Abstract
This article synthesizes what is known about the relationship between social disadvantage and measures of health literacy (HL), and reviews the research examining whether low HL is an explanatory factor connecting social disadvantage, health outcomes, and health disparities. Written from a United States perspective, this article offers a novel conceptual framework that presents how the social determinants of health might interact with HL to result in health disparities. The framework articulates relationships that reflect public health pathways and health care pathways, which include their related health literacies. The article continues with several cautionary statements based on the inherent limitations of current HL research, including problems and concerns specific to the attribution of HL as an explanatory factor for extant socioeconomic and racial/ethnic health disparities. The article closes with recommendations regarding future research directions. [HLRP: Health Literacy Research and Practice. 2021;5(3):e233–e243.]
Plain Language Summary:
Socially disadvantaged populations have worse health and health literacy compared to privileged populations. Scientists, health care providers, and policymakers are interested in the possible role health literacy plays in explaining health differences. The article reviews our current understandings of whether and how population characteristics and related exposures to risk interact with low health literacy to generate worse health to inform interventions.
Despite 30 years of active research, how social disadvantage and health literacy (HL) interact, and whether HL can explain some of the observed relationships between social determinants of health, health outcomes, and health disparities remain critical questions for the fields of clinical medicine and public health. This narrative review, written from a United States perspective, describes how social determinants of health might relate to low HL to result in health disparities. It further presents a novel conceptual framework that reflects both health care pathways (including health literate health care organizations) as well as public health pathways (e.g., the socioecological model, differential exposures, and life course perspectives) and their related HLs. This article also provides relevant caveats related to the attribution of HL as an explanatory factor for extant socioeconomic and racial/ethnic health disparities. Finally, this review article provides research recommendations and suggests future directions to help close gaps in our understanding of complex relationships between social determinants of health, HL, and health.
Limited Health Literacy and Social Disadvantage
Vulnerable populations represent subgroups of the larger population that, because of social, economic, political, structural, geographic, and historical forces, are exposed to a greater risk of risks, and are thereby at a disadvantage with respect to their health and health care (Paasche-Orlow et al., 2005). Vulnerable populations are exposed to contextual conditions that distinguish them from the rest of the population. It is estimated that one-third to one-half of the U.S. adult population has low HL, which is defined by the U.S. Institute of Medicine as a limited capacity to obtain, process, and understand the basic health information and services needed to make informed health decisions (National Academies Press, 2004). Although low HL affects people across the spectrum of sociodemo-graphics, low HL disproportionally affects vulnerable populations (Kutner et al., 2006). Vulnerable populations include the older adults, people with disabilities, people with lower socioeconomic status, racial/ethnic minorities, people with limited English proficiency (LEP), and people with limited education (Fleary & Ettienne, 2019). The most comprehensive assessment of variation in HL skills across different social groups occurred as a part of the National Assessment of Adult Literacy (NAAL) (Kutner et al., 2006). Assessments were performed in person; they had to be age 16 years or older and speak English or Spanish fluently. Results of the NAAL suggested significant differences in the distribution of HL skills by race and ethnicity; educational attainment; income; and language spoken before starting school. A more recent study using data from the 2013 Health Information National Trends Survey confirmed these findings (DeWalt et al., 2004).
Low HL can be a marker for (or manifestation of) many life circumstances, including but not restricted to limited access to education, access to poor quality education, LEP, learning differences and disabilities, and cognitive impairment. People with low HL are more likely to have poor health, higher rates of chronic disease, and a nearly 2-fold higher mortality rate as compared to people with adequate HL (Cavanaugh et al., 2008). As such, compared to those with adequate HL, persons with low HL also are more likely to experience disparities in health and health care access, and have lower rates of receiving screening and preventive services. Patients with low HL exhibit patterns of utilization of care reflecting a greater degree of unmet needs, such as excess emergency department (ED) visits and hospitalizations, even when comorbid conditions and health insurance status are statistically held constant. Patients with low HL are more likely to have poorer knowledge of their disease processes, medication regimens, and exhibit worse medication adherence and inadequate skills and methods for managing their disease (Logan, 2017; Vernon et al., 2007). Low HL also has a negative effect on doctor-patient communication. Patients with low HL tend to be more passive in their visits with clinicians, have visits that are less interactive, are less likely to engage in decision-making, and are more likely to report that interactions with their physicians are not helpful or empowering. A study conducted over a decade ago estimated that low HL leads to excess health expenditures of greater than $100 billion annually (Mantwill et al., 2015).
Evidence Connecting Health Literacy with Health Disparities
The problem of health disparities experienced within vulnerable populations is largely one of the differential exposures and associated behaviors. This framing eliminates some of the “shame and blame” often associated with the higher burden of disease among people who are socially disadvantaged. As such, social vulnerability is not necessarily an attribute that is intrinsic to people or subpopulations; instead, vulnerability status is determined by how society and its institutions are constructed. Low HL is tightly and simultaneously linked to several social determinants of health. Some investigators and health policy experts have even considered low HL itself to be a social determinant of health (Pelikan et al., 2018). Others suggest that HL is key to improving control over modifiable social determinants of health (Rowlands et al., 2017), describing it as a mediator or effect modifier. Wherever one falls in this debate, the high burden of low HL among vulnerable populations has led many to believe that low HL is a contributor to both health and health care disparities. In turn, an ensuing set of questions include (1) Might HL partially explain the health and health care disparities associated with the social determinants of health? (2) Might HL lead to differential effects of exposures or interventions on specific subgroups of the general population? Although these questions are of paramount importance, relatively little research has provided an empirically rigorous answer (Cooper & Schillinger, 2011).
In public health practice in the U.S., racial/ethnic minorities, immigrants with LEP, and those of lower socioeconomic status (having low income, having obtained a high school diploma or less), are generally regarded as vulnerable groups. Recent research, including a systematic review, focuses on race/ethnicity and educational attainment with respect to the question of whether HL explains some of the relationships between social circumstances and health outcomes (Bennett et al., 2009). In addition, the extant research is varied regarding the HL assessments used and health-related outcomes examined. In general, multivariable modeling has been used to determine independent effects of predictors and mediating variables on specific health outcomes. Some evidence has reported a mediating function of HL on health and health care outcomes across racial/ethnic and educational disparities. Some evidence suggests the potential effect of HL and numeracy on racial/ethnic disparities in health behaviors and knowledge. In all research with positive associations, the effect of the mediation was partial; HL did not fully explain broader relationships.
More specific research about health disparities related to educational attainment, health disparities related to race/ethnicity, health disparities between ethnic and linguistic subgroups, and prospective studies are outlined below.
