Abstract
Many high quality studies have emerged from public databases, such as Surveillance, Epidemiology, and End Results (SEER), National Health and Nutrition Examination Survey (NHANES), The Cancer Genome Atlas (TCGA), and Medical Information Mart for Intensive Care (MIMIC); however, these data are often characterized by a high degree of dimensional heterogeneity, timeliness, scarcity, irregularity, and other characteristics, resulting in the value of these data not being fully utilized. Data-mining technology has been a frontier field in medical research, as it demonstrates excellent performance in evaluating patient risks and assisting clinical decision-making in building disease-prediction models. Therefore, data mining has unique advantages in clinical big-data research, especially in large-scale medical public databases. This article introduced the main medical public database and described the steps, tasks, and models of data mining in simple language. Additionally, we described data-mining methods along with their practical applications. The goal of this work was to aid clinical researchers in gaining a clear and intuitive understanding of the application of data-mining technology on clinical big-data in order to promote the production of research results that are beneficial to doctors and patients.
Keywords: Clinical big data, Data mining, Machine learning, Medical public database, SEER, NHANES, TCGA, MIMIC
Background
With the rapid development of computer software/hardware and internet technology, the amount of data has increased at an amazing speed. “Big data” as an abstract concept currently affects all walks of life [1], and although its importance has been recognized, its definition varies slightly from field to field. In the field of computer science, big data refers to a dataset that cannot be perceived, acquired, managed, processed, or served within a tolerable time by using traditional IT and software and hardware tools. Generally, big data refers to a dataset that exceeds the scope of a simple database and data-processing architecture used in the early days of computing and is characterized by high-volume and -dimensional data that is rapidly updated represents a phenomenon or feature that has emerged in the digital age. Across the medical industry, various types of medical data are generated at a high speed, and trends indicate that applying big data in the medical field helps improve the quality of medical care and optimizes medical processes and management strategies [2, 3]. Currently, this trend is shifting from civilian medicine to military medicine. For example, the United States is exploring the potential to use of one of its largest healthcare systems (the Military Healthcare System) to provide healthcare to eligible veterans in order to potentially benefit > 9 million eligible personnel [4]. Another data-management system has been developed to assess the physical and mental health of active-duty personnel, with this expected to yield significant economic benefits to the military medical system [5]. However, in medical research, the wide variety of clinical data and differences between several medical concepts in different classification standards results in a high degree of dimensionality heterogeneity, timeliness, scarcity, and irregularity to existing clinical data [6, 7]. Furthermore, new data analysis techniques have yet to be popularized in medical research [8]. These reasons hinder the full realization of the value of existing data, and the intensive exploration of the value of clinical data remains a challenging problem.
Computer scientists have made outstanding contributions to the application of big data and introduced the concept of data mining to solve difficulties associated with such applications. Data mining (also known as knowledge discovery in databases) refers to the process of extracting potentially useful information and knowledge hidden in a large amount of incomplete, noisy, fuzzy, and random practical application data [9]. Unlike traditional research methods, several data-mining technologies mine information to discover knowledge based on the premise of unclear assumptions (i.e., they are directly applied without prior research design). The obtained information should have previously unknown, valid, and practical characteristics [9]. Data-mining technology does not aim to replace traditional statistical analysis techniques, but it does seek to extend and expand statistical analysis methodologies. From a practical point of view, machine learning (ML) is the main analytical method in data mining, as it represents a method of training models by using data and then using those models for predicting outcomes. Given the rapid progress of data-mining technology and its excellent performance in other industries and fields, it has introduced new opportunities and prospects to clinical big-data research [10]. Large amounts of high quality medical data are available to researchers in the form of public databases, which enable more researchers to participate in the process of medical data mining in the hope that the generated results can further guide clinical practice.
This article provided a valuable overview to medical researchers interested in studying the application of data mining on clinical big data. To allow a clearer understanding of the application of data-mining technology on clinical big data, the second part of this paper introduced the concept of public databases and summarized those commonly used in medical research. In the third part of the paper, we offered an overview of data mining, including introducing an appropriate model, tasks, and processes, and summarized the specific methods of data mining. In the fourth and fifth parts of this paper, we introduced data-mining algorithms commonly used in clinical practice along with specific cases in order to help clinical researchers clearly and intuitively understand the application of data-mining technology on clinical big data. Finally, we discussed the advantages and disadvantages of data mining in clinical analysis and offered insight into possible future applications.
Overview of common public medical databases
A public database describes a data repository used for research and dedicated to housing data related to scientific research on an open platform. Such databases collect and store heterogeneous and multi-dimensional health, medical, scientific research in a structured form and characteristics of mass/multi-ownership, complexity, and security. These databases cover a wide range of data, including those related to cancer research, disease burden, nutrition and health, and genetics and the environment. Table 1 summarizes the main public medical databases [11–26]. Researchers can apply for access to data based on the scope of the database and the application procedures required to perform relevant medical research.
Table 1.
Overview of main medical public database
| Database | Range | Location | Founded year | Cost | URL | References |
|---|---|---|---|---|---|---|
| Surveillance, Epidemiology, and End Results (SEER) | Tumor | USA | 1973 | Partially free | https://seer.cancer.gov/ | [11] |
| Medical Information Mart for Intensive Care (MIMIC) | Intensive medical | USA | 2001 | Free | https://mimic.physionet.org/ | [12] |
| National Health and Nutrition Examination Survey (NHANES) | Children and adults health | USA | 1999 | Free | https://wwwn.cdc.gov/nchs/nhanes/ | [13] |
| Global Burden of Disease (GBD) | Epidemic trends and burden of disease | Global | 1988 | Free | http://ghdx.healthdata.org/ | [14] |
| UK Biobank (UKB) | Health-related genetic data and phenotypic data | UK | 2006 | Partially free | https://www.ukbiobank.ac.uk/ | [15] |
| The Cancer Genome Atlas (TCGA) | Cancer genomics | USA | 2006 | Free | http://cancergenome.nih.gov/ | [16] |
| Gene Expression Omnibus (GEO) | Sequencing and gene expression | USA | 2000 | Free | https://www.ncbi.nlm.nih.gov/geo/ | [17] |
| International Cancer Genome Consortium (ICGC) | Cancer genomics | Global | 2008 | Free | https://dcc.icgc.org/ | [18] |
| China Kadoorie Biobank (CKB) | Chronic diseases | China | 2004 | Partially free | https://www.ckbiobank.org/site/ | [19] |
| Comparative Toxicogenomics Database (CTD) | Environmental chemicals and human health | USA | 2004 | Free | http://ctdbase.org/ | [20] |
| Paediatric Intensive Care (PIC) | Paediatric Intensive | China | 2010 | Free | http://pic.nbscn.org/ | [21] |
| Biologic Specimen and Data Repositories Information Coordinating Center (BioLINCC) | Cardiovascular, pulmonary, and hematological | USA | 2009 | Free | https://biolincc.nhlbi.nih.gov/ | [22] |
| China Health and Nutrition Survey (CHNS) | Health and nutrition | China | 1989 | Partially free | http://www.cpc.unc.edu/projects/china | [23] |
| China Health and Retirement Longitudinal Study (CHARLS) | Ageing and health | China | 2011 | Free | http://charls.pku.edu.cn/ | [24] |
| eICU Collaborative Research Database (eICU-CRD) | Intensive medical | USA | 2018 | Free | https://eicu-crd.mit.edu/ | [25] |
| Health and Retirement Study (HRS) | Aging health and social support | Global | 1992 | Free | https://hrs.isr.umich.edu/ | [26] |
Data mining: an overview
Data mining is a multidisciplinary field at the intersection of database technology, statistics, ML, and pattern recognition that profits from all these disciplines [27]. Although this approach is not yet widespread in the field of medical research, several studies have demonstrated the promise of data mining in building disease-prediction models, assessing patient risk, and helping physicians make clinical decisions [28–31].
