Abstract
Introduction:
This study explored whether structural stigma, defined by U.S. state policies related to sexual minority rights, moderated the relationship between sexual identity identity and heavy drinking, alcohol problems, and marijuana use among men and women.
Methods:
Using combined data from the National Alcohol Survey (NAS) series (2000, 2005, 2010, and 2015), the sample included 11,115 men (421 sexual minority and 10,694 heterosexual) and 14,395 women (413 sexual minority and 13,982 heterosexual). State policy environment was assessed using a time-varying dichotomous indicator of comprehensive protections for sexual minorities (4–6 protections vs. limited or no protections). Gender-stratified logistic regression analyses examined the differential effect of the policy environment by sexual identity on three past-year substance use outcomes: high-intensity drinking (8+ drinks/day), any DSM-5 alcohol use disorder, and marijuana use.
Results:
Among women, sexual minority status was associated with increased odds of all alcohol and marijuana use outcomes. Among men, sexual minority status was associated with decreased odds of high-intensity drinking but increased use of marijuana. Comprehensive policy protections were associated significantly decreased odds of high-intensity drinking among sexual minority men and marginally significant decreases among women.
Conclusions:
Comprehensive policy protections appear to be protective for high-intensity drinking among sexual minority men and women. Findings underscore the importance of supportive policies in reducing risk of alcohol-related problems among sexual minorities.
Keywords: hazardous drinking, marijuana use, sexual minority, structural stigma, policy
Structural stigma has been identified as an under-acknowledged driver of health disparities.1–3 Structural stigma refers to norms and policies within societal, institutional, and cultural levels that negatively impact the opportunities, access, and well-being of a particular group.4 Changes in structural stigma, such as extending rights of legal marriage to same-sex couples, appear to reduce disparities. In 2015, the U.S. Supreme Court extended same-sex marriage rights to all states, providing access to legal marriage for same-sex couples living in states that had not yet extended, or explicitly banned, equal marriage rights. Prior to this change, studies found evidence of less psychological distress and better self-reported health among sexual minorities living in states that had previously provided access to legal marriage for same-sex couples compared to those living in states that did not.2,5–11 Similarly, studies in the United States and Australia found sexual minorities living in regions where more residents support same-sex marriage reported better health outcomes (e.g., lower disparities in smoking, better overall self-rated health, and better mental health) than sexual minorities living in regions with lower support.12,13 Such supportive policy contexts have significant positive impacts on sexual minority health, but generally have no impact or only modest positive impacts on health outcomes among heterosexual individuals.2,12–14
Cross-sectional, population-based research in the United States has documented greater risk for hazardous drinking and drug use among sexual minority adults compared to heterosexual adults.15–17 Differences in hazardous alcohol use (e.g., heavy episodic drinking, drinking at levels exceeding recommended guidelines, alcohol use disorders) are particularly pronounced and consistent among sexual minority women compared to heterosexual women,15,16,18 while differences in harmful use of alcohol by sexual identity are less consistent among men.19,20 Sexual minority women and sexual minority men have higher odds of using marijuana compared to heterosexual counterparts.15,21 Systematic reviews of sexual minority health inclusive of research from other countries have echoed these findings of elevated risk for hazardous drinking and drug use.22,23
Although recent studies based on a large, national prospective cohort study of adolescents suggest that living in state and local contexts with protective policies for sexual minorities may reduce disparities by sexual identity for alcohol, tobacco, or other drug use among adolescents,24,25 few studies based on probability samples have examined the impact of the policy environment on hazardous drinking or other drug outcomes among sexual minority adults. One notable exception was a study using two waves of cross-sectional data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), which found that alcohol use disorders increased by 41.9% among sexual minority adults living in states that explicitly banned same-sex marriage compared to states without such bans.2 This prior study used a dichotomous measure of institutional discrimination comparing states that voted on and passed constitutional amendments defining marriage as occurring only between a man and a woman to states that did not have such an amendment on the ballot. Documenting the harmful impact of institutional discrimination is important; however, studies using different policy measures are also needed to investigate whether protections against discrimination are protective against hazardous drinking or other negative health outcomes. Furthermore, this prior study did not stratify analyses by gender, which is an important limitation in the context of research documenting that disparities in risks for hazardous drinking and drug use are more pronounced and consistent among sexual minority women than sexual minority men compared to their heterosexual counterparts.26 The importance of disaggregating analyses by gender is demonstrated by a recent study of the impact of supportive policy environments on self-reported health among sexual minorities, which found that comprehensive policy protections were associated with better self-reported health for sexual minority men, but not sexual minority women.7
Research points to the value of using multiple indicators of social and political climates in examining the impact of structural stigma on minority health,7,24,27,28 particularly indicators that capture state-level anti-discrimination laws.27 In the context of gaps in the literature with respect to the impact of policy environments on substance use outcomes among sexual minority adults stratified by gender, the current study aims to examine the differential effects of state policy environments, defined by state policies protecting the rights of sexual minorities, on the relationship between sexual identity and hazardous drinking and marijuana use, separately among women and men. We hypothesized that environments with comprehensive policy protections would be associated with reduced odds of hazardous drinking and marijuana use among sexual minority women and men, and these policies would have no impact on hazardous drinking and marijuana use among heterosexual women and men.
METHODS
Data and Sample Characteristics
Data are from four waves (2000, 2005, 2010, and 2015) of the NAS, a cross-sectional probability survey of adults ages 18 or older in the United States. Data were collected prior to the 2015 U.S. Supreme Court decision that extended the rights of same-sex couples to marry across all states. Survey data contained oversamples of racial/ethnic minorities, and they were weighted to be representative of the U.S. population. The combined dataset contained data from 29,571 respondents; sexual minority status could be determined for 25,510 respondents. Sample characteristics are presented in Table 1 by gender and sexual identity.
TABLE 1.