Health Disparities Related to Educational Attainment
Although several cross-sectional studies have explored HL as a meditating factor in the relationships between socioeconomic disparities and health outcomes, the following research specifically evaluates the relationship among HL, other variables, and educational attainment. An assessment by Bennett et al. (2009) (a population of nearly 3,000 adults older than age 65 years who participated in the NAAL) found that HL mediated the relationship between educational attainment and self-rated health, as well as indicators of health care access and utilization, including receipt of flu vaccines, receipt of mammograms, and dental care.
In contrast, another study (of more than 3,000 seniors who participated in the Prudential Health Insurance Study) found that HL explained the relationship between education and physical and mental health scores, but not preventive care use, such as flu vaccine, mammograms, and dental care (Howard et al., 2006). A study by Yin et al. (2009) (of parents who participated in NAAL) found that HL mediated the relationship between educational attainment and HL-related tasks regarding child health, dosing medications, and pediatrician appointments.
Sentell and Halpin (2006) studied approximately 24,000 community-dwelling participants in the NAAL (performed in the 1990s) and found that HL mediated the relationship between education and the presence of chronic illness and a health condition that limited ability to function in society (Schillinger et al., 2006). Similarly, in a study of more than 14,000 persons with diabetes in a large, pre-paid integrated health plan, Sarkar et al. (2010) found that HL mediated the relationship between educational attainment and patient's use of an electronic patient portal, which was associated with better health outcomes (Bailey et al., 2009). Finally, Schillinger et al. (2006) studied a diverse sample of more than 400 public hospital patients with diabetes and found that HL mediated the relationship between education and hemoglobin A1c (a standard measure of diabetes control) (Osborn et al., 2009).
Health Disparities Related to Race/Ethnicity
As to whether HL explains racial and ethnic disparities in health or health care outcomes, several cross-sectional studies—some already mentioned, some additional—have looked at the explanatory power of HL with respect to Black/White differences in health outcomes; few studies have assessed other racial or ethnic differences. Bennett et al. (2009) found that HL mediated the relationship between race and self-rated health as well as flu vaccine receipt, but not mammography or dental care (Sentell & Halpin, 2006). Howard et al. (2006), studying the NAAL participants, found that HL mediated the relationship between race and mental health but not physical health, and not the receipt of preventive care (Sarkar et al., 2010).
Sentell and Halpin in their study of approximately 24,000 community-dwelling participants found that HL mediated the relationship between race and long-term illness and a limiting health condition, just as HL did with education (Schillinger et al., 2006). In a study of 373 parents, Bailey et al. (2009) found that HL mediated the relationship between race and misunderstandings about liquid medication dosing (Wolf et al., 2006). Osborn et al. (2011) found that diabetes-related numeracy mediated the relationship between race and hemoglobin A1c (a measure of blood sugar control), an effect seen primarily in patients with diabetes who used insulin (Osborn et al., 2011). In patients with prostate cancer, Wolf et al. (2006) found that HL mediated the relationship between race and the level of prostate-specific-antigen at the time of presentation with prostate cancer (Curtis et al., 2012). Osborn et al. (2009) found that HL mediated the relationship between HL and diabetes medication adherence (Gwynn et al., 2016). Another study suggested that, although HL reduced the effect of race/ethnicity in Black and Hispanic people on asthma-related quality of life and asthma control (and for Black people only on ED visits), differences between Black and White people for asthma-related hospitalizations persisted (Smith et al., 2012). Finally, a study of more than 225 mostly Black and White patients demonstrated that HL mediated the relationship between race and a measure of patient activation (Sentell et al., 2013).
Health Disparities Between Ethnic and Linguistic Subgroups
Relatively few studies have explored the effects of HL in health disparities experienced by Hispanic or Asian subgroups, and still fewer have examined HL's role in explaining health disparities associated with LEP. A study comparing Spanish to English speakers in an ED suggested only the former were less likely to show up for follow-up appointments if they had low HL (Sentell & Braun, 2012). A study of Asian Americans found that low HL was not significantly associated with meeting colorectal cancer screening guidelines, but LEP was associated (Schenker et al., 2011). However, the combination of LEP and low HL had synergistic effects among Asian Americans. A large study (Sentell & Braun, 2012) that featured diverse participants found that low HL was only significantly related to health status in White people and unknown races, but not within any Asian group. However, the study found the highest odds of poor health status occurred among Chinese, Vietnamese, and Hispanics with low HL and LEP. (Sentell & Braun, 2012). Similar synergistic effects were observed on patient-reported interpersonal communication outcomes in a large sample of English- and Spanish-speaking primary care patients (Sudore et al., 2009). Low HL and LEP each was associated with worse communication within the receptive, expressive, and interactive domains of interpersonal communication, whereas the combination was associated with the worst communication.
Prospective Studies
Only five prospective studies have examined the question of whether HL functions as a mediator or moderator of health disparities. In a longitudinal cohort study with 342 Black, Hispanic, and White adults with persistent asthma, HL mediated the relationship between race/ethnicity and asthma-related hospitalizations and ED visits (Sperber et al., 2013). In a before and after trial, Volandes et al. (2008) found that HL mediated the relationship between race and changes in advanced care preferences (Karter et al., 2015). After viewing a video, patient preferences, particularly among those with low HL, changed to preferring less aggressive care, an effect that was more pronounced among Black patients. An experiment of the differential effects between Black and White people and HL that studied response to a telephone-based osteoarthritis self-management support intervention found a significant interaction between HL and race/ethnicity on change in pain; Black people with low HL had the highest improvement in pain in the intervention compared to the usual care group (Sperber et al., 2013). Finally, a natural experiment (involving more than 8,000 ethnically diverse patients with diabetes to enhance medication adherence, implementation of an intervention to promote mail-order pharmacy use that was not tailored for patients with low HL) reported a differential up-take of the intervention that further disadvantaged patients with low HL, especially among Hispanic and lower income subgroups (Karter et al., 2015). A trial of literacy-appropriate, easy-to-understand video narratives and testimonials (presented in English and Spanish to encourage advance care planning demonstrated improvements across HL levels) yielded benefits for Spanish speakers, although the interaction between study arms and language was not statistically significant (Sudore et al., 2018).
The Need for a Novel Model That Incorporates The Public Health Perspective
In reviewing this literature, it is important to note that many studies applied clinical epidemiologic approaches to address the larger question whether low HL can explain health disparities by either exploring the interactions among HL and a particular social determinant (e.g., effect modification by race or education) on health outcomes or performing formal meditational analyses. In so doing, investigators attempted to answer whether HL had differential effects on health outcomes based on a person's race or educational attainment or whether HL explained observed differences in outcomes by race or education.
