Abstract
Neuroaxonal loss is believed to underpin the progressive disability that characterizes multiple sclerosis (MS). While focal inflammatory demyelination is a principal cause of acute axonal transection and subsequent axonal degeneration, the gradual attrition of permanently demyelinated axons may also contribute to tissue damage, particularly in the progressive phase of the disease. Therefore, remyelination is considered a putative neuroprotective strategy. In this article, we review the potential pitfalls of remyelination trials, provide a framework for their appropriate design and temper the expectations, at times unrealistic, of researchers, regulators and the pharmaceutical industry.
Multiple sclerosis (MS) is a complex disease of the CNS, characterized by inflammation, demyelination, neuroaxonal loss, and gliosis. Focal inflammatory demyelinating lesions are a pathologic hallmark of the disease and a primary contributor to both acute clinical relapse and the accumulation of longer-term disability. With the advent of disease-modifying therapy (DMT) more than 20 years ago, and the more recent development of highly efficacious agents, the inflammatory component of MS can be successfully arrested in majority of the cases. Therefore, the therapeutic development focus is now shifting toward the repair of damage, neuroprotection, and, potentially, restoration of functional deficit.1
Neuroaxonal loss is believed to underpin the progressive disability that characterizes MS. Although focal inflammatory demyelination is a principal cause of acute axonal transection and subsequent axonal degeneration, the gradual attrition of permanently demyelinated axons may also contribute to tissue damage, particularly in the progressive phase of the disease.
Indeed, several lines of experimental evidence suggest that permanent demyelination may contribute to accelerated axonal degeneration by rendering axons vulnerable to physiologic stress.2,3 Chronic demyelination increases the energy demands of axonal conduction, ultimately compromising axoplasmic adenosine triphosphate production, leading to an ionic imbalance and Ca2+-mediated axonal degeneration.4 In addition, lack of trophic support from myelin or oligodendrocytes and disruption of normal axon-myelin interactions may result in degeneration of chronically demyelinated axons.5,6 Loss of demyelinated axons may also be exacerbated by activation and proliferation of astrocytes.7,8
Therefore, remyelination is considered a putative neuroprotective strategy with important functions including lesion repair, protection of axons from inflammatory mediators and immune effector cells, and restoration of conduction velocity.2,3,9
Approaches to remyelination vary and include increased oligodendrocyte progenitor cell recruitment (semaphorins) and maturation (Notch, LINGO-1 and Wnt pathways; or vitamin D, thyroid hormone or activation of the retinoid X receptor), promotion of neuronal activity, or the targeting of microglia.10 Although a detailed description of remyelinating strategies is beyond the scope of the current article and has been comprehensively reviewed elsewhere,10-13 the ultimate result of remyelination is a repair of myelin and its potential neuroprotective and restorative effect.
A growing interest from pharmaceutical companies to develop remyelinating therapies has followed,11 and several clinical trials of potential remyelinating agents, including mesenchymal stem cells, clemastine, high-dose biotin, and opicinumab (anti-LINGO), have recently been conducted. In addition, there are a number of ongoing remyelination trials of domperidone, quetiapine, and nanocrystalline gold.14 A more complete list of current trials can be found in Ref. 13.
Failure of some trials, despite the fact that the therapeutic agent in question demonstrated remyelinating capacity in preclinical studies, prompted us to review the potential pitfalls of remyelination trials, provide a framework for their appropriate design, and temper the expectations, at times unrealistic, of researchers, regulators, and the pharmaceutical industry.
The remyelinating capacity of therapeutic agents is typically tested using an acute lesion model (both experimental and clinical), but then applied to chronic lesions.
Remyelination is more likely to succeed in the acute MS lesion, whereas the environment for successful remyelination may be unfavorably altered in chronic lesions.15-18 There are indications that a window of opportunity exists for the process of remyelination to be successful,17,19 which may be related to proreparative interactions between various cell populations and cytokines within the early MS lesion.16,20-24 For example, macrophages and acute inflammatory mediators may promote, and astrocytes may inhibit, the migration and differentiation of oligodendrocyte progenitor cells. The window of opportunity for remyelination may therefore open following sufficient expansion and differentiation of perilesional and lesional oligodendrocyte precursor cells and end with the conversion of acute to chronic inflammation25 As a result, the lesion environment is likely to become less permissive for remyelination in long-standing lesions.16 Although there are no available data to verify a “window of opportunity” concept in human clinical trials of remyelinating agents, some clinical studies of spontaneous remyelination suggest that first 3–6 months after acute demyelination represent the best window of opportunity for successful restoration of myelin.23
Therefore, the remyelinating capacity of a certain therapeutic agent, determined using an acute lesion model, should not necessarily be directly translated into clinical trials based on the remyelination of chronic lesions. On the contrary, mechanism of action (phase 2) studies of remyelinating agents must be conducted on acute and chronic lesions separately before proceeding to clinically based phase 3 trials.
