ABSTRACT
Rates of posttraumatic stress disorder (PTSD) and alcohol misuse are known to be high among postdeployment Veterans. Previous research has found that personality factors may be relevant predictors of postdeployment drinking, yet results have been inconsistent and may be influenced by the selection of drinking outcome. This study aimed to examine relations among PTSD, negative urgency, and the five factor models of personality with multiple alcohol consumption patterns, including maximum drinks in a day, number of binge drinking episodes, at-risk drinking, and average weekly drinks in a sample of 397 Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn Veterans. The pattern of results suggested that the association among personality, PTSD, and drinking may depend on which drinking outcome is selected. For example, maximum drinks in a day was significantly associated with younger age, male gender, low agreeableness, and an interaction between negative urgency and PTSD, whereas number of binge drinking days was significantly associated with younger age, extraversion, low agreeableness, and negative urgency. This study highlights the heterogeneity of drinking patterns among Veterans and the need for careful consideration and transparency of outcomes selection in alcohol research.
KEYWORDS: Five factor model of personality, alcohol use, multiplicity
What is the public significance of this article?— (1) We examined four different types of alcohol consumption: maximum consumed in a day, at-risk drinking, frequency of binge drinking, and average drinks per week. The relationship between personality factors such as agreeableness, extraversion, and negative urgency and alcohol misuse depended on how we define alcohol consumption. These results highlight the need for researchers to consider and report on multiple measures of alcohol consumption in future studies.
(2) We found that Veterans who report negative urgency, which is the tendency to act rashly when experiencing negative emotions, are more likely to report high levels of alcohol consumption. Having posttraumatic stress disorder and high negative urgency was associated with some forms of alcohol misuse such as drinking large quantities of alcohol in a single day.
(3) Of the five-factor personality variables, low agreeableness was associated with frequency of binge drinking and quantity of binge drinking. Extraversion was associated with at-risk drinking and frequency of binge drinking.
High levels of US military deployments over the last two decades have led to numerous causes for concern for Veteran readjustment to civilian life in the postdeployment phase. Research suggests the prevalence rate of posttraumatic stress disorder (PTSD) among Veterans is higher than it is in the rest of the civilian population, occurring in an estimated 23% of all military personnel participating in Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF; Fulton et al., 2015). The comorbidity between PTSD and alcohol misuse is well-established, with rates of comorbidity as high as 63% (Debell et al., 2014). Among Veterans, Seal and colleagues found Veterans of Iraq and Afghanistan conflicts with a diagnosis of PTSD were four times more likely to be diagnosed with an alcohol use disorder (Seal et al., 2011). Given the high rates of PTSD and alcohol use among Veterans, coupled with the multiple potential entry points for services within the VA medical system, research that identifies risk factors associated with alcohol misuse in Veteran samples is needed to improve screening and intervention.
Personality and alcohol consumption
Converging lines of research suggest personality traits such as neuroticism and conscientiousness from the Five Factor Model (FFM; McCrae & Costa, 1989) and impulsivity may predispose individuals to an externalizing expression of PTSD, including substance use (for review, see Miller, 2003). Previous research has consistently found low conscientiousness, low agreeableness, and high neuroticism to be associated with alcohol outcomes (Malouff, Thorsteinsson, Rooke, & Schutte, 2007). Other models have identified disinhibition factors, closely related to low conscientiousness and low agreeableness, associated with alcohol consumption in college students (Ibáñez et al., 2010). Results of a cluster analysis on a Veteran sample suggested personality traits cluster with self-reported drinking motives to differentially predict risk for PTSD, alcohol use, and comorbid PTSD-alcohol use (Hawn et al., 2018). For instance, those high in extraversion, agreeableness, and conscientiousness and low in drinking to cope motives and neuroticism were the lowest risk for PTSD symptom severity and alcohol use, whereas those high in neuroticism, high across all drinking motives, low in conscientiousness, and low in extraversion and agreeableness had the highest risk for both PTSD symptom severity and alcohol use (Hawn et al., 2018). More research is needed to understand how personality, deployment-related PTSD, and alcohol use are related in Veteran samples.
Negative urgency and alcohol consumption
High negative affect and impulsivity are commonly associated with PTSD in civilian (Miller, 2003) and Veteran (James, Strom, & Leskela, 2014) populations. High negative affect and impulsivity have also been linked to alcohol use in civilian (Settles et al., 2012) and Veteran (Hawn et al., 2019) populations. Together, these findings suggest impulsivity may play an important role in the connection between PTSD and alcohol use, particularly in heavily traumatized populations such as military personnel. However, impulsivity has been criticized for lacking specificity as a construct, and researchers have called for more clearly defined constructs capturing rash action (Strickland & Johnson, 2020). Negative urgency (NU), defined as the tendency to act rashly in response to negative affective states (Whiteside, Lynam, Miller, & Reynolds, 2005), is a specific facet of personality that may be of particular relevance to posttraumatic alcohol use. It has been suggested that NU is associated with disrupted cognitive processing (i.e., reduced executive functioning, impaired risk assessment) in the face of intense emotion and therefore accounts for an individual’s subsequent externalizing behavior (Kaiser, Milich, Lynam, & Charnigo, 2012). Settles et al. (2012) found NU to be a strong predictor of various externalizing behaviors, including substance use across multiple populations and developmental periods. Although NU is generally associated with high levels of neuroticism (e.g., trait negative affect) and low levels of conscientiousness of the FFM of personality, there is evidence NU may provide a more fine-grained understanding of the psychological processes underlying problematic behavior, which may point to more fruitful intervention targets (Cyders & Smith, 2008; Seibert, Miller, Pryor, Reidy, & Zeichner, 2010; Whiteside & Lynam, 2003).
