Abstract
Purpose:
Pregnant women are facing numerous COVID-19 related burdens including social isolation, financial insecurity, uncertainty about the impact of the virus on fetal development, and prenatal care restrictions. We tested the psychometric properties of a new instrument designed to assess the extent and types of pandemic-related stress experienced by pregnant women.
Materials and Methods:
4,451 pregnant women from across the U.S. were recruited via social media and completed an online questionnaire in April-May 2020. The questionnaire included measures of psychological, sociodemographic, and obstetric factors and the new Pandemic-Related Pregnancy Stress Scale (PREPS).
Results:
Confirmatory factor analyses of the PREPS showed excellent model fit. Three factors -- Perinatal Infection Stress (5 items), Preparedness Stress (7 items), and Positive Appraisal (3 items) -- converged and diverged with expected psychological factors, and scales created from these factors demonstrated acceptable to good reliability (α’s 0.68-0.86). In addition, mean PREPS scores were associated with perceived risk of infection, and with financial and vocational COVID-19 related burdens.
Conclusion:
The PREPS is a robust instrument to assess multidimensional COVID-19 pandemic prenatal stress. It is a valuable tool for future research to examine vulnerability to pandemic stress and how this stress may affect women and their offspring.
Keywords: COVID-19, Prenatal maternal stress, Pandemic-related pregnancy stress, Psychometrics
Introduction
The COVID-19 public health crisis has dramatically changed the daily lives of pregnant women. Following the announcement by the World Health Organization that COVID-19 was a global pandemic on March 11, 20201, reports of restrictions on intrapartum care (e.g., limitations on accompaniment at delivery, having to wear a face mask during birth, no postpartum visitations, cancelled or reduced frequency of antenatal visits) began emerging2,3. As knowledge about the effects of COVID-19 during pregnancy was rapidly evolving, little reassurance about the risks of the virus or its effect on the fetus and the pregnancy was initially available. In addition, women pregnant during the pandemic faced various pandemic-related stressors such as social isolation, impoverishment, and risks associated with sheltering in place, potentially with an abusive partner4,5.
Preliminary reports suggest that the COVID-19 pandemic and its associated social and economic consequences have increased stress and mental health among pregnant women6,7. However, there is a lack of systematic research that measures pregnancy specific pandemic-related stress. This is a major concern given the well-documented evidence linking elevated stress during pregnancy8, especially stress specific to pregnancy9, as well as exposures to disasters occurring during pregnancy10-12, with adverse outcomes including birth complications, low birth weight, and preterm birth. The unique storm of psychological and social stressors associated with the pandemic -- including diminished social support, lack of access to prenatal care, and increased psychological uncertainty -- exposes a critical need to develop psychometrically validated instruments for assessing the impact of the pandemic on pregnant women. Such instruments will enable examination of stress-related effects of the pandemic on pregnant women and their offspring and inform evidence-based public health interventions.
As such, the goals of the current study were 1) to test the psychometric properties (i.e, construct, convergent and divergent validity, reliability) of an instrument to assess stress related to the COVID-19 pandemic experienced by pregnant women and 2) to identify how pandemic related burdens including those related to COVID-19 infection (proximity to infected people, diagnosis of infection, and perceived risk), prenatal care access, employment status, and financial loss are associated with pandemic-related pregnancy stress.
Methods
Participants and Study Design
Between April 24th and May 15th 2020 we recruited a sample of 4,451 pregnant women on social media (Facebook, Instagram, & Reddit) for the COVID-19 Pregnancy Experiences (COPE) Study -- a longitudinal project to assess psychosocial impacts of the COVID-19 pandemic on pregnant women and their offspring. Facebook paid advertisement targeted women in the U.S. who showed pregnancy related interests. Additionally, research assistants posted an identical advertisement for the study on pregnancy-related social media groups and pages. The advertisement included a request to share pregnancy-related experiences during COVID-19 by completing the COPE Study questionnaire online. The questionnaire, which included pregnancy-related and general psychological instruments as well as COVID-19 related and obstetric questions, was completed through Qualtrics, a secure online survey platform. Inclusion criteria were being currently pregnant, ≥ 18 years old, and able to read and write in English. Participants who completed the questionnaire were enrolled in a raffle with a 1/100 chance to win a $100 gift card. The study was approved on April 21, 2020 by the Institutional Review Board of Stony Brook University (IRB2020-00227).
