Abstract
Introduction
Post-traumatic stress disorder (PTSD) has an adverse impact on the emotional health of prenatal maternal women and their offspring. During the Coronavirus Disease 2019 (COVID-19) pandemic, pregnant women are vulnerable to traumatic events and are prone to PTSD symptoms. The aim of the study was to explore the predictive effects of insomnia and somatization on PTSD in pregnant women by utilizing generalized additive model (GAM).
Materials and Methods
A total of 1638 pregnant women from three local cities in China underwent online survey on sleep quality, somatization, and PTSD symptoms tested by the Insomnia Severity Index (ISI), the subscale somatization of Symptom Checklist-90 (SCL-90-S) and the Checklist for DSM-5 (PCL-5), respectively.
Results
Insomnia was positively correlated with PTSD symptoms in pregnant women (p = 1.79×10−5). Interestingly, insomnia and somatization showed a complex non-primary linear interaction in predicting PTSD (p = 2.00×10−16).
Conclusion
Our results suggest that insomnia is a prominent predictor of PTSD symptoms in pregnant women in the context of public emergencies. In addition, the effects of insomnia and somatization on PTSD symptoms are characterized by complex non-primary linear relationships.
Keywords: emotion, COVID-19, insomnia, somatization, pregnant
Introduction
Currently, the Coronavirus Disease 2019 (COVID-19) pandemic has spread rapidly around the world, resulting in nearly 90.59 million confirmed cases and 1.93 million deaths (January 11, 2021). COVID-19 is regarded as a potential traumatic event, which is closely associated with the increase of PTSD symptoms in the general population.1,2,4 In the context of this epidemic, many pregnant women gave up or lose the opportunity for regular antenatal check-ups because of the potential risk of infection, the need for home isolation and the lack of medical resources, which may increase the risk of developing PTSD.3,4 Prenatal PTSD not only affects the premature delivery and the lower birth weight of the offspring,5 but causes their own mental disorders.6,7 Recently, a cross-sectional survey conducted before and during the COVID-19, which showed that compared to pre-pandemic group, pregnant women of the pandemic group scored higher in the depression, anxiety and stress.8 Another meta-analysis study showed that the overall prevalence of PTSD is 20%.9 Therefore, in the context of COVID-19, it is of great significance to identify the risk factors for the prevention of PTSD in perinatal pregnant women.
Insomnia has been considered as a symptom associated with primary mental health diseases.10 Voitsidis et al11 explored sleep difficulties during the COVID-19 pandemic in the Greek population and found that 37.6% of participants reported sleep problems, especially women. And the insomnia and PTSD detection detectable rate of pregnant women was 19% and 20% respectively.9 Krakow et al12 found that the severity of PTSD is closely associated with the quality of sleep. Insomnia occurs in 66–90% of people with PTSD.13 Patients with more severe insomnia have more severe PTSD symptoms at the beginning of treatment of PTSD. A longitudinal study examined the severity of PTSD among postwar veterans who had experienced a 12-month war in Iraq, which indicated that insomnia in the 4th month was an important predictor of depression and PTSD symptoms in the 12th month.14 Therefore, it is hypothesized that insomnia will predict PTSD symptoms in pregnant women during the 2019-nCoV epidemic.
Further, PTSD patients are more likely to report somatization symptoms than patients with other mental disorders.15 Somatization refers to the development of somatic symptoms without organic damage.16 Elklit and Christiansen16 suggested that even trauma victims without any serious injury may report more somatic symptoms than non-traumatic controls. A survey of 264 women attending the Department of Veterans Affairs primary care clinic showed that after controlling demographic variables, the status of veterans and other mood and anxiety disorders, PTSD was the best predictor of somatization.17 Kounou et al18 examined the relationship between post-traumatic response, PTSD symptoms, somatization, and quality of life in a sample of refugees for two years after the 2011 Ivory Coast socio-political crisis. The study found that somatization was a key feature of traumatic experiences, and targeting somatization combined with trauma-centered therapy improved the prognosis of PTSD patients. In view of the close association between PTSD and somatization, somatization may also be a potential factor that moderates the relationship between PTSD and insomnia in pregnant women.
This study aimed to investigate the predictive effect of insomnia and somatic symptoms on PTSD. We hypothesized 1) with the COVID-19 epidemic progress, the symptoms of PTSD in pregnant women gradually increased; 2) there was an interaction between insomnia and somatization on PTSD symptoms; 3) both insomnia and somatization may predict the severity of PTSD symptoms. Because of the non-normal distribution of the current data, we used the Generalized Additive Model (GAM) to reduce risk related to the linear regression hypothesis. The main purpose of our findings may provide meaningful insights for early identification and intervention of PTSD in pregnant women.