Data-mining models
Data-mining has two kinds of models: descriptive and predictive. Predictive models are used to predict unknown or future values of other variables of interest, whereas descriptive models are often used to find patterns that describe data that can be interpreted by humans [32].
Data-mining tasks
A model is usually implemented by a task, with the goal of description being to generalize patterns of potential associations in the data. Therefore, using a descriptive model usually results in a few collections with the same or similar attributes. Prediction mainly refers to estimation of the variable value of a specific attribute based on the variable values of other attributes, including classification and regression [33].
Data-mining methods
After defining the data-mining model and task, the data mining methods required to build the approach based on the discipline involved are then defined. The data-mining method depends on whether or not dependent variables (labels) are present in the analysis. Predictions with dependent variables (labels) are generated through supervised learning, which can be performed by the use of linear regression, generalized linear regression, a proportional hazards model (the Cox regression model), a competitive risk model, decision trees, the random forest (RF) algorithm, and support vector machines (SVMs). In contrast, unsupervised learning involves no labels. The learning model infers some internal data structure. Common unsupervised learning methods include principal component analysis (PCA), association analysis, and clustering analysis.
Data-mining algorithms for clinical big data
Data mining based on clinical big data can produce effective and valuable knowledge, which is essential for accurate clinical decision-making and risk assessment [34]. Data-mining algorithms enable realization of these goals.
Supervised learning
A concept often mentioned in supervised learning is the partitioning of datasets. To prevent overfitting of a model, a dataset can generally be divided into two or three parts: a training set, validation set, and test set. Ripley [35] defined these parts as a set of examples used for learning and used to fit the parameters (i.e., weights) of the classifier, a set of examples used to tune the parameters (i.e., architecture) of a classifier, and a set of examples used only to assess the performance (generalized) of a fully-specified classifier, respectively. Briefly, the training set is used to train the model or determine the model parameters, the validation set is used to perform model selection, and the test set is used to verify model performance. In practice, data are generally divided into training and test sets, whereas the verification set is less involved. It should be emphasized that the results of the test set do not guarantee model correctness but only show that similar data can obtain similar results using the model. Therefore, the applicability of a model should be analysed in combination with specific problems in the research. Classical statistical methods, such as linear regression, generalized linear regression, and a proportional risk model, have been widely used in medical research. Notably, most of these classical statistical methods have certain data requirements or assumptions; however, in face of complicated clinical data, assumptions about data distribution are difficult to make. In contrast, some ML methods (algorithmic models) make no assumptions about the data and cross-verify the results; thus, they are likely to be favoured by clinical researchers [36]. For these reasons, this chapter focuses on ML methods that do not require assumptions about data distribution and classical statistical methods that are used in specific situations.
Decision tree
A decision tree is a basic classification and regression method that generates a result similar to the tree structure of a flowchart, where each tree node represents a test on an attribute, each branch represents the output of an attribute, each leaf node (decision node) represents a class or class distribution, and the topmost part of the tree is the root node [37]. The decision tree model is called a classification tree when used for classification and a regression tree when used for regression. Studies have demonstrated the utility of the decision tree model in clinical applications. In a study on the prognosis of breast cancer patients, a decision tree model and a classical logistic regression model were constructed, respectively, with the predictive performance of the different models indicating that the decision tree model showed stronger predictive power when using real clinical data [38]. Similarly, the decision tree model has been applied to other areas of clinical medicine, including diagnosis of kidney stones [39], predicting the risk of sudden cardiac arrest [40], and exploration of the risk factors of type II diabetes [41]. A common feature of these studies is the use of a decision tree model to explore the interaction between variables and classify subjects into homogeneous categories based on their observed characteristics. In fact, because the decision tree accounts for the strong interaction between variables, it is more suitable for use with decision algorithms that follow the same structure [42]. In the construction of clinical prediction models and exploration of disease risk factors and patient prognosis, the decision tree model might offer more advantages and practical application value than some classical algorithms. Although the decision tree has many advantages, it recursively separates observations into branches to construct a tree; therefore, in terms of data imbalance, the precision of decision tree models needs improvement.
The RF method
The RF algorithm was developed as an application of an ensemble-learning method based on a collection of decision trees. The bootstrap method [43] is used to randomly retrieve sample sets from the training set, with decision trees generated by the bootstrap method constituting a “random forest” and predictions based on this derived from an ensemble average or majority vote. The biggest advantage of the RF method is that the random sampling of predictor variables at each decision tree node decreases the correlation among the trees in the forest, thereby improving the precision of ensemble predictions [44]. Given that a single decision tree model might encounter the problem of overfitting [45], the initial application of RF minimizes overfitting in classification and regression and improves predictive accuracy [44]. Taylor et al. [46] highlighted the potential of RF in correctly differentiating in-hospital mortality in patients experiencing sepsis after admission to the emergency department. Nowhere in the healthcare system is the need more pressing to find methods to reduce uncertainty than in the fast, chaotic environment of the emergency department. The authors demonstrated that the predictive performance of the RF method was superior to that of traditional emergency medicine methods and the methods enabled evaluation of more clinical variables than traditional modelling methods, which subsequently allowed the discovery of clinical variables not expected to be of predictive value or which otherwise would have been omitted as a rare predictor [46]. Another study based on the Medical Information Mart for Intensive Care (MIMIC) II database [47] found that RF had excellent predictive power regarding intensive care unit (ICU) mortality [48]. These studies showed that the application of RF to big data stored in the hospital healthcare system provided a new data-driven method for predictive analysis in critical care. Additionally, random survival forests have recently been developed to analyse survival data, especially right-censored survival data [49, 50], which can help researchers conduct survival analyses in clinical oncology and help develop personalized treatment regimens that benefit patients [51].