2. Although chronic demyelination appears to be harmful for axonal survival in the long term, this effect may not be clinically measurable within the time frame of a clinical trial.
A significant body of experimental data supports the notion that chronic demyelination is harmful for axonal survival. A preventive role of remyelination was demonstrated in several animal studies, reviewed recently.10 However, there is limited clinical research examining the magnitude of this effect and its clinical relevance in MS.
Using the visual system as a model, we recently demonstrated that chronic demyelination of the optic nerve caused by optic neuritis accelerates the loss of retinal ganglion cell axons, as measured by thinning of the retinal nerve fiber layer (RNFL). Furthermore, we showed that progressive RNFL thinning is associated with the degree of optic nerve demyelination and reflects the topography of pathology in the optic nerve.26 However, the effect was small and, considering the length of follow-up in our study (average 4 years), slow to manifest.
Therefore, to establish the detrimental impact of chronic demyelination on neuroaxonal survival using clinical outcome measures, a prohibitively long observation period may be required. Consequently, a positive effect of remyelination, aimed at alleviating this damage, will be equally difficult to detect in the time frame of a typical 12–36-month phase 2 clinical trial.
Moreover, compared with structural biomarkers, functional measures are typically more variable and less sensitive,27 reflecting a spectrum of physiologic variables. The use of functional outcome measures to detect a positive effect of remyelination therapy may therefore prove to be an insurmountable task. For example, in a recent clinical trial of clemastine, a significant, albeit small, improvement of optic pathway conduction speed (suggesting remyelination) did not translate into functional recovery (low contrast visual acuity)28 over the 150-day study period.
3. What should we expect from remyelination-restoration of lost function or prevention of future functional deficit?
In a recently published comprehensive review of remyelinating strategies, Lubetzki et al.10 questioned “whether a remyelinating strategy should improve pre-existing disability (implying viable demyelinated axons that can be repaired) or prevent subsequent disability worsening (aiming for a neuroprotective role of myelin regeneration).” The answer to this question should determine the choice of “reasonable clinical outcomes that can be expected from pro-remyelination medications.”11
Although intermittent conduction block can occur in chronically demyelinated axons, particularly in the context of increased body temperature, there is no direct experimental evidence to suggest that chronic CNS demyelination per se directly leads to permanent loss of conduction along the axons, and as a result cause significant sensory, motor, or other functional deficits.29 (Note that in congenital disorders of dysmyelination, such as Pelizaeus Merzbacher Disease (PMD), mutation typically results in demyelination on a much larger scale compared with the one seen in MS and also frequently associated with axonal damage and neuronal loss. Combination of those factors is likely to give rise to progressive motor dysfunction often seen in patients with PMD30).
