Abstract
In an effort to control the COVID-19 pandemic, large-scale vaccination is being implemented in various countries using anti-SARS-CoV-2 vaccines based on mRNAs, adenovirus vectors, and inactivated viruses. However, there are concerns regarding adverse effects, such as the induction of fever attributed to mRNA vaccines and pre-existing immunity against adenovirus vectored vaccines or their possible involvement in the development of thrombosis. The induction of antibodies against the adenovirus vector itself constitutes another hindrance, rendering boosting vaccinations ineffective. Additionally, it has been questioned whether inactivated vaccines that predominantly induce humoral immunity are effective against newly arising variants, as some isolated strains were found to be resistant to the serum from COVID-19-recovered patients.
Although the number of vaccinated people is steadily increasing on a global scale, it is still necessary to develop vaccines to address the difficulties and concerns mentioned above. Among the various vaccine modalities, live attenuated vaccines have been considered the most effective, since they closely replicate a natural infection without the burden of the disease. In our attempt to provide an additional option to the repertoire of COVID-19 vaccines, we succeeded in isolating temperature-sensitive strains with unique phenotypes that could serve as seeds for a live attenuated vaccine.
In this review article, we summarize the characteristics of the currently approved SARS-CoV-2 vaccines and discuss their advantages and disadvantages. In particular, we focus on the novel temperature-sensitive variants of SARS-CoV-2 that we have recently isolated, and their potential application as live-attenuated vaccines. Based on a thorough evaluation of the different vaccine modalities, we argue that it is important to optimize usage not only based on efficacy, but also on the phases of the pandemic. Our findings can be used to inform vaccination practices and improve global recovery from the COVID-19 pandemic.
Keywords: COVID-19, SARS-CoV-2, Live attenuated vaccine, Vaccine
1. Introduction
In 2019, an infectious disease named coronavirus disease 2019 (COVID-19) emerged in Wuhan, China. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel coronavirus related to SARS-CoV, was identified as the pathogen responsible for this disease [1]. As of March 2021, more than one hundred million cases and more than two million deaths due to COVID-19 have been reported worldwide [2]. Even those who recover from COVID-19 report long-term sequelae, such as fatigue, loss of taste, and olfactory disorders [3].
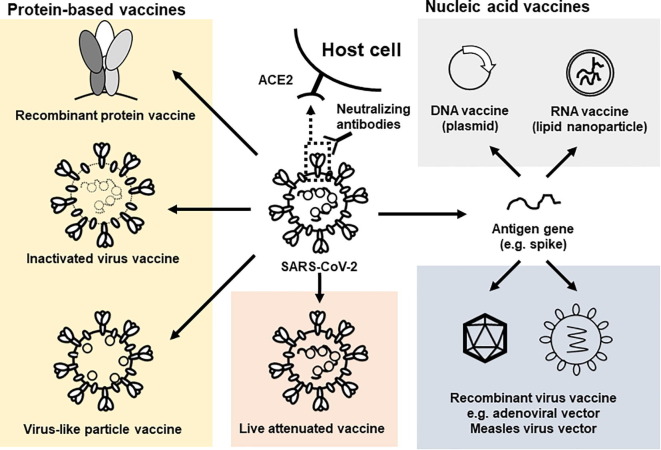
SARS-CoV-2 is an enveloped, positive-sense, single-stranded RNA virus of the Betacoronavirus genus, with a genome length of approximately 30 kb. The genome encodes a large polyprotein (ORF1ab), four structural proteins, and several other open reading frames. ORF1ab is cleaved into 16 nonstructural proteins [4]. The structural spike (S) glycoprotein consists of a head subunit S1 and a stalk subunit S2, and forms trimeric structures on the surface of SARS-CoV-2 virions. The receptor-binding domain (RBD) is located in the S1 subunit and facilitates viral attachment to the human angiotensin-converting enzyme 2 (hACE2), the known SARS-COV-2 receptor in humans [5]. Following attachment, the S protein is cleaved by host cell proteases, such as transmembrane serine protease 2 (TMPRSS2) and cathepsin, thereby inducing the fusion of the viral and cell membranes [6], [7], [8]. Because the RBD is critical for cell attachment and entry, it is considered an ideal target for vaccines that trigger the production of neutralizing antibodies [9]. Various types of SARS-CoV-2 vaccines have already been developed and evaluated worldwide (Fig. 1 ). Some of these vaccines, including adenovirus vectored vaccines, mRNA vaccines, and inactivated vaccines, have been approved for clinical use. However, new SARS-CoV-2 variants have recently been detected in the United Kingdom (B.1.1.7), South Africa (B.1.351), Brazil (P.1), the United States (B1.1.429), and India (B.1.617) among other countries [10], [11], [12]. These variants have several amino acid changes in the S protein, some of which are in the RBD.
Fig. 1.
SARS-CoV-2 vaccine candidates under development. SARS-CoV-2 infects host cells through the binding of the spike protein with hACE2 that serves as receptor. Therefore, the spike protein is considered a target antigen for vaccine development. Recombinant spike protein, inactivated virus and virus-like particle vaccines are used as protein-based vaccines. Inactivated vaccines are treated with chemical reagents such as formalin and β-propiolactone. These treatments lead to the fixing of proteins or to genome damage (indicated by the dotted line), respectively. Virus-like particles are composed of structural proteins only, and do not contain the viral genome. They are structurally similar to the wild type particles, but the nucleocapsid proteins which bind to the viral genome, are not positioned correctly. Different approaches to deliver the spike-encoding gene into the cells include DNA plasmids, encapsulated RNAs or virus vectors. Moreover, live attenuated viruses can be developed by generating cold-adapted or temperature-sensitive strains, or by codon de-optimization.
B.1.1.7, B.1.351 and P.1 variants have been spreading since the end of 2020. All these variants exhibit an N501Y substitution in the RBD. Deep mutational scanning of this domain has shown that this substitution increases the affinity of the RBD for hACE2, thus increasing the infectivity of the virus [13]. Additionally, there are amino acid substitutions at K417 and E484, such as those detected in the B.1.351 and P.1 variants, which have been reported to change virus antigenicity and to decrease susceptibility to neutralization by sera from recovered COVID-19 patients [14], [15]. Furthermore, the B1.617 variant that was detected in India has been spreading quickly, replacing the B.1.1.7 variant of England as the most abundant strain. [16], [17]. This variant exhibits L452R and E484Q substitutions, in addition to K417N and E484K, which also change the antigenicity and decrease the neutralization susceptibility to sera of infected or vaccinated individuals [18]. Thus, there is a concern as to whether the currently approved vaccines are effective against these SARS-CoV-2 variants.