Materials and Methods
Participants
All participants came from three local cities: Wuhan, Beijing and other urban areas. The information was collected through an online survey from February 28, 2020 to April 9, 2020, which was run on a smartphone. Inclusion criteria included 1) perinatal pregnancy women >20 years old; 2) no history of major organic or somatization damage, and no diagnosis of any mental disorders such as schizophrenia, depression or anxiety. All these screening items related to mental health problems must be self-reported by filling in demographic information; 3) no medication within two weeks; 4) no history of drug, smoking or alcohol abuse. All participants signed the informed consent form. This study was approved by the Institutional Review Board of the Institute of Psychology, Chinese Academy of Sciences. It was performed in accordance with the ethical standards stipulated in the 1964 Declaration of Helsinki.
The minimized sample size was estimated by previous literature about 15% PTSD on the COVID-19.19 Finally, 1638 healthy pregnant women were included in this study. The average age was 30.20 years old, the average gestation period was 25.40 weeks, and the average pregnancy times and birth times were 1.64 and 1.18, respectively (Table 1).
Table 1.
Mean Value and Standard Deviation (SD) of Variables
| Area | Wuhan | Beijing | Others | Area Mean | p value |
|---|---|---|---|---|---|
| Sample Size | 522 | 493 | 623 | ||
| Age (years) | 29.54±0.35 | 29.28±0.36 | 31.49±0.32 | 30.20±0.20 | < 0.001 |
| BMI | 25.06±0.16 | 23.77±0.17 | 24.18±0.15 | 24.34±0.10 | < 0.001 |
| Score of SES | 0.10±0.09 | −0.13±0.09 | 0.09±0.08 | 0.002±0.05 | 0.198 |
| Weeks of Pregnancy | 25.48±0.52 | 25.00±0.54 | 25.65±0.48 | 25.40±0.30 | 0.660 |
| Times of Pregnancy | 1.64±0.04 | 1.67±0.04 | 1.57±0.04 | 1.62±0.02 | 0.188 |
| Times of Births | 1.18±0.02 | 1.12±0.02 | 1.16±0.02 | 1.15±0.01 | 0.029 |
| Score of SCL-90 | 16.59±0.28 | 16.94±0.29 | 17.90±0.25 | 17.19±0.16 | 0.001 |
| Score of PCL-5 | 3.75±0.37 | 5.40±0.37 | 6.15±0.33 | 5.16±0.21 | < 0.001 |
| Score of ISI | 3.74±0.20 | 4.12±0.20 | 4.62±0.18 | 4.19±0.11 | 0.003 |
Notes: The p values of SCL-90, PCL-5, and the ISI score were obtained without controlling for other variables.
Symptom Measurements
Participants were asked to evaluate their feelings and symptoms based on the epidemic. When they responded to the questions of the rating scales, they must follow the introduction of measurement methods. We conducted a retrospective study, which data of PTSD symptom, insomnia symptom and somatization symptom were collected from all participants. In addition, socio-economic status was also involved as a covariate to control the potential confounding effect when examining the association between PTSD, insomnia, and somatization.
PTSD Symptom
The PTSD symptoms of each participant were assessed with the Chinese version of the PTSD Checklist for DSM-5 (PCL-5). It consists of 20 items, with scores ranging from “1 = never” to “5 = severe”, including intrusive symptoms (symptom B), avoidance symptoms (symptom C), cognitive and negative emotional changes (symptom D), arousal and reactive changes (symptom E). This scale has good reliability and validity in Chinese local studies (Cronbach’s α = 0.94).20 The higher the score, the more severe the participants’ PTSD symptoms. In order to prevent the overlap between items, a sleep-related item was removed in the statistical analysis (the 20th question in PCL-5: difficulty in falling asleep or very light sleep).
Insomnia Symptom
The Insomnia Severity Index (ISI) is a short self-report tool with seven questions to measure participants’ perceptions of both nocturnal and daytime insomnia symptoms (Cronbach’s α = 0.90 for community sample; Cronbach’s α = 0.91 for insomnia clinical sample).21 Participants were asked to recall their sleep status during “the passed 2 weeks”. The dimensions of the assessment are: severity of sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, sleep disturbances that interfere with daytime functions, noticeability of sleep problems by others, and distress caused by sleep difficulties.21 Using a 5-level score, from “0 = none” to “4 = extremely severe”, the total score ranges from 0 to 28. The higher the score, the more severe the insomnia of the participants.
