Abstract
Abstract
Medial collateral ligament (MCL) is the most commonly injured ligament of the knee. Acute Grade III MCL injuries can be managed conservatively except bony avulsion, intra-articular entrapment and Stener lesion, which requires surgical treatment by repair with or without augmentation. Chronic MCL injuries are treated surgically with various reconstruction techniques that are well established in the literature, which requires use of autograft or allograft and multiple tunnel placement with multiple implants for graft fixation. These techniques possess higher chances of tunnel convergence and hardware-related complications, further increasing surgery cost, especially for multi ligament injuries. Finally, all these MCL reconstruction surgeries are technically challenging. Here, we propose our technique of single-row repair in cases of chronic femoral side MCL insufficiency with grade III valgus laxity. This technique reattaches the torn ligament at its near anatomical attachment site using a single, double-loaded 5.5-mm suture anchor. This technique preserves and uses the native MCL, requiring no separate graft and no tunnel preparation. Hence, no graft site morbidity and tunnel-related complications, along with maintenance of proprioception. It is a cost-effective, reproducible, and technically simple procedure with good functional outcome.
Level I
knee
Level II
collateral ligaments
Technique Video
Video demonstrates the surgical video of a patient with left knee chronic grade III MCL insufficiency, treated with single row MCL repair, in supine position, viewing from anterolateral portal.
Introduction
The medial collateral ligament (MCL) is reported to be the most commonly injured ligament in the knee, accounting for 42% of ligamentous knee injuries.1 It is injured in association with anterior cruciate ligament (ACL) in 20% to 38% cases.2 The injury more frequently occurs in the active and athletic population playing contact and noncontact sports.
The anatomy of MCL has been well studied and described in the literature; the MCL does not work alone as an individual entity, but as a complex comprising superficial MCL (sMCL), deep MCL (dMCL), and posterior oblique ligament (POL).3 Superficial MCL is the primary stabilizer to valgus stress with deep MCL acting as secondary stabilizer at varying degrees of flexion, whereas POL is the primary stabilizer to valgus stress in full extension.4,5
According to American Medical Association6 and modified Hughston classification7 system, MCL ligament injuries have been categorized into various grades. All Grade I (MCL sprain with <5-mm joint laxity) are treated conservatively. The majority of surgeons in Grade II (partial MCL tear with 5-10-mm joint laxity) recommend conservative treatment,8 although some found that there remained residual laxity after treating grade II tears conservatively9 and, therefore, suggested surgery.2
In Grade III (complete tear with >1-cm joint laxity), conservative management can be tried in clearly defined tear patterns with neutral/varus knee alignment, but most surgeons prefer operative management, as conservative treatment may lead to residual laxity and delayed definitive management of concurrent ACL/PCL in multiligamentous injuries.10,11 Diffuse MCL injury, intra-articular entrapment, Stener lesion, and bony avulsion are managed by acute MCL repair with or without augmentation with autograft, allograft, or internal bracing.12
In chronic MCL insufficiency, the majority of consensus is toward operative management with MCL reconstruction using autograft or allograft. Popular techniques for MCL reconstruction like LaPrade and Wijdicks,13 Kim et al.,14 and Joshi et al.15 are technically demanding procedures that require use of multiple grafts, multiple tunnel placement, and multiple fixation devices. These procedures and devices, therefore, make the procedure costly and challenging, especially in cases of multiligament reconstruction procedures.
Here, we describe our technique of single-row repair in chronic femoral side MCL insufficiency by reattaching the torn ligament at its near anatomical position using single, double-loaded 5.5-mm suture anchor similar to the technique of chronic rotator cuff repair. This technique preserves and uses native MCL, and hence, there is no graft or tunnel placement required. This technique, thereby, prevents graft site morbidity and tunnel-related complications and maintains proprioception. The use of a single implant makes it cost-effective. Technically, it is a simple and reproducible procedure.