Yet, from a public health perspective, given the disproportionately high prevalence of low HL among vulnerable populations, these types of analytic approaches may be overly reductionist. Insofar as low HL is more prevalent in socially disadvantaged populations, and as low HL appears to be an explanatory factor in the development of illness or its complications across populations, interventions to effectively address low HL are likely to result in a reduction in health disparities. Yet, this effect may be because low HL is unequally distributed across the U.S. population more than a unique explanatory power of low HL, meaning that HL-appropriate interventions could yield population-wide impacts that could reduce health and health care disparities even if HL is not a mediator. This suggests the need for a socioecologically oriented model.
Conceptual Framework for the Relationships Among Social Determinants of Health, Health Literacy, and Health Disparities
To advance our understanding of the inter-relationships among social determinants of health, health literacy and health disparities, I present a novel conceptual framework (Figure 1) that integrates a socioecological framework with the more traditional causal frameworks associated with HL. Socioecological models emphasize multiple levels of influence on health (such as individual, interpersonal, organizational, community and public policy) and embrace the idea that behaviors both shape and are shaped by their surrounding social environment. The proposed conceptual model synthesizes research from multiple disciplines (such as clinical epidemiology, health services research, economics, political science, anthropology, health communication science, and public health) to better explain the potential pathways by which the social determinants of health, HL, and health disparities interact. The framework, and its explication, elucidate pathways; the associated factors additionally provide potential targets for intervention in the effort to reduce health disparities. The model acknowledges that HL is not necessarily a fixed attribute. Rather, HL can be improved directly through interventions that enable experience and build skills, or indirectly through interventions that reduce HL demands or alter the environment by shifting the balance in favor of health-promoting resources vs. unhealthy exposures.
Figure 1.
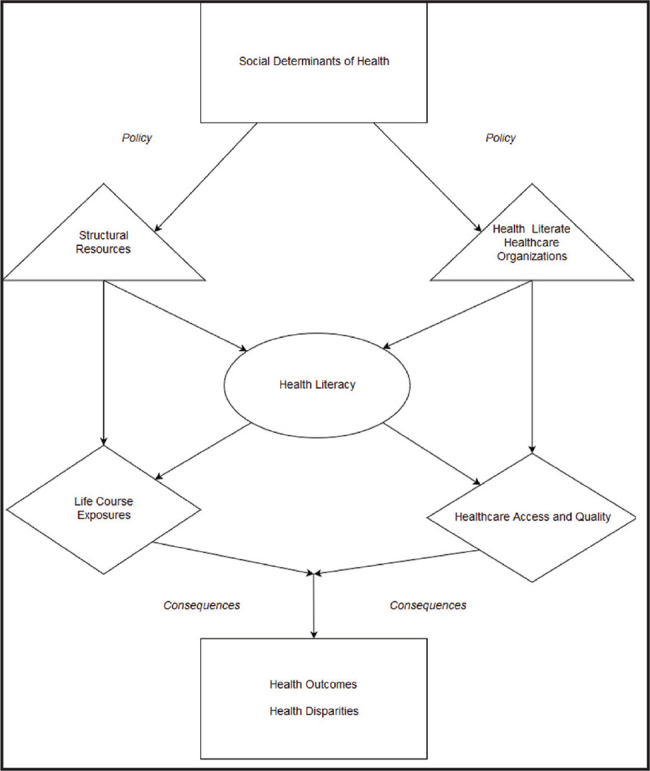
Conceptual framework for the pathways that connect social determinants of health, health literacy, and health disparities. Pathways on the right represent health care pathways; those on the left represent public health pathways.
Figure 1 illustrates the two predominant pathways through which social determinants of health and social disadvantage can interact with low HL to result in health disparities. The first is the public health pathway that suggests the structural factors that reflect the maldistribution of health-promoting resources and unhealthy life course exposures across the general population in the U.S. The second is the health care pathway that suggests the organizational factors that reflect the responsiveness of health systems to the needs of clinical populations in the U.S., with respect to access to and quality of care. Differences in resources and exposures in public health and community settings, as well as differences in access and quality in clinical settings, both generate consequences that contribute to worse health outcomes and health disparities. To aid in understanding, several of the constructs and variables within Figure 1 are described below.
Social Determinants of Health
The top box (and construct) in Figure 1 is the starting point for all pathways and reflects the unequal distribution of health-promoting resources and unhealthy life course exposures resulting from differences in social status, often instigated, reinforced, or perpetuated by social policy and practice. This construct focuses on subpopulations of low income/poverty status; low educational attainment; racial and ethnic minority populations subject to marginalization and oppression; and those with LEP/linguistic isolation.
Structural Resources and Life Course Exposures
In Figure 1, the triangle and diamond on the left and below represent the factors within the public health pathway that are protective to health and those that jeopardize health, that together often shape health behaviors. These factors, so-called “structural determinants,” flow from historical and current institutional, local, state, and federal policies and practices and generate facts on the ground that can profoundly affect people, families, and neighborhoods. Exposure to these structural determinants is a function of the social status and flows from the determinants of health, such as lower socioeconomic status and racial and ethnic minority status. The balance between health-promoting resources and risk exposures over the life course are a major determinant of the health of people and communities. Some of these structural factors include air quality/pollution; safe and green spaces for physical activity and recreation; features of the built environment and associated zoning regulations; transportation infrastructure; housing/segregation; the retail food environment/food deserts; commercial marketing environments (such as advertisements on billboards for unhealthy products); employment opportunities and occupational hazards; community stress and trauma; presence or absence of public health-promoting regulations; social support; social cohesion; and social investment.
Mediating and Moderating Related Health Literacy Domains (Public Health Pathway)
Within the public health pathway, HL is depicted as both a product of the social determinants of health as well as a potential asset that can positively influence the balance between health-promoting resources and unhealthy risk exposures, and/or mitigate the ill effects of unhealthy exposures. Health exposures can be influenced by environmental HL (Finn & O'Fallon, 2017), occupational HL, nutritional HL (Rauscher & Myers, 2014), mental HL (Jorm, 2012), and the larger construct of “public health literacy” (Freedman et al., 2009). Public HL can be an attribute of an individual, a community, or an entire population. Public HL refers to the degree to which people and groups can obtain, process, understand, evaluate, and act upon information needed to make public health decisions that benefit the community. Public HL aims to engage more stakeholders in public health efforts and address determinants of health. It requires an understanding of conceptual foundations related to the socioecological model of health, critical skills, and a civic orientation. Although advocacy and policy change are its currency, improving the health of the public is its ultimate objective.