Sample Characteristics by Gender and Sexual Identity (N = 25,510)
| Women (N = 14,395) | Men (N = 11,115) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Heterosexual (N = 13,982) | SMW (N = 413) | Heterosexual (N = 10,694) | SMM (N = 421) | |||||||
| n | % | n | % | n | % | n | % | |||
| Marital/relationship status | *** | *** | ||||||||
| Single, divorced, widowed | 6,742 | 39.4 | 258 | 55.8 | 3,788 | 32.2 | 296 | 62.8 | ||
| Married/living as a couple | 7,197 | 60.6 | 155 | 44.3 | 6,879 | 67.8 | 125 | 37.2 | ||
| Age | *** | |||||||||
| 18–39 | 4,271 | 39.2 | 190 | 60.5 | 3,982 | 43.1 | 163 | 49.2 | ||
| 40+ | 9,398 | 60.8 | 218 | 39.5 | 6,601 | 57.0 | 257 | 50.8 | ||
| Children in the household | *** | |||||||||
| No | 8,690 | 59.7 | 288 | 66.1 | 6,833 | 62.5 | 377 | 84.8 | ||
| Yes | 5,264 | 40.3 | 124 | 33.9 | 3,838 | 37.5 | 44 | 15.2 | ||
| Race and ethnicity | * | |||||||||
| White/Caucasian | 7,957 | 71.1 | 215 | 65.6 | 6,579 | 70.5 | 247 | 64.2 | ||
| Black/African | 2,930 | 11.7 | 101 | 13.5 | 1,631 | 10.4 | 77 | 16.4 | ||
| American | ||||||||||
| Hispanic | 2,572 | 11.5 | 73 | 10.8 | 1,961 | 12.7 | 76 | 11.5 | ||
| Other | 523 | 5.8 | 24 | 10.2 | 523 | 6.4 | 21 | 7.8 | ||
| Education | * | |||||||||
| High school or less | 5,709 | 40.3 | 186 | 42.9 | 4,215 | 41.1 | 123 | 32.0 | ||
| College or more | 8,217 | 59.7 | 227 | 57.1 | 6,427 | 58.9 | 298 | 68.0 | ||
| Employment | * | |||||||||
| Employed | 7,259 | 55.7 | 228 | 63.3 | 7,203 | 70.1 | 272 | 69.1 | ||
| Unemployed | 6,689 | 44.4 | 185 | 36.7 | 3,467 | 29.9 | 148 | 30.9 | ||
| Survey year | *** | *** | ||||||||
| 2000 | 3,794 | 28.4 | 86 | 20.1 | 3,284 | 28.5 | 84 | 16.2 | ||
| 2005 | 3,379 | 25.8 | 85 | 21.6 | 3,033 | 26.1 | 81 | 18.8 | ||
| 2010 | 3,734 | 25.0 | 91 | 22.8 | 2,320 | 25.3 | 107 | 27.8 | ||
| 2015 | 3,075 | 20.9 | 151 | 35.5 | 2,057 | 20.1 | 149 | 37.2 | ||
| State-level same-sex policy protections | ||||||||||
| Limited or none (−4 to 3) | 9,797 | 71.0 | 268 | 63.4 | * | 7,633 | 71.2 | 246 | 60.0 | *** |
| Comprehensive (4+) | 4,170 | 29.0 | 145 | 36.6 | 3,054 | 28.8 | 175 | 40.0 | ||
Note. The combined dataset contained data from 29,571 respondents; sexual minority status could be categorized for 25,510 respondents. SMW, sexual minority women (bisexual and lesbian identities). SMM, sexual minority men (bisexual and gay identities). Ten policy protections were scored as negative (−1), absent (0), or protective (+1). Valid percentages are listed; missing data was generally minimal. Unweighted cell sizes are presented, but prevalence estimates are weighted. Pearson chi-squared statistics comparing across sexual identity are corrected for the survey design with the second-order Rao and Scott correction, converted into an F statistic.
p < .05.
p < .01.
p < .001.
Measures
State Policy Environment.
We created an index of ten policies relevant to sexual minorities, which were adapted from the Movement Advancement Project (MAP).29 The time-varying policy index included six potential policy protections enacted by states in the year of each survey: (1) legalized marriage for same-sex couples; (2) nondiscrimination protections in adoption or foster parenting for same-sex couples; (3) prohibition against discrimination by employers (both private and public/government); (4) housing nondiscrimination laws; (5) laws prohibiting discrimination in public accommodations (e.g., services or entry in public places); and (6) hate crimes laws that cover sexual minorities. The index also included four potential negative policies: (1) bans that explicitly prohibit same-sex marriage, (2) policies that allow denial of adoption and/or foster care by same-sex couples, (3) state bans on cities/counties passing non-discrimination laws, and (4) religious exemption laws permitting discrimination based on religious or moral grounds. Each protective policy was assigned a value of 1 and each negative policy was assigned a value of −1. Partial points were assigned if states provided some form of legal recognition for same-sex couples other than marriage (0.5 for domestic partnerships or civil unions) or protection against employment discrimination for state employees (0.5). (See Table 1 for details of the definitions for each of the policy classifications.) Items on the index were summed by state for each year of the survey, resulting in a possible score ranging from −4 to 6 (see Table 2 for each state’s score by year).
TABLE 2.
State Policy Index Score by State and Survey Year (−4 to 6)
| State | 2000 | 2005 | 2010 | 2015 |
|---|---|---|---|---|
| AK | −1.0 | −0.5 | −0.5 | 1.5 |
| AL | −2.0 | −2.0 | −2.0 | −2.0 |
| AR | −1.0 | −1.0 | −2.0 | −2.0 |
| AZ | −1.0 | 0.5 | 0.5 | 2.5 |
| CA | 4.0 | 5.0 | 4.5 | 6.0 |
| CO | 0.0 | 1.0 | 3.0 | 5.0 |
| CT | 4.0 | 4.5 | 5.0 | 5.0 |
| DC | 4.0 | 4.5 | 5.0 | 5.0 |
| DE | 1.0 | 1.0 | 4.0 | 5.0 |
| FL | −1.0 | −1.0 | −1.0 | 0.0 |
| GA | 0.0 | −1.0 | −1.0 | −1.0 |
| HI | 0.0 | 1.0 | 2.0 | 5.0 |
| IA | 1.0 | 1.0 | 5.0 | 5.0 |
| ID | 0.0 | −1.0 | −1.0 | 1.0 |
| IL | 0.0 | 0.0 | 3.0 | 5.0 |
| IN | −1.0 | −0.5 | −0.5 | 0.5 |
| KS | −1.0 | 0.0 | 0.0 | 0.5 |
| KY | 0.0 | 0.0 | 0.5 | 0.5 |
| LA | 0.0 | 0.5 | 0.0 | 0.0 |
| MA | 5.0 | 6.0 | 6.0 | 6.0 |
| MD | −1.0 | 3.0 | 3.0 | 5.0 |
| ME | 0.0 | 3.0 | 3.0 | 5.0 |
| MI | 0.0 | −1.0 | −1.0 | −1.0 |
| MN | 3.0 | 3.0 | 3.0 | 5.0 |
| MO | 1.0 | 0.0 | 0.0 | 0.0 |
| MS | −2.0 | −2.0 | −2.0 | −3.0 |
| MT | −0.5 | −0.5 | −0.5 | 1.5 |
| NC | −1.0 | −1.0 | −1.0 | 1.0 |
| ND | −1.0 | −1.0 | −1.0 | −1.0 |
| NE | −1.0 | −1.0 | −1.0 | −1.0 |
| NH | 4.0 | 4.0 | 5.0 | 5.0 |
| NJ | 4.0 | 4.5 | 5.5 | 6.0 |
| NM | 1.0 | 4.5 | 4.5 | 5.0 |
| NV | 2.0 | 2.0 | 3.5 | 6.0 |
| NY | 1.5 | 4.5 | 5.5 | 6.0 |
| OH | 0.0 | −1.0 | −1.0 | −0.5 |
| OK | −2.0 | −2.0 | −2.0 | 0.0 |
| OR | 1.0 | 0.0 | 4.5 | 6.0 |
| PA | −0.5 | 0.5 | −0.5 | 1.5 |
| RI | 4.0 | 4.0 | 4.0 | 6.0 |
| SC | −1.0 | −1.0 | −1.0 | 1.0 |
| SD | 0.0 | 0.0 | −1.0 | −1.0 |
| TN | 0.0 | 0.0 | 0.0 | −1.0 |
| TX | −1.0 | 0.0 | 0.0 | 0.0 |
| UT | −1.0 | −1.0 | −1.0 | 3.0 |
| VA | −1.0 | −0.5 | −1.0 | 1.5 |
| VT | 4.5 | 4.5 | 5.0 | 5.0 |
| WA | 0.5 | 0.5 | 3.5 | 5.0 |
| WI | 4.0 | 5.0 | 4.5 | 6.0 |
| WV | −1.0 | −1.0 | −1.0 | 1.0 |
| WY | −0.5 | −0.5 | −0.5 | 1.0 |