2. Approved vaccines
2.1. mRNA vaccines
mRNA vaccines have been approved in many countries for emergency use in response to the COVID-19 pandemic, and their efficacy has been confirmed in humans. Therefore, such nucleic acid vaccines are becoming recognized as the mainstay of next-generation vaccines. mRNA vaccines are known to induce a highly effective humoral and cellular immune response because transfected mRNAs express antigen proteins in vivo, and antigen-presenting cells capture the synthesized antigens and present them to CD4+ helper T cells via MHC class II or to CD8+ cytotoxic T cells via MHC class I. Delivery of mRNAs to the cytoplasm of cells for protein expression has been difficult due to their instability. However, introducing several chemical modifications in the nucleotides used for their synthesis has been shown to improve stability and decrease the innate immune response, leading to higher levels of antigen expression [19]. Additionally, encapsulation of RNA within lipid nano particles (LNPs) improves the transfection efficacy and protects RNA from degradation during delivery [20].
Moderna Inc., a pioneering mRNA biotechnology company, started the first clinical trial for a SARS-CoV-2 vaccine in March 2020, and the vaccine’s efficacy was reported to be 94.1% based on a phase III trial [21]. BNT162b2, another mRNA vaccine developed by BioNTech SE, in collaboration with Pfizer Inc., showed 95% efficacy in a phase III clinical trial [22]. These two mRNA vaccines have been approved and are being administered in many countries (Table 1 ).
Table 1.
Approved vaccines.
| Developers | Efficacy | Modality | Countries where approved | References |
|---|---|---|---|---|
| Pfizer Inc. BioNTech SE |
95% | mRNA | USA, E.U., Canada Japan and other countries |
[78], [79] |
| Moderna, Inc | 94.1% | mRNA | USA, E.U., Canada Japan and other countries |
[80], [81] |
| AstraZeneca plc | 70% | Adenovirus vector | India, E.U., U.K., Japan and other countries | [82] |
| Johnson & Johnson | 66.3% | Adenovirus vector | USA., E.U and other countries |
[83] |
| The Gamaleya Center | 92%* | Adenovirus vector | Russia, Argentina and other countries |
[84] |
| CanSino Biologics Inc’s | 65.7%* | Adenovirus vector | China, Mexico and other countries |
[85] |
| Sinopharm Group Co., Ltd. | 79%* | Inactivated virus | China and other countries |
[86] |
| Sinovac Biotech Ltd. | 50% | Inactivated virus | China and other countries |
[87] |
*These efficacies were reported on the REUTERS website.
So far, more than three hundred million mRNA vaccine-doses have been inoculated in the Unites States of America only, and their safety has been confirmed [23]. In addition to their efficacy as vaccines, they also possess an advantage in terms of their developmental process. Even if changes in the sequence information of the antigen encoded by the mRNA vaccines are required, non-clinical studies and clinical trials can be executed quickly, because they have been established as a solid vaccine platform. Therefore, mRNA vaccines can be implemented as a first line of defense against emerging infectious diseases in the future.
Although the mRNA vaccines have been demonstrated to be highly efficacious in clinical trials and large-scale inoculations, there are still some concerns, mainly over adverse effects. It has been reported that 58.89% of mRNA-vaccinated healthcare workers experienced fatigue, and 21.99% had fever. These adverse effects may lead to an increase in vaccine hesitancy [24]. Another serious concern related to mRNA vaccines is their specific storage requirements. BioNTech SE and Moderna Inc. guarantee their vaccines’ effectiveness when stored at −80˚C or −30˚C, respectively. Therefore, dedicated freezers are necessary prior to the implementation of a large-scale mRNA vaccination program, in addition to adequate means of transport under the same conditions. Although this does not constitute a major concern in large, wealthy cities, fulfilling these requirements is difficult in rural and less populated areas, and in developing countries. Therefore, it may be difficult to control SARS-CoV-2 infection on a global scale by mRNA vaccination only.
2.2. Adenoviral vectored vaccines
Recombinant viruses are constructed by inserting the coding sequence of an antigen into a viral genome, or by replacing a part of it. Upon infection, the antigen’s coding sequence can be delivered to the cytoplasm or the nucleus of the infected host cell, leading to expression. Adenoviruses are non-enveloped double-stranded DNA viruses, some types of which infect humans and may cause various symptoms such as common cold, pneumonia, encephalitis, or gastroenteritis. Adenoviruses are commonly considered backbone vectors for gene therapy. The deletion of essential genes for replication, such as E2A and DNA polymerase, creates replication-incompetent strains [25], [26], [27] that have already been used in clinical trials. For example, recombinant adenovirus-p53 has been approved and used against human cancers in China [28].
A number of replication-incompetent adenovirus-based SARS-CoV-2 vaccines have been developed and are under evaluation worldwide [29], [30], [31]. Adenovirus vectored vaccines from AstraZeneca Plc, Johnson & Johnson and Gamaleya, and CanSino Biologics were approved and used in clinical settings. These vaccines were reported to induce robust humoral and cellular immune responses, similar to those reported for mRNA vaccines [32]. Therefore, this type of vaccine may be effective against new SARS-CoV-2 variants such as those isolated in India, Brazil, South Africa, and UK. Another advantage this vaccine modality has over mRNA vaccines is its stability, which makes it easier to handle and store.