SVMs
The SVM is a relatively new classification or prediction method developed by Cortes and Vapnik and represents a data-driven approach that does not require assumptions about data distribution [52]. The core purpose of an SVM is to identify a separation boundary (called a hyperplane) to help classify cases; thus, the advantages of SVMs are obvious when classifying and predicting cases based on high dimensional data or data with a small sample size [53, 54].
In a study of drug compliance in patients with heart failure, researchers used an SVM to build a predictive model for patient compliance in order to overcome the problem of a large number of input variables relative to the number of available observations [55]. Additionally, the mechanisms of certain chronic and complex diseases observed in clinical practice remain unclear, and many risk factors, including gene–gene interactions and gene-environment interactions, must be considered in the research of such diseases [55, 56]. SVMs are capable of addressing these issues. Yu et al. [54] applied an SVM for predicting diabetes onset based on data from the National Health and Nutrition Examination Survey (NHANES). Furthermore, these models have strong discrimination ability, making SVMs a promising classification approach for detecting individuals with chronic and complex diseases. However, a disadvantage of SVMs is that when the number of observation samples is large, the method becomes time- and resource-intensive, which is often highly inefficient.
Competitive risk model
Kaplan–Meier marginal regression and the Cox proportional hazards model are widely used in survival analysis in clinical studies. Classical survival analysis usually considers only one endpoint, such as the impact of patient survival time. However, in clinical medical research, multiple endpoints usually coexist, and these endpoints compete with one another to generate competitive risk data [57]. In the case of multiple endpoint events, the use of a single endpoint-analysis method can lead to a biased estimation of the probability of endpoint events due to the existence of competitive risks [58]. The competitive risk model is a classical statistical model based on the hypothesis of data distribution. Its main advantage is its accurate estimation of the cumulative incidence of outcomes for right-censored survival data with multiple endpoints [59]. In data analysis, the cumulative risk rate is estimated using the cumulative incidence function in single-factor analysis, and Gray’s test is used for between-group comparisons [60].
Multifactor analysis uses the Fine-Gray and cause-specific (CS) risk models to explore the cumulative risk rate [61]. The difference between the Fine-Gray and CS models is that the former is applicable to establishing a clinical prediction model and predicting the risk of a single endpoint of interest [62], whereas the latter is suitable for answering etiological questions, where the regression coefficient reflects the relative effect of covariates on the increased incidence of the main endpoint in the target event-free risk set [63]. Currently, in databases with CS records, such as Surveillance, Epidemiology, and End Results (SEER), competitive risk models exhibit good performance in exploring disease-risk factors and prognosis [64]. A study of prognosis in patients with oesophageal cancer from SEER showed that Cox proportional risk models might misestimate the effects of age and disease location on patient prognosis, whereas competitive risk models provide more accurate estimates of factors affecting patient prognosis [65]. In another study of the prognosis of penile cancer patients, researchers found that using a competitive risk model was more helpful in developing personalized treatment plans [66].
Unsupervised learning
In many data-analysis processes, the amount of usable identified data is small, and identifying data is a tedious process [67]. Unsupervised learning is necessary to judge and categorize data according to similarities, characteristics, and correlations and has three main applications: data clustering, association analysis, and dimensionality reduction. Therefore, the unsupervised learning methods introduced in this section include clustering analysis, association rules, and PCA.
Clustering analysis
The classification algorithm needs to “know” information concerning each category in advance, with all of the data to be classified having corresponding categories. When the above conditions cannot be met, cluster analysis can be applied to solve the problem [68]. Clustering places similar objects into different categories or subsets through the process of static classification. Consequently, objects in the same subset have similar properties. Many kinds of clustering techniques exist. Here, we introduced the four most commonly used clustering techniques.
Partition clustering
The core idea of this clustering method regards the centre of the data point as the centre of the cluster. The k-means method [69] is a representative example of this technique. The k-means method takes n observations and an integer, k, and outputs a partition of the n observations into k sets such that each observation belongs to the cluster with the nearest mean [70]. The k-means method exhibits low time complexity and high computing efficiency but has a poor processing effect on high dimensional data and cannot identify nonspherical clusters.
Hierarchical clustering
The hierarchical clustering algorithm decomposes a dataset hierarchically to facilitate the subsequent clustering [71]. Common algorithms for hierarchical clustering include BIRCH [72], CURE [73], and ROCK [74]. The algorithm starts by treating every point as a cluster, with clusters grouped according to closeness. When further combinations result in unexpected results under multiple causes or only one cluster remains, the grouping process ends. This method has wide applicability, and the relationship between clusters is easy to detect; however, the time complexity is high [75].
Clustering according to density
The density algorithm takes areas presenting a high degree of data density and defines these as belonging to the same cluster [76]. This method aims to find arbitrarily-shaped clusters, with the most representative algorithm being DBSCAN [77]. In practice, DBSCAN does not need to input the number of clusters to be partitioned and can handle clusters of various shapes; however, the time complexity of the algorithm is high. Furthermore, when data density is irregular, the quality of the clusters decreases; thus, DBSCAN cannot process high dimensional data [75].
Clustering according to a grid
Neither partition nor hierarchical clustering can identify clusters with nonconvex shapes. Although a dimension-based algorithm can accomplish this task, the time complexity is high. To address this problem, data-mining researchers proposed grid-based algorithms that changed the original data space into a grid structure of a certain size. A representative algorithm is STING, which divides the data space into several square cells according to different resolutions and clusters the data of different structure levels [78]. The main advantage of this method is its high processing speed and its exclusive dependence on the number of units in each dimension of the quantized space.
In clinical studies, subjects tend to be actual patients. Although researchers adopt complex inclusion and exclusion criteria before determining the subjects to be included in the analyses, heterogeneity among different patients cannot be avoided [79, 80]. The most common application of cluster analysis in clinical big data is in classifying heterogeneous mixed groups into homogeneous groups according to the characteristics of existing data (i.e., “subgroups” of patients or observed objects are identified) [81, 82]. This new information can then be used in the future to develop patient-oriented medical-management strategies. Docampo et al. [81] used hierarchical clustering to reduce heterogeneity and identify subgroups of clinical fibromyalgia, which aided the evaluation and management of fibromyalgia. Additionally, Guo et al. [83] used k-means clustering to divide patients with essential hypertension into four subgroups, which revealed that the potential risk of coronary heart disease differed between different subgroups. On the other hand, density- and grid-based clustering algorithms have mostly been used to process large numbers of images generated in basic research and clinical practice, with current studies focused on developing new tools to help clinical research and practices based on these technologies [84, 85]. Cluster analysis will continue to have extensive application prospects along with the increasing emphasis on personalized treatment.