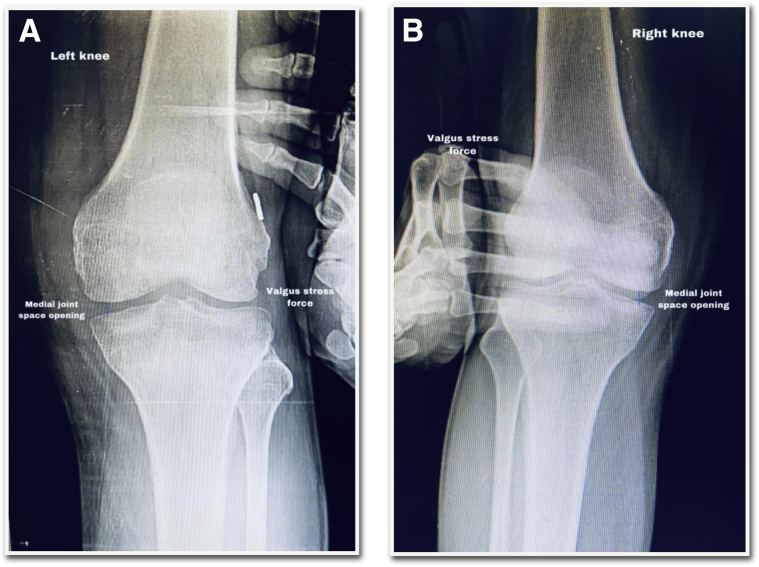
Before planning the surgery, a preoperative stress radiograph (Fig 1A) helps to assess medial joint opening and confirmation of MCL injury, while magnetic resonance imaging (Fig 1B) is useful in identifying the exact location of MCL tear.
Fig 1.
(A) Preoperative anteroposterior valgus stress radiograph of left knee demonstrates significant medial joint space opening, indicating MCL insufficiency injury. (B) Coronal T1-weighted MRI of left knee demonstrates MCL tear at the proximal femoral attachment site shown by # (hash) sign, with intact midsubstance and distal tibial attachment shown by ∗ (asterisk). MCL, medial collateral ligament; MRI, magnetic resonance imaging.
Surgical Technique
Patient Positioning
Under spinal anesthesia, a well-padded pneumatic tourniquet cuff is applied to the proximal thigh of the operative limb. Patient is placed in a supine position with the knee hanging at 90° at the caudal end of the operating table. The limb is supported by lateral side support to stabilize it while valgus stress force is applied. Painting and draping is done taking all aseptic precautions. Tourniquet inflated at 300 mm of Hg.
Portals Placement
Standard anterolateral primary viewing portal is placed just below the lower pole of patella and lateral to the patellar tendon. A 4 mm, 30° arthroscope is inserted for initial joint inspection. Second anteromedial horizontal portal is made under direct supervision using spinal needle to prevent iatrogenic injury to medial meniscus.
Diagnostic Arthroscopy and Medial Joint Assessment
With arthroscope in anterolateral viewing portal, a 4 mm probe is inserted through anteromedial portal. Initial assessment at 00 and 300 reveals significant medial joint space opening on application of valgus stress force, confirming grade III MCL laxity indicating both components (sMCL and POL) insufficiency (Video 1).
Our Surgical Technique of Single-Row MCL Repair
Operative limb is held in 200-300 knee flexion with hip in slight external rotation. Longitudinal skin incision approximately 5-7 cm in length is taken on the medial aspect of knee, centered over the medial epicondyle, subcutaneous tissue with superficial fascia incised without opening the joint (Fig 2A). MCL grade III laxity is confirmed again at 00 and 30° applying valgus stress force. It has been confirmed that MCL heals with residual laxity at femoral site. It also ensures that the distal tibial MCL attachment is intact. The lax tissue comprising of sMCL and POL is held with forceps and is sharply incised with no. 11 scalpel blade, along with underlying periosteum. This exposes the whole medial femoral epicondyle, keeping meniscofemoral ligaments intact (Fig 2B). The residual lax MCL complex is pulled proximally with help of allis forceps to make it taught (Fig 2C). The anatomical proximal attachment site of MCL is approximately 3.2 mm proximal and 4.8 mm posterior to the medial femoral epicondyle. The bone bed is prepared using rasp to enhance healing of proximal MCL after repair. A punch tap is used to create a hole for anchor placement at the above-mentioned site. A double-loaded HEALICOIL PK 5.5-mm suture anchor with Two ULTRABRAID (#2) (Smith & Nephew, Andover, MA) is screwed in. Cobraid blue ultrabraid suture is used in mattress fashion to cut into in sMCL and dMCL. Blue ultrabraid suture is used in same mattress fashion to cut into the POL (Fig 2D). The fiber wires are then pulled together to bring the retracted MCL tissue back to its original location. First POL is tightened with knee in full extension using simple surgical knots, keeping it in neutral rotation and varus. Then sMCL and dMCL are tightened by changing the knee flexion to 30°, maintaining neutral rotation and varus. The knee is tested for the entire range of motion to assess medial stability.
Fig 2.