The Consequences
The depiction of the maldistribution of resources and exposures between populations, compounded by a disproportionately high rate of low HL of the types described above among vulnerable populations, has real consequences for health behavior and health status. These include higher rates of chronic diseases such as obesity, type 2 diabetes, cardiovascular disease and stroke, asthma, cancer, chronic pain, and disability from both physical and mental health problems (Köppen et al., 2018; Lincoln et al., 2008; Sudore et al., 2006; Wolf et al., 2005).
Health Literate Health Care Organizations
The triangle on the right side of Figure 1 represents the next step in the health care pathway connecting social determinants of health, HL, and health disparities. Brach et al. (2012) defined health literate health care organizations (HLHCOs) as those that ensure HL is deeply and explicitly integrated into all of their activities and that HL informs both strategic and operational planning. Appropriate measures to evaluate specific HL initiatives are developed and used. More importantly, the measurement of overall organizational performance assesses success with vulnerable populations. However, because of inadequacies and bias in health policy, health care financing, health care regulation, health professions training, health care innovation, and health care practice, there is significant variation in the degree to which U.S. health care systems are responsive to the needs of socioeconomically and ethnically diverse patients with varying levels of HL. As such, the extent to which health systems demonstrate the attributes of HLHCOs reflects a structural determinant of health.
Health Care Access and Quality
The depiction of Figure 1 underscores a basic tenet of the U.S. health care system, whereby the patients who maximally benefit from health care often have the greatest capacity and resources, including but not limited to HL. The health care system's weaknesses are undergirded by issues related to unequal access to care, including incomplete and/or unequal health insurance coverage; unnecessary barriers to obtaining public insurance; overly complex health insurance practices; insufficient provider workforce for specific (underserved) populations; lack of a diverse health care workforce; under-valuing or under-resourcing primary care; and segregation of health care (including an obligatory over-reliance on overex-tended safety net health systems among vulnerable populations). There are additional features within many U.S. health systems that further undermine the quality of care that are particularly salient for vulnerable populations and patients with low HL. These include inadequate preparation, training and maldistribution of the clinical workforce (Institute of Medicine, 2000), and associated poor provider performance (especially with respect to interpersonal processes of care) (Institute of Medicine, 2004); insufficient caregiver involvement and support; lack of ethnic and linguistic diversity in the workforce (McCabe & Healey, 2018); lack of involvement of vulnerable populations in the design of health care services and its associated innovations; lack of peer and lay health educator models; lack of HL-appropriate digital health/e-health innovations; lack of resources and integrated interventions to assess and address social needs; fragmentation of health care; lack of inter-visit communication; incomplete trust in the provider; and insufficient or inappropriate policies, regulatory standards, oversight, measurement and/or incentives to reduce disparities and promote health care equity (Grumbach & Mendoza, 2008; Schillinger et al., 2004; Stepanikova et al., 2016).
Mediating and Moderating Health Literacy Domains (Health Care Pathway)
Within the depicted health care pathway, HL is a product of HLHCOs as well as a potential asset that can positively influence the balance between HL-related demands health care systems place on patients and the HL-related skills of patients and families. The latter can mitigate the effects of receiving care in systems that are unresponsive to the needs of persons with low HL. Much has been studied and written about the patient-related HL skills required to optimally function within U.S. health care settings. These skills include communicative HL capabilities, such as speaking, listening, reading, and increasingly writing (e.g., secure messages in electronic patient portals) of health-related content, quantitative skills (e.g., health numeracy), and health insurance literacy (e.g., the ability to navigate bureaucratic procedures and advocate for oneself) (Dubbin et al., 2013; Schillinger et al., 2017).
The Consequences
Overall, the lack of evolution and diffusion of the model of HLHCOs, combined with the fragmentation, overextension, and under-resourcing characteristic of many safety net health care systems (further compounded by a disproportionately high rate of low HL of the types described above among vulnerable patients), yields consequences for health care disparities, with respect to access, processes of care, and outcomes. The latter include presenting late to medical attention, often with more advanced disease, demonstrating more missed appointments (Baskaradoss, 2016), poorer self-management skills, lesser degrees of patient activation, suboptimal clinician-patient communication, less shared decision-making, lower trust, worse quality of care, and greater rates of medical error and patient safety events. The consequences of the depicted health care pathway, together with the public health pathway (which leads vulnerable populations to be even more reliant on health care because of a higher burden of disease) includes greater complication rates, worse health outcomes, higher costs of care and utilization of services, and greater premature morbidity and mortality.
Caveats Regarding Health Literacy as an Explanatory Factor in Health Disparities
The scientific endeavor combines unbiased experimentation with objective observations of the natural world to accumulate knowledge to approximate truth. However, although medicine is largely seen as a force for good, clinical science has a checkered record. At times, its tools and its authority have been used to promote or perpetuate inhumane policies and practices ranging from unethical research and medical practices that have harmed lower income and racial/ethnic and religious minority populations, subjecting them to “racial hygiene” (a eugenics-based approach, institutionalized by Nazi Germany, based on medical beliefs of the day regarding racial hierarchies, marked by efforts to avoid the “contamination” of “higher races” with “lower ones”) that led to race-based genocide (Proctor, 2002).
When examining the question of whether and how HL affects health, researchers need to be mindful that literacy represents a resource which, for racial/ethnic minority subgroups, historically has been withheld to oppress, or has been measured and then used to judge groups as inferior or ineligible to participate as citizens, or as an alternate means to oppress (Goldman, 2004). There are several related challenges in HL research that researchers, policymakers, and practitioners must be aware of that temper confidence in the validity of the research and its synthesis just presented, and which support the need to carry out additional, complementary research to better approximate truth and not perpetuate mistruths. The specific challenges of measurement and attribution are discussed in the remainder of this section.
To begin, there are diverse challenges in this field associated with research measurement (Schillinger & Sarkar, 2009). How best to measure patient HL, and whether or not HL measures are detecting true differences in capacities and skills in marginalized populations, can be problematic and controversial. A recent review of all HL research measures (Health Literacy Tool Shed, 2021) found that 200 unique measures have been created and employed, including 14 in Spanish, with most (52%) requiring paper and pencil responses, and some measures (12%) requiring more than 15 minutes to administer. Of the 200, 128 (64%) measured general HL, 76 (38%) measured disease or content-specific HL, and only 1 (0.5%) measured a public health literacy domain (water environmental literacy). Thirty-one (15.5%) assessed pronunciation, 25 (12.5%) assessed conceptual knowledge, and 43 (21.5%) assessed comprehension.
As previously described, health disparities are produced and perpetuated by multilevel forces operating at the individual, family, health system, community, and public policy levels that mutually reinforce each other to produce injustice and perpetuate inequity. Because conventional literacy assessments are bounded by cultural and linguistic assumptions derived from the majority population, more research is needed to assess patient HL in a comprehensive, holistic, and unbiased manner, and to expand the assessment of reliability and validity across subgroups of interest to avoid misattributing health disparities solely to limited HL.