Somatization Symptom
The subscale somatization of Symptom Checklist-9022 (SCL-90-S) was used to access participants’ somatization symptoms, which includes 12 questions of SCL-90, such as item 1, 4, 12, 27, 40, 42, 49, 52, 53, 56, and 58. The subscale that indicates physical discomfort includes complaints of cardiovascular, gastrointestinal, respiratory, headaches, back pain, muscle soreness, and other somatic anxiety symptoms. The scale was rated as 5 levels (from 1 to 5) from “1 = none” to “5 = severe”.
Socio-Economic Status (SES)
The measurement of SES is calculated by education level, occupation and family property, where occupations are assigned based on Ganzeboom & Treiman model.23 In order to calculate the comprehensive indicators of the participants’ SES, SPSS for Mac 15.1 was used to conduct a factor analysis on education level, professional status, and family property. A principal factor with characteristic vector greater than 1 was obtained, which explains 55.16% of the variance. The factor load matrix used the coefficient of the primary factor 1 (Education level). The formula is as follows:
SES = [0.803×Z(Education)+0.737×Z(Income)+0.681×Z(Occupation)]/0.552
Statistical Analysis
First, the Shapiro–Wilk test of Skewness and Kurtosis was used to test the normal distribution of the collected data in SPSS for Mac 15.1. In view of the non-normal distribution of the current data, we used the “bam” function of the “mgcv” package in R to fit the GAM with controlling for the participants’ age,24 BMI,25 SES,26 weeks of pregnancy27 (WP), times of pregnancy (TP) and times of births (TB) by putting them into the GAM equation in a linear fashion. If any data is missing, all data from that participant were deleted.
In order to examine whether there are any differences between different pregnant periods, we divided all participants into three groups: first-trimester (pregnancy period ≤12 weeks), second-trimester (12<pregnancy period <28 weeks) and third-trimester (pregnancy ≥28 weeks). Then, one-way ANOVA was used to investigate the group difference in outcome measurements.
The principle of GAM is to minimize residuals (goodness of fit) while maximizing minimalism (lowest possible degree of freedom). Compared with traditional linear fitting, GAM can adapt to various changes of Y, such as the commonly used exponential and logarithmic changes. The model is no longer limited to fitting linear relationships, but also can fit nonlinear relationships. The dependent variable Y no longer only obeys Gaussian distribution, but also obeys Poisson, negative binomial distribution, etc.28
Before fitting analysis, data values were normalized and the region variables was treated as classification variable data (code: data$Area<-as.factor(data$Area)). The equation is as follows:
(A): ISI ~ s(Days) + s(SCL-90-S) + Area + SES + Age + BMI + WP + TP + TB
(B): PTSD ~ s(Days) + s(SCL-90-S) + s(ISI) + s(SCL-90-S, ISI) + Area + SES + Age + BMI + WP + TP + TB
(A) was used to examine the relationship between somatization and insomnia; (B) was performed to test the predictive effect of somatization and insomnia on PTSD. In these equations, s(variable) represents the nonlinear relationship between the variable and the PCL-90 score; the variable without s(variable) represents the linear relationship with the PCL-90 score; and s(SCL-90-S, ISI) represents the interaction effect of SCL-90-S and ISI. Except for classified variables, all other linear values are control variables. When the p value is less than 0.016 (Bonferroni Correction for 3 hypotheses), it is considered as statistically significant.
Results
Descriptive Statistics
Table 1 displays the demographic characteristics of the current study. Thirty-six participants reported high levels of PTSD with PCL-5 score of 33 or higher, indicating that the prevalence of PTSD in this sample was 2.2%. As for the somatization, 25 participants reported a high level of somatization with the SCL-90 total score of 36 or higher, indicating that the prevalence of somatization in this sample was 1.53%. In terms of sleep quality, the clinical mild insomnia rate was 13.86%, the moderate insomnia rate was 2.69%, and the severe insomnia rate was 0.48%. There were no main effects of pregnant periods in PCL-5 (F = 0.809, p = 0.445), SCL-90 (F = 0.38, p = 0.687) and ISI (F = 0.81, p = 0.445) score.