Measures
The Pandemic-Related Pregnancy Stress Scale (PREPS) is a novel instrument that was created by a multidisciplinary research and clinical team with expertise in developing validated instruments to assess prenatal maternal stress and coping13. Item themes were based on news articles and media interviews regarding women’s experiences during the COVID-19 pandemic2,3 as well as the limited research that was available at the time6,7. Item wording was tested for face validity by pregnant and non-pregnant women before the COPE Study launch. Originally, 17 PREPS items assessed thoughts and concerns pregnant women might have due to the COVID-19 pandemic and its related impacts with a response scale from 1 = Very Little to 5 = Very Much. Structural analysis of the PREPS based on 788 women recruited in April 2020 indicated that 15 of the 17 items comprise three interpretable and internally consistent, independent but correlated factors related to stress about preparation for birth and the postpartum (e.g., “I am worried that the pandemic could ruin my birth plans”, “I am concerned that I am not getting enough healthy food or sleep or exercise because of COVID-19 restrictions”), stress related to worries about infection (e.g., “I am worried that my baby could get COVID-19 at the hospital after birth”, “I am concerned that a COVID-19 infection could harm my pregnancy (such as miscarriage or preterm birth)”), and aspects of the pandemic which were experienced favorably (“I feel that being pregnant is giving me strength during the pandemic”, “I feel that COVID-19 is helping me appreciate my pregnancy more”). These three factors were labeled, respectively: PREPS-Preparedness, PREPS-Infection, and PREPS-Positive Appraisal13. The remaining 2 items, which did not load on any of the three factors, were dropped from further analyses. Scale scores were calculated as the mean response of items on the corresponding factor (range 1 to 5).
Sociodemographic and obstetric factors included parity, maternal age, gestational age, ethnicity and race, financial status (Below average/ Average/ Above average), and relationship status (Married or cohabiting/ Serious relationship/ Single/ Other).
COVID-19 exposure and pandemic impacts included confirmed COVID-19 diagnosis during pregnancy: “Did you receive a medical diagnosis of COVID-19 during your pregnancy?” (No/ Yes); close proximity to someone with COVID-19: “During your pregnancy, have you had direct contact with someone medically diagnosed with COVID-19?” (No/ Yes); perceived risk of having COVID-19: “Do you think that you had COVID-19 during your pregnancy even if you were not tested?” (No/ Unsure/ Yes); COVID-19 related income loss: “Have you, or someone you rely on, lost income due to COVID-19?” (No/ Yes); and essential worker status (No/ Yes).
Fear of childbirth was measured using the two-item Fear of Birth Scale14. Women were asked about their feelings regarding the upcoming birth on a Visual Analogue Scale (VAS) with the following anchors: Calm versus Worried and No Fear versus Strong Fear. Internal consistency was excellent (α = 0.90) and scale scores were calculated as the mean response of the items.
Pregnancy-specific stress was assessed using the Revised Prenatal Distress Questionnaire (NuPDQ)9. Women rated the extent to which they are “feeling bothered, upset, or worried” about 17 pregnancy-relevant stressors on a scale from 0 = Not at All to 2 = Very Much. The instrument had strong internal consistency (α = 0.80).
Perceived risk of COVID infection for non-pregnant loved-ones was assessed with a single item, “I am worried that people I care about will get COVID-19” which was rated on a scale from 1 = Very Little to 5 = Very Much.
