Abstract
Since SARS-CoV-2 virus emerging in winter 2019 in Wuhan, Hubei, China, COVID-19 has spread among different countries. The novel corona virus has affected more than 15,000,000 people all around the world. Becoming pandemic, COVID-19 is a major concern for both people and health systems. Novel corona virus affects multiple organs such as lungs and kidneys which can lead to acute respiratory distress syndrome and acute kidney injury (AKI) ending to death. Furthermore, patients with COVID-19 may present different atypical symptoms making the diagnoses more complicated. The current patient presented to the emergency department with a 7-day history of hemoptysis and hematuria which are among the less common symptoms among patients infected with SARS-CoV-2 virus. In addition to delayed diagnosis, atypical symptoms and signs make management and treatment more difficult. Awareness of new, atypical symptoms and the effective treatment is associated with better outcome and prognosis.
Keywords: COVID-19, Hemoptysis, Hematuria, Corona virus, SARS-CoV-2
INTRODUCTION
Since COVID-19 arising in late December 2019 in Wuhan, Hubei, China, many patients are infected with this novel pathogen, named as SARS-CoV-2 virus. Nowadays, COVID-19 (first known as 2019-nCoV) has spread worldwide and affected almost 16,000,000 people in different countries. Resulting in high morbidity and mortality rate, COVID-19 pandemic is now a major concern and threat for health systems.
Although the most common symptoms of the disease are fever, cough, shortness of breath, myalgia and fatigue (1), evidences show that patients with COVID-19 may complain of atypical symptoms such as upper respiratory tract or gastrointestinal symptoms. In addition to lungs, the novel corona virus can affect multiple organs such as heart, brain and kidneys. Hematuria is one of the less common symptoms among patients with acute kidney injury (AKI) induced by SARS-CoV-2 virus (2). On the other hand, hemoptysis is among the rare symptoms with a prevalence of up to 5% (3, 4).
Presenting with less common or atypical symptoms makes the disease harder to diagnose. To the best of our knowledge, this patient is the first case of COVID-19 infection presenting concurrent hemoptysis and hematuria as the first symptoms of infection.
CASE SUMMARIES
A 21-year-old Afghan man presented to the emergency department with a 7-day history of fever, chills, hemoptysis and hematuria. He denied any recent exposure to any patient with COVID-19. He had no significant history of rheumatologic disorders or any other diseases. The patient had tachypnea and tachycardia on admission. He demonstrated normal blood pressure. Oxygen saturation was measured 86% in room air by pulse oximetry which reached 96% using the 60% venture mask. On examination, his lungs displayed bilateral coarse crackles. Electrocardiography findings were normal.
At the time of hospital admission, laboratory tests showed HGB: 14.7 gr/dl; WBC: 11.61×103/mm3; PLT: 162×103/mm3; D-dimer: 900 ng/ml; CRP: 12 mg/dl; ESR: 60. In arterial blood gas analysis, pH: 7.35, pCO2: 50.7 and HCO3: 27.3 were noted. Urine analysis was notable for protein: 1+; WBC: 12–14; RBC: 20–25 and blood: 2+. Other laboratory parameters were in normal ranges. No bacterial growth was seen in blood and urine culture. Respiratory mucus smear and culture were also negative for Mycobacterium tuberculosis and bacterial infection.
Due to his respiratory signs, a spiral computed tomography (CT) scan of lungs was performed which revealed evidences of bilateral ground glass opacity and multifocal consolidation distributed along the subpleural regions suggesting for COVID-19 (Figure 1 A-C). Reverse transcriptase polymerase chain reaction test for COVID- 19 was performed to confirm the diagnosis which showed positive result.
Figure 1.
