Abstract
Objectives/background
Sleep is critical to recovery, but inpatient sleep is often disrupted. During the COVID-19 pandemic, social distancing efforts to minimize spread may have improved hospitalized children's sleep by decreasing unnecessary overnight disruptions. This study aimed to describe the impact of these efforts on pediatric inpatient sleep using objective and subjective metrics.
Methods
Sleep disruptions for pediatric inpatients admitted prior to and during the COVID-19 pandemic were compared. Hand hygiene sensors tracking room entries were utilized to measure objective overnight disruptions for 69 nights pre-pandemic and 154 pandemic nights. Caregiver surveys of overnight disruptions, sleep quantity, and caregiver mood were adopted from validated tools: the Karolinska Sleep Log, Potential Hospital Sleep Disruptions and Noises Questionnaire, and Visual Analog Mood Scale.
Results
Nighttime room entries initially decreased 36% (95% CI: 30%, 42%, p < 0.001), then returned towards baseline, mirroring the COVID-19 hospital census. However, surveyed caregivers (n_pre = 293, n_post = 154) reported more disrupted sleep (p < 0.001) due to tests (21% vs. 38%), anxiety (23% vs. 41%), and pain (23% vs. 48%). Caregivers also reported children slept 61 fewer minutes (95% CI: −12 min, −110 min, p < 0.001). Caregivers self-reported feeling more sad, weary, and worse overall (p < 0.001 for all).
Conclusions
Despite a decrease in objective room entries during the pandemic, caregivers reported their children were disrupted more and slept less. Caregivers also self-reported worse mood. This highlights the effects of the COVID-19 pandemic on subjective experiences of hospitalized children and their caregivers. Future work targeting stress and anxiety could improve pediatric inpatient sleep.
Keywords: Pediatrics, COVID-19, Sleep disruptions
1. Introduction
The importance of getting adequate sleep for children's physical and mental health has been widely demonstrated [1,2]. During periods of hospitalization, sleep is especially important due to its role in the processes of physical recovery [2]. As a result, patients who sleep less often take longer to recover [3]. Despite these known benefits, sleep in the hospital is often disrupted, with all pediatric age groups reporting less sleep and more awakenings in the hospital than at home [4]. Caregivers of patients on the pediatric hospital medicine ward have reported that checking vital signs, nurse/physician interruptions, and medication administrations are the most frequent causes of sleep interruption [5]. However, many of these interruptions are unnecessary [6], spurring the American Academy of Nursing's Choosing Wisely Campaign, which states that a patient's sleep “should not be disrupted unless their condition or care specifically requires it.” [7].
During the coronavirus disease of 2019 (COVID-19) pandemic, hospitals implemented social distancing measures and policies to reduce unnecessary interventions in order to minimize virus transmission and preserve personal protective equipment (PPE) [8]. Although less contact between patient and provider may be thought to have some deleterious effects on the quality of patient care, one potential positive consequence of these systemic changes is the inherent ability to improve the sleep of patients admitted to hospitals due to fewer room entries. Previous work has demonstrated that interventions targeting policy changes and clinician education can lead to fewer sleep disruptions [[9], [10], [11], [12]].
To the best of our knowledge, there has not been any examination of how the pandemic has affected the sleep of hospitalized children and their caregivers. We aimed to investigate the impact of COVID-19 physical distancing policies on overnight pediatric patient room entries, caregiver-reported pediatric sleep disruptions, and caregiver mood.
2. Methods
2.1. Study population
The study population consisted of a convenience sample of pediatric patients who were recruited at the University of Chicago Comer Children's Hospital. Eligible patients included children between the ages of 4 weeks–18 years who had spent the previous night on the pediatric general medicine inpatient ward, which also includes the neurology and gastroenterology services. The caregivers surveyed in this study had all spent the previous night with their child in the hospital room and spoke English. All patients were in single rooms and none of the children were recovering from recent surgery. Exclusion criteria, designed to obtain a study population of generally healthy children, included recent procedures and diagnoses that are known to disrupt sleep such as tracheostomy, nasogastric or gastrostomy tube, or sleep apnea. Those on bed rest, having long-term epilepsy monitoring, or who were known abuse victims were also excluded. This study was reviewed and approved by the Institutional Review Board at the University of Chicago Medicine and verbal consent was obtained from all participants.