COVID-19 related personal growth was assessed using four items based on related research on personal growth15 associated with major stressful events (e.g., “The COVID-19 pandemic helped me realize that I’m stronger than I thought I was”). These items were rated on a scale from 1 = Very Little to 5 = Very Much and their mean item response was calculated. The scale had acceptable internal consistency (α = 0.70).
Statistical Analysis
Statistical analysis was performed using SPSS 26.016 and AMOS 24.017. To replicate the three-factor structure of the PREPS previously identified13, we conducted Confirmatory Factor Analysis (CFA) using the following criteria to determine good model fit: the Comparative Fit Index and the Tucker-Lewis index (CFI and TLI ≥ .90), the root-mean-square error of approximation (RMSEA ≤ .08), and the standardized root-mean-square residual (SRMR ≤ .08)18-20. Internal consistency coefficients (Cronbach's α) greater than 0.70 were considered acceptable21. Construct validity was assessed by examining convergent and discriminant validity using bivariate Pearson's correlation coefficients. Good convergent validity was determined by moderate-strong correlation (r > 0.5) and discriminant validity by low correlation (r ≤ 0.2)22. Mean differences were assessed using t-tests and One-way Analysis of Variance with p < 0.05 considered statistically significant.
Results
Demographic characteristics
Average age for study participants was 30.81±4.66 and most were married or cohabiting (n = 4,074, 91.5%). Most participants were non-Hispanic-White (n = 3,651, 82.0%) with 206 (4.6%) Black or African American and 420 (9.4%) Latina or Hispanic. Additional obstetric and COVID-19 impact frequencies can be found in Table 1.
Table 1.
Mean differences of Pandemic-Related Pregnancy Stress Scale scores among women with different basic obstetric characteristics and COVID-19 related impacts (N = 4,451)
| N (%) | Preparedness | Infection | Positive Appraisal |
|
|---|---|---|---|---|
| Parity | t = 9.48*** | t = 1.35 | t = 9.33*** | |
| Primipara | 2270 (51.1) | 3.47±0.81 | 3.37±0.89 | 2.40±0.91 |
| Multipara | 2176 (48.9) | 3.24±0.83 | 3.34±0.93 | 2.15±0.88 |
| Trimester | F = 6.39** | F = 6.35** | F = 3.10* | |
| 1st | 439 (9.9) | 3.24±0.89a | 3.27±0.91a | 2.27±0.5ab |
| 2nd | 1714 (38.6) | 3.39±0.83b | 3.41±0.91b | 2.31±0.90a |
| 3rd | 2293 (51.5) | 3.35±0.81b | 3.33±0.99a | 2.24±0.89b |
| Contact with someone with medically diagnosed COVID-19 | t = 1.50 | t = 1.36 | t = 1.06 | |
| No | 3945 (88.7) | 3.35±0.83 | 3.35±0.91 | 2.28±0.91 |
| Yes | 505 (11.3) | 3.41±0.86 | 3.41±0.88 | 2.23±0.89 |