On the other hand, there are serious concerns about the adverse effects related to adenovirus vectored vaccines. For example, thrombosis was reported after ChAdOx1 nCov-19 vaccination in a range from 1 case per 26,000 to 1 case per 127,000 doses [33]. The mechanism of this effect remains unknown, but some hypotheses were proposed that the vaccination induced platelet-activating antibodies against platelet factor 4, causing symptoms resembling autoimmune heparin-induced thrombocytopenia. Additionally, it was suggested that the transcription of S protein variants enabled alternative splicing events, giving rise to C-terminal truncated soluble forms with the capacity to bind to ACE2-expressing endothelial cells in blood vessels, triggering the development of severe side effects [34], [35]. The European Medicines Agency has already registered thrombosis as a serious disorder, and Denmark has stopped vaccinating with adenovirus vectored vaccines. Additionally, there is another concern that the efficacy might be impaired by pre-existing immunity against other adenoviruses [36]. To avoid this problem, various adenoviruses, such as chimpanzee adenoviruses, have been used for vaccine development. However, people immunized with these vaccines may generate antibodies targeting the vector, thus reducing the efficacy of additional or boosting inoculations.
2.3. Inactivated vaccines
Viruses can be inactivated using chemical reagents, such as formalin and beta-propiolactone, without significantly affecting their antigenicity. Thus, whole virus particles or parts of the virus can be used for vaccines. Aluminum hydroxide adjuvants are commonly added to enhance the immune response induced by this type of vaccine, such as those for influenza virus, Japanese encephalitis, and poliovirus, which are controlled by neutralizing antibodies. Inactivated vaccines for these viruses have been used for a long time in several countries, and are considered to be highly safe [37].
An inactivated SARS-CoV-2 vaccine was first reported in July 2020 [38]. Gao et al. inactivated the virus with beta-propiolactone, and the vaccine candidate was evaluated in mouse, rat, and non-human primate models. This vaccine induced anti-S and anti-RBD antibodies, and the serum from immunized animals showed neutralizing activity. To date, four SARS-CoV-2 inactivated vaccines (Sinopharm, Sinovac, Sinopharm-Wuhan, and Bharat Biotech) have been approved and are being used in China, U.A.E, and India. These inactivated vaccines are treated with β-propiolactone, which damages the genome but not the proteins, so the particles of these vaccines are like the authentic viruses. This similarity may be effective for the induction of highly reactive antibodies, but the lower stability of the unfixed proteins might be a disadvantage over the formalin-treated inactivated vaccines.
In the development of SARS-CoV-2 vaccines, the S protein, especially the RBD, has been used for recombinant protein-based vaccine production. Taking into account the mechanism for SARS-CoV-2 entry into the host, various recombinant protein vaccine candidates have been generated by substituting amino acids or modifying cleavage sites to stabilize the trimeric structure of the S protein [39], [40].
Variants containing E484K or L452R substitutions in the RBD have been reported to be resistant to neutralization by sera from recovered COVID-19 patients [41], [42]. The immune response induced by inactivated vaccines may not be fully effective against the new variants with mutations in the RBD due to their altered antigenicity. Optimization of inactivated SARS-CoV-2 vaccines is therefore required to increase the efficacy against the variants. For example, it may be necessary to update the vaccine seed viruses against several variants every year, or to make a multivalent vaccine. Alternatively, it may be more effective to induce cellular immunity because CD4+ and CD8+T cell responses are known to be critical for recovery from SARS-CoV-2 infection [43], [44]. It was reported that a recombinant protein-based varicella zoster vaccine with AS01B adjuvant, induced cellular immunity [45]. So, by selecting appropriate adjuvants, it may also be possible to develop an inactivated vaccine against SARS-CoV-2 with broad efficacy against mutant strains.
3. Live attenuated vaccines
Known live attenuated vaccines include those against the measles virus, rubella virus, varicella zoster virus, and influenza virus. The strains used for these vaccines were attenuated mainly through adaptation to cold culture conditions, or through non-human animals [46], [47], resulting in viruses with slower proliferation rates in the human body, compared to the wild type virus strains. Regardless of their slow replication, they can induce a strong immune response. For example, the vOka strain of the varicella zoster virus is an example of a live attenuated vaccine obtained from passages in guinea pig embryonic fibroblasts [48]. Furthermore, the influenza virus strains Ann Arbor 60 and 66, were isolated by the passaging of the wild type virus at 25 °C. These strains are used as master donor viruses for live attenuated intranasal influenza vaccines. They can replicate more slowly than the wild type strain at 37 °C and cannot proliferate at 39 °C [49], [50], [51], [52].
To generate a candidate for a SARS-CoV-2 live attenuated vaccine, we isolated temperature-sensitive (TS) mutants from a Japanese clinical isolate, which could replicate at low temperatures (32 °C or 34 °C) but showed impaired proliferation at 37 °C [53]. This phenotype is similar to that of a live attenuated influenza vaccine strain used in clinical settings. Importantly, these TS mutants showed lower pathogenicity than the wild type parent strain in Syrian hamsters. We detected a similar amount of virus in nasal wash specimens from TS- or wild type-infected hamsters, but the virus titer was significantly lower in the lungs of TS-infected hamsters than in those of wild type-infected hamsters. Additionally, TS-infected hamsters generated sufficient neutralizing antibodies to protect them from re-infection with the wild-type virus. Whole genome sequencing of these mutants and analysis of revertant strains suggested that mutations in the nsp3 and nsp14 genes were responsible for the TS phenotype. The mutations in nsp14 were unique ones that, to our knowledge, have not been reported to be associated with a TS phenotype. In contrast, mutations in the nsp3 gene were reported to be responsible for the TS phenotype in mouse hepatitis virus, a coronavirus that infects mice [54]. Seo et al. obtained a cold-adapted SARS-CoV-2 mutant by passaging at cold temperatures [55]. This cold-adapted mutant did not show a well-defined temperature sensitivity, but induced protective immunity in hACE2 transgenic mice and showed lower pathogenicity compared to the wild type virus. Recently, codon de-optimization has been used as a tool to attenuate viruses [56], [57]. One such strain of SARS-CoV-2 is being evaluated in a phase I clinical trial [58].