Association rules
Association rules discover interesting associations and correlations between item sets in large amounts of data. These rules were first proposed by Agrawal et al. [86] and applied to analyse customer buying habits to help retailers create sales plans. Data-mining based on association rules identifies association rules in a two-step process: 1) all high frequency items in the collection are listed and 2) frequent association rules are generated based on the high frequency items [87]. Therefore, before association rules can be obtained, sets of frequent items must be calculated using certain algorithms. The Apriori algorithm is based on the a priori principle of finding all relevant adjustment items in a database transaction that meet a minimum set of rules and restrictions or other restrictions [88]. Other algorithms are mostly variants of the Apriori algorithm [64]. The Apriori algorithm must scan the entire database every time it scans the transaction; therefore, algorithm performance deteriorates as database size increases [89], making it potentially unsuitable for analysing large databases. The frequent pattern (FP) growth algorithm was proposed to improve efficiency. After the first scan, the FP algorithm compresses the frequency set in the database into a FP tree while retaining the associated information and then mines the conditional libraries separately [90]. Association-rule technology is often used in medical research to identify association rules between disease risk factors (i.e., exploration of the joint effects of disease risk factors and combinations of other risk factors). For example, Li et al. [91] used the association-rule algorithm to identify the most important stroke risk factor as atrial fibrillation, followed by diabetes and a family history of stroke. Based on the same principle, association rules can also be used to evaluate treatment effects and other aspects. For example, Guo et al. [92] used the FP algorithm to generate association rules and evaluate individual characteristics and treatment effects of patients with diabetes, thereby reducing the readability rate of patients with diabetes. Association rules reveal a connection between premises and conclusions; however, the reasonable and reliable application of information can only be achieved through validation by experienced medical professionals and through extensive causal research [92].
PCA
PCA is a widely used data-mining method that aims to reduce data dimensionality in an interpretable way while retaining most of the information present in the data [93, 94]. The main purpose of PCA is descriptive, as it requires no assumptions about data distribution and is, therefore, an adaptive and exploratory method. During the process of data analysis, the main steps of PCA include standardization of the original data, calculation of a correlation coefficient matrix, calculation of eigenvalues and eigenvectors, selection of principal components, and calculation of the comprehensive evaluation value. PCA does not often appear as a separate method, as it is often combined with other statistical methods [95]. In practical clinical studies, the existence of multicollinearity often leads to deviation from multivariate analysis. A feasible solution is to construct a regression model by PCA, which replaces the original independent variables with each principal component as a new independent variable for regression analysis, with this most commonly seen in the analysis of dietary patterns in nutritional epidemiology [96]. In a study of socioeconomic status and child-developmental delays, PCA was used to derive a new variable (the household wealth index) from a series of household property reports and incorporate this new variable as the main analytical variable into the logistic regression model [97]. Additionally, PCA can be combined with cluster analysis. Burgel et al. [98] used PCA to transform clinical data to address the lack of independence between existing variables used to explore the heterogeneity of different subtypes of chronic obstructive pulmonary disease. Therefore, in the study of subtypes and heterogeneity of clinical diseases, PCA can eliminate noisy variables that can potentially corrupt the cluster structure, thereby increasing the accuracy of the results of clustering analysis [98, 99].
The data-mining process and examples of its application using common public databases
Open-access databases have the advantages of large volumes of data, wide data coverage, rich data information, and a cost-efficient method of research, making them beneficial to medical researchers. In this chapter, we introduced the data-mining process and methods and their application in research based on examples of utilizing public databases and data-mining algorithms.
The data-mining process
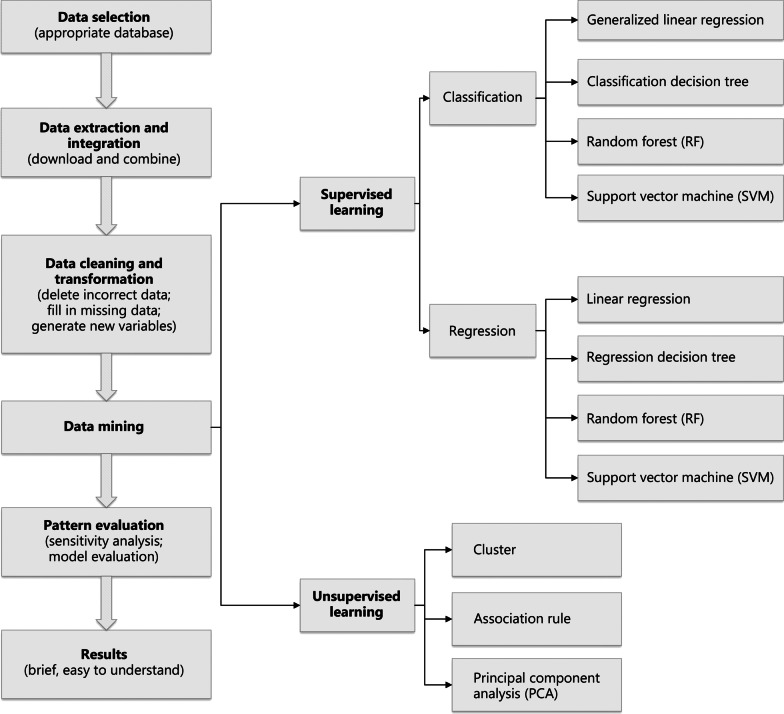
Figure 1 shows a series of research concepts. The data-mining process is divided into several steps: (1) database selection according to the research purpose; (2) data extraction and integration, including downloading the required data and combining data from multiple sources; (3) data cleaning and transformation, including removal of incorrect data, filling in missing data, generating new variables, converting data format, and ensuring data consistency; (4) data mining, involving extraction of implicit relational patterns through traditional statistics or ML; (5) pattern evaluation, which focuses on the validity parameters and values of the relationship patterns of the extracted data; and (6) assessment of the results, involving translation of the extracted data-relationship model into comprehensible knowledge made available to the public.
Fig. 1.
The steps of data mining in medical public database
Examples of data-mining applied using public databases
Establishment of warning models for the early prediction of disease
A previous study identified sepsis as a major cause of death in ICU patients [100]. The authors noted that the predictive model developed previously used a limited number of variables, and that model performance required improvement. The data-mining process applied to address these issues was, as follows: (1) data selection using the MIMIC III database; (2) extraction and integration of three types of data, including multivariate features (demographic information and clinical biochemical indicators), time series data (temperature, blood pressure, and heart rate), and clinical latent features (various scores related to disease); (3) data cleaning and transformation, including fixing irregular time series measurements, estimating missing values, deleting outliers, and addressing data imbalance; (4) data mining through the use of logical regression, generation of a decision tree, application of the RF algorithm, an SVM, and an ensemble algorithm (a combination of multiple classifiers) to established the prediction model; (5) pattern evaluation using sensitivity, precision, and the area under the receiver operating characteristic curve to evaluate model performance; and (6) evaluation of the results, in this case the potential to predicting the prognosis of patients with sepsis and whether the model outperformed current scoring systems.
