Abstract
Background
Acute kidney injury (AKI) is common in coronavirus disease-2019 (COVID-19) and the severity of AKI is linked to adverse outcomes. In this study, we investigated the factors associated with in-hospital outcomes among hospitalized patients with COVID-19 and AKI.
Methods
In this multicenter retrospective observational study, we evaluated the characteristics and in-hospital renal and patient outcomes of 578 patients with confirmed COVID-19 and AKI. Data were collected from 34 hospitals in Turkey from March 11 to June 30, 2020. AKI definition and staging were based on the Kidney Disease Improving Global Outcomes criteria. Patients with end-stage kidney disease or with a kidney transplant were excluded. Renal outcomes were identified only in discharged patients.
Results
The median age of the patients was 69 years, and 60.9% were males. The most frequent comorbid conditions were hypertension (70.5%), diabetes mellitus (43.8%), and chronic kidney disease (CKD) (37.6%). The proportions of AKI stages 1, 2, and 3 were 54.0%, 24.7%, and 21.3%, respectively. 291 patients (50.3%) were admitted to the intensive care unit. Renal improvement was complete in 81.7% and partial in 17.2% of the patients who were discharged. Renal outcomes were worse in patients with AKI stage 3 or baseline CKD. The overall in-hospital mortality in patients with AKI was 38.9%. In-hospital mortality rate was not different in patients with preexisting non-dialysis CKD compared to patients without CKD (34.4 versus 34.0%, p = 0.924). By multivariate Cox regression analysis, age (hazard ratio [HR] [95% confidence interval (95%CI)]: 1.01 [1.0–1.03], p = 0.035], male gender (HR [95%CI]: 1.47 [1.04–2.09], p = 0.029), diabetes mellitus (HR [95%CI]: 1.51 [1.06–2.17], p = 0.022) and cerebrovascular disease (HR [95%CI]: 1.82 [1.08–3.07], p = 0.023), serum lactate dehydrogenase (greater than two-fold increase) (HR [95%CI]: 1.55 [1.05–2.30], p = 0.027) and AKI stage 2 (HR [95%CI]: 1.98 [1.25–3.14], p = 0.003) and stage 3 (HR [95%CI]: 2.25 [1.44–3.51], p = 0.0001) were independent predictors of in-hospital mortality.
Conclusions
Advanced-stage AKI is associated with extremely high mortality among hospitalized COVID-19 patients. Age, male gender, comorbidities, which are risk factors for mortality in patients with COVID-19 in the general population, are also related to in-hospital mortality in patients with AKI. However, preexisting non-dialysis CKD did not increase in-hospital mortality rate among AKI patients. Renal problems continue in a significant portion of the patients who were discharged.
Introduction
As of December 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affected more than 79 million individuals, causing 1.7 million deaths worldwide [1]. The kidneys are the second most frequently affected organ by SARS-CoV-2, after the lungs [2]. Although the initial reports from China reported that only 3–5% of coronavirus disease-2019 (COVID-19) cases developed acute kidney injury (AKI) [3–9], data from Europe and the United States (US) revealed an incidence of up to 34% [10–14].
AKI is an important complication of COVID-19 and is related to higher in-hospital mortality [15]. Furthermore, AKI is an important prognostic marker of disease severity and survival [15, 16]. The incidence of AKI is higher in patients who require intensive care support [5, 6, 15, 17–19] and 13.3–35.2% of patients with critical disease required kidney replacement therapy (KRT) [8, 10, 17, 19–21]. The severity of AKI was also related to the mortality rate, which was higher in those with AKI stage 2–3 or with high serum urea and creatinine levels at presentation [17], particularly in those who require KRT [16]. The mortality rate was increased approximately 1.73-fold (74.8%) in the intensive care unit (ICU) patients who received KRT [20]. In summary, AKI affects the prognosis of patients with COVID-19, increases the morbidity and mortality rates and the need for KRT, imposing a further burden on both patients and the healthcare system.
It is not clear whether AKI in patients with COVID-19 is causally related to a cytopathic effect of the virus or to the systemic inflammatory response and cytokine storm [22]. The pathogenetic mechanisms leading to AKI are complex and include prerenal AKI due to hypovolemia or cardiorenal syndrome and renal AKI secondary to cytokine release syndrome or rhabdomyolysis leading to acute tubular necrosis, virus-mediated injury, drug nephrotoxicity, and intravascular coagulation [23].
The impact of AKI on patient outcomes may differ due to factors such as geographical area, differences of health-care systems or hospital capacities. There is no large-scale study which document the outcomes of AKI in COVID-19 patients from geographical region in which Turkey is located. In addition, although the increased mortality risk in CKD patients with COVID 19 has been well demonstrated [24–27], it is not clear whether non-dialysis CKD has an impact on patient outcomes among COVID-19 patients with AKI. We were able to document the previous serum creatinine values in a significant proportion of the patients and thus could clearly demonstrate the presence of CKD in our study population. Therefore, we conducted a multicenter retrospective study to evaluate the demographic, and clinical findings and the patient and renal outcomes and related risk factors including non-dialysis-dependent CKD in hospitalized patients with COVID-19 and AKI in Turkey.
Materials and methods
Study design and participants
In this retrospective multicenter observational cohort study, we included hospitalized adult COVID-19 patients who had AKI at presentation or developed AKI during hospitalization in 34 centers in Turkey from March 11 to June 30, 2020. Data collection was terminated on July 13, 2020. This study was approved by the Scientific Committee of the Ministry of Health (approval no: 2020-05-04T14_16_17) and Marmara University Ethics Committee under a broad regulatory protocol allowing for analysis of patient-level data (Approval no: 09.2020.553). The Ethics Committee waived the requirement for informed consent.
Patients with end-stage kidney disease (ESKD), kidney transplantation, pregnancy and patients who were readmitted for AKI and/or any other reason were excluded. Patients who had been transferred to another hospital after hospitalization or not yet been discharged at the time the study end were excluded from the data analysis.
All patients with clinical and laboratory findings and chest computed tomography (CT) findings consistent with COVID-19 were included in the study, irrespective of the result of a reverse transcriptase-polymerase chain reaction (RT-PCR) assay for SARS-CoV-2 on a specimen obtained by nasopharyngeal swab.
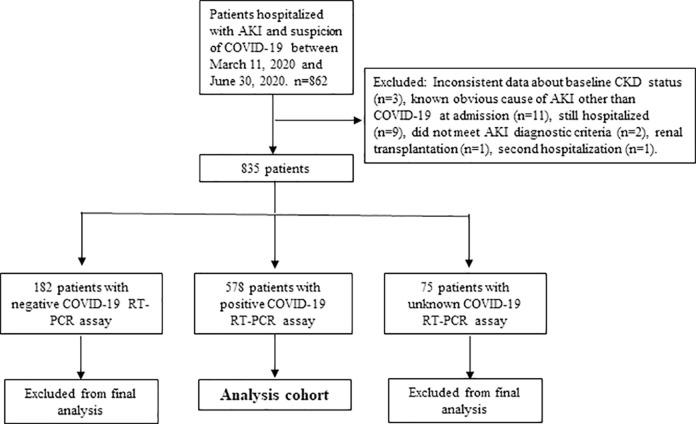
Among 862 patients, 18 patients were excluded from the study due to inconsistent data about baseline CKD status (n = 3), known obvious cause of AKI other than COVID-19 (n = 11), unmet AKI diagnostic criteria (n = 2), kidney transplantation (n = 1), second hospitalization (n = 2) (Fig 1). Among the remaining 835 patients, COVID-19 PCR was negative in 182 patients (21.8%), unknown in 75 (9%), and positive in 578 patients (69.2%). The demographic, laboratory, and clinical data of these patients according to AKI stage are shown in S1 Table. To prevent diagnostic bias, patients negative or unknown by RT-PCR assay and considered possible or probable cases according to the European Centers for Disease Control and Prevention (ECDC) criteria [28] were excluded from the final analysis and only COVID-19 PCR positive patients (confirmed cases) were used in the final analysis. Possible and probable cases were described as meeting the clinical criteria of COVID-19 including fever, cough or shortness of breath and the presence of the diagnostic imaging criteria, respectively. A flowchart of patient selection was shown in Fig 1.
Fig 1. Flowchart of patient selection for the study.
The diagram shows the numbers of individuals (n) excluded at different stages and the identification of cases for the analysis.
Data collection
We obtained demographic, clinical and laboratory data, radiologic findings, treatment characteristics and outcomes (patient and renal) from the electronic medical records. Previous comorbidities and medications were documented. Laboratory data included renal and liver function tests, albumin, electrolytes, lactate dehydrogenase (LDH), complete blood count, C-reactive protein (CRP), ferritin, procalcitonin, fibrinogen, d-dimer at the time of admission, as well as chest CT findings. Laboratory and clinical data during hospitalization [need for dialysis, admission to ICU, intubation, and extracorporeal membrane oxygenation (ECMO) requirement, macrophage activation syndrome (MAS), shock/severe hypotension, and secondary bacterial infection during hospitalization] were also recorded (Table 1 and S1 Table).
Table 1. Characteristics of COVID-19 RT-PCR positive patients during hospital admission and hospital stay, by AKI severity.