Because the study aim was to examine the potential protective effects of supportive policies on outcomes, a dichotomous variable was constructed to compare respondents living in states with four or more policy protections for sexual minorities (classified as comprehensive protections) compared to those living in states with limited or no protections. The construction of a comprehensive (4+) versus limited or no protective policies (−4 to 3) aligns with the designation of “high equality states” in the Movement Advancement Project’s classification scheme. The construction of a dichotomous policy variable was also guided by other research focused on the impact of policy protections on sexual minority health outcomes.7,27,30 For example, other studies have examined health outcomes associated with any policy protections (such as states with hate crimes laws that specific sexual orientation and/or state policies banning sexual orientation employment discrimination in both public and private settings)31 or any state-level protections against discrimination in employment, housing, or public accommodations.27 Other recent studies have used multiple policies to construct a policy environment variable, such as “comprehensive policy protections” defined as five out of five possible nondiscrimination policies7 or “high policy support” based on 11 policies relevant to sexual minorities.30
Sexual minority participants were significantly more likely to live in states with comprehensive (4+) protections (36.6% and 40% respectively for women and men) than heterosexual participants (approximately 29% for both groups; see Table 1). In general, there was a trend toward increased protections for sexual minorities over the time frame represented in the study. In 2000, only eight states and the District of Columbia offered comprehensive protections. Although protections at the state level increased over the survey waves, as of 2015, 22 states and the District of Columbia offered comprehensive policy protections, which is still a minority of jurisdictions. There was some variability within states over time. For example, California and Wisconsin dropped from scores of 5.0–4.5 between 2005 and 2010 as a result state-level votes constitutional amendments that effectively banned same-sex marriage until 2013 and 2014 respectively.
Sexual Identity.
Sexual identity was assessed from a question that invited respondents to select the category that best identified their sexual identity. Given the small sample sizes for different sexual minority subgroups, lesbian/gay and bisexual respondents were combined using an indicator of sexual minority status. In the 2015 survey, response options included “something else”; based on prior research documenting higher risk for hazardous drinking among individuals who identify as “something else” compared to those who identify as heterosexual,32 these respondents also were coded as sexual minorities.
Alcohol Use Disorder (DSM-5 AUD 2+).
Past year alcohol use disorder (AUD) was defined as endorsing symptoms in 2 or more of 11 domains (failure to fulfill role obligations; drinking despite social or interpersonal problems; drinking when physically hazardous; tolerance; with-drawal; using more than or for longer than intended; persistent desire to cut down/control use; giving up important activities; spending a lot of time getting alcohol, using or recovering from use; drinking despite physical or psychological problems; and craving) in the fifth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5).33 This 2+ measure includes respondents with at least mild AUD, encompassing those with moderate and severe AUD as well.
High-Intensity Drinking (HID 8+).
The NAS surveys assessed drinking quantity (e.g., “During the last 12 months, what is the largest number of drinks you had on any single day?”) and frequency of drinking various amounts (e.g., every day or nearly every day, 3–4 times a week, 1–2 times a week, 1–3 times a month, less than once a month, once in those 12 months, and never in those 12 months). We constructed a variable for consumption of eight or more drinks in a single day, one or more times in the past year (vs. none). This measure was based on prior research suggesting an association between alcohol-related problems and consuming larger amounts of alcohol per day34 and documenting sexual orientation disparities in high-intensity binge drinking among adults in the United States.35,36 Although high-intensity drinking is associated with greater odds of past year AUD, quantity/frequency measures are not included in the DSM-5 criteria for AUD. Thus, HID measures are important to include in research designed to identify drinkers most at risk of potential harm.37
Marijuana Use.
Past 12-month marijuana use was dichotomized as any use versus no use.
Demographics.
We included several demographic characteristics known to be associated with alcohol and marijuana use. These were age, race and ethnicity, highest year of education, employment status, marital/relationship status, and having children (ages 17 or under) living in the household (see Table 1). We also included state of residence to account for state-level fixed effects, as well as an indicator for survey year (2000, 2005, 2010, 2015) to adjust for changes over time.
Analysis
All analyses were conducted in Stata (version 16). To ensure that our estimates reflected survey sampling probabilities, we used sample-weighted logistic regression models to adjust point estimates for survey design features. In addition to using the sampling weights, we also adjusted the standard errors to reflect clustering of respondents at the state level and accounted for any number of unspecified differences between respondents in different states by including a categorical state indicator in our models. Studies examining the effects of state-level policies on drinking using similarly weighted data from national surveys have used this approach.38–40
We conducted multivariate, gender-stratified logistic regression analyses to test the independent effects of state policy environment and sexual minority status on measures of harmful drinking and marijuana use, controlling for demographics and other covariates. We then ran models to examine whether state policy environment moderated the relationship between sexual identity and hazardous drinking and marijuana use measures.
In addition to presenting model coefficients, we calculated marginal effects of the policy environment to test the effect of a protective policy context (policy score 4+ vs. < 4) on each outcome by sexual minority status. We then graphically displayed predictive margins for all models to present predicted probabilities of the alcohol and marijuana outcomes for each group (i.e., heterosexual and sexual minority respondents) by different levels of the policy score (i.e., < 4, 4+).