| Had been medically diagnosed with COVID-19 | t = 0.71 | t = 0.79 | t = 0.02 | |
| No | 4397 (98.8) | 3.36±0.83 | 3.35±0.91 | 2.27±0.90 |
| Yes | 53 (1.2) | 3.44±0.88 | 3.45±0.82 | 2.27±1.05 |
| Thought to have had COVID-19 but no medical diagnosis | F = 48.89*** | F = 40.12** | F = 0.44 | |
| No | 2914 (66.3) | 3.27±0.82a | 3.27±0.91a | 2.27±0.90 |
| Unsure | 1103 (25.1) | 3.49±0.80b | 3.55±0.87b | 2.29±0.87 |
| Yes | 380 (8.6) | 3.60±0.86b | 3.45±0.97b | 2.26±0.96 |
| Prenatal appointment cancelled | t = 12.18*** | t = 7.64*** | t = 0.32 | |
| No | 2074 (46.6) | 3.20±0.84 | 3.24±0.91 | 2.28±0.92 |
| Yes | 2376 (53.4) | 3.50±0.80 | 3.45±0.89 | 2.27±0.89 |
| Essential worker | t = 0.70 | t = 0.05 | t = 2.21* | |
| No | 2664 (59.9) | 3.35±0.82 | 3.35±0.91 | 2.30±0.92 |
| Yes | 1786 (40.1) | 3.37±0.85 | 3.36±0.90 | 2.24±0.87 |
| Lost income due to COVID-19 | t = 7.26*** | t = 4.76*** | t = 2.79** | |
| No | 2413 (59.9) | 3.27±0.83 | 3.30±0.89 | 2.24±0.88 |
| Yes | 2037 (40.1) | 3.45±0.82 | 3.43±0.93 | 2.31±0.93 |
p <0.05
p < 0.01
p < 0.001
Construct validity and reliability
The CFA replicated the factor structure of the PREPS reported previously 13 and had excellent model fit as indicated by CFI = 0.93, TLI = 0.91, RMSEA= 0.07, and SRMR = 0.057 (Figure 1). Seven items loaded on the first factor, PREPS-Preparedness. The subscale created from items on this factor was internally consistent (α = 0.81) with inter-item correlations all > 0.25. Five items loaded on the second factor, PREPS-Infection; the subscale based on this factor was also internally consistent (α = 0.86) with inter-item correlations all > 0.39. The third factor, PREPS-Positive Appraisal, was comprised of three items. The internal consistency of this subscale (α = 0.68) was slightly lower than the usual α = 0.70 criterion but inter-item correlation coefficients of all items were > 0.33.
Figure 1. Standardized estimates of Confirmatory Factor Analysis of the Pandemic-Related Pregnancy Stress Scale (N = 4,500).
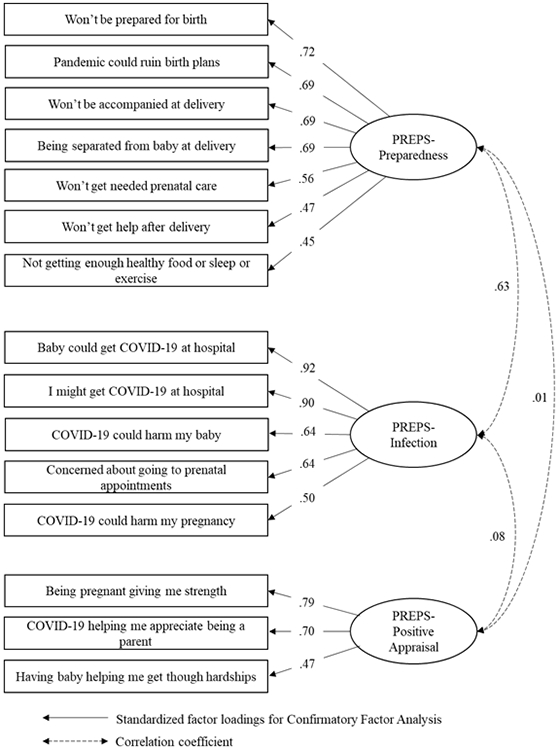
Note: items COVID-19 could harm my pregnancy and COVID-19 could harm my baby were correlated r = 0.55
As can be seen in Table 2, the PREPS-Preparedness factor converged with Fear of Childbirth and with Pregnancy-Specific Stress and diverged from Personal Growth. The PREPS-Infection factor converged with Non-Pregnancy COVID-19 Infection Concerns and with Fear of Childbirth and diverged from Personal Growth. The PREPS-Positive subscale converged with Personal Growth and diverged from Fear of Childbirth, Pregnancy-Specific Stress and from Non-Pregnancy COVID-19 Infection Concerns.
Table 2.
