Key Points
Question
What are the findings on cardiac imaging in children with myocarditis after COVID-19 vaccination?
Findings
In this case series of 15 children who were hospitalized with myocarditis after receipt of the BNT162b2 messenger RNA COVID-19 vaccine for 1 to 5 days, boys were most often affected after the second vaccine dose, 3 patients had ventricular systolic dysfunction, and 12 patients had late gadolinium enhancement on cardiac magnetic resonance imaging. There was no mortality, and all but 1 patient had normal echocardiogram results on follow-up 1 to 13 days after discharge.
Meaning
COVID-19 vaccine-associated myocarditis may have a benign short-term course in children; however, the long-term risks remain unknown.
Abstract
Importance
The BNT162b2 (Pfizer-BioNTech) messenger RNA COVID-19 vaccine was authorized on May 10, 2021, for emergency use in children aged 12 years and older. Initial reports showed that the vaccine was well tolerated without serious adverse events; however, cases of myocarditis have been reported since approval.
Objective
To review results of comprehensive cardiac imaging in children with myocarditis after COVID-19 vaccine.
Design, Setting, and Participants
This study was a case series of children younger than 19 years hospitalized with myocarditis within 30 days of BNT162b2 messenger RNA COVID-19 vaccine. The setting was a single-center pediatric referral facility, and admissions occurred between May 1 and July 15, 2021.
Main Outcomes and Measures
All patients underwent cardiac evaluation including an electrocardiogram, echocardiogram, and cardiac magnetic resonance imaging.
Results
Fifteen patients (14 male patients [93%]; median age, 15 years [range, 12-18 years]) were hospitalized for management of myocarditis after receiving the BNT162b2 (Pfizer) vaccine. Symptoms started 1 to 6 days after receipt of the vaccine and included chest pain in 15 patients (100%), fever in 10 patients (67%), myalgia in 8 patients (53%), and headache in 6 patients (40%). Troponin levels were elevated in all patients at admission (median, 0.25 ng/mL [range, 0.08-3.15 ng/mL]) and peaked 0.1 to 2.3 days after admission. By echocardiographic examination, decreased left ventricular (LV) ejection fraction (EF) was present in 3 patients (20%), and abnormal global longitudinal or circumferential strain was present in 5 patients (33%). No patient had a pericardial effusion. Cardiac magnetic resonance imaging findings were consistent with myocarditis in 13 patients (87%) including late gadolinium enhancement in 12 patients (80%), regional hyperintensity on T2-weighted imaging in 2 patients (13%), elevated extracellular volume fraction in 3 patients (20%), and elevated LV global native T1 in 2 patients (20%). No patient required intensive care unit admission, and median hospital length of stay was 2 days (range 1-5). At follow-up 1 to 13 days after hospital discharge, 11 patients (73%) had resolution of symptoms. One patient (7%) had persistent borderline low LV systolic function on echocardiogram (EF 54%). Troponin levels remained mildly elevated in 3 patients (20%). One patient (7%) had nonsustained ventricular tachycardia on ambulatory monitor.
Conclusions and Relevance
In this small case series study, myocarditis was diagnosed in children after COVID-19 vaccination, most commonly in boys after the second dose. In this case series, in short-term follow-up, patients were mildly affected. The long-term risks associated with postvaccination myocarditis remain unknown. Larger studies with longer follow-up are needed to inform recommendations for COVID-19 vaccination in this population.
This case series reviews comprehensive cardiac imaging in children with myocarditis after COVID-19 vaccine.
Introduction
SARS-CoV-2 was first identified in China and evolved rapidly to a global pandemic. Vaccines to prevent SARS-CoV-2 infection are the current standard approach for curbing the pandemic. In the US, the BNT162b2 messenger RNA (mRNA) (Pfizer-BioNTech), mRNA-1273 (Moderna), and Ad26.COV2.S (Janssen) vaccines were granted emergency use authorization for adults. On May 10, 2021, the emergency use authorization for the BNT162b2 vaccine was extended to children aged 12 years and older.1
Myocarditis has been reported as a rare complication of vaccination against other viruses.2 It was not reported in the initial messenger RNA COVID-19 vaccine trials, although the ability to detect rare events was limited by sample size. Since the emergency use authorization, myocarditis in adolescents and young adults after COVID-19 vaccine has been reported.3,4,5 In this series, we detail the occurrence of myocarditis after COVID-19 vaccination in an adolescent population, including comprehensive cardiac imaging evaluation and follow-up.