As with personality more broadly, few studies have incorporated NU in models linking PTSD to alcohol misuse. Given the intense state-level negative affect associated with PTSD, it follows that people with predispositions to NU may be more prone to engage in rash action, such as excessive alcohol consumption, in the face of trauma-related distress. Prior research has demonstrated a significant, positive main effect of NU on both average weekly alcohol consumption and past month binge drinking days among Veterans (Hawn et al., 2019). In a small study of Veterans, a series of mediation models suggested NU mediates the relationship between PTSD and callous aggression, general disinhibition, and substance abuse (Dutra & Sadeh, 2018). However, such a model suggests that PTSD has a causal link to NU. However, working from a theory of NU as a trait, we suggest NU may moderate the effects of PTSD, such that those with PTSD and high NU will be more likely to engage in alcohol misuse.
Out of one, many – the challenge of multiple levels of aggregation
Further complicating our understanding of alcohol misuse, there are a multitude of potential drinking-related outcomes (e.g., binge drinking, risky or hazardous drinking, sustained drinking, alcohol dependence, alcohol abuse), and most studies have focused on only one or two drinking outcomes at a time, most often binge drinking or alcohol use disorders (Malouff et al., 2007; Stewart, 1996). In a 2007 meta-analysis of personality and different alcohol outcome studies, results showed problematic drinking behavior was associated with low conscientiousness, low agreeableness, and high neuroticism across measures of problematic alcohol use (Malouff et al., 2007). The authors also found that type of alcohol outcome (i.e., clinical diagnosis or alcohol-related problems versus quantity of alcohol) moderated the observed effects of neuroticism and extraversion. Specifically, when the quantity of alcohol was examined, the effect sizes for conscientiousness, agreeableness, and neuroticism were smaller, and the effect size for extraversion was larger compared to when clinical diagnosis of an alcohol disorder or total level of alcohol problems was examined.
Malouff and collegues argued that diagnosis/problems may have greater clinical relevance; however, we suggest alcohol intake may be useful for screening purposes due to research that has suggested high rates of underreporting of alcohol use disorders among Veterans (Eisen et al., 2012) and the well-established negative health and psychosocial outcomes associated with excessive alcohol consumption. Diary or calendar recall methods are useful for capturing a wealth of data about the frequency and quantity of alcohol consumption, allowing for nuanced examination of drinking patterns and correlates (Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998). At the same time, they present a theoretic and data analytic challenge to researchers; that is, which outcome to examine? Total number of drinks? Frequency of drinking? The most consumed in a single day? Does one consider whether someone ever engaged in binge drinking, even once, to be equivalent to someone who binge drinks once or twice a week (e.g., NIAAA criteria for at-risk or heavy alcohol use; NIAAA, n.d.)?
Without consensus in field about the best way to measure alcohol-related outcomes, researchers face what has been called the problem of multiplicity which, together with incomplete reporting, has been described as one of the greatest contributors to the lack of reproducibility in the sciences (Goodman, Fanelli, & Ioannidis, 2016). This further leads to difficulty in determining the robustness of findings across studies that use different measures, metrics, or methods of aggregation (Cybulski, Mayo-Wilson, & Grant, 2016). Many researchers have called for increased transparency in reporting the availability and selection of outcomes (Goodman et al., 2016). Thus, this study aims to examine the influence of outcome selection (e.g., weekly consumption, binge drinking, at-risk drinking, and the maximum consumed on a single day) on the pattern of results to inform future research on which alcohol consumption metrics may be most associated with PTSD and/or personality.
Present study
The present study has two primary aims. Our first aim is to understand the extent to which PTSD, NU, and the FFM personality traits account for unique variance in past-month drinking of Veterans. We test the hypothesis that NU and PTSD interact, such that those with PTSD who are high in NU will be at increased risk for problematic alcohol consumption. Second, we examine multiple metrics of alcohol consumption (e.g., at-risk drinking, number of binge drinking days, maximum drinks in a single day, and average drinks per week) to determine if PTSD, NU, and FFM are differentially associated with different consumptions patterns.
Methods
Participants
Data were drawn from a larger study on stress-induced alcohol consumption among Veterans who had deployed to conflicts post-September 11, 2001, that involved a laboratory-administered alcohol challenge. Eligible participants were between the ages of 21 and 40. Participants were recruited from 2011–2017, primarily through flyers mailed to Veterans registered with the local VA Medical Center. Potential participants were prescreened over the telephone and had to be regular drinkers (i.e., drink alcohol on at least four days in the month prior to the screener) and not have a distaste for beer. Participants were excluded during the initial screen if they endorsed experiencing a recent history of alcohol dependence or withdrawal or were currently cutting back on drinking. Additional exclusion criteria included history of a moderate or severe traumatic brain injury, the presence of a condition that affected hypothalamic-pituitary-adrenal axis functioning (e.g., individuals taking psychoactive medications, antihistamines, or anti-inflammatory medications, hypertension, chronic pain, Addison’s disease), smokers who could not abstain from smoking for at least four hours, and severe obesity (i.e., BMI ≥ 40). With the exception of nicotine and caffeine, participants could not be dependent on drugs. Additionally, pregnant or nursing women were excluded from participation.