RESULTS
Independent Effects of Sexual Minority Status and Policy
Among women, sexual minority status was associated with increased odds of DSM-5 AUD (OR = 2.50, p < .001), high-intensity drinking (OR = 1.89, p = .009), and marijuana use (OR = 3.64, p < .001), but there was no association between a supportive policy environment and any of the outcomes. Among men, sexual minority status was associated with decreased odds of high-intensity drinking (OR = 0.57, p = .011) but increased odds of marijuana use (OR = 1.81, p = .006). (See Table 3).
TABLE 3.
Weighted Logistic Regression Models Adjusting for Clustering of Respondents at the State Level
| DSM-5 AUD | HID 8+ | Marijuana | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% Cl | P | OR | 95% Cl | P | OR | 95% Cl | P | |
| Women | |||||||||
| Independent Effects Models | |||||||||
| Comprehensive policy protections (4+) | 0.96 | [0.61, 1.51] | 0.875 | 0.88 | [0.52, 1.48] | 0.620 | 1.07 | [0.61, 1.86] | 0.816 |
| Sexual minority status | 2.50 | [1.55, 4.03] | 0.000 | 1.89 | [1.17, 3.06] | 0.009 | 3.64 | [2.27, 5.85] | 0.000 |
| Differential Effects Models | |||||||||
| Comprehensive policy protections (4+) | 0.97 | [0.61, 1.53] | 0.888 | 0.95 | [0.57, 1.58] | 0.849 | 1.14 | [0.67, 1.92] | 0.629 |
| Sexual minority status | 2.53 | [1.33, 4.81] | 0.005 | 2.53 | [1.54, 4.16] | 0.000 | 4.62 | [2.96, 7.21] | 0.000 |
| Policy environment * sexual minority status | 0.97 | [0.40, 2.34] | 0.950 | 0.39 | [0.14, 1.05] | 0.063 | 0.53 | [0.23, 1.23] | 0.141 |
| Men | |||||||||
| Independent Effects Models | |||||||||
| Comprehensive policy protections (4+) | 0.74 | [0.42, 1.29] | 0.287 | 0.80 | [0.63, 1.02] | 0.072 | 1.53 | [0.93, 2.50] | 0.095 |
| Sexual minority status | 1.12 | [0.82, 1.54] | 0.481 | 0.57 | [0.37, 0.88] | 0.011 | 1.81 | [1.18, 2.77] | 0.006 |
| Differential Effects Models | |||||||||
| Comprehensive policy protections (4+) | 0.73 | [0.41, 1.30] | 0.284 | 0.83 | [0.66, 1.05] | 0.122 | 1.50 | [0.92, 2.46] | 0.105 |
| Sexual minority status | 1.03 | [0.68, 1.56] | 0.890 | 0.82 | [0.52, 1.28] | 0.373 | 1.63 | [0.88, 3.02] | 0.120 |
| Policy environment * sexual minority status | 1.24 | [0.61, 2.52] | 0.558 | 0.31 | [0.16, 0.63] | 0.001 | 1.26 | [0.64, 2.49] | 0.501 |
Note. Weighted logistic regression models control for age, partner status, children in the household, race and ethnicity, educational attainment, employment status, survey year, and state and adjust standard errors for clustering of respondents at the state level. DSM-5 AUD = alcohol use disorder as defined by American Psychiatric Association’s Diagnostic & Statistical Manual (DSM), fifth edition; HID 8+ = high-intensity drinking (eight or more drinks in a single day).
Differential Effects of Policy Environment by Sexual Minority Status
Among women, there was a marginally significant interaction between protective policy environment and sexual minority status with respect to high-intensity drinking (OR = 0.39, p = .063), such that comprehensive policy protections were associated with a trend toward decreased odds of high-intensity drinking among sexual minority women only. Among men, there was a significant interaction between protective policy environment and sexual minority status with respect to high-intensity drinking (OR = 0.31, p = .001). As displayed in Table 4 and Figure 1, comprehensive policy protections were associated with decreased probability of HID 8+ among heterosexual and sexual minority men, but the difference was only statistically significant among sexual minority men (Pr = −0.02, p = .114 vs. Pr = −.11, p = .001).
TABLE 4.
Predictive Margins and Marginal Effects of Comprehensive State-level Same-Sex Policy Protections by Gender and Sexual Identity
| Women | Marginal Effect | P | men | Marginal Effect | P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Policy Score < 4 | Policy Score 4+ | Policy Score < 4 | Policy Score 4+ | |||||||||
| Est | 95% Cl | Est | 95% Cl | Est | 95% Cl | Est | 95% Cl | |||||
| DSM-5 AUD | ||||||||||||
| Heterosexual | 0.05 | [0.05, 0.06] | 0.05 | [0.04, 0.06] | 0.00 | 0.887 | 0.12 | [0.10, 0.14] | 0.09 | [0.06, 0.12] | −0.03 | 0.263 |
| Sexual minority | 0.11 | [0.06, 0.17] | 0.11 | [0.05, 0.16] | −0.01 | 0.895 | 0.12 | [0.08, 0.16] | 0.11 | [0.07, 0.15] | −0.01 | 0.775 |
| HID 8+ | ||||||||||||
| Heterosexual | 0.06 | [0.05, 0.06] | 0.05 | [0.04, 0.07] | 0.00 | 0.848 | 0.20 | [0.19, 0.21] | 0.17 | [0.15, 0.19] | −0.02 | 0.114 |
| Sexual minority | 0.12 | [0.07, 0.17] | 0.05 | [0.01, 0.10] | −0.07 | 0.071 | 0.17 | [0.11, 0.23] | 0.06 | [0.03, 0.08] | −0.11 | 0.001 |
| Marijuana Use | ||||||||||||
| Heterosexual | 0.07 | [0.05, 0.08] | 0.07 | [0.05, 0.09] | 0.01 | 0.634 | 0.10 | [0.09, 0.12] | 0.14 | [0.10, 0.18] | 0.04 | 0.124 |
| Sexual minority | [0.15, 0.28] | 0.15 | [0.06, 0.24] | −0.06 | 0.330 | 0.15 | [0.08, 0.22] | 0.24 | [0.14, 0.34] | 0.09 | 0.139 | |
Note. Predictive margins are from weighted logistic regression models controlling for age, partner status, children in the household, race and ethnicity, educational attainment, employment status, survey year, and state and adjusting standard errors for clustering of respondents at the state level. DSM-5 AUD = alcohol use disorder as defined by American Psychiatric Association’s Diagnostic & Statistical Manual (DSM), fifth edition; HID 8+ = high-intensity drinking (eight or more drinks in a single day).
Figure 1.