Methods
Population
This case series included all patients younger than 19 years admitted at our center with acute myocarditis after COVID-19 vaccination. Myocarditis was defined as chest pain and an elevated troponin level in the absence of an alternative diagnosis. The institutional review board at Boston Children’s Hospital approved this study and granted an exemption from informed consent owing to use of deidentified data and the requirements of 45 CFR §46. This study followed the reporting guideline for case series.
Data Collection and Definitions
Clinical data elements including demographic characteristics, laboratory values, and hospital course were collected from the electronic medical record. Patients’ race and ethnicity were self-reported by patients or parents according to the US Census categories6 and were collected because of their known association with COVID-19–related illnesses. Elevated troponin T level was defined as a troponin value greater than 0.01 ng/mL. Cardiac evaluation for all patients included electrocardiogram (ECG), echocardiogram, and cardiac magnetic resonance (CMR) imaging. Ventricular systolic dysfunction was defined as a left ventricular (LV) ejection fraction equal to or greater than 55% on echocardiogram or CMR results. Echocardiographic peak global longitudinal strain was measured from an apical 4-chamber view and peak global circumferential strain from a parasternal short-axis view at the midpapillary level using software (Tom Tec Image Arena, version 4.6; TOMTEC). Strain values were considered abnormal if the z score was less than or equal to −2 for age. Diastolic dysfunction was defined as a z score less than or equal to −2 for age, for septal e′ tissue Doppler, LV free wall e′, or the E/e′ ratio. CMR assessment included LV ejection fraction, T2-weighted myocardial imaging, LV global native T1, LV global T2, extracellular volume fraction, and late gadolinium enhancement (LGE).
Statistical Analysis
Descriptive statistics were calculated for all study variables. Quantitative variables were summarized as median and range and categorical variables as frequencies and percentages.
Results
Fifteen patients were admitted at the Department of Cardiology, Boston Children's Hospital for management of myocarditis after COVID-19 vaccination between May 1 and July 15, 2021. The median age was 15 years (range, 12-18 years), and most patients were male (n = 14 [93%]). Patients self-identified as non-Hispanic White (n = 8 [53%]), Hispanic White (n = 2 [15%]), other Hispanic (n = 1 [8%]), other non-Hispanic (n = 1 [8%]), and unknown (n = 3 [20%]) (Table). All patients received the BNT162b2 mRNA vaccine. Symptoms occurred after the second dose of the vaccine in all but 1 case. No patients had a known prior COVID-19 infection, although 1 had reactive SARS-CoV-2 antibodies to the nucleocapsid protein.
Table. Characteristics of 15 Patients With Myocarditis After COVID-19 Vaccine.
| Characteristic | Median (range) | |
|---|---|---|
| At time of admission | Outpatient follow-up | |
| Age, y | 15 (12 to 18) | NA |
| Sex, No. (%) | ||
| Male | 14 (93) | NA |
| Female | 1 (7) | NA |
| Onset of symptom after vaccine, d | 3 (1 to 6) | NA |
| Race/ethnicity, No. (%) | ||
| Non-Hispanic White | 8 (53) | NA |
| Hispanic White | 2 (15) | NA |
| Other Hispanica | 1 (8) | NA |
