Abstract
Vesicouterine fistula is one of the rare varieties of urogenital fistula. Type I urogenital fistula or Youssef syndrome is characterised by menouria, amenorrhoea and urinary continence and it mostly follows lower segment caesarean delivery. There are only scattered case reports to help guide diagnostic and therapeutic options for this condition. These patients mostly need a combination of diagnostic modalities to confirm the diagnosis. Here, we present one such case of para 4 live 4 with classical symptoms of Youssef syndrome following a laparotomy for uterine rupture repair. CT urography confirmed the diagnosis and cystoscopy helped localise the exact location. Transabdominal fistula excision and repair was done. The paper also presents a summary of diagnostic and therapeutic options for this condition as reported in previous case reports for easy reference for practising gynaecologists and urologists.
Keywords: urinary and genital tract disorders, heamaturia, urological surgery, obstetrics and gynaecology
Background
Youssef syndrome, which was a rare entity, has now become a frequent complication with increasing rates of lower segment caesarean delivery. Classically, the syndrome is characterised by menouria or efflux of menstrual blood with urine periodically, amenorrhoea and urinary continence as described by Youssef in 1957.1 The presentation may not be typical always with some degree of urinary incontinence in few. Women might present with this complication at varied times, even years after the inciting event such as caesarean delivery. Here, we describe one such case from our institution. Also, the authors have reviewed the available literature and presented a summary of management options observed so far.
Case presentation
A 32-year-old multiparous home maker presented to us with complaints of cyclical haematuria and amenorrhoea following a laparotomy for uterine rupture repair after vaginal birth 1 year ago. She has had two caesarean deliveries, 10 and 6 years ago, and a vaginal birth after caesarean section, 4 years ago prior to this. There was no history of any urinary leak or symptoms of urinary tract infection. General physical examination and pelvic examination revealed no abnormality and all haematological and hormonal parameters were within normal limits.
Investigations
Ultrasonography (USG) of the pelvis detected no abnormality. With suspicion of urogenital fistula, she was subjected to CT urography which revealed contrast opacified fistulous tract between anterior uterine wall and posterior wall of urinary bladder measuring 1.7 cm in maximum thickness suggestive of vesicouterine fistula (figure 1).
Figure 1.
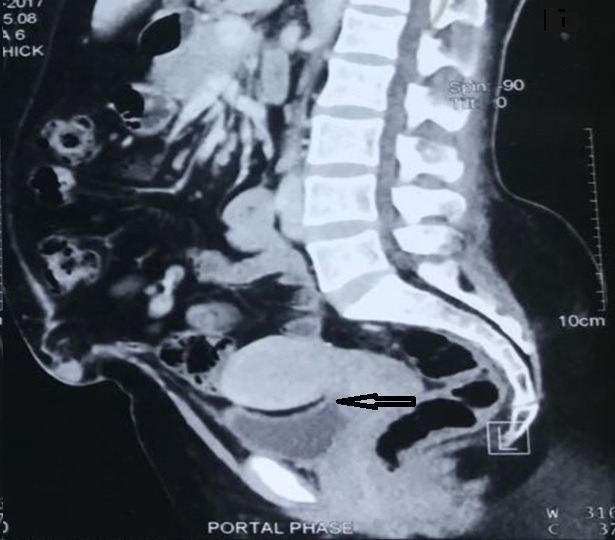
CT urography with contrast suggestive of vesicouterine fistula (black arrow).
Differential diagnosis
The clinical impression of urogenital fistula was thus confirmed by CT urography. The authors considered vesical endometriosis as a differential diagnosis but it could not explain the reason for amenorrhoea.
Treatment
Management was done with a multidisciplinary approach comprising of gynaecologist and urologists. Intraoperatively, cystoscopy was done which revealed a 2×2 cm supratrigonal fistula 4 cm away from ureteric orifice (figure 2). A transabdominal approach was used for exploration and repair of fistula. A 2×2 cm fistula was visualised connecting anterior wall of uterus with posterior wall of bladder, which was excised. After adequate mobilisation, bladder defect was closed in two layers and uterine rent was repaired. An omental patch was placed between the two stitch lines.
Figure 2.