| Total (n = 578) | AKI 1 (n = 312) | AKI 2 (n = 143) | AKI 3, (n = 123) | p | |
|---|---|---|---|---|---|
| Age (years) | 69 (59–77) | 67 (57–77) | 67 (61–77) | 72 (60–79) | 0.169 |
| Male, n/N (%) | 352/578 (60.9) | 184/312 (59) | 85/143 (59.4) | 83/123 (67.5) | 0.241 |
| Comorbid conditions, n/N (%) | |||||
| Diabetes mellitus | 249/569 (43.8) | 129/310 (41.6) | 68/139 (48.9) | 52/120 (43.3) | 0.351 |
| Hypertension | 399/569 (70.5) | 224/307 (73) | 105/140 (75) | 70/119 (58.8) | 0.007 |
| Chronic kidney disease | 192/510 (37.6) | 103/289 (35.6) | 47/127 (37.0) | 42/94 (44.7) | 0.287 |
| Obesity | 27/462 (5.8) | 12/250 (4.8) | 8/121 (6.6) | 7/91 (7.7) | 0.552 |
| Chronic obstructive pulmonary disease | 89/549 (16.2) | 50/301 (16.6) | 19/133 (14.3) | 20/115 (17.4) | 0.772 |
| Coronary heart disease | 172/541 (31.8) | 85/290 (29.3) | 51/134 (38.1) | 36/117 (30.8) | 0.191 |
| Heart failure | 85/528 (16.1) | 49/286 (17.1) | 25/129 (19.4) | 11/113 (9.7) | 0.098 |
| Cerebrovascular disease | 39/546 (7.1) | 18/298 (6) | 10/135 (7.4) | 11/113 (9.7) | 0.426 |
| Cancer | 69/554 (12.5) | 26/303 (8.6) | 24/137 (17.5) | 19/114 (16.7) | 0.010 |
| Chronic liver disease | 10/556 (1.8) | 3/304 (1) | 4/137 (2.9) | 3/115 (2.6) | 0.338 |
| Autoimmune/autoinflammatory disease | 25/556 (4.5) | 13/305 (4.3) | 10/136 (7.4) | 2/115 (1.7) | 0.097 |
| Medications, n/N (%) | |||||
| ACE-I or ARB | 266/505 (52.7) | 166/276 (60.1) | 59/128 (46.1) | 41/101 (40.6) | 0.001 |
| Ca antagonists | 171/491 (34.8) | 95/264 (36) | 44/127 (34.6) | 32/100 (32) | 0.775 |
| Beta blockers | 216/491 (44) | 115/262 (43.9) | 62/130 (47.7) | 39/99 (39.4) | 0.455 |
| Other antihypertensives | 113/476 (23.7) | 60/260 (23.1) | 27/120 (22.5) | 26/96 (27.1) | 0.685 |
| Insulin | 122/484 (25.2) | 58/259 (22.4) | 38/123 (30.9) | 26/102 (25.5) | 0.202 |
| Oral antidiabetics | 127/486 (26.1) | 71/260 (27.3) | 31/123 (25.2) | 25/103 (24.3) | 0.808 |
| Statins | 88/477 (18.4) | 41/254 (16.1) | 27/122 (22.1) | 20/101 (19.8) | 0.346 |
| Antiaggregant or anticoagulant drugs | 251/501 (50.1) | 133/265 (50.2) | 67/130 (51.5) | 51/106 (48.1) | 0.871 |
| Smoking status, n/N (%) 0.254 | |||||
| Never | 221/411 (53.8) | 124/232 (53.4) | 61/102 (59.8) | 36/77 (46.8) | |
| Current | 34/411 (8.3) | 21/232 (9.1) | 4/102 (3.9) | 9/77 (11.7) | |
| Former | 156/411 (38) | 87/232 (37.5) | 37/102 (36.3) | 32/77 (41.6) | |
| Symptoms related to COVID-19, n/N (%) | |||||
| Fever | 380/565 (67.3) | 208/310 (67.1) | 95/139 (68.3) | 77/116 (66.4) | 0.942 |
| Fatigue | 356/563 (63.2) | 194/308 (63) | 93/140 (66.4) | 69/115 (60) | 0.566 |
| Dyspnea | 375/569 (65.9) | 185/310 (59.7) | 100/140 (71.4) | 90/119 (75.6) | 0.002 |
| Cough | 408/564 (72.3) | 225/310 (72.6) | 101/139 (72.7) | 82/115 (71.3) | 0.962 |
| Anorexia | 132/540 (24.4) | 86/301 (28.6) | 29/129 (22.5) | 17/110 (15.5) | 0.020 |
| Myalgia | 192/542 (35.4) | 107/303 (35.3) | 46/131 (35.1) | 39/108 (36.1) | 0.985 |
| Headache | 82/545 (15) | 47/300 (15.7) | 16/133 (12) | 19/112 (17) | 0.507 |
| Sore throat | 72/546 (13.2) | 39/303 (12.9) | 22/133 (16.5) | 11/110 (10) | 0.315 |
| Diarrhea | 32/551 (5.8) | 19/306 (6.2) | 8/133 (6) | 5/112 (4.5) | 0.791 |
| Others | 40/508 (7.9) | 22/282 (7.8) | 9/120 (7.5) | 9/106 (8.5) | 0.960 |
| Asymptomatic | 4/519 (0.8) | 3/283 (1.1) | 1/127 (0.8) | 0/109 (0) | |
| Possible source of COVID-19, n/N (%) 0.226 | |||||
| Family-house | 139/541 (25.7) | 82/291 (28.2) | 31/136 (22.8) | 26/114 (22.8) | |
| Nursing home or prison | 10/541 (1.8) | 5/291 (1.7) | 3/136 (2.2) | 2/114 (1.8) | |
| Health institution | 21/541 (3.9) | 7/291 (2.4) | 9/136 (6.6) | 5/114 (4.4) | |
| Social life (meeting or dinner) | 68/541 (12.6) | 32/291 (11) | 22/136 (16.2) | 14/114 (12.3) | |
| Travel abroad | 10/541 (1.8) | 2/291 (0.7) | 6/136 (4.4) | 2/114 (1.8) | |
| Domestic travel | 1/541 (0.2) | 1/291 (0.3) | 0/136 (0) | 0/114 (0) | |
| Unknown | 292/541 (54) | 162/291 (55.7) | 65/136 (47.8) | 65/114 (57) | |
| Radiologic examination, n/N (%) | |||||
| Patients with a chest CT scan | 563/572 (98.4) | 304/309 (98.4) | 141/143 (98.6) | 118/120 (98.3) | 1.000 |
| Patients with specific chest CT findings | 529/564 (93.8) | 284/305 (93.1) | 132/140 (94.3) | 113/119 (95) | 0.749 |
| Patients with specific bilaterally chest CT findings | 472/549 (86) | 250/297 (84.2) | 121/139 (87.1) | 101/113 (89.4) | 0.270 |
| Specific chest CT findings, n/N (%) | |||||
| Ground glass opacity | 503/535 (94) | 270/289 (93.4) | 129/137 (94.2) | 104/109 (95.4) | 0.755 |
| Reticular opacity | 155/28 (36.2) | 84/232 (36.2) | 36/110 (32.7) | 35/86 (40.7) | 0.515 |
| Bronchial wall thickening | 79/428 (18.5) | 45/231 (19.5) | 21/111 (18.9) | 13/86 (15.1) | 0.666 |
| Pleural effusion | 100/427 (23.4) | 42/229 (18.3) | 32/110 (29.1) | 26/88 (29.5) | 0.029 |
| Thoracic lymphadenopathy | 53/424 (12.5) | 28/230 (12.2) | 14/108 (13) | 11/86 (12.8) | 0.975 |
| Oxygen saturation in room air at diagnosis, n/N (%) <0.001 | |||||
| Normal | 129/551 (23.4) | 89/297 (30) | 26/136 (19.1) | 14/118 (11.9) | |
| 90–95% | 210/551 (38.1) | 131/297 (44.1) | 46/136 (33.8) | 33/118 (28) | |
| <90% | 212/551 (38.5) | 77/297 (25.9) | 64/136 (47.1) | 71/118 (60.2) | |
| Severity of COVID-19 infection, n/N (%) <0.001 | |||||
| Asymptomatic | 13/578 (2.2) | 9/312 (2.9) | 3/143 (2.1) | 1/123 (0.8) | |
| Mild to moderate | 196/578 (33.9) | 132/312 (42.3) | 46/143 (32.2) | 18/123 (14.6) | |
| Severe | 256/578 (44.3) | 132/312 (42.3) | 62/143 (43.4) | 62/123 (50.4) | |
| Critical | 113/578 (19.6) | 39/312 (12.5) | 32/143 (22.4) | 42/123 (34.1) | |
| Time between first symptom and COVID-19 diagnosis (days) | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (3–4) | 0.639 |
| Data for renal function within the last year | |||||
| Serum creatinine (μmol/L) | 86.6 (70.7–109.6) | 88.4 (70.6–108.8) | 84.9 (70.7–114.9) | 85.7(70.7–114.9) | 0.840 |
| eGFR (mL/min/1.73 m2) | 65.4 (40.6–96.6) | 64.5 (41.8–95.3) | 70.3 (39.1–100) | 69.1 (40.2–100.4) | 0.821 |
| CKD stages in patients with known eGFR within the last year, n/N (%) | 0.677 | ||||
| eGFR>90 ml/min/1.73m2 | 130/447 (29.1) | 66/239 (27.6) | 35/115 (30.4) | 29/93 (31.2) | |
| eGFR 60–90 ml/min/.73m2 | 126/447 (28.2) | 71/239 (29.7) | 33/115 (28.7) | 22/93(23.7) | |
| CKD stage 3 | 113/447 (25.3) | 60/239 (25.1) | 27/115 (23.5) | 26/93 (28) | |
| CKD stage 4 | 55/447 (12.3) | 32/239 (13.4) | 15/115 (13.0) | 8/93(8.6) | |
| CKD stage 5 | 23/447 (5.1) | 10/239 (4.2) | 5/115 (4.3) | 8/93 (8.6) | |
| Laboratory parameters at hospital admission | |||||
| Urea (mmol/L) | 9.3 (6.0–14.0) | 8.7 (5.7–12.3) | 9.7 (6.6–16.1) | 10.0 (6.8–18.3) | 0.001 |
| Creatinine (μmol/L) | 117.6 (88.4–164.4) | 114.9 (89.3–144.1) | 123.8 (86.6–176.8) | 123.8 (81.3–238.7) | 0.118 |
| Na (mmol/L) | 137 (134–140) | 137 (134–140) | 136 (133–140) | 136 (133–140) | 0.625 |
| K (mmol/L) | 4.4 (3.9–4.8) | 4.4 (4–4.7) | 4.4 (3.9–4.8) | 4.2 (3.9–4.8) | 0.871 |
| AST (U/L) | 32 (20–49.4) | 28 (19.2–42) | 36 (20.5–57) | 38.1 (24–61) | <0.001 |
| ALT (U/L) | 23 (14–35) | 22 (14–33.1) | 23 (15–37) | 24 (14–44) | 0.268 |
| LDH (U/L) | 320 (239–443) | 296.5 (229.5–409.5) | 321 (233–505) | 381.5 (298–523) | <0.001 |
| Albumin (g/L) | 35 (30–39) | 37 (32–39) | 32 (28–37) | 31 (28–36) | <0.001 |
| Ferritin (μg/L) | 360 (162–748) | 290 (154–649) | 376.5 (150–887) | 502.5 (302.6–913) | <0.001 |
| Fibrinogen (g/L) | 4.7 (3.5–6.2) | 4.6 (3.3–6.2) | 4.5 (3.5–6.0) | 5.0 (4.2–6.5) | 0.140 |
| D-dimer (mg/L) | 14.6 (8.1–28.44) | 13.2 (7.0–26.5) | 15.8 (8.5–27.9) | 15.1 (10.3–31.6) | 0.218 |
| Procalcitonin (ng/L) | 350 (130–1145) | 200 (100–760) | 510 (270–1540) | 840 (235–1700) | <0.001 |
| Hemoglobin (g/dl) | 12.1 (10.6–13.8) | 12.7 (11–14.1) | 11.7 (10.2–13.2) | 11.6 (10.5–13) | <0.001 |
| Leucocyte count(/mm3) | 7835 (5500–11250) | 7700 (5300–10630) | 7870 (5540–11780) | 8825 (5980–11600) | 0.150 |
| Neutrophil count (/mm3) | 5750 (3700–9110) | 5370 (3530–8100) | 5750 (3700–9360) | 7216 (4400–10600) | 0.001 |
| Lymphocyte count (/mm3) | 1100 (700–1520) | 1200 (800–1600) | 1090 (750–1440) | 805 (500–1390) | <0.001 |
| Thrombocyte count (x1000/mm3) | 202.5 (151–274) | 211 (161–281) | 187 (134–277) | 197 (149–255) | 0.041 |
| CRP levels†, n/N (%) <0.001 | |||||
| Normal | 28/576 (4.9) | 24/312 (7.7) | 3/142 (2.1) | 1/122 (0.8) | |
| 1/5-fold x ULN | 91/576 (15.8) | 60/312 (19.2) | 22/142 (15.5) | 9/122 (7.4) | |
| 5/10-fold x ULN | 103/576 (17.9) | 55/312 (17.6) | 29/142 (20.4) | 19/122 (15.6) | |
| 10/20-fold x ULN | 150/576 (26) | 84/312 (26.9) | 30/142 (21.1) | 36/122 (29.5) | |
| >20-fold x ULN | 204/576 (35.4) | 89/312 (28.5) | 58/142 (40.8) | 57/122 (46.7) | |
| Specific treatments for COVID-19, n/N (%) | |||||
| Hydroxychloroquine | 560/578 (96.9) | 305/312 (97.8) | 137/143 (95.8) | 118/123 (95.9) | 0.435 |
| Oseltamivir | 324/578 (56.1) | 185/312 (59.3) | 77/143 (53.8) | 62/123 (50.4) | 0.201 |
| Macrolide | 471/578 (81.5) | 265/312 (84.9) | 115/143 (80.4) | 91/123 (74) | 0.028 |
| Favipiravir | 369/578 (63.8) | 180/312 (57.7) | 99/143 (69.2) | 90/123 (73.2) | 0.003 |
| Glucocorticoid | 111/578 (19.2) | 38/312 (12.2) | 27/143 (18.9) | 46/123 (37.4) | <0.001 |
| Lopinavir-ritonavir | 39/578 (6.7) | 18/312 (5.8) | 8/143 (5.6) | 13/123 (10.6) | 0.163 |
| Tocilizumab | 73/578 (12.6) | 43/312 (13.8) | 13/143 (9.1) | 17/123 (13.8) | 0.340 |
| Convalescent plasma | 19/578 (3.3) | 6/312 (1.9) | 4/143 (2.8) | 9/123 (7.3) | 0.019 |
| Apheresis/immunoadsorption | 9/578 (1.6) | 2/312 (0.6) | 1/143 (0.7) | 6/123 (4.9) | 0.006 |
| IL-1 inhibitors (anakinra/canakinumab) | 0/578 (0) | 0/312 (0.3) | 0/143 (0) | 0/123 (0) | |
| JAK2 inhibitors | 1/578 (0.2) | 1/312 (0.3) | 0/143 (0) | 0/123 (0) | |
| Unfavorable prognostic signs at any time during hospital stay, n/N (%) | |||||
| Lymphopenia | 614/834 (73.6) | 303/437 (69.3) | 169/217 (77.9) | 142/180 (78.9) | 0.013 |
| Anemia (Hb <10 g/dL) | 446/834 (53.5) | 183/437 (41.9) | 125/217 (57.6) | 138/180 (76.7) | <0.001 |
| Thrombocytopenia | 261/830 (31.4) | 119/437 (27.2) | 71/215 (33) | 71/178 (39.9) | 0.008 |
