Abstract
Comprehensive care includes the spiritual and the bio-psycho-social person. The aim of this study is to explain how people with diabetes mellitus manage holistic treatment. Search for multi-database papers: Ovid, CINAHL, and PubMed. PICOT-based keyword description is P: any diabetes population, I: holistic care, C: any comparison, O: blood sugar, T: whenever. The English article, journal quest, full-text article available, and published article were criteria for inclusion in this study. In the quest journal, a strategic manner is performed using three keywords: holistic, diabetes mellitus, and blood sugar. We reviewed ten papers. The result showed that comprehensive care was explained in terms of technology, holistic care program, and holistic care relating to complementary alternative medicine. Discussion in this study is that holistic care services give significant results in the treatment of people with diabetes mellitus.
Keywords: A systematic review, complementary therapies, diabetes mellitus, disease management
Introduction
Diabetes mellitus (DM) is one of the priorities of four non-communicable diseases that are the target of follow-up by world leaders. DM is a hyperglycemia syndrome that can affect all organs of the body and cause various kinds of complaints. The prevalence of DM in the world in the last decade continues to increase.[1] In 2018, 463 million people experienced DM, which is projected in 2030 to reach 578 million, and in 2045 to 700 million.[2] Two-thirds of DM patients live in urban areas, and the majority are of working age. Estimates of 2045 deaths and DM care costs will be a major problem in social, financial, and health systems throughout the world.[2] The lifelong treatment process causes DM patients to experience fatigue, stress and increased life load. This will have an impact on the biological, psychological, social, and spiritual disorders of the patient Centers for Disease Control.[3] Complex conditions further increase blood glucose levels in patients. Blood glucose levels that are not controlled progressively can cause various complications. Complications that occur are heart disease, stroke, kidney failure, DM foot disorder, leg amputation, vision loss, and nerve damage.[1]
Comprehensive and holistic management is expected to be able to improve the condition of mind, emotions, and behavior of DM patients so that blood glucose is regulated, and the quality of life is improved.[1] Holistic nursing is an aspect of overall human experience and condition, both physically, emotionally, socially, culturally, and spiritually on the response and effects of the disease experienced by individuals, families, groups, communities, and populations.[4,5] Holistic philosophy intervention with traditional approaches is complementary therapy.[5] The reason patients use complementary therapy because it is harmonious; patients can get involved in making treatment decisions and improve their quality of life. 82% of patients also choose complementary therapy because they report the side effects of conventional medicine.[5] In 301 samples, the report, entitled the use of complementary treatment for DM patients, found that 81 (26.9%) patients had sought alternative therapies and 50 (16.6%) patients continued to use alternatives, as many as 43 (14.3%) patients used the product daily, and 24 (8%) patients used alternative medicines for up to 6 months. The result of glycated hemoglobin (HbA1C) decreased significantly.[6] Other studies explain the level of use of alternative and complementary therapies in 147 DM patients is 36.7%. The majority of their use in women found HbA1c, fasting blood glucose, serum post-prandial blood glucose levels decreased significantly in the group of complementary therapy use.[7] The purpose of this study is to explain the management of holistic care in people with diabetes mellitus.
Methods
Strategy searching for studies
The literature search use Ovid, CINAHL, and PubMed. Determination of keyword-based on PICOT framework, as follows P: any diabetes population, I: holistic care, C: any comparison, O: blood sugar, T: any time. We used MeSH as the keywords.
Study Selection
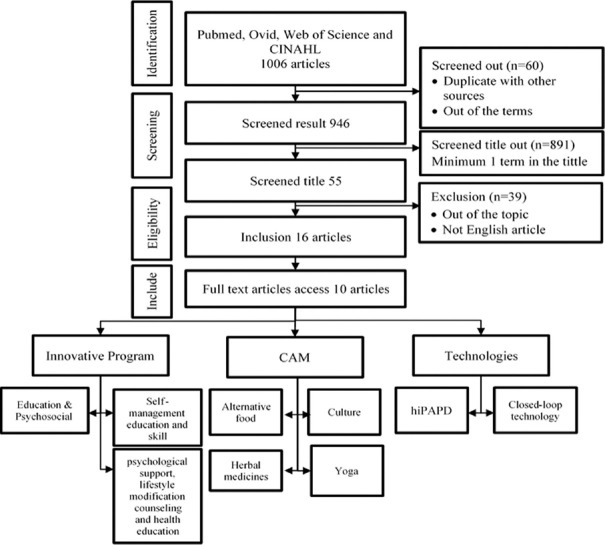
Figure 1 – Article selection Process.