A clear, but by no means isolated example of this challenge is the use of HL measures that require proper pronunciation of medical terms to assess HL, such as the REALM (Rapid Estimate of Adult Literacy in Medicine). It is not hard to imagine that biased measurement may occur for a measure in which a White researcher scores a patient's HL by determining whether a patient has read and pronounced a medical term “correctly.” This can be true for some Black patients whose pronunciation of some words in the English language may differ from the “mainstream” linguistic culture (Goldman, 2004). The problem of cultural hegemony in literacy assessment, and the untoward downstream effects of related mismeasurement, has been well elucidated in the social psychology field (Harris, 2010).
A second research challenge is attribution. The critique here is both general to social epidemiology and specific to HL research. For example, do the observations that low HL is more common in marginalized populations, and that in some cases observed social disparities in health outcomes appear to be statistically mediated by low HL suggest that the relationship indeed is causal? There are alternative hypothesized mechanisms by which low HL may be associated with health care quality and health outcomes in research exploring the causes of health disparities among vulnerable populations that are not causal (Harris, 2010). These mechanisms include:
Confounds: low HL may simply be a marker for or a result of sociodemographic and behavioral factors or life course exposures or experiences that by themselves directly or indirectly lead to morbidity and mortality. Although most studies attempt to account for confounds using multivariable analytic methods, it is widely recognized that socioeconomic variables obtained at one point in time (such as income) only incompletely capture income over the life course, or that income does not necessarily signify assets and wealth. As such, residual confounding is not only possible, but is almost certain to exist. Similarly, although variables such as race or immigration status are often collected, these measures do not begin to capture the experience of being Black or an immigrant in the U.S.
Reverse or cyclical causation: low HL may be a consequence of high disease burden or poor disease control, and thus associated with worse health trajectories (cyclical effect). As an example, people with longstanding diabetes that is poorly controlled have been shown to experience worse cognitive function as a complication of the disease. In turn, this may contribute to the downward trajectory in self-management due to poor understanding, but it may be captured as low HL within a cross-sectional HL assessment, all occurring in a patient whose clinical course has already been largely determined.
Attention bias: What we choose to measure and what we choose not to measure inevitably influences inferences regarding cause and effect. Low HL may affect outcomes through a demand-capacity mismatch, with the health care system placing inappropriate communication demands on patients; or communication resources are poorly distributed for the population with the greatest needs. The latter hypothesis suggests changes at the health system level provide intervention targets to mitigate health disparities related to low HL. Whereas greater attention is finally being paid to the communication attributes of clinicians and health care organizations as they relate to patient HL, there has been little work to operationalize a measure of clinician or systems responsiveness to the needs of population with low HL (Brach et al., 2014). This has hindered progress in reducing HL and racial and ethnic disparities in health care.
Attribution bias: Finally, insofar as literacy skills, be they HL or otherwise, reflect a resource that results from privilege and power, the absence of literacy reflects a particular manifestation of oppression and marginalization, be it historical or ongoing. Following this argument, those with low HL have inexorably been exposed to other forms of systematic deprivation, including forms of intergenerational oppression that are difficult or impossible to measure at the individual level. In this case, low HL, despite consistently demonstrating statistically significant meditational relationships, may present itself as an overly simplistic, stereotype-laden, and potentially dangerously false explanation for observed health disparities.
Future Directions
When it comes to shedding light on the fundamental causes of health disparities, articulating mechanisms leading to health disparities, and intervening to promote health equity, HL research needs to evolve in many ways to achieve its promise. First, future research should focus on developing alternative HL measures that are not subject to bias and mismeasurement in marginalized populations and should attend to ensuring the reliability and validity of these measures across population subgroups. Second, more attention needs to be paid to comprehensively measure confounding variables, with a particular emphasis to avoid attribution bias. Second, because most HL research has focused on patients' HL deficits, much more work needs to be done to operationalize a measure of clinician or systems' responsiveness to the needs of populations with low HL, including the communication attributes of clinicians and health care organizations (Brach et al., 2014; Crossley et al., 2020; Institute of Medicine, 2012; Schillinger, 2007).
Third, while making significant advances during the last 20 years, the field of HL research in the U.S. has involved a relative paucity of investigators from under-represented minority (URM) groups, groups that otherwise are active in the field of health disparities research. This may be due, in part, to the inherent assumptions, biases, and limitations that are in HL research. Although there is a growing body of community-based participatory research in the field of HL, there remains a critical need to extend and enhance HL research by including the experience, voices, and intellectual capacity of a multidisciplinary cohort of URM researchers. Only by expanding inclusivity in this way will the field of HL be able to be optimally harnessed to reduce health and health care disparities.
Fourth, descriptive research must be designed and powered to enable the simultaneous disentanglement of socioeconomic status, race/ethnicity (representative of all major ethnic subgroups) and LEP from HL, and to enable valid and informative meditational analyses, with a particular emphasis on longitudinal studies. Fifth, investment in interventional research must increase to (1) ensure an ability to stratify effectiveness results by sociodemographic characteristics as well as by HL level to identify effect modification; (2) enable formal exploration of mediational effects, including the impacts of HL relative to other explanatory factors; and (3) include public HL interventions. Relatedly, a lack of differential effectiveness should not prevent the dissemination, uptake, and adoption of effective HL-appropriate interventions. Rather, given the disproportionate burden of low HL in vulnerable populations, such interventions should be seen as an important means to reduce health disparities.
Conclusions
Low HL is more common in populations that are socially disadvantaged, and there is a growing body of research to suggest that HL may be an explanatory factor in pathways that generate health disparities, especially those associated with social determinants of health such as lower educational attainment and racial/ethnic status. To better understand the potential mechanisms whereby HL can mediate health disparities associated with the social determinants of health, this article presents a novel conceptual framework that can inform research, policy, and practice for those interested in promoting health equity in the U.S. and potentially beyond. The framework describes two primary pathways that generate consequences for health outcomes based, in part, on HL. The first operates through multilevel factors related to the unequal distribution of resources and exposures and their related environmental and public health literacies. The second operates through underdeveloped (and arguably discriminatory) institutional capacities of the health care systems, and the related individual communicative literacies of the patients that rely on these systems. Both pathways emerge within a complex society characterized by competing forces that reflect both a history of marginalization and oppression of vulnerable subgroups as well as a tradition of civic engagement and advocacy for progressive change that is the foundation of democracy. The field of HL represents a progressive force whose objectives and early achievements can help reverse deeply ingrained policies, structures, and practices at the health care and broader societal levels that create, perpetuate, or even amplify health disparities (Paasche-Orlow et al., 2018). HL research—both descriptive and interventional—is still somewhat nascent; it needs to further evolve and expand to accurately situate HL as a target to reduce health disparities.