Procedure
Following initial screening for inclusion and exclusion criteria by telephone or online via Research Electronic Data Capture (REDCap; Harris et al., 2009), all participants were asked to provide verbal consent or indicate agreement with a consent statement online before responding to screening questions. Eligible participants were scheduled for an on-campus visit, completed in-person informed consent, and completed the self-report questionnaires and a clinical interview. Participants were compensated 20 US dollars for this portion of the study.
Measures
Demographics
A study-specific questionnaire was used to obtain data on participant demographics (e.g., age, gender, race, ethnicity, military branch).
UPPS+P impulsive behavior scale (Cyders et al., 2007)
The revised version of the UPPS (Whiteside et al., 2005), UPPS+P, assesses five domains of impulsive behavior: NU, (lack of) premeditation, (lack of) perseverance, sensation seeking, and positive urgency. Items are scored on a scale of 1–4 and averaged. Only the NU scale was used for the current analyses. Reliability coefficient for the NU scale was .89.
NEO five-factor inventory (NEO-FFI; McCrae & Costa, 1989)
The NEO-FFI is a shortened version of the NEO Personality Inventory (NEO-PI), with only 60 questions compared to the original 180 derived from the 12 strongest items in each factor. The factors measured with the NEO-FFI are neuroticism (NRT), openness to experience (OPN), extraversion (EXT), conscientiousness (CON), and agreeableness (AGR). Respondents are instructed to rate each item on a five-point Likert scale, from SD (strongly disagree) to SA (strongly agree). Reliability coefficients for the NEO-FFI scales ranged from .76 – .87.
Clinician administered PTSD scale (CAPS; Blake et al., 1998)
The CAPS is a diagnostic interview for current and lifetime PTSD. Participants first completed a life events checklist, indicating if they ever experienced, witnessed, or learned about 17 types of potentially traumatic events. Given the focus on deployment-related PTSD of the larger study, deployment events meeting Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) A criteria were assessed first (e.g., combat-exposure, military sexual trauma occurring during deployment, loss of fellow soldier to suicide during deployment). If the participant endorsed a qualifying event, they were interviewed about past month PTSD symptoms. If they did not meet current PTSD symptoms, they were asked if they ever experienced the symptoms discussed and were interviewed for the most severe lifetime symptoms (whether deployment related or not). If participants did not meet PTSD criteria for the deployment event, they were asked to identify their “worst” event and, if meeting DSM-IV A criteria, were assessed for lifetime and current symptoms. The inter-rater reliability was high (i.e., kappa = .92) for the CAPS diagnostic algorithm, and internal consistency was acceptable for the total severity score (α = .89) and each of the three PTSD symptom cluster severity scores (ranging from .67–.82) in this sample. Past month diagnostic status (deployment-related or nondeployment-related) was used in the current analyses.
Mini-international neuropsychiatric interview (MINI; Sheehan et al., 1998)
The clinician-delivered structured clinical interview using DSM-IV criteria was used to assess alcohol dependence and alcohol abuse disorders. This measure demonstrates excellent inter-rater reliability, with all kappa values above 0.75 and the majority over 0.90 or higher. Furthermore, the majority of kappas for test-retest reliability were above 0.75, indicating very good test-retest reliability.
Timeline followback (TLFB; Sobell & Sobell, 1996)
The TLFB collects data regarding quantity and frequency of drinking during the prior 30 days. The TLFB has been psychometrically validated and used extensively to derive primary drinking behavior. The TLFB demonstrates test-retest reliability correlations above .85 (Sobell & Sobell, 1996). Individuals were categorized as at-risk or not-at-risk social drinkers (defined according to NIAAA published criteria as more than 4 standard drinks a day OR more than 14 drinks per week for men, and more than 3 standard drinks a day OR more than 7 drinks per week for women). The total number of binges was calculated as the count of days in which more than 4 standard drinks for men or more than 3 standard drinks for women were consumed. Weekly average was calculated by dividing total drinks consumed in 30 days by 4.285. Finally, the maximum number of drinks reported in a single day was calculated.
Data analysis plan
To test study questions, the effects of FFM personality traits, PTSD, NU, as well as the interaction between PTSD and NU over and above the covariates age and gender on the different drinking outcomes were estimated. Specifically, ordinary least squares regression was used in predicting weekly average drinks and maximum drinks per day, logistic regression was used in predicting at-risk drinking status, and negative binomial regression was used in predicting number of binge drinking days. These different types of regression were used because of the different types of outcomes: continuous, dichotomous, and count, respectively. Analyses were conducted in Mplus Version 8 (Muthen & Muthen, 2017). For all models, the Maximum Likelihood Robust estimator was used in conjunction with Montecarlo Integration for at-risk drinking and number of binge drinking days. In addition to the models described, we used Mplus to conduct Monte Carlo Simulations (Muthén & Muthén, 2002) to conduct a posthoc power analysis to determine what power we had to detect the observed effects.
Results
In total, 397 participants with complete past-month PTSD diagnosis were included in this study. Demographic characteristics are generally consistent with overall active-duty US Military personnel at the time of data collection (Department of Defense, 2015). Participants were predominately White (66.8% [n = 265]; 21.2% Black [n = 84], 8.6% Other [n = 34], 3.5% [n = 14] missing) with a mean age of 30.4 years (SD = 4.5) and were 90.2% (n = 358) male. Participants were 52.4% (n = 208) Veterans of the Army, 19.4% (n = 77) Marines, 10.8% (n = 43) Navy, 4.3% (n = 17) Air Force, and the remaining 13.1% (n = 52) from Reserves/Guards. Overall, the sample reported high levels of alcohol consumption. Participants reported drinking over the previous 30 days an average maximum of 6.77 drinks in a day (SD = 5.54), 2.58 binges (SD = 3.83), and 9.30 drinks per week (SD = 8.88); 63.2% (n = 251) of the sample reported engaging in at-risk drinking as defined by NIAAA criteria. 25.9% (n = 103) of participants endorsed current (past month) PTSD meeting DSM-IV criteria. 8.6% (n = 34) met criteria for alcohol dependence and an additional 14.4% (n = 57) met criteria for alcohol abuse, according to DSM-IV criteria. Descriptive statistics and correlations between the main study variables are presented in Table 1.