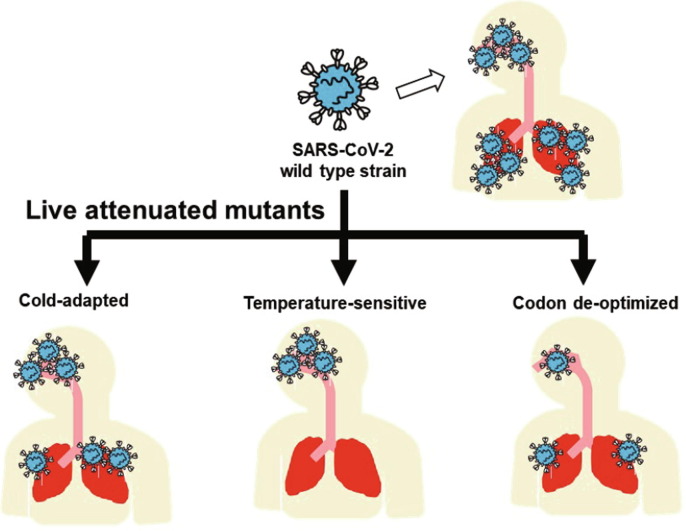
Live attenuated SARS-CoV-2 vaccine candidates have different characteristics (Fig. 2 ). SARS-CoV-2 wild-type strains spread through droplets and replicate in the upper and lower respiratory tracts and in the lungs. In contrast, cold-adapted and TS mutants cannot do so [53]. Codon de-optimized virus strains proliferate more slowly than the wild-type strain in the human body and in vitro [57]. CODAGENIX Inc. has been constructing and evaluating codon de-optimized SARS-CoV-2 strain [59]. It is considered that these low proliferation rates contribute to the attenuated phenotype, but induce robust humoral and cellular immune responses. The currently used mRNA vaccines and adenovirus vectored vaccines encode only the spike protein, therefore limiting the immune response against only this viral antigen. However, live attenuated vaccines can induce immunity to several viral antigens, enhancing the chances of protection. For example, it was reported that an adenovirus vectored vaccine coding for the nucleocapsid protein was effective in mice and hamsters, suggesting that T-cell responses to this protein might also contribute to protect from infection [60]. The immune response against a variety of antigens generated by live attenuated vaccines may be an advantage over the current mRNA and adenovirus vectored vaccines.
Fig. 2.
Live attenuated SARS-CoV-2 vaccine candidates. Cold-adapted mutants replicate more slowly in the lower respiratory tract and lungs, compared to the wild type strain. Temperature-sensitive mutants cannot replicate at these locations. Codon de-optimized mutants show lower proliferation rates than the wild type strain, at any location.
Additionally, intranasal administration of live attenuated SARS-CoV-2 strains may stimulate the production of IgA, which is capable of preventing infection even by variant strains. The live attenuated influenza virus vaccine, an intranasally-administered, cold-adapted strain, induces IgA secretion and CD8+ T cell response [61], [62]. The secreted IgA contributes to cross-protection against different strains of the influenza virus [63]. One study reported that systemic neutralizing antibodies, passively administered or induced by vaccination, could not protect the nasal cavity from SARS-CoV-2 infection [64]. In contrast, mucosal IgA secretion has been reported to enhance SARS-CoV-2 neutralization [65]. Therefore, IgA induction by live attenuated vaccine candidates may contribute to protection against SARS-CoV-2 variants.
Although live attenuated vaccines are among one of the most powerful vaccine modalities, there are several problems related to their use. The most serious problem is that there is a chance of the viruses regaining their toxicity due to mutations after vaccination. A possible solution to this problem is to combine multiple responsible mutations. We have found mutations in different genes, such as nsp3 and nsp14, to be responsible for the temperature sensitivity. Several reverse genetics methods for SARS-CoV-2 have been reported, such as BAC DNA and CPER methods [66], [67]. Using these methods, it is possible to construct strains with various mutations, and thus maintain live attenuation, even when one responsible mutation is replaced by the wild type sequence.
In addition, adverse reactions due to the proliferation of the live attenuated vaccine strains in the nasal cavity should be evaluated. SARS-CoV-2 infection has been associated with the induction of cytokine storm and thrombosis [68], [69]. Moreover, olfactory dysfunction has been reported as a symptom and sequela of COVID-19, although the detailed mechanism underlying it has not yet been investigated [3]. The temperature-sensitive strains that we isolated were able to proliferate in the nasal cavity as the wild-type strain, thereby potentially disrupting the epithelial tissues. Therefore, its effects need to be evaluated in detail.
4. Discussion
Smallpox is one of the most harmful infectious diseases known to affect humans [70]. Jenner isolated a less pathogenic poxvirus and revealed that infection with this virus prevented the development of smallpox [71]. This was the first live attenuated vaccine, and the smallpox virus was eradicated because the vaccine was highly effective and easily preserved, even with the resources available at the time. Similarly, the number of poliovirus cases has decreased by over 99% since the late 1980 s [72], thanks to the use of vaccines. The orally administered vaccine against poliovirus is another live attenuated vaccine used to further reduce global polio case counts after the initial implementation of a policy to use an inactivated vaccine against poliovirus in the 1950 s [73], [74].
Although the live attenuated oral polio vaccine is still used for the global poliovirus eradication program in some countries, it has been eventually replaced by the inactivated vaccine in developed countries. In countries where the live attenuated vaccine is still in use, its drawbacks have become more evident as the number of infected people decreases. The live attenuated virus in the oral polio vaccine is able to replicate in the subject, and thus mutate, giving rise to vaccine-derived polioviruses (VDPV) that can reacquire neurovirulence and cause vaccine-associated paralytic poliomyelitis (PAPP). Although this rarely occurs, this is a serious adverse event and the number of reported cases of VDPV causing PAPP has recently caught the attention of the healthcare system. In order to avoid the occurrence of pathogenic VDPV, next-generation live attenuated viruses with safer and more stable genetic designs have been developed, and their practical implementation is expected [75].
For developing live attenuated SARS-CoV-2 vaccines, we also need to take into account the same issues that cause VDPV. For example, the introduction of multiple mutations, which are responsible for the attenuation mentioned above, is one of the methods to decrease the risk of reversion to a virulent phenotype. In addition, several factors involved in pathogenicity have been identified and described. For example, ORF8 has been reported to be a virulence factor associated with inflammation, and the furin cleavage site of the spike protein is important for virulence as well [76], [77]. The combination of these mutations may contribute to develop safer live attenuated vaccines.