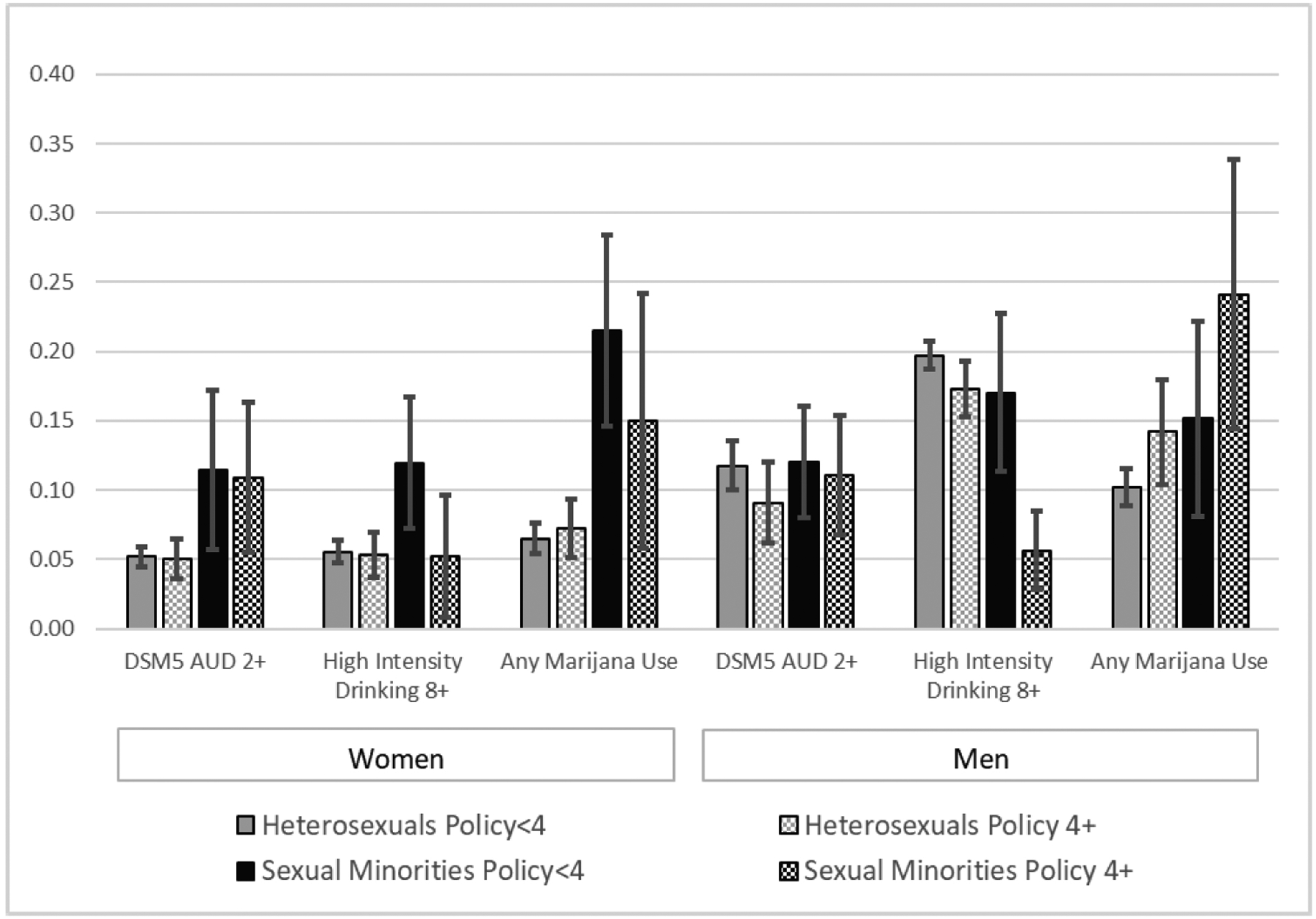
Predictive margins (with 95% CI) of comprehensive state policy protection environment by gender and sexual identity.
DISCUSSION
The current study examined whether supportive state policy environments—defined by policies protecting the rights of sexual minorities—moderated the relationship between sexual identity and two behavioral health measures: hazardous drinking and marijuana use. We found partial support for our hypotheses. Among men, we found strong evidence of differential effects of policy environment by sexual minority status with respect to high-intensity drinking. A protective policy environment was associated with decreased odds of high-intensity drinking among both heterosexual and sexual minority men, but the magnitude of this protective effect was significant only among sexual minority men. Among women, policy environment was associated with trend toward decreased odds of high-intensity drinking among sexual minority women but not heterosexual women. Policy context was not significantly associated with AUD in any group.
The current study found a protective effect of comprehensive policy protections in relation to high-intensity drinking among sexual minorities. The trend toward a protective effect for sexual minority women in relation to high-intensity drinking is of interest, given the notably higher odds for this behavior relative to heterosexual women. These findings extend and confirm those of a growing body of literature documenting positive impacts of sexual minority policy protections on self-reported health,7,27 psychological well-being,31,41,42 AUD,2 and drug use.24 The findings of the current study are important given research documenting that high-intensity drinking, such as drinking eight or more drinks at one time (approximately twice the standard heavy-drinking threshold), is associated with greater risk for AUD34 and other negative health consequences, such as driving while intoxicated and alcohol-related injuries.43 Factors that may moderate negative impacts of excessive alcohol use are important for ongoing intervention efforts to address alcohol-related morbidity and mortality and to reduce disparities in health by sexual identity.
Our findings differed from Hatzenbuehler et al. (2010) in that we did not find a significant impact of the policy environment on AUD by sexual minority status. The divergence in findings may be due, at least in part, to differences in policy definitions. While our study explored the potential protective effects of multiple policy protections, Hatzenbuehler et al. examined the harmful impact of discriminatory state bans against same-sex marriage. They used two waves of data from a longitudinal, nationally representative sample to examine the impact of constitutional amendments that banned same-sex marriage and found that AUD (and other psychiatric disorders) increased between survey waves among sexual minority (but not heterosexual) adults living in states that adopted bans.2 Comparable increases in AUD were not found in comparison states that had not enacted bans against same-sex marriage. The impact of exposure to stigmatizing messaging in campaign debates or referenda that devalue the rights of stigmatized minority groups may have uniquely harmful impacts on psychological health. For example, research on the psychological impact of debates about marriage bans in U.S. states showed exposure to stigmatizing campaign messages was associated with decreased positive affect, increased negative affect, more depressive symptoms and greater stress among sexual minorities.5,6 Policies that explicitly seek to limit the rights of sexual minorities, and messaging surrounding those detrimental policy initiatives, may differentially impinge upon the health of sexual minority residents in those areas.