References
- Bailey , S. C. , Pandit , A. U. , Yin , S. , Federman , A. , Davis , T. C. , Parker , R. M. , & Wolf , M. S. ( 2009. ). Predictors of misunderstanding pediatric liquid medication instructions . Family Medicine , 41 ( 10 ), 715 – 721 PMID: [PubMed] [Google Scholar]
- Baskaradoss , J. K. ( 2016. ). The association between oral health literacy and missed dental appointments . The Journal of the American Dental Association , 147 ( 11 ), 867 – 874 . 10.1016/j.adaj.2016.05.011 PMID: [DOI] [PubMed] [Google Scholar]
- Bennett , I. M. , Chen , J. , Soroui , J. S. , & White , S. ( 2009. ). The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults . Annals of Family Medicine , 7 ( 3 ), 204 – 211 . 10.1370/afm.940 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brach , C. ( 2017. ). The Journey to become a health literate organization: a snapshot of health system improvement . Studies in Health Technology and Informatics , 240 , 203 – 237 PMID: [PMC free article] [PubMed] [Google Scholar]
- Brach , C. , Dreyer , B. P. , & Schillinger , D. ( 2014. ). Physicians' roles in creating health literate organizations: A call to action . Journal of General Internal Medicine , 29 ( 2 ), 273 – 275 . 10.1007/s11606-013-2619-6 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brach , C. , Keller , D. , Hernandez , L. M. , Baur , C. , Parker , R. , Dreyer , B. , Schyve , P. , Lemerise , A. J. , & Schillinger , D . ( 2012. ). Ten attributes of health literate health care organizations . https://nam.edu/wp-content/uploads/2015/06/BPH_Ten_HLit_Attributes.pdf [Google Scholar]
- Cavanaugh , K. , Huizinga , M. M. , Wallston , K. A. , Gebretsadik , T. , Shin-tani , A. , Davis , D. , Gregory , R. P. , Fuchs , L. , Malone , R. , Cherrington , A. , Pignone , M. , DeWalt , D. A. , Elasy , T. A. , & Rothman , R. L. ( 2008. ). Association of numeracy and diabetes control . Annals of Internal Medicine , 148 ( 10 ), 737 – 746 . 10.7326/0003-4819-148-10-200805200-00006 PMID: [DOI] [PubMed] [Google Scholar]
- Cooper , L. , & Schillinger , D . ( 2011. ). The role of health literacy in health disparities research. In Innovations in health literacy research: workshop summary (pp. 7 – 12 ). Institute of Medicine of the National Academies; . [Google Scholar]
- Crossley , S. A. , Balyan , R. , Liu , J. , Karter , A. J. , McNamara , D. , & Schillinger , D. ( 2020. ). Predicting the readability of physicians' secure messages to improve health communication using novel linguistic features: The ECLIPPSE study . Journal of Communication in Healthcare , 13 , 344 – 356 . 10.1080/17538068.2020.1822726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis , L. M. , Wolf , M. S. , Weiss , K. B. , & Grammer , L. C. ( 2012. ). The impact of health literacy and socioeconomic status on asthma disparities . The Journal of Asthma , 49 ( 2 ), 178 – 183 . 10.3109/02770903.2011.648297 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt , D. A. , Berkman , N. D. , Sheridan , S. , Lohr , K. N. , & Pignone , M. P. ( 2004. ). Literacy and health outcomes . Gen Intern Med , 19 ( 12 ): 1228 – 1239 . 10.1111/j.1525-1497.2004.40153.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubbin , L. A. , Chang , J. S. , & Shim , J. K. ( 2013. ). Cultural health capital and the interactional dynamics of patient-centered care . Social Science & Medicine , 93 , 113 – 120 . 10.1016/j.socscimed.2013.06.014 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn , S. , & O'Fallon , L. ( 2017. ). The emergence of environmental health literacy--From its roots to its future potential . Environmental Health Perspectives , 125 ( 4 ), 495 – 501 . 10.1289/ehp.1409337 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleary , S. A. , & Ettienne , R. ( 2019. ). Social disparities in health literacy in the United States . Health Literacy Research and Practice , 3 ( 1 ), e47 – e52 . 10.3928/24748307-20190131-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman , D. A. , Bess , K. D. , Tucker , H. A. , Boyd , D. L. , Tuchman , A. M. , & Wallston , K. A. ( 2009. ). Public health literacy defined . American Journal of Preventive Medicine , 36 ( 5 ), 446 – 451 . 10.1016/j.amepre.2009.02.001 PMID: [DOI] [PubMed] [Google Scholar]
- Goldman , D. ( 2004. ). The modern-day literacy test: Felon disenfranchisement and race discrimination . Stanford Law Review , 57 , 611 . [Google Scholar]
- Grumbach , K. , & Mendoza , R. ( 2008. ). Disparities in human resources: Addressing the lack of diversity in the health professions . Health Affairs (Project Hope) , 27 ( 2 ), 413 – 422 . 10.1377/hlthaff.27.2.413 PMID: [DOI] [PubMed] [Google Scholar]
- Gwynn , K. B. , Winter , M. R. , Cabral , H. J. , Wolf , M. S. , Hanchate , A. D. , Henault , L. , Waite , K. , Bickmore , T. W. , & Paasche-Orlow , M. K. ( 2016. ). Racial disparities in patient activation: Evaluating the mediating role of health literacy with path analyses . Patient Education and Counseling , 99 ( 6 ), 1033 – 1037 . 10.1016/j.pec.2015.12.020 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris , V. J. ( 2010. ). African-American conceptions of literacy: A historical perspective . Theory into Practice , 31 ( 4 ), 276 – 286 . 10.1080/00405849209543554 [DOI] [Google Scholar]
- Health Literacy Tool Shed . ( 2021. ). Health literacy tool shed. Find the right health literacy measurement tool for your research . https://healthliteracy.bu.edu/ [Google Scholar]
- Howard , D. H. , Sentell , T. , & Gazmararian , J. A. ( 2006. ). Impact of health literacy on socioeconomic and racial differences in health in an elderly population . Journal of General Internal Medicine , 21 , 857 – 861 . 10.1111/j.1525-1497.2006.00530.x PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . ( 2000. ). America's health care safety net: Intact but endangered . https://www.ncbi.nlm.nih.gov/books/NBK224521/ [PubMed] [Google Scholar]
- Institute of Medicine . ( 2004. ). Health literacy: A prescription to end confusion . https://pubmed.ncbi.nlm.nih.gov/25009856/ [Google Scholar]