| Other non-Hispanica | 1 (8) | NA |
| Unknowna | 3 (20) | NA |
| Day at follow-up, d | NA | 6 (1 to 13) |
| Duration of symptoms, d | 3 (1 to 9) | NA |
| Chest pain, No. (%) | 15 (100) | 1 (7) |
| Fever, No. (%) | 10 (67) | 0 (0) |
| Myalgia, No. (%) | 8 (53) | 0 (0) |
| Headache, No. (%) | 6 (40) | 0 (0) |
| Fatigue, No. (%) | 6 (40) | 3 (20) |
| Duration of hospitalization, d | 2 (1 to 5) | NA |
| Immunomodulatory treatment, No. (%) | 7 (47) | 7 (47) |
| Laboratory values | ||
| Troponin level, ng/mL (normal ≤0.01) | 0.25 (0.08 to 3.15) | 0.01 (0.01 to 0.16) |
| BNP, pg/mL (normal <10) | 22 (10 to 184) | 12 (10 to 64) |
| CRP, mg/dL (normal ≤0.50) | 3.01 (0.69 to10.00) | 0.24 (0.03 to 0.86) |
| ECG | ||
| Diffuse ST segment elevation, No. (%) | 9 (60) | 6 (40) |
| T-wave inversion, No. (%) | 0 (0) | 3 (30) |
| Echocardiogram | ||
| Ejection fraction (%) | 58.6 (43.7 to 64.7) | 59.3 (54.4 to 71.5) |
| Circumferential strain (%) | −23.4 (−34.2 to −15.3) | −28.8 (−35.0 to −23.2) |
| Circumferential strain z score | −1.8 (−4.0 to 1.1) | −0.3 (−1.9 to 1.4) |
| Longitudinal strain (%) | −19.2 (−26.8 to −11.1) | −20.7 (−24.4 to −15.1) |
| Longitudinal strain z score | −0.9 (−3.3 to 1.8) | −0.3 (−2.0 to 1.0) |
| Septal e', cm/s | 12.6 (11.0 to 18.2) | 13.0 (9.4 to 18.4) |
| Septal e' z score | −0.5 (−1.3 to 2.2) | −0.4 (−2.0 to 2.2) |
| Septal E/e' ratio | 6.9 (5.0 to 8.4) | 7.9 (4.1 to 10.1) |
| Septal E/e' ratio z score | −0.1 (−1.2 to 0.9) | 0.6 (−1.8 to 1.9) |
| Lateral e', cm/s | 15.3 (11.1 to 22.7) | 16.9 (10.4 to 25.6) |
| Lateral e' z score | −1.3 (−2.7 to 1.3) | −0.7 (−2.8 to 2.3) |
| Lateral E/e' ratio | 5.9 (3.0 to 7.6) | 5.7 (3.4 to 9.2) |
| Lateral E/e' ratio z score | 0.5 (−1.4 to 1.7) | 0.4 (−1.2 to 2.6) |
| Cardiac MRI | ||
| Time from onset of symptoms, d | 3 (1 to 7) | NA |
| Regional hyperintensity on T2-weighted imaging, No. (%) | 2 (13) | NA |
| Extracellular volume fraction (%) | 27 (22 to 37) | NA |
| LV global T2, ms | 51.5 (47.0 to 57.6) | NA |
| LV global native T1, ms | 1048 (963 to 1121) | NA |
| Late gadolinium enhancement, No. (%) | 12 (80) | NA |
Abbreviations: BNP, brain natriuretic peptide; CRP, C-reactive protein; e′, early diastolic tissue Doppler velocity; E, mitral inflow early diastolic pulsed-Doppler velocity; ECG, electrocardiogram; LV, left ventricular; MRI, magnetic resonance imaging; T2, transverse relaxation time; T1, longitudinal relaxation time.
SI conversion factors: To convert BNP to nanograms per liter, multiply by 1; CRP to milligrams per liter, multiply by 10; and troponin to micrograms per liter, multiply by 1.0.
Race/ethnicity was self-reported by patients or parents according to the US Census categories6 and were collected because of their known association with COVID-19–related illnesses.
Chest pain in 15 of 15 patients (100%) started at median 3 days (range, 1-6 days) after receiving the vaccine and lasted 1 to 9 days. Other symptoms included fever in 10 patients (67%), myalgia in 8 patients (53%), and headache in 6 patients (40%). Seven patients (47%) were treated with intravenous immunoglobulins (2 g/kg) and methylprednisolone (1 mg/kg/dose twice a day, transitioned to prednisone at time of discharge). Hospital length of stay was a median of 2 days (range, 1-5 days), and no patients required intensive care unit admission.