Associations among Pandemic-Related Pregnancy Stress Scale (PREPS) scores and psychological measures (N = 4,500)
| Range | M+SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. PREPS-Preparedness | 1–5 | 3.36±0.83 | --- | |||||
| 2. PREPS- Infection | 1-5 | 3.36±0.91 | 0.65*** | --- | ||||
| 3. PREPS- Positive Appraisal | 1-5 | 2.27±0.90 | 0.05*** | 0.11*** | --- | |||
| 4. Fear of Childbirth | 0-100 | 56.54±23.58 | 0.61 *** | 0.51 *** | −0.07*** | --- | ||
| 5. Pregnancy-Specific Stress | 0-2 | 0.86±0.34 | 0.58 *** | 0.43*** | 0.04** | 0.52*** | --- | |
| 6. Perceived Infection Risk for Loved-Ones | 1-5 | 3.91±1.01 | 0.46*** | 0.68 *** | 0.10*** | 0.33*** | 0.30*** | --- |
| 7. Personal Growth | 1-5 | 2.93±0.82 | 0.16*** | 0.20*** | 0.52 *** | 0.05** | 0.11*** | 0.18*** |
p <0.05
p < 0.01
p < 0.001
Note: Bolded correlations were used to indicate convergent validity of PREPS factors.
Magnitude of stress and associated factors
Average levels of Preparedness Stress and Perinatal Infection Stress were between 3 and 4 on the 1-5 scale (Table 2). 27.2% and 29.1% of the women scored 4 or above on the scales, respectively, indicating high levels of COVID-19 related stress. Average levels of Positive Appraisal were between 2 and 3 on the 1-5 scale (Table 2). 34.4% of the women scored less than 2 indicating low levels of Positive Appraisal.
We also investigated the association of PREPS factors with obstetric characteristics (parity and trimester) and with COVID-19 related impacts, namely COVID-19 infection (proximity, diagnosis, and perceived risk), prenatal care appointment alteration, vocational status, and financial loss (Table 1). The distinctiveness of the PREPS factors was supported by the pattern of group differences. Greater Preparedness Stress was reported by primiparas, by women in their second or third trimester versus first trimester, women who believed they might have had COVID-19 (although not medically diagnosed with it), those who lost income due to the pandemic, and by women who had prenatal care appointments cancelled or rescheduled. Greater Perinatal Infection Stress was reported by women in their second trimester versus first and third trimester, women who thought they might have had COVID-19, those who lost income due to the COVID-19 pandemic, and those who had prenatal care appointments cancelled or rescheduled. Greater Positive Appraisal was reported by primiparas, those who were in their second trimester versus those in the third trimester, those who were not essential workers, and those who lost income due to COVID-19.
Discussion
Findings indicate that the PREPS is a valid and robust instrument to assess stress experienced by pregnant women related to the COVID-19 pandemic. The PREPS confirms that the impacts of the COVID-19 pandemic on pregnant women are multidimensional and revolve around various aspects of the pandemic.6 Study results corroborate emerging findings regarding the substantial magnitude of stress and anxiety experienced by women due to the COVID-19 pandemic.6,7 Furthermore, while lower in magnitude compared to pandemic-related stress, we have evidence that women appraise some aspects of the pandemic favorably, although the lower internal consistency of this factor (most likely attributable to the small number of items in the scale23) suggests that this finding should be considered tentative.
Perceived risk of COVID-19 infection (i.e., believing one might have been infected without medical verification), but not actual diagnosis of COVID-19 infection, or proximity to someone who was diagnosed, was associated with greater pandemic-related pregnancy stress. This finding may highlight the psychological burden inherent in situations with a high degree of health uncertainty and little means of assuaging such worries (such as limited access to testing for the virus, which has been the case in some parts of the U.S.)24. Prenatal care appointment cancellation or rescheduling and COVID-19 related income loss were also associated with greater pandemic-related pregnancy stress. Women living in virus “hot-spots” with higher local rates of COVID-19 infection may have experienced particularly greater disruptions of care with associated stressful impact.