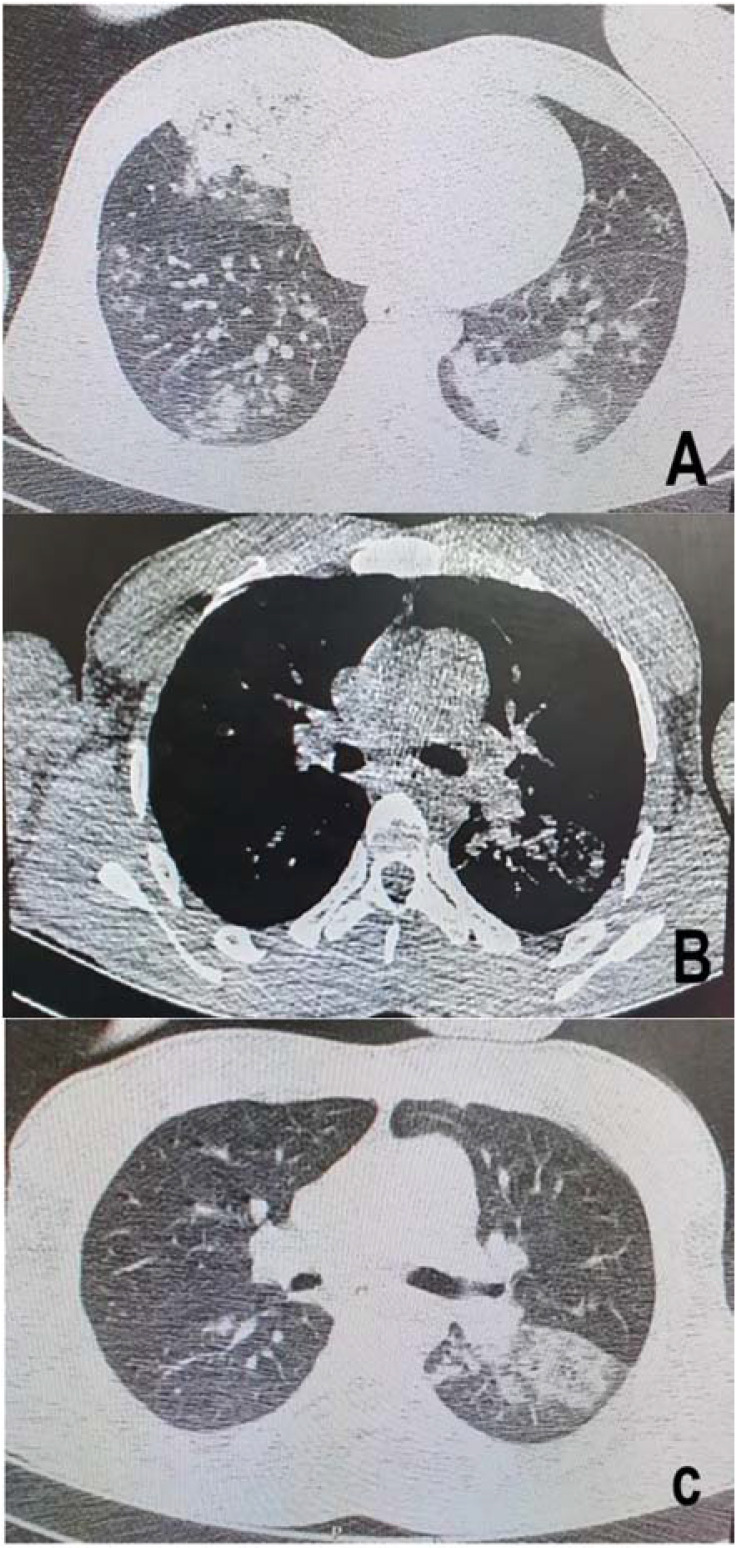
CT scan findings on day of admission. Spiral CT scan of lungs revealed evidences of A. bilateral ground glass opacity and B and C. multifocal consolidation distributed along the subpleural regions.
During hospitalization, hemoptysis and dyspnea worsened and the patient deteriorated. Since hemoptysis was uncontrolled and tachypnea was worsened, the patient underwent endotracheal intubation on the second day of hospitalization. Active airway bleeding was noticed during intubation.
Due to his concurrent hemoptysis and hematuria, the patient was suspected to have vasculitis. Therefore, rheumatologic tests including ANA, Anti ds-DNA, C ANCA, P ANCA, anti CCP, RF, SSA-RO and SSA-LA were performed for the patient. All the performed rheumatologic tests were negative. On the third day of hospitalization, laboratory examinations were notable for HGB: 13.7 gr/dl; WBC: 0.8×103/mm3(lymphocyte count was undetectable); PLT= 84×103/mm3; BUN=52 mg/dl; Cr=2.66 mg/dl, lactate dehydrogenase (LDH) =774 U/l and aspartate aminotransferase (AST)=50 U/l. Venous blood gas analyses showed a pH of 7.12; a PCO2 of 53.6 and a HCO3 of 17.2.
Despite supportive, anti-viral and antibiotic therapy, the patient died due to respiratory failure and multi-organ damage on the third day of hospitalization.
DISCUSSION
Nowadays, COVID-19 pandemic is a major threat for both people and health care systems. Unfortunately, still there is no effective treatment against this novel virus and more patients are affected and lost every day. Hence, the burden of the disease is rising quickly.
A cohort study carried out by Huang et al., demonstrated that the most common symptoms at initiation of the disease were fever (98%), cough (76%), and myalgia or fatigue (44%) (3). Symptoms including sputum production, headache and diarrhea were less common. Hemoptysis is among the less common symptoms with a prevalence of 0–5% (3). Furthermore, researches showed that SARS-CoV-2 can target multiple organs leading to appearance of new different symptoms among infected patients. Presenting with less common or atypical symptoms makes the diagnosis harder and results in delay in diagnosis of the main underlying disease. Furthermore, atypical symptoms and signs are more difficult to manage and treat. Hemoptysis, hematuria and fever were the only presenting symptoms in current patient at onset of the disease. Due to concurrent hemoptysis and hematuria, rheumatologic diseases especially vasculitis were considered and the patient underwent rheumatological evaluations which all were negative.