- Institute of Medicine . ( 2012. ). How can health care organizations become more health literate? https://www.nap.edu/catalog/13402/how-can-health-care-organizations-become-more-health-literate-workshop#toc [Google Scholar]
- Jorm , A. F. ( 2012. ). Mental health literacy: Empowering the community to take action for better mental health . The American Psychologist , 67 ( 3 ), 231 – 243 . 10.1037/a0025957 PMID: [DOI] [PubMed] [Google Scholar]
- Karter , A. J. , Parker , M. M. , Duru , O. K. , Schillinger , D. , Adler , N. E. , Moffet , H. H. , Adams , A. S. , Chan , J. , Herman , W. H. , & Schmittdiel , J. A. ( 2015. ). Impact of a pharmacy benefit change on new use of mail order pharmacy among diabetes patients: The Diabetes Study of Northern California (DISTANCE) . Health Services Research , 50 ( 2 ), 537 – 559 . 10.1111/1475-6773.12223 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köppen , P. J. , Dorner , T. E. , Stein , K. V. , Simon , J. , & Crevenna , R. ( 2018. ). Health literacy, pain intensity and pain perception in patients with chronic pain . Wiener Klinische Wochenschrift , 130 ( 1–2 ), 23 – 30 . 10.1007/s00508-017-1309-5 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner , M. , Greenburg , E. , Ying , J. , & Paulsen , C . ( 2006. ). The health literacy of America's adults: Results from the 2003 national assessment of adult Literacy. NCES 2006-483 . https://eric.ed.gov/?id=ED493284
- Lincoln , A. , Espejo , D. , Johnson , P. , Paasche-Orlow , M. , Speckman , J. L. , Webber , T. L. , & White , R. F. ( 2008. ). Limited literacy and psychiatric disorders among users of an urban safety-net hospital's mental health outpatient clinic . The Journal of Nervous and Mental Disease , 196 ( 9 ), 687 – 693 . 10.1097/NMD.0b013e31817d0181 PMID: [DOI] [PubMed] [Google Scholar]
- Logan , R. A. ( 2017. ). Seeking an expanded, multidimensional conceptual approach to health literacy and health disparities research . Studies in Health Technology and Informatics , 240 , 96 – 123 . 10.3233/ISU-160809 PMID: [DOI] [PubMed] [Google Scholar]
- Mantwill , S. , Monestel-Umaña , S. , & Schulz , P. J. ( 2015. ). The relationship between health literacy and health disparities: A systematic review . PLoS One , 10 , e0145455 Advance online publication. 10.1371/journal.pone.0145455 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe , R. , & Healey , P. G. T. ( 2018. ). Miscommunication in doctor-patient communication . Topics in Cognitive Science , 10 , 409 – 424 . 10.1111/tops.12337 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies Press . ( 2004. ). Health literacy: A prescription to end confusion . https://pubmed.ncbi.nlm.nih.gov/25009856/ [PubMed] [Google Scholar]
- Osborn , C. Y. , Cavanaugh , K. , Wallston , K. A. , Kripalani , S. , Elasy , T. A. , Rothman , R. L. , & White , R. O. ( 2011. ). Health literacy explains racial disparities in diabetes medication adherence . Journal of Health Communication , 16 ( Suppl. 3 ), 268 – 278 . 10.1080/10810730.2011.604388 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn , C. Y. , Cavanaugh , K. , Wallston , K. A. , White , R. O. , & Rothman , R. L. ( 2009. ). Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control . Diabetes Care , 32 ( 9 ), 1614 – 1619 . 10.2337/dc09-0425 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow , M. K. , Parker , R. M. , Gazmararian , J. A. , Nielsen-Bohlman , L. T. , & Rudd , R. R. ( 2005. ). The prevalence of limited health literacy . Journal of General Internal Medicine , 20 ( 2 ), 175 – 184 . 10.1111/j.1525-1497.2005.40245.x PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow , M. K. , Schillinger , D. , Weiss , B. D. , Bickmore , T. , Cabral , H. , Chang , P. , Bailey , S. C. , Dewalt , D. A. , Fernandez , A. , Fransen , M. , Leung , A. , McCaffery , K. , Meade , C. D. , McCormack , L. A. , Protheroe , J. , Parker , R. , Rothman , R. , Rubin , D. , Rudd , R. , Ownby , R. L. ( 2018. ). Health literacy and power . HLRP: Health Literacy Research and Practice , 2 ( 3 ), e132 – e133 . 10.3928/24748307-20180629-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelikan , J. M. , Ganahl , K. , & Roethlin , F. ( 2018. ). Health literacy as a determinant, mediator and/or moderator of health: Empirical models using the European Health Literacy Survey dataset . Global Health Promotion , 25 ( 4 ), 1757975918788300 10.1177/1757975918788300 PMID: [DOI] [PubMed] [Google Scholar]
- Proctor , R. N. ( 2002. ). Medicine under the Nazis . Harvard University Press; . [Google Scholar]
- Rauscher , K. J. , & Myers , D. J. ( 2014. ). Occupational health literacy and work-related injury among U.S. adolescents . International Journal of Injury Control and Safety Promotion , 21 ( 1 ), 81 – 89 . 10.1080/17457300.2013.792288 PMID: [DOI] [PubMed] [Google Scholar]
- Rowlands , G. , Shaw , A. , Jaswal , S. , Smith , S. , & Harpham , T. ( 2017. ). Health literacy and the social determinants of health: A qualitative model from adult learners . Health Promotion International , 32 ( 1 ), 130 – 138 . 10.1093/heapro/dav093 PMID: [DOI] [PubMed] [Google Scholar]
- Sarkar , U. , Karter , A. J. , Liu , J. Y. , Adler , N. E. , Nguyen , R. , López , A. , & Schil-linger , D. ( 2010. ). The literacy divide: Health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE) . Journal of Health Communication , 15 ( Suppl. 2 ), 183 – 196 . 10.1080/10810730.2010.499988 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenker , Y. , Fernandez , A. , Sudore , R. , & Schillinger , D. ( 2011. ). Interventions to improve patient comprehension in informed consent for medical and surgical procedures: A systematic review . Medical Decision Making , 31 , 151 – 173 . 10.1177/0272989X10364247 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger , D. ( 2007. ). Literacy and health communication: Reversing the ‘inverse care law’ . The American Journal of Bioethics , 7 , 15 – 18 . 10.1080/15265160701638553 PMID: [DOI] [PubMed] [Google Scholar]