(A) Viewing from the medial side of a patient in supine position with left knee held in 20° flexion. Skin incision is shown for medial aspect of left knee and centered over medial epicondyle, as well as subcutaneous tissue and superficial fascia incision. Lax MCL tissue is identified, demonstrated by # (hash) sign, and proximal blue mark demonstrates medial epicondyle, and distal blue mark demonstrates medial joint line. An asterisk (∗) shows graft passage for ACL reconstruction. (B) Proximal MCL with underlying periosteum is shown detached from medial epicondyle up to meniscofemoral ligament, which is shown by an asterisk (∗). (C) sMCl demonstrated by hashtag (#) sign and POL by an asterisk (∗), where dMCL lies underneath them. Allis tissue forceps are used to hold and pull the retracted tissue after elevating it subperiosteally. (D) Two cobraid blue ULTRABRAID sutures were used in mattress fashion for the sMCL and the dMCL, as shown by hashtag (#) and two blue ULTRABRAID sutures that were applied in mattress fashion to the POL, as shown by an asterisk (∗), whereas $ (dollar) sign shows the placement of HEALICOIL PK 5.5-mm suture anchor. ACL, anterior cruciate ligament; dMCL, deep medial collateral ligament; MCL, medial collateral ligament, sMCL, superficial medial collateral ligament; POL, posterior oblique ligament.
Once the single-row MCL repair is done, then the arthroscope is again inserted through anterolateral portal to assess medial joint opening. The arthroscope clearly demonstrates significant reduction in the medial joint space opening on valgus stress force, as evidenced by the difficulty of the probe to enter the medial joint space compared to the prerepair status (Fig 3A, 3B). The wound is sutured in layers, arthroscopy portals are closed, and compressive dressing is applied.
Fig 3.
(A) A 4-mm probe is passed through anteromedial portal, demonstrating significant medial joint space opening on valgus stress force and indicating grade III MCL laxity, while camera was placed in anterolateral viewing portal. (B) With arthroscope placed in anterolateral viewing portal, the 4-mm probe inserted through anteromedial portal had difficulty in passage, indicating significant reduction in medial joint space on valgus stress after MCL repair compared to prerepair status. MCL, medial collateral ligament.
A postoperative valgus stress radiograph demonstrates good healing of MCL at the repaired site assessed by the medial joint opening (Fig 4A) compared to the contralateral normal side (Fig 4B).
Fig 4.
(A) Postoperative anteroposterior valgus stress radiograph of operated left knee demonstrates significant reduction in medial joint space opening. (B) Valgus stress radiograph of the contralateral normal right side demonstrates similar medial joint space compared to the repaired side.
Postoperative Rehabilitation Protocol
Operative limb is held in static knee brace for 6 weeks. Static quadriceps and hamstring strengthening exercises with ankle movements are started on the same day as surgery. Straight leg raises with hip abduction and adduction permitted. Knee mobilization exercises are started the next day after the surgery, gradually to progress to 30° range of motion in the first week, 60° by the second week, and 90° by the third week, and full range of motion by the end of 4 weeks. Patient does not bear weight on the knee for 6 weeks, patient can start bearing partial weight from 6 to 8 weeks, and after 8 weeks, patient can be allowed to bear full weight on the operative limb while wearing a hinged knee brace. Normal walking and stair climbing with half squats allowed after 8 weeks. Strengthening exercises are started after 12 weeks. Sport-specific exercises are started after 6 months, and patient is allowed to resume sporting activities by the end of 9 months. This protocol can be modified for an individual patient, depending upon the concomitant knee injuries treated.
Discussion
It is widely accepted that the MCL has better healing capacity than ACL, which has led to the consensus that MCL tears can be managed conservatively and ACL tears require reconstruction.2,16 Most surgeons prefer conservative management in Grade I and II MCL injuries,17 and some even prefer a similar protocol in grade III acute MCL injuries with or without associated cruciate ligament injury. But this has several disadvantages like quadriceps atrophy, residual laxity, and prolongation of the definitive surgery.9,18
In the acute scenario, diffuse injury to MCL, intra-articular entrapment, Stener lesion, and bony avulsion require MCL repair with or without augmentation. Primary ACL and MCL repair with internal bracing can be performed in the acute setting with the advantage of avoiding quadriceps atrophy, maintaining proprioception, and preserving the patient’s ligaments.12
In chronic insufficiency, MCL reconstruction is the treatment of choice. Dong et al.19 compared MCL triangular reconstruction with MCL repair without an internal brace in the setting of ACL-MCL injuries and found equivalent outcomes regarding ROM, medial stability, and subjective outcomes, but a higher rate of anteromedial instability in the repair group.