Table 1.
Correlations and descriptive statistics of main predictors and outcomes
| M(SD) n(%) a |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 30.4 (4.53) | ||||||||||||
| 2. Gender (male)a | 358 (90.2%) | .02 | |||||||||||
| 3. Neuroticism | 19.7 (8.81) | −.01 | .13* | ||||||||||
| 4. Extraversion | 28.8 (7.45) | −.13* | −.09 | −.52** | |||||||||
| 5. Openness | 31.6 (6.52) | −.08 | .04 | .04 | .23** | ||||||||
| 6. Agreeableness | 28.9 (6.65) | .03 | .07 | −.29** | .28** | .18** | |||||||
| 7. Conscientiousness | 34.2 (7.04) | .02 | −.02 | −.43** | .25** | .05 | .17** | ||||||
| 8. PTSDa | 103 (25.9%) | −.03 | .02 | .38** | −.24** | −.04 | −.18** | −.14** | |||||
| 9. Negative Urgency | 2.12 (0.599) | .04 | .10 | .61** | −.26** | −.04 | −.27** | −.46** | .28** | ||||
| 10. Max/Day | 6.77 (5.54) | −.10 | −.14** | .09 | .02 | −.08 | −.21** | −.04 | .18** | .14** | |||
| 11. At-Riska | 251 (63.2%) | −.17** | −.04 | .11* | .12* | .07 | −.11* | −.05 | .13** | .18** | .51** | ||
| 12. # Binge Days | 2.58 (3.83) | −.12* | −.01 | .11* | .01 | −.00 | −.15** | −.08 | .14** | .18** | .52** | .50** | |
| 13. Average/Week | 9.30 (8.88) | −.07 | −.08 | .09 | .01 | −.03 | −.17** | −.07 | .21** | .18** | .66** | .49** | .85** |
n = 397
aDescriptive statics show percentage male, meeting criteria for PTSD, and meeting criteria for at-risk drinking. In correlations and subsequent analyses, male gender, being PTSD negative, not meeting at-risk drinking criteria served as reference groups.
Regression models
Results of the regression models predicting drinking outcomes are presented in Table 2.
Table 2.
Multivariate regressions of drinking behaviors on PTSD, personality factors, and negative urgency
| Max/Day |
At-Risk |
#Binge Days |
Weekly Average |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B | ß | SE ß | B | ß | SE ß | OR | B | ß | SE ß | B | ß | SE ß |
| Age | −.120* | −.098* | .041 | −.077** | −.172** | .057 | .926 | −.037* | −.383* | .156 | −.135 | −.069 | .044 |
| Gender | −2.243*** | −.119*** | .033 | −.314 | −.046 | .057 | .731 | −.021 | −.015 | .185 | −2.335 | −.078 | .043 |
| Neuroticism | .007 | .011 | .069 | .022 | .096 | .089 | 1.022 | .004 | .079 | .288 | −.068 | −.067 | .092 |
| Extraversion | .091 | .122 | .067 | .067*** | .248*** | .068 | 1.070 | .025* | .423* | .191 | .102 | .086 | .051 |
| Openness | −.060 | −.070 | .058 | .016 | .051 | .059 | 1.016 | −.002 | −.031 | .178 | −.014 | −.010 | .065 |
| Agreeableness | −.136** | −.164** | .055 | −.035 | −.114 | .062 | .966 | −.024 | −.365* | .182 | −.158 | −.118 | .071 |
| Conscientiousness | .029 | .037 | .047 | .015 | .051 | .066 | 1.015 | .002 | .037 | .199 | .005 | .004 | .055 |
| Negative Urgency | .159 | .017 | .081 | .401 | .119 | .084 | 1.492 | .472** | .650** | .209 | 1.884 | .127* | .065 |
| PTSD | 1.234 | .098 | .055 | .440 | .096 | .065 | 1.553 | .229 | .231 | .185 | 3.280** | .162** | .052 |
| PTSD X Negative Urgency | 3.575** | .205*** | .058 | 1.107* | .174* | .085 | 2.997 | .039 | .029 | .205 | 2.906 | .104 | .057 |
| Total R Squared | .137*** | .189*** | – | .106** | |||||||||
N = 397. PTSD = diagnosis of posttraumatic stress disorder according to DSM-IV criteria. Results of four regression analyses predicting maximum drinks in a single day (Max/Day), at-risk drinking status (At-Risk; defined according to NIAAA published criteria as more than 4 standard drinks a day OR more than 14 drinks per week for men, and more than 3 standard drinks a day OR more than 7 drinks per week for women), number of binge-drinking days (#Bing Days; count of days in which more than 4 standard drinks for men or more than 3 standard drinks for women were consumed), and weekly average (calculated by dividing total drinks consumed in 30 days by 4.285).