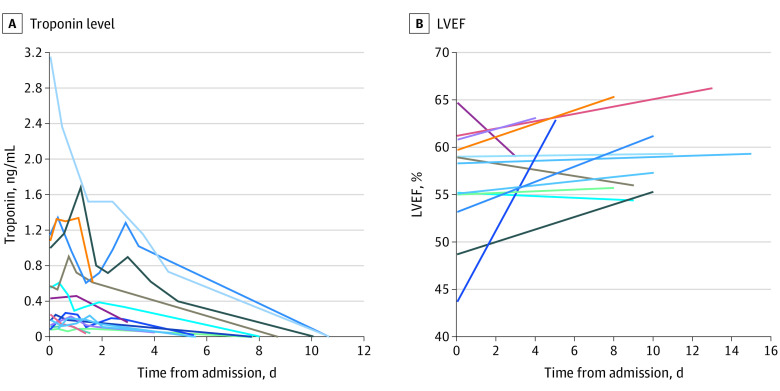
Troponin
Troponin levels were elevated in all patients at admission (median, 0.25 ng/mL [range, 0.08-3.15 ng/mL]) and peaked 0.1 to 2.3 days after admission (Table). At the time of discharge, the troponin level had substantially decreased but remained elevated in all patients (Figure 1).
Figure 1. Troponin Level and Left Ventricular Ejection Fraction (LVEF).
A, Troponin level during hospital admission and follow-up. B, LVEF during hospital admission and follow-up. Each line represents values over time for separate patients.
SI conversion factor: To convert troponin to micrograms per liter, multiply by 1.0.
Echocardiogram
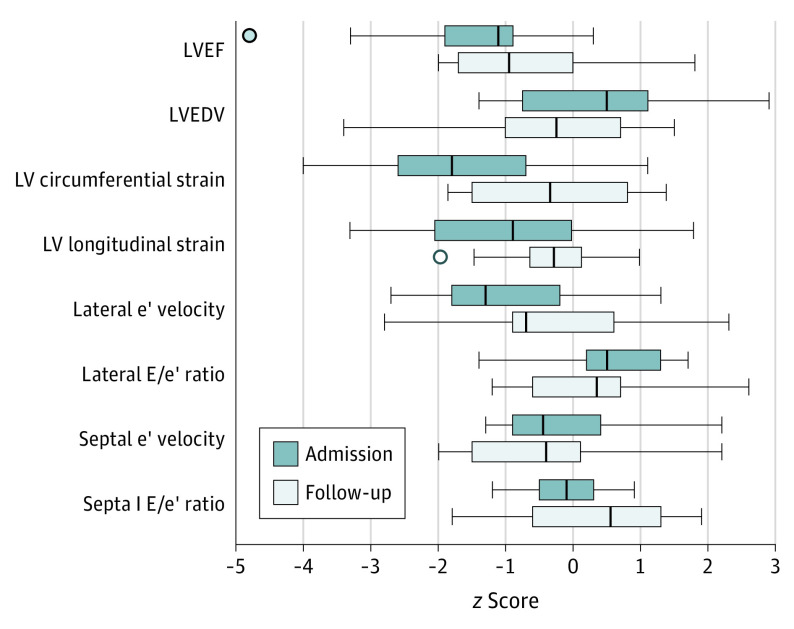
On admission echocardiogram, 3 patients (20%) had global LV systolic ventricular dysfunction (EF 44%, 49%, and 53%), one of whom also had regional wall motion abnormality at the apex. Two patients (13%) with systolic dysfunction had abnormal diastolic function indices, and 1 patient (7%) with borderline EF (55%) had evidence of diastolic dysfunction. Five patients (33%) had abnormal global longitudinal or global circumferential strain (Figure 2; eFigure 1 and eTable in the Supplement). No patients had a coronary artery aneurysm or pericardial effusion.
Figure 2. z Scores at Time of Hospital Admission and Follow-up.
Boxes indicate the 25th percentile, median, and 75th percentile. Dots represent outliers. Whiskers indicate the minimum and maximum ranges. LV indicates left ventricular; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction.
Electrocardiogram
The most frequent finding was diffuse ST-segment elevation consistent with pericarditis, present on admission in 6 patients (40%), and at some time during hospital admission in 8 patients (53%). Four additional patients had nonspecific ST segment changes. One patient (normal systolic and diastolic ventricular function; LGE on CMR) had nonsustained ventricular tachycardia during hospital admission. ST-T wave changes persisted at time of hospital discharge in 9 patients (69%). No patient had PR interval, QRS duration, or QTc duration prolongation.
