Abstract
Background:
Drug overdoses have contributed to considerable years of life lost. However, focusing solely on drug overdoses, whereby drug poisoning defines the underlying cause of death, obscures the wider burden of the drug mortality crisis. We aim to describe 21 years of trends in “psychotropic-drug-implicated deaths,” those where psychotropic drugs are a contributing (but not the underlying) cause of death.
Methods:
We analyze deaths extracted from CDC WONDER from 1999-2019 to generate annual counts and rates for psychotropic-drug-implicated deaths in the United States, including by underlying cause of death and drug implicated.
Results:
Over 21 years, 51,446 psychotropic-drug-implicated deaths occurred (33,885 medical; 17,561 external). Both medical and external psychotropic-drug-implicated deaths rose dramatically, increasing 2.5 and 5.0 times, respectively. Diseases of the circulatory system predominated underlying causes of medical deaths (74%). Non-drug suicide, transport accidents, and drownings constitute 54% of external underlying causes. Among the various underlying causes of death, psychotropic-drug-implicated deaths represent a considerable proportion, especially among external causes, with the proportion greatly increasing over the observation period. The drug implicated evolves from cocaine to opioids to psychostimulants, with the latter rising considerably.
Conclusions:
The drug mortality crisis extends beyond overdose and may temper improvements observed within other causes of mortality, such as cardiovascular disease, transport accidents, and drownings. As with overdoses, psychotropic-drug-implicated deaths have risen dramatically during the 21st century. They include striking increases for drugs, such as psychostimulants, receiving less attention with overdoses. Research is needed to address prevention, intervention, and policy for psychotropic-drug-implicated deaths beyond overdose mortality.
Keywords: drugs, mortality, overdose, population health
1.0. INTRODUCTION
The United States experienced considerable growth in fatal overdoses over the past 20 years, which contributed greatly to years of life lost (Case and Deaton 2014; Dowell et al. 2017; Ho 2017; Imtiaz et al. 2018; Jalal et al. 2018) and to broader societal costs (Birnbaum et al. 2011). Opioids have been a primary driver of increasing overdoses, unfolding in three waves corresponding to mortality associated with prescription opioids followed by heroin and most recently synthetic opioids such as fentanyl (Ciccarone 2019). Furthermore, overdose deaths from other prescription medications, such as benzodiazepines and stimulants, as well as cocaine and methamphetamine have also escalated (Bachhuber et al. 2016; Scholl et al. 2019). In this article, we examine whether the burden of the drug mortality crisis has grown even wider than overdose mortality indicates. By analyzing mortality data in which psychotropic drugs were a contributing but not the underlying cause of death, we consider the degree to which the drug mortality crisis extends beyond individuals lost to overdoses, and how such non-overdose deaths may even temper recent reductions in other causes of mortality.
Drug overdose deaths are often contrasted with other categories of mortality to demonstrate their impact on population health. For example, a common refrain is that opioid overdoses now account for more deaths annually than motor vehicle accidents (Hedegaard et al. 2015; Jones et al. 2015; Rudd et al. 2016; Unick et al. 2013). Indeed, external causes of death including motor vehicle fatalities (Sauber-Schatz et al. 2016; Weast 2018), non-drug-induced poisoning deaths such as those due to carbon monoxide (Hampson 2016), and drownings (Umapathi et al. 2020) have declined during the period in which drug overdoses have increased. Such declines are not limited to external causes of death; rates of medical causes of death have also decreased, including two leading causes of death in the U.S. Deaths from diseases of the circulatory system declined considerably since 2000, including among all major categories such as cardiovascular disease, heart disease, and stroke and across gender and racial groups (Sidney et al. 2016). Deaths from cancer also declined over the same period (Sidney et al. 2016; Curtin 2019). By contrast, other categories of deaths have increased alongside drug overdoses during the past two decades, including suicide (Rossen et al. 2018), deaths attributable to falls (Burns and Kakara 2018; Peterson and Kegler 2020), and deaths attributable to alcohol (White et al. 2020). However, drug overdoses are often contrasted with these other causes of death as if independent. Instead, drug use and dependence must be considered together with their contribution to the burden of morbidity and mortality more generally (Degenhardt and Hall 2012).
The U.S. CDC categorizes drug-related deaths in a manner that focuses on drugs as the underlying cause of death rather than a wider scope of deaths in which psychotropic drugs are implicated as a contributing factor. The CDC’s definition of drug overdose mortality requires that poisoning from the drug is the underlying cause of death to be counted as an overdose. These deaths have ICD-10 underlying cause of death codes for “drug poisoning” (see methods section) and are not limited to psychotropic drugs. Also, in some tabulations, overdose deaths are combined with particular ICD codes and termed “drug-induced mortality” (Kochanek et al. 2019). However, these deaths can also be due to any substance whether psychotropic or not, only apply to a specific set of ICD codes, and do not include any non-poisoning external causes of death where psychotropic drugs may have been a factor.
These constraints, together with considerable focus on overdose deaths in scientific and media representations of the problem, obscures how growth in psychotropic drug-related problems have shaped patterns of mortality beyond overdose as an underlying cause of death. In this article, we focus on deaths in which psychotropic drugs were a contributing but not underlying cause of death, which we refer to as “psychotropic-drug-implicated deaths.” By examining the cooccurrence of deaths due to other causes involving a psychotropic drug, we gain clarity into the greater toll of the current drug-related mortality crisis beyond overdose deaths. In this article, we assess trends in psychotropic-drug-implicated deaths since 1999 and how this varies by the underlying cause of death. Countervailing trends may impede improvements otherwise experienced for certain causes of death or exacerbate causes of death that are increasing.
2.0. METHODS
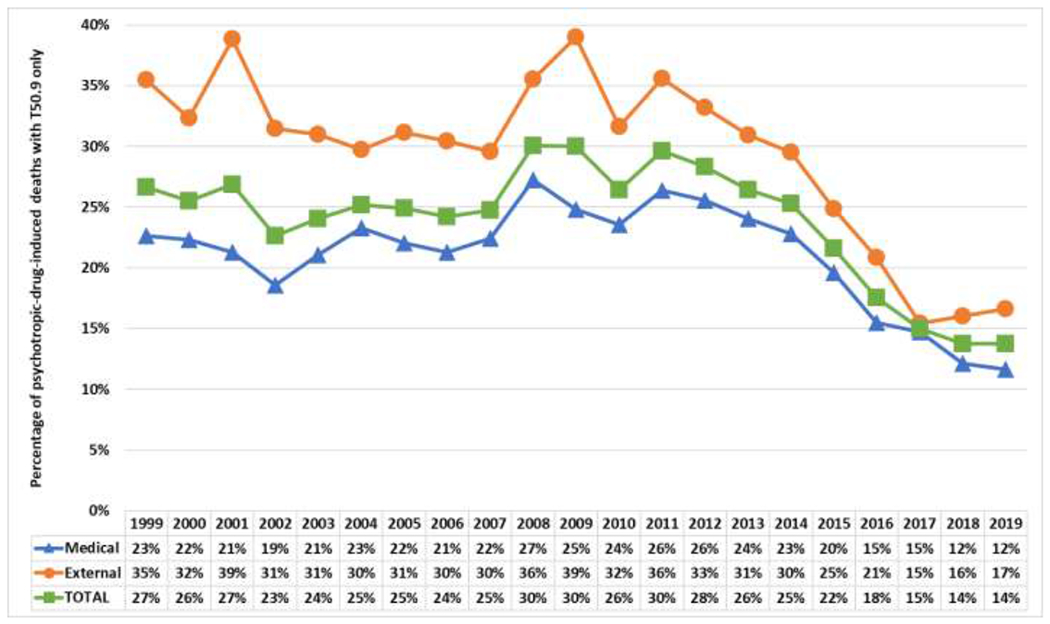
We utilized CDC WONDER Multiple Cause of Death data for a twenty-one-year period, 1999-2019, which contains every death in the U.S. Cause of death codes allowed identification of the “underlying cause” as well as any other cause (“multiple cause”) implicated in the death (up to 10). The CDC classifies drug overdoses as those with ICD-10 underlying cause of death codes for “drug poisoning” (X40-X44, X60-X64, X85, and Y10-Y14). Thus, the CDC definition includes all substances that lead to poisoning in their definition, psychotropic or not. For this article, we consider only those that are combined with multiple cause of death codes in the following categories for psychotropic substances to compute the psychotropic drug overdose rate: poisoning by, adverse effect of and underdosing of narcotics and psychodysleptics (T40.0-T40.9); antiepileptic, sedative-hypnotic and antiparkinsonism drugs (T42.0-T42.8); and psychotropic drugs, not elsewhere classified (T43.0-T43.9). Within the present manuscript, we examine deaths where the underlying cause of death was not indicated as drug poisoning, but in which the multiple cause of death codes listed above were included as contributing causes. Thus, these deaths are not tallied with psychotropic drug overdoses, but a drug was present at the time of death and listed as a contributing cause of the death. Hence, we refer to them as psychotropic-drug-implicated deaths. When a substance is completely unknown, it may also potentially get coded as unspecified drugs, medicaments, and biological substances (T50.9). However, given that this category can include non-psychotropic substances as well, we do not include it in primary analyses, but show select analogous figures in Appendix C, which lead to similar conclusions.