Exploring prognostic risk factors in cancer patients
Wu et al. [101] noted that traditional survival-analysis methods often ignored the influence of competitive risk events, such as suicide and car accident, on outcomes, leading to deviations and misjudgements in estimating the effect of risk factors. They used the SEER database, which offers cause-of-death data for cancer patients, and a competitive risk model to address this problem according to the following process: (1) data were obtained from the SEER database; (2) demography, clinical characteristics, treatment modality, and cause of death of cecum cancer patients were extracted from the database; (3) patient data were deleted when there were no demographic, clinical, therapeutic, or cause-of-death variables; (4) Cox regression and two kinds of competitive risk models were applied for survival analysis; (5) the results were compared between three different models; and (6) the results revealed that for survival data with multiple endpoints, the competitive risk model was more favourable.
Derivation of dietary patterns
A study by Martínez Steele et al. [102] applied PCA for nutritional epidemiological analysis to determine dietary patterns and evaluate the overall nutritional quality of the population based on those patterns. Their process involved the following: (1) data were extracted from the NHANES database covering the years 2009–2010; (2) demographic characteristics and two 24 h dietary recall interviews were obtained; (3) data were weighted and excluded based on subjects not meeting specific criteria; (4) PCA was used to determine dietary patterns in the United States population, and Gaussian regression and restricted cubic splines were used to assess associations between ultra-processed foods and nutritional balance; (5) eigenvalues, scree plots, and the interpretability of the principal components were reviewed to screen and evaluate the results; and (6) the results revealed a negative association between ultra-processed food intake and overall dietary quality. Their findings indicated that a nutritionally balanced eating pattern was characterized by a diet high in fibre, potassium, magnesium, and vitamin C intake along with low sugar and saturated fat consumption.
Conclusion
The use of “big data” has changed multiple aspects of modern life, with its use combined with data-mining methods capable of improving the status quo [86]. The aim of this study was to aid clinical researchers in understanding the application of data-mining technology on clinical big data and public medical databases to further their research goals in order to benefit clinicians and patients. The examples provided offer insight into the data-mining process applied for the purposes of clinical research. Notably, researchers have raised concerns that big data and data-mining methods were not a perfect fit for adequately replicating actual clinical conditions, with the results potentially capable of misleading doctors and patients [86]. Therefore, given the rate at which new technologies and trends progress, it is necessary to maintain a positive attitude concerning their potential impact while remaining cautious in examining the results provided by their application.
In the future, the healthcare system will need to utilize increasingly larger volumes of big data with higher dimensionality. The tasks and objectives of data analysis will also have higher demands, including higher degrees of visualization, results with increased accuracy, and stronger real-time performance. As a result, the methods used to mine and process big data will continue to improve. Furthermore, to increase the formality and standardization of data-mining methods, it is possible that a new programming language specifically for this purpose will need to be developed, as well as novel methods capable of addressing unstructured data, such as graphics, audio, and text represented by handwriting. In terms of application, the development of data-management and disease-screening systems for large-scale populations, such as the military, will help determine the best interventions and formulation of auxiliary standards capable of benefitting both cost-efficiency and personnel. Data-mining technology can also be applied to hospital management in order to improve patient satisfaction, detect medical-insurance fraud and abuse, and reduce costs and losses while improving management efficiency. Currently, this technology is being applied for predicting patient disease, with further improvements resulting in the increased accuracy and speed of these predictions. Moreover, it is worth noting that technological development will concomitantly require higher quality data, which will be a prerequisite for accurate application of the technology.
Finally, the ultimate goal of this study was to explain the methods associated with data mining and commonly used to process clinical big data. This review will potentially promote further study and aid doctors and patients.
Abbreviations
- BioLINCC
Biologic Specimen and Data Repositories Information Coordinating Center
- CHARLS
China Health and Retirement Longitudinal Study
- CHNS
China Health and Nutrition Survey
- CKB
China Kadoorie Biobank
- CS
Cause-specific risk
- CTD
Comparative Toxicogenomics Database
- eICU-CRD
EICU Collaborative Research Database
- FP
Frequent pattern
- GBD
Global burden of disease
- GEO
Gene expression omnibus
- HRS
Health and Retirement Study
- ICGC
International Cancer Genome Consortium
- MIMIC
Medical Information Mart for Intensive Care
- ML
Machine learning
- NHANES
National Health and Nutrition Examination Survey
- PCA
Principal component analysis
- PIC
Paediatric intensive care
- RF
Random forest
- SEER
Surveillance, epidemiology, and end results
- SVM
Support vector machine
- TCGA
The Cancer Genome Atlas
- UKB
UK Biobank
Authors’ contributions
WTW, YJL and JL designed the review. JL, AZF, TH, LL and ADX reviewed and criticized the original paper. All authors read and approved the final manuscript.
Funding
This study was supported by the National Social Science Foundation of China (No. 16BGL183).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Wen-Tao Wu and Yuan-Jie Li have contributed equally to this work
Contributor Information
Wen-Tao Wu, Email: 15680833716@163.com.
Yuan-Jie Li, Email: liyj2010@xjtu.edu.c.
Ao-Zi Feng, Email: 15838129317@163.com.
Li Li, Email: lily_1021@yeah.net.
Tao Huang, Email: htao36@163.com.
An-Ding Xu, Email: tlil@jnu.edu.cn.
Jun Lyu, Email: lyujun2020@jnu.edu.cn.
References
- 1.Herland M, Khoshgoftaar TM, Wald R. A review of data mining using big data in health informatics. J Big Data. 2014;1(1):1–35. doi: 10.1186/2196-1115-1-2. [DOI] [Google Scholar]
- 2.Wang F, Zhang P, Wang X, Hu J. Clinical risk prediction by exploring high-order feature correlations. AMIA Annu Symp Proc. 2014;2014:1170–1179. [PMC free article] [PubMed] [Google Scholar]
- 3.Xu R, Li L, Wang Q. dRiskKB: a large-scale disease-disease risk relationship knowledge base constructed from biomedical text. BMC Bioinform. 2014;15:105. doi: 10.1186/1471-2105-15-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramachandran S, Erraguntla M, Mayer R, Benjamin P, Editors. Data mining in military health systems-clinical and administrative applications. In: 2007 IEEE international conference on automation science and engineering; 2007. 10.1109/COASE.2007.4341764.