| LDH (>2-fold x ULN) ‡ | 400/811 (49.3) | 173/431 (40.1) | 109/209 (52.2) | 118/171 (69) | <0.001 |
| AST (>2-fold x ULN) ‡‡ | 350/831 (42.1) | 138/436 (31.7) | 103/217 (47.5) | 109/178 (61.2) | <0.001 |
| Macrophage activation syndrome | 165/751 (22) | 60/401 (15) | 47/193 (24.4) | 58/157 (36.9) | <0.001 |
| Shock/severe hypotension | 289/789 (36.6) | 79/417 (18.9) | 91/203 (44.8) | 119/169 (70.4) | <0.001 |
| Secondary bacterial infection | 336/760 (44.2) | 122/401 (30.4) | 99/193 (51.3) | 115/166 (69.3) | <0.001 |
| CRP levels† | <0.001 | ||||
| Normal | 17/578 (2.9) | 17/312 (5.4) | 0/143 (0) | 0/123 (0) | |
| 1/5-fold x ULN | 40/578 (6.9) | 28/312 (9) | 9/143 (6.3) | 3/123 (2.4) | |
| 5/10-fold x ULN | 59/578 (10.2) | 40/312 (12.8) | 16/143 (11.2) | 3/123 (2.4) | |
| 10/20-fold x ULN | 124/578 (21.5) | 78/312 (25) | 27/143 (18.9) | 19/123 (15.4) | |
| >20-fold x ULN | 338/578 (58.5) | 149/312 (47.8) | 91/143 (63.6) | 98/123 (79.7) | |
| Intensive care unit admission, n/N (%) | 291/578 (50.3) | 100/312 (32.1) | 83/143 (58) | 108/123 (87.8) | <0.001 |
| Managements in the intensive care unit, n/N (%) | |||||
| Intubation | 232/288 (80.6) | 66/100 (66) | 65/81 (80.2) | 101/107 (94.4) | <0.001 |
| ECMO | 18/265 (6.8) | 5/92 (5.4) | 1/72 (3.4) | 12/101 (11.9) | 0.021 |
| Slow continuous dialysis | 53/260 (20.4) | 12/89 (13.5) | 10/72 (13.9) | 31/99 (31.3) | 0.003 |
| Duration of stay in intensive care unit (days) | 9 (5–16) | 8.5 (4–18) | 8 (5–16) | 9 (6–16) | 0.851 |
| AKI timing, n/N (%) | |||||
| AKI at hospital admission | 251/578 (43.4) | 145/312 (46.5) | 53/143 (37.1) | 53/123 (43.1) | 0.170 |
| AKI during hospital stay | 327/578 (51.6) | 167/132 (53.5) | 90/143 (62.9) | 70/123 (56.9) | 0.170 |
| Suspected causes of AKI, n/N (%) <0.001 | |||||
| Prerenal | 251/578 (43.4) | 183/312 (58.7) | 52/143 (36.4) | 16/123 (13) | |
| Renal | 311/578 (53.8) | 119/312 (38.1) | 91/143 (63.6) | 101/123 (82.1) | |
| Postrenal | 6/578 (1) | 4/312 (1.3) | 0/143 (0) | 2/123 (1.6) | |
| Others | 10/578 (1.7) | 6/312 (1.9) | 0/143 (0) | 4/123 (3.3) | |
| Suspected specific causes of AKI, n/N (%) <0.001 | |||||
| Dehydration | 141/578 (24.4) | 110/312 (35.3) | 24/143 (16.8) | 7/123 (5.7) | |
| GIS loss | 10/578 (1.7) | 7/312 (2.2) | 2/143 (1.4) | 1/123 (0.8) | |
| Heart failure | 19/578 (3.3) | 9/312 (2.9) | 8/143 (5.6) | 2/123 (1.6) | |
| Other prerenal causes | 81/578 (14) | 57/312 (18.3) | 18/143 (12.6) | 6/123 (4.9) | |
| Sepsis | 233/578 (40.3) | 80/312 (25.6) | 63/143 (44.1) | 90/123 (73.2) | |
| Thrombotic microangiopathy | 8/578 (1.4) | 3/312 (1) | 2/143 (1.4) | 3/123 (2.4) | |
| Extended prerenal causes | 36/578 (6.2) | 17/312 (5.4) | 16/143 (11.2) | 3/123 (2.4) | |
| Rhabdomyolysis | 2/578 (0.3) | 0/312 (0) | 0/143 (0) | 2/123 (1.6) | |
| Nephrotoxic drugs | 32/578 (5.5) | 19/312 (6.1) | 10/143 (7) | 3/123 (2.4) | |
| Postrenal (urological) causes | 6/578 (1) | 4/312 (1.3) | 0/143 (0) | 2/123 (1.6) | |
| Others | 10/578 (1.7) | 6/312 (1.9) | 0/143 (0) | 4/123 (3.3) | |
| Time between hospitalization and AKI (days) | 5 (3–8) | 4 (3–7) | 5 (3–8) | 5 (3–9) | 0.304 |
| Dialysis requirement in the ward, n/N (%) | 91/554 (16.4) | 11/304 (3.6) | 19/134 (14.2) | 61/116 (52.6) | <0.001 |
| KRT indications, n/N (%) | |||||
| Increase in serum BUN/creatinine levels | 42/115 (36,5) | 9/19 (47,4) | 9/27 (33,3) | 24/69 (34,8) | |
| Hyperkalemia | 10/115 (8.7) | 0/19 (0) | 3/27 (11.1) | 7/69 (10.1) | |
| Metabolic acidosis | 27/115 (23.5) | 3/19 (15.8) | 7/27 (25.9) | 17/69 (24.6) | |
| Hypervolemia | 22/115 (19.1) | 3/19 (15.8) | 4/27 (14.8) | 15/69 (21.7) | |
| Severe uremic symptoms | 3/115 (2.6) | 1/19 (5.3) | 0/27 (0) | 2/69 (2.9) | |
| Others | 11/115 (9.6) | 3/19 (15.8) | 4/27 (14.8) | 4/69 (5.8) | |
| Renal Outcome, n/N (%) <0.001 | |||||
| Complete recovery | 285/349 (81.7) | 213/251 (84.9) | 59/76 (77.6) | 13/22 (59.1) | |
| Partial recovery | 60/349 (17.2) | 37/251 (14.7) | 16/76 (21.1) | 7/22 (31.8) | |
| No improvement and/or dialysis dependence | 4/349 (1.1) | 1/251 (0.4) | 1/76 (1.3) | 2/22 (9.1) | |
| Duration of AKI in discharged patients (days) | 6 (3–9) | 5 (3–8) | 6 (4–10) | 9 (5–14) | <0.001 |
| Patient Outcome, n/N (%) | <0.001 | ||||
| Discharged | 353/578 (61.1) | 253/312 (81.1) | 77/143 (53.8) | 23/123 (18.7) | |
| Dead | 225/578 (38.9) | 59/312 (18.9) | 66/143 (46.2) | 100/123 (81.3) | |
| Total hospital stays (days) | 12 (8–19) | 12 (7.5–18) | 13 (10–19) | 14 (10–24) | 0.014 |
ACE-I, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; COVID-19, coronavirus disease 2019; eGFR, estimated glomerular filtration rate; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactate dehydrogenase; x ULN, increase above upper normal limit; CRP, C-reactive protein; IL-1, interleukin 1; JAK2, Janus kinase; ECMO, extracorporeal membrane oxygenation; KRT, kidney replacement therapy.
Data were expressed as median [Q1-Q3] or as number (percent).
†The upper limit of the normal range of CRP was 5 mg/L (47.6 nmol/L).
‡The upper limit of the normal range of LDH was 248 U/L.
‡‡The upper limit of the normal range of AST was 37 U/L.
Definitions and measurements
COVID-19 clinical status was classified as asymptomatic, mild-to-moderate, severe, or critical according to the World Health Organization Report of the WHO–China Joint Mission on Coronavirus Disease 2019 (COVID-19) [29].
The definition and staging of AKI were based on the 2012 Kidney Disease: Improving Global Outcomes (KDIGO) criteria [30]. As the KDIGO criteria may underestimate the incidence of AKI, we also used an automatically calculated prebuilt operational algorithm for AKI diagnosis and staging according to the serum creatinine value in the last 365 days [31].
Diagnosis and staging of AKI and CKD were performed according to a serum creatinine value within the previous 365 days. Patients who had no serum creatinine measurement in the last 365 days were not accepted as CKD, whereas those with renal function recovery during follow-up were considered as AKI. Renal recovery was defined as the serum creatinine level decreasing to the reference range and/or to >30% decrease compared to values at admission. Patients who experienced complete renal recovery at discharge were accepted as non-CKD. For patients who developed AKI during hospitalization, we used the KDIGO criteria for diagnosis and staging of AKI. AKI staging was performed according to the peak creatinine value. CKD was considered when the estimated glomerular filtration rate (eGFR) was < 60 mL/dk/1.73 m2 by the CKD-EPI formula [32].
The underlying cause of AKI was determined from clinical and other laboratory findings and/or the follow-up of the renal function. If renal recovery has occurred within 3 days of fluid replacement, prerenal AKI was considered. In addition, AKI due to cardiac decompensation without any obvious cause(s) was accepted as prerenal AKI if it resolved over a short period. Renal AKI was considered in patients with sepsis or shock or severe and prolonged prerenal AKI, with a diagnosis of acute tubular necrosis, and exposure to nephrotoxic drugs or radiocontrast medium was regarded as nephrotoxic AKI if there was no other identified cause.
Outcomes
We defined length of stay at the hospital as the period from the first day of hospitalization to the day of discharge or death. The primary outcomes were patient and renal outcomes. Patient outcome was in-hospital death. Renal outcomes were categorized as follows: (1) Complete recovery: serum creatinine level decreased to baseline or to within normal limits; (2) partial recovery: serum creatinine level decreased but higher than 30% above baseline or reference value; (3) no improvement and/or dialysis dependence. Renal outcomes were determined only for discharged patients at the end of the hospital stay.
Statistical analysis
The analyses were performed using the IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were expressed as numbers and percentages for categorical variables and as median and interquartile range (IQR) for numerical variables. The conformity of variables to normal distribution was assessed using visual (histogram and probability graphs) and analytical methods (Kolmogorov-Smirnov/Shapiro-Wilk tests). For multiple group comparisons of categorical variables, chi-square test or Fisher’s exact test were used for categorical variables as appropriate. In comparison of two independent groups, Mann-Whitney U test was used for non-normally distributed numerical variables. The Kruskal–Wallis test was used for non-normally distributed numerical variables in multiple group comparisons. In multivariate Cox regression analysis, we assessed interactions of AKI development during hospitalization with demographic and clinic parameters that suggested potential effect in univariate analysis. Independent risk factors of in-hospital mortality were assessed using multivariate Cox regression analysis. We checked the correlations and interactions between explanatory variables which might have potential effect on in-hospital mortality in the univariate analysis or when clinically relevant. Final multivariate models were derived using stepwise backward LR method from the initial model created with the candidate variables in Cox regression analysis. Statistical significance level was set at p<0.05.
Results
Clinical characteristics
The demographic, laboratory, and clinical data of the patients, according to AKI stage, are listed in Table 1. The patients’ median age was 69 (59–77) years, and 60.9% were male. The most frequent baseline comorbidities were hypertension (70.5%), diabetes mellitus (43.8%), and chronic kidney disease (37.6%). About 53% of the patients were on angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) therapy. The rates of mild-to-moderate, severe, and critical disease at hospital admission were 33.9%, 44.3%, and 19.6%, respectively. A total of 291 patients (50.3%) were admitted to the ICU, among whom 80.6% and 6.8% were intubated and treated with ECMO, respectively. Fifty-three of 260 (20.4%) patients admitted to ICU required KRT for any indication.