*p < .05, **p < .01, ***p < .001
Maximum drinks per day
Age, gender, AGR, and the interaction between PTSD and NU were significant predictors of max/day. Comparison of the standardized coefficients suggests that the interaction between PTSD and NU was the strongest predictor in the model. This model accounted for 13.7% of the variance in the maximum drinks per day. Specifically, younger individuals and males reported higher number of drinks in single day. Those who are less agreeable also consumed a higher maximum number. The simple slopes for the interaction between PTSD and NU suggests that for those with PTSD, more NU was associated with a higher number of max/day (β = 3.734, p < .05). In other words, accounting for the other variables in the model, for those with PTSD, for every SD increase in NU an increase of 1.13 max drinks per day would be expected. This effect was not significant (NS) for those without PTSD (β = .159, NS), see Figure 1.
Figure 1.
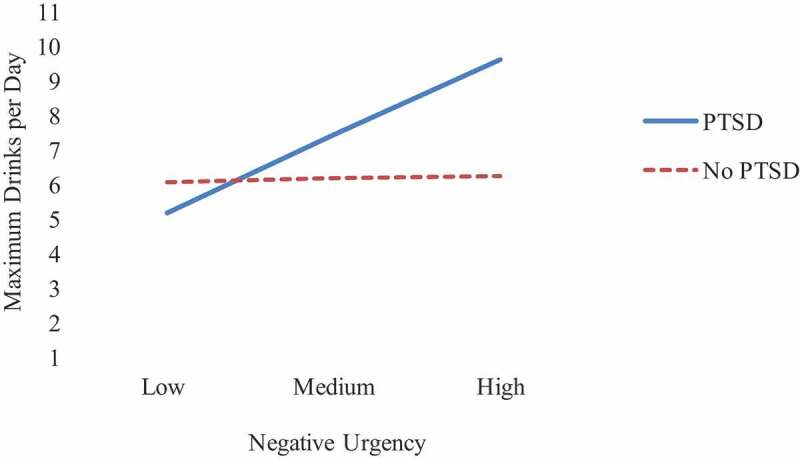
Depiction of interaction between negative urgency and PTSD to predict maximum drinks per day. Low, medium and high negative urgency reflects −1 standard deviation below the mean, at the mean, and 1 standard deviation above the mean
At-risk drinking status
In predicting at-risk drinking status, age, EXT, and the interaction between PTSD and NU were significant. This model accounted for 18.9% of the variance in at-risk drinking status. Specifically, younger individuals and those who reported more EXT are more likely to reporting being at-risk drinkers. The simple slopes of interaction between PTSD and NU show that for those with PTSD, more NU was associated with higher risk for being an at-risk drinker (β = 1.505, p < .01). This effect was not significant for those without PTSD (β = .400, NS), similar to the pattern observed for max/day.
Number of binge drinking days
In predicting the number of binge drinking days, age, EXT, AGR, and NU were significant. Specifically, younger individuals and those reporting higher levels of EXT, lower levels of AGR, and higher NU reported more binge drinking days. The nonsignificant interaction between PTSD and NU suggests that for those with (β = .511, p < .05) or without PTSD (β = .649, p < .01), more NU is associated with more binge drinking days.
Weekly average drinks
In predicting weekly average drinks, no demographic or FFM variables were significantly (p < .05) predictive. PTSD was significantly associated with average drinks per week, suggesting that those with PTSD consumed 3.28 more drinks than those without PTSD. This model accounted for 10.6% of the variance average weekly alcohol consumption. The interaction term between PTSD and NU was marginally significant (p < .10). Probing this marginally significant interaction indicated the simple slope of NU for those with PTSD was significant (β = 4.790, p < .01), but this was marginal for those without PTSD (β = 1.884, p = .056).
Post hoc power analysis
Although these may be underestimates of power, we found that for the most part we were underpowered (>.8) to detect small effects on our outcomes. Specifically, we were underpowered (>.8) to detect effects for any of our predictors of weekly average drinks or on number of binge drinking days. We had sufficient power to predict effects of agreeableness and NU predicting maximum drinks per day, and the effects of age and extraversion on at-risk drinking status. We were underpowered to detect any other effects on these two outcomes.
Discussion
This study aimed to explore the association among PTSD, the FFM of personality, and NU on drinking patterns among postdeployment Veterans. Previous research has consistently found low CON, low AGR, and high NRT to be associated with alcohol outcomes (Malouff et al., 2007). We found robust zero-order effects for AGR but inconsistent findings for NRT and no effect of CON. The regression models including the FFM, NU, and the interaction between PTSD and NU revealed different patterns, which we discuss in more detail.
In the regression models, the personality factors showed inconsistent associations with the various alcohol consumption outcomes while accounting for the variance explained by PTSD, age, and gender. Results showed those with low AGR and those with high NU and PTSD (but not those with PTSD and low NU) were more likely to consume higher levels of alcohol in a single day (i.e., maximum drinks per day). Similarly, at-risk drinking (defined as engaging in at least one binge drinking episode or drinking 14 drinks in a week for men, 7 drinks in a week for women) was associated with being extraverted and those with high NU and PTSD. EXT and low AGR were associated with frequency of binge drinking, as was NU, but not PTSD. These findings also suggest EXT and AGR influence drinking outcomes that capture acute drinking, such as at-risk and binge drinking behaviors, versus outcomes that capture general consumption, such as weekly average. Findings are partially consistent with previous research that people with high EXT and low NRT report more habitual drinking but not more drinks per occasion (Peterson, Morey, & Higgins, 2005), whereas CON and impulsivity have been associated with weekly consumption (Sellés, Tomás, Costa, & Mahía, 2015).