This patient had notable levels of D-dimer (900 ng/ml) and LDH (774 U/l) in laboratory examinations. Also the serum levels of AST showed a mild increase during hospitalization (50 U/l). Studies showed that serum levels of D-dimer, AST and LDH are increased among patients with COVID-19 (3, 5). Furthermore the levels of hemoglobin, white blood cell count and platelets decreased during hospitalization. A recent meta-analysis carried out by Lippi et al., showed that patients with COVID-19 had significantly lower levels of platelets and thrombocytopenia (platelet count less than 150×103/μl) was associated with disease severity and higher morbidity and mortality (6). Authors showed that thrombocytopenia was associated with three-fold increased risk of severe COVID-19. However, the exact mechanism of COVID-19 induced platelet depletion is still unknown. Leukopenia (i.e. white blood cell count under 4.0×109/L) and lymphocytopenia (i.e. lymphocyte count less than 1.0×109/L) are common among patients with SARS- CoV-2 virus infection. A recent study carried out in China showed that 25% and 63% of patients on admission had leukopenia and lymphocytopenia, respectively (3). Furthermore, the level of hemoglobin was decreased from 14.1 to 13.7 gr/dl; however, the final level was still within normal range.
SARS-CoV-2 affects different organs and leads to multi-organ damage and failure. Studies reported that AKI occurred among almost 6% of the patients with COVID-19. Acute kidney injury is associated with an increased risk of mortality among these patients (7, 8). Li et al. reported that increased level of proteinuria, hematuria, BUN and Cr were associated with higher risk of death among patients with COVID-19 (2). However, the exact mechanism leading to kidney injury is still unknown. Hematuria and proteinuria are among the most common signs of AKI among patients infected with SARS-CoV-2 virus. The current patient complained of hematuria that lasted for a week. Urine analysis revealed a protein of 1+ and a blood of 2+ in urine sample. This patient suffered from AKI and the serum levels of creatinine and blood urea nitrogen increased highly during hospitalization (2.66 mg/dl and 52 mg/dl, respectively).
There is no effective medical treatment for kidney injury induced by COVID-19. Lotfi et al. suggested that supportive treatment should be considered for patients who suffer from acute renal failure due to infection with the novel corona virus (7). Despite aggressive supportive treatment, the levels of BUN and Cr continued to rise and the patient deteriorated. Finding effective treatment strategies for less common symptoms is necessary to avoid morbidity and mortality in affected patients.
Computed tomography scan is one of the most common diagnostic tools used for patients with respiratory symptoms. Ground glass opacity(GGO), mixed GGO, crazy-paving patterns, peripheral and subpleural consolidations and bilateral involvement of both lower lungs are among the typical findings of CT scan among patients with COVID-19 (9, 10). In this patient a spiral CT scan of lungs was performed which revealed evidences of bilateral ground glass opacity and multifocal consolidation distributed along the subpleural regions. There was no atypical manifestation in radiological evaluations. Since typical CT scan findings were detected in this patient, the infection with the virus was suspected. Hence, a reverse transcriptase polymerase chain reaction test for COVID-19 was performed and the diagnosis of COVID-19 was confirmed.
This patient is the case of COVID-19 infection presenting with concurrent hemoptysis and hematuria as the first symptoms of infection. The current patient represents the complexity of the pathogenesis of the disease caused by SARS-CoV-2 virus.
CONCLUSION
We presented this rare case with concurrent hemoptysis and hematuria as the initial symptoms of infection with SARS- CoV-2 virus in a patient without any other comorbidity. Awareness of new, atypical symptoms makes the diagnosis of disease earlier which may lead to better outcomes and survival improvement. Finding the pathogenesis, effective medical treatment and management for such symptoms should be studied in further researches.
Footnotes
Conflicts of interest
The authors have no conflicts of interest.
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020;382(18):1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Z, Wu M, Yao J, Guo J, Liao X, Song S, et al. Caution on kidney dysfunctions of COVID-19 patients. The Lancet Infectious Diseases 2020.
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casey K, Iteen A, Nicolini R, Auten J. COVID-19 pneumonia with hemoptysis: Acute segmental pulmonary emboli associated with novel coronavirus infection. Am J Emerg Med 2020;38(7):1544.e1–1544.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020;323(11):1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta 2020;506:145–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lotfi B, Farshid S, Dadashzadeh N, Valizadeh R, Rahimi MM. Is coronavirus disease 2019 (COVID-19) associated with renal involvement? A review of century infection. Jundishapur Journal of Microbiology 2020;13(4):1–6. [Google Scholar]
- 8.Mubarak M, Nasri H. COVID-19 nephropathy; an emerging condition caused by novel coronavirus infection. Journal of Nephropathology 2020;9(3):1–2. [Google Scholar]
- 9.Kanne JP. Chest CT Findings in 2019 Novel Coronavirus (2019-nCoV) Infections from Wuhan, China: Key Points for the Radiologist. Radiology 2020;295(1):16–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi F, Yu Q, Huang W, Tan C. 2019 Novel Coronavirus (COVID-19) Pneumonia with Hemoptysis as the Initial Symptom: CT and Clinical Features. Korean J Radiol 2020;21(5):537–40. [DOI] [PMC free article] [PubMed] [Google Scholar]