There may be other reasons that AUD did not differ by policy context in the current study. Other sources of minority stress may persist despite policy protections. For example, same-sex couples still experience unequal treatment and stigma in interpersonal interactions despite marriage equality.11,44 Research has also found that community-level social climate (which was not assessed in the current study) is an important predictor of sexual minority health outcomes,12,27,45 and supportive policy environments are more protective of sexual minority people’s health in the context social climates that affirm their identities.27 The health-promoting implications of concurrent improvements in policy and social climate may become more evident over time vis-à-vis shifts toward more affirming public attitudes and policies. For example, a study examining cross-sectional national data spanning 15 years in Sweden found disparities in psychological health among sexual minorities diminished as the political and social climate improved over time.46 Furthermore, sexual minority experiences of structural stigma appear to be mediated by interpersonal and individual factors such as social support13 and rejection sensitivity47,48 that were not accounted for in the current study.
In independent effects models, sexual minority status was associated with increased odds of marijuana use by women and men. It may be that more permissive norms related to drug use in sexual minority communities identified in other studies49 persist regardless of state policy context. Research has found support for sexual minority rights (e.g., legalization of marriage for same-sex couples) and public opinion favoring legalization of marijuana often occur in tandem.50 Future studies might explore whether policy and social climate related to marijuana use differentially impacts sexual minorities. In our study, sexual minorities were significantly more likely than heterosexual respondents to live in states with policy protections, and these states may also be more likely to have greater availability of marijuana and a more permissive climate related to marijuana use. This deserves further study.
Limitations
Although this study has a number of strengths, including use of nationally-representative data, important limitations should be noted. Research using probability samples are often limited by relatively small numbers of sexual minority respondents.51,52 Consequently, it is possible these results may be influenced by the small sample size. Although the surveys oversampled Black/African American and Hispanic/Latinx individuals, we did not have a sufficient sample size to investigate how policy contexts may differentially impact sexual minority women and men of color in relation to White sexual minorities or heterosexual Black and Latinx counterparts. For example, some studies suggest differences in risk by race and ethnicity among sexual minority men.53 Future research examining the impact of policies on sexual minority adults, stratified by race and ethnicity, would be informative to the design and implementation of potential social-structural and health promotion interventions. Our study did not include measures of perceived drug availability or norms, and our analyses also did not control for other state-level policies and measures of public opinion that may impact health behaviors or health outcomes, such as policies and public support for marijuana legalization. We also did not have a measure of cannabis use disorder in the survey data; our measure of any marijuana use may not adequately capture problem use. Furthermore, although data were collected at different time points, the NAS is a cross-sectional survey, and it is not possible to assess causal relationships.
Our sample size did not allow disaggregation of bisexual respondents from other sexual minority respondents, which is a limitation given studies suggesting hazardous drinking and drug use are particularly pronounced among bisexual individuals.15,19,26 However, in post hoc analyses combining women and men, disaggregating respondents who identified as bisexual from those who identified as gay/lesbian showed no change in the overall findings. Specifically, living in a state with comprehensive policy protections was associated with a larger decrease in the probability of high-intensity drinking among both bisexual and gay/lesbian respondents compared to heterosexual respondents. There were no differences in high-intensity drinking between those identifying as bisexual and those identifying as gay/lesbian. We also ran post hoc analyses excluding marital/relationship status as a control and found no difference from the overall results. Finally, we also ran post hoc analyses with a higher weight (2 points) for legalized marriage (as debates and changes in these policies were highly visible and have been documented as impactful in prior research); in these analyses the protective effect for high-intensity drinking remained robust and were significant for both sexual minority women and sexual minority men. Future studies with larger samples of sexual minority respondents are needed to investigate how the impact of policies on hazardous drinking and marijuana use might vary by both sex and sexual identity or by relationship status.
In spite of these limitations, the findings from this study contribute to a growing body of literature suggesting protective policy and social contexts are associated with better psychological and physical health among sexual minorities.54 It is interesting that our study found the policy environment was associated with a trend toward reduced high-intensity drinking among heterosexual men, although the protective effect of a living in a state with comprehensive policy protections was significant only for sexual minority men. A unique study by Solazzo et al. examined state-level anti-discrimination policies, sexual minority-friendly social climate, and the interaction between policy and climate and found no impact health status among individuals who identified as heterosexual.27 By contrast, another study by Hatzenbuehler et al.12 found higher levels of local approval of same-sex marriage lowered the probabilities of smoking and fair/poor self-rated health among both lesbian, gay, bisexual, and transgender (LGBT)-identified and heterosexual adults. Future research is needed to investigate potential positive impacts of protective policies among sexual identity groups across a larger range of outcomes.
In research concerning social and health outcomes of sexual and gender minorities, there has been increased focus on the influence of structural stigma, including its role in alcohol use disparities.1,55,56 As studies of structural stigma seek to unpack effects on health outcomes and disparities, better understanding the role of policy is paramount. For example, an increasing number of states in the United States are adopting laws that allow for discrimination against sexual and gender minorities, such as denial of health care to LGBT individuals or of services for same-sex couples, for reasons attributed to religious beliefs.57 Emerging research suggests residence in states with discriminatory policies is associated with increased psychological distress among sexual minorities.42 In this changing context, studies are needed to further investigate the impact of anti-LGBT policies on alcohol and drug outcomes among sexual minorities. There also is a need for ongoing surveillance of laws prohibiting discrimination, as well as how these laws and their enforcement impact health outcomes.58
Our findings underscore the value of reducing structural stigma as a strategy for addressing disparities in health by sexual identity. Findings from the current study are also compatible with calls to further investigate coping and resilience among sexual minorities in individual, interpersonal, and social realms.59–61 Resilience-based interventions62–64 may amplify effects of protective policies across the sexual minority spectrum and also may help buffer the negative impacts of living in regions without enforcement of such protections. There is a need for more research on specific strategies for advancing health equity and promoting health in diverse LGBT populations, particularly research grounded in frameworks that recognize the interactions between structural and individual stigma, use an intersectional stigma-informed lens,65,66 and focus on individual and community strengths.67
Conclusions
The current study found that residence in states with comprehensive policy protections for sexual minorities was associated with decreased odds of high-intensity drinking among both sexual minority women and sexual minority men compared to sexual minority counterparts living in states with fewer or no protections; a difference that was statistically significant for sexual minority men. Findings underscore the importance of reducing structural stigma as a strategy for reducing health disparities by sexual identity. There is a need for further research designed to monitor the impact of policy on health given the U.S. context, in which policies that protect the rights of sexual and gender minorities, or that explicitly allow for denial of healthcare or other services on religious grounds, continue to evolve.