Normal Distribution Test
The PCL-5, ISI and SCL-90-S scores were tested by normal distribution test. The scores of the three scales in this batch were all distributed with positive skewness (p < 0.001). In addition, the skewness value (g1) and kurtosis value (g2) of these three were positive, and the frequency histograms were shown in Figure 1.
Figure 1.
Frequency distribution histogram of PCL-5 (A), ISI (B) and SCL-9-S (C) respectively.
GAM Analysis
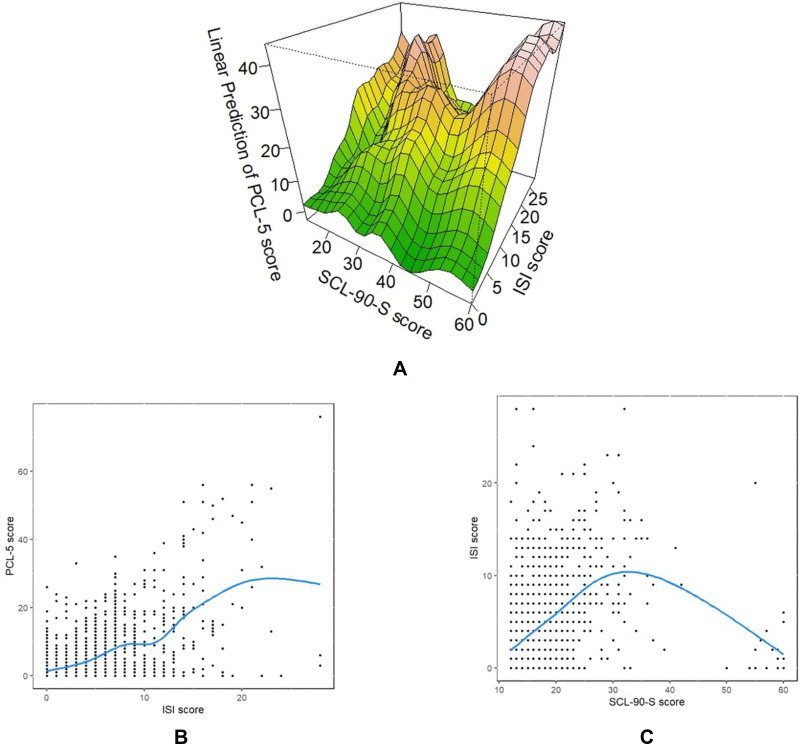
There was an interactive effect between ISI score and SCL-90-S somatization on PTSD (REML = 5373.5, F = 4.71, R2 = 0.46, p < 2.00×10−16, Figure 2A). As shown in Figure 2A, when the score of SCL-90-S was in range of 30–44, the relationship between the score of ISI and PCL-5 showed an inverse U shape, in which the score of PCL-5 was increasing first and then decreasing with the increase of the score of ISI. Yet when the score of SCL-90-S was lower than 30 or higher than 44, the relationship between SCL-90-S score and ISI score was positive. There was marginally significant correlation between somatization score and PCL-5 score (REML = 5373.5, F = 1.75, R2 = 0.45, p = 0.09, Figure S1). Additionally, the ISI score was significantly correlated with the PCL-5 score (Figure 2B, F = 4.93, p = 1.79×10−5). However, there was no significant correlation between PCL-5 score and the duration of the epidemic (F = 1.75, p = 0.15, Figure S2).
Figure 2.
Linear plots of GAM analysis: (A) Interaction between ISI and SCL-90-S on PCL-5; (B) Scatter and linear plot of ISI and PCL-5 score; (C) Scatter and linear plot of SCL-90-S and ISI score. The interaction can be observed by an inverted U-shaped relationship between insomnia and somatization symptoms. When the somatization level is in the middle, the state of insomnia is the worst. Since insomnia score is greatly influenced by somatization, this association will lead to changes in the progression (slope) of PTSD and show a moderating effect.
As shown in Figure 2C, the GAM model fitting showed an inverted U-shaped curve between insomnia severity (ISI score) and somatization (SCL-90-S score, REML = 4600.3, R2 = 0.21, F = 74.87 p < 2.00×10−16). When the SCL-90-S score was between 0 and 33 (approximation), insomnia increased with the increase in degree of somatization, while when the SCL-90-S score was above 33, the insomnia score decreased with the increase in somatization. As depicted above, the model tests found that the R2 for linear prediction of SCL-90-S score on ISI (1) and the SCL-90-S predictive effect on PTSD symptoms (2) were 0.21 and 0.45, respectively.