We found PTSD was significantly associated with all four drinking patterns (at-risk, binge, maximum per day, weekly average) at the zero-order level. These findings are consistent with and extend beyond the extant literature, which demonstrates an association between PTSD and alcohol consumption (Debell et al., 2014). However, in the regression models, PTSD was associated with maximum/day, at-risk status, and weekly average. Interestingly, PTSD was not significantly associated with frequency of binge drinking controlling for covariates. A possible explanation is that the binge variable defined by the NIAAA may not be suitable to detect the effect of PTSD in Veterans due to the relatively high degree of alcohol consumption compared to the general population (Ames & Cunradi, 2004; Carter, Capone, & Eaton Short, 2011).
The finding that NU is significantly associated with all alcohol outcomes, either as a main effect or modifying PTSD, is consistent with research that has found that individuals with higher NU were more likely to develop binge drinking and alcohol use disorder than those with lower NU (Shin, Hong, & Jeon, 2012), and previous research demonstrating significant main effects of NU on alcohol-related outcomes among OEF/OIF/OND Veterans (Hahn, Tirabassi, Simons, & Simons, 2015; Hawn et al., 2019). Together, these findings suggest a general predisposition to negative affect (i.e., NRT) does not necessarily predict alcohol misuse outcomes in post-deployment Veterans, whereas negative affect associated with PTSD specifically (i.e., weekly average) or modified by high NU (i.e., max/day or at-risk status) does predict some forms of alcohol misuse when other relevant covariates are controlled.
Regarding multiplicity of outcomes, our findings suggest the likelihood of finding significant relationships among drinking behaviors, PTSD, and personality factors may depend on which outcomes are selected. It is possible that different patterns of drinking behavior may reflect different underlying processes and highlight the need to carefully consider which outcomes are relevant in research aimed at uncovering those processes. For example, it is possible that specific metrics of alcohol consumption, such as maximum number of drinks consumed in a day or weekly average consumption, may better capture trauma-related drinking among Veteran samples compared to more personality-driven metrics of alcohol consumption, such as frequency of binge drinking. However, it is only with replication and complete reporting that we will be able to understand whether these differences reflect meaningful differences in underlying biopsychosocial processes or emerge as artifacts in design, measurement, or analysis (Goodman et al., 2016). Thus, replication of these results across other Veteran and/or civilian samples or using other methodologies (e.g., ecological momentary assessment, biometrics) would suggest there are meaningful differences in these drinking patterns, which could point to meaningful interventions.
Limitations
Interpreting these results should be done with several limitations in mind. As previously mentioned, participants who self-reported history of alcohol dependence or who were currently trying to cut back or abstain from alcohol use were prescreened out from study participation. It is possible those with the highest risk of alcohol consumption may be lower in this sample than the general Veteran population. Despite these screening procedures, 23% of participants met DSM-IV criteria for alcohol abuse or dependence once the full assessment was completed. A study of VA medical records found that 10% of Iraq and Afghanistan Veterans were diagnosed with alcohol abuse or dependence (Seal et al., 2011), suggesting this sample still captures individuals across a wide spectrum of alcohol use. It is unknown, however, whether these results extend to those who are restricting or abstaining from alcohol use, whether due to past drinking problems or other health, social, or religious reasons. Alcohol consumption was based on 30-day recall, which has been shown to be an underestimate of consumption compared to daily diaries, although these differences appear relatively small (Carney et al., 1998). Participants were also prescreened if they self-reported current major depression, inability to abstain from smoking for four hours, or medical conditions or use of medications affecting the HPA-axis (including most psychiatric medications). This limits findings to Veterans with relatively few psychiatric diagnoses. Given the high rates of psychiatric and substance use comorbidities associated with heavy alcohol use (Stecker, Fortney, Owen, McGovern, & Williams, 2010), future research is needed to determine if these patterns of associations are similar among Veterans with more complex psychiatric profiles. Given the vast heterogeneity of PTSD expression (Olbert, Gala, & Tupler, 2014), it is possible a different pattern of results would emerge if we had used symptom count or symptom severity, or examined individual symptoms clusters, such as hyperarousal or avoidance. Therefore, further exploration of these relationships is warranted. The cross-sectional design of the study limits our ability to account for potential mediating effects, such as an indirect causal effect of PTSD on the relationship between NU and alcohol-related outcomes. Examination of these relationships within a longitudinal framework that follows individuals from pre- to post-deployment is needed to shed light on whether there is a causal relationship among personality, drinking, and PTSD. Finally, post hoc power analyses indicated we were largely underpowered to detect hypothesized effects. Although we did find significant effects for some that we were underpowered to detect, we cannot rule out that nonsignificant effects may be due to lack of power.
Conclusions
The significant influences of EXT, AGR, PTSD, and NU on certain alcohol phenotypes but not others in the present sample speak to the need for increased breadth of research with regard to measurement of multiple patterns of alcohol use among Veterans. Thus, a critical strength to the present study is the more fine-tuned analysis of alcohol-related outcomes explored. We argue that testing and reporting a variety of alcohol use phenotypes is critical for identifying consensus outcomes, improving reproducibility, and identifying the extent to which differences in drinking patterns and behaviors meaningfully inform theories of alcohol misuse, particularly in relation to PTSD (e.g., self-medication hypothesis).