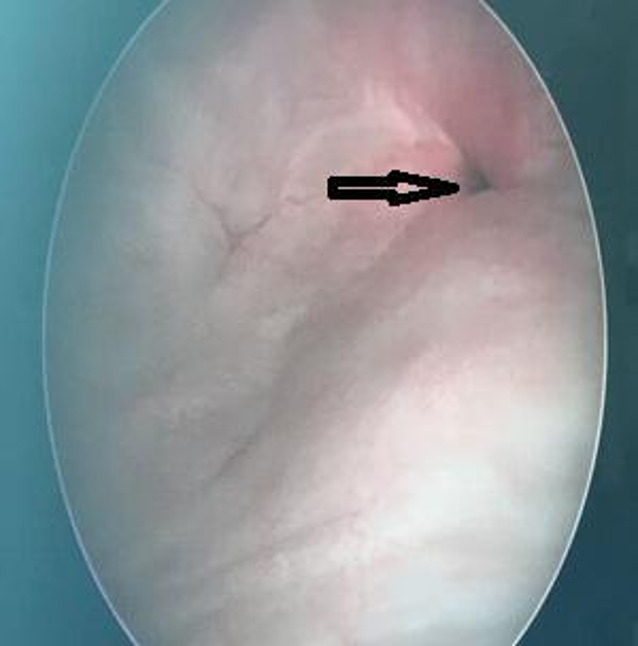
Cystoscopy finding of 2×2 cm supratrigonal fistula (black arrow).
Outcome and follow-up
Postoperatively, bladder catheterisation was continued for 14 days following which the patient had normal voiding habits. On follow-up, the patient was found to have regular menstrual cycles with no other complaints for 3 years now.
Discussion
Since the time Youssef described a set of symptoms characterising a particular variety of vesicouterine fistula called the Youssef syndrome, many cases have been reported with similar or slightly varied features. Józwik and Józwik further analysed different types of vesicouterine fistula and classified them into three types.2 Type I or Youssef syndrome is characterised by amenorrhoea, menouria and complete continence of urine. Type II is menouria, vaginal menses and constant or periodic incontinence of urine and type III is normal vagina menses and constant or periodic incontinence of urine. All three types more or less need similar diagnostic and therapeutic modalities. These fistulae are a result of many inciting events, most common being the lower segment caesarean delivery. It could be due to inadequate mobilisation, direct injury, suturing of bladder with uterus, devascularisation, haematoma or infection.3 Other causes are instrumental vaginal delivery, prolonged labour, placenta percreta, anterior colporrhaphy, radiotherapy, invasive malignancy, embolisation, trauma, migration of intrauterine device, tuberculosis and cervical cerclage.3
The reason for urinary continence and unidirectional flow of urine and menstrual blood could be the location of fistula, that is, supraisthmic, wherein isthmus acts as a sphincter or could be due to pressure difference in the two cavities wherein the intrauterine pressure is higher than intravesical pressure.4 When studied at microscopic level, the vesicouterine fistulae are said to have an endometrial lining at the uterine end which explains the possibility of success with hormonal management for the closure.5 6
The diagnosis of this condition requires high degree of suspicion as the inciting event could have happened years ago. Commonly used modalities include USG, cystoscopy, hysterosalpingography, MRI, CT urography and colour Doppler. A combination of these investigations will give a confirmation of diagnosis. Smaller fistulas can close spontaneously or with continuous bladder drainage. Other non-surgical options are hormonal treatment and cystoscopic fulguration. With surgical management transabdominal approach is required as the location of the fistula is high-up. It can be via laparotomy or minimal access. Time of repair is generally 3 months after the event to allow for the resolution of inflammation and oedema. Commonly used technique of repair is O’Connor method where fistula is excised and bladder and uterine rents are adequately mobilised and repaired individually. An omental flap can be placed between the two for better vascularisation. Postoperatively, duration of bladder drainage depends on the degree of repair and can be via per urethral catheterisation with or without suprapubic drainage.
The available literature on this condition comprise mostly of scattered case reports. The authors of this paper attempted to review about 50 such case reports. If not typical of type I vesicouterine fistula or Youssef syndrome, all cases were description of vesicouterine fistula of varying degrees. Cases representing all possible diagnostic and therapeutic options were selected and summarised for future easy reference in table 1.
Table 1.