Discussion
In this study, we examined the predictive effect of insomnia and somatization on PTSD symptoms in prenatal women during COVID-19. GAM model indicated that insomnia could significantly predict PTSD symptoms. The interaction of insomnia and somatization on PTSD was also detected. In addition, the relationship between insomnia and somatization showed an inverted U-shaped curve.
Consistent with previous studies, the severity of insomnia was significantly associated with the symptoms of PTSD. However, most of studies were focused on non-pregnant populations. For instance, several studies showed that patients with PTSD symptoms woke up more frequently during sleep,29–32 and lack of sleep is one of the risk factors for PTSD symptoms.33 Psarros et al conducted a PTSD study of fire survivors and found that except for nocturnal and awakening time, almost all sleep discomfort symptoms in PTSD patients were statistically more frequent than those in the control group.34 In the current study, insomnia was significantly associated with PTSD in pregnant women, and the predictive effect of insomnia on PTSD in prenatal women may be due to the severity of the epidemic. It is worth noting that women with PTSD are more likely to have insomnia than men with PTSD,29,35–37 suggesting that women are more likely to experience stress after a traumatic event. For instance, in PTSD patients, disruptions in sleep maintenance were found only in women but not men, suggesting that impaired sleep quality may increase the risk of developing PTSD in women.38 Pregnant women as one of the special period of lifespan are sensitive to mental disorders during COVID-19 pandemic.8 Sanchez et al found that pregnant women with sleep disturbances were more likely to experience PTSD.39 Though there were few studies focus on the relationship between pregnant insomnia and PTSD symptoms directly, previous studies found that insomnia in pregnancy period is associated with mental health disorders which are closely related to PTSD symptoms, eg anxiety,40 depression.41 In the context of the COVID-19 pandemic, with the popularity of the internet and smartphones, pregnant women had access to negative information about the development of the epidemic from the news media, which undoubtedly aggravated their worries, anxiety about their own health and their fetus. As a result, negative emotions may further worsen PTSD symptoms.14
Although the individuals with PTSD were more likely reported symptom of somatization,15,18 the association between somatization and PTSD symptoms was not significant. This result is consistent with several studies.42,43 Different instruments might contribute to insignificant association of these two variables in this study. In most of relevant investigations, Brief Symptom Inventory44 and MMPI-2 hypochondriasis scale45 are more commonly used to measure somatization in previous studies while we used the subscale of SCL-90-S. The other reason might be the different severity of PTSD involved in the studies. We found that the participants in this study had only mild symptoms of PTSD, which might lead to the insignificant relationship between PTSD and somatization.
We also detected the interaction between insomnia and somatization. It is suggested that the predictive effect of insomnia on PTSD may be influenced by somatization. Our result showed that when the score of SCL-90-S was in range of 30–44, the relationship between insomnia symptom and PTSD symptom showed an inverse U shape, in which the score of PCL-5 was increasing first and then decreasing with the increase of the score of ISI. However, when the score of SCL-90-S was lower than 30 or higher than 44, the relationship between SCL-90-S score and ISI score was positive. To our best knowledge, no study has reached a similar conclusion. We speculate that this interaction is due to inconsistent relationships of insomnia or somatization with PTSD: insomnia positively predicated PTSD symptoms, but somatization failed to detect a similar relationship in this study. Moreover, somatization scores vary widely, ranging from 30 to 60 (Figure S1 which may contribute to the current interaction effect. This U-shaped relationship between insomnia and somatization is not in line with previous studies.46 The possible cause of the U-shaped trend may be the potential strong response bias to the subjective measurement of somatization. In addition, some confounding factors such as social support, pregnant women’s personality characteristics and other lifestyles may also contribute to this U-shape relationship between insomnia and somatization. In view of the complex bio-behavioral mechanism of somatization, it is necessary to develop a systematic and objective somatization measurement method in mental health and clinical field.
There are still some limitations in this study. First, the sample size of this prevalence study is relatively small. Thus, caution should be taken when drawing any conclusions about the predictors of PTSD symptoms. Second, this study is a cross-sectional study, which prevents the explanation of causality. Therefore, even if the relationship between insomnia and PTSD symptoms is significant, we cannot conclude that identification of insomnia will cause the recognition of PTSD. In the future investigation, a longitudinal study using the same sample may look into the development of PTSD symptoms over a long period of time, which will help to better understand the predictors of PTSD symptoms in pregnant women. In addition, further longitudinal studies on the association between PTSD and somatization as well as the insomnia in prenatal women is warranted in the future. Third, the use of self-reporting measures to collect data may lead to response bias. We could not guarantee that all the participants followed the instruction strictly. It is likely that the participants might respond to the items according to their real feelings, which might confuse with previous traumatic events. However, great efforts have been made to ensure the confidentiality of the report. Finally, when the data was collected, the COVID-19 epidemic situation in China has been controlled to a certain extent, so the impact of the epidemic on the COVID-19 stress response during this period was not more severe than that in the early stage of the epidemic. However, this result undoubtedly reflects the complex relationship between insomnia, somatization and PTSD symptoms during the COVID-19 pandemic.