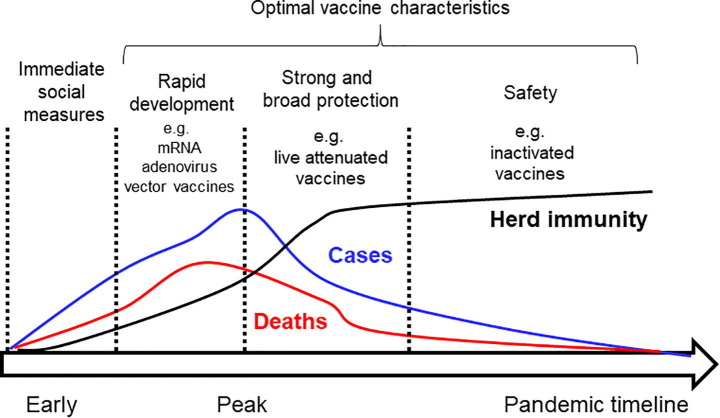
New technologies have been developed and improved since the development of these vaccines, and a wide range of vaccine modalities are currently available. A comprehensive understanding of each type can help policymakers decide which are the most appropriate for a specific stage in a pandemic, such as that of COVID-19 (Fig. 3 ). For example, nucleic acid and recombinant viral vectored vaccines, which are based on an antigen’s coding sequence, can be rapidly developed owing to advances in sequencing technologies. These vaccines should be adequate for the early stages of the pandemic, in combination with immediate social measures, such as lockdowns and containment of infected populations, to minimize or prevent further spread. Live attenuated vaccines take more time to develop because they rely on the amplification and weakening of the pathogenic attributes of the original virus. However, they can induce an immune response similar to that induced by a natural infection targeting several viral antigens, and are thus presumably more effective than the other vaccine types, although further studies are needed to provide the necessary evidence. Therefore, live attenuated vaccines are expected to be one of the most effective vaccines against different variants that may arise. Finally, although inactivated vaccines take longer to produce and may be less effective against variants, they may be a viable vaccine option for boosting immunizations due to their milder side effects, as the one for the seasonal influenza virus.
Fig. 3.
Differential vaccine selection for specific pandemic stages. Vaccine characteristics that are optimal for specific pandemic stages are described. Rapidly developed vaccines, such as nucleic acid and recombinant virus vaccines, can impede the rise in cases of infection in the early stages of a pandemic. Humoral and cellular immunity targeting several antigens induced by live attenuated vaccines should be more effective during periods of high morbidity and mortality. After most of the population is immunized, highly safe vaccines, like recombinant protein-based vaccines, would be more appropriate to be administered as boosters.
Overall, a strategy comprising the use of different types of vaccines, depending on the stage of a pandemic outbreak, could help improve control measures against the spread and survival of a pandemic-causing virus in the human population. COVID-19 has put humanity in an unprecedented situation. The acquired information and knowledge gained by testing different vaccine modalities in the COVID-19 pandemic will pave the way for improved and better strategies to combat future pandemics.
mRNAs have demonstrated to be highly effective, but limitations such as the requirement of a particularly strict cold-chain for their preservation, make it difficult to control SARS-CoV-2 infection on a global scale, relying mainly on this vaccine modality. Live attenuated vaccines using strains like the ones we isolated, would add an important modality to complement current ones.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We appreciate the assistance from Mitsuyo Kosaka (BIKEN). We thank Paola Miyazato (BIKEN) for reviewing the manuscript. We would like to thank Editage (www.editage.com) for English language editing.
References
- 1.Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Center C-M-JHCR.
- 3.Logue J.K., Franko N.M., McCulloch D.J., McDonald D., Magedson A., Wolf C.R., et al. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open. 2021;4(2):e210830. doi: 10.1001/jamanetworkopen.2021.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perlman S., Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat Rev Microbiol. 2009;7(6):439–450. doi: 10.1038/nrmicro2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lan J., Ge J., Yu J., Shan S., Zhou H., Fan S., et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581(7807):215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 6.Shang J., Wan Y., Luo C., Ye G., Geng Q., Auerbach A., et al. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci USA. 2020;117(21):11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ou X., Liu Y., Lei X., Li P., Mi D., Ren L., et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun. 2020;11(1) doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lv Z., Deng Y.-Q., Ye Q., Cao L., Sun C.-Y., Fan C., et al. Structural basis for neutralization of SARS-CoV-2 and SARS-CoV by a potent therapeutic antibody. Science. 2020;369(6510):1505–1509. doi: 10.1126/science.abc5881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giandhari J., Pillay S., Wilkinson E., Tegally H., Sinayskiy I., Schuld M., et al. Early transmission of SARS-CoV-2 in South Africa: An epidemiological and phylogenetic report. Int J Infect Dis. 2021;103:234–241. doi: 10.1016/j.ijid.2020.11.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kemp S.A., Collier D.A., Datir R., Ferreira I., Gayed S., Jahun A., et al. Neutralising antibodies in Spike mediated SARS-CoV-2 adaptation. medRxiv. 2020 [Google Scholar]
- 12.Galloway SE, Paul P, MacCannell DR, Johansson MA, Brooks JT, MacNeil A, et al. Emergence of SARS-CoV-2 B.1.1.7 Lineage - United States, December 29, 2020-January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:95-9. [DOI] [PMC free article] [PubMed]
- 13.Starr T.N., Greaney A.J., Hilton S.K., Ellis D., Crawford K.H.D., Dingens A.S., et al. Deep Mutational Scanning of SARS-CoV-2 Receptor Binding Domain Reveals Constraints on Folding and ACE2 Binding. Cell. 2020;182(5):1295–1310.e20. doi: 10.1016/j.cell.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baum A., Fulton B.O., Wloga E., Copin R., Pascal K.E., Russo V., et al. Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science. 2020;369(6506):1014–1018. doi: 10.1126/science.abd0831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wibmer C.K., Ayres F., Hermanus T., Madzivhandila M., Kgagudi P., Oosthuysen B., et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nat Med. 2021;27(4):622–625. doi: 10.1038/s41591-021-01285-x. [DOI] [PubMed] [Google Scholar]
- 16.England. PH. SARS-COV-2 variants of concern and variants under investigation in England Technical briefing 10. 7. May 2021.