The association of positive appraisal with personal growth and not with either type of pandemic-related pregnancy stress suggests that positive appraisal may reflect a specific coping style. Positive appraisal was greatest among women who lost income due to the COVID-19 pandemic and those who identified as nonessential workers. For these women, whose everyday life has been disrupted by COVID-19 and whose vocational and financial future is unknown, focusing on the positive impact of the pandemic on their pregnancy may enable them to cope more successfully with their difficult circumstances. Findings from other research in the U.S. indicates that the COVID-19 pandemic is leading many American women to postpone childbearing25, although in contrast, a recent study from Italy suggested that pregnancy may be regarded as a way to introduce change or a positive outlook on life during the pandemic26. This evidence, coupled with our own findings that positive appraisal was more common in primiparas, highlights the need for further research focused on childbearing during the pandemic.
Clinical and research implications
The PREPS is a valuable tool for future work to identify risk and resilience factors in pregnant women during the pandemic. As the COVID-19 public health crisis evolves, additional research will be critical to evaluate the impacts of COVID-19 pandemic related stress and coping on pregnancy outcomes and mental and physical health in pregnant and postpartum women. Identifying how COVID-19 related stress is affecting pregnant women’s lives and for whom these impacts are greatest will facilitate the development of targeted interventions.
Strengths and Limitations
A strength of this study lies in its large sample of pregnant women in the U.S. from whom data were collected using robust instruments within approximately 6-8 weeks of the World Health Organization announcement1 of the COVID-19 global pandemic. The study was limited by underrepresentation of women of color. Restrictions on face-to-face human research have hindered data collection with affected individuals and increased the value of “real-time” online data such as this study. Future research should strive to collect data from racially and ethnically diverse groups and also incorporate epidemiological, interview-based assessments and medical chart data to replicate and extend these findings.
Conclusions
The COVID-19 pandemic is acutely affecting the well-being of pregnant women. The PREPS is a valid and reliable instrument to assess COVID-19 related concerns about preparedness for birth and postpartum, infection, and also positive appraisal. Situational, perceptual, vocational, and obstetric factors are associated with COVID-19 related concerns and appraisals and should be further investigated.
Funding:
This work was supported by Stony Brook University OVPR & IEDM COVID-19 Seed Grant Program. Brittain Mahaffey received support from NIH Grant K23HD092888 during preparation of this article.
Footnotes
Disclosure: The authors report no conflicts of interest.
References
- 1.World Health Organization. WHO director-general's opening remarks at the media briefing on COVID-19 11March2020. Geneva, Switzerland. 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020Accesse May 27 2020 [Google Scholar]
- 2.de Freytas-Tamura K Pregnant and scared of ‘Covid hospitals,’ they’re giving birth at home. NY Times. April21, 2020. Available from: https://www.nytimes.com/2020/04/21/nyregion/coronavirus-home-births.html?smid.Accessed May 12, 2020. [Google Scholar]
- 3.Gupta S Pregnant during a pandemic. Available from: https://www.cnn.com/2020/03/30/health/gupta-coronavirus-podcast-transcript-march-30-wellness/index.html.Accessed May 27, 2020.