Conclusion
This study demonstrates the effect of insomnia and somatization on PTSD symptoms in pregnant women during the COVID-19 pandemic. Insomnia has a positive predictive effect on the severity of PTSD symptoms while insomnia and somatization have a significant complex non-primary linear interaction on PTSD symptoms. This finding provides meaningful insights for psychological and physical assistance to identify and diagnose PTSD symptoms in prenatal women in a timely manner. It is worth noting that special attention should be paid to the sleep quality of pregnant women in emergency situations. In addition, the interaction between insomnia and somatization symptoms on PTSD symptoms suggests that somatization may play an important role in the development of PTSD, which is more complex than the relationship between insomnia and PTSD. These findings strengthen valuable recommendations for public health services and primary care for pregnant women.
Acknowledgments
At the point of finishing this paper, we’d like to express our gratitude to all the experimental operators who has collected a large amount of data in various regions. Additionally, we’d like to thank those leaders, teachers, working staff, and all the pregnant subjects who has made his/her contribution to this study. Without their help, it would be much harder for us to finish this study.
Funding Statement
This work was supported by the National Natural Science Foundation of China (Grant number 31671163) and the CAS Key Laboratory of Mental Health, Institute of Psychology (grant number KLMH2011ZK07), as well as the Open Research Fund of the CAS Key Laboratory of Behavioral Science, Institute of Psychology.
Abbreviations
COVID-19, Coronavirus Disease 2019; PTSD, post-traumatic stress disorder; PCL-5, PTSD Checklist for DSM-5; ISI, Insomnia Severity Index; SCL-90-S, subscale somatization of Symptom Checklist-90; SES, Socio-economic status; GAM, generalized additive model; BMI, body mass index; WP, weeks of pregnancy; TP, times of pregnancy; TB, times of births.
Data Sharing Statement
The data used in this study is tracking data, the database has not been fully established currently, and we would consider to sharing the data after it is established well. If you have any questions about the data, please contact corresponding authors: Gao-Xia Wei (weigx@psych.ac.cn) or Xiangyang Zhang (zhangxy@psych.ac.cn).
Ethical Standards
This study was approved by the institutional review board of the Institute of Psychology, Chinese Academy of Sciences (Approval date: 20200221). It was performed following the ethical standards laid down in the 1964 Declaration of Helsinki. The written informed consent forms were obtained from all participants.
Key Message
Special attention should be paid to the sleep quality of pregnant women in emergency situations. Somatization may play an important role in the development of PTSD, which is more complex than the relationship between insomnia and PTSD.
Disclosure
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y, Ma S, Yang C, et al. Acute psychological effects of Coronavirus Disease 2019 outbreak among healthcare workers in China: a Cross-Sectional Study. Transl Psychiatry. 2020;10(1):348. doi: 10.1038/s41398-020-01031-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seng JS, Low LMK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol. 2009;114(4):839. doi: 10.1097/AOG.0b013e3181b8f8a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seng JS, Rauch SA, Resnick H, et al. Exploring posttraumatic stress disorder symptom profile among pregnant women. J Psychosomatic Obstet Gynecol. 2010;31(3):176–187. doi: 10.3109/0167482X.2010.486453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post‐traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG. 2011;118(11):1329–1339. doi: 10.1111/j.1471-0528.2011.03071.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morland L, Goebert D, Onoye J, et al. Posttraumatic stress disorder and pregnancy health: preliminary update and implications. Psychosomatics. 2007;48(4):304–308. doi: 10.1176/appi.psy.48.4.304 [DOI] [PubMed] [Google Scholar]