Supplementary Material
Statement of Public Health Significance:
Residence in states with comprehensive policy protections for sexual minority adults was associated with decreased odds of high-intensity drinking among both sexual minority women and sexual minority men compared to counterparts living in states with fewer or no protections. Findings underscore the importance of addressing structural stigma to reduce health disparities.
Acknowledgments.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. In addition to their funders, the authors would also like to acknowledge the work of Deidre Patterson, MPH, for her assistance in preparing the National Alcohol Survey data for these analyses as well as Ellen Perry, MSW, and Emily Yette, PhD, for assistance with state policy classification.
Funding.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This work was supported by the National Institute on Drug Abuse R01DA036606, awarded to K. Trocki and L. Drabble, M-PIs; National Institute on Minority Health and Health Disparities of the National Institutes of Health R03MD011481, awarded to K. Trocki and L. Drabble, M-PIs; National Institute on Alcohol Abuse and Alcoholism P50AA005595; National Alcohol Survey dataset T32AA007240.
Footnotes
Disclosure. The authors have no relevant financial interest or affiliations with any commercial interests related to the subjects discussed within this article.
REFERENCES
- [1].Hatzenbuehler ML. Structural stigma and the health of lesbian, gay, and bisexual populations. Curr Dir Psychol Sci. 2014;23(2):127–132. [Google Scholar]
- [2].Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. 2010;100(3):452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hatzenbuehler ML, Link B. Introduction to the special issues on structural stigma and health. Soc Sci Med. 2014;103:1–6. [DOI] [PubMed] [Google Scholar]
- [5].Frost DM, Fingerhut AW. Daily exposure to negative campaign messages decreases same-sex couples’ psychological and relational well-being. Group Processes Intergroup Relations. 2016;19(4):477–492. [Google Scholar]
- [6].Riggle ED, Rostosky SS, Horne SG. Marriage amendments and lesbian, gay, and bisexual individuals in the 2006 election. Sex Res Soc Policy. 2009;6(1):80–89. [Google Scholar]
- [7].Gonzales G, Ehrenfeld JM. The association between state policy environments and self-rated health disparities for sexual minorities in the United States. Int J Environ Res Public Health. 2018;15(6):1136. doi: 10.3390/ijerph15061136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Carpenter C, Eppink ST, Gonzales G Jr, McKay T. Effects of Access to Legal Same-Sex Marriage on Marriage and Health: Evidence from BRFSS. National Bureau of Economic Research; 2018, Cambridge, MA: National Bureau of Economic Research; 2018; Working Paper 24651.http://www.nber.org/papers/w24651. [Google Scholar]
- [9].Kail BL, Acosta KL, Wright ER. State-level marriage equality and the health of same-sex couples. Am J Public Health. 2015;105(6):1101–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Raifman J, Moscoe E, Austin SB, McConnell M. Difference-in-differences analysis of the association between state same-sex marriage policies and adolescent suicide attempts. JAMA Pediatr. 2017;171(4):350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kennedy HR, Dalla RL. “It may be legal, but it is not treated equally”: marriage equality and well-being implications for same-sex couples. J Gay Lesbian Soc Serv. 2020;32(1):67–98. [Google Scholar]
- [12].Hatzenbuehler ML, Flores AR, Gates GJ. Social attitudes regarding same-sex marriage and LGBT health disparities: results from a national probability sample. J Soc Issues. 2017;73(3):508–528. [Google Scholar]
- [13].Perales F, Todd A. Structural stigma and the health and wellbeing of Australian LGB populations: exploiting geographic variation in the results of the 2017 same-sex marriage plebiscite. Soc Sci Med. 2018, 208, 190–199. [DOI] [PubMed] [Google Scholar]
- [14].Tatum AK. The interaction of same-sex marriage access with sexual minority identity on mental health and subjective wellbeing. J Homosex. 2017;64(5):638–653. [DOI] [PubMed] [Google Scholar]
- [15].McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction. 2009;104(8):1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Drabble LA, Mericle AA, Karriker-Jaffe KJ, Trocki KF. Harmful drinking, tobacco, and marijuana use in the 2000–2015 National Alcohol Surveys: examining differential trends by sexual identity. Subst Abuse. 2020;(online in advance of print): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Blosnich JR, Farmer GW, Lee JG, Silenzio VM, Bowen DJ. Health inequalities among sexual minority adults: evidence from ten US states, 2010. Am J Prev Med. 2014;46(4):337–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Operario D, Gamarel KE, Grin BM, et al. Sexual minority health disparities in adult men and women in the United States: National Health and Nutrition Examination Survey, 2001–2010. Am J Public Health. 2015;105(10):e27–e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Green KE, Feinstein BA. Substance use in lesbian, gay, and bisexual populations: an update on empirical research and implications for treatment. Psychol Addict Behav. 2012;26(2):265–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hughes T Alcohol use and alcohol-related problems among sexual minority women. Alcoholism Treatment Q. 2011;29(4):403–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Trocki KF, Drabble LA, Midanik LT. Tobacco, marijuana use and sensation-seeking: comparisons across gay, lesbian, bisexual, and heterosexual groups. Psychol Addict Behav. 2009;23(4):620–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].King M, Semlyen J, Tai SS,et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Plöderl M, Tremblay P. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry. 2015;27(5):367–385. [DOI] [PubMed] [Google Scholar]
- [24].Hatzenbuehler ML, Jun H-J, Corliss HL, Austin SB. Structural stigma and sexual orientation disparities in adolescent drug use. Addict Behav. 2015;46:14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hatzenbuehler ML, Jun H-J, Corliss HL, Austin SB. Structural stigma and cigarette smoking in a prospective cohort study of sexual minority and heterosexual youth. Ann Behav Med. 2014;47(1):48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hughes TL, Veldhuis CB, Drabble LA, Wilsnack SC. Substance use among sexual minority women: a global scoping review. PLoS One. 2020;15(3), Article e0229869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Solazzo A, Brown TN, Gorman BK. State-level climate, anti-discrimination law, and sexual minority health status: an ecological study. Soc Sci Med. 2018;196:158–165. [DOI] [PubMed] [Google Scholar]
- [28].Pachankis JE, Bränström R. Hidden from happiness: structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. J Consult Clin Psychol. 2018;86(5):403–415. [DOI] [PubMed] [Google Scholar]
- [29].Movement Advancement Project. Mapping LGBT Equality in America. Denver, CO: Author; 2015. [Google Scholar]
- [30].Hatzenbuehler ML, McKetta S, Goldberg N,et al. Trends in state policy support for sexual minorities and HIV-related outcomes among men who have sex with men in the United States, 2008–2014. JAIDS J Acquir Immune Defic Syndr. 2001;85(1):39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health. 2009;99(12):2275–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Eliason MJ, Radix A, McElroy JA, Garbers S, Haynes SG. The “something else” of sexual orientation: measuring sexual identities of older lesbian and bisexual women using National Health Interview Survey questions. Womens Health Issues. 2016;26:S71–S80. [DOI] [PubMed] [Google Scholar]