Among the 578 patients with AKI, 312 (54.0%), 143 (24.7%) and 123 (21.3%) had stage 1, 2, and 3 AKI, respectively (Table 1). The prevalence of critical disease was higher in patients with stage 3 AKI at admission. The baseline serum AST, LDH, ferritin, and procalcitonin levels were higher and the baseline albumin, hemoglobin, blood lymphocyte, and platelet counts were lower in patients with AKI stage 3. AKI stage 3 was more common in patients admitted to ICU and the need for mechanical ventilation was also higher than other stages. ECMO and slow continuous dialysis treatment were also higher in these patients. Unfavorable laboratory clinical findings including lymphopenia, anemia, increase in LDH (greater than twofold the upper limit of normal [ULN]) and aspartate aminotransferase (AST) (greater than twofold the ULN), MAS, shock/severe hypotension, and secondary bacterial infection were more common in patients with AKI stage 3 at any time during hospitalization. Intrarenal etiologies of AKI were more frequent in patients with stage 3 AKI compared to those with AKI stage 1 or 2.
The timing of initial development of AKI
The demographic and clinical characteristics of the patients according to the timing of AKI diagnosis are shown on S2 Table. Preexisting CKD or RAAS blockage usage was more common in patients who were diagnosed with AKI at hospital admission, whereas those with baseline hypertension developed AKI more frequently during their hospital stay. The incidence of lymphopenia, macrophage activation syndrome, shock/severe hypotension, and intensive care unit admission was higher in patients who developed AKI during hospitalization. In-hospital mortality rate were increased in those who developed AKI during hospital stay. In Cox-regression analysis, intensive care admission and lymphopenia were independently associated with AKI developed during hospitalization (S3 Table).
AKI patients with baseline chronic kidney disease
The demographic, clinical, and laboratory data according to baseline CKD are listed in Table 2 and S4 Table. Sixty-three patients who had no prior serum creatinine measurement and showed full renal recovery at the time of discharge were considered as “non-CKD”. Among the 510 patients, 192 (37.6%) had CKD at baseline.
Table 2. Characteristics and outcomes of COVID-19 RT-PCR positive patients on the basis of baseline chronic kidney disease.
| Variable | Baseline Chronic Kidney Disease | |||
|---|---|---|---|---|
| Total (n = 510) | No (n = 318) | Yes (n = 192) | p | |
| Age (years) | 69 (59–77.2) | 64 (54–74) | 72.5 (65–79) | <0.001 |
| Male, n/N (%) | 305/510 (59.8) | 208/318 (65.4) | 97/192 (50.2) | 0.001 |
| Comorbid conditions, n/N (%) | ||||
| Diabetes mellitus | 226/506 (44.7) | 119/315 (37.8) | 107/191 (56.0) | <0.001 |
| Hypertension | 362/502 (72.1) | 190/310 (61.3) | 172/192 (89.6) | <0.001 |
| Obesity | 24/429 (5.6) | 10/248 (4.0) | 14/181 (7.7) | 0.135 |
| Chronic obstructive pulmonary disease | 83/489 (17.0) | 38/303 (12.5) | 45/186 (24.2) | 0.001 |
| Coronary heart disease | 159/480 (33.1) | 73/299 (24.4) | 86/181 (47.5) | <0.001 |
| Heart failure | 79/470 (16.8) | 29/296 (9.8) | 50/174 (28.7) | <0.001 |
| Cerebrovascular disease | 36/488 (7.4) | 19/303 (6.3) | 17/185 (9.2) | 0.284 |
| Cancer | 61/495 (12.3) | 45/310 (14.5) | 16/185 (8.6) | 0.066 |
| Chronic liver disease | 10/495 (2.0) | 8/308 (2.6) | 2/187 (1.1) | 0.332 |
| Autoimmune/autoinflammatory disease | 24/495 (4.8) | 20/309 (6.5) | 4/186 (2.2) | 0.031 |
| Medications, n/N (%) | ||||
| ACE-I or ARB | 246/460 (53.5) | 136/276 (49.3) | 110/184 (59.8) | 0.029 |
| Ca antagonists | 159/450 (35.3) | 76/266 (28.6) | 83/184 (45.1) | <0.001 |
| Beta blockers | 205/449 (45.7) | 96/265 (36.2) | 109/184 (59.2) | <0.001 |
| Other antihypertensives | 97/433 (22.4) | 46/261(17.6) | 51/172 (29.7) | 0.005 |
| Insulin | 117/446 (26.2) | 42/262 (16.0) | 75/184 (40.8) | <0.001 |
| Oral antidiabetics | 120/447 (26.8) | 73/264 (27.7) | 47/183 (25.7) | 0.666 |
| Statins | 82/439 (18.7) | 31/259 (12.0) | 51/180 (28.3) | <0.001 |
| Antiaggregant or anticoagulant drugs | 232/455 (51.0) | 99/267 (37.1) | 133/188 (70.7) | <0.001 |
| Smoking status, n/N (%) 0.002 | ||||
| Never | 207/386 (53.6) | 120/223 (53.8) | 87/163 (53.4) | |
| Current | 27/386 (7.0) | 24/223 (10.8) | 3/163 (1.8) | |
| Former | 152/386 (39.4) | 79/223 (35.4) | 73/163 (44.8) | |
| Symptoms related to COVID-19, n/N (%) | ||||
| Fever | 345/500 (69.0) | 201/310 (64.8) | 144/199 (75.8) | 0.013 |
| Fatigue | 325/500 (65.0) | 186/310 (60.0) | 139/190 (73.2) | 0.003 |
| Dyspnea | 331/505 (65.5) | 194/314 (61.8) | 137/191 (71.7) | 0.026 |
| Cough | 366/500 (73.2) | 220/309 (71.2) | 146/191 (76.4) | 0.213 |
| Anorexia | 129/481 (26.8) | 66/299 (22.1) | 63/182 (34.6) | 0.003 |
| Myalgia | 179/482 (37.1) | 95/298 (32.0) | 84/194 (44.8) | 0.003 |
| Headache | 72/484 (14. 9) | 39/300 (13.0) | 33/184 (17.9) | 0.149 |
| Sore throat | 67/485 (13.8) | 33/301 (11.0) | 34/184 (18.5) | 0.022 |
| Diarrhea | 29/489 (5.9) | 23/303 (7.6) | 6/186 (3.2) | 0.050 |
| Others | 29/449 (6.5) | 25/286 (8.7) | 4/163 (2.5) | 0.009 |
| Asymptomatic | 4/457 (0.9) | 3/286 (1.0) | 1/171 (0.6) | - |
| Oxygen saturation in room air at diagnosis, n/N (%) 0.026 | ||||
| Normal | 120/489 (24.5) | 80/299 (26.8) | 40/190 (21.1) | |
| 90–95% | 195/489 (39.9) | 105/299 (35.1) | 90/190 (47.4) | |
| <90% | 174/489 (35.6) | 114/299 (38.1) | 60/190 (31.6) | |
| Severity of COVID-19 infection, n/N (%) 0.649 | ||||
| Asymptomatic | 13/510 (2.5) | 9/318 (2.8) | 4/192 (2.1) | |
| Mild to moderate | 180/510 (36.1) | 120/318 (37.7) | 64/192 (33.3) | |
| Severe | 220/510 (43.1) | 131/318 (41.2) | 89/192 (46.4) | |
| Critical | 93/510 (18.2) | 58/318 (18.2) | 35/192 (18.2) | |
| Data of renal function within the last year. | ||||
| Serum creatinine (μmol/L) | 85.8 (70.7–109.6) | 72.5 (62.8–81.3) | 120.2 (97.3–161.8) | <0.001 |
| eGFR (mL/min/1.73 m2) | 65.4 (40.6–96.6) | 91.3 (72.2–112) | 36.4 (23.9–52.2) | <0.001 |
| Laboratory parameters at hospital admission | ||||
| Urea (mmol/L) | 9.3 (6.0–14.0) | 7.5 (5.3–11.0) | 13.0 (8.8–18.8) | <0.001 |
| Creatinine (μmol/L) | 117.6 (88.4–164.5) | 100.4 (79.6–132.6) | 159.6 (123.8–236.5) | <0.001 |
| Na (mmol/L) | 137 (134–140) | 137 (134–140) | 137 (134–140) | 0.708 |
| K (mmol/L) | 4.4 (3.9–4.8) | 4.2 (3.8–4.6) | 4.6 (4.1–5) | <0.001 |
| AST (U/L) | 32 (20–49.4) | 34 (21.8–52.7) | 25 (18–40) | <0.001 |
| ALT (U/L) | 23 (14–35) | 25 (16–38) | 18 (12–30) | <0.001 |
| LDH (U/L) | 320 (239–443) | 334 (239–574.2) | 298 (237.2–376.5) | <0.001 |
| Albumin (g/L) | 34.7 (30–38.9) | 35 (30–39.4) | 35 (30.8–38) | 0.411 |
| Ferritin (μg/L) | 260 (160.5–750) | 371 (162.2–778.2) | 309 (154.5–636.4) | 0.147 |
| Fibrinogen (g/L) | 4.7 (3.5–6.2) | 4.9 (3.9–6.3) | 4.3 (2.9–5.9) | <0.001 |
| D-dimer (mg/L) | 15.1 (8.1–27.9) | 14.1 (7.7–31.0) | 14.8 (8.5–24.7) | 0.929 |
| Procalcitonin (ng/L) | 350 (130–1147.5) | 355 (110–1140) | 260 (130–1065) | 0.861 |
| Hemoglobin (g/dl) | 12.1 (10.6–13.8) | 12.7 (11–14.2) | 11.4 (10.1–13) | <0.001 |
| Leucocyte count (/mm3) | 7835 (5500–11262) | 7540 (5400–10737) | 8490 (6240–11800) | 0.014 |
| Neutrophil count (/mm3) | 5750 (3700–9110) | 5400 (3500–9070) | 6500 (4190–9230) | 0.023 |
| Lymphocyte count (/mm3) | 1100 (700–1520) | 1120 (740–1600) | 1100 (720–1500) | 0.526 |
| Thrombocyte count (x1000/mm3) | 202.5 (151–274.5) | 200.5 (152–276.5) | 217.5 (154.5–283.2) | 0.327 |
| CRP levels†, n/N (%) | 0.356 | |||
| Normal | 28/509 (5.5) | 19/317 (6.0) | 9/192 (4.7) | |
| 1/5-fold x ULN | 83/509 (16.3) | 57/317 (18.0) | 26/192 (13.5) | |
| 5/10-fold x ULN | 94/509 (18.5) | 62/317 (19.6) | 32/192 (16.7) | |
| 10/20-fold x ULN | 136/509 (26.7) | 77/317 (24.3) | 59/192 (30.7) | |
| >20-fold x ULN | 168/509 (33.0) | 102/317 (32.2) | 66/192 (34.4) | |
| Unfavorable prognostic signs at any time during hospital stay, n/N (%) | ||||
| Lymphopenia | 387/510 (75.9) | 240/318 (75.5) | 147/192 (76.6) | 0.831 |
| Anemia (Hb <10 g/dL) | 248/510 (48.6) | 150/318 (47.2) | 98/192 (51.0) | 0.412 |
| Thrombocytopenia | 161/506 (31.8) | 102/316 (32.3) | 59/190 (31.1) | 0.844 |
| LDH (>2-fold x ULN) ‡ | 257/493 (52.1) | 171/307 (55.7) | 86/186 (46.2) | 0.051 |
| AST (>2-fold x ULN) ‡‡ | 212/507 (41.8) | 154/316 (48.7) | 58/191 (30.4) | <0.001 |
| Macrophage activation syndrome | 104/472 (22.0) | 72/287 (25.1) | 32/185 (17.3) | 0.053 |
| Shock/severe hypotension | 167/492 (33.9) | 110/302 (36.4) | 57/190 (30.0) | 0.171 |