Cardiac Magnetic Resonance
CMR imaging was performed in all patients 1 to 7 days after the onset of symptoms. Systolic LV dysfunction was present in 3 patients (25%). Findings consistent with myocarditis were found in 13 patients (87%). LGE was present in 12 patients, and most often found in the inferolateral (n = 3) and anterolateral (n = 4) regions (eTable and eFigure 2 in the Supplement). The extracellular volume fraction was borderline elevated (28%-30%) in 4 patients (27%) and elevated (>30%) in 3 patients (25%). LV global native T1 was borderline elevated (1080-1100 milliseconds) in 2 patients and elevated (>1100 milliseconds) in 2 patients. Two patients had regional hyperintensity on T2-weighted imaging. LV global T2 was borderline elevated (56-60 milliseconds) in 1 patient.
Follow-up
Follow-up information after hospital discharge was available for all patients (virtual visit in 1 patient; in-person with testing in 14 patients) and occurred 1 to 13 days after discharge. Four patients (27%) were asymptomatic with normal troponin level, ECG, and echocardiogram results.
Four patients (27%) had persistent symptoms, including fatigue in 3 patients (25%) and continued chest pain in 1 patient (7%). None of the patients with persistent symptoms had decreased EF at time of initial presentation (1 with abnormal strain) and 3 patients (75%) had abnormal CMR results with LGE.
One asymptomatic patient (7%) had persistent borderline low LV EF (54%), reduced circumferential strain (z score, −2.3), and reduced lateral e′ velocity (z score, −2.8) measured by echocardiogram at 8 days after discharge; all other patients had normal echocardiogram results. Ventricular systolic function recovered (EF>55%) in 2 to 11 days (Figure 1).
ECG changes persisted in 4 patients (33%) and included nonspecific ST-T wave changes in 4 patients (33%) or new T-wave inversion in 3 patients (20%). One patient (7%) with nonsustained ventricular tachycardia during hospital admission had recurrence of nonsustained ventricular tachycardia on 6 days of ambulatory ECG monitoring, despite initiation of β-blocker therapy.
Troponin levels remained mildly elevated at follow-up in 3 patients (20%) (Figure 1). One patient (7%) with a persistently elevated troponin level (0.05 ng/mL) had continuing fatigue. All patients with persistently elevated troponin levels had had prior abnormalities on CMR (2 patients with LGE, 1 patient with elevated extracellular volume fraction).
Discussion
In this early experience of 15 cases, myocarditis typically occurred in male patients after the second dose of the COVID-19 vaccine. All patients in this series had a benign course; none required intensive care unit admission and all were discharged alive from the hospital within 5 days. LV systolic function at presentation was normal in most patients and normalized within a few days in all but 1 patient who had persistent borderline low LV function. This finding differs from other forms of myocarditis in which LV systolic dysfunction and arrhythmias are more common, with 50% of children requiring intensive care unit admission, a mean hospital length of stay of 14.4 days, and a mortality rate of 7.8%.7,8,9
Although vaccine-associated cases of myocarditis to date have had uncomplicated short-term course, the long-term prognosis remains unclear. Of note, CMR LGE was a frequent finding at time of diagnosis. In this clinical setting, LGE reflects an increased volume of distribution of the gadolinium-based contrast agent in the affected region likely related to myocyte necrosis and/or extracellular edema. In nonvaccine-associated myocarditis, the presence of LGE is associated with increased risk for adverse cardiovascular events during follow-up.10,11,12 Thus, longitudinal studies of patients with myocarditis after COVID-19 vaccine will be important to better understand long-term risks.
To date, there have been 1226 reports of myocarditis after messenger RNA vaccination to the Vaccine Adverse Event Reporting System (VAERS), including 687 in persons aged less than 30 years.13 Crude reporting rates using vaccine administration data estimates the highest rate among male individuals aged 12 to 17 years (62.8 cases per million), similar to our observations. Despite the risks of myocarditis associated with vaccination, the benefits of vaccination likely outweigh risks in children and adolescents. It is estimated that COVID-19 vaccination in males aged 12 to 29 years can prevent 11 000 COVID-19 cases, 560 hospitalizations, 138 intensive care unit admissions, and 6 deaths compared with 39 to 47 expected myocarditis cases.