- 5.Vie LL, Scheier LM, Lester PB, Ho TE, Labarthe DR, Seligman MEP. The US army person-event data environment: a military-civilian big data enterprise. Big Data. 2015;3(2):67–79. doi: 10.1089/big.2014.0055. [DOI] [PubMed] [Google Scholar]
- 6.Mohan A, Blough DM, Kurc T, Post A, Saltz J. Detection of conflicts and inconsistencies in taxonomy-based authorization policies. IEEE Int Conf Bioinform Biomed. 2012;2011:590–594. doi: 10.1109/BIBM.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo J, Wu M, Gopukumar D, Zhao Y. Big data application in biomedical research and health care: a literature review. Biomed Inform Insights. 2016;8:1–10. doi: 10.4137/BII.S31559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellazzi R, Zupan B. Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform. 2008;77(2):81–97. doi: 10.1016/j.ijmedinf.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Sahu H, Shrma S, Gondhalakar S. A brief overview on data mining survey. Int J Comput Technol Electron Eng. 2011;1(3):114–121. [Google Scholar]
- 10.Obermeyer Z, Emanuel EJ. Predicting the future - big data, machine learning, and clinical medicine. N Engl J Med. 2016;375(13):1216–1219. doi: 10.1056/NEJMp1606181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doll KM, Rademaker A, Sosa JA. Practical guide to surgical data sets: surveillance, epidemiology, and end results (SEER) database. JAMA Surg. 2018;153(6):588–589. doi: 10.1001/jamasurg.2018.0501. [DOI] [PubMed] [Google Scholar]
- 12.Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7(1):121–134. doi: 10.3945/an.115.009258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palmer LJ. UK Biobank: Bank on it. Lancet. 2007;369(9578):1980–1982. doi: 10.1016/S0140-6736(07)60924-6. [DOI] [PubMed] [Google Scholar]
- 16.Cancer Genome Atlas Research Network, Weinstein JN, Collisson EA, Mills GB, Shaw KR, Ozenberger BA, et al. The cancer genome atlas pan-cancer analysis project. Nat Genet. 2013;45(10):1113–20. 10.1038/ng.2764. [DOI] [PMC free article] [PubMed]
- 17.Davis S, Meltzer PS. GEOquery: a bridge between the Gene Expression Omnibus (GEO) and BioConductor. Bioinformatics. 2007;23(14):1846–1847. doi: 10.1093/bioinformatics/btm254. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J, Bajari R, Andric D, Gerthoffert F, Lepsa A, Nahal-Bose H, et al. The international cancer genome consortium data portal. Nat Biotechnol. 2019;37(4):367–369. doi: 10.1038/s41587-019-0055-9. [DOI] [PubMed] [Google Scholar]
- 19.Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis AP, Grondin CJ, Johnson RJ, Sciaky D, McMorran R, Wiegers J, et al. The comparative toxicogenomics database: update 2019. Nucleic Acids Res. 2019;47(D1):D948–D954. doi: 10.1093/nar/gky868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng X, Yu G, Lu Y, Tan L, Wu X, Shi S, et al. PIC, a paediatric-specific intensive care database. Sci Data. 2020;7(1):14. doi: 10.1038/s41597-020-0355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giffen CA, Carroll LE, Adams JT, Brennan SP, Coady SA, Wagner EL. Providing contemporary access to historical biospecimen collections: development of the NHLBI Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) Biopreserv Biobank. 2015;13(4):271–279. doi: 10.1089/bio.2014.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2014;15(Suppl 1):2–7. doi: 10.1111/obr.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS) Int J Epidemiol. 2014;43(1):61–68. doi: 10.1093/ije/dys203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU collaborative research database, a freely available multi-centre database for critical care research. Sci Data. 2018;5:180178. doi: 10.1038/sdata.2018.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher GG, Ryan LH. Overview of the health and retirement study and introduction to the special issue. Work Aging Retire. 2018;4(1):1–9. doi: 10.1093/workar/wax032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iavindrasana J, Cohen G, Depeursinge A, Müller H, Meyer R, Geissbuhler A. Clinical data mining: a review. Yearb Med Inform. 2009:121–33. [PubMed]
- 28.Zhang Y, Guo SL, Han LN, Li TL. Application and exploration of big data mining in clinical medicine. Chin Med J. 2016;129(6):731–738. doi: 10.4103/0366-6999.178019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ngiam KY, Khor IW. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. 2019;20(5):e262–e273. doi: 10.1016/S1470-2045(19)30149-4. [DOI] [PubMed] [Google Scholar]
- 30.Huang C, Murugiah K, Mahajan S, Li S-X, Dhruva SS, Haimovich JS, et al. Enhancing the prediction of acute kidney injury risk after percutaneous coronary intervention using machine learning techniques: a retrospective cohort study. PLoS Med. 2018;15(11):e1002703. doi: 10.1371/journal.pmed.1002703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahimian F, Salimi-Khorshidi G, Payberah AH, Tran J, Ayala Solares R, Raimondi F, et al. Predicting the risk of emergency admission with machine learning: development and validation using linked electronic health records. PLoS Med. 2018;15(11):e1002695. doi: 10.1371/journal.pmed.1002695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kantardzic M. Data Mining: concepts, models, methods, and algorithms. Technometrics. 2003;45(3):277. [Google Scholar]
- 33.Jothi N, Husain W. Data mining in healthcare—a review. Procedia Comput Sci. 2015;72:306–313. doi: 10.1016/j.procs.2015.12.145. [DOI] [Google Scholar]
- 34.Piatetsky-Shapiro G, Tamayo P. Microarray data mining: facing the challenges. SIGKDD. 2003;5(2):1–5. doi: 10.1145/980972.980974. [DOI] [Google Scholar]
- 35.Ripley BD. Pattern recognition and neural networks. Cambridge: Cambridge University Press; 1996. [Google Scholar]
- 36.Arlot S, Celisse A. A survey of cross-validation procedures for model selection. Stat Surv. 2010;4:40–79. doi: 10.1214/09-SS054. [DOI] [Google Scholar]
- 37.Shouval R, Bondi O, Mishan H, Shimoni A, Unger R, Nagler A. Application of machine learning algorithms for clinical predictive modelling: a data-mining approach in SCT. Bone Marrow Transp. 2014;49(3):332–337. doi: 10.1038/bmt.2013.146. [DOI] [PubMed] [Google Scholar]
- 38.Momenyan S, Baghestani AR, Momenyan N, Naseri P, Akbari ME. Survival prediction of patients with breast cancer: comparisons of decision tree and logistic regression analysis. Int J Cancer Manag. 2018;11(7):e9176. doi: 10.5812/ijcm.9176. [DOI] [Google Scholar]
- 39.Topaloğlu M, Malkoç G. Decision tree application for renal calculi diagnosis. Int J Appl Math Electron Comput. 2016. 10.18100/ijamec.281134.