Summary of management options
| Sl. no | Title | Age (years) | Symptoms | Preceding event | Diagnostic modality and finding | Management | Surgical technique | Postoperative bladder drainage | Follow-up |
| 1 | Pregnancy with neglected Youssef syndrome a case report7 | 29 | 18 weeks pregnancy with haematuria | Cyclical haematuria following third CS 3 years ago | MRI: linear tract visualised between the two cavities Cystoscopy: membrane seen bulging through the defect in bladder on evacuation of bladder |
Laparotomy, hysterotomy and evacuation of products of conception followed by repair of uterus and bladder | O’Connor’s technique with omental flap | Bladder catheter for 3 weeks | No urinary incontinence or haematuria |
| 2 | A case of vesicouterine fistula: unwanted medical anomaly but consequentiality of most-wanted medical intervention ‘caesarean section’8 | 35 | Cyclical haematuria, amenorrhoea and recurrent UTI since 6 years from 11th postoperative day | Second CS 6 years ago | TAS: endometrial fluid communicating with bladder IVU: right pyelonephritis Cystoscopy: fistulous opening in supratrigonal region |
Laparotomy, hysterectomy and bladder repair | Trilayered closure of bladder with 2–0 vicryl | 24 hours bladder irrigation with suprapubic catheter and perurethral catheter. Suprapubic catheter was removed on day 10 |
Cystoscopy after 2 months: healthy scar No symptoms |
| 3 | Vesicouterine fistula (Youssef syndrome): case report and literature review3 |
38 | Continuous haematuria from day 1 postoperative for 3 months followed by cyclical haematuria from 6 months postoperative to 1 year. Two episodes of urethral obstruction requiring catheterisation | Third caesarean 2 years ago | Cystoscopy: fistulous opening | History of relief in symptoms for 1 year during combined oral contraceptive intake Hysterectomy and repair of bladder |
Two-layered closure of bladder | Bladder catheter for 14 days | 2 years since surgery: no symptoms |
| 4 | Youssef’s syndrome9 | 26 | Amenorrhoea and intermittent red urine since 2 ½ years came for tubal ligation reversal | Second CS 2½ years ago | Transcervical instillation of methylene blue: blue urine Sonohysterosalpingography and colour Doppler: no fluid in uterine cavity and tube but in bladder Hysteroscopy: bladder Foley’s catheter seen Cystoscopy: blue dye instilled through cervix seen entering into bladder IVP: normal |
Transabdominal excision of fistula and repair and tubal ligation reversal | Two-layered closure of bladder with 2–0 polyglactin and single-layer closure of uterus with no. 1 polyglactin and omental patch in between | Bladder catheter for 2 weeks | Normal menses and clear urine |
| 5 | Youssef’s syndrome following cesarean section10 | 40 | Urinary incontinence, haematuria and amenorrhoea | CS 1 year ago | TVS: normal Methylene blue though urethral Foley’s catheter: leak though cervical os IVP: normal Cystoscopy: fistula on posterior bladder wall; catheter pushed through this came out of cervical os |
Laparotomy and extraperitoneal approach for fistula excision and repair | O’Connor technique Bladder and uterine mucosa closed by two layers with 2–0 polyglycolic suture |
Urethral Foley’s catheter for 14 days | – |
| 6 | Post-caesarean vesicouterine fistula: Youssef’s syndrome – A case report11 | 31 | Cyclical haematuria and secondary amenorrhoea for 2 years | Second CS 3 years ago | USG: normal HSG: Immediate filling of bladder through fistulous tract; uterine cavity not demonstrated |
Transabdominal transperitoneal repair | Bladder was repaired with vicryl 2–0 in two layers and uterus repaired in two layers | Urethral catheter for 2 weeks | Regular menstrual cycles and no urinary complaints. Postoperative HSG: normal |
| 7 | Vesicouterine Fistula (Youssef’s syndrome): Imaging Findings12 |
28 | Urinary leak | CS 2 months ago | Methylene blue test: positive Excretory urography: endometrial cavity opacified Pelvic CT: uterine and vaginal cavity opacification; no definite fistula Hysterography: 5 mm sized fistula between uterus and bladder Cystoscopy: fistula demonstrated |
Cystoscopic fulguration of fistula | – | Transurethral catheter for 4 weeks | No urine incontinence but cyclic haematuria; open surgical repair done |
| 8 | Cystographic images of Youssef syndrome: flower on top of the bladder13 |