Indeed, both experimental and clinical studies demonstrate that, after brief conduction block caused by an acute inflammatory milieu (and associated functional impairment), survived but chronically demyelinated fibers largely recover the ability to conduct (and, therefore, their functional capability) following a redistribution of sodium channels along the axonal membrane, albeit more slowly and in an energy-inefficient manner.31 Therefore, repair of myelin sheaths, while restoring faster (saltatory) conduction in survived demyelinated axons, is not likely to measurably improve neurologic deficits, which are primarily attributable to neuroaxonal loss sustained during the acute phase of lesion formation.5,32
A frequently cited study33 supporting the link between remyelination of extensive demyelinated areas and functional recovery is based on an unusual dietary model of demyelination in cats, the so-called Feline Irradiated Diet-Induced Demyelination (FIDID). However, the myelinotoxic mechanisms of FIDID model remain unknown. In addition, demyelination following irradiated diet is accompanied by clear signs of inflammation such as extensive vacuolation of white matter and macrophage infiltration. Therefore, it is unclear whether initial functional deficit reported in FIDID animals is caused by demyelination or is a result of concomitant toxic and inflammatory processes, resolution of which may partly be responsible for functional recovery.33
The association of functional deficit during acute demyelination with inflammation, rather than with loss of myelin sheaths per se, is also supported by absence of functional impediment in toxin-based models of demyelination that do not typically include the inflammatory component.10 Yamazaki et al.34 similarly concluded that resolution of inflammation plays a critical role in functional motor recovery after toxic demyelination in a recent experimental study examining association between remyelination and functional recovery. Nevertheless, because chronic demyelination can potentially accelerate axonal injury and death within MS lesions, restoring myelin sheaths is likely to prevent or reduce future neuroaxonal loss and hinder disability progression. However, given the small impact of chronic demyelination on neurodegeneration,24 a manifestly weak structure-function relationship, and high functional redundancy built into physiologic systems (for example, the relationship between loss of retinal ganglion cells in glaucoma35 or optic neuritis36 and visual field changes), clinically measurable prevention of deterioration would require a lengthy observation period. Therefore, existing clinical trial paradigms, in which therapies must show a clinical benefit, such as slowing progression of disability as measured by established physical (Expanded Disability Status Scale, 9HPT, and T25FW), cognitive (Symbol Digit Modalities Test and Paced Auditory Serial Addition Test), or composite (Multiple Sclerosis Functional Composite) disability outcomes within the confines of a 2–3-year period of observation, are ill equipped to demonstrate the efficacy of remyelinating therapies. Although it is tempting to speculate that the use of functional outcomes was the reason for failure of some recent clinical remyelination trials, this must await further investigation.
A less conventional approach to this problem may be required. First, it is imperative to prove beyond doubt that chronic CNS demyelination negatively affects the clinical course of MS or at least accelerates axonal loss. Once convincingly established, the search for remyelinating agents will be warranted, and electrophysiologic or imaging biomarkers of remyelination, rather than functional outcomes, justifiably included as primary end points in clinical trials. Thus, for instance, visual evoked potentials can be used to assess increase in speed of conduction (and, accordingly, the degree of remyelination) along the visual pathway in patients with chronic lesions in optic nerve or optic radiation (which are very frequent in MS),28,37-39 whereas latency of auditory and somatosensory evoked potentials also reliably reflect myelination changes in corresponding tracts.40 The is also large variety of imaging techniques such as MTR, DTI, and myelin water fraction to assess de/remyelination in chronic MS lesions.41-44 Although the proposed approach is currently, and for the foreseeable future, not accepted by regulatory authorities, we believe that the time is ripe for researchers, peak bodies, and the pharmaceutical industry to work together to change the status quo.
Glossary
- DMT
disease-modifying therapy
- FIDID
Feline Irradiated Diet-Induced Demyelination
- MS
multiple sclerosis
- PMD
Pelizaeus Merzbacher Disease
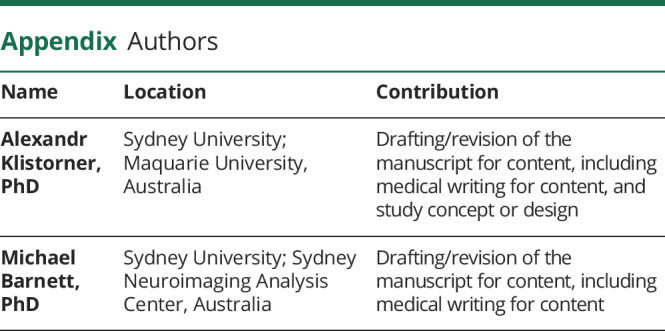
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/NN for full disclosures.