Robert Laprade13 described the anatomical and isometric MCL reconstruction technique by recreating both the sMCL and POL using two separate grafts, four tunnels—two each in femur and tibia. Grafts were fixed with bioabsorbable screws and suture anchor. This anatomical reconstruction technique improved overall patient function and restored valgus instability with no patient having recurrent laxity at an average follow up of 18 months. Disadvantage of this technique is that it is technically demanding and costly, with a high chance of tunnel coalescence and required multiple grafts.
Kim et al.14 used a single semitendinosus graft, keeping the distal tibial attachment intact to reconstruct both sMCL and POL. It was limited to two tunnels—one in the femur and one in the tibia, with two implants. He mentioned good to excellent outcomes, with 92% of patients having less than 3 mm of valgus opening, at an average follow up of 52 months. Lind et al.20 and Stannard et al.21 also reported good subjective outcomes with their similar techniques, in which only 50% of Lind’s and 32% of Stannard’s patients had a valgus opening less than 3 mm at an average follow up of 40 months. However, anterior attachment of semitendinosus in relation to sMCL at tibia, as mentioned in above techniques, leads to nonanatomical and anisometric reconstruction.
Joshi et al.15 modified the Kim et al. technique14 by rerouting and weaving the semitendinosus to tibial remnant of sMCL and reproducing a near-anatomical MCL and POL reconstruction, in contrast to LaPrade and Wijdicks,13 but with only two tunnels and two implants. It was more anatomical and isometric than Kim et al.’s technique.
All of these above-mentioned procedures described for MCL reconstruction in chronic insufficiency requires multiple grafts, multiple tunnel placements, multiple implants adding to cost and technical difficulties. Except LaPrade’s13 technique, all other techniques are relatively nonanatomical and anisometric, but still provide good stability and functional outcome.
Here, we describe a relatively simple technique of single-row MCL repair in cases of chronic femoral side MCL insufficiency. This technique restores the near normal anatomy by using and preserving the native MCL, which helps in maintaining proprioception. In our technique, we use a single, double-loaded 5.5-mm suture anchor, so it is cost-effective. It doesn’t require any separate graft; hence, there is no graft site morbidity. This technique doesn’t require tunnel preparation; hence, there are no chances of tunnel coalescence, even in cases of multiligament reconstruction. Although our technique is simple to reproduce, there are both advantages and disadvantages, which are summarized in Table 1.
Table 1.
Advantages and Disadvantages of the Single-Row MCL Repair Technique
| Advantages | Disadvantages |
|---|---|
| Technically simple and reproducible. | Our technique is relatively nonanatomical at the femoral insertion site, as we chose a common attachment for sMCL and POL. |
| Preserves the native MCL, hence helps in maintaining proprioception. | MCL repair can be difficult if the tissue quality is too bad. |
| Use of a single implant reduces the cost and hardware-related complications. | We performed this technique only in cases of femoral side insufficiency, and further studies are required in tibial side tears. |
| No graft requirement, hence no graft site morbidity. | This technique cannot be performed in chronic midsubstance tear. |
| No tunnel requirement, hence, no tunnel coalescence in multiligament injury reconstruction. | |
| Use of the periosteal tissue for better healing. | |
| Similar functional outcome obtained when compared with other reconstruction techniques. |
MCL, medial collateral ligament, POL, posterior oblique ligament; sMCL, superficial medial collateral ligament.
In conclusion, we tried to replicate the same theory in chronic MCL injury, as followed in management of chronic rotator cuff tears in which single-row repair is done by pulling back the retracted cuff tissue and reattaching it to its anatomical site by suture anchors, hence, the term single-row MCL repair. Early functional outcomes are encouraging, as analyzed clinically and radiologically. We propose that this technique can be performed in cases of chronic tibial side MCL injury, as well in the similar manner. All previous literature emphasizes different reconstruction techniques in cases of chronic MCL injuries. We believe our technique demonstrates that MCL repair can be performed, even in chronic insufficiency similar to that in acute setting, provided its avulsed from either side, but long-term studies are required.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Video demonstrates the surgical video of a patient with left knee chronic grade III MCL insufficiency, treated with single row MCL repair, in supine position, viewing from anterolateral portal.