| Secondary bacterial infection | 208/476 (43.7) | 128/292 (43.9) | 80/184 (43.5) | 1.000 |
| CRP levels†, n/N (%) | 0.940 | |||
| Normal | 17/510 (3.3) | 12/318 (3.8) | 5/192 (2.6) | |
| 1/5-fold x ULN | 38/510 (7.5) | 23/318 (7.2) | 15/192 (7.8) | |
| 5/10-fold x ULN | 56/510 (11.0) | 34/318 (10.7) | 22/192 (11.5) | |
| 10/20-fold x ULN | 114/510 (22.4) | 73/318 (23.0) | 41/192 (21.4) | |
| >20-fold x ULN | 285/510 (55.9) | 176/318 (55.3) | 109/192 (56.8) | |
| Intensive care unit admission, n/N (%) | 239/510 (46.9) | 150/318 (47.2) | 89/192 (46.4) | 0.927 |
| Managements in the intensive care unit, n/N (%) | ||||
| Intubation | 182/237 (76.8) | 116/148 (78.4) | 66/89 (74.2) | 0.525 |
| ECMO | 16/223 (7.2) | 8/137 (5.8) | 8/86 (9.3) | 0.425 |
| Slow continuous dialysis | 39/221 (17.6) | 22/135 (16.3) | 17/86 (19.8) | 0.588 |
| Duration of stay in intensive care unit (days) | 9 (5.8–17) | 10 (6–19) | 8 (5–16) | 0.115 |
| AKI timing, n/N (%) | ||||
| AKI at hospital admission | 225/510 (44.1) | 125/318 (39.3) | 100/192 (52.1) | 0.006 |
| AKI during hospital stay | 285/510 (55.9) | 193/318 (60.7) | 92/192 (47.9) | 0.006 |
| Suspected causes of AKI, n/N (%) 0.222 | ||||
| Prerenal | 229/510 (44.9) | 151/318 (47.5) | 78/192 (40.6) | |
| Renal | 269/510 (52.7) | 158/318 (49.7) | 111/192 (57.8) | |
| Postrenal | 5/510 (1.0) | 3/318 (0.9) | 2/192 (1.0) | |
| Others | 7/510 (1.4) | 6/318 (1.9) | 1/192 (0.5) | |
| Suspected specific causes of AKI, n/N (%) 0.136 | ||||
| Dehydration | 134/510 (26.3) | 82/318 (25.8) | 52/192 (27.1) | |
| GIS loss | 9/510 (1,8) | 6/318 (1.9) | 3/192 (1,6) | |
| Heart failure | 15/510 (2.9) | 9/318 (2.8) | 6/192 (3,1) | |
| Other prerenal causes | 71/510 (13,9) | 54/318 (17.0) | 17/192 (8.9) | |
| Sepsis | 202/510 (39.6) | 112/318 (35.2) | 90/192 (46.9) | |
| Thrombotic microangiopathy | 4/510 (0.8) | 4/318 (1,3) | 0/192 (0) | |
| Extended prerenal causes | 32/510 (6,3) | 21/318 (6.6) | 11/192 (5.7) | |
| Rhabdomyolysis | 2/510 (0,4) | 1/318 (0,3) | 1/192 (0,5) | |
| Nephrotoxic drugs | 29/510 (5,7) | 20/318 (6,3) | 9/192 (4,7) | |
| Postrenal (urological) causes | 5/510 (1.0) | 3/318 (0,9) | 2/192 (1.0) | |
| Others | 7/510 (1,4) | 6/318 (1,9) | 1/192 (0.5) | |
| AKI Stage, n/N (%) 0.287 | ||||
| Stage 1 | 289/510 (56.7) | 186/318 (58.5) | 103/192 (53.6) | |
| Stage 2 | 127/510 (24.9) | 80/318 (25.2) | 47192 (24.5) | |
| Stage 3 | 94/510 (18.4) | 52/318 (16.4) | 42/192 (21.9) | |
| Time between hospitalization and AKI diagnosis (days) | 5 (3–8) | 5 (2.3–8) | 5 (3–7) | 0.654 |
| Dialysis requirement in the ward, n/N (%) | 77/490 (15.7) | 34/289 (11.8) | 43/201 (21.4) | 0.005 |
| KRT indications, n/N (%) 0.185 | ||||
| Increase in serum BUN/creatinine levels | 32/94 (34.0) | 16/46 (34.8) | 16/48 (33.3) | |
| Hyperkalemia | 8/94 (8.5) | 6/46 (13.0) | 2/48 (4.2) | |
| Metabolic acidosis | 24/94 (25.5) | 14/46 (30.4) | 10/48 (20.8) | |
| Hypervolemia | 18/94 (19.1) | 5/46 (10.9) | 13/48 (27.1) | |
| Severe uremic symptoms | 3/94 (3.2) | 2/46 (4.3) | 1/48 (2.1) | |
| Others | 9/94 (9.6) | 3/46 (6.5) | 6/48 (12.5) | |
| Renal Outcome, n/N (%) | <0.001 | |||
| Complete recovery | 285/333 (85.6) | 192/209 (91.9) | 93/124 (75) | |
| Partially recovery | 46/333 (13.8) | 17/209 (8.1) | 29/124 (23.4) | |
| Dialysis dependence | 2/333 (0.6) | 0/209 (0) | 2/124 (1.6) | |
| Duration of AKI in discharged patients (days) | 6 (3–9) | 5 (3–8) | 7 (4–10) | <0.001 |
| Patient Outcome, n/N (%) | ||||
| Discharged | 336/510 (65.9) | 210/318 (66.0) | 126/192 (65.6) | |
| Dead | 174/510 (34.1) | 108/318 (34.0) | 66/192 (34.4) | |
| Total hospital stays (days) | 12 (8–19) | 12 (8–20) | 12 (8–18) | 0.446 |
ACE-I, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; COVID-19 coronavirus disease 2019; eGFR, estimated glomerular filtration rate; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactate dehydrogenase; x ULN, increase above upper normal limit; CRP, C-reactive protein; ECMO, extracorporeal membrane oxygenation; KRT, kidney replacement therapy.
Data were expressed as median [Q1-Q3] or as number (percent).
†The upper limit of the normal range of CRP was 5 mg/L (47.6 nmol/L).
‡The upper limit of the normal range of LDH was 248 U/L.
‡‡The upper limit of the normal range of AST was 37 U/L.
In patients with an eGFR level in the last year (n = 447), the prevalence of CKD stage 3, 4, and 5 was 25.3%, 12.3%, and 5.1%, respectively. Patients who had CKD were older and had more comorbidities, including diabetes mellitus, hypertension, chronic obstructive pulmonary disease, and heart disease.
The incidence of AKI at admission was higher in patients with CKD than those without CKD (52.1% vs. 39.3%, respectively, p = 0.006). The requirement for hemodialysis in CKD patients followed on the ward was more frequent, whereas intensive care admission and slow continuous dialysis rates were not different compared to non-CKD patients (Table 2).
Survival
The demographic and clinical characteristics of discharged and deceased patients are listed in Table 3 and S5 Table. There were 225 (38.9%) deaths in the overall cohort. During hospitalization, 34.4% of patients with CKD and 34.0% of patients without CKD died. The in-hospital mortality rate was 18.9% (n = 59), 46.2% (n = 66), and 81.3% (n = 100) among those with AKI stages 1, 2, and 3, respectively.
Table 3. Characteristics of COVID-19 RT-PCR positive patients based on patient survival.
| Variable | Total (n = 578) | Discharged (n = 353) | Dead (n = 225) | p |
|---|---|---|---|---|
| Age (years) | 69 (59–77) | 67 (57–77) | 72 (63–78) | 0.001 |
| Male, n/N (%) | 352/578 (60.9) | 203/353 (57.5) | 149/225 (66.2) | 0.036 |
| Comorbid conditions, n/N (%) | ||||
| Diabetes mellitus | 249/569 (43.8) | 143/349 (41) | 106/220 (48.2) | 0.091 |
| Hypertension | 399/566 (70.5) | 256/346 (74) | 143/220 (65) | 0.022 |
| Chronic kidney disease | 192/510 (37.6) | 126/336 (37.5) | 66/174 (37.9) | 0.924 |
| Obesity | 27/462 (5.8) | 18/292 (6.2) | 9/170 (5.3) | 0.701 |
| Chronic obstructive lung disease | 89/549 (16.2) | 53/343 (15.5) | 36/206 (17.5) | 0.533 |
| Coronary heart disease | 172/541 (31.8) | 101/338 (29.9) | 71/203 (35) | 0.218 |
| Heart failure | 85/528 (16.1) | 52/331 (15.7) | 33/197 (16.8) | 0.753 |
| Cerebrovascular disease | 39/546 (7.1) | 15/341 (4.4) | 24/205 (11.7) | 0.001 |
| Cancer | 69/554 (12.5) | 26/342 (7.6) | 43/212 (20.3) | <0.001 |
| Chronic liver disease | 10/556 (1.8) | 5/343 (1.5) | 5/213 (2.3) | 0.518 |
| Autoimmune/autoinflammatory disease | 25/556 (4.5) | 15/343 (4.4) | 10/213 (4.7) | 0.859 |
| Medications, n/N (%) | ||||
| ACE-I or ARB | 266/505 (52.7) | 193/321 (60.1) | 73/184 (39.7) | <0.001 |
| Ca antagonists | 171/491 (34.8) | 113/309 (36.6) | 58/182 (31.9) | 0.291 |
| Beta blockers | 216/491 (44) | 141/309 (45.6) | 75/182 (41.2) | 0.340 |
| Other antihypertensives | 113/476 (23.7) | 70/304 (23) | 43/172 (25) | 0.627 |
| Insulin | 122/484 (25.2) | 73/304 (24) | 49/180 (27.2) | 0.432 |
| Oral antidiabetics | 127/486 (26.1) | 82/304 (27) | 45/182 (24.7) | 0.585 |
| Statins | 88/477 (18.4) | 48/302 (15.9) | 40/175 (22.9) | 0.059 |
| Antiaggregant or anticoagulant drugs | 251/501 (50.1) | 152/312 (48.7) | 99/189 (52.4) | 0.427 |
| Smoking status, n/N (%) 0.488 | ||||
| Never | 221/411 (53.8) | 148/265 (55.8) | 73/146 (50) | |
| Current | 34/411 (8.3) | 20/265 (7.5) | 14/146 (9.6) | |
| Former | 156/411 (38) | 97/265 (36.6) | 59/146 (40.4) | |
| Symptoms related to COVID-19, n/N (%) | ||||
| Fever | 380/565 (67.3) | 235/351 (67) | 145/214 (67.8) | 0.843 |
| Fatigue | 356/563 (63.2) | 228/347 (65.7) | 128/216 (59.3) | 0.123 |
| Dyspnea | 375/569 (65.9) | 206/351 (58.7) | 169/218 (77.5) | <0.001 |
| Cough | 408/564 (72.3) | 255/349 (73.1) | 153/215 (71.2) | 0.624 |
| Anorexia | 132/540 (24.4) | 87/339 (25.7) | 45/201 (22.4) | 0.392 |
| Myalgia | 192/542 (35.4) | 129/343 (37.6) | 63/199 (31.7) | 0.163 |
| Headache | 82/545 (15) | 50/343 (14.6) | 32/202 (15.8) | 0.690 |
| Sore throat | 72/546 (13.2) | 52/344 (15.1) | 20/202 (9.9) | 0.082 |
| Diarrhea | 32/551 (5.8) | 25/347 (7.2) | 7/204 (3.4) | 0.067 |
| Others | 40/508 (7.9) | 23/323 (7.1) | 17/185 (9.2) | 0.405 |
| Asymptomatic | 4/519 (0.8) | 4/324 (1.2) | 0/195 (0) | |
| Radiologic examination, n/N (%) | ||||
| Patients with a chest CT scan | 563/572 (98.4) | 349/351 (99.4) | 214/221 (96.8) | 0.031 |
| Patients with specific chest CT findings | 529/564 (93.8) | 327/350 (93.4) | 202/214 (94.4) | 0.645 |
| Patients with specific bilaterally chest CT findings | 472/549 (86) | 282/341 (82.7) | 190/208 (91.3) | 0.005 |