References
- 1.Garber JY, Barnett MH. We should focus more on finding therapeutic targets for the non-inflammatory damage in MS–yes. Mult Scler J. 2018;24(suppl 2):1272-1274. [DOI] [PubMed] [Google Scholar]
- 2.Brück W, Kuhlmann T, Stadelmann C. Remyelination in multiple sclerosis. J Neurol Sci. 2003;206(2):181-185. [DOI] [PubMed] [Google Scholar]
- 3.Kornek B, Storch MK, Weissert R, et al. . Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative study of axonal injury in active, inactive and remyelinated lesons. Am J Pathol. 2000;157(1):267-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Correale J, Storch MK, Weissert R, et al. Progressive multiple sclerosis : from pathogenic mechanisms to treatment multiple sclerosis. Brain. 2017;140(3):527-546. [DOI] [PubMed] [Google Scholar]
- 5.Trapp BD, Ransohoff R, Fisher E, Rudick R. Neurodegeneration in multiple sclerosis: relationship to neurological disability. Neuroscientist. 1999;5:48-57. [Google Scholar]
- 6.Peterson LK, Fujinami RS. Inflammation, demyelination, neurodegeneration and neuroprotection in the pathogenesis of multiple sclerosis. J Neuroimmunol. 2007;184(1–2):37-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Correale J, Farez MF, Cardona AE. The role of astrocytes in multiple sclerosis progression. Front Neurol. 2015;6:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liddelow SA, Guttenplan KA, Clarke LE, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Groot CJA, Ruuls SR, Theeuwes JMW, et al. Immunocytochemical characterization of the expression of inducible and constitutive isoforms of nitric oxide synthase in demyelinating multiple scleroisis lesions. J Neuropathol Exp Neurol. 1997;56(1):10-20. [DOI] [PubMed] [Google Scholar]
- 10.Lubetzki C, Zalc B, Williams A, Stadelmann C, Stankoff B. Remyelination in multiple sclerosis: from basic science to clinical translation. Lancet Neurol. 2020;19(8):678-688. [DOI] [PubMed] [Google Scholar]
- 11.Plemel JR, Liu WQ, Yong VW. Remyelination therapies: a new direction and challenge in multiple sclerosis. Nat Rev Drug Discov. 2017;16(9):617-634. [DOI] [PubMed] [Google Scholar]
- 12.Olsen JA, Akirav EM. Remyelination in multiple sclerosis: cellular mechanisms and novel therapeutic approaches. J Neurosci Res. 2015;93(5):687-696. [DOI] [PubMed] [Google Scholar]
- 13.Cunniffe N, Coles A. Promoting remyelination in multiple sclerosis. J Neurol. 2019;268(1):30-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baldassari LE, Feng J, Clayton BLL, et al. Developing therapeutic strategies to promote myelin repair in multiple sclerosis. Expert Rev Neurother. 2019;19(10):997-1013. [DOI] [PubMed] [Google Scholar]
- 15.Ruffini F, Kennedy TE, Antel JP. Inflammation and remyelination in the central nervous system. Am J Pathol. 2004;164(5):1519-1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chari DM, Blakemore WF. New insights into remyelination failure in multiple sclerosis: implications for glial cell transplantation. Mult Scler. 2002;8(4):271-277. [DOI] [PubMed] [Google Scholar]
- 17.Blakemore WF, Chari DM, Gilson JM, Crang AJ. Modelling large areas of demyelination in the rat reveals the potential and possible limitations of transplanted glial cells for remyelination in the CNS. Glia. 2002;38(2):155-168. [DOI] [PubMed] [Google Scholar]
- 18.Kuhlmann T, Miron V, Cui Q, et al. Differentiation block of oligodendroglial progenitor cells as a cause for remyelination failure in chronic multiple sclerosis. Brain. 2008;131(pt 7):1749-1758. [DOI] [PubMed] [Google Scholar]
- 19.Chari DM, Blakemore WF. Efficient recolonization of progenitor-depleted areas of the CNS by adult oligodendrocyte progenitor cells. Glia. 2002;37(4):307-313. [PubMed] [Google Scholar]
- 20.Foote AK, Blakemore WF. Inflammation stimulates remyelination in areas of chronic demyelination. Brain. 2005;128(pt 3):528-539. [DOI] [PubMed] [Google Scholar]
- 21.Zhao C, Fancy SP, Kotter MR, Li WW, Franklin RJ. Mechanisms of CNS remyelination--the key to therapeutic advances. J Neurol Sci. 2005;233(1–2):87-91. [DOI] [PubMed] [Google Scholar]
- 22.Irvine KA, Blakemore WF. Remyelination protects axons from demyelination-associated axon degeneration. Brain. 2008;131(pt 6):1464-1477. [DOI] [PubMed] [Google Scholar]
- 23.Dubois-Dalcq M, Williams A, Stadelmann C, Stankoff B, Zalc B, Lubetzki C. From fish to man: understanding endogenous remyelination in central nervous system demyelinating disease. Brain. 2008;131(pt 7):1686-1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franklin R, Zhao C, Sim FJ. Astrocyte and macrophage interactions in promoting oligodendrocyte remyelination in the CNS. In: Glial Interfaces in the Nervous System. IOS Press; 2002:95-104. [Google Scholar]