Figure 1.
Article selection Process
Search strategies defined in the study selection process and Appendix 1. Ten articles fulfill the inclusion criteria in this study are English articles, search from the journal, article available in full text, and original article. Strategic ways in searching journals were done by using the keywords holistic, diabetes mellitus, and blood sugar.
Results
The result showed holistic care in the patient with diabetes mellitus refers to innovative care program three articles, holistic care using technology two articles, and holistic complementary and alternative medicine Five articles.
Table 1. Result of Study.
Table 1.
Result of Study
| Study | Type of DM | Design | Sample | Variables | Result |
|---|---|---|---|---|---|
| Likitmaskul, Sahakitrungruang[10] | T1DM | Quasi-experiment | 85 | self-monitoring of blood glucose (SMBG), HbA1C, blood sugar, eating disorders | Education and skills regarding diabetes self - management improved glycemic control. The program increases patient, family, and health - care worker interaction and communication. |
| Bott, Bott[8] | T1DM | Quasi-experiment | 76 | HbA1C, blood sugar, eating disorders, knowledge, motivation, competence regarding diet, the adaptation of insulin dosage | Treatment performance was significantly associated with baseline HbA1c, motivation stability, blood glucose level self - monitoring, perception management, and subsequent out-patient care improvements. |
| Chalermsri, Paisansudhi[9] | T2DM | Retrospective chart analysis | 757 | demographic data, glycemic control, screening for diabetic complications, and health maintenance. | The present study showed that the quality of treatment clinic at the medical OPD had greater efficacy than usual care, which is screening, glycemic control, and diabetic complications prevention. |
| Vargas-Lombardo, Jipsion[12] | T1DM T2DM |
A transversal analytical study | 107 | Patient acceptance’ | All the participants in the project demonstrated this with the acceptance of the hiPAPD model. The model provides services in remote and marginal areas that promote education, health, self-care, and social integration. |
| Young, Thabit[11] | T1DM | Case study | 3 | Live’s experiences during used closed-loop technology for 1 month | The first man experiences “changing lives, getting a better version of myself.” Use this tool and feel safe and comfortable. Participants explained to 32-year-old women that this tool improves work performance, flexibility, and “the greatest power that I have ever had.” He explained to men 30 years old that this tool puts a burden on the mind. All participants reported technological barriers and challenges such as portability of the system, frequent alarms, and poor connectivity of the devices. |
| Sachdeva, Khalique[14] | T2DM | Qualitative study | 25 | Cultural determinants in diabetes care | Diabetes care requires better results from cultural factors. Prevention and care programs, diabetes providers are expected to provide treatments that are consistent with the culture of the patient, and this is also correlated with local eating habits. |
| Popoola[13] | T2DM | Qualitative study: ethnography study | 35 | Holistic experiences | Their belief gives them the spiritual strength to handle diabetes because they all find a way of living a holistic life. |
| Chawla, Thakur[15] | TIDM T2DM |
Literature review | Herbal drug | The lack of awareness causes diabetes, which suddenly increases the risk of ketoacidosis and diabetic coma. If not handled properly, it will lead to complicated chronic diabetes. By using a holistic approach to herbal medicine, the multi-organ dysfunction syndrome which emerges from this metabolic disorder can be reduced/postponed. Further studies are needed to ensure the development of a useful framework for the standardization of herbal medicines, accompanied by recommendations for regulatory standards for future research efforts. | |
| Baldi, Choudhary[16] | TIDM T2DM |
Literature review | Nutraceuticals as therapeutic agents | Herbal treatments that have the best clinical evidence include American ginseng, C. indica, A. vera, T. foenum-graecum, and Opuntia (Nopal). The α-lipoic acid, vitamins C and E, and magnesium are nutraceutical agents to improve insulin sensitivity and glycemic control. | |
| Kutty and Raju[17] | T2DM | Commentary | Yoga, blood glucose | Research by Kyizom, Singh, Singh, Tandon, and Kumar (2010), got the result that the beneficial effects of yoga therapy in conjunction with conventional medical treatment. Blood glucose is effectively controlled in conjunction with yoga therapy when traditional treatment is done. |
T1DM: Type 1 Diabetes Mellitus; T2DM: Type 2 Diabetes Mellitus; QoL: Quality of Life; HbA1C / A1c: Glycemic Control; OPD: Out Patient Department; hiPAPD: Holistic, Interactive and Persuasive Model to Facilitate Self-care of the diabetic Patients
Innovation holistic care program
There were three studies with an innovative program. Bott, Bott[8] integrated education, experience, and psychosocial program; Chalermsri, Paisansudhi[9] provided a holistic approach consisting of psychological support, lifestyle modification counseling and health education in the clinic; and Likitmaskul, Sahakitrungruang[10] implemented self-management education and skill.