- 7.Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol. 2001;97(1):17–22. [DOI] [PubMed] [Google Scholar]
- 8.Puertas-Gonzalez JA, Mariño-Narvaez C, Peralta-Ramirez MI, Romero-Gonzalez B. The psychological impact of the COVID-19 pandemic on pregnant women. Psychiatry Res. 2021;301:113978. doi: 10.1016/j.psychres.2021.113978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X, Chen J, Zhang M, et al. One year of evidence on mental health in the COVID-19 crisis - a systematic review and meta-analysis. medRxiv. 2021. 2021.2002.2001.21250929. doi: 10.1101/2021.02.01.21250929 [DOI] [Google Scholar]
- 10.Matteson-Rusby SE, Pigeon WR, Gehrman P, Perlis ML. Why treat insomnia? Prim Care Companion J Clin Psychiatry. 2010;12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. doi: 10.1016/j.psychres.2020.113076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krakow B, Melendrez D, Pedersen B, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;49(11):948–953. doi: 10.1016/S0006-3223(00)01087-8 [DOI] [PubMed] [Google Scholar]
- 13.Colvonen PJ, Ellison J, Haller M, Norman SB. Examining Insomnia and PTSD over time in veterans in residential treatment for substance use disorders and PTSD. Behav Sleep Med. 2019;17(4):524–535. doi: 10.1080/15402002.2018.1425869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67(12):1240–1258. doi: 10.1002/jclp.20845 [DOI] [PubMed] [Google Scholar]
- 15.Andreski P, Chilcoat H, Breslau N. Post-traumatic stress disorder and somatization symptoms: a prospective study. Psychiatry Res. 1998;79(2):131–138. doi: 10.1016/S0165-1781(98)00026-2 [DOI] [PubMed] [Google Scholar]
- 16.Elklit A, Christiansen DM. Predictive factors for somatization in a trauma sample. Clin Practice Epidemiol Mental Health. 2009;5(1):1. doi: 10.1186/1745-0179-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Escalona R, Achilles G, Waitzkin H, Yager J. PTSD and somatization in women treated at a VA primary care clinic. Psychosomatics. 2004;45(4):291–296. doi: 10.1176/appi.psy.45.4.291 [DOI] [PubMed] [Google Scholar]
- 18.Kounou KB, Brodard F, Gnassingbe A, et al. Posttraumatic stress, somatization, and quality of life among Ivorian refugees. J Trauma Stress. 2017;30(6):682–689. [DOI] [PubMed] [Google Scholar]
- 19.Karatzias T, Shevlin M, Murphy J, et al. Posttraumatic stress symptoms and associated comorbidity during the COVID‐19 pandemic in Ireland: a population‐based study. J Trauma Stress. 2020;33(4):365–370. doi: 10.1002/jts.22565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu P, Wang L, Cao C, et al. The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. J Anxiety Disord. 2014;28(4):345–351. doi: 10.1016/j.janxdis.2014.03.008 [DOI] [PubMed] [Google Scholar]
- 21.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Derogatis LR, Unger R. Symptom checklist‐90‐revised. Corsini Encyclopedia Psychol. 2010; 1–2. doi: 10.1002/9780470479216.corpsy0970 [DOI] [Google Scholar]
- 23.Ganzeboom HB, Treiman DJ. Internationally comparable measures of occupational status for the 1988 international standard classification of occupations. Soc Sci Res. 1996;25(3):201–239. doi: 10.1006/ssre.1996.0010 [DOI] [Google Scholar]
- 24.Tabet M, Flick LH, Cook CA, Xian H, Chang JJ. Age at first birth and psychiatric disorders in low-income pregnant women. J Women’s Health. 2016;25(8):810–817. doi: 10.1089/jwh.2015.5236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maguen S, Madden E, Cohen B, et al. The relationship between body mass index and mental health among Iraq and Afghanistan veterans. J Gen Intern Med. 2013;28(2):563–570. doi: 10.1007/s11606-013-2374-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muzik M, McGinnis EW, Bocknek E, et al. PTSD symptoms across pregnancy and early postpartum among women with lifetime PTSD diagnosis. Depress Anxiety. 2016;33(7):584–591. doi: 10.1002/da.22465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch Women’s Mental Health. 2013;16(6): 453–463. doi: 10.1007/s00737-013-0365-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu S, Chen P, Lin H, Xie C, Chen X. Promoting carsharing attractiveness and efficiency: an exploratory analysis. Transport Res Part D Transport Environ. 2018;65:229–243. doi: 10.1016/j.trd.2018.08.015 [DOI] [Google Scholar]