Clinical implications of this research are at least twofold. First, the finding that personality and PTSD were differentially associated with the different drinking outcomes suggests screening for alcohol-related problems should consider a range of drinking behaviors. For example, rather than or in addition to asking how many drinks do they typically consume in a week, asking what is the most they have consumed in a day may improve detection of alcohol-related problems. Given the multiple entry points in the VA health system for Veterans, widespread screening may help identify and refer Veterans in need of services for alcohol and PTSD. Second, the results from this study tentatively suggest screening for NU among postdeployment Veterans may provide valuable insight into risk and treatment targets. Although there are no evidence-based treatments for NU, clinicians working to address comorbid alcohol misuse and PTSD may want to consider the role that negative urgency, as a specific form of impulsivity, may play in the client’s drinking behaviors, particularly if the client is consuming excessive amounts of alcohol in a single setting. Targeting specific feelings of NU and identifying adaptive responses, such as psychological flexibility (Dutra & Sadeh, 2018), may lead to improved outcomes, although more research is needed.
Funding Statement
The main study was funded by NIAAA under grants R01 AA020179 and K02 AA023239 (PI: Amstadter). Sage Hawn’s time was funded by NIAAA F31 AA025820. REDCap survey software was funded under grant UL1TR002649 from the NCRR.
Disclosure statement
We have no known conflict of interest to disclose.
References
- Ames, G., & Cunradi, C. (2004). Alcohol use and preventing alcohol-related problems among young adults in the military. Alcohol Research & Health, 28(4), 252–258. [Google Scholar]
- Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Charney, D. S., & Keane, T. M. (1998). Clinician-administered PTSD scale for DSM-IV (CAPS-IV). Boston, MA: National Center for Posttraumatic Stress Disorder. [Google Scholar]
- Carney, M. A., Tennen, H., Affleck, G., Del Boca, F. K., & Kranzler, H. R. (1998). Levels and patterns of alcohol consumption using timeline follow-back, daily diaries and real-time “electronic interviews.” Journal of Studies on Alcohol, 59(4), 447–454. doi: 10.15288/jsa.1998.59.447 [DOI] [PubMed] [Google Scholar]
- Carter, A. C., Capone, C., & Eaton Short, E. (2011). Co-occurring posttraumatic stress disorder and alcohol use disorders in veteran populations. Journal of Dual Diagnosis, 7(4), 285–299. doi: 10.1080/15504263.2011.620453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cybulski, L., Mayo-Wilson, E., & Grant, S. (2016). Improving transparency and reproducibility through registration: The status of intervention trials published in clinical psychology journals. Journal of Consulting and Clinical Psychology, 84(9), 753–767. doi: 10.1037/ccp0000115 [DOI] [PubMed] [Google Scholar]
- Cyders, M. A., & Smith, G. T. (2008). Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin, 134(6), 807–828. doi: 10.1037/a0013341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders, M. A., Smith, G. T., Spillane, N. S., Fischer, S., Annus, A. M., & Peterson, C. (2007). Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment, 19(1), 107. doi: 10.1037/1040-3590.19.1.107 [DOI] [PubMed] [Google Scholar]
- Debell, F., Fear, N. T., Head, M., Batt-Rawden, S., Greenberg, N., Wessely, S., & Goodwin, L. (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425. doi: 10.1007/s00127-014-0855-7 [DOI] [PubMed] [Google Scholar]
- Department of Defense . (2015). 2015 demographics: Profile of the military community. http://download.militaryonesource.mil/12038/MOS/Reports/2015-Demographics-Report.pdf
- Dutra, S. J., & Sadeh, N. (2018). Psychological flexibility mitigates effects of PTSD symptoms and negative urgency on aggressive behavior in trauma-exposed veterans. Personality Disorders: Theory, Research, and Treatment, 9(4), 315–323. doi: 10.1037/per0000251 [DOI] [PubMed] [Google Scholar]
- Eisen, S. V., Schultz, M. R., Vogt, D., Glickman, M. E., Elwy, A. R., Drainoni, M.-L., … Martin, J. (2012). Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. American Journal of Public Health, 102(S1), S66–73. doi: 10.2105/AJPH.2011.300609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton, J. J., Calhoun, P. S., Wagner, H. R., Schry, A. R., Hair, L. P., Feeling, N., … Beckham, J. C. (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. doi: 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Goodman, S. N., Fanelli, D., & Ioannidis, J. P. A. (2016). What does research reproducibility mean? Science Translational Medicine, 8(341), 341ps12. doi: 10.1126/scitranslmed.aaf5027 [DOI] [PubMed] [Google Scholar]
- Hahn, A. M., Tirabassi, C. K., Simons, R. M., & Simons, J. S. (2015). Military sexual trauma, combat exposure, and negative urgency as independent predictors of PTSD and subsequent alcohol problems among OEF/OIF veterans. Psychological Services, 12(4), 378–383. doi: 10.1037/ser0000060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn, S. E., Chowdhury, N., Kevorkian, S., Sheth, D., Brown, R. C., Berenz, E., … Amstadter, A. B. (2019). Examination of the effects of impulsivity and risk-taking propensity on alcohol use in OEF/OIF/OND veterans. Journal of Military, Veteran and Family Health, 5, 88–99. doi: 10.3138/jmvfh.2018-0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn, S. E., Kurtz, E. D., Brown, E., Brown, R. C., Berenz, E. C., McDonald, S., … Amstadter, A. (2018). A cluster-analytic approach to determining drinking motives and personality typologies: Trauma group differences and respective relations to PTSD and problematic alcohol use. Psychology of Addictive Behaviors, 32(5), 528. doi: 10.1037/adb0000382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibáñez, M. I., Moya, J., Villa, H., Mezquita, L., Ruipérez, M. Á., & Ortet, G. (2010). Basic personality dimensions and alcohol consumption in young adults. Personality and Individual Differences, 48(2), 171–176. doi: 10.1016/j.paid.2009.09.017 [DOI] [Google Scholar]