2.2. Data collection
Hospital policies to increase social distancing were enacted on March 10th, 2020. We defined the data collected prior to that date from a previously ongoing study on inpatient sleep as “pre-pandemic” and data collected after that date through August 17th, 2020 as “pandemic.”
2.2.1. Room entries
Data collection primarily focused on objective measures of overnight disruptions as well as subjective perceptions of sleep and nighttime disruptions. Objective overnight disruptions were measured as the frequency of room entries using infrared technology incorporated into the GOJO SMARTLINK Hand-Hygiene system (GOJO Industries Inc., 2020, Akron, OH). This system, designed to monitor hand-hygiene compliance, tracks both hand sanitizer dispenses as well as room entries and exits via heat-sensing Activity Counters. To calculate hand-hygiene compliance, the number of sanitizer dispenses is divided by the number of room entries. For this study, only the Activity Counter data were utilized to analyze room entries [9]. Room entries were analyzed between January 1, 2020 and August 10, 2020.
2.2.2. Caregiver surveys
Subjective data were collected using a Pediatric Sleep Assessment, which included adaptations of several validated instruments including the Karolinska Sleep Log, Potential Hospital Sleep Disruption and Noises Questionnaire (PHSDNQ), and Visual Analog Mood Scale. The Karolinska Sleep Log is a validated tool that includes questions about typical sleep habits at home when the patient is not sick, sleep quality the previous night in the hospital, and any daytime sleep [13]. The PHSDNQ, which has been validated in adult populations and shown to have concurrent validity in pediatric populations, asks about a variety of factors that may disrupt a patient's sleep in the hospital including different medical interventions, patient symptoms, and environmental factors using a Likert-type scale [5,14]. The Visual Analog Mood Scale has been validated in adult populations and collects information on current caregiver mood [15]. In addition, surveys for patients older than 2 years included a validated Pediatric Sleep Questionnaire, and surveys for patients younger than 2 years included an adaption of the validated expanded Brief Infant Sleep Questionnaire [4,5]. Responses to the survey were stored using the REDCap Database Version 9.5.6 (Vanderbilt University, 2020, Nashville, TN). Caregivers pre-pandemic were surveyed in person, and during the pandemic, surveys were conducted over the phone.
2.3. Data analysis
2.3.1. Room entries
Room entry data were analyzed for both nighttime (11:00pm to 7:00am) and 24-hr room entries. One room entry was defined as the aggregate of all recorded room exits in a three-minute window in order to count a group as one single entry. Room entries without associated exits were not counted so as to avoid counting the caregiver's entrance to the room as a disruption. Nightly patient-occupied rooms were defined as those that had any room entries between the hours of 6pm and 7am in order to include rooms that had zero entries between 11pm and 7am. For 24-hour room entries, all rooms with fewer than two room entries were excluded to remove any rooms that did not have a patient in them. This number was determined by assuming that an occupied room would have a minimum of two entries for twice daily vital sign checks.
For both room entry timeframes, pre-pandemic and pandemic data were compared with an interrupted time series analysis (ITSA) to test for changes in room entries over time. The SEGMENTED function in R-4.0.2 was used to create a model and estimate final fitting parameters to the data as well as the corresponding uncertainties. This function utilizes a bootstrap restarting algorithm to estimate breakpoints from inputted estimates, analyzing the resultant data segments [16]. Fitted models were analyzed with the Davies test in order to determine statistical significance of breakpoints.
2.3.2. Caregiver surveys
Given the non-normal distribution of caregiver responses to the PHSDNQ, results were dichotomized at the median response. A response of 1 (not at all disruptive) was counted as “no disruption”, and a response from 2 (somewhat disruptive) to 5 (extremely disruptive) was counted as “disruption.” [5,14] The percentage of patients disrupted by each factor was calculated using the dichotomized data and the pre-pandemic and pandemic cohorts were compared using chi-squared tests. Means for caregiver reported patient sleep time and nighttime awakenings taken from the Karolinska Sleep Log were calculated and compared between timeframes for those younger than two years old and those two years or older using two factor t-tests. Visual Analog Mood Scale responses were summarized by median and interquartile range (IQR) analysis, and the distributions were compared using Wilcoxon rank-sum tests. Demographics were tested for significant differences using chi-squared tests. Data was analyzed with R-4.0.2. Because of concern for multiple comparisons, we used a conservative p-value of significance of p < 0.001.
3. Results
3.1. Study population
Between September 2018 and February 2020, 293 caregivers completed surveys. These surveys were utilized as our pre-pandemic cohort and were compared against 154 pandemic caregiver surveys collected between April 2020 and August 2020. Although there were significant racial and ethnic differences (p < 0.001), both cohorts consisted of patients from a diversity of racial and ethnic backgrounds with 71% and 52% identifying as Black/African American, 11% and 14% identifying as Hispanic, and 15% and 31% identifying as White/Caucasian in the pre-pandemic and pandemic cohorts respectively. There were also significant age group differences (p < 0.001), with fewer patients in the pandemic era younger than 2 (43% vs. 18%) and ages 2–5 (30% vs. 18%) and more patients ages 10–13 (5% vs. 21%) and 14 years and older (6% vs. 26%). In the 69 nights before the pandemic, of the total 60 general pediatric rooms, an average of 56 rooms were occupied each night. This fell to an average of 48 occupied rooms during the first 154 nights of the pandemic with the lowest recorded nightly census being 31 rooms. Consistent with all pediatric institutions across the country, we saw a decrease in the number of patients hospitalized with viral and respiratory illnesses during the pandemic (58% vs. 7%, p < 0.001) (Table 1 ).
Table 1.
Demographic information and primary diagnoses of surveyed patients.
| Pre-Pandemic n = 293 | Pandemic n = 154 | P-value | |
|---|---|---|---|
| Age | <0.001∗ | ||
| Younger than 2 | 125 (43%) | 27 (18%) | |
| 2 to 5 | 88 (30%) | 28 (18%) | |
| 6 to 9 | 46 (16%) | 22 (14%) | |
| 10 to 13 | 16 (5%) | 33 (21%) | |
| 14 and older | 18 (6%) | 44 (29%) | |
| Gender | 0.08 | ||
| Female | 146 (50%) | 65 (42%) | |
| Race/Ethnicity | <0.001∗ | ||
| Black/African American | 207 (71%) | 78 (52%) | |
| White/Caucasian | 43 (15%) | 47 (31%) | |
| Hispanic | 32 (11%) | 21 (14%) | |
| Asian/Pacific Islander | 3 (1%) | 3 (2%) | |
| Other | 7 (2%) | 2 (1%) | |
| Primary Dx | <0.001∗ | ||
| Respiratory | 169 (58%) | 11 (7%) | |
| MSK/skin | 41 (14%) | 27 (18%) | |
| GI/Liver | 24 (8%) | 22 (14%) | |
| Neuro/CNS | 15 (5%) | 32 (21%) | |
| Kidney/GU | 11 (4%) | 6 (4%) | |
| Othera | 26 (9%) | 38 (25%) | |
| Unknown | 7 (2%) | 18 (12%) |
Groups were compared using Chi-squared tests.
∗ = p < 0.001.
Common diagnoses in this group include sickle cell disease, hyperglycemia, leukemia, hypercalcemia, fever, dehydration, and failure to thrive.
3.2. Room entries
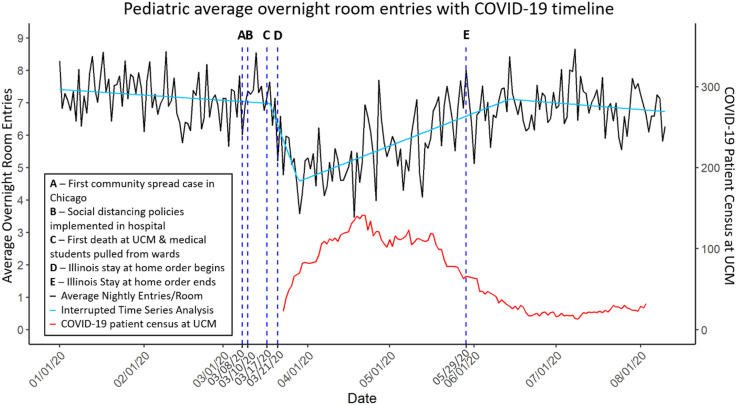
Consistent with previous work [4], pre-pandemic nightly room entries starting on January 1st, 2020 averaged a baseline of 7.2 room entries with no statistically significant slope over time. At the start of the pandemic, nighttime room entries initially decreased to 4.6 room entries equating to a 36% reduction (95% CI: 32%, 40%, p < 0.001). Room entries then increased by an average of 0.033 room entries per day (95% CI: 0.026, 0.040, p < 0.001). In June, soon after the end of the state's stay at home order, nightly entries returned to an average of 6.9 room entries each night, equating to 96% of pre-pandemic levels (95% CI: 92%, 100%, p = 0.01) (Fig. 1 ). Analysis of 24-hour entries showed a similar trend, starting at a pre-pandemic baseline of 37.7 room entries and initially decreased to 20.8 room entries, equating to a 45% reduction (95% CI: 38%, 52%, p < 0.001). 24-hour entries then returned towards pre-pandemic levels at a rate of 0.13 room entries per day (95% CI: 0.11, 0.15, p < 0.001), stabilizing in July to an average of 32.8 room entries each day, equating to 87% of pre-pandemic levels (95% CI: 81%, 93%, p < 0.001).
Fig. 1.
Interrupted time series analysis of average overnight room entries from GOJO heat-sensor data. Interrupted time series analysis is depicted by the teal line, which shows a 36% decrease in intercept at the onset of the pandemic (95% CI: 32%, 40%, p < 0.001). Abbreviations: University of Chicago Medicine (UCM).
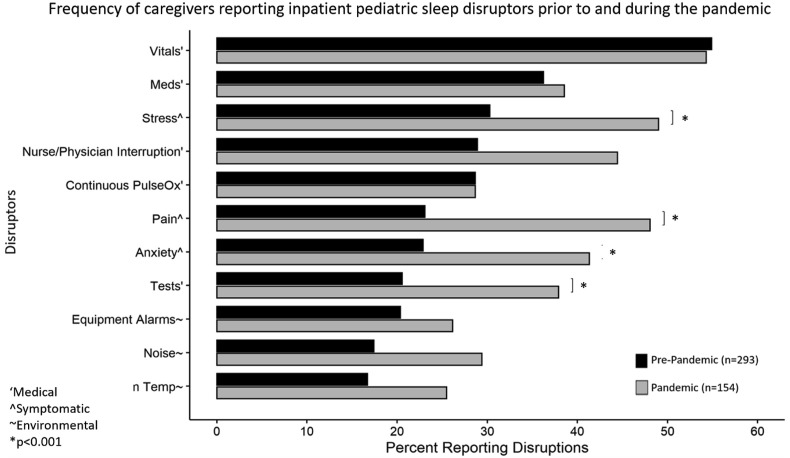
3.3. Subjective sleep disruptions
During the pandemic, caregivers reported significantly more disruptions to their children's sleep overnight due to medical tests (21% vs. 38%, p < 0.001) and symptomatic disruptors of stress (30% vs. 49%, p < 0.001), anxiety (23% vs. 41%, p < 0.001), and pain (23% vs. 48%, p < 0.001). There were no statistically significant changes to perceived disruptions from vital sign checks, nurse/physician interruptions, medication administration, pulse oximetry, equipment alarms, temperature, or noise (Fig. 2 ).
Fig. 2.
Caregiver survey responses to the Potential Hospital Sleep Disruption and Noises Questionnaire. Pre-pandemic and pandemic responses were compared using chi-squared tests. ∗ = p < 0.001.
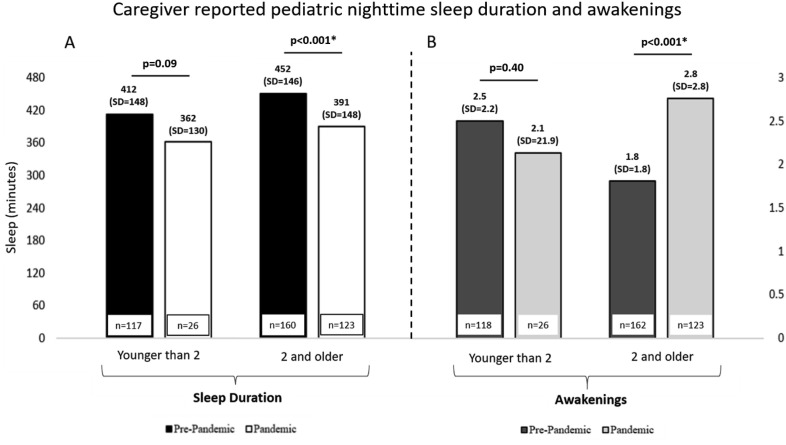
3.4. Sleep duration and awakenings
In addition to increased disruptors, caregivers of children two years and older reported that the patients experienced an average of 1.0 (95% CI: 0.2, 1.8, p < 0.001) more nighttime awakening during the pandemic, rising from an average of 1.8 pre-pandemic (n = 162) to 2.8 during the pandemic (n = 123). Caregivers also reported an average of 61 min less patient sleep during the pandemic (95% CI: −12, −110, p < 0.001) for patients two years and older, decreasing from 452 min pre-pandemic to 391 min during the pandemic. No statistically significant change in reported awakenings or sleep duration was seen for patients younger than two years old (Fig. 3 ).
Fig. 3.
Caregiver-reported patient mean nighttime sleep duration (A) and awakenings (B) using the Karolinska Sleep Log. Pre-pandemic and pandemic responses were compared using two factor t-tests. ∗ = p < 0.001.
3.5. Caregiver mood
When asked how they were feeling, caregivers reported on a 0 to 10 scale being more sad (0 (0–4) vs. 2 (0–6), p < 0.001) and weary (2 (0–5) vs. 5 (2–8), p < 0.001) as well as less calm (9 (6–10) vs. 7 (5–10), p < 0.001) during the pandemic. Caregivers also reported feeling worse overall during the pandemic (8 (7–10) vs. 7 (6–9), p < 0.001) (Table 2 ).
Table 2.
Caregiver self-reported moods.
| Pre-pandemic n = 294 Median (IQR) |
Pandemic n = 121 Median (IQR) |
P-value | |
|---|---|---|---|
| How alert do you feel? | 10 (7–10) | 8 (7–10) | p = 0.11 |
| How sad do you feel? | 0 (0–4) | 2 (0–6) | p < 0.001∗ |
| How tense do you feel? | 2 (0–5) | 4 (0–6) | p = 0.001 |
| How much of an effort is it to do anything? | 1 (0–5) | 1 (0–5) | p = 0.46 |
| How happy do you feel? | 8 (6–10) | 7 (5–9) | p = 0.001 |
| How weary do you feel? | 2 (0–5) | 5 (2–8) | p < 0.001∗ |
| How calm do you feel? | 9 (6–10) | 7 (5–10) | p < 0.001∗ |
| How sleepy do you feel? | 5 (1–9) | 5 (1–7) | p = 0.23 |
| Overall how do you feel? (0=very bad, 10=very good) | 8 (7–10) | 7 (6–9) | p < 0.001∗ |
Caregiver responses to the Visual Analog Mood Scale. Pre-pandemic and pandemic responses were compared using Wilcoxon rank-sums tests. ∗ = p < 0.001.
4. Discussion
This study examined the effect of hospital-wide social distancing policies during the COVID-19 pandemic on pediatric inpatient room entries, caregiver-reported pediatric sleep disruptions, and caregiver mood. Nighttime room entries initially decreased by 36% and then returned towards pre-pandemic levels. However, subjective caregiver reports of nighttime medical sleep disruptors for patients unexpectedly increased for tests, as did reports of symptomatic disruptors such as stress, anxiety, and pain. According to caregiver reports, patients two and older experienced more awakenings and less sleep while hospitalized during the pandemic. During this time, caregivers also reported that they themselves felt more weary and sad, less calm, and worse overall.
Objective and subjective disruption measures unexpectedly showed opposite trends, which may have been due to increased stress and anxiety resulting from the pandemic. The sharp increases in reported sleep disruptors from stress and anxiety as well as caregivers feeling less calm highlight the change in feelings during the pandemic. Hospitals became visible symbols of illness during the COVID-19 pandemic, and patients and their families may have feared contracting COVID-19 while in the hospital. Many hospitals and emergency departments saw a decrease in patient volume related to other diagnoses during the pandemic, which is also posited to be due to avoidance of the hospital and fear of COVID-19 [17,18]. For patients who did require hospitalization, caregivers may have felt more reluctant to be there compared to pre-pandemic times. Besides the pandemic itself, social unrest stemming from the attention to racial injustices around the country during this period as well as economic uncertainty may also have increased stress and anxiety. This is especially notable since most of the patients in this study identified as Black/African American and reside on the South Side of Chicago. That said, no statistically significant differences in results were found in race/ethnicity subgroup analysis. Since the subjective measures of disruptions rely on perception, interactions that may not have been perceived as disruptive pre-pandemic may have been perceived as disruptive during the pandemic, increasing perceived disruptions despite objective disruptions decreasing. Also, social distancing guidelines encouraged clinicians to batch tasks to reduce the number of essential room entries, which could have resulted in fewer room entries but more disruptive interactions. Additionally, patients hospitalized during the pandemic may have been more medically complex and required more involved care, resulting in more perceived disruptions being reported. Regarding objective disruptions, room entries increasing after the initial decrease may suggest some staff fatigue from social distancing policies leading to a gradual decrease in adherence, which highlights the difficulty of sustaining an intervention after initial implementation in a complex system such as a hospital [19,20].
This study has multiple implications for clinicians. The increase in reported sleep disruptors indicate a particular need to consider symptomatic factors including stress and anxiety in order to improve sleep for children in the hospital during this current pandemic. Addressing this increase in stress and anxiety due to being in the hospital during the pandemic may be critical to improving sleep outcomes. Care teams should consider ways that they can openly discuss the stress and anxiety surrounding hospitalization with patients and their families. Informational campaigns targeting safety, cleanliness, and infection risk of hospitals may help to allay patient and caregiver fears about hospitalization and improve their inpatient experience. Since nighttime tests are being perceived as more disruptive, there is an even greater need to minimize unnecessary tests administered during the night to those truly required by their medical condition in order for patients to experience improved sleep. This study also highlights the importance of subjective metrics for comprehensive quality improvement needs assessments as well as measures of the efficacy of interventions.
One limitation of this study is the differences in age, race/ethnicity, and primary diagnoses between the two study cohorts which could have affected results. Secondly, as this single-site study took place at an urban, academic medical center, the generalizability of these results may be affected. Additionally, the number of occupied rooms each night was not available, so assumptions were made on how to most accurately select those rooms based on room entry data. Survey collection during the pandemic was completed over the phone which could have introduced both a selection and a response bias compared to pre-pandemic in-person survey methods. Finally, no objective measure of sleep was used, so caregiver reports of patient sleep may misrepresent true sleep habits.
In summary, although objective measures of room entries showed a decrease in overnight disruptions during the COVID-19 pandemic, caregivers reported more nighttime disruptions and worse sleep for their hospitalized children. More work is needed to examine how to best address the concerns and subjective experiences of patients and their families in order to achieve better sleep in the hospital and improve the patient experience of hospitalized children and their caregivers. Future work involves the implementation and evaluation of an intervention targeting this reported stress and anxiety with the goal of improving pediatric inpatient sleep.
Funding
This research was supported by the University of Chicago Bucksbaum Institute for Clinical Excellence, the University of Chicago Pritzker School of Medicine Summer Research Program, and the National Heart, Lung, and Blood Institute [5K24HL136859-04].
Role of funder
The funders did not participate in the work.
Footnotes
None.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.05.020.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Paruthi S., Brooks L.J., D'Ambrosio C., et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of sleep medicine. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meltzer L.J., Davis K.F., Mindell J.A. Patient and parent sleep in a children's hospital. Pediatr Nurs. 2012 Mar-Apr;38(2):64–71. [PubMed] [Google Scholar]
- 3.Delaney L.J., Van Haren F., Lopez V. Sleeping on a problem: the impact of sleep disturbance on intensive care patients - a clinical review. Ann Intensive Care. 2015;5 doi: 10.1186/s13613-015-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erondu A.I., Orlov N.M., Peirce L.B., et al. Characterizing pediatric inpatient sleep duration and disruptions. Sleep Med. 2019;57:87–91. doi: 10.1016/j.sleep.2019.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peirce L.B., Orlov N.M., Erondu A.I., et al. Caregiver and staff perceptions of disruptions to pediatric inpatient sleep. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2018;14(11):1895–1902. doi: 10.5664/jcsm.7488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orlov N.M., Arora V.M. Things we do for No ReasonTM: routine overnight vital sign checks. J Hosp Med. 2020;15(5) doi: 10.12788/jhm.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Nursing Choosing wisely. Twenty-five things nurses and patients should question. https://www.choosingwisely.org/wp-content/uploads/2015/02/AANursing-Choosing-Wisely-List.pdf Published online July 2018.
- 8.Arora V.M., Arora V.M., Meltzer D. Implementing physical distancing in the hospital: a key strategy to prevent nosocomial transmission of COVID-19. J Hosp Med. 2020;15(5) doi: 10.12788/jhm.3434. [DOI] [PubMed] [Google Scholar]
- 9.Mokhlesi B., Arora V.M., Arora V.M. Effectiveness of SIESTA on objective and subjective metrics of nighttime hospital sleep disruptors. J Hosp Med. 2019;14(1) doi: 10.12788/jhm.3091. [DOI] [PubMed] [Google Scholar]
- 10.Edelson D., Carey K., Twu N. Acuity-based nighttime vital sign assessments: a randomized controlled trial. Abstracts. https://shmabstracts.org/abstract/acuity-based-nighttime-vital-sign-assessments-a-randomized-controlled-trial/
- 11.Stiver K., Sharma N., Kayla Geller, et al. “Quiet at Night”: reduced overnight vital sign monitoring linked to both safety and improvements in patients' perception of hospital sleep quality. Patient Exp J. 2017;4(1):90–96. doi: 10.35680/2372-0247.1185. [DOI] [Google Scholar]
- 12.Cook D.J., Arora V.M., Chamberlain M., et al. 2020. Improving hospitalized children's sleep by reducing excessive overnight Blood pressure monitoring. Pediatrics. Published online August 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaida K., Takahashi M., Åkerstedt T., et al. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin Neurophysiol. 2006;117(7):1574–1581. doi: 10.1016/j.clinph.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Grossman M.N., Anderson S.L., Worku A., et al. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2017;13(2):301–306. doi: 10.5664/jcsm.6468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monk T.H. A visual analogue scale technique to measure global vigor and affect. Psychiatry Res. 1989;27(1):89–99. doi: 10.1016/0165-1781(89)90013-9. [DOI] [PubMed] [Google Scholar]
- 16.Muggeo V. Segmented: an R package to fit regression models with broken-line relationships. R News. 2008;8:20–25. [Google Scholar]
- 17.Hartnett K.P. Vol. 69. MMWR Morb Mortal Wkly Rep; 2020. Impact of the COVID-19 pandemic on emergency department visits — United States. January 1, 2019–may 30, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeffery M.M., D'Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Int Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernstein M., Hou J.K., Weizman A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2016;14(10):1371–1375. doi: 10.1016/j.cgh.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 20.Scoville R., Little K., Rakover J., et al. Institute for Healthcare Improvement; Cambridge, MA: 2016. Sustaining improvement. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1