We then classified the remaining ICD-10 underlying cause of death codes as medical (AA00-F09; F20-R99) or external (V01-Y98, excluding drug poisoning codes listed above) causes of death. Broadly, medical causes of death include death due to diseases, disorders, malformations, or other medical conditions. Essentially, medical deaths are caused by processes internal to the human body. In contrast, external causes of death involve mortality attributable to accidents (including transport accidents), drowning, non-drug poisonings, exposure, self-harm, assault, overexertion, and similar incidents. We also note that in 2006 the CDC ceased using a series of codes for drug-related mental and behavioral disorders (F10-F19) to indicate poisonings due to overdose. Previously, a small number of overdoses were coded therein. As these are not our focus, these presumed overdoses are described in Appendix A and not included within psychotropic-drug-implicated deaths, but rather included in drug overdoses. We include a full list of the multiple cause of death codes, their descriptions, and our classifications in Appendix B.
To investigate specific controlled substances implicated in these deaths, we examine deaths implicating opioids (T40.0-T40.4; T40.6), cocaine (T40.5), cannabis (T40.7), benzodiazepines (T42.4), and psychostimulants with abuse potential (T43.6). We also disaggregate opioids into heroin (T40.1), natural and semi-synthetic (T40.2), methadone (T40.3), and synthetic other than methadone (T40.4).
As these analyses provide an overview of trends in psychotropic-drug-implicated deaths and are a complete census of deaths, we rely first upon descriptive statistics, with data shown graphically. Additionally, we use CDC standard joinpoint regression methodology for assessing significant changes (p<.05) in aggregate rates over time (Kim et al. 2000) using the National Cancer Institute’s Joinpoint software (NCI 2021).
3.0. RESULTS
3.1. Age-adjusted death rates over time
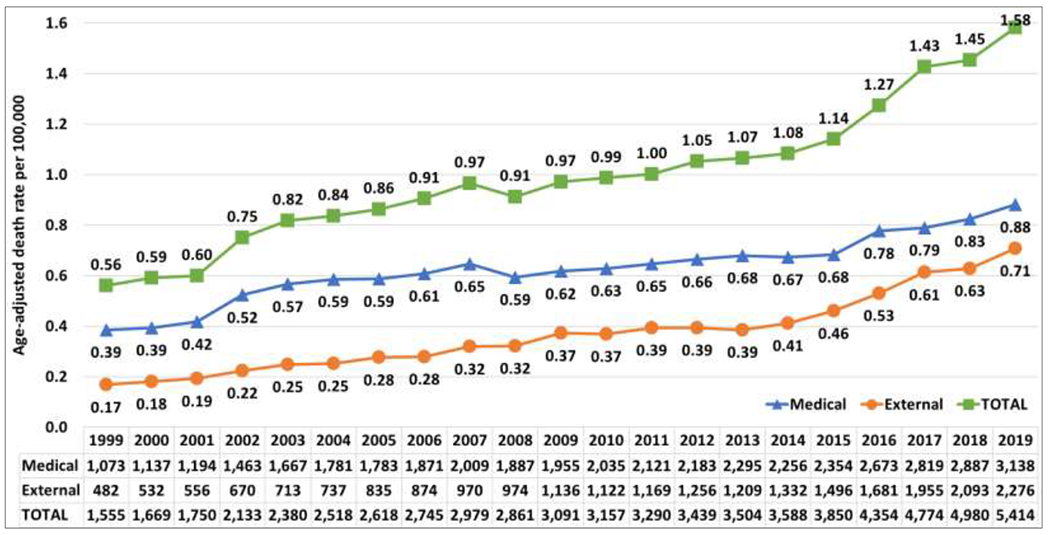
Figure 1 shows trends in all deaths and by medical and external causes of death in which a psychotropic drug was implicated. The lines represent age-adjusted death rates per 100,000, while the table beneath shows the number of deaths. An increasing trend is immediately clear. From 1999 to 2019, the rate of annual psychotropic-drug-implicated medical deaths increased 2.5 times from 0.31 to 0.78 per 100,000. During the same period, the rate of annual psychotropic-drug-implicated external deaths increased 5.0 times from 0.12 to 0.58. Thus, in total, the annual psychotropic-drug-implicated death rate rose from 0.40 to 1.37 per 100,000. The increases in all three trends are statistically significant. Summing all deaths over this period, 51,446 deaths (33,885 medical and 17,561 external) occurred where psychotropic drugs were noted as a contributing cause of death, but such deaths are not reflected in mortality confined to overdose deaths. During the same period, there were 649,697 psychotropic drug overdoses. If combined, the total increases 7.9% beyond overdose deaths alone.
Figure 1:
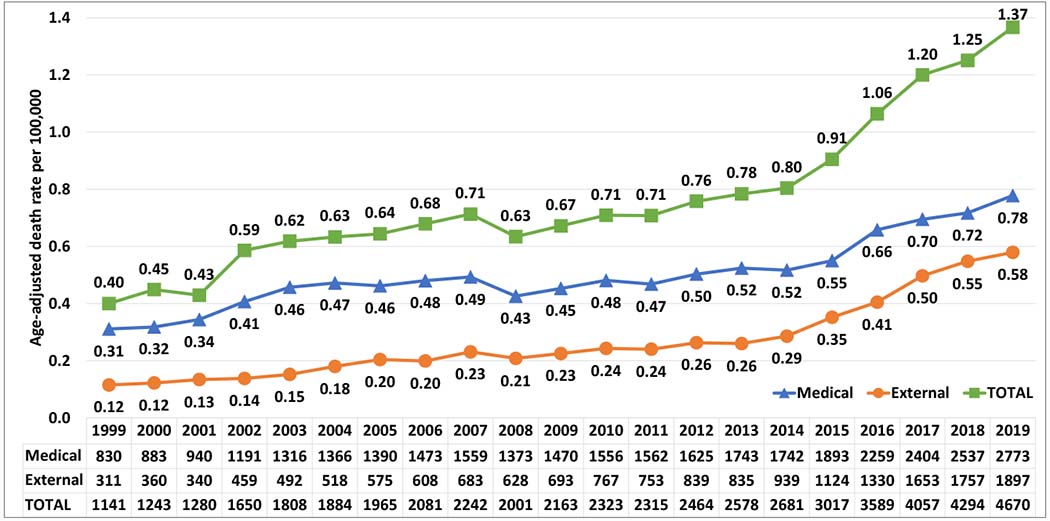
Psychotropic-drug-implicated age-adjusted death rate per 100,000 (lines) and number of deaths (table) by year, total and by type
Note: Psychotropic-drug-implicated deaths are defined as those with multiple cause of death ICD-10 codes T40, T42, and T43, but not an underlying. cause of death of drug poisoning (X40-X44, X60-X64, X85, and Y10-Y14). For underlying cause of death ICD-12 codes defined as medical and external, see Appendix B.
Note: For the total death rate, there is a significant increasing trend (p<.05) across all years 1999-2019 with a best-fitting model of 2 joinpoints and 3 slopes (1999-2003, 2003-2013, 2013-2019). For the medical death rate, there is a significant increasing trend (p<.05) from 1999-2003 and 2014-2019 with a best-fitting model of 2 joinpoints and 3 slopes. For the external death rate, there is a significant increasing trend (p<.05) across all years 1999-2019 with a best-fitting model of 1 joinpoint and 2 slopes (1999-2014, 2014-2019).
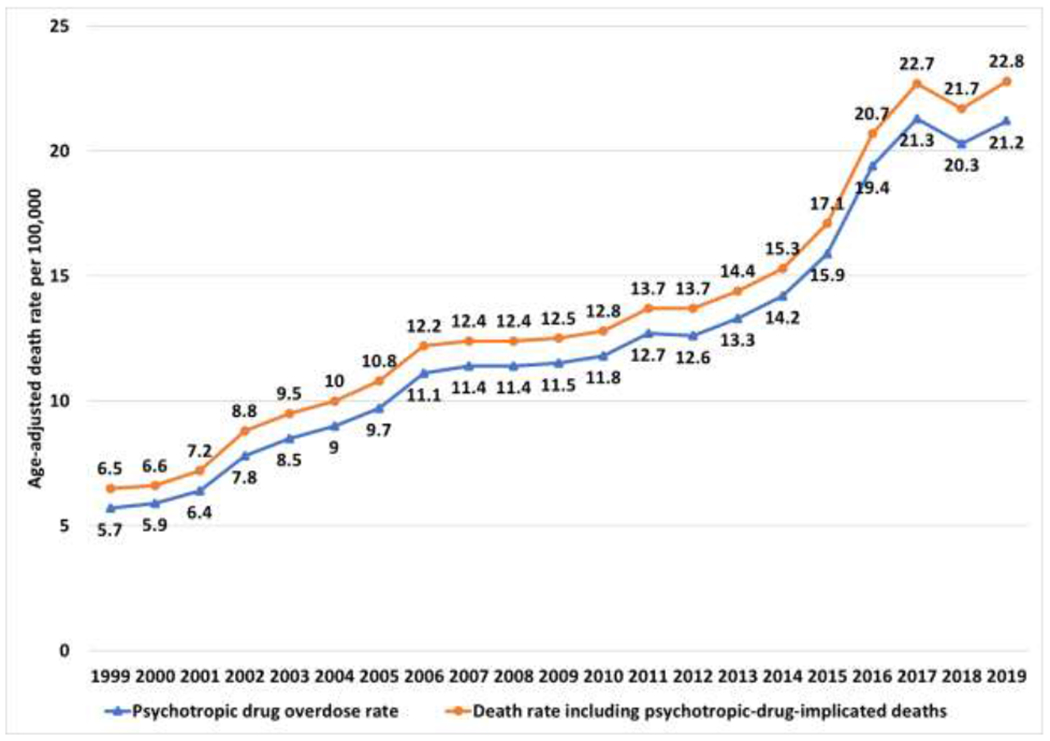
Figure 2 further demonstrates the difference in the death rate due to psychotropic drugs if psychotropic-drug-implicated deaths are included alongside overdoses. For both, there is a statistically significant increase through 2017. On average across all years, the death rate with psychotropic-drug-implicated deaths included is higher by about 0.8 deaths per 100,000. However, there is variability in this amount. From 1999 to 2001, this gap is about 0.4. From 2002 to 2014, the difference is between 0.6 and 0.9 in most years. In 2015, a concerning increase begins to occur. Each year from 2014 to 2019, the gap increased by about 0.1, such that by 2019, the death rate for all psychotropic-drug-related deaths is higher by 1.3 per 100,000 than those specific to psychotropic drug overdose mortality.
Figure 2:
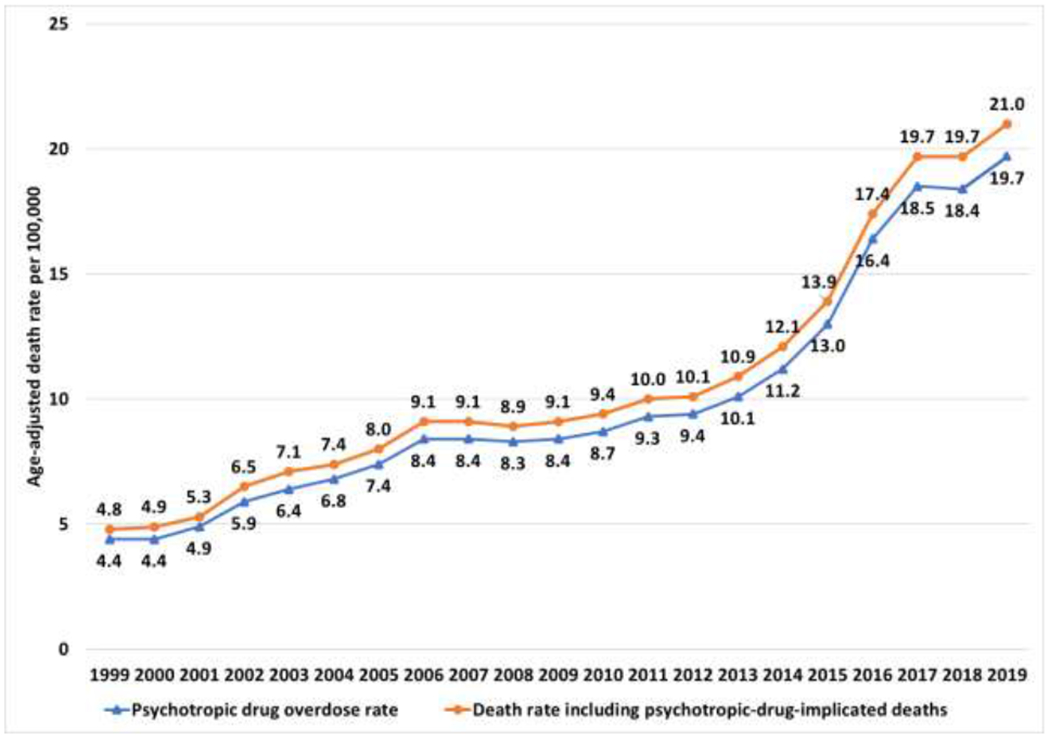
Death rate per 100,000 for psychotropic drug overdose as underlying cause of death and with psychotropic-drug-implicated deaths included
Note: Bottom line includes psychotropic drug poisonings only (i.e. underlying cause of death X40-X44, X60-X64, X85, Y10-14, or F10-F19, and a multiple cause of death code T40, T42, or T43). Top line includes all deaths with multiple cause of death code T40, T42, or T43 regardless of underlying cause.
Note: For both rates displayed, there is a significant increasing trend (p<.05) from 1999-2006, 2010-2014, and 2014-2017 with a best-fitting model of 4 joinpoints and 5 slopes.
3.2. By Category of Underlying Cause of Death
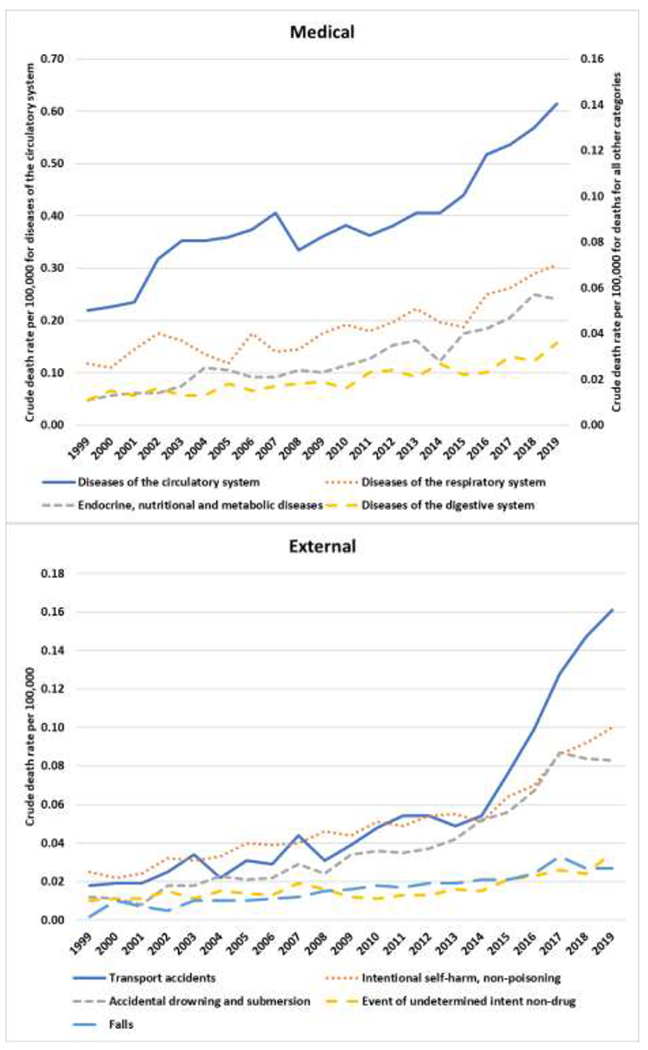
Figure 3 breaks down the medical (top) and external (bottom) causes of death by specific ICD-10 categories. From the top of Figure 3, we see that the vast majority of psychotropic-drug-implicated medical deaths fall under diseases of the circulatory system. These 25,191 deaths account for 74.3% of all psychotropic-drug-implicated medical deaths, dwarfing the next category, diseases of the respiratory system with 2748 deaths. Endocrine, nutritional, and metabolic disease; diseases of the digestive system; and certain infectious and parasitic disease round out the top five psychotropic-drug-implicated medical causes of death. In the bottom of Figure 3, there is a more varied picture. Both transport accidents and non-poisoning intentional self-harm (i.e. suicide from causes other than drugs or alcohol) are the two most common psychotropic-drug-implicated external causes, resulting in 3725 and 3266 deaths, respectively. With 2514 deaths, drowning is also a common external cause. These top three categories account for over half (54.1%) of all psychotropic-drug-implicated external causes. Figure 4 shows temporal trends of medical and external causes, limiting the figure to those causes with at least 1000 deaths across all years. Due to the outsized number of circulatory disease deaths, this category is shown on its own axis in the top panel of Figure 4, while the remaining three categories are on the secondary axis. The consistent upward trend across the four categories is apparent. All categories of external causes also increase in the bottom panel. For most years, suicides and transport accidents are fairly similar as the predominant categories. However, the rapid increase in psychotropic-drug-implicated transport accident deaths from 2014 to 2019 is striking, overtaking suicides as the leading external cause. Given the low count during the early years, age-adjusted death rates are considered unreliable, but crude death rates are shown in Appendix D.
Figure 3:
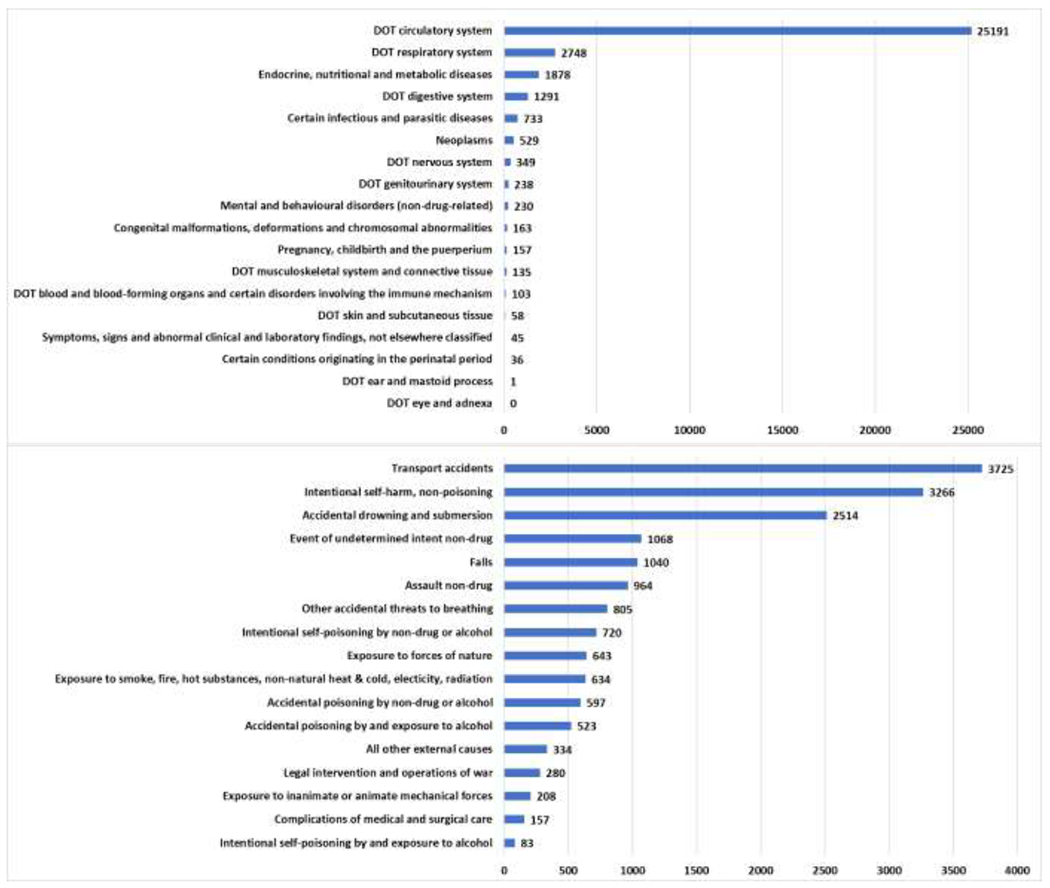
Psychotropic-drug-implicated deaths by underlying cause of death
Note: DOT = “Diseases of the”; Medical and external deaths are on different scale axes.
Figure 4:
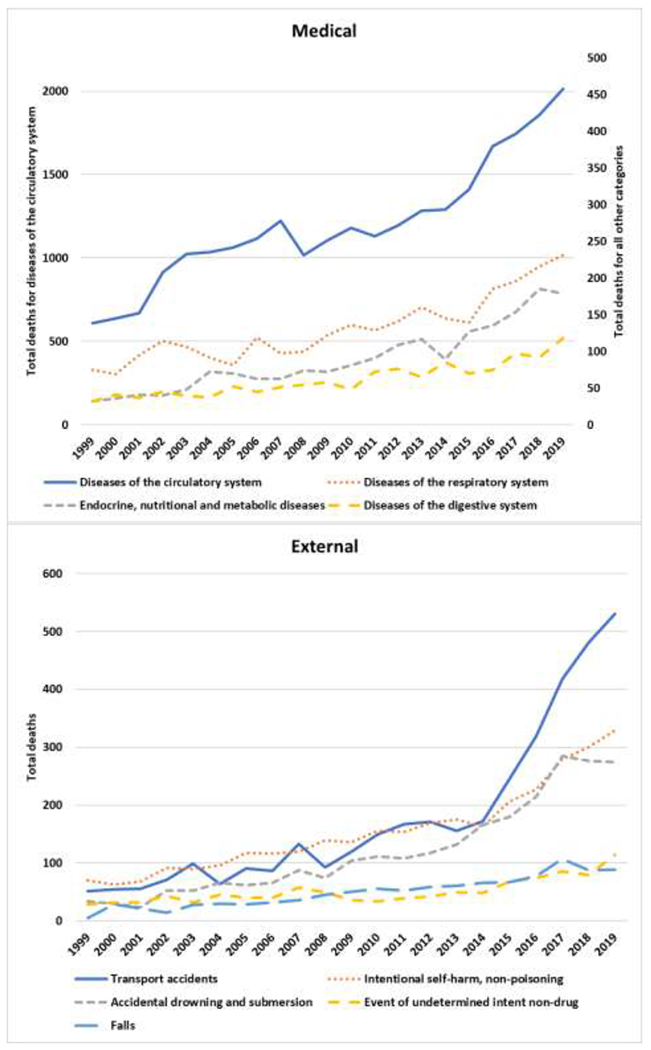
Psychotropic-drug-implicated deaths by year and common underlying causes of death (those with more than 1000 across all years)
Table 1 shows the degree to which psychotropic-drug-implicated deaths contribute to deaths within the categories of underlying causes by considering 1 in how many such deaths are psychotropic-drug-implicated. Categories are listed in the order shown in Figure 3. While the number reported in Figure 3 for the most common psychotropic-drug-implicated category, diseases of the circulatory system (25,191), might seem small in comparison to the total deaths (17,855,050), those numbers still indicate that 1 in every 709 circulatory system deaths over the 21 years of observation were psychotropic-drug-implicated. We also show 1999 and 2019 for comparison. Although there were fewer circulatory system deaths overall in 2019 compared to 1999 despite growth in the U.S. population, psychotropic-drug-implicated deaths increased considerably and became a larger proportion of circulatory deaths. Whereas 1 in every 1564 deaths were psychotropic-drug-implicated in 1999, 1 in every 434 circulatory system deaths were by 2019. While not as common among other medical causes of death, nearly every category experienced an increased proportion of deaths that were psychotropic-drug-implicated.
Table 1:
Psychotropic-drug-induced deaths relative to all deaths within ICD-10 underlying cause of death categories
| All years 1999-2019 | 1999 | 2019 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| All deaths | Psychotropic-drug-implicated are about 1 in X deaths | All deaths | Psychotropic-drug-implicated are about 1 in X deaths | All deaths | Psychotropic-drug-implicated are about 1 in X deaths | |
|
|
|
|
||||
| Medical | ||||||
| Diseases of the circulatory system | 17,855,050 | 709 | 954,339 | 1,564 | 874,613 | 434 |
| Diseases of the respiratory system | 5,187,487 | 1,888 | 229,863 | 3,065 | 271,026 | 1,173 |
| Endocrine, nutritional and metabolic diseases | 2,254,532 | 1,200 | 92,872 | 2,902 | 140,107 | 783 |
| Diseases of the digestive system | 1,979,096 | 1,533 | 82,876 | 2,590 | 112,894 | 957 |
| Certain infectious and parasitic diseases | 1,400,955 | 1911 | 59,984 | 3,749 | 64,706 | 980 |
| Neoplasms | 12,349,887 | 23,346 | 563,065 | 62,563 | 615,191 | 12,555 |
| Diseases of the nervous system | 3,054,820 | 8,753 | 84,077 | 7,643 | 233,715 | 7,791 |
| Diseases of the genitourinary system | 1,337,306 | 5,619 | 53,127 | 5,313 | 72,871 | 3,644 |
| Mental and behavioral disorders, unrelated to drugs | 1,947,228 | 8,466 | 33,509 | 2,234 | 118,796 | 10,800 |
| Congenital malformations, deformations and chromosomal abnormalities | 212,302 | 1,302 | 10,393 | 2,598 | 9,713 | 883 |
| Pregnancy, childbirth and the puerperium | 17,553 | 112 | 406 | — | 1,103 | 158 |
| Diseases of the musculoskeletal system and connective tissue | 291,083 | 2,156 | 13,347 | 1,668 | 14,553 | 1,617 |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 209,777 | 2,037 | 9,067 | 2,267 | 10,815 | 1,082 |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 711,692 | 15,815 | 26,672 | 8,891 | 32,408 | 6,482 |
| Certain conditions originating in the perinatal period | 271,207 | 7,534 | 14,259 | 14,259 | 10,412 | 10,412 |
| Diseases of the skin and subcutaneous tissue | 89,668 | 1,546 | 3,697 | — | 5,229 | 475 |
| Diseases of the ear and mastoid process | 1,483 | 1,483 | 74 | — | 90 | — |
| Diseases of the eye and adnexa | 999 | — | 44 | — | 56 | — |
| External | ||||||
| Transport accidents | 896,725 | 241 | 45,927 | 901 | 41,143 | 78 |
| Intentional self-harm, non-poisoning | 663,023 | 203 | 24,287 | 347 | 41,353 | 126 |
| Accidental drowning and submersion | 74,207 | 30 | 3,529 | 104 | 3,692 | 13 |
| Event of undetermined intent non-drug | 36,853 | 35 | 1,405 | 48 | 2,093 | 18 |
| Falls | 531,413 | 511 | 13,162 | 2,632 | 39,443 | 443 |
| Assault non-drug | 362,859 | 376 | 16,709 | 726 | 18,777 | 174 |
| Other accidental threats to breathing | 129,639 | 161 | 5,503 | 550 | 7,076 | 124 |
| Intentional self-poisoning by non-drug or alcohol | 30,206 | 42 | 1,688 | 84 | 1,302 | 26 |
| Exposure to forces of nature | 29,141 | 45 | 1,488 | 124 | 1,806 | 27 |
| Exposure to smoke, fire, hot substances, non-natural heat & cold, electricity, radiation | 71,453 | 113 | 3,950 | 658 | 3,069 | 43 |
| Accidental poisoning by non-drug or alcohol | 19,847 | 33 | 711 | 102 | 1,310 | 18 |
| Accidental poisoning by and exposure to alcohol | 30,525 | 58 | 320 | 32 | 2,291 | 57 |
| All other external causes | 182,439 | 546 | 9,463 | 1,577 | 8,815 | 294 |
| Legal intervention and operations of war | 9,849 | 35 | 399 | 67 | 653 | 19 |
| Exposure to inanimate or animate mechanical forces | 56,443 | 271 | 2,953 | 422 | 2,593 | 123 |
| Complications of medical and surgical care | 61,535 | 392 | 2,742 | 343 | 5,258 | 1,052 |
| Intentional self-poisoning by and exposure to alcohol | 771 | 9 | 24 | 3 | 46 | 9 |
The numbers for the external causes show an even starker trend, where psychotropic-drug-implicated deaths constitute an outsized number within every category, and nearly every category experienced a very large increase in the proportion of such deaths between 1999 and 2019. Like circulatory system deaths, transport accident deaths improved overall. However, psychotropic-drug-implicated deaths increased from 1 in 901 transport accidents in 1999 to an incredible 1 in 78 in 2019. Even among a category where overall deaths increased substantially such as non-poisoning intentional self-harm (i.e. suicide), the number of psychotropic-drug-implicated deaths increased from 1 in 347 to 126. Psychotropic drugs contributed to a staggering 1 in 13 drownings in 2019 (and 1 in 30 over the entire period). The increase was also considerable for falls (1 in 2632 to 1 in 443), non-drug assaults (1 in 726 to 1 in 174), accidental threats to breathing (1 in 550 to 1 in 124), exposure to forces of nature (1 in 124 to 1 in 27), and exposure to smoke, fire, heat, cold, electricity, and radiation (1 in 658 to 1 in 43).
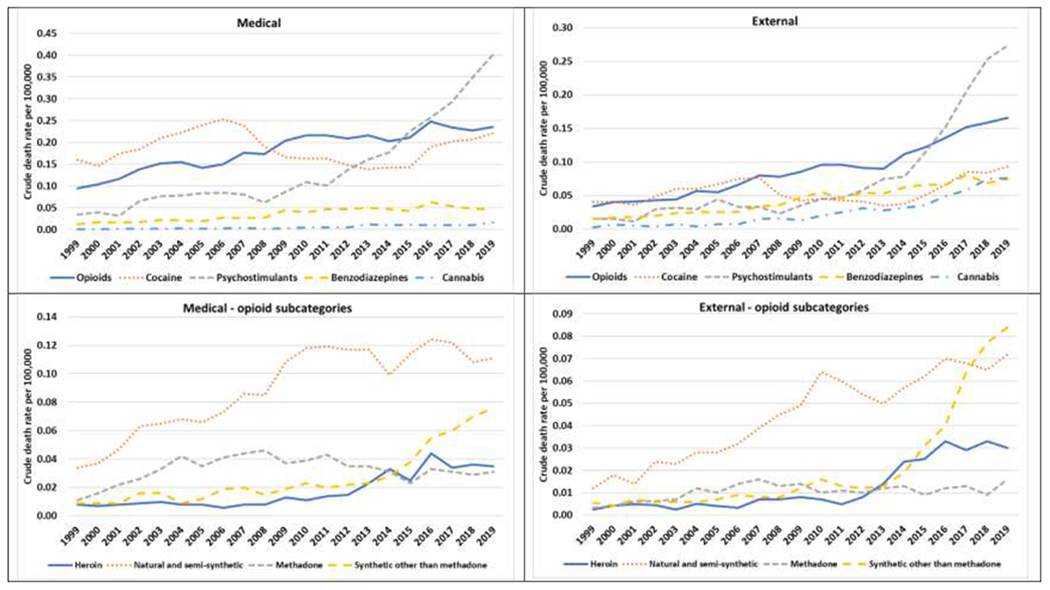
3.3. By Substance Implicated
The left panels of Figure 5 consider trends in specific controlled substances implicated in medical deaths. The top panel considers broad classes of drugs. Opioid-implicated medical deaths increase steadily across the period of observation, as do benzodiazepines, but at a much lower level. Cocaine goes through two periods of increase from 2000 to 2006 and, after a decline, again from 2015 to 2019. In fact, cocaine is the leading implicated drug in medical deaths from 1999 to 2008. Afterwards, opioids are the leading implicated drug. However, this predominance only lasts until 2014, after which psychostimulants are the leading implicated drug. Psychostimulants are low through 2008, after which they increase dramatically. Cannabis is rarely implicated in medical deaths. The bottom panel breaks down opioid categories. Natural and semi-synthetic opioids (e.g. oxycodone, hydrocodone, morphine, codeine) are the leading implicated opioids in medical deaths across the entire period, generally increasing but with some fluctuations. Heroin and especially non-methadone synthetic opioids (e.g. fentanyl, tramadol) increase in recent years, but have not approached natural and semi-synthetic opioids.
Figure 5:
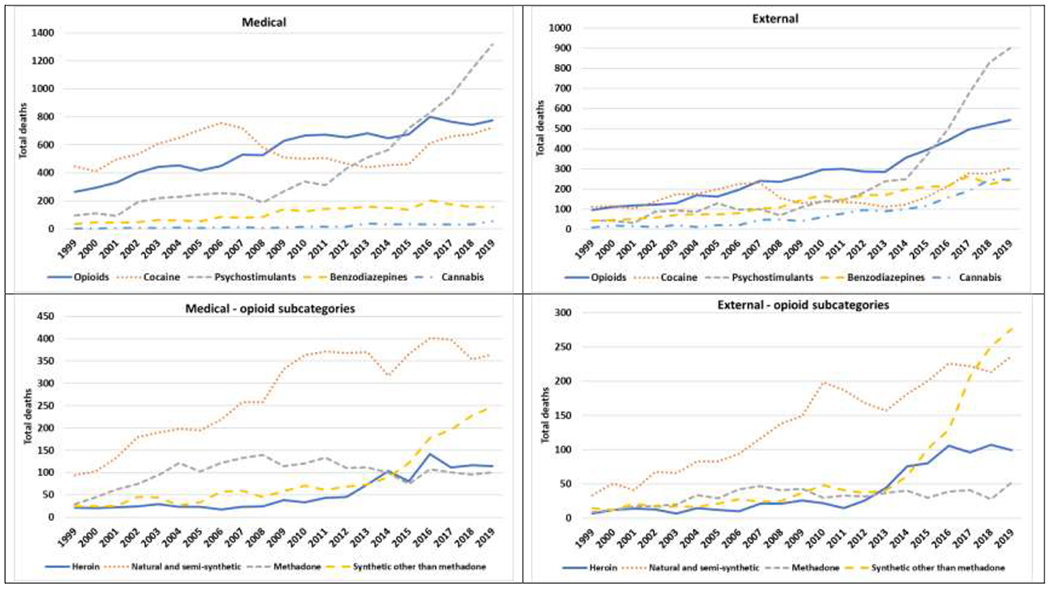
Psychotropic-drug-implicated deaths by substance implicated, by drug class (top) and opioid type (bottom)
Note: As noted by the CDC, the percentage of drug overdose deaths that identified the specific drugs involved varied by year, ranging from 75%-79% from 1999 through 2013 and increasing from 81% in 2014 to 94% in 2019 (Hedegaard, et al., 2020). See Appendix C for additional information on unidentified substances.
The right panels of Figure 5 show analogous results by substance for psychotropic-drug-implicated external causes of death. In the top panel, all drug classes are relatively low in terms of number of external deaths through 2007, but with increasing trends in cocaine, opioids, and benzodiazepines. But as cocaine decreases after 2007, opioids become the leading implicated drug until 2015. As with medical causes, psychostimulants increase markedly and then outpace the other drugs. Considering opioids specifically, similar to medical causes, natural and semi-synthetic opioids are the most implicated opioid in almost all years. Unlike medical causes, the increase in heroin and synthetic opioids is more substantial, with the latter becoming the predominant opioid implicated in external deaths in 2018. Also, unlike medical causes, psychotropic-drug-implicated deaths for cannabis increased steadily since 2006, such that the number of cannabis-implicated deaths are similar to cocaine and benzodiazepines by 2018.
We further place the role of psychotropic-drug-implicated deaths among specific implicated substances in context in Table 2 by considering the proportion of all deaths by substance. For cocaine, psychostimulants, benzodiazepines, and opioids from 1999 to 2019, about 1 in 10, 7, 24, and 29 deaths, respectively were psychotropic-drug-implicated rather than poisonings (i.e. overdoses). Although cannabis-implicated deaths are much rarer, about 1 in 4 were psychotropic-drug-implicated. From 1999 to 2019, these numbers are similar and even decreased somewhat among some substances as overdoses rose dramatically. Nonetheless, these frequencies demonstrate that a substantial proportion of all deaths where particular drugs were implicated were attributable to a cause other than overdose.
Table 2:
Psychotropic-drug-induced deaths relative to all deaths within ICD-10 multiple cause of death categories for select psychotropic drugs
| All years 1999-2019 | 1999 | 2019 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| All deaths | Psychotropic-drug-implicated are about 1 in X deaths | All deaths | Psychotropic-drug-implicated are about 1 in X deaths | All deaths | Psychotropic-drug-implicated are about 1 in X deaths | |
|
|
|
|
||||
| Cocaine | 157,928 | 10 | 4,494 | 8 | 16,912 | 16 |
| Psychostimulants | 94,161 | 7 | 700 | 5 | 18,386 | 8 |
| Benzodiazepines | 124,439 | 24 | 1,219 | 16 | 10,111 | 25 |
| Cannabis | 7,268 | 4 | 49 | 4 | 1,101 | 4 |
| Opioids | 515,285 | 29 | 8,647 | 24 | 51,178 | 39 |
| Heroin | 132,347 | 67 | 2,103 | 75 | 14,233 | 67 |
| Natural and semi-synthetic | 195,986 | 22 | 2,915 | 23 | 12,487 | 21 |
| Methadone | 75,968 | 27 | 831 | 21 | 2,893 | 19 |
| Synthetic other than methadone | 164,154 | 51 | 772 | 20 | 36,883 | 70 |
Note: “All deaths” column includes all deaths where substance was listed as a multiple cause of death regardless of underlying cause. As noted by the CDC, the percentage of drug overdose deaths that identified the specific drugs involved varied by year, ranging from 75%-79% from 1999 through 2013 and increasing from 81% in 2014 to 94% in 2019 (Hedegaard, et al., 2020). See Appendix C for additional information on unidentified substances.
4.0. DISCUSSION
It is well recognized that overdose has contributed greatly to early mortality in the U.S. during the 21st century (Birnhaum et al. 2011; Case and Deaton 2014; Dowell et al. 2017; Ho 2017; Imtiaz et al. 2018; Jalal et al. 2018). In this article, we focused on psychotropic-drug-implicated mortality, which includes deaths where a psychotropic drug was listed as a contributing (not underlying) cause of death. We contend that this permits a broader picture of the toll of the drug mortality crisis not captured by overdose. We find that psychotropic-drug-implicated deaths increased dramatically over the period when drug overdoses increased and have progressively contributed to higher death rates related to drugs in recent years. Opioids had only a short period of predominance as the implicated drug from about 2008 to 2014, preceded largely by cocaine, which coincides with the peak in pharmaceutical opioid use and misuse in the U.S. (Ciccarone 2019). Increasing implementation of policies designed to curb pharmaceutical opioid abuse may have contributed to more recent receding trends. The rise in psychostimulants (such as methamphetamine and prescription stimulants) to predominate psychotropic-drug-implicated deaths in recent years is striking and contrasts with the rise in overdose deaths driven over the same period by considerable increases in overdoses due to opioids such as heroin and fentanyl (Ciccarone 2019). This trend in psychostimulant-implicated deaths runs parallel to large increases in methamphetamine border seizures in recent years (U.S. Department of Justice 2021). Even examining the opioid-specific psychotropic-drug-implicated deaths, natural and semi-synthetic opioids remain predominant, although synthetics have made gains for external causes of death in recent years. Further, examining only overdoses overlooks the contribution of cannabis to other causes of mortality. Although contributing little to medical deaths, there has been a steady rise in cannabis-implicated external causes across the years in which cannabis policy changes occurred. Collectively, these differences point to psychotropic-drug-implicated deaths as worthy of further study in their own right, beyond the overdose crisis. Further, they highlight how clinical practice and public health policy must be reoriented to connect people who use drugs, who disproportionately lack access to healthcare and may be at greater risk of cardiovascular disease and external causes of death, to appropriate medical and treatment professionals.
Many increasing trends for psychotropic-drug-implicated categories of death run counter to overall declines in those same causes. For medical causes, the overwhelming majority of psychotropic-drug-implicated deaths were diseases of the circulatory system, increasing considerably over this period and becoming a greater proportion of deaths in this category. Yet, this increase occurred while circulatory deaths declined overall. Thus, for such causes of death otherwise experiencing mortality improvements, we may have observed even greater progress if not for the wider drug crisis and the growing contribution of drug-implicated deaths. Indeed, while there was a rapid reduction in deaths from diseases of the circulatory system through 2010, there has been a considerable deceleration in that decline since 2011 (Sidney et al. 2016) as psychotropic-drug-implicated deaths escalated. As such deaths become of greater concern as people age through the life course, these deaths cohere with broader patterns of midlife mortality related to drugs (Kelly and Vuolo 2021) stemming from the deleterious effects of chronic use, and efforts should be made to incorporate relevant health promotion efforts alongside those made to address overdose deaths among midlife adults. For many external causes of death, such as transport accidents, other poisonings, and drownings, these countervailing trends are also present. On the other hand, suicide has increased dramatically as drug overdoses increased. The extent to which the overall growth in suicides is attributable to both psychotropic-drug-implicated suicides and intentional drug overdose should be an area of future study. Regardless, psychotropic-drug-implicated deaths constitute a large proportion within external causes, with that proportion increasing considerably.
Given the pharmacological properties and effects of chronic use of certain psychotropic drugs, finding certain psychotropic-drug-implicated deaths, although understudied, is not necessarily surprising. With medical deaths, chronic use of substances contributes to elevated prevalence of systemic disease (Degenhardt and Hall 2012). For example, the risk of cardiac events and death, even in young people, is increased by use of cocaine and prescription psychostimulants (Kaye and Darke 2012; Favrod-Coune and Broers 2010), methamphetamine (Kaye et al. 2007), and opioids (Khodneva et al. 2016). The pharmacological properties and intoxicating effects also increase the risk of external causes of death, including suicide (Bohnert et al. 2017; Homstrand et al. 2015; Wilcox et al. 2004), falls (Neutel et al. 2002; Woolcott et al. 2009), drowning (Pajunen et al. 2017; Vincenzi 2016), and motor vehicle accidents (Dassanayake et al. 2011). Although these relationships are supported in the literature, the burden of these co-occurrences increased considerably according to our results. Further, although overdose liability of cannabis is extraordinarily low, attention to forms of drug-implicated mortality is necessary as access and use expands. Thus, intervention and prevention strategies are needed to curb these trends, although they will need to be tailored to specific causes of death.
There are some limitations and considerations regarding this analysis of psychotropic-drug-implicated mortality. First, the various underlying causes of death are wide-ranging. We do not intend to imply that psychotropic-drug-implicated deaths should be studied in unison. Rather, different research agendas are needed for distinct groups of causes and classes of substances, as prevention, intervention, and policy strategies needed to curb these trends will vary. This analysis was intended as a first step toward highlighting the need for such research, including a better understanding of the contextual factors driving these trends. Even within categories, unique approaches will be needed. For example, different interventions to prevent transport accident fatalities may be required for intoxicated drivers compared to intoxicated pedestrians. We also recognize that some very rare mortality categories are unlikely due to the wider drug use crisis, such as “legal interventions and operations of war.”
Second, scholars have identified that mortality data quality for drug-related causes of death varies across states and this may affect estimates of drug-related mortality (Buchanich et al. 2018). Although conjecture, the numbers here are most likely underestimates, as psychotropic drugs as a contributing cause might be overlooked by coroners and medical examiners when the underlying cause of death is not drug poisoning. As a matter of practice, the results here indicate that coroners and medical examiners should heighten attention to the presence of psychotropic drugs, particularly within categories of mortality where we found common occurrences or increasing trends. Indeed, drug testing as a matter of practice increased across our observation period, which particularly affects counts of deaths by substance (Hedegaard et al. 2020). Further, if a substance is completely unknown, it would get coded as T50.9 (unspecified drugs, medicaments, and biological substances). As Appendix C shows, as testing increased, the number of deaths coded T50.9 decreased substantially. Thus, some psychotropic-drug-implicated deaths were likely included in this category, especially prior to the increase in testing. As not all deaths in this category would qualify as psychotropic-drug-implicated, we do not include it here, but do show in Appendix C how it would affect rates if included, which leads to similar conclusions.
Even with these limitations, this examination of psychotropic-drug-implicated deaths allows for a clearer picture of the toll of the drug mortality crisis beyond individuals lost to drug overdoses specifically. To date, definitions have not included external causes, but should incorporate them, particularly given the proportion of such deaths in which psychotropic drugs are implicated. With medical causes, it is likely that such deaths occur often among individuals not under a specialist’s care or even any healthcare. Rather, contact with the healthcare system for individuals at risk for psychotropic-drug-implicated medical deaths may primarily occur through emergency health professionals. Thus, within a context of disparities in access to healthcare (Wright and Perry 2010), efforts should be made to engage and identify patients whose drug-using behavior may necessitate referral to specialist care to inhibit medical causes of death, such as a cardiologist, as well as interventions for those at high risk for external causes of death. Future research should examine demographic profiles of deaths across underlying cause of death categories to determine those most at risk. We note that the focus on psychotropic-drug-implicated deaths is all the more important given the COVID-19 pandemic. COVID-19 will likely get coded as the underlying cause of death in many cases, even if a psychotropic drug may have been additionally implicated. Given the shared risk factors for COVID-19 and opioid overdose, signals of potential increases in fatal and nonfatal overdoses during the pandemic, and the effect of the pandemic on treatment availability (Haley and Saitz 2020; Ochalek et al. 2020; Slavova et al. 2020; Sun et al. 2020; Wainwright et al. 2020), many deaths where drugs are implicated may go unnoticed according to common definitions. Overall, psychotropic-drug-implicated mortality presents an opportunity for further efforts to improve population health through prevention, intervention, and policy.
HIGHLIGHTS.
Psychotropic-drug-implicated deaths, where psychotropic drugs are contributing but not primary cause, rose dramatically since 1999
Cardiovascular deaths dominate medical causes; suicide, transport accidents, drownings 54% of external causes
Predominant implicated drug evolves from cocaine to opioids to psychostimulants
Drug mortality crisis extends beyond overdose, tempers reductions in other mortality causes
Research on prevention, intervention, and policy for psychotropic-drug-implicated deaths needed
Funding source
This work was funded by the National Institute on Drug Abuse (grant # R21DA046447). The funding agency had no role in the research; the views expressed in this paper do not represent those of the funding agency.
Appendix A: Presumed overdoses with ICD-10 underlying cause of death codes F10-F19
The F-series of ICD-10 codes represents mental and behavioral disorders. Within these codes are a group related to psychotropic substance use (e.g. opioid related disorders; sedative, hypnotic, or anxiolyitic related disorder; cocaine related disorders; other stimulant related disorders). For the period up to 2006, a small portion of deaths were coded within these categories, while also containing the multiple cause of death codes for the substances noted in the main manuscript. Thus, they fit the definition of a psychotropic-drug-implicated death used here because they are a fatality with a non-overdose underlying cause code combined with the proper multiple cause of death code. Such coded deaths are shown in Appendix A Figure. However, as was made clear in CDC coding instruction changes in 2007 (Xu et al. 2010) and reflected in the drop off in Appendix A Figure, these deaths should be coded as drug poisoning and included with psychotropic drug overdoses (and thus not drug-implicated deaths as defined here). As such, we do not include these deaths with the medical causes of death shown in the main manuscript, with the exception of Figure 2 where they are included with the other psychotropic drug overdoses. To our knowledge, these deaths have not been retroactively coded as overdoses, appearing in both restricted data and public data available on CDC WONDER. We also note that these deaths are not due to coding practices in any particular state or county, as they are not geographically confined to a state or county, but rather appear broadly in those years.
Appendix A Figure:
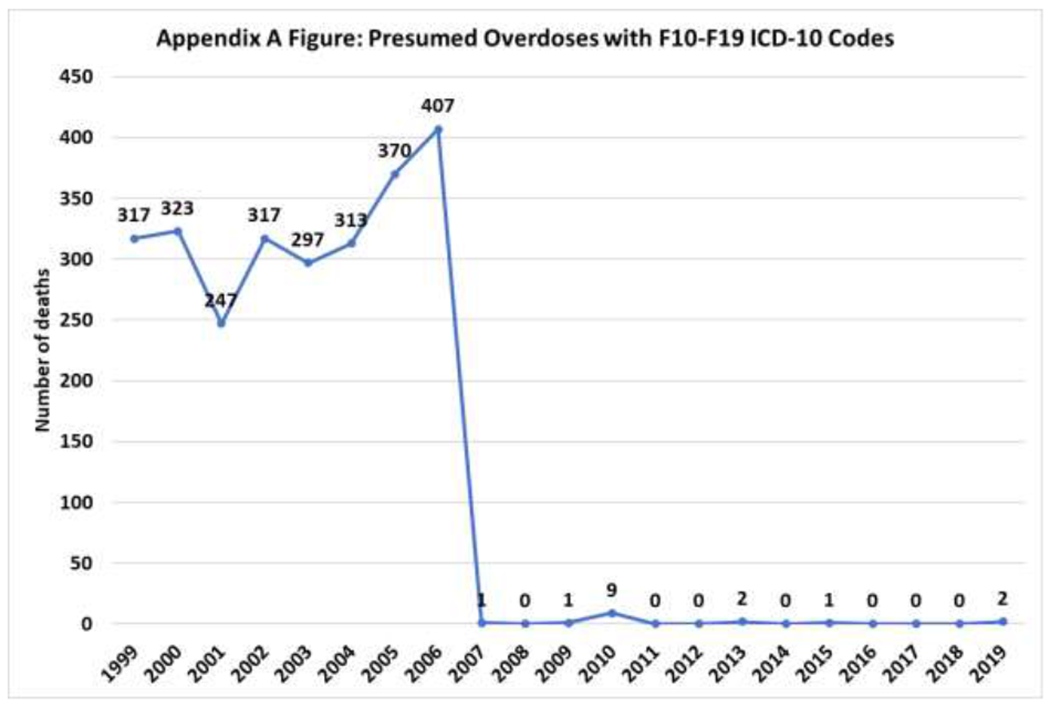
Presumed Overdoses with F10-F19 ICD-10 Codes
Appendix A References
- Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. 2010. Deaths: final data for 2007. Natl Vital Stat Rep. 2010;58(19):1–136. [PubMed] [Google Scholar]
Appendix B: ICD-10 underlying cause of death codes
| Description | Codes |
|---|---|
| Medical | |
| Certain infectious and parasitic diseases | A00–B99 |
| Neoplasms | C00–D48 |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | D50–D89 |
| Endocrine, nutritional and metabolic diseases | E00–E90 |
| Mental and behavioral disorders, unrelated to drugs | F00-F09; F20-F99 |
| Diseases of the nervous system | G00–G99 |
| Diseases of the eye and adnexa | H00–H59 |
| Diseases of the ear and mastoid process | H60–H95 |
| Diseases of the circulatory system | I00–I99 |
| Diseases of the respiratory system | J00–J99 |
| Diseases of the digestive system | K00–K93 |
| Diseases of the skin and subcutaneous tissue | L00–L99 |
| Diseases of the musculoskeletal system and connective tissue | M00–M99 |
| Diseases of the genitourinary system | N00–N99 |
| Pregnancy, childbirth and the puerperium | O00–O99 |
| Certain conditions originating in the perinatal period | P00–P96 |
| Congenital malformations, deformations and chromosomal abnormalities | Q00–Q99 |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | R00–R99 |
| External | |
| Transport accidents | V01–V99 |
| Falls | W00-W19 |
| Exposure to inanimate or animate mechanical forces | W20-W64 |
| Accidental drowning and submersion | W65-W74 |
| Other accidental threats to breathing | W75-W84 |
| Exposure to smoke, fire, hot substances, non-natural heat & cold, electricity, radiation | W85-W99; X00-X19 |
| Contact with venomous animals and plants | X20-X29 |
| Exposure to forces of nature | X30-X39 |
| Accidental poisoning by and exposure to alcohol | X45 |
| Accidental poisoning by non-drug or alcohol | X46-X49 |
| Overexertion, travel and privation | X50-X57 |
| Accidental exposure to other and unspecified factors | X58-X59 |
| Intentional self-poisoning by and exposure to alcohol | X65 |
| Intentional self-poisoning by non-drug or alcohol | X66-X69 |
| Intentional self-harm, non-poisoning | X70-X84 |
| Assault non-drug | X86-Y09 |
| Event of undetermined intent non-drug | Y15-Y34 |
| Legal intervention and operations of war | Y35-Y36 |
| Complications of medical and surgical care | Y40-Y84 |
| Sequelae of external causes of morbidity and mortality | Y85-Y89 |
| Supplementary factors related to causes of morbidity and mortality classified elsewhere | Y90-Y98 |
| Presumed Overdoses | |
| Mental and behavioral disorders, drug-related | F10-F19 |
Appendix C: Select figures with ICD-10 code T50.9 (unspecified drugs, medicaments and biological substances) included
Appendix Figure C.1:
Percentage of psychotropic-drug-implicated deaths coded T50.9 if T50.9 is included
Appendix Figure C.2:
Psychotropic-drug-implicated age-adjusted death rate per 100,000 (lines) and number of deaths (table) by year, total and by type with ICD-10 code T50.9 included
Note: Psychotropic-drug-implicated deaths defined as those with multiple cause of death ICD-10 codes T40, T42, T43, and T50.9, but not an underlying cause of death of drug overdose (X40-X44, X60-X64, X85, and Y10-Y14). For underlying cause of death ICD-10 codes defined as medical and external, see Appendix B.
Appendix Figure C.3:
Death rate per 100,000 for psychotropic drug overdose as underlying cause of death and with psychotropic-drug-implicated deaths included with ICD-10 code T50.9 included
Note: Bottom line includes psychotropic drug poisonings only (i.e. underlying cause of death X40-X44, X60-X64, X85, Y10-14, or F10-F19, and a multiple cause of death code T40, T42, T43, or T50.9). Top line includes all deaths with multiple cause of death code T40, T42, T43, or T50.9 regardless of underlying cause.
Appendix D: Figures with low cell counts as crude death rate per 100,000 instead of counts
Appendix Figure D.1:
Psychotropic-drug-implicated crude death rate by year and common underlying causes of death (those with more than 1000 across all years)
Note: The CDC considers rates computed from less than 20 deaths to be unreliable.
Appendix Figure D.2:
Psychotropic-drug-implicated crude death rate per 100,000 by substance implicated, by drug class (top) and opioid type (bottom)
Note: As noted by the CDC, the percentage of drug overdose deaths that identified the specific drugs involved varied by year, ranging from 75%–79% from 1999 through 2013 and increasing from 81% in 2014 to 94% in 2019 (Hedegaard, et al., 2020). See Appendix C for additional information on unidentified substances.
Note: The CDC considers rates computed from less than 20 deaths to be unreliable.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None declared.
REFERENCES
- Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016;106(4):686–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–667. [DOI] [PubMed] [Google Scholar]
- Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017; 112(7):1193–1201. [DOI] [PubMed] [Google Scholar]
- Buchanich JM, Balmert LC, Williams KE, Burke DS. The effect of incomplete death certificates on estimates of unintentional opioid-related overdose deaths in the United States, 1999-2015. Public Health Rep. 2018;133(4):423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns E, Kakara R. Deaths from falls among persons aged ≥65 years—United States, 2007–2016. Morb Mortal Wkly Rep. 2018;67(18):509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci. 2014;112(49):15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin SC. Trends in cancer and heart disease death rates among adults aged 45-64: United States, 1999-2017. Natl Vital Stat Rep. 2019;68(5):1–8. [PubMed] [Google Scholar]
- Dassanayake T, Michie P, Carter G, Jones A. Effects of benzodiazepines, antidepressants and opioids on driving. Drug Saf. 2011;34(2):125–156. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70. [DOI] [PubMed] [Google Scholar]
- Dowell D, Arias E, Kochanek K, et al. Contribution of opioid-involved poisoning to the change in life expectancy in the United States, 2000-2015. JAMA. 2017;318(11):1065–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favrod-Coune T, Broers B. The health effect of psychostimulants: a literature review. Pharmaceuticals. 2010;3(7):2333–2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley DF, Saitz R. The Opioid Epidemic During the COVID-19 Pandemic. JAMA. 2020;324(16):1615–1617. [DOI] [PubMed] [Google Scholar]
- Hampson NB. US mortality due to carbon monoxide poisoning, 1999–2014. Accidental and intentional deaths. Ann Am Thorac Soc. 2016; 13( 10):1768–1774. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Chen LH, Warner M. Drug-poisoning deaths involving heroin: United States, 2000-2013 (NCHS Data Brief, No. 190). Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2015. [Google Scholar]
- Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2019 (NCHS Data Brief, No. 394). Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2020. [Google Scholar]
- Ho JY. 2017. The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992–2011 .Demography. 2017;54(3):1175–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imtiaz A, Probst C, Rehm J. 2018. Substance use and population life expectancy in the USA: interactions with health inequalities and implications for policy. Drug Alcohol Rev. 2018;37(S1):S263–S267. [DOI] [PubMed] [Google Scholar]
- Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361(6408):eaau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users—United States, 2002–2013 .Morb Mortal Wkly Rep. 2015;64(26):719–725. [PMC free article] [PubMed] [Google Scholar]
- Kaye S, Darke S. The diversion and misuse of pharmaceutical stimulants: what do we know and why should we care? Addiction. 2012;107(3):467–477. [DOI] [PubMed] [Google Scholar]
- Kaye S, McKetin R, Duflou J, Darke S. Methamphetamine and cardiovascular pathology: a review of the evidence. Addiction. 2007;102(8):1204–1211. [DOI] [PubMed] [Google Scholar]
- Kelly BC, Vuolo M. Developing explanatory models for life course shifts in the burden of substance use to inform future policy and practice. Int J Drug Policy. 2021; Online early. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khodneva Y, Muntner P, Kertesz S, Kissela B, Safford MM. Prescription opioid use and risk of coronary heart disease, stroke, and cardiovascular death among adults from a prospective cohort (REGARDS Study). Pain Med. 20161;17(3):444–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stata Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep. 2019;68(9):1–76. [PubMed] [Google Scholar]
- National Cancer Institute. Joinpoint regression program, Version 4.9.0.0, March 2021. Washington DC: Statistical Research and Applications Branch, National Cancer Institute; 2021 [Google Scholar]
- CI Neutel, Perry S, Maxwell C. Medication use and risk of falls. Pharmacoepidemiol Drug Saf. 2002;11(2):97–104. [DOI] [PubMed] [Google Scholar]
- Ochalek TA, Cumpston KL, Wills BK, Gal TS, Moeller FG. Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA. 2020;324(16):1673–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajunen T, Vuori E, Vincenzi FF, Lillsunde P, Smith G, Lunetta P. Unintentional drowning: role of medicinal drugs and alcohol. BMC public health. 2017;17(1):388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson AB, Kegler SR. Deaths from fall-related traumatic brain injury—United States, 2008–2017. Morb Mortal Wkly Rep. 2020;69(9):225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen LM, Hedegaard H, Khan D, Warner M. County-level trends in suicide rates in the US, 2005–2015. Am J Prev Med. 2018;55(1):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. Morb Mortal Wkly Rep. 2016;64(50-51): 1378–1382. [DOI] [PubMed] [Google Scholar]
- Sauber-Schatz EK, Ederer DJ, Dellinger AM, Baldwin GT. Vital signs: motor vehicle injury prevention—United States and 19 comparison countries. Morb Mortal Wkly Rep. 2016;65(26):672–677. [DOI] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths— United States, 2013–2017.Morb Mortal Wkly Rep. 2019;67(51-52): 1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidney S, Quesenberry CP, Jaffe MG, et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;l(5):594–599. [DOI] [PubMed] [Google Scholar]
- Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214:108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Bao Y, Kosten T, Strang J, Shi J, Lu L. Challenges to opioid use disorders during COVID-19. Am J Addict. 2020;29(3):174–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umapathi KK, Thavamani A, Dhanpalreddy H, Khatana J, Roy A. Incidence trends and predictors of in-hospital mortality in drowning in children and adolescents in the United States: a national inpatient database analysis. Clin Pediatr. 2020;59(2):134–141. [DOI] [PubMed] [Google Scholar]
- Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin-and opioid-related overdoses, 1993–2009. PloS One. 2013;8(2):e54496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Justice. 2020 Drug Enforcement Administration National Drug Threat Assessment. Washington, DC: U.S. Department of Justice, Drug Enforcement Administration; 2021. [Google Scholar]
- Vincenzi FF. Drug-induced long QT syndrome increases the risk of drowning. Med Hypotheses. 2016;87:11–13. [DOI] [PubMed] [Google Scholar]
- Wainwright JJ, Mikre M, Whitley P, et al. Analysis of drug test results before and after the US declaration of a national emergency concerning the COVID-19 outbreak. JAMA. 2020;324(16):1674–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weast R Temporal factors in motor-vehicle crash deaths: ten years later. J Safety Res. 2018;65:125–131. [DOI] [PubMed] [Google Scholar]
- White AM, Castle IJ, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol- related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1): 178–187. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–S19. [DOI] [PubMed] [Google Scholar]
- Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, Marra CA. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–1960. [DOI] [PubMed] [Google Scholar]
- Wright ER, Perry BL. 2010. Medical sociology and health services research: past accomplishments and future policy challenges. J Health Soc Behav. 2010;51:S107–S119. [DOI] [PubMed] [Google Scholar]