- [33].American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed.Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- [34].Greenfield TK, Ye Y, Bond J, et al. Risks of alcohol use disorders related to drinking patterns in the US general population. J Stud Alcohol Drugs. 2014;75(2):319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Fish JN. Sexual orientation-related disparities in high-intensity binge drinking: findings from a nationally representative sample. LGBT Health. 2019;6(5):242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Fish JN, Hughes TL, Russell ST. Sexual identity differences in high-intensity binge drinking: findings from a US national sample. Addiction. 2018;113(4):749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Linden-Carmichael AN, Vasilenko SA, Lanza ST, Maggs JL. High-intensity drinking versus heavy episodic drinking: prevalence rates and relative odds of alcohol use disorder across adulthood. Alcoholism Clin Exp Res. 2017;41(10):1754–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Roberts SC, Mericle AA, Subbaraman MS, et al. State policies targeting alcohol use during pregnancy and alcohol use among pregnant women 1985–2016: evidence from the behavioral risk factor surveillance system. Womens Health Issues. 2019;29(3):213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Roberts SC, Mericle AA, Subbaraman MS, et al. Differential effects of pregnancy-specific alcohol policies on drinking among pregnant women by race/ethnicity. Health Equity. 2018;2(1):356–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Roberts SC, Mericle AA, Subbaraman MS, Thomas S, Kerr W, Berglas NF. Variations by education status in relationships between alcohol/pregnancy policies and birth outcomes and prenatal care utilization: a legal epidemiology study. J Public Health Manag Pract. 2020; 26(Suppl 2, Advancing Legal Epidemiology) :S71–S83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Hatzenbuehler ML. The influence of state laws on the mental health of sexual minority youth. JAMA Pediatr. 2017;171(4):322–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Raifman J, Moscoe E, Austin SB, Hatzenbuehler ML, Galea S. Association of state laws permitting denial of services to same-sex couples with mental distress in sexual minority adults: a difference-in-difference-in-differences analysis. JAMA Psychiatr. 2018;75(7):671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Patrick ME, Azar B. High-intensity drinking. Alcohol Res Current Rev. 2018;39(1):49–55. [PMC free article] [PubMed] [Google Scholar]
- [44].LeBlanc AJ, Frost DM, Bowen K. Legal marriage, unequal recognition, and mental health among same-sex couples. J Marriage Fam. 2018;80(2):397–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Woodford MR, Paceley MS, Kulick A, Hong JS. The LGBQ social climate matters: policies, protests, and placards and psychological well-being among LGBQ emerging adults. J Gay Lesbian Soc Serv. 2015;27(1):116–141. [Google Scholar]
- [46].Hatzenbuehler ML, Bränström R, Pachankis JE. Societal-level explanations for reductions in sexual orientation mental health disparities: results from a ten-year, population-based study in Sweden. Stigma Health. 2018;3(1):16–26. [Google Scholar]
- [47].Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Soc Sci Med. 2014;103:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Feinstein BA, Goldfried MR, Davila J. The relationship between experiences of discrimination and mental health among lesbians and gay men: an examination of internalized homonegativity and rejection sensitivity as potential mechanisms. J Consult Clin Psychol. 2012;80(5):917–927. [DOI] [PubMed] [Google Scholar]
- [49].Cochran SD, Grella CE, Mays VM. Do substance use norms and perceived drug availability mediate sexual orientation differences in patterns of substance use? Results from the California Quality of Life Survey II. J Stud Alcohol Drugs. 2012;73(4):675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Schnabel L, Sevell E. Should Mary and Jane be legal? Americans’ attitudes toward marijuana and same-sex marriage legalization, 1988–2014. Public Opin Q. 2017;81(1):157–172. [Google Scholar]
- [51].Meyer IH, Wilson PA. Sampling lesbian, gay, and bisexual populations. J Couns Psychol. 2009;56(1):23–31. [Google Scholar]
- [52].Drabble LA, Trocki KF, Korcha RA, Klinger JL, Veldhuis CB, Hughes TL. Comparing substance use and mental health outcomes among sexual minority and heterosexual women in probability and non-probability samples. Drug Alcohol Depend. 2018;185:285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Gilbert PA, Drabble L, Daniel-Ulloa J, Trocki KF. Alcohol outcomes by sexual orientation and race/ethnicity: few findings of higher risk. J Stud Alcohol Drugs. 2017;78(3):406–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Hatzenbuehler ML, Keyes KM, McLaughlin KA. The protective effects of social/contextual factors on psychiatric morbidity in LGB populations. Int J Epidemiol. 2011;40(4):1071–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am Psychol. 2016;71(8):742–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Richman LS, Hatzenbuehler ML. A multilevel analysis of stigma and health: Implications for research and policy. Policy Insights Behav Brain Sci. 2014;1(1):213–221. [Google Scholar]
- [57].Movement Advancement Project. Equality Maps: Religious Exemption Laws. 2020. https://www.lgbtmap.org/equality-maps/religious_exemption_laws.Published 2020. AccessedMay 17, 2020 [Google Scholar]
- [58].Blake VK, Hatzenbuehler ML. Legal remedies to address stigma-based health inequalities in the United States: challenges and opportunities. Milbank Q. 2019;97(2):480–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Hill CA, Gunderson CJ. Resilience of lesbian, gay, and bisexual individuals in relation to social environment, personal characteristics, and emotion regulation strategies. Psychol Sex Orientation Gender Divers. 2015;2(3):232–252. [Google Scholar]
- [60].Meyer IH. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol Sex Orientation Gender Divers. 2015;2(3):209–213. [Google Scholar]
- [61].Ja’nina J, Longmire-Avital B. Resilience and depression: the roles of racial identity, sexual identity, and social support on well-being for black LGB emerging adults. J Black Sex Relationships. 2018;4(4):1–15. [Google Scholar]
- [62].Herrick AL, Lim SH, Wei C, et al. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15(1):25–29. [DOI] [PubMed] [Google Scholar]
- [63].Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2014;18(1):1–9. [DOI] [PubMed] [Google Scholar]
- [64].Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J Couns Clin Psychol. 2015;83(5):875–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Turan JM, Elafros MA, Logie CH, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med.. 2019;17(1):article 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Bowleg L The problem with the phrase women and minorities: intersectionality —an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Gahagan J, Colpitts E. Understanding and measuring LGBTQ pathways to health: a scoping review of strengths-based health promotion approaches in LGBTQ health research. J Homosexuality. 2017;64(1):95–121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