Bott, Bott[8] developed an Interactive Care and Training System for Experienced Patients (TTPEP). A total of 76 patients of diabetes type 1 got psychosocial modules, had been trained in specialist diabetes centers, and had already undergone increased insulin therapy. The system was able to increase glycemic control due to a significant reduction in the incidence of severe hypoglycemia. Mean HbA1c values remained unchanged; however, several patients strengthened the harmony between healthy HbA1c and low risk of severe hypoglycemia. Also, the system was able to reduce the number of sick-leave days and days of hospitalization, although the difference for the latter was not statistically significant. The more controlled glycemic control has been linked to improved self - efficacy beliefs, less external control feeling, and enhanced interaction with the care practitioners. Nonetheless, during the follow - up time, patient coping strategies, and perceived social support did not change. Whether the average 8% HbA1c following program participation is a disappointing result will lead to ambivalent interpretations. At follow-up, patients attained a mean HbA1c level of about 7.5% in earlier basic care and teaching intervention studies. Such trials, however, included patients with shorter duration of diabetes (2-9 years), and patients who were not primarily affected by late diabetic complications. In contrast, the present sample had an average duration of 13 years with diabetes, with at least incipient late symptoms at baseline 59%. It should be noted that patients who have participated in this plan represent a group of somewhat difficult patients, as they have already invested in structured treatment and treatment programs but have not met their treatment goals.
Chalermsri, Paisansudhi[9] research showed a significant improvement in glycemic control in patients prior to enrollment in the Siriraj Continuity of Care Clinic (CC Clinic) and Internal Medicine Regular Outpatient Department (OPD). The result of this study showed that the amount of diabetic patients in the target HbA1c reported in the CC clinic is less than 7% higher than the group OPD. The percentage in the OPD group is 24.3%, and the CC clinic group is 32.1%. The CC clinic focuses on the holistic care management of patients with chronic diseases. CC Clinic provides a holistic approach consisting of psychological support, lifestyle modification counseling, and health education. Our data show the overall benefits of glycemic control registration with CC clinics, diabetes complications screening rates, malignancy screening, and other health - care aspects. The authors suggest that our findings can at least partially be explained by the continuity of care, the educational aspect of the CC clinical program, and the higher amount of time spent with each patient in the CC clinic.
Likitmaskul, Sahakitrungruang[10] revealed self-management education for diabetes, namely DSME, and skills for the patient and family have a significant impact on their DSME skills and controls of glycemic. DSME and skills program started by trained all of health care teams. All patients who initially used the analog insulin regimen were replaced with blood glucose self-monitoring, called SMBG, with four times per day for free. Two groups of three-day diabetes were formed to provide patients with diabetes, families, and groups to learn basic DSME in the first year. Four groups of two-day diabetes were created in four geographical regions of Thailand in the 2nd and 3rd years to provide awareness and satisfaction with diabetes. Participants in this studied were 85 patients type 1 Diabetes and 25 hospitals with 31 healthcare squads. End of the session, the proportion of HbA1C patients <7.5 percent increased from 18.3 percent to 24.5 percent. HbA1C patients rose from 23.9 percent to 30.6 percent from 7.5 to 8.5 percent. Severe hypoglