Abstract
Background:
This pilot study aimed to test whether increase in daily steps and day-to-day consistency in daily steps during the first several weeks of a physical activity intervention predicted outcomes.
Methods:
This was a secondary analysis from two concurrent studies testing a positive psychology-motivational interviewing intervention to increase physical activity and positive affect in individuals with type 2 diabetes. Steps were measured with accelerometers at study assessments (baseline, end-of-treatment, and 8-week follow-up), and were measured daily throughout the intervention by participants using provided pedometers. We calculated change in steps from intervention week 1 to week 3, along with variability in daily steps over the first 3 weeks, using the best fitting regression line modeling their change. Multiple regression analyses tested whether these predictors were associated with change in physical activity at the end of treatment and at 8-week follow-up. Additionally, we explored the utility of specific cutoffs (e.g., 500 steps) for early step change using a minimum p-value approach.
Results:
In 52 participants, larger step increases by week 3 predicted activity increase at end-of-treatment and follow-up. Variability in early steps was not associated with outcomes. Early increase cutoffs of 500 and 2000 steps may have practical relevance.
Conclusions:
Early response to a physical activity intervention appears to be a useful predictor of outcome and could be used to identify those unlikely to succeed in a given intervention early in treatment.
Keywords: Physical activity, type 2 diabetes, behavioral intervention, positive psychology
Introduction
Type 2 diabetes (T2D) is the 7th leading cause of death in the United States [1], and greatly increases risk of cardiovascular disease [2]. Physical activity can reduce the risk of complications and improve overall health for people with T2D [3]; however, most people with T2D do not meet recommended levels of physical activity [4]. While behavioral interventions to improve physical activity have been successful [5], there is wide variability in response to these types of treatment. Better understanding who is likely to succeed with a given treatment early on would allow for provision of additional support for those unlikely to do well.
Across many types of behavioral and psychological treatments, early improvement has been shown to be a strong predictor of outcome at end of treatment (EOT) and beyond [6, 7]. This is the case with behavioral weight loss, as evidenced by a recent review showing that those who do not achieve beyond some cutoff of initial weight loss in the first 1–2 months of treatment (typically ranging from 0.5% to 3% weight loss) have lower post-treatment and long-term weight loss success [7]. The predictive value of weight loss in the first month of treatment has been shown to hold up to 8 years later in a sample of 2290 individuals with T2D from the Look AHEAD study [8]. Similar patterns have been found in psychological treatments for depression and anxiety, where early symptom reduction is one of the strongest predictors of treatment success [6]. To our knowledge, the predictive value of early response to a physical activity intervention has never been studied.
Variability in daily physical activity level early in an intervention may also be a relevant predictor of treatment outcomes. Variability in body weight early on during a weight loss attempt has predicted less weight loss or more weight gain 1–2 years later [9–11]. Regarding physical activity, current recommendations do not provide information about whether the same benefits are gained from being active every day compared to engaging in higher amounts of activity more intermittently [12]. Measuring whether day-to-day variability in activity during the first weeks of treatment is associated with physical activity levels later on could help to answer this question.
The present study was a secondary analysis of a behavioral/psychological intervention to increase physical activity in patients with T2D that examined whether patterns of daily steps during the first 3 weeks of treatment were associated with steps and moderate-to-vigorous physical activity (MVPA) at EOT and 8-week follow-up. We hypothesized that a larger increase in steps over the first 3 weeks would predict higher physical activity increases at EOT and follow-up, and that less variability in daily steps in the first 3 weeks, independent of overall change during that time period, would also predict higher physical activity increases. We also explored cutoffs for early step increase that best predicted steps and MVPA at EOT and follow-up.
Methods
The BEHOLD Studies
The BEHOLD studies were two concurrent randomized controlled trials of a positive psychology-motivational interviewing (PP-MI) intervention designed to increase positive affect and physical activity in adults with T2D [13]. The hospital system’s institutional review board approved both studies. BEHOLD-8 tested an 8-week PP-MI intervention compared to a motivational interviewing health behavior change control, and BEHOLD-16 tested a 16-week PP-MI intervention compared to a diabetes health behavior education control condition. The two PP-MI interventions had almost identical content, with BEHOLD-16 including several additional topics. Both interventions, as well as the controls, were delivered via weekly 30-minute telephone calls with PhD-level clinical psychologists or psychiatrists in addition to a printed study manual. Each weekly session consisted of 15 minutes discussing a positive psychology exercise and 15 minutes discussing physical activity using a motivational interviewing framework. Assessments were conducted at baseline, EOT (8 weeks in BEHOLD-8, 16 weeks in BEHOLD-16), and 8-week follow-up (16 weeks in BEHOLD-8, 24 weeks in BEHOLD-16). The primary outcomes of the studies were feasibility and acceptability of the intervention, and the main secondary outcome was change in physical activity, measured via accelerometer.
Intervention content
The PP-MI intervention was designed to increase physical activity via traditional motivational interviewing-based and goal-setting approaches, and by promoting psychological well-being, based on research showing that greater psychological well-being is associated with greater health behavior engagement, independent of the negative effects of depression [14]. The positive psychology intervention component was divided into modules (gratitude, personal strengths, and meaning). Each week participants completed one positive psychology activity (e.g., writing a letter of gratitude, identifying a personal strength and using it in a new way) and noted the positive emotions they experienced. The motivational interviewing portion of the intervention included goal-setting to increase physical activity, identifying and problem-solving barriers to being active, and using neighborhood, equipment, and social resources for being active. Participants were encouraged to track their physical activity using a provided pedometer, and they reported daily steps to their study interventionist each week. Throughout the intervention, interventionists encouraged participants to notice links between the positive emotions they were cultivating and their drive to increase physical activity. See Supplementary Table 1 for detail on all sessions.
Participants
Participants were adults (age 18+) with a diagnosis of T2D (hemoglobin A1c [A1C] ≥ 6.5% and/or fasting glucose ≥ 126 mg/dl) confirmed by their diabetes clinician and/or medical record review, and low physical activity, defined as ≤ 150 minutes/week of self-reported MVPA on the International Physical Activity Questionnaire [15], consistent with the American Diabetes Association physical activity recommendations [12]. Exclusion criteria were (1) cognitive impairment assessed via a 6-item screen developed to measure cognitive capacity to participate in clinical research studies [16], (2) lack of telephone access, (3) inability to read and write in English, (4) medical conditions that impede physical activity (e.g., severe arthritis), and (5) current participation in another mind-body program, lifestyle intervention (e.g., cardiac rehabilitation), or other clinical trials. Only PP-MI participants with step data in week 1 and week 3 were included in the present study.
Procedures
Recruitment used the hospital’s electronic medical record data registry to identify potentially eligible patients with confirmation of eligibility by the outpatient provider. Opt out letters were mailed to these patients, followed by a phone call from study staff describing the study. Those interested attended an in-person visit to complete written informed consent. After enrollment, they were given a waist-worn Actigraph GT3X+ accelerometer (Actigraph, Pensacola, FL) to wear for 7 days. They then returned for their in-person baseline visit at which time accelerometer data were checked for completeness and they were randomly assigned to PP-MI or control. Accelerometers were also worn at EOT and 8-week follow-up.
Predictor and Outcome Variables
Early step change
Early step change was calculated as the difference between average pedometer-measured steps in intervention week 1 and week 3. In week 1, participants were asked to start monitoring their current level of activity but not to make changes yet. In week 2 and beyond they were encouraged to start setting goals to increase, based on activity level the prior week. This time window was chosen to give participants a chance to start making changes but still remain in the early part of the total intervention.
Early step variability
Early step variability was calculated using daily step counts from weeks 1–3. The maximum number of days reported was 21, although some participants did not track their steps on all days (the average was 19 days of pedometer wear). In these cases, the model appropriately spaced recorded step counts. Growth curve analysis modeled step change trajectories over the first 3 weeks of treatment. Daily step variability was calculated as the root mean square error (RMSE) of daily steps around the best fitting linear regression line for reported steps. Sample participants with low and high step variability are shown in Figure 1.
Figure 1.
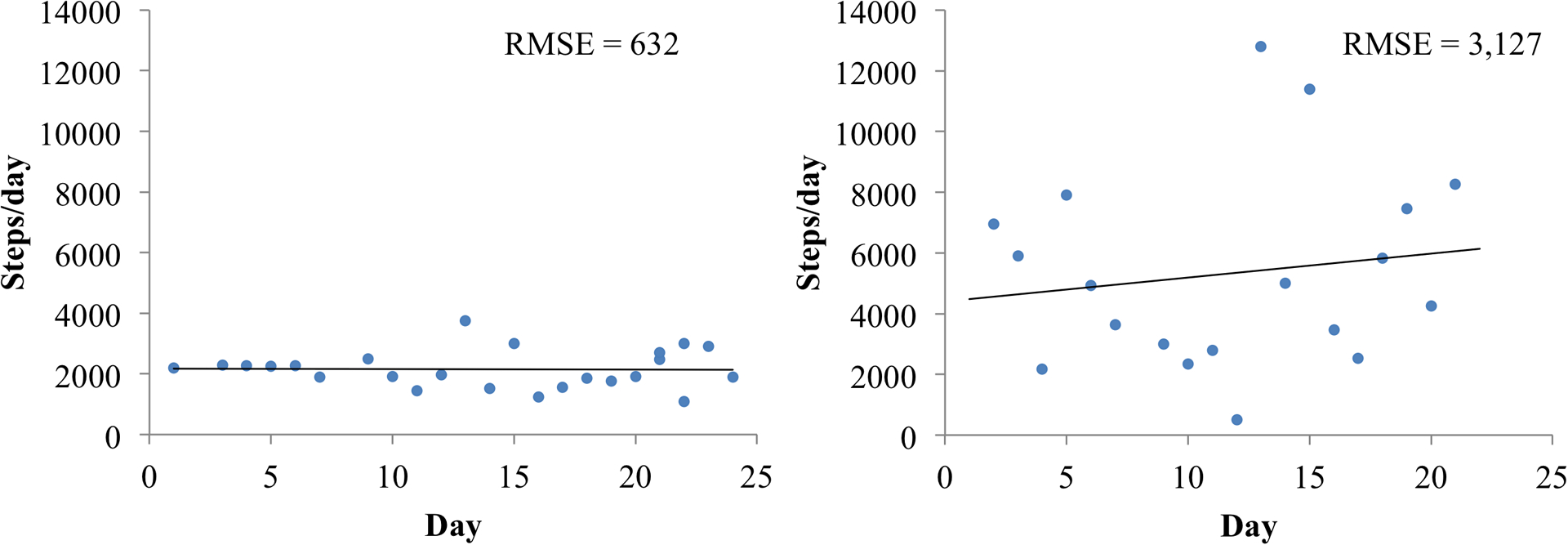
Example participants with a low (left) and high (right) daily step variability. RMSE = root mean square error.
MVPA and steps
MVPA and steps were measured as outcome variables based on accelerometer data collected at baseline, EOT, and 8-week follow-up. Participants were required to have 4+ days of 8 hours of wear time for the accelerometer data to be considered valid and MVPA was defined as at least 1952 counts/minute [17].
Analysis Plan
The relationships between (a) early step change and (b) accelerometer-measured steps and MVPA at EOT and 8-week follow-up were tested with linear regression analyses controlling for baseline accelerometer-measured steps or MVPA and study length. The relationships between (a) early step variability and (b) steps and MVPA at EOT and 8-week follow-up were also tested with linear regression, controlling for baseline accelerometer-measured steps or MVPA, the slope of change in steps over the first 3 weeks, and study length. Effect sizes were estimated as the change in R2 when adding the predictor to the model. A minimum p-value approach was used to explore specific cutoffs for early change in steps [18]. This approach tests several cutoffs for step increase from week 1 to 3 and compares the p-value of each regression to identify which cutoff most strongly predicted later activity change in this sample. The chosen cutoffs were then further described by comparing step trajectories for each group.
Results
Descriptive information about the sample (N = 52) can be found in Table 1. Thirteen participants were excluded due to missing pedometer data in weeks 1 and 3. This group did not differ from included participants in age, gender, or baseline activity, but was more racially diverse (p = 0.047; 54% vs. 79% white). On average, steps increased by 779 steps in the first 3 weeks of treatment, by 1400 steps at EOT, and by 573 steps from baseline to 8-week follow-up.
Table 1.
Summary statistics.
| Variable | Mean (SD) or N (%) | ||
|---|---|---|---|
| Baseline (N=52) | End-of-treatment (N=48) | 8-week follow-up (N=43) | |
| Age | 65.3 (10.0) | ||
| Female | 28 (53.9%) | ||
| Non Hispanic White | 41 (78.9%) | ||
| BMI | 31.1 (5.5) | ||
| A1C | 7.2 (1.0) | ||
| Average steps/day | 4474.8 (1805.0) | 5874.9 (2903.8) | 5047.7 (2949.9) |
| MVPAa minutes/day | 11.8 (10.3) | 20.9 (21.7) | 17.4 (20.4) |
| Step variability | 1923.4 (707.0) | ||
| Week 1–3 step change | 778.8 (1582.4) | ||
MVPA = moderate to vigorous physical activity.
Change in mean steps from week 1–3 was positively associated with steps and MVPA at EOT (steps: b = 0.82, SEb = 0.20, p < 0.001, R2 Δ = 0.19; MVPA: b = 0.01, SEb = 0.00, p < 0.001, R2 Δ = 0.22) and at 8-week follow-up (steps: b = 0.77, SEb = 0.23, p = 0.001, R2 Δ = 0.17; MVPA: b = 0.01, SEb = 0.00, p = 0.002, R2 Δ = 0.18), controlling for baseline physical activity and study length. Step variability over the first 3 weeks, in contrast, was not significantly associated with steps or MVPA at EOT (steps: b = 1.03, SEb = 0.52, p = 0.053, R2 Δ = 0.05; MVPA: b = 0.01, SEb = 0.00, p = 0.135, R2 Δ = 0.03) or 8-week follow-up (steps: b = 0.53, SEb = 0.61, p = 0.380, R2 Δ = 0.01; MVPA: b = 0.01, SEb = 0.00, p = 0.129, R2 Δ = 0.04), controlling for baseline physical activity, study length, and slope of step change from week 1–3.
Results from the early step cutoff analyses are shown in Table 2. Step increase cutoffs between 0 and 2000 steps were tested. The cutoff of 500 steps had a small p-value for EOT steps and a larger but still significant p-value for 8-week follow-up step change. P-values for this cutoff approached, but did not reach significance for MVPA outcomes. Only 7 participants reached the larger 2000 step cutoff, but they demonstrated a large comparative improvement in steps at EOT and follow-up compared to those who did not reach the early 2000-step cutoff for both steps and MVPA. Accelerometer-measured step trajectories for participants above and below each chosen cutoff are shown in Fig. 2.
Table 2.
Results from exploratory tests of different cutoffs for early step increase as predictors of change in accelerometer-measured steps and MVPA at end-of-treatment and follow-up, controlling for study length.
| Accelerometer-measured steps as outcome | ||||||
|---|---|---|---|---|---|---|
| End-of-treatment | Follow-up | |||||
| Week 1–3 average step change cutoff | N above | N below | b | P | b | p |
| 0 | 37 | 15 | 1667.42 | 0.040 | 700.55 | 0.436 |
| 500 | 29 | 23 | 1830.90 | 0.010 | 1583.88 | 0.046 |
| 750 | 25 | 27 | 1937.23 | 0.007 | 1503.01 | 0.063 |
| 1000 | 22 | 30 | 1929.05 | 0.007 | 1488.29 | 0.066 |
| 1500 | 12 | 40 | 957.62 | 0.245 | 1480.30 | 0.101 |
| 2000 | 7 | 45 | 2389.53 | 0.020 | 3043.92 | 0.008 |
| Accelerometer-measured MVPA as outcome | ||||||
| End-of-treatment | Follow-up | |||||
| Week 1–3 average step change cutoff | N above | N below | b | P | b | p |
| 0 | 37 | 15 | 6.88 | 0.284 | 3.59 | 0.582 |
| 500 | 29 | 23 | 11.16 | 0.051 | 9.98 | 0.086 |
| 750 | 25 | 27 | 11.30 | 0.052 | 7.73 | 0.192 |
| 1000 | 22 | 30 | 13.68 | 0.017 | 10.00 | 0.093 |
| 1500 | 12 | 40 | 12.69 | 0.052 | 12.42 | 0.060 |
| 2000 | 7 | 45 | 26.65 | 0.001 | 22.60 | 0.007 |
MVPA = moderate-to-vigorous physical activity.
Figure 2.
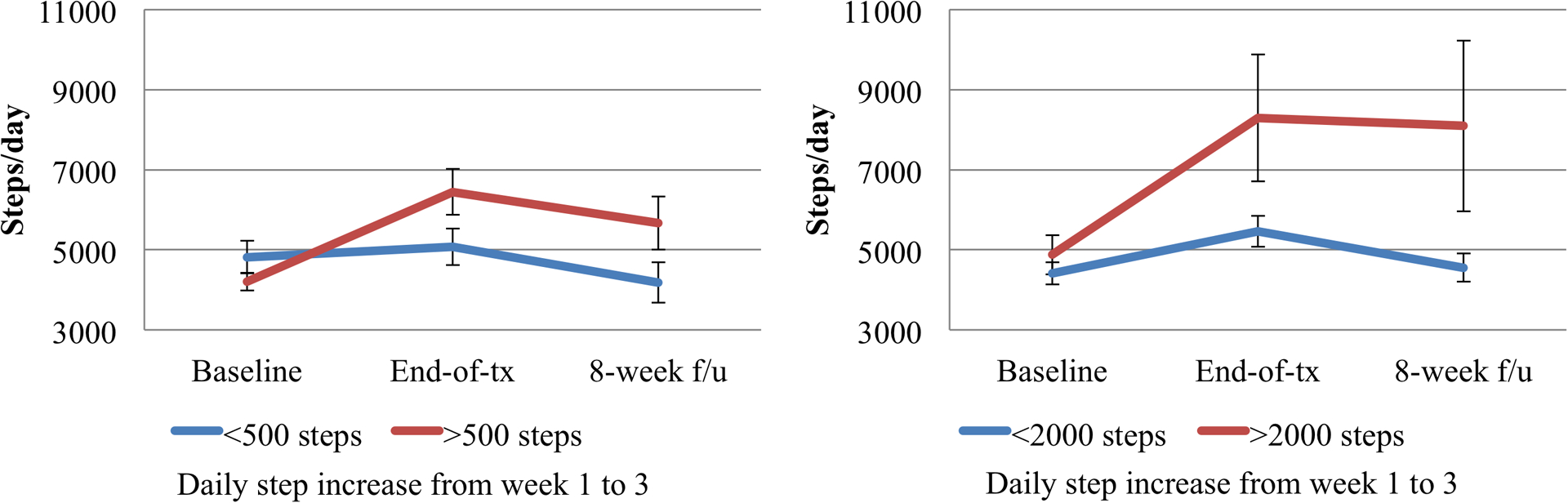
Mean (standard error) accelerometer-measured steps per day by early step increase cutoffs.
Discussion
Assessing early response to physical activity interventions is important, as an ability to rapidly assess whether a specific treatment is going to be helpful can allow for transition to alternative approaches that may better fit participants’ preferences and needs. This secondary analysis aimed to examine whether patterns of daily steps during the first 3 weeks of a PP-MI intervention to increase physical activity were associated with steps and MVPA at EOT and 8-week follow-up. As hypothesized based on research on early response to other types of treatment [6, 7], a larger step increase over the first 3 treatment weeks predicted a larger improvement in physical activity at EOT and follow-up. For each 100 daily step increase by week 3, EOT daily steps increased by an additional 82 steps and 8-week follow-up daily steps increased by an additional 77 steps. Change in steps by week 3 explained between 17 and 22% of the variance in step or MVPA change at EOT or follow-up.
Contrary to hypotheses, daily step variability during the first 3 weeks of the intervention was not associated with outcomes, with small effect sizes. While prior research tracking variability in weight during weight loss has suggested importance in early consistent weight loss for long-term outcomes [9, 10], the present study differed in that the variable of interest was a behavior rather than a physical measurement. The day-to-day pattern of physical activity may matter less than the total amount done over the week. This is encouraging from a clinical perspective, suggesting that flexibility in scheduling physical activity can be promoted.
Further, an exploratory analysis looking for a clinically relevant early step increase cutoff found two potentially meaningful early cutoffs by treatment week 3. The first was a modest 500-step increase, of which 56% of the sample achieved. Increasing by at least 500 steps/day by week 3 was significantly associated with a larger step increase at EOT and 8-week follow-up. As shown in Fig. 1, participants below the cutoff only increased their steps on average by 258/day at EOT, and by 8 weeks later they actually decreased their daily steps on average by 634/day compared to baseline. The 500-step cutoff could inform identification of individuals unlikely to show meaningful improvement via this intervention, who may benefit from rapid transition to a more intensive or alternative approach. A more stringent cutoff of a 2000-step-per-day increase only included 7 participants (13%). However, this small subgroup had a much more drastic relative step and MVPA increase at the EOT and 8 weeks later. This large early increase may signal highly motivated participants who are likely to increase their physical activity significantly and to maintain these changes. Due to the exploratory nature of these analyses and the relatively small sample, these cutoffs should be tested in additional larger samples in order to determine their reliability. If stability is shown, these cutoffs can be used to inform a stepped care approach to physical activity starting with the PP-MI intervention and switching to a more intensive program for those below the early change cutoff.
Strengths of the study include its use of objectively measured MVPA and steps via research-grade accelerometers at assessments and daily step counts throughout the intervention. Limitations include self-report of daily steps (via provided pedometers), modest sample size, combining two interventions of different lengths, a primarily white sample, and exclusion of participants with missing early pedometer data. Longer-term follow-up to assess whether early step change predicted physical activity more than 8 weeks post-intervention was not conducted.
Assessing early response to treatment is critical, as physical activity interventions are not effective for all participants. Wearable activity trackers are affordable with high acceptability [19] and can ease identification of non-responders in real time. Interventions to aid non-responders in increasing physical activity are needed, especially for individuals with T2D for whom physical activity plays a key role in maintaining and improving health. A future stepped care approach could use the validated cutoff to identify participants who either (a) are doing well and should remain in the initial intervention or (b) have not achieved the early step increase cutoff and therefore should be switched to a higher intensity intervention (e.g., more frequent interventionist contact, provision of exercise equipment, adding a social support component).
In conclusion, in a physical activity intervention for individuals with T2D, step increase during the first 3 weeks predicted higher step and MVPA increases at the EOT and follow-up; variability of daily steps early in treatment did not predict step change; and early step increase cutoffs of 500 or 2000 steps/day may best predict improvements during the intervention and follow-up. Once confirmed in larger samples, these findings can help providers determine when extra support or an alternative approach is needed for a participant to successfully increase physical activity. Future research is needed to confirm the step cutoffs proposed in this study, and next step studies could test a stepped care approach using these early cutoffs.
Supplementary Material
Acknowledgements:
Funding for the BEHOLD studies comes from the National Institute of Diabetes and Digestive and Kidney Diseases (R21DK109313, PI: Huffman) and the American Diabetes Association (grant 1-17-ICTS-099, PI: Huffman). Time spent on these analyses was funded by the National Heart Lung and Blood Institute (K23HL123607, PI: Celano; R01HL113272, PI: Huffman; and K23HL148017, PI: Feig).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Trial Registration: ClinicalTrials.gov identifiers NCT03150199 and NCT03001999
Informed consent: Informed consent was obtained from all study participants.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helinski declaration and its later amendments or comparable ethical standards.
References
- 1.Benjamin EJ, Muntner P, Alonso A, et al. (2019) Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 139:e56–e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Huo X, Gao L, Guo L, et al. (2016) Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. lancet Diabetes Endocrinol 4:115–124. doi: 10.1016/S2213-8587(15)00508-2 [DOI] [PubMed] [Google Scholar]
- 3.Blomster JI, Chow CK, Zoungas S, et al. (2013) The influence of physical activity on vascular complications and mortality in patients with type 2 diabetes mellitus. Diabetes Obes Metab 15:1008–1012. doi: 10.1111/dom.12122 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (2020) National diabetes statistics report 2020: estimates of diabetes and its burden in the United States. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 2 Jun 2020
- 5.Plotnikoff RC, Costigan SA, Karunamuni ND, Lubans DR (2013) Community-based physical activity interventions for treatment of type 2 diabetes: a systematic review with meta-analysis. Front Endocrinol (Lausanne) 4:3. doi: 10.3389/fendo.2013.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beard JIL, Delgadillo J (2019) Early response to psychological therapy as a predictor of depression and anxiety treatment outcomes: A systematic review and meta-analysis. Depress Anxiety 36:866–878. doi: 10.1002/da.22931 [DOI] [PubMed] [Google Scholar]
- 7.Unick JL, Pellegrini CA, Demos KE, Dorfman L (2017) Initial Weight Loss Response as an Indicator for Providing Early Rescue Efforts to Improve Long-term Treatment Outcomes. Curr Diab Rep 17:69. doi: 10.1007/s11892-017-0904-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Unick JL, Neiberg RH, Hogan PE, et al. (2015) Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity (Silver Spring) 23:1353–1356. doi: 10.1002/oby.21112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benson L, Zhang F, Espel-Huynh H, et al. (2020) Weight variability during self-monitored weight loss predicts future weight loss outcome. Int J Obes (Lond) 44:1360–1367. doi: 10.1038/s41366-020-0534-6 [DOI] [PubMed] [Google Scholar]
- 10.Feig EH, Lowe MR (2017) Variability in Weight Change Early in Behavioral Weight Loss Treatment: Theoretical and Clinical Implications. Obesity 25:1509–1515. doi: 10.1002/oby.21925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lowe MR, Benson L, Singh S (2020) Individual differences in within-subject weight variability: There’s a signal in the noise. Physiol Behav 226:113112. doi: 10.1016/j.physbeh.2020.113112 [DOI] [PubMed] [Google Scholar]
- 12.Colberg SR, Sigal RJ, Fernhall B, et al. (2010) Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care 33:e147–67. doi: 10.2337/dc10-9990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zambrano J, Celano CM, Chung W-J, et al. Exploring the feasibility and impact of positive psychology-motivational interviewing interventions to promote positive affect and physical activity in type 2 diabets: Design and methods from the BEHOLD-8 and BEHOLD-16 clinical trials. Heal Psychol Behav Med [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kubzansky LD, Huffman JC, Boehm JK, et al. (2018) Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. J Am Coll Cardiol 72:1382–1396. doi: 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craig CL, Marshall AL, Sjöström M, et al. (2003) International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc 35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 16.Callahan CM, Unverzagt FW, Hui SL, et al. (2002) Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 40:771–81. doi: 10.1097/00005650-200209000-00007 [DOI] [PubMed] [Google Scholar]
- 17.Gorman E, Hanson HM, Yang PH, et al. (2014) Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur Rev Aging Phys Act 11:35–49. doi: 10.1007/s11556-013-0132-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woo SY, Kim S (2020) Determination of cutoff values for biomarkers in clinical studies. Precis Futur Med 4:2–8. doi: 10.23838/pfm.2019.00135 [DOI] [Google Scholar]
- 19.Ringeval M, Wagner G, Denford J, et al. (2020) Fitbit-Based Interventions for Healthy Lifestyle Outcomes: Systematic Review and Meta-Analysis. J Med Internet res 22:e23954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