- 40.Li H, Wu TT, Yang DL, Guo YS, Liu PC, Chen Y, et al. Decision tree model for predicting in-hospital cardiac arrest among patients admitted with acute coronary syndrome. Clin Cardiol. 2019;42(11):1087–1093. doi: 10.1002/clc.23255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ramezankhani A, Hadavandi E, Pournik O, Shahrabi J, Azizi F, Hadaegh F. Decision tree-based modelling for identification of potential interactions between type 2 diabetes risk factors: a decade follow-up in a Middle East prospective cohort study. BMJ Open. 2016;6(12):e013336. doi: 10.1136/bmjopen-2016-013336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carmona-Bayonas A, Jiménez-Fonseca P, Font C, Fenoy F, Otero R, Beato C, et al. Predicting serious complications in patients with cancer and pulmonary embolism using decision tree modelling: the EPIPHANY Index. Br J Cancer. 2017;116(8):994–1001. doi: 10.1038/bjc.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Efron B. Bootstrap methods: another look at the jackknife. In: Kotz S, Johnson NL, editors. Breakthroughs in statistics. New York: Springer; 1992. pp. 569–593. [Google Scholar]
- 44.Breima L. Random forests. Mach Learn. 2010;1(45):5–32. doi: 10.1023/A:1010933404324. [DOI] [Google Scholar]
- 45.Franklin J. The elements of statistical learning: data mining, inference and prediction. Math Intell. 2005;27(2):83–85. doi: 10.1007/BF02985802. [DOI] [Google Scholar]
- 46.Taylor RA, Pare JR, Venkatesh AK, Mowafi H, Melnick ER, Fleischman W, et al. Prediction of in-hospital mortality in emergency department patients with sepsis: a local big data-driven, machine learning approach. Acad Emerg Med. 2016;23(3):269–278. doi: 10.1111/acem.12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee J, Scott DJ, Villarroel M, Clifford GD, Saeed M, Mark RG. Open-access MIMIC-II database for intensive care research. Annu Int Conf IEEE Eng Med Biol Soc. 2011:8315–8. 10.1109/IEMBS.2011.6092050. [DOI] [PMC free article] [PubMed]
- 48.Lee J. Patient-specific predictive modelling using random forests: an observational study for the critically Ill. JMIR Med Inform. 2017;5(1):e3. doi: 10.2196/medinform.6690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wongvibulsin S, Wu KC, Zeger SL. Clinical risk prediction with random forests for survival, longitudinal, and multivariate (RF-SLAM) data analysis. BMC Med Res Methodol. 2019;20(1):1. doi: 10.1186/s12874-019-0863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Taylor JMG. Random survival forests. J Thorac Oncol. 2011;6(12):1974–1975. doi: 10.1097/JTO.0b013e318233d835. [DOI] [PubMed] [Google Scholar]
- 51.Hu C, Steingrimsson JA. Personalized risk prediction in clinical oncology research: applications and practical issues using survival trees and random forests. J Biopharm Stat. 2018;28(2):333–349. doi: 10.1080/10543406.2017.1377730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dietrich R, Opper M, Sompolinsky H. Statistical mechanics of support vector networks. Phys Rev Lett. 1999;82(14):2975. doi: 10.1103/PhysRevLett.82.2975. [DOI] [Google Scholar]
- 53.Verplancke T, Van Looy S, Benoit D, Vansteelandt S, Depuydt P, De Turck F, et al. Support vector machine versus logistic regression modelling for prediction of hospital mortality in critically ill patients with haematological malignancies. BMC Med Inform Decis Mak. 2008;8:56. doi: 10.1186/1472-6947-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu W, Liu T, Valdez R, Gwinn M, Khoury MJ. Application of support vector machine modelling for prediction of common diseases: the case of diabetes and pre-diabetes. BMC Med Inform Decis Mak. 2010;10:16. doi: 10.1186/1472-6947-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Son YJ, Kim HG, Kim EH, Choi S, Lee SK. Application of support vector machine for prediction of medication adherence in heart failure patients. Healthc Inform Res. 2010;16(4):253–259. doi: 10.4258/hir.2010.16.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schadt EE, Friend SH, Shaywitz DA. A network view of disease and compound screening. Nat Rev Drug Discov. 2009;8(4):286–295. doi: 10.1038/nrd2826. [DOI] [PubMed] [Google Scholar]
- 57.Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133(6):601–609. doi: 10.1161/CIRCULATIONAHA.115.017719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26(11):2389–2430. doi: 10.1002/sim.2712. [DOI] [PubMed] [Google Scholar]
- 59.Klein JP. Competing risks. WIREs Comp Stat. 2010;2(3):333–339. doi: 10.1002/wics.83. [DOI] [Google Scholar]
- 60.Haller B, Schmidt G, Ulm K. Applying competing risks regression models: an overview. Lifetime Data Anal. 2013;19(1):33–58. doi: 10.1007/s10985-012-9230-8. [DOI] [PubMed] [Google Scholar]
- 61.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. doi: 10.1080/01621459.1999.10474144. [DOI] [Google Scholar]
- 62.Koller MT, Raatz H, Steyerberg EW, Wolbers M. Competing risks and the clinical community: irrelevance or ignorance? Stat Med. 2012;31(11–12):1089–1097. doi: 10.1002/sim.4384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170(2):244–256. doi: 10.1093/aje/kwp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang J, Li Y, Liu Q, Li L, Feng A, Wang T, et al. Brief introduction of medical database and data mining technology in big data era. J Evid Based Med. 2020;13(1):57–69. doi: 10.1111/jebm.12373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yu Z, Yang J, Gao L, Huang Q, Zi H, Li X. A competing risk analysis study of prognosis in patients with esophageal carcinoma 2006–2015 using data from the surveillance, epidemiology, and end results (SEER) database. Med Sci Monit. 2020;26:e918686. doi: 10.12659/MSM.918686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang J, Pan Z, He Y, Zhao F, Feng X, Liu Q, et al. Competing-risks model for predicting the prognosis of penile cancer based on the SEER database. Cancer Med. 2019;8(18):7881–7889. doi: 10.1002/cam4.2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Miotto R, Wang F, Wang S, Jiang X, Dudley JT. Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform. 2018;19(6):1236–1246. doi: 10.1093/bib/bbx044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alashwal H, El Halaby M, Crouse JJ, Abdalla A, Moustafa AA. The application of unsupervised clustering methods to Alzheimer's disease. Front Comput Neurosci. 2019;13:31. doi: 10.3389/fncom.2019.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Macqueen J. Some methods for classification and analysis of multivariate observations. In: Proceedings of the fifth Berkeley symposium on mathematical statistics and probability, Oakland, CA: University of California Press;1967.