- 17.Alaa Abdel Latif JLM, Manar Alkuzweny, Ginger Tsueng, Marco Cano, Emily Haag, Jerry Zhou, Mark Zeller, Nate Matteson, Chunlei Wu, Kristian G. Andersen, Andrew I. Su, Karthik Gangavarapu, Laura D. Hughes, and the Center for Viral Systems Biology. India Mutation Report. outbreak.info. 2021.
- 18.Edara VV, Norwood C, Floyd K, Lai L, Davis-Gardner ME, Hudson WH, et al. Reduced binding and neutralization of infection- and vaccine-induced antibodies to the B.1.351 (South African) SARS-CoV-2 variant. bioRxiv. 2021:2021.02.20.432046.
- 19.Oh S., Kessler J.A. Design, Assembly, Production, and Transfection of Synthetic Modified mRNA. Methods. 2018;133:29–43. doi: 10.1016/j.ymeth.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reichmuth A.M., Oberli M.A., Jaklenec A., Langer R., Blankschtein D. mRNA vaccine delivery using lipid nanoparticles. Ther Deliv. 2016;7(5):319–334. doi: 10.4155/tde-2016-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coronavirus (COVID-19) Vaccinations. https://ourworldindata.org/covid-vaccinations.
- 24.Kadali R.A.K., Janagama R., Peruru S., Malayala S.V. Side effects of BNT162b2 mRNA COVID-19 vaccine: A randomized, cross-sectional study with detailed self-reported symptoms from healthcare workers. Int J Infect Dis. 2021;106:376–381. doi: 10.1016/j.ijid.2021.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gorziglia M.I., Kadan M.J., Yei S., Lim J., Lee G.M., Luthra R., et al. Elimination of both E1 and E2 from adenovirus vectors further improves prospects for in vivo human gene therapy. J Virol. 1996;70(6):4173–4178. doi: 10.1128/jvi.70.6.4173-4178.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lusky M., Christ M., Rittner K., Dieterle A., Dreyer D., Mourot B., et al. In vitro and in vivo biology of recombinant adenovirus vectors with E1, E1/E2A, or E1/E4 deleted. J Virol. 1998;72(3):2022–2032. doi: 10.1128/jvi.72.3.2022-2032.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amalfitano A., Hauser M.A., Hu H., Serra D., Begy C.R., Chamberlain J.S. Production and characterization of improved adenovirus vectors with the E1, E2b, and E3 genes deleted. J Virol. 1998;72(2):926–933. doi: 10.1128/jvi.72.2.926-933.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qu H., Xia Y.u., Li X. Recombinant Human p53 Adenovirus Injection (rAd-p53) Combined with Chemotherapy for 4 Cases of High-grade Serous Ovarian Cancer. Curr Gene Ther. 2020;20(4):313–320. doi: 10.2174/1566523220666200826100245. [DOI] [PubMed] [Google Scholar]
- 29.van Doremalen N, Lambe T, Spencer A, Belij-Rammerstorfer S, Purushotham JN, Port JR, et al. ChAdOx1 nCoV-19 vaccine prevents SARS-CoV-2 pneumonia in rhesus macaques. Nature. 2020;586:578-82. [DOI] [PMC free article] [PubMed]
- 30.Mercado N.B., Zahn R., Wegmann F., Loos C., Chandrashekar A., Yu J., et al. Single-shot Ad26 vaccine protects against SARS-CoV-2 in rhesus macaques. Nature. 2020;586(7830):583–588. doi: 10.1038/s41586-020-2607-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng L., Wang Q., Shan C., Yang C., Feng Y., Wu J., et al. An adenovirus-vectored COVID-19 vaccine confers protection from SARS-COV-2 challenge in rhesus macaques. Nat Commun. 2020;11(1) doi: 10.1038/s41467-020-18077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ewer K.J., Barrett J.R., Belij-Rammerstorfer S., Sharpe H., Makinson R., Morter R., et al. T cell and antibody responses induced by a single dose of ChAdOx1 nCoV-19 (AZD1222) vaccine in a phase 1/2 clinical trial. Nat Med. 2021;27(2):270–278. doi: 10.1038/s41591-020-01194-5. [DOI] [PubMed] [Google Scholar]
- 33.Pai M.C.B., Stall N.M. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021. Vaccine-induced immune thrombotic thrombocytopenia (VITT) following adenovirus vector COVID-19 vaccination. [Google Scholar]
- 34.Cines D.B., Bussel J.B. SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia. N Engl J Med. 2021;384(23):2254–2256. doi: 10.1056/NEJMe2106315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kowarz E., Krutzke L., Reis J., Bracharz S., Kochanek S., Marschalek R. “Vaccine-Induced Covid-19 Mimicry” Syndrome: Splice reactions within the SARS-CoV-2 Spike open reading frame result in Spike protein variants that may cause thromboembolic events in patients immunized with vector-based vaccines. Res Square. 2021 [Google Scholar]
- 36.Fausther-Bovendo H., Kobinger G.P. Pre-existing immunity against Ad vectors: humoral, cellular, and innate response, what's important? Hum Vaccin Immunother. 2014;10(10):2875–2884. doi: 10.4161/hv.29594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jackson L.A., Gaglani M.J., Keyserling H.L., Balser J., Bouveret N., Fries L., et al. Safety, efficacy, and immunogenicity of an inactivated influenza vaccine in healthy adults: a randomized, placebo-controlled trial over two influenza seasons. BMC Infect Dis. 2010;10(1) doi: 10.1186/1471-2334-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao Q., Bao L., Mao H., Wang L., Xu K., Yang M., et al. Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 2020;369(6499):77–81. doi: 10.1126/science.abc1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amanat F., Strohmeier S., Rathnasinghe R., Schotsaert M., Coughlan L., Garcia-Sastre A., et al. Introduction of two prolines and removal of the polybasic cleavage site leads to optimal efficacy of a recombinant spike based SARS-CoV-2 vaccine in the mouse model. bioRxiv. 2020 doi: 10.1128/mBio.02648-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liang J.G., Su D., Song T.-Z., Zeng Y., Huang W., Wu J., et al. S-Trimer, a COVID-19 subunit vaccine candidate, induces protective immunity in nonhuman primates. Nat Commun. 2021;12(1) doi: 10.1038/s41467-021-21634-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jangra S, Ye C, Rathnasinghe R, Stadlbauer D, Personalized Virology Initiative study g, Krammer F, et al. SARS-CoV-2 spike E484K mutation reduces antibody neutralisation. Lancet Microbe. 2021. [DOI] [PMC free article] [PubMed]
- 42.Deng Xianding, Garcia-Knight Miguel A., Khalid Mir M., Servellita Venice, Wang Candace, Morris Mary Kate, et al. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell. 2021;184(13):3426–3437.e8. doi: 10.1016/j.cell.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sette Alessandro, Crotty Shane. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861–880. doi: 10.1016/j.cell.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tarke A., Sidney J., Methot N., Zhang Y., Dan J.M., Goodwin B., et al. Negligible impact of SARS-CoV-2 variants on CD4 (+) and CD8 (+) T cell reactivity in COVID-19 exposed donors and vaccinees. bioRxiv. 2021 doi: 10.1016/j.xcrm.2021.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dendouga Najoua, Fochesato Michel, Lockman Laurence, Mossman Sally, Giannini S.L. Cell-mediated immune responses to a varicella-zoster virus glycoprotein E vaccine using both a TLR agonist and QS21 in mice. Vaccine. 2012;30(20):3126–3135. doi: 10.1016/j.vaccine.2012.01.088. [DOI] [PubMed] [Google Scholar]
- 46.Parks C.L., Lerch R.A., Walpita Pramila, Wang Hai-Ping, Sidhu M.S., Udem S.A. Comparison of predicted amino acid sequences of measles virus strains in the Edmonston vaccine lineage. J Virol. 2001;75(2):910–920. doi: 10.1128/JVI.75.2.910-920.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Makino S., Sasaki K., Nakamura N., Nakagawa M., Nakajima S. Studies on the modification of the live AIK measles vaccine. II. Development and evaluation of the live AIK-C measles vaccine. Kitasato Arch Exp Med. 1974;47:13–21. [PubMed] [Google Scholar]
- 48.Takahashi Michiaki, Otsuka Terumasa, Okuno Yoshiomi, Asano Yoshizo, Yazaki Takehiko, Isomura Shin. Live vaccine used to prevent the spread of varicella in children in hospital. Lancet. 1974;304(7892):1288–1290. doi: 10.1016/s0140-6736(74)90144-5. [DOI] [PubMed] [Google Scholar]
- 49.Hilimire Thomas A., Nogales Aitor, Chiem Kevin, Ortego Javier, Martinez-Sobrido Luis. Increasing the Safety Profile of the Master Donor Live Attenuated Influenza Vaccine. Pathogens. 2020;9(2):86. doi: 10.3390/pathogens9020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murphy Brian R., Coelingh Kathleen. Principles underlying the development and use of live attenuated cold-adapted influenza A and B virus vaccines. Viral Immunol. 2002;15(2):295–323. doi: 10.1089/08828240260066242. [DOI] [PubMed] [Google Scholar]
- 51.Cox Nancy J., Kitame Fumio, Kendal Alan P., Maassab Hunein F., Naeve Clayton. Identification of sequence changes in the cold-adapted, live attenuated influenza vaccine strain, A/Ann Arbor/6/60 (H2N2) Virology. 1988;167(2):554–567. [PubMed] [Google Scholar]
- 52.Cox A, Dewhurst S. A Single Mutation at PB1 Residue 319 Dramatically Increases the Safety of PR8 Live Attenuated Influenza Vaccine in a Murine Model without Compromising Vaccine Efficacy. J Virol. 2015;90:2702-5. [DOI] [PMC free article] [PubMed]
- 53.Okamura S, Kashiwabara A, Suzuki H, Ueno S, Miyazato P, Takekawa S, et al. Live attenuated SARS-CoV-2 vaccine candidate: Protective immunity without serious lung lesions in Syrian hamsters. bioRxiv. 2021:2021.02.15.430863.
- 54.Deng Xufang, Mettelman Robert C., O’Brien Amornrat, Thompson John A., O’Brien Timothy E., Baker Susan C., et al. Analysis of Coronavirus Temperature-Sensitive Mutants Reveals an Interplay between the Macrodomain and Papain-Like Protease Impacting Replication and Pathogenesis. J Virol. 2019;93(12) doi: 10.1128/JVI.02140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Seo S.H., Jang Y. Cold-Adapted Live Attenuated SARS-Cov-2 Vaccine Completely Protects Human ACE2 Transgenic Mice from SARS-Cov-2 Infection. Vaccines (Basel) 2020;8 doi: 10.3390/vaccines8040584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coleman JR, Papamichail D, Skiena S, Futcher B, Wimmer E, Mueller S. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320:1784-7. [DOI] [PMC free article] [PubMed]
- 57.Mueller Steffen, Stauft Charles B., Kalkeri Raj, Koidei Fusataka, Kushnir Anna, Tasker Sybil, et al. A codon-pair deoptimized live-attenuated vaccine against respiratory syncytial virus is immunogenic and efficacious in non-human primates. Vaccine. 2020;38(14):2943–2948. doi: 10.1016/j.vaccine.2020.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clinicaltrials_gov. Safety and Immunogenicity of COVI-VAC, a Live Attenuated Vaccine Against COVID-19. 2020.