- James, L. M., Strom, T. Q., & Leskela, J. (2014). Risk-taking behaviors and impulsivity among veterans with and without PTSD and mild TBI. Military Medicine, 179(4), 357–363. doi: 10.7205/MILMED-D-13-00241 [DOI] [PubMed] [Google Scholar]
- Kaiser, A. J., Milich, R., Lynam, D. R., & Charnigo, R. J. (2012). Negative urgency, distress tolerance, and substance abuse among college students. Addictive Behaviors, 37(10), 1075–1083. doi: 10.1016/j.addbeh.2012.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff, J. M., Thorsteinsson, E. B., Rooke, S. E., & Schutte, N. S. (2007). Alcohol involvement and the five-factor model of personality: A meta-analysis. Journal of Drug Education, 37(3), 277–294. doi: 10.2190/DE.37.3.d [DOI] [PubMed] [Google Scholar]
- McCrae, R., & Costa, P. (1989). The NEO-PI/NEO-FFI manual supplement. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Miller, M. W. (2003). Personality and the etiology and expression of PTSD: A three-factor model perspective. Clinical Psychology-Science and Practice, 10(4), 373–393. doi: 10.1093/clipsy/bpg040 [DOI] [Google Scholar]
- Muthen, L. K., & Muthen, B. (2017). Mplus version 8 user’s guide. Los Angeles, CA: Muthen & Muthen. [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2002). How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling, 9(4), 599–620. doi: 10.1207/S15328007SEM0904_8 [DOI] [Google Scholar]
- NIAAA . (n.d.). What are the different drinking levels? - Rethinking drinking. Retrieved June 12, 2020, from https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Drinking-Levels.aspx
- Olbert, C. M., Gala, G. J., & Tupler, L. A. (2014). Quantifying heterogeneity attributable to polythetic diagnostic criteria: Theoretical framework and empirical application. Journal of Abnormal Psychology, 123(2), 452–462. doi: 10.1037/a0036068 [DOI] [PubMed] [Google Scholar]
- Peterson, J. B., Morey, J., & Higgins, D. M. (2005). You drink, I drink: Alcohol consumption, social context and personality. Individual Differences Research, 3, 1. [Google Scholar]
- Seal, K. H., Cohen, G., Waldrop, A., Cohen, B. E., Maguen, S., & Ren, L. (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116(1), 93–101. doi: 10.1016/j.drugalcdep.2010.11.027 [DOI] [PubMed] [Google Scholar]
- Seibert, L. A., Miller, J. D., Pryor, L. R., Reidy, D. E., & Zeichner, A. (2010). Personality and laboratory-based aggression: Comparing the predictive power of the five-factor model, BIS/ BAS,and impulsivity across context. Journal of Research in Personality, 44(1), 13–21. doi: 10.1016/j.jrp.2009.09.003 [DOI] [Google Scholar]
- Sellés, P. M., Tomás, M. T. C., Costa, J. A. G., & Mahía, F. C. (2015). Predictors of weekly alcohol drinking and alcohol-related problems in binge-drinking undergraduates. Adicciones, 27(2), 119–131. [PubMed] [Google Scholar]
- Settles, R. E., Fischer, S., Cyders, M. A., Combs, J. L., Gunn, R. L., & Smith, G. T. (2012). Negative urgency: A personality predictor of externalizing behavior characterized by neuroticism, low conscientiousness, and disagreeableness. Journal of Abnormal Psychology, 121(1), 160–172. doi: 10.1037/a0024948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan, D. V., Lecrubier, Y., Harnett-Sheehan, K., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. (1998). The Mini International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview. Journal of Clinical Psychiatry, 59(suppl 20), 22–33. [PubMed] [Google Scholar]
- Shin, S. H., Hong, H. G., & Jeon, S.-M. (2012). Personality and alcohol use: The role of impulsivity. Addictive Behaviors, 37(1), 102–107. doi: 10.1016/j.addbeh.2011.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell, L. C., & Sobell, M. B. (1996). Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation. [Google Scholar]
- Stecker, T., Fortney, J., Owen, R., McGovern, M. P., & Williams, S. (2010). Co-occurring medical, psychiatric, and alcohol-related disorders among veterans returning from Iraq and Afghanistan. Psychosomatics, 51(6), 503–507. doi: 10.1016/S0033-3182(10)70743-X [DOI] [PubMed] [Google Scholar]
- Stewart, S. H. (1996). Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin, 120, 83–112. doi: 10.1037/0033-2909.120.1.83 [DOI] [PubMed] [Google Scholar]
- Strickland, J. C., & Johnson, M. W. (2020). Rejecting impulsivity as a psychological construct: A theoretical, empirical, and sociocultural argument. Psychological Review. doi: 10.1037/rev0000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside, S. P., & Lynam, D. R. (2003). Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: Application of the UPPS impulsive behavior scale. Experimental and Clinical Psychopharmacology, 11(3), 210. doi: 10.1037/1064-1297.11.3.210 [DOI] [PubMed] [Google Scholar]
- Whiteside, S. P., Lynam, D. R., Miller, J. D., & Reynolds, S. K. (2005). Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. European Journal of Personality, 19(7), 559–574. doi: 10.1002/per.556 [DOI] [Google Scholar]