Limitations
This study has limitations. Limitations to this series include the lack of COVID-19 vaccine administration data, which does not permit calculation of incidence or identification of risk factors for myocarditis. Mild cases may have been missed due to the novelty of this complication and the lack of routine screening.
Conclusions
Myocarditis may be a rare complication after COVID-19 vaccination in patients aged less than 19 years. In this case series study, the short-term clinical course was mild in most patients; however, the long-term risks remain unknown. Risks and benefits of COVID-19 vaccination must be considered to guide recommendations for vaccination in this population.
eFigure 1. A) Peak Global Circumferential and B) Peak Global Longitudinal Strain During Hospital Admission and Follow-up
eFigure 2. Cardiac Magnetic Resonance Short and Long-Axis Views Showing Late Gadolinium Enhancement in the Basal Inferolateral Left Ventricular Segment
eTable. Detailed Characteristics of Patients With Myocarditis Following COVID-19 Vaccine
References
- 1.Food and Drug Administration . Emergency Use Authorization letter for Pfizer-BioNTech COVID-19 Vaccine. May 10, 2021. Accessed July 1, 2021. https://www.fda.gov/media/144412/download
- 2.Engler RJ, Nelson MR, Collins LC Jr, et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS One. 2015;10(3):e0118283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shay DK, Shimabukuro TT, DeStefano F. Myocarditis occurring after immunization with mRNA-based COVID-19 vaccines. JAMA Cardiol. Published online June 29, 2021. doi: 10.1001/jamacardio.2021.2821 [DOI] [PubMed] [Google Scholar]
- 4.Montgomery J, Ryan M, Engler R, et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. Published online June 29, 2021. doi: 10.1001/jamacardio.2021.2833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshall M, Ferguson ID, Lewis P, et al. Symptomatic acute myocarditis in seven adolescent following Pfizer-BioNTech COVID-19 vaccination. Pediatrics. Published online June 4, 2021. doi: 10.1542/peds.2021-052478 [DOI] [PubMed] [Google Scholar]
- 6.United States Census Bureau : Race. Accessed July 16th, 2021. https://www.census.gov/quickfacts/fact/note/US/RHI625219
- 7.Foerster SR, Canter CE, Cinar A, et al. Ventricular remodeling and survival are more favorable for myocarditis than for idiopathic dilated cardiomyopathy in childhood. Circ Heart Fail. 2010;3(6):689-697. [DOI] [PubMed] [Google Scholar]
- 8.Anderson BR, Silver ES, Richmond ME, Liberman L. Usefulness of arrhythmias as predictors of death and resource utilization in children with myocarditis. Am J Cardiol. 2014;114(9):1400-1405. [DOI] [PubMed] [Google Scholar]
- 9.Klugman D, Berger JT, Sable CA, He J, Khandelwal SG, Slonim AD. Pediatric patients hospitalized with myocarditis. Pediatr Cardiol. 2010;31(2):222-228. [DOI] [PubMed] [Google Scholar]
- 10.Aquaro GD, Perfetti M, Camastra G, et al. ; Cardiac Magnetic Resonance Working Group of the Italian Society of Cardiology . Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function. J Am Coll Cardiol. 2017;70(16):1977-1987. [DOI] [PubMed] [Google Scholar]
- 11.Yang F, Wang J, Li W, et al. The prognostic value of late gadolinium enhancement in myocarditis and clinically suspected myocarditis. Eur Radiol. 2020;30(5):2616-2626. [DOI] [PubMed] [Google Scholar]
- 12.Imazio M, Angelico G, Andriani M, et al. Prevalence and prognostic impact of septal late gadolinium enhancement in acute myocarditis with or without preserved left ventricular function. Am J Cardiol. 2018;122(11):1955-1958. [DOI] [PubMed] [Google Scholar]
- 13.Gargano JW, Wallace M, Hadler SC, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients. MMWR Morb Mortal Wkly Rep. 2021;70(27):977-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. A) Peak Global Circumferential and B) Peak Global Longitudinal Strain During Hospital Admission and Follow-up
eFigure 2. Cardiac Magnetic Resonance Short and Long-Axis Views Showing Late Gadolinium Enhancement in the Basal Inferolateral Left Ventricular Segment
eTable. Detailed Characteristics of Patients With Myocarditis Following COVID-19 Vaccine