| Specific chest CT findings, n/N (%) | ||||
| Ground glass opacity | 503/535 (94) | 307/330 (93) | 196/205 (95.6) | 0.221 |
| Reticular opacity | 155/428 (36.2) | 98/270 (36.3) | 57/158 (36.1) | 0.963 |
| Bronchial wall thickening | 79/428 (18.5) | 49/270 (18.1) | 30/158 (19) | 0.829 |
| Pleural effusion | 100/427 (23.4) | 52/269 (19.3) | 48/158 (30.4) | 0.009 |
| Thoracic lymphadenopathy | 53/424 (12.5) | 35/268 (13.1) | 18/156 (11.5) | 0.648 |
| Oxygen saturation in room air at diagnosis, n/N (%) | <0.001 | |||
| Normal | 129/551 (23.4) | 111/335 (33.1) | 18/216 (8.3) | |
| 90–95% | 210/551 (38.1) | 155/335 (46.3) | 55/216 (25.5) | |
| <90% | 212/551 (38.5) | 69/335 (20.6) | 143/216 (66.2) | |
| Severity of COVID-19 infection <0.001 | ||||
| Asymptomatic | 13/578 (2.2) | 12/353 (3.4) | 1/225 (0.4) | |
| Mild to moderate | 196/578 (33.9) | 169/353 (47.9) | 27/225 (12) | |
| Severe | 256/578 (44.3) | 145/353 (41.1) | 111/225 (49.3) | |
| Critical | 113/578 (19.6) | 27/353 (7.6) | 86/225 (38.2) | |
| Data for renal function within the last year | ||||
| Serum creatinine (μmol/L) | 88.4 (70.7–106.1) | 88.4 (70.7–123.8) | 79.6 (70.7–106.1) | 0.010 |
| eGFR (mL/min/1.73 m2) | 65.3 (40.6–96.6) | 63.1 (36.9–90.3) | 74.7 (48.7–102.1) | 0.005 |
| CKD stages in patients with known eGFR 0.040 within the last year (n = 317), n/N (%) | ||||
| eGFR>90 ml/min/1.73m2 | 130/447 (29.1) | 67/273 (24.5) | 63/174 (36.2) | |
| eGFR 60–90 ml/min/.73m2 | 126/447 (28.2) | /273 (29.3) | 46/174 (26.4) | |
| CKD stage 3 | 113/447 (25.3) | 69/273 (25.3) | 44/174 (25.3) | |
| CKD stage 4 | 55/447 (12.3) | 40/273 (14.7) | 15/174 (8.6) | |
| CKD stage 5 | 23/447 (5.1) | 17/273 (6.2) | 6/174 (3.4) | |
| CKD stage 4 and 5 (eGFR<30 ml/dk/1.73 m2) | 78/578 (13.5) | 57/353 (16.1) | 21/225 (38.9) | 0.024 |
| Laboratory parameters at hospital admission | ||||
| Urea (mmol/L) | 9.3 (6.0–14.0) | 9.2 (6.0–13.6) | 9.3 (6.0–14.8) | 0.783 |
| Creatinine (μmol/L) | 117.6 (88.4–164.4) | 123.8 (95.5–160.9) | 106.1 (79.6–168.0) | 0.005 |
| Na (mmol/L) | 137 (134–140) | 137 (134–140) | 136 (133–140) | 0.357 |
| K (mmol/L) | 4.4 (3.9–4.8) | 4.4 (4–4.8) | 4.245 (3.8–4.7) | 0.009 |
| AST (U/L) | 32 (20–49.4) | 26.5 (19–40) | 41 (27–66) | <0.001 |
| ALT (U/L) | 23 (14–35) | 21 (14–32.5) | 24.55 (14–43) | 0.014 |
| LDH (U/L) | 320 (239–443) | 285 (224–383) | 383 (297–570) | <0.001 |
| Albumin (g/L) | 34.7 (30–38.9) | 37.0 (32.6–39.8) | 31.0 (28.0–35.0) | <0.001 |
| Ferritin (μg/L) | 360 (162–748) | 267 (137–632) | 511.35 (286–968) | <0.001 |
| Fibrinogen (g/L) | 4.8 (3.5–6.2) | 4.5 (3.3–6.0) | 4.9 (3.9–6.3) | 0.029 |
| D-dimer (mg/L) | 14.6 (8.1–27.9) | 13.5 (7.9–24.0) | 15.1 (9.3–33.1) | 0.056 |
| Procalcitonin (ng/L) | 350 (130–114.5) | 230 (100–780) | 830 (220–1780) | <0.001 |
| Hemoglobin (g/dl) | 12.1 (10.6–13.8) | 12.45 (11–14) | 11.8 (10–13.3) | <0.001 |
| Leucocyte count(/mm3) | 7835 (5500–11250) | 7420 (5370–10200) | 8700 (5900–12290) | 0.003 |
| Neutrophil count (/mm3) | 5750 (3700–9110) | 5300 (3600–7810) | 7100 (4200–10310) | <0.001 |
| Lymphocyte count (/mm3) | 1100 (700–1520) | 1200 (900–1600) | 885 (580–1400) | <0.001 |
| Thrombocyte count (x1000/mm3) | 202.5 (151–274) | 209.5 (160,6–280) | 190 (138–266) | 0,016 |
| CRP levels†, n/N (%) <0.001 | ||||
| Normal | 28/576 (4,9) | 26/352 (7,4) | 2/224 (0,9) | |
| 1/5-fold x ULN | 91/576 (15,8) | 76/352 (21,6) | 15/224 (6,7) | |
| 5/10-fold x ULN | 103/576 (17,9) | 72/352 (20,5) | 31/224 (13,8) | |
| 10/20-fold x ULN | 150/576 (26) | 89/352 (25,3) | 61/224 (27,2) | |
| >20-fold x ULN | 204/576 (35,4) | 89/352 (25,3) | 115/224 (51,3) | |
| Unfavorable prognostic signs at any time during hospital stay, n/N (%) | ||||
| Lymphopenia | 88/577 (15.3) | 47/353 (13.3) | 41/224 (18.3) | 0.104 |
| Anemia (Hb <10 g/dL) | 443/578 (76.6) | 249/353 (70.5) | 194/225 (86.2) | <0.001 |
| Thrombocytopenia | 293/578 (50.7) | 135/353 (38.2) | 158/225 (70.2) | <0.001 |
| LDH (>2-fold x ULN) ‡ | 189/574 (32.9) | 82/353 (23.2) | 107/221 (48.4) | <0.001 |
| AST (>2-fold x ULN) ‡‡ | 303/559 (54.2) | 142/347 (40.9) | 161/212 (75.9) | <0.001 |
| Macrophage activation syndrome | 254/575 (44.2) | 102/353 (28.9) | 152/222 (68.5) | <0.001 |
| Shock/severe hypotension | 124/519 (23.9) | 32/340 (9.4) | 92/179 (51.4) | <0.001 |
| Secondary bacterial infection | 213/557 (38.2) | 21/342 (6.1) | 192/215 (89.3) | <0.001 |
| CRP levels†, n/N (%) | <0.01 | |||
| Normal | 17/578 (2.9) | 17/353 (4.8) | 0/225 (0) | |
| 1/5-fold x ULN | 40/578 (6.9) | 38/353 (10.8) | 2/225 (0.9) | |
| 5/10-fold x ULN | 59/578 (10.2) | 51/353 (14.4) | 8/225 (3.6) | |
| 10/20-fold x ULN | 124/578 (21.5) | 90/353 (25.5) | 34/225 (15.1) | |
| >20-fold x ULN | 338/578 (58.5) | 157/353 (44.5) | 181/225 (80.4) | |
| Intensive care unit admission, n/N (%) | 291/578 (50.3) | 72/353 (20.4) | 219/225 (97.3) | <0.001 |
| Managements in the intensive care unit, n/N (%) | ||||
| Intubation | 232/288 (80.6) | 25/72 (34.7) | 207/216 (95.8) | <0.001 |
| ECMO | 18/543 (3.3) | 0/70 (0) | 18/195 (9.2) | 0.003 |
| Slow continuous dialysis | 53/260 (20.4) | 9/71 (12.7) | 44/159 (23.3) | 0.039 |
| Duration of stay in intensive care unit (days) | 9 (6–17) | 8.5 (6–16) | 9 (5–17) | 0.965 |
| AKI timing, n/N (%) | ||||
| AKI at hospital admission | 251/578 (43.4) | 171/251 (68.1) | 80/251 (31.9) | 0.003 |
| AKI during hospital stay | 327/578 (56.6) | 182/327 (55.7) | 145/327 (44.3) | 0.003 |
| AKI Stage, n/N (%) <0.001 | ||||
| Stage 1 | 312/578 (54) | 253/353 (71.7) | 59/225 (26.2) | |
| Stage 2 | 143/578 (24.7) | 77/353 (21.8) | 66/225 (29.3) | |
| Stage 3 | 123/578 (21.3) | 23/353 (6.5) | 100/225 (44.4) | |
| Suspected causes of AKI, n/N (%) | <0.001 | |||
| Prerenal | 251/578 (43.4) | 220/353 (62.3) | 31/225 (13.8) | |
| Renal | 311/578 (53.8) | 124/353 (35.1) | 187/225 (83.1) | |
| Postrenal | 6/578 (1) | 5/353 (1.4) | 1/225 (0.4) | |
| Others | 10/578 (1.7) | 4/353 (1.1) | 6/225 (2.7) | |
| Time between hospitalization and AKI diagnosis (days) | 5 (3–8) | 4 (2–7) | 5 (3–9) | 0.304 |
| Dialysis requirement in the ward, n/N (%) | 91/554 (16.4) | 10/343 (2.9) | 81/211 (38.4) | <0.001 |
| Total hospital stays (days) | 12 (8–19) | 12 (8–17) | 13 (9–21) | 0.103 |
ACE-I, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; COVID-19, coronavirus disease 2019; eGFR, estimated glomerular filtration rate; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDH, lactate dehydrogenase; x ULN, increase above upper normal limit; CRP, C-reactive protein; ECMO, extracorporeal membrane oxygenation.
Data were expressed as median [Q1-Q3] or as number (percent).
†The upper limit of the normal range of CRP was 5 mg/L (47.6 nmol/L).
The upper limit of the normal range of LDH was 248 U/L.
‡‡The upper limit of the normal range of AST was 37 U/L.
In the multivariate Cox regression analysis; age, male gender, diabetes, and cerebrovascular disease, LDH (greater than twofold the ULN), and AKI stages were independently associated with in-hospital mortality (Table 4). Adjusted in-hospital mortality was increased in patients with AKI stage 2 (HR 1.98, 95%CI 1.25–3.14, p = 0.003) and stage 3 (HR 2.25, 95%CI 1.44–3.51, p = 0.0001) compared to those with AKI stage 1.
Table 4. Covariates associated with death by Cox survival analysis.
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | P | |
| Age (years) | 1.01 | 0.99–1.03 | 0.068 | 1.01 | 1.00–1.03 | 0.035 |
| Male gender | 1.46 | 1.01–2.11 | 0.042 | 1.47 | 1.04–2.09 | 0.029 |
| Diabetes mellitus | 1.55 | 1.03–2.32 | 0.034 | 1.51 | 1.06–2.17 | 0.022 |
| Hypertension | 0.94 | 0.62–1.43 | 0.797 | |||
| Cerebrovascular disease | 1.90 | 1.11–3.26 | 0.019 | 1.82 | 1.08–3.07 | 0.023 |
| Malignancy | 1.12 | 0.70–1.78 | 0.631 | |||
| Oxygen saturation in room air at hospital admission (<90%) | 1.25 | 0.68–2.29 | 0.463 | |||
| eGFR in previous year (ml/min/1.73m2) | 0.99 | 0.99–1.00 | 0.402 | |||
| Serum albumin (g/L) | 0.74 | 0.54–1.03 | 0.082 | 0.74 | 0.54–1.01 | 0.064 |
| CRP (>20-fold x ULN) | 0.88 | 0.61–1.26 | 0.494 | |||
| LDH (>2-fold x ULN) | 1.45 | 0.95–2.20 | 0.079 | 1.55 | 1.05–2.30 | 0.027 |
| Lymphocyte count (mm3) | 1.00 | 1.00–1.00 | 0.708 | |||
| Thrombocyte count (mm3) | 0.99 | 0.99–1.00 | 0.047 | 0.99 | 0.99–1.00 | 0.052 |
| AKI stage 1 (ref) | ||||||
| AKI stage 2 | 1.85 | 1.15–2.98 | 0.011 | 1.98 | 1.25–3.14 | 0.003 |
| AKI stage 3 | 2.19 | 1.40–3.43 | <0.001 | 2.25 | 1.44–3.51 | <0.001 |
CRP, C-reactive protein; LDH, lactate dehydrogenase.