- 59.Wang Y, Yang C, Song Y, Coleman JR, Stawowczyk M, Tafrova J, et al. Scalable live-attenuated SARS-CoV-2 vaccine candidate demonstrates preclinical safety and efficacy. Proceedings of the National Academy of Sciences. 2021;118:e2102775118. [DOI] [PMC free article] [PubMed]
- 60.Matchett WE, Joag V, Stolley JM, Shepherd FK, Quarnstrom CF, Mickelson CK, et al. Nucleocapsid vaccine elicits spike-independent SARS-CoV-2 protective immunity. bioRxiv. 2021:2021.04.26.441518. [DOI] [PMC free article] [PubMed]
- 61.Clements M L, Betts R F, Tierney E L, Murphy B R. Serum and nasal wash antibodies associated with resistance to experimental challenge with influenza A wild-type virus. J Clin Microbiol. 1986;24(1):157–160. doi: 10.1128/jcm.24.1.157-160.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bodewes R, Fraaij PL, Geelhoed-Mieras MM, van Baalen CA, Tiddens HA, van Rossum AM, et al. Annual vaccination against influenza virus hampers development of virus-specific CD8(+) T cell immunity in children. J Virol. 2011;85:11995-2000. [DOI] [PMC free article] [PubMed]
- 63.Asahi-Ozaki Yasuko, Yoshikawa Tomoki, Iwakura Yoichiro, Suzuki Yujiro, Tamura Shin-ichi, Kurata Takeshi, et al. Secretory IgA antibodies provide cross-protection against infection with different strains of influenza B virus. J Med Virol. 2004;74(2):328–335. doi: 10.1002/jmv.20173. [DOI] [PubMed] [Google Scholar]
- 64.Zhou Dongyan, Chan Jasper Fuk-Woo, Zhou Biao, Zhou Runhong, Li Shuang, Shan Sisi, et al. Robust SARS-CoV-2 infection in nasal turbinates after treatment with systemic neutralizing antibodies. Cell Host Microbe. 2021;29(4):551–563.e5. doi: 10.1016/j.chom.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang Z., Lorenzi J.C.C., Muecksch F., Finkin S., Viant C., Gaebler C., et al. Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci Transl Med. 2021;13 doi: 10.1126/scitranslmed.abf1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ye C, Chiem K, Park JG, Oladunni F, Platt RN, 2nd, Anderson T, et al. Rescue of SARS-CoV-2 from a Single Bacterial Artificial Chromosome. mBio. 2020;11. [DOI] [PMC free article] [PubMed]
- 67.Torii Shiho, Ono Chikako, Suzuki Rigel, Morioka Yuhei, Anzai Itsuki, Fauzyah Yuzy, et al. Establishment of a reverse genetics system for SARS-CoV-2 using circular polymerase extension reaction. Cell Rep. 2021;35(3):109014. doi: 10.1016/j.celrep.2021.109014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yuan Xueting, Tong Xunliang, Wang Yan, Wang He, Wang Liuming, Xu Xiaomao. Coagulopathy in elderly patients with coronavirus disease 2019. Aging Med (Milton) 2020;3(4):260–265. doi: 10.1002/agm2.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Song Peipei, Li Wei, Xie Jianqin, Hou Yanlong, You Chongge. Cytokine storm induced by SARS-CoV-2. Clin Chim Acta. 2020;509:280–287. doi: 10.1016/j.cca.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.CDC. History of Smallpox. https://www.cdc.gov/smallpox/history/history.html.
- 71.Riedel Stefan. Smallpox and biological warfare: a disease revisited. Proc (Bayl Univ Med Cent) 2005;18(1):13–20. doi: 10.1080/08998280.2005.11928026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.WHO. Poliomyelitis. https://www.who.int/news-room/fact-sheets/detail/poliomyelitis.
- 73.Trevelyan Barry, Smallman-Raynor Matthew, Cliff Andrew D. The Spatial Dynamics of Poliomyelitis in the United States: From Epidemic Emergence to Vaccine-Induced Retreat, 1910–1971. Ann Assoc Am Geogr. 2005;95(2):269–293. doi: 10.1111/j.1467-8306.2005.00460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Miller Elizabeth. The most ambitious vaccine introduction in history. Vaccine. 2014;32(36):4599–4601. doi: 10.1016/j.vaccine.2014.05.057. [DOI] [PubMed] [Google Scholar]
- 75.Yeh Ming Te, Bujaki Erika, Dolan P.T., Smith Matthew, Wahid Rahnuma, Konz John, et al. Engineering the Live-Attenuated Polio Vaccine to Prevent Reversion to Virulence. Cell Host Microbe. 2020;27(5):736–751.e8. doi: 10.1016/j.chom.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Flower T.G., Buffalo C.Z., Hooy R.M., Allaire M., Ren X., Hurley J.H. Structure of SARS-CoV-2 ORF8, a rapidly evolving coronavirus protein implicated in immune evasion. bioRxiv. 2020 doi: 10.1073/pnas.2021785118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Johnson Bryan A., Xie Xuping, Bailey Adam L., Kalveram Birte, Lokugamage Kumari G., Muruato Antonio, et al. Loss of furin cleavage site attenuates SARS-CoV-2 pathogenesis. Nature. 2021;591(7849):293–299. doi: 10.1038/s41586-021-03237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Pfizer-BioNTech.html.
- 79.Chagla Z. The BNT162b2 (BioNTech/Pfizer) vaccine had 95% efficacy against COVID-19 >/=7 days after the 2nd dose. Ann Intern Med. 2021;174:JC15. doi: 10.7326/ACPJ202102160-015. [DOI] [PubMed] [Google Scholar]
- 80.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/Moderna.html.
- 81.Chagla Z. In high-risk adults, the Moderna vaccine had 94% efficacy against COVID-19 >/=14 d after the 2nd dose. Ann Intern Med. 2021;174:JC28. doi: 10.7326/ACPJ202103160-028. [DOI] [PubMed] [Google Scholar]
- 82.Chagla Z. In adults, the Oxford/AstraZeneca vaccine had 70% efficacy against COVID-19 >14 d after the 2nd dose. Ann Intern Med. 2021;174:JC29. doi: 10.7326/ACPJ202103160-029. [DOI] [PubMed] [Google Scholar]
- 83.Oliver Sara E., Gargano Julia W., Scobie Heather, Wallace Megan, Hadler Stephen C., Leung Jessica, et al. The Advisory Committee on Immunization Practices' Interim Recommendation for Use of Janssen COVID-19 Vaccine - United States, February 2021. MMWR Morb Mortal Wkly Rep. 2021;70(9):329–332. doi: 10.15585/mmwr.mm7009e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Russia’s Sputnik REUTERS.V https://www.reuters.com/article/us-health-coronavirus-russia-vaccine-idUSKBN2A21IT.
- 85.https://www.reuters.com/article/us-health-coronavirus-vaccine-pakistan-idUSKBN2A81N0.
- 86.https://www.reuters.com/article/uk-health-coronavirus-china-vaccine-idUKKBN2940ID.
- 87.https://www.who.int/news/item/01-06-2021-who-validates-sinovac-covid-19-vaccine-for-emergency-use-and-issues-interim-policy-recommendations.