References
- 1.Bollen S. Epidemiology of knee injuries: diagnosis and triage. Br J Sports Med. 2000;34:227–228. doi: 10.1136/bjsm.34.3.227-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ateschrang A., Dobele S., Freude T., Stockle U., Schroter S., Kraus T.M. Acute MCL and ACL injuries: First results of minimal-invasive MCL ligament bracing with combined ACL single-bundle reconstruction. Arch Orthop Trauma Surg. 2016;136:1265–1272. doi: 10.1007/s00402-016-2497-6. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 4.Griffith C.J., LaPrade R.F., Johansen S., Armitage B., Wijdicks C., Engebretsen L. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am J Sports Med. 2009;37:1762–1770. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 5.Griffith C.J., Wijdicks C.A., LaPrade R.F., Armitage B.M., Johansen S., Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. 2009;37:140–148. doi: 10.1177/0363546508322890. [DOI] [PubMed] [Google Scholar]
- 6.American Medical Association . Standard nomenclature of athletic injuries; Chicago, IL: 1966. Committee on the Medial Aspects of Sports. Subcommittee on Classification of Sports Injuries; p. 157. AMA. [Google Scholar]
- 7.Hughston JC, Andrews JR, Cross MJ, Moschi A: Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Joint Surg Am 58:159-172, 197. [PubMed]
- 8.Millett P.J., Pennock A.T., Sterett W.I., Steadman J.R. Early ACL reconstruction in combined ACL-MCL injuries. J Knee Surg. 2004;17:94–98. doi: 10.1055/s-0030-1248204. [DOI] [PubMed] [Google Scholar]
- 9.Zaffagnini S., Bignozzi S., Martelli S., Lopomo N., Marcacci M. Does ACL reconstruction restore knee stability in combined lesions?: An in vivo study. Clin Orthop Relat Res. 2007;454:95–99. doi: 10.1097/BLO.0b013e31802b4a86. [DOI] [PubMed] [Google Scholar]
- 10.Van der List J.P., DiFelice G.S. Preservation of the anterior cruciate ligament: A treatment algorithm based on tear location and tissue quality. Am J Orthop (Belle Mead NJ) 2016;45:E393–E405. [PubMed] [Google Scholar]
- 11.DiFelice G.S., van der List J.P. Arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthrosc Tech. 2016;5:e1057–e1061. doi: 10.1016/j.eats.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van der List J.P., Difelice G.S. Primary repair of the medial collateral ligament with internal bracing. Arthrosc Tech. 2017;6:e933–e937. doi: 10.1016/j.eats.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LaPrade R.F., Wijdicks C.A. Surgical technique: Development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806–814. doi: 10.1007/s11999-011-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim S.-J., Lee D.-H., Kim T.-E., Choi N.-H. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br. 2008;90:1323–1327. doi: 10.1302/0301-620X.90B10.20781. [DOI] [PubMed] [Google Scholar]
- 15.Joshi A., Singh N., Thapa S., Pradhan I. Weave technique for reconstruction of medial collateral ligament and posterior oblique ligament: an anatomic approach using semitendinosus tendon. Arthrosc Tech. 2019;8:e1417–e1423. doi: 10.1016/j.eats.2019.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woo S.L.-Y., Vogrin T.M., Abramowitch S.D. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg. 2000;8:364–372. doi: 10.5435/00124635-200011000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Duffy P.S., Miyamoto R.G. Management of medial collateral ligament injuries in the knee: an update and review. Phys Sportsmed. 2010;38:48–54. doi: 10.3810/psm.2010.06.1782. [DOI] [PubMed] [Google Scholar]
- 18.Halinen J., Lindahl J., Hirvensalo E., Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: A prospective randomized study. Am J Sports Med. 2006;34:1134–1140. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]
- 19.Dong J., Wang X.F., Men X., et al. Surgical treatment of acute grade III medial collateral ligament injury combined with anterior cruciate ligament injury: Anatomic ligament repair versus triangular ligament reconstruction. Arthroscopy. 2015;31:1108–1116. doi: 10.1016/j.arthro.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 20.Lind M., Jakobsen B.W., Lund B., Hansen M.S., Abdallah O., Christiansen S.E. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37:1116–1122. doi: 10.1177/0363546509332498. [DOI] [PubMed] [Google Scholar]
- 21.Stannard J.P., Black B.S., Azbell C., Volgas D.A. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25:429–434. doi: 10.1055/s-0032-1322605. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video demonstrates the surgical video of a patient with left knee chronic grade III MCL insufficiency, treated with single row MCL repair, in supine position, viewing from anterolateral portal.
Video demonstrates the surgical video of a patient with left knee chronic grade III MCL insufficiency, treated with single row MCL repair, in supine position, viewing from anterolateral portal.