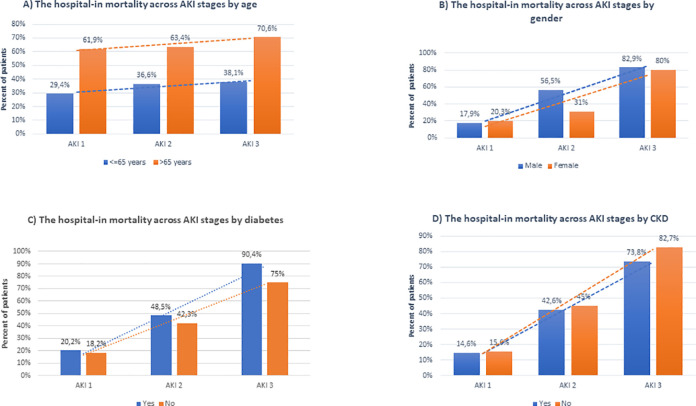
The in-hospital mortality rates across AKI stages by age, gender, diabetes mellitus, and CKD were shown in Fig 2.
Fig 2.
The in-hospital mortality rate across acute kidney injury (AKI) stages by age (A), gender (B), diabetes mellitus (C), and chronic kidney disease (CKD) (D).
Renal outcomes
Patients who died during hospitalization were excluded from the analysis of renal outcomes (S6 Table). Renal improvement was complete in 81.7% (285 of 349 patients) and partial in 17.2% (60 of 349 patients) of the patients. In 1.1% of the patients (4 of 349 patients), there was no improvement in renal function (n = 1) or the patient remained dialysis-dependent (n = 3) at discharge.
The complete recovery rate was 84.2%, 76.6%, and 56.5% in AKI stages 1, 2, and 3, respectively (S3 Table). The complete recovery rate was 75.0% and 91.9% in patients with CKD and non-CKD, respectively (p = 0.042). Although partial recovery was more frequent in patients with CKD (23.4% vs. 8.1%, p = 0.010), few patients were dialysis-dependent at discharge (0 [0%] and two [1.6%]) patients in the non-CKD and CKD groups, respectively) (Table 2). In a patient who was dialysis-dependent at discharge, baseline CKD status was unknown.
Discussion
In this multicenter retrospective study, we documented the characteristics and renal and patient outcomes of 578 hospitalized patients with COVID-19 and AKI. The in-hospital mortality rate was remarkably high in these patients and increased with AKI stage. Older age, male gender, baseline diabetes mellitus and cerebrovascular disease, increased LDH, and severity of AKI were independently associated with mortality. The renal outcomes were also worse in patients with prior CKD and those with AKI stage 3.
The incidence of AKI among patients with COVID-19 and its association with outcomes were assessed in a systematic review and meta-analysis that included 20 cohorts covering 13,137 patients [33]. In this analysis, the prevalence of AKI among patients with COVID-19 was 17% (range, 0.5–80%). The variance in the prevalence of AKI among the cohorts was attributed to different clinical practices and patient characteristics as well as the severity of underlying disease and/or of AKI (28). In patients with AKI, the mortality rate was estimated at 52% (range, 7–100%) [33]. Similarly, AKI was consistently associated with increased mortality, although the magnitude of the increased risk varied. The mortality rate was increased in patients with AKI compared to those without AKI (pooled OR, 15.27; 95% CI, 4.82–48.36) [33]. In this study, the mortality rate was 38.9% in patients with COVID-19 and AKI. In our cohort, 50.3% of the patients were admitted to ICU, among whom 80.6% and 6.8% were intubated and treated with ECMO, respectively.
Diabetes and hypertension were independent risk factors for AKI in patients with COVID-19. Hence, it was not surprising that these frequencies were higher in our cohort of patients with COVID-19 and AKI. However, the frequency of CKD (37.6%) was higher than that in most previous studies (5% of all patients; range, 0.6–57.1%) [33]. In our cohort, we determined the eGFR values within the last year of 447 of the 578 patients; therefore, the CKD incidence may be more precise. By contrast, the prevalence of CKD was documented in all patients (regardless of AKI) in two previous studies [5, 34], whereas our AKI cohort included only patients with acute injury-on-chronic kidney disease. In a cohort of 3235 patients with COVID-19, the CKD prevalence was significantly higher in patients with AKI compared to those without AKI (17.3% vs. 4.4%, respectively, p < 0.001). It is expected that patients with COVID-19 and CKD are susceptible to AKI [35].
The mortality risk is increased in patients with COVID-19 and various forms of CKD [24–27, 36]. In a study of United Kingdom study involving more than 17 million people using the OpenSAFELY health analytics platform, patients with CKD (eGFR < 60 mL/min/1.73 m2) had an increased risk for mortality, particularly those with advanced CKD, dialysis, or kidney transplant [27]. European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) registry data and the ERA- COVID-19 Database (ERACODA) collaboration also demonstrated that dialysis and kidney transplant recipients with COVID-19 had an increased mortality risk [24, 25]. A nationwide study in Turkey revealed that the risk of ICU admission and in-hospital mortality was increased in patients with CKD stage 3–5 compared to those without kidney disease [26].
Data on the outcome of AKI in COVID-19 patients with baseline pre-dialysis CKD are sparse [35, 37]. Patients with COVID-19 plus CKD and AKI had a higher mortality rate compared to those with only AKI or CKD (74.7% vs. 53.8% vs. 67%, respectively) [35]. Peng et al. reported that AKI diagnosis before the onset date of any other organ dysfunction (AKI-early) was less frequent in patients with CKD [37]. In our study, the frequency of CKD stage 3, 4, and 5 non-dialysis was 25.3%, 12.3%, and 5.1%, respectively, among the patients with AKI. The mortality rates were not different in patients with CKD (even across CKD subgroups) compared to patients who did not have CKD. Previous observational studies showed that CKD may modify the impact of AKI on mortality in non-COVID era [38–41]. The Program to Improve Care in Acute Renal Disease (PICARD) study revealed the unexpected reduced in-hospital mortality rate in patients who had prior CKD among critically ill patients with AKI [39]. In a large-scale study, preexisting CKD had similar adjusted in-hospital mortality risk across AKI stages, whereas mortality or ESKD risk increased in patients with baseline CKD during follow-up after discharge [41]. In contrast, increased in-hospital death rate was reported in CKD patients with AKI stage 2 and 3, but not AKI stage 1 [42]. Underlining mechanism(s) of these associations is not clear because of observational nature of the studies. It was postulated that earlier AKI diagnosis and/or nephrology consultation may influence the medical care or attention delivered to patients with CKD which might have resulted in favorable or at least unchanged patient outcomes in this population [39, 40]. On the other hand, small increase in serum creatinine levels at hospital admission was not a risk factor for in-hospital mortality in patients with CKD stage 4 to 5 [43]. It may reflect limited clinical significance of stage 1 AKI in advanced CKD due to erratic oscillations in serum creatinine (and/or transient renal ischemia which may result in increase in serum creatinine in CKD patients who already have reduced renal reserve [42]. Furthermore, acute renal and systemic injury may be more intensive in non-CKD patients compared to patients with CKD in certain AKI stages even if the same definitions based on serum creatinine measurement for the staging of AKI are used.
Older age, male gender, and comorbidities, including diabetes and cerebrovascular disease, were independently associated with mortality in patients with COVID-19 and AKI. These are risk factors for mortality in patients with COVID-19 [44]. Notably, the severity of AKI according to the KDIGO stage, was also a risk factor for mortality in our multivariate regression analysis. Two studies have reported the distribution of AKI stages and patient outcomes by AKI stage [11, 19]. The frequencies of AKI stages were reportedly 45.7–46.5% stage 1, 22.4–22.9% stage 2 and 31.1–31.4% stage 3, and the mortality rate increased with the severity of AKI [11, 19]. In our cohort, the proportions of AKI stages were 54%, 24.7%, and 21.3% for AKI stage 1, 2, and 3, respectively.
There are few studies to document kidney outcomes in patients with AKI and COVID-19 [45, 46]. The rates of renal recovery in these studies have varied from 65% to 74.1%. In the present cohort, complete renal recovery was observed as 80.7% which was relatively higher compared to these studies. The lower frequency of AKI stage 3 (21.3%) among the AKI patients compared to other studies (approximately 42%) may explain higher rate of renal recovery in our cohort. We also observed that complete recovery rates were worse in patients with baseline CKD or AKI stage 3.
Distinct direct or indirect pathogenic mechanisms have been implicated in AKI development in patients with COVID-19 [23, 47]. Some post-mortem studies showed direct kidney invasion by the virus [48, 49], but others did not [50–52]. In our cohort, the frequencies of prerenal and renal AKI among patients with AKI were 43.4% and 53.8%, respectively. However, we did not have urinalysis results, precluding determination of the etiology of AKI. A previous study from New York suggested that 66% of patients with AKI had a prerenal AKI state according to the urine sodium level [11].
This study had several limitations. First, a matched control group of patients without AKI or patients with non-COVID-19 AKI was not included in the survival analysis. Second, we had no urinalysis data for diagnosing the cause of AKI and identifying abnormalities such as hematuria and/or proteinuria, which are frequently observed in these patients. Third, we did not have any follow-up data after discharge. Also, we could not examine the effects of medications for the treatment of COVID-19 on the results because of the lack of information on the dose and duration of administration. Finally, because this was an observational study, we cannot interpret the causality of the relationship between exposures and outcomes.
The management of COVID-19 and AKI is not significantly different from other causes of AKI. The strategies in prevention of AKI includes early fluid management in hypovolemia or fluid and vasopressor resuscitation in septic shock may reduce the risk of AKI [47]. In COVID-19 patients who already have AKI, the goals of management should be to improve patient outcomes and prevent deterioration of AKI. The management include hemodynamic optimization to correct hypovolemia or hypervolemia, glucose management, avoiding nephrotoxic drugs or radiocontrast when possible and standard caring in multiorgan failure [47]. In patients who need KRT, it is important to provide KRT resources and to begin appropriate KRT modality with adequate dose at the right time.
In conclusion, AKI is associated with remarkably high mortality among hospitalized COVID-19 patients. The severity of AKI parallel with the severity of COVID-19 and COVID-19 related in-hospital outcomes. The risk factors reportedly associated with mortality in patients with COVID-19, such as older age, male gender, and comorbidities, including diabetes mellitus, were also valid among patients with COVID-19 and AKI. Renal problems continue in a significant portion of discharged patients, though few patients depend on dialysis. As AKI stage increases, the complete recovery rate decreases. The complete recovery rate of AKI is lower in patients with CKD than in patients with non-CKD. Early management is needed to improve patient and renal outcomes in patients with COVID-19 and AKI.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(SAV)
Acknowledgments
We thank OMEGA Contract Research Organization in Turkey for data processing and statistical analysis.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was unconditionally supported by the Turkish Society of Nephrology.