- 70.Forgy EW. Cluster analysis of multivariate data: efficiency versus interpretability of classifications. Biometrics. 1965;21:768–769. [Google Scholar]
- 71.Johnson SC. Hierarchical clustering schemes. Psychometrika. 1967;32(3):241–254. doi: 10.1007/BF02289588. [DOI] [PubMed] [Google Scholar]
- 72.Zhang T, Ramakrishnan R, Livny M. BIRCH: an efficient data clustering method for very large databases. ACM SIGMOD Rec. 1996;25(2):103–114. doi: 10.1145/235968.233324. [DOI] [Google Scholar]
- 73.Guha S, Rastogi R, Shim K. CURE: an efficient clustering algorithm for large databases. ACM SIGMOD Rec. 1998;27(2):73–84. doi: 10.1145/276305.276312. [DOI] [Google Scholar]
- 74.Guha S, Rastogi R, Shim K. ROCK: a robust clustering algorithm for categorical attributes. Inf Syst. 2000;25(5):345–366. doi: 10.1016/S0306-4379(00)00022-3. [DOI] [Google Scholar]
- 75.Xu D, Tian Y. A comprehensive survey of clustering algorithms. Ann Data Sci. 2015;2(2):165–193. doi: 10.1007/s40745-015-0040-1. [DOI] [Google Scholar]
- 76.Kriegel HP, Kröger P, Sander J, Zimek A. Density-based clustering. WIRES Data Min Knowl. 2011;1(3):231–240. doi: 10.1002/widm.30. [DOI] [Google Scholar]
- 77.Ester M, Kriegel HP, Sander J, Xu X, editors. A density-based algorithm for discovering clusters in large spatial databases with noise. In: Proceedings of 2nd international conference on knowledge discovery and data mining Portland, Oregon: AAAI Press; 1996. p. 226–31.
- 78.Wang W, Yang J, Muntz RR. STING: a statistical information grid approach to spatial data mining. In: Proceedings of the 23rd international conference on very large data bases, Morgan Kaufmann Publishers Inc.; 1997. p. 186–95.
- 79.Iwashyna TJ, Burke JF, Sussman JB, Prescott HC, Hayward RA, Angus DC. Implications of heterogeneity of treatment effect for reporting and analysis of randomized trials in critical care. Am J Respir Crit Care Med. 2015;192(9):1045–1051. doi: 10.1164/rccm.201411-2125CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ruan S, Lin H, Huang C, Kuo P, Wu H, Yu C. Exploring the heterogeneity of effects of corticosteroids on acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care. 2014;18(2):R63. doi: 10.1186/cc13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Docampo E, Collado A, Escaramís G, Carbonell J, Rivera J, Vidal J, et al. Cluster analysis of clinical data identifies fibromyalgia subgroups. PLoS ONE. 2013;8(9):e74873. doi: 10.1371/journal.pone.0074873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sutherland ER, Goleva E, King TS, Lehman E, Stevens AD, Jackson LP, et al. Cluster analysis of obesity and asthma phenotypes. PLoS ONE. 2012;7(5):e36631. doi: 10.1371/journal.pone.0036631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guo Q, Lu X, Gao Y, Zhang J, Yan B, Su D, et al. Cluster analysis: a new approach for identification of underlying risk factors for coronary artery disease in essential hypertensive patients. Sci Rep. 2017;7:43965. doi: 10.1038/srep43965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hastings S, Oster S, Langella S, Kurc TM, Pan T, Catalyurek UV, et al. A grid-based image archival and analysis system. J Am Med Inform Assoc. 2005;12(3):286–295. doi: 10.1197/jamia.M1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Celebi ME, Aslandogan YA, Bergstresser PR. Mining biomedical images with density-based clustering. In: International conference on information technology: coding and computing (ITCC’05), vol II. Washington, DC, USA: IEEE; 2005. 10.1109/ITCC.2005.196.
- 86.Agrawal R, Imieliński T, Swami A, editors. Mining association rules between sets of items in large databases. In: Proceedings of the ACM SIGMOD conference on management of data. Washington, DC, USA: Association for Computing Machinery; 1993. p. 207–16. 10.1145/170035.170072.
- 87.Sethi A, Mahajan P. Association rule mining: A review. TIJCSA. 2012;1(9):72–83. [Google Scholar]
- 88.Kotsiantis S, Kanellopoulos D. Association rules mining: a recent overview. GESTS Int Trans Comput Sci Eng. 2006;32(1):71–82. [Google Scholar]
- 89.Narvekar M, Syed SF. An optimized algorithm for association rule mining using FP tree. Procedia Computer Sci. 2015;45:101–110. doi: 10.1016/j.procs.2015.03.097. [DOI] [Google Scholar]
- 90.Verhein F. Frequent pattern growth (FP-growth) algorithm. Sydney: The University of Sydney; 2008. pp. 1–16. [Google Scholar]
- 91.Li Q, Zhang Y, Kang H, Xin Y, Shi C. Mining association rules between stroke risk factors based on the Apriori algorithm. Technol Health Care. 2017;25(S1):197–205. doi: 10.3233/THC-171322. [DOI] [PubMed] [Google Scholar]
- 92.Guo A, Zhang W, Xu S. Exploring the treatment effect in diabetes patients using association rule mining. Int J Inf Pro Manage. 2016;7(3):1–9. [Google Scholar]
- 93.Pearson K. On lines and planes of closest fit to systems of points in space. Lond Edinb Dublin Philos Mag J Sci. 1901;2(11):559–572. doi: 10.1080/14786440109462720. [DOI] [Google Scholar]
- 94.Hotelling H. Analysis of a complex of statistical variables into principal components. J Educ Psychol. 1933;24(6):417. doi: 10.1037/h0071325. [DOI] [Google Scholar]
- 95.Jolliffe IT, Cadima J. Principal component analysis: a review and recent developments. Philos Trans A Math Phys Eng Sci. 2016;374(2065):20150202. doi: 10.1098/rsta.2015.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang Z, Castelló A. Principal components analysis in clinical studies. Ann Transl Med. 2017;5(17):351. doi: 10.21037/atm.2017.07.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Apio BRS, Mawa R, Lawoko S, Sharma KN. Socio-economic inequality in stunting among children aged 6–59 months in a Ugandan population based cross-sectional study. Am J Pediatri. 2019;5(3):125–132. doi: 10.11648/j.ajp.20190503.18. [DOI] [Google Scholar]
- 98.Burgel PR, Paillasseur JL, Caillaud D, Tillie-Leblond I, Chanez P, Escamilla R, et al. Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. Eur Respir J. 2010;36(3):531–539. doi: 10.1183/09031936.00175109. [DOI] [PubMed] [Google Scholar]
- 99.Vogt W, Nagel D. Cluster analysis in diagnosis. Clin Chem. 1992;38(2):182–198. doi: 10.1093/clinchem/38.2.182. [DOI] [PubMed] [Google Scholar]
- 100.Layeghian Javan S, Sepehri MM, Layeghian Javan M, Khatibi T. An intelligent warning model for early prediction of cardiac arrest in sepsis patients. Comput Methods Programs Biomed. 2019;178:47–58. doi: 10.1016/j.cmpb.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 101.Wu W, Yang J, Li D, Huang Q, Zhao F, Feng X, et al. Competitive risk analysis of prognosis in patients with cecum cancer: a population-based study. Cancer Control. 2021;28:1073274821989316. doi: 10.1177/1073274821989316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Martínez Steele E, Popkin BM, Swinburn B, Monteiro CA. The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Popul Health Metr. 2017;15(1):6. doi: 10.1186/s12963-017-0119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]