- Schillinger , D. , Barton , L. R. , Karter , A. J. , Wang , F. , & Adler , N. ( 2006. ). Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes . Public Health Reports , 121 , 245 – 254 . 10.1177/003335490612100305 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger , D. , Bindman , A. , Wang , F. , Stewart , A. , & Piette , J. ( 2004. ). Functional health literacy and the quality of physician-patient communication among diabetes patients . Patient Education and Counseling , 52 ( 3 ), 315 – 323 . 10.1016/S0738-3991(03)00107-1 PMID: [DOI] [PubMed] [Google Scholar]
- Schillinger , D. , McNamara , D. , Crossley , S. , Lyles , C. , Moffet , H. H. , Sarkar , U. , Duran , N. , Allen , J. , Liu , J. , Oryn , D. , Ratanawongsa , N. , & Karter , A. J. ( 2017. ). The next frontier in communication and the ECLIPPSE Study: Bridging the linguistic divide in secure messaging . Journal of Diabetes Research , 2017 , 1348242 10.1155/2017/1348242 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger , D. , & Sarkar , U. ( 2009. ). Numbers don't lie, but do they tell the whole story? Diabetes Care , 32 ( 9 ), 1746 – 1747 doi: 10.2337/dc09=1071 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger , D. , Tran , J. , & Fine , S. ( 2018. ). Do low income youth of color see “the bigger picture” when discussing type 2 diabetes: A qualitative evaluation of a public health literacy campaign . International Journal of Environmental Research and Public Health , 15 , E840 Advance online publication. 10.3390/ijerph15050840 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seibert , R. G. , Winter , M. R. , Cabral , H. J. , Wolf , M. S. , Curtis , L. M. , & Paasche-Orlow , M. K. ( 2019. ). Health literacy and income mediate racial/ethnic asthma disparities . HLRP: Health Literacy Research and Practice , 3 ( 1 ), e9 – e18 . 10.3928/24748307-20181113-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentell , T. , Braun , K. L. , Davis , J. , & Davis , T. ( 2013. ). Colorectal cancer screening: Low health literacy and limited English proficiency among Asians and Whites in California . Journal of Health Communication , 18 ( Suppl. 1 ), 242 – 255 . 10.1080/10810730.2013.825669 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentell T , Braun KL . ( 2012. ). Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California . Journal of Health Communication , 17 ( Suppl. 3 ), 82 – 99 . 10.1080/10810730.2012.712621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentell , T. L. , & Halpin , H. A. ( 2006. ). Importance of adult literacy in understanding health disparities . Journal of General Internal Medicine , 21 ( 8 ), 862 – 866 . 10.1111/j.1525-1497.2006.00538.x PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith , P. C. , Brice , J. H. , & Lee , J. ( 2012. ). The relationship between functional health literacy and adherence to emergency department discharge instructions among Spanish-speaking patients . Journal of the National Medical Association , 104 ( 11–12 ), 521 – 527 . 10.1016/S0027-9684(15)30218-2 PMID: [DOI] [PubMed] [Google Scholar]
- Sperber , N. R. , Bosworth , H. B. , Coffman , C. J. , Lindquist , J. H. , Oddone , E. Z. , Weinberger , M. , & Allen , K. D. ( 2013. ). Differences in osteoarthritis self-management support intervention outcomes according to race and health literacy . Health Education Research , 28 ( 3 ), 502 – 511 . 10.1093/her/cyt043 PMID: [DOI] [PubMed] [Google Scholar]
- Stepanikova , I. , Mollborn , S. , Cook , K. S. , Thom , D. H. , & Kramer , R. M. ( 2006. ). Patients' race, ethnicity, language, and trust in a physician . Journal of Health and Social Behavior , 47 , 390 – 405 . 10.1177/002214650604700406 PMID: [DOI] [PubMed] [Google Scholar]
- Sudore , R. L. , Landefeld , C. S. , Pérez-Stable , E. J. , Bibbins-Domingo , K. , Williams , B. A. , Schillinger , D. ( 2009. ). Unraveling the relationship between literacy, language proficiency, and patient-physician communication . Patient Education and Counseling , 75 ( 3 ), 398 – 402 doi: 10.1016/j.pec.2009.02.019 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudore , R. L. , Mehta , K. M. , Simonsick , E. M. , Harris , T. B. , Newman , A. B. , Satterfield , S. , Rosano , C. , Rooks , R. N. , Rubin , S. M. , Ayonayon , H. N. , & Yaffe , K. ( 2006. ). Limited literacy in older people and disparities in health and healthcare access . Journal of the American Geriatrics Society , 54 , 770 – 776 . 10.1111/j.1532-5415.2006.00691.x PMID: [DOI] [PubMed] [Google Scholar]
- Sudore , R. L. , Schillinger , D. , Katen , M. T. , Shi , Y. , Boscardin , W. J. , Osua , S. , & Barnes , D. E. ( 2018. ). Engaging diverse English and Spanish-speaking older adults in advance care planning . JAMA Internal Medicine , 178 ( 12 ), 1616 – 1625 . 10.1001/jamainternmed.2018.4657 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon , J. A. , Trujilo , A. , Rosenbaum , S. J. , & DeBuono , B . ( 2007. ). Low health hiteracy: Implications for National Health Policy . https://hsrc.himmelfarb.gwu.edu/sphhs_policy_facpubs/172/ [Google Scholar]
- Volandes , A. E. , Paasche-Orlow , M. , Gillick , M. R. , Cook , E. F. , Shaykevich , S. , Abbo , E. D. , & Lehmann , L. ( 2008. ). Health literacy not race predicts end-of-life care preferences . Journal of Palliative Medicine , 11 , 754 – 762 . 10.1089/jpm.2007.0224 PMID: [DOI] [PubMed] [Google Scholar]
- Wolf , M. S. , Gazmararian , J. A. , & Baker , D. W. ( 2005. ). Health literacy and functional health status among older adults . Archives of Internal Medicine , 165 ( 17 ), 1946 – 1952 . 10.1001/archinte.165.17.1946 PMID: [DOI] [PubMed] [Google Scholar]
- Wolf , M. S. , Knight , S. J. , Lyons , E. A. , Durazo-Arvizu , R. , Pickard , S. A. , Arseven , A. , Arozullah , A. , Colella , K. , Ray , P. , & Bennett , C. L. ( 2006. ). Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer . Urology , 68 ( 1 ), 89 – 93 . 10.1016/j.urology.2006.01.064 PMID: [DOI] [PubMed] [Google Scholar]
- Yin , H. S. , Johnson , M. , Mendelsohn , A. L. , Abrams , M. A. , Sanders , L. M. , & Dreyer , B. P. ( 2009. ). The health literacy of parents in the United States: A nationally pepresentative study . Pediatrics , 124 ( Suppl. 3 ), S289 – S298 . 10.1542/peds.2009-1162E [DOI] [PubMed] [Google Scholar]