References
- 1.https://www.who.int/publications/m/item/weekly-epidemiological -update—-29-december-2020. [Google Scholar]
- 2.Pan XW, Xu D, Chen WJ, Chen JX, Ye JQ, Zuo L, et al. Acute kidney injury during the COVID-19 outbreak. Nephrol Dial Transplant. 2020;35(9):1635–41. Epub 2020/09/06. doi: 10.1093/ndt/gfaa218 ; PubMed Central PMCID: PMC7529117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13. Epub 2020/02/03. doi: 10.1016/S0140-6736(20)30211-7 ; PubMed Central PMCID: PMC7135076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diao B, Wang C, Wang R, Feng Z, Tan Y, Wang H, et al. Human Kidney is a Target for Novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. medRxiv. 2020:2020.03.04.20031120. doi: 10.1101/2020.03.04.20031120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. Epub 2020/02/29. doi: 10.1056/NEJMoa2002032 ; PubMed Central PMCID: PMC7092819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. Epub 2020/02/08. doi: 10.1001/jama.2020.1585 ; PubMed Central PMCID: PMC7042881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L, Li X, Chen H, Yan S, Li D, Li Y, et al. Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China. Am J Nephrol. 2020;51(5):343–8. Epub 2020/04/02. doi: 10.1159/000507471 ; PubMed Central PMCID: PMC7179524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–81. Epub 2020/02/28. doi: 10.1016/S2213-2600(20)30079-5 ; PubMed Central PMCID: PMC7102538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. Epub 2020/04/21. doi: 10.1016/j.jcv.2020.104364; PubMed Central PMCID: PMC7194884 conflicts of interest. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323(16):1612–4. Epub 2020/03/20. doi: 10.1001/jama.2020.4326 ; PubMed Central PMCID: PMC7082763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98(1):209–18. Epub 2020/05/18. doi: 10.1016/j.kint.2020.05.006 ; PubMed Central PMCID: PMC7229463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohamed MMB, Lukitsch I, Torres-Ortiz AE, Walker JB, Varghese V, Hernandez-Arroyo CF, et al. Acute Kidney Injury Associated with Coronavirus Disease 2019 in Urban New Orleans. Kidney360. 2020;1(7):614–22. doi: 10.34067/kid.0002652020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–9. Epub 2020/04/23. doi: 10.1001/jama.2020.6775 ; PubMed Central PMCID: PMC7177629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolhe NV, Fluck RJ, Selby NM, Taal MW. Acute kidney injury associated with COVID-19: A retrospective cohort study. PLOS Medicine. 2020;17(10):e1003406. doi: 10.1371/journal.pmed.1003406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–38. Epub 2020/04/06. doi: 10.1016/j.kint.2020.03.005 ; PubMed Central PMCID: PMC7110296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. Epub 2020/03/15. doi: 10.1016/S0140-6736(20)30566-3 ; PubMed Central PMCID: PMC7270627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Argenziano MG, Bruce SL, Slater CL, Tiao JR, Baldwin MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. Epub 2020/05/31. doi: 10.1136/bmj.m1996; PubMed Central PMCID: PMC7256651 at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no competing interests with regards to the submitted work; MMS reports grants from Amgen, outside the submitted work; JJC reports personal fees from Allergan, outside the submitted work; RGB reports grants from Alpha1 Foundation and COPD Foundation, outside the submitted work; GH reports grants from Janssen Research, outside the submitted work; the remaining authors have nothing to disclose. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. Epub 2020/01/28. doi: 10.1016/S0140-6736(20)30183-5 ; PubMed Central PMCID: PMC7159299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pei G, Zhang Z, Peng J, Liu L, Zhang C, Yu C, et al. Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia. J Am Soc Nephrol. 2020;31(6):1157–65. Epub 2020/04/30. doi: 10.1681/ASN.2020030276 ; PubMed Central PMCID: PMC7269350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ICNARC report on COVID-19 in critical care 01 May 2020. Available from: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports.
- 21.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical Characteristics of Covid-19 in New York City. N Engl J Med. 2020;382(24):2372–4. Epub 2020/04/18. doi: 10.1056/NEJMc2010419 ; PubMed Central PMCID: PMC7182018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pan XW, Xu D, Zhang H, Zhou W, Wang LH, Cui XG. Identification of a potential mechanism of acute kidney injury during the COVID-19 outbreak: a study based on single-cell transcriptome analysis. Intensive Care Med. 2020;46(6):1114–6. Epub 2020/04/03. doi: 10.1007/s00134-020-06026-1 ; PubMed Central PMCID: PMC7106051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Izzedine H, Jhaveri KD. Acute kidney injury in patients with COVID-19: an update on the pathophysiology. Nephrol Dial Transplant. 2020. Epub 2020/09/06. doi: 10.1093/ndt/gfaa184; PubMed Central PMCID: PMC7499744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hilbrands LB, Duivenvoorden R, Vart P, Franssen CFM, Hemmelder MH, Jager KJ, et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol Dial Transplant. 2020;35(11):1973–83. Epub 2020/11/06. doi: 10.1093/ndt/gfaa261 ; PubMed Central PMCID: PMC7665620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jager KJ, Kramer A, Chesnaye NC, Couchoud C, Sanchez-Alvarez JE, Garneata L, et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98(6):1540–8. Epub 2020/09/27. doi: 10.1016/j.kint.2020.09.006 ; PubMed Central PMCID: PMC7560263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozturk S, Turgutalp K, Arici M, Odabas AR, Altiparmak MR, Aydin Z, et al. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrol Dial Transplant. 2020;35(12):2083–95. Epub 2020/12/05. doi: 10.1093/ndt/gfaa271 ; PubMed Central PMCID: PMC7716804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6. Epub 2020/07/09. doi: 10.1038/s41586-020-2521-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.European Centre for Disease Prevention and Control. Case definition for coronavirus disease 2019 (COVID-19) Accessed 29, May 2020. Available from: https://www.ecdc.europa.eu/en/covid19/surveillance/case-definition.
- 29.World Health Organization. Report of the WHO–China Joint Mission on Coronavirus Disease 2019 (COVID-19), 16–24. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 30.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Workgroup. KDIGO clinical practice guideline for acute kidney injury. Kidney International Supplements. 2(1):1–138. doi: 10.1038/kisup.2012.1 [DOI] [Google Scholar]
- 31.NHS England. Acute kidney injury (AKI) algorithm [Accessed May 5, 2020]. Available from: https://www.england.nhs.uk/akiprogramme/aki-algorithm.
- 32.Levey AS, Stevens LA. Estimating GFR using the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation: more accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55(4):622–7. Epub 2010/03/27. doi: 10.1053/j.ajkd.2010.02.337 ; PubMed Central PMCID: PMC2846308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robbins-Juarez SY, Qian L, King KL, Stevens JS, Husain SA, Radhakrishnan J, et al. Outcomes for Patients With COVID-19 and Acute Kidney Injury: A Systematic Review and Meta-Analysis. Kidney Int Rep. 2020;5(8):1149–60. Epub 2020/08/11. doi: 10.1016/j.ekir.2020.06.013 ; PubMed Central PMCID: PMC7314696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. Epub 2020/03/29. doi: 10.1136/bmj.m1091; PubMed Central PMCID: PMC7190011 at www.icmje.org/coi_disclosure.pdf and declare: support from the Tongji Hospital for Pilot Scheme Project and the Chinese National Thirteenth Five Years Project in Science and Technology, National Commission of Health, People’s Republic of China, for the submitted work; no financial relationships with any organisation that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russo E, Esposito P, Taramasso L, Magnasco L, Saio M, Briano F, et al. Kidney disease and all-cause mortality in patients with COVID-19 hospitalized in Genoa, Northern Italy. J Nephrol. 2020. Epub 2020/10/08. doi: 10.1007/s40620-020-00875-1; PubMed Central PMCID: PMC7538179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flythe JE, Assimon MM, Tugman MJ, Chang EH, Gupta S, Shah J, et al. Characteristics and Outcomes of Individuals With Pre-existing Kidney Disease and COVID-19 Admitted to Intensive Care Units in the United States. Am J Kidney Dis. 2020. Epub 2020/09/23. doi: 10.1053/j.ajkd.2020.09.003; PubMed Central PMCID: PMC7501875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peng S, Wang HY, Sun X, Li P, Ye Z, Li Q, et al. Early versus late acute kidney injury among patients with COVID-19-a multicenter study from Wuhan, China. Nephrol Dial Transplant. 2020;35(12):2095–102. Epub 2020/12/05. doi: 10.1093/ndt/gfaa288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Groeneveld AB, Tran DD, van der Meulen J, Nauta JJ, Thijs LG. Acute renal failure in the medical intensive care unit: predisposing, complicating factors and outcome. Nephron. 1991;59(4):602–10. Epub 1991/01/01. doi: 10.1159/000186651 . [DOI] [PubMed] [Google Scholar]
- 39.Khosla N, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini E, et al. Preexisting chronic kidney disease: a potential for improved outcomes from acute kidney injury. Clin J Am Soc Nephrol. 2009;4(12):1914–9. Epub 2009/12/08. doi: 10.2215/CJN.01690309 ; PubMed Central PMCID: PMC2798877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehta RL. Refining Predictive Models in Critically Ill Patients with Acute Renal Failure. Journal of the American Society of Nephrology. 2002;13(5):1350–7. doi: 10.1097/01.asn.0000014692.19351.52 [DOI] [PubMed] [Google Scholar]
- 41.Pannu N, James M, Hemmelgarn BR, Dong J, Tonelli M, Klarenbach S, et al. Modification of outcomes after acute kidney injury by the presence of CKD. Am J Kidney Dis. 2011;58(2):206–13. Epub 2011/04/19. doi: 10.1053/j.ajkd.2011.01.028 . [DOI] [PubMed] [Google Scholar]
- 42.Neyra JA, Mescia F, Li X, Adams-Huet B, Yessayan L, Yee J, et al. Impact of Acute Kidney Injury and CKD on Adverse Outcomes in Critically Ill Septic Patients. Kidney Int Rep. 2018;3(6):1344–53. Epub 2018/11/20. doi: 10.1016/j.ekir.2018.07.016 ; PubMed Central PMCID: PMC6224792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lafrance JP, Miller DR. Defining acute kidney injury in database studies: the effects of varying the baseline kidney function assessment period and considering CKD status. Am J Kidney Dis. 2010;56(4):651–60. Epub 2010/08/03. doi: 10.1053/j.ajkd.2010.05.011 . [DOI] [PubMed] [Google Scholar]
- 44.Gansevoort RT, Hilbrands LB. CKD is a key risk factor for COVID-19 mortality. Nat Rev Nephrol. 2020;16(12):705–6. Epub 2020/08/28. doi: 10.1038/s41581-020-00349-4 ; PubMed Central PMCID: PMC7447963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan L, Chaudhary K, Saha A, Chauhan K, Vaid A, Zhao S, et al. AKI in Hospitalized Patients with COVID-19. J Am Soc Nephrol. 2020. Epub 2020/09/05. doi: 10.1681/ASN.2020050615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ng JH, Hirsch JS, Hazzan A, Wanchoo R, Shah HH, Malieckal DA, et al. Outcomes Among Patients Hospitalized With COVID-19 and Acute Kidney Injury. Am J Kidney Dis. 2020. Epub 2020/09/23. doi: 10.1053/j.ajkd.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nadim MK, Forni LG, Mehta RL, Connor MJ Jr., Liu KD, Ostermann M, et al. COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup. Nat Rev Nephrol. 2020;16(12):747–64. Epub 2020/10/17. doi: 10.1038/s41581-020-00356-5 ; PubMed Central PMCID: PMC7561246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–27. Epub 2020/04/25. doi: 10.1016/j.kint.2020.04.003 ; PubMed Central PMCID: PMC7194105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Farkash EA, Wilson AM, Jentzen JM. Ultrastructural Evidence for Direct Renal Infection with SARS-CoV-2. J Am Soc Nephrol. 2020;31(8):1683–7. Epub 2020/05/07. doi: 10.1681/ASN.2020040432 ; PubMed Central PMCID: PMC7460898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rossi GM, Delsante M, Pilato FP, Gnetti L, Gabrielli L, Rossini G, et al. Kidney Biopsy Findings in a Critically Ill COVID-19 Patient With Dialysis-Dependent Acute Kidney Injury: A Case Against "SARS-CoV-2 Nephropathy". Kidney Int Rep. 2020;5(7):1100–5. Epub 2020/05/20. doi: 10.1016/j.ekir.2020.05.005 ; PubMed Central PMCID: PMC7230145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Santoriello D, Khairallah P, Bomback AS, Xu K, Kudose S, Batal I, et al. Postmortem Kidney Pathology Findings in Patients with COVID-19. J Am Soc Nephrol. 2020;31(9):2158–67. Epub 2020/07/31. doi: 10.1681/ASN.2020050744 ; PubMed Central PMCID: PMC7461662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schaller T, Hirschbuhl K, Burkhardt K, Braun G, Trepel M, Markl B, et al. Postmortem Examination of Patients With COVID-19. JAMA. 2020;323(24):2518–20. Epub 2020/05/22. doi: 10.1001/jama.2020.8907 ; PubMed Central PMCID: PMC7243161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.