38 | Continuous urinary incontinence for 13 years | Obstructed labour and vaginal delivery of stillborn neonate | IVU: normal upper tracts and small capacity bladder Cystogram: bilateral grade 2 vesicoureteral reflux and reflux into uterus; flower pot appearance Cystoscopy: vesicovaginal fistula and another opening into uterine cervix |
Continent urinary diversion | – | – | – |
| 9 | A rare case of nocturnal urinary incontinence and menuria after lower segment cesarean section14 |
23 | Chronic pelvic pain, nocturnal bedwetting and cyclic haematuria during periods since 2 years | CS 2 years ago for prolonged second stage of labour followed by bladder cathetrisation for 45 days due to haematuria | USG: normal Diagnostic hysterolaparoscopy and cystoscopy: small depression in posterior bladder wall; methylene blue injected though cervix to see spillage: negative; biopsy taken from the depression: endometrial glands Laparotomy: no fistulous tract |
Injection leuprolide 1.25 mg for 3 months | – | – | After periods resumed: urinary incontinence resolved and no menouria |
| 10 | Vesicouterine fistula: Youssef’s syndrome15 | 28 | Cyclical haematuria (menouria) and secondary amenorrhoea since 4 years, occasional wetting of vagina | CS for non-progress of labour followed by catheterisation for 2 weeks for haematuria | USG: normal MRI: fistulous communication between bladder and uterus Cystoscopy and hysteroscopy: fistula at supratrigonal and supraisthmic region |
Transabdominal tranvesical VUF repair; both ureters canalised | Uterus closed with no. 1 polyglactin suture transversely and bladder closed in two layers with no. 2 and no. 3 polyglactin sutures. Vesicouterine periotneum closed to act as transposition | Suprapubic followed by perurethral catheter removed after 3 weeks GnRH analogues given |
4 weeks: MRI: well-defined hypointense scar Regular menstrual cycles and no urinary complaints |
| 11 | Treatment of vesicouterine fistula by fulguration16 | 29 | Leakage of urine few days after delivery for 2 months followed by bladder catheterisation for 2 months | Second CS 4 months ago | Cystogram: fistulous tract between bladder and uterus Cystoscopy: a small epithelialised fistula orifice cannulated with 5F catheter |
Fistula thoroughly fulgurated with 6F fulgurating electrode | – | Foley’s catheter for 6 weeks | 6 weeks: cystogram: no fistula 9 months: no urinary leakage |
| 12 | Youssef syndrome: an appraisal of hormonal treatment17 | 28 25 |
Case 1: amenorrhea and episodes of haematuria Case 2: amenorrhoea and cyclical menouria for 9 months |
Case 1: CS followed by haematuria which cleared after a week Case 2: CS 9 months back |
Case 1: IVU: leak of contrast medium into uterus during cystogram phase Hysterogram: fistula from uterus to bladder Cystoscopy: supratrigonal irregular opening of 12 mm Case 2: IVU: normal Hysterography: leakage of contrast into bladder Cystoscopy: 3 mm fistula above trigone |
Case 1: levonorgesterol 0.25 mg and ethinyl estradiol 0.05 mg Case 2: levonorgesterol 0.25 mg and ethinyl estradiol 0.05 mg for 6 months |
– | – | Case 1: dose doubled after 3 months due to breakthrough bleeding; did not work; surgery with transabdominal transperitoneal approach Case 2: 6 months: normal menses with non-haematuria |
CS, caesarean section; GnRH, gonadotropin releasing hormone; HSG, hysterosalpingography; IVP, intravenous pyelography; IVU, intravenous urogram; TAS, transabdominal sonography; TVS, transvaginal sonography; USG, ultrasonography; UTI, urinary tract infection; VUF, vesicouterine fistula.
Patient’s perspective.
I was only 32 years old and not having menses. Family, friends and some local doctors were of the opinion that I had attained an early menopause and it was okay as I already had three children. Though the recurrent blood in urine was bothering me, I was reassured that it was nothing but slight infection of the urine. Then, I came to this hospital for confirmation that it is all okay. Here, the doctors suspected some problem and got CT scan done for me. I was surprised with the diagnosis but I am happy that after the surgery I have no urinary problems with normal periods like before.
Learning points.
Vesicouterine fistula is mostly an iatrogenic complication with lower segment caesarean section as the most common cause.
It stresses the importance of surgical skills and surgical principles.
With type I vesicouterine fistula or Youssef syndrome the patients may not present sooner as there is no urinary incontinence.
