiaries relied on social media as a primary source of COVID-19 information, this may not be negligible as it represents about 1.2 million beneficiaries when translated into absolute numbers. This suggests that there is a need to create credible and accurate information tailored to Medicare populations who use social media as an information source. While social media provides an opportunity to promote vaccine information to a large audience relatively quickly, it can also serve to promulgate falsehoods and conspiracy theories that may damage trust.6 Thus, COVID-19 information shared online should be scrutinized more closely and public and private partnerships can be used to create and curate accurate and credible information.
We also found that Medicare beneficiaries who relied on health care providers as their primary source of COVID-19 information tended to have poor perceptions of COVID-19 severity and low likelihood of COVID-19 vaccine uptake. Although we could not investigate the underlying mechanism, there may be multiple potential explanations for this finding. One explanation may be attributable to high COVID-19 vaccine hesitancy among health care providers. Indeed, a scoping review demonstrated that the extent of COVID-19 vaccine hesitancy among health care providers is high and is driven by concerns about safety, efficacy, and potential side effects of the COVID-19 vaccines.14 This may affect decision-making about COVID-19 vaccination with their patients. Since health care providers have a moral imperative and duty to play a critical role in increasing vaccine uptake, education and policy-based interventions should be implemented to ensure mass vaccinations.
It is notable that those who relied on other webpages/Internet or friends or family members were likely to have low perceptions of COVID-19 severity and likelihood of COVID-19 vaccine uptake, but no significant association was observed after adjusting for perceptions of COVID-19 severity in the relationship between the source of COVID-19 information and the likelihood of COVID-19 vaccine uptake. This may indicate that targeted programs to improve perceptions of COVID-19 severity may be effective in increasing vaccination rates among those who relied on other webpages/Internet or friends or family members.
Our results also indicate that efforts to change perception of COVID-19 severity may only partially increase vaccine uptake. Although a majority of Medicare beneficiaries were aware of the risk of COVID-19, a substantial portion may be still concerned about vaccine safety. Indeed, 80% of Medicare beneficiaries reported not getting a COVID-19 vaccine due to concerns about side effects and distrust of government.15 The rapid development of COVID-19 vaccines may have provided limited time to educate the public. More concerning, however, is the possibility that misinformation about COVID-19 vaccine could spread, especially through less reliable information sources like social media.
Limitations
Our study had several limitations. First, the data were self-reported and subject to bias and measurement error. Second, we accounted for differences in sample characteristics by primary source of COVID-19 information, but unobserved differences in individual-level factors may still have remained. Thus, any attempt to draw a causal interpretation should be with a caution. Third, we cannot account for how perception of COVID-19 severity and the likelihood of COVID-19 vaccine uptake may have evolved since Fall 2020 after COVID-19 vaccines were subsequently made available in the USA. Finally, about half of the initial sample were excluded from analysis because of missing data in dependent variables, possibility raising some concerns about the generalizability of our findings.
CONCLUSIONS
Our findings demonstrate that the primary source of information Medicare beneficiaries use to learn about COVID-19 was significantly associated with perceptions of COVID-19 severity as well as the likelihood of COVID-19 vaccine uptake. Particularly, those who relied on social media or health care providers were notable due to their relatively lower likelihood of COVID-19 vaccine uptake. Our results also indicate that efforts to change perception of COVID-19 severity may only partially increase vaccine uptake. Taken together, our findings suggest that the primary source of COVID-19 information is a critical determinant of COVID-19 vaccine uptake. Our findings can inform decision-making about the effective communication sources to reach Medicare beneficiaries for public health messaging regarding COVID-19 vaccination.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentation: None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pew Research Center. Intent to get a COVID-19 vaccine reises to 60% as confidence in research and development process increases. In. Washington, DC: Pew Research Center; 2020.
- 2.Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States. In. Atalata, GA: Centers for Disease Control and Prevention; 2021.
- 3.Caldwell T. The slowing Covid-19 vaccination rate is worrying experts. Here's what some states are doing to change the trend. 2021.
- 4.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly BJ, Southwell BG, McCormack LA, et al. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect Dis. 2021;21(1):338. doi: 10.1186/s12879-021-06023-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guidry JPD, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Bosworth A, Finegold K, Samson L, Sheingold S, Tarazi W, Zuckerman R. Risk of Covid-19 infection, hospitalization, and death in fee-for-service Medicare. In. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2021. [Google Scholar]
- 10.Park S, Jung J, Larson EB. Preventable health behaviors, COVID-19 severity perceptions, and vaccine uptake in traditional Medicare and Medicare Advantage: a survey-based study. J Gen Intern Med. 2021;36(6):1837–1840. doi: 10.1007/s11606-021-06801-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng BP, Park C. The role of media sources for COVID-19 information on engaging in recommended preventive behaviors among Medicare beneficiaries aged >/= 65 years. J Gerontol B Psychol Sci Soc Sci. 2021. [DOI] [PMC free article] [PubMed]
- 12.Luo H, Qu H, Basu R, Rafferty AP, Patil SP, Cummings DM. Willingness to get a COVID-19 vaccine and reasons for hesitancy among Medicare beneficiaries: results from a national survey. J Public Health Manag Pract. 2021. [DOI] [PubMed]
- 13.Centers for Medicare and Medicaid Services. Data users’ guide: COVID-19 Fall Supplemental Public Use File. In. Baltimore, MD: Centers for Medicare and Medicaid Services; 2021. [PubMed]
- 14.Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021. [DOI] [PMC free article] [PubMed]
- 15.Centers for Medicare and Medicaid Services. Medicare Current Beneficiary Survey Fall 2020 COVID-19 Data Snapshot. In. Baltimore, MD: Centers for Medicare and Medicaid Services; 2021. [PubMed]