- 29.van Liempt S. Sleep disturbances and PTSD: a perpetual circle? Eur J Psychotraumatol. 2012;3(1):19142. doi: 10.3402/ejpt.v3i0.19142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Breslau N, Roth T, Burduvali E, Kapke A, Schultz L, Roehrs T. Sleep in lifetime posttraumatic stress disorder: a community-based polysomnographic study. Arch Gen Psychiatry. 2004;61(5):508–516. doi: 10.1001/archpsyc.61.5.508 [DOI] [PubMed] [Google Scholar]
- 31.Calhoun PS, Wiley M, Dennis MF, Means MK, Edinger JD, Beckham JC. Objective evidence of sleep disturbance in women with posttraumatic stress disorder. J Traumatic Stress. 2007;20(6):1009–1018. doi: 10.1002/jts.20255 [DOI] [PubMed] [Google Scholar]
- 32.Habukawa M, Uchimura N, Maeda M, Kotorii N, Maeda H. Sleep findings in young adult patients with posttraumatic stress disorder. Biol Psychiatry. 2007;62(10):1179–1182. doi: 10.1016/j.biopsych.2007.01.007 [DOI] [PubMed] [Google Scholar]
- 33.Cox RC, McIntyre WA, Olatunji BO. Interactive effects of insomnia symptoms and trauma exposure on PTSD: examination of symptom specificity. Psychol Trauma Theory, Res, Practice, Policy. 2018;10(5):508. doi: 10.1037/tra0000336 [DOI] [PubMed] [Google Scholar]
- 34.Psarros C, Theleritis C, Economou M, et al. Insomnia and PTSD one month after wildfires: evidence for an independent role of the “fear of imminent death”. Int J Psychiatry Clin Pract. 2017;21(2):137–141. doi: 10.1080/13651501.2016.1276192 [DOI] [PubMed] [Google Scholar]
- 35.Paparrigopoulos T, Tzavara C, Theleritis C, Psarros C, Soldatos C, Tountas Y. Insomnia and its correlates in a representative sample of the Greek population. BMC Public Health. 2010;10(1):531. doi: 10.1186/1471-2458-10-531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170(4):372–382. doi: 10.1176/appi.ajp.2012.12040432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huntley ED, Hall Brown TS, Kobayashi I, Mellman TA. Validation of the Fear of Sleep Inventory (FOSI) in an urban young adult African American sample. J Trauma Stress. 2014;27(1):103–107. doi: 10.1002/jts.21882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kobayashi I, Huntley E, Lavela J, Mellman TA. Subjectively and objectively measured sleep with and without posttraumatic stress disorder and trauma exposure. Sleep. 2012;35(7):957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez SE, Friedman LE, Rondon MB, Drake CL, Williams MA, Gelaye B. Association of stress-related sleep disturbance with psychiatric symptoms among pregnant women. Sleep Med. 2020;70:27–32. doi: 10.1016/j.sleep.2020.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gentile S. Anxiety and sleep disorders, psychopharmacology, and pregnancy. Psychopharmacol Pregnancy. 2014:87–102. doi: 10.1007/978-3-642-54562-7_7 [DOI] [Google Scholar]
- 41.Osnes RS, Eberhard-Gran M, Follestad T, Kallestad H, Morken G, Roaldset JO. Mid-pregnancy insomnia and its association with perinatal depressive symptoms: a Prospective Cohort Study. Behav Sleep Med. 2021;19(3):285–302. doi: 10.1080/15402002.2020.1743705 [DOI] [PubMed] [Google Scholar]
- 42.North CS, Kawasaki A, Spitznagel EL, Hong BA. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J Nerv Ment Dis. 2004;192(12):823–829. doi: 10.1097/01.nmd.0000146911.52616.22 [DOI] [PubMed] [Google Scholar]
- 43.Samelius C. Abused women: health, somatization, and posttraumatic stress, Institutionen för molekylär och klinisk medicin. 2007. Available from: https://www.diva-portal.org/smash/record.jsf?pid=diva2%3A23661&dswid=8685. [Google Scholar]
- 44.Derogatis LR. Brief Symptom Inventory (BSI) Administration, Scoring, and Procedures Manual. 1982;9:44–56. [Google Scholar]
- 45.Duckworth JC, Anderson WP. MMPI and MMPI-2: Interpretation Manual for Counselors and Clinicians. Taylor & Francis. 2019. [Google Scholar]
- 46.Ghadiri Sourman Abadi F, Abdolmohammadi K, Babapour KJ, Asl RV. Prediction of somatization on the basis of self-esteem, insomnia and paranoid thoughts in university students. Qom Univ Med Sci J. 2016;10(10):61–68. [Google Scholar]