High degree of suspicion if required to make a diagnosis. The management is mostly surgical with excision of fistula and repair of bladder and uterus. Hysterectomy can be combined with repair if indicated.
After histopathological evidence of oestrogen receptors in the fistula lining, hormonal management has become an area of interest.
Footnotes
Contributors: AB and RM managed the case. AKR and MA prepared the manuscript. AB and AKR critically revised the manuscript. All authors accepted the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Youssef AF. Menouria following lower segment cesarean section; a syndrome. Am J Obstet Gynecol 1957;73:759–67. 10.1016/0002-9378(57)90384-8 [DOI] [PubMed] [Google Scholar]
- 2.Józwik M, Józwik M. Clinical classification of vesicouterine fistula. Int J Gynaecol Obstet 2000;70:353–7. 10.1016/S0020-7292(00)00247-2 [DOI] [PubMed] [Google Scholar]
- 3.Machado Junior RA, Machado Junior LC, Lourenço LLE. Vesicouterine fistula (Youssef syndrome): case report and literature review. Rev Bras Ginecol Obstet 2018;40:563–9. 10.1055/s-0038-1666998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingelman-Sundberg A. The effect of urine on the endometrium. Int J Gynaecol Obstet 2007;99:4–5. 10.1016/j.ijgo.2007.05.001 [DOI] [PubMed] [Google Scholar]
- 5.Józwik M, Józwik M. Hormonal dependence of fistulas communicating with the uterus. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:719–20. 10.1007/s00192-007-0311-2 [DOI] [PubMed] [Google Scholar]
- 6.Józwik M, Józwik M, Sulkowska M, et al. The presence of sex hormone receptors in the vesicouterine fistula. Gynecol Endocrinol 2004;18:37–40. 10.1080/09513590310001651768 [DOI] [PubMed] [Google Scholar]
- 7.Ohri DS, Ohri DN, Ray DN. Pregnancy with neglected Youssef syndrome a case report. Int J Clin Obstet Gynaecol 2019;3:196–8. 10.33545/gynae.2019.v3.i1d.32 [DOI] [Google Scholar]
- 8.Bakshi K, Lokam K, Sasikumar J. A case of vesicouterine fistula: unwanted medical anomaly but consequentiality of most-wanted medical intervention 'caesarean section'. J Clin Diagn Res 2014;8:189–90. 10.7860/JCDR/2014/5733.3940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shinde G, Rathod K, Dedhia M. Youssef’s Syndrome. Bombay Hosp J 2011;53:681–3. [Google Scholar]
- 10.Birge O, Ozbey EG, Erkan MM, et al. Youssef's syndrome following cesarean section. Case Rep Obstet Gynecol 2015;2015:605325. 10.1155/2015/605325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taingson M, Adze J, Bature S, et al. Post-caesarean vesicouterine fistula: Youssef’s syndrome – A case report. Arch Int Surg 2017;7:132–4. 10.4103/ais.ais_40_17 [DOI] [Google Scholar]
- 12.Karadeli E, Kayahan Ulu EM, Tarhan NC. Vesicouterine Fistula (Youssef’s syndrome): Imaging Findings. Yeditepe Medical Journal 2008:137–41. [Google Scholar]
- 13.Goel A, Goel S, Singh BP, et al. Cystographic images of Youssef syndrome: flower on top of the bladder. Urology 2012;79:e69–70. 10.1016/j.urology.2012.01.032 [DOI] [PubMed] [Google Scholar]
- 14.Chaudhry P, Shrivastava DS, Bhute S. A rare case of nocturnal urinary incontinence and Menuria after lower segment cesarean section. J Med Sci 2016;2:23–5. 10.5005/jp-journals-10045-0029 [DOI] [Google Scholar]
- 15.Bhattacharjee S, Kohli UA, Sood A, et al. Vesicouterine fistula: Youssef's syndrome. Med J Armed Forces India 2015;71:S175–7. 10.1016/j.mjafi.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Molina LR, Lynne CM, Politano VA. Treatment of vesicouterine fistula by fulguration. J Urol 1989;141:1422–3. 10.1016/S0022-5347(17)41333-4 [DOI] [PubMed] [Google Scholar]
- 17.Hemal AK, Wadhwa SN, Kriplani A, et al. Youssef's syndrome: an appraisal of hormonal treatment. Urol Int 1994;52:55–7. 10.1159/000282572 [DOI] [PubMed] [Google Scholar]