- 4.Campbell AM. An increasing risk of family violence during the covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports. 2020:100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: Increased vulnerability and reduced options for support. International journal of mental health nursing. 2020. In Press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saccone G, Florio A, Aiello F, et al. Psychological impact of COVID-19 in pregnant women. American Journal of Obstetrics & Gynecology. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lobel M, Dunkel Schetter C. Pregnancy and prenatal stress. In: Freidman HS (ed.) Encyclopedia of Mental Health (Second Edition). Oxford: Academic Press; 2016:318–329. [Google Scholar]
- 8.Ibrahim SM, Lobel M. Conceptualization, measurement, and effects of pregnancy-specific stress: Review of research using the original and revised prenatal distress questionnaire. Journal of Behavioral Medicine. 2019:1–18. [DOI] [PubMed] [Google Scholar]
- 9.Currie J, Rossin-Slater M. Weathering the storm: Hurricanes and birth outcomes. Journal of Health Economics. 2013;32:487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu EM, Liu J, Tseng TH. The impact of a natural disaster on the incidence of fetal losses and pregnancy outcomes. 2015. Available from: https://uh.edu/~emliu./921/combined_manuscript.pdf.Accessed May 27, 2020. [Google Scholar]
- 11.Glynn LM, Wadhwa PD, Dunkel-Schetter C, Chicz-DeMet A, Sandman CA. When stress happens matters: Effects of earthquake timing on stress responsivity in pregnancy. American Journal of Obstetrics & Gynecology. 2001;184:637–642. [DOI] [PubMed] [Google Scholar]
- 12.Abdoli A, Falahi S, Kenarkoohi A, Shams M, Mir H, Jahromi MAM. The COVID-19 pandemic, psychological stress during pregnancy, and risk of neurodevelopmental disorders in offspring: A neglected consequence. Journal of Psychosomatic Obstetrics & Gynecology. 2020: In press. [DOI] [PubMed] [Google Scholar]
- 13.Preis H, Mahaffey B, Heiselman C, Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the COVID-19 pandemic. American Journal of Obstetrics and Gynecology-Maternal Fetal Medicine. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haines HM, Pallant JF, Karlstrom A, Hildingsson I. Cross-cultural comparison of levels of childbirth-related fear in an australian and swedish sample. Midwifery. 2011;27:560–7. [DOI] [PubMed] [Google Scholar]
- 15.Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological inquiry. 2004;15:1–18. [Google Scholar]
- 16.IBM Corp. IBM SPSS statistics for windows, version 24.0 Armonk, NY: IBM Corp. 2016. [Google Scholar]
- 17.Arbuckle JL. AMOS (version 23.0) Chicago: IBM SPSS. 2014. [Google Scholar]
- 18.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling. 1999;6:1–55. [Google Scholar]
- 19.Hoyle RH. Structural equation modeling: Concepts, issues, and applications. CA: Sage Publications; 1995. [Google Scholar]
- 20.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, eds. Testing Structural Equation Models. CA: Sage; 1993:136–162. [Google Scholar]
- 21.Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. 2007;60:34–42. [DOI] [PubMed] [Google Scholar]
- 22.Swank JM, Mullen PR. Evaluating evidence for conceptually related constructs using bivariate correlations. Measurement and Evaluation in Counseling and Development. 2017;50:270–274. [Google Scholar]
- 23.Vaske JJ, Beaman J, Sponarski CC. Rethinking internal consistency in Cronbach's alpha. Leisure Sciences. 2017;39:163–173. [Google Scholar]
- 24.Choi WHH, Lee GL, Chan CHY, Cheung RYH, Lee ILY, Chan CLW. The relationships of social support, uncertainty, self-efficacy, and commitment to prenatal psychosocial adaptation. Journal of Advanced Nursing. 2012;68:2633–2645. [DOI] [PubMed] [Google Scholar]
- 25.Lindberg LD, VandeVusse A, Mueller J, et al. , Early Impacts of the COVID-19 Pandemic: Findings from the 2020 Guttmacher Survey of Reproductive Health Experiences. New York (NY): Guttmacher Institute; 2020. [accessed 7/4/2020] https://www.guttmacher.org/report/early-impacts-covid-19-pandemic-findings-2020-guttmacher-survey-reproductive-health [Google Scholar]
- 26.Micelli E, Cito G, Cocci A, et al. , Desire for parenthood at the time of COVID-19 pandemic: an insight into the Italian situation. J Psychosom Obstet Gynecol. 2020. In press. DOI: 10.1080/0167482X.2020.1759545 [DOI] [PubMed] [Google Scholar]