- 25.Kotter MR, Stadelmann C, Hartung H-P. Enhancing remyelination in disease: can we wrap it up? Brain. 2011;134(pt 7):1882-1900. [DOI] [PubMed] [Google Scholar]
- 26.You Y, Barnett MH, Yiannikas C, et al. Chronic demyelination exacerbates neuroaxonal loss in MS patients with unilateral optic neuritis. Neurol Neuroimmunol Neuroinflammation. 2020;7(3):e700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yeh EA, Marrie RA, Reginald YA, et al. Functional-structural correlations in the afferent visual pathway in pediatric demyelination. Neurology. 2014;83(23):2147-2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green AJ, Gelfand JM, Cree BA, et al. Clemastine fumarate as a remyelinating therapy for multiple sclerosis (ReBUILD): a randomised, controlled, double-blind, crossover trial. Lancet. 2017;390(10111):2481-2489. [DOI] [PubMed] [Google Scholar]
- 29.Felts PA, Baker TA, Smith KJ. Conduction in segmentally demyelinated mammalian central axons. J Neurosci. 1997;17(19):7267-7277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sima A, Barnett MH, Yiannikas C, et al. Neuronal loss in Pelizaeus–Merzbacher disease differs in various mutations of the proteolipid protein 1. Acta Neuropathol. 2009;118(4):531-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith KJ, Waxman SG. The conduction properties of demyelinated and remyelinated axons. In: Waxman SG, ed. Multiple Sclerosis as Neuronal Disease. Elsevier Academic Press; 2005:85-100. [Google Scholar]
- 32.Lemus HN, Warrington AE, Rodriguez M. Multiple sclerosis: mechanisms of disease and strategies for myelin and axonal repair. Neurol Clin. 2018;36(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duncan ID, Brower A, Kondo Y, Curlee JF, Schultz RD. Extensive remyelination of the CNS leads to functional recovery. Proc Natl Acad Sci U S A. 2009;106(16):6832-6836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamazaki R, Ohno N, Huang JK. Acute motor deficit and subsequent remyelination-associated recovery following internal capsule demyelination in mice. J Neurochem. 2021;156(6):917-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, pappilledema and toxic neuropathy. Arch Ophthalmol. 1982;100(1):135-146. [DOI] [PubMed] [Google Scholar]
- 36.Costello F, Hodge W, Pan YI, Eggenberger E, Coupland S, Kardon RH. Tracking retinal nerve fiber layer loss after optic neuritis: a prospective study using optical coherence tomography. Mult Scler. 2008;14(7):893-905. [DOI] [PubMed] [Google Scholar]
- 37.Heidari M, Radcliff AB, McLellan GJ, et al. Evoked potentials as a biomarker of remyelination. Proc Natl Acad Sci U S A. 2019;116(52):27074-27083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alshowaeir D, Yiannikas C, Garrick R, et al. Latency of multifocal visual evoked potentials in nonoptic neuritis eyes of multiple sclerosis patients associated with optic radiation lesions. Invest Ophthalmol Vis Sci. 2014;55(6):3758-3764. [DOI] [PubMed] [Google Scholar]
- 39.Klistorner A, Chai Y, Leocani L, et al. Assessment of opicinumab in acute optic neuritis using multifocal visual evoked potential. CNS Drugs. 2018;32(12):1159-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farley BJ, Morozova E, Dion J, et al. Evoked potentials as a translatable biomarker to track functional remyelination. Mol Cell Neurosci. 2019;99:103393. [DOI] [PubMed] [Google Scholar]
- 41.van der Weijden CWJ, García DV, Borra RJH, et al. Myelin quantification with MRI: a systematic review of accuracy and reproducibility. Neuroimage. 2020;226:117561. [DOI] [PubMed] [Google Scholar]
- 42.Jelescu IO, Zurek M, Winters KV, et al. In vivo quantification of demyelination and recovery using compartment-specific diffusion MRI metrics validated by electron microscopy. Neuroimage. 2016;132:104-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klistorner SA, Barnett MH, Wasserthal J, et al. Differentiating axonal loss and demyelination in chronic MS lesions: a novel approach using single streamline diffusivity analysis. PLoS One. 2021;16(1):e0244766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang Y, Sun P, Wang Q, et al. Differentiation and quantification of inflammation, demyelination and axon injury or loss in multiple sclerosis. Brain. 2015;138(pt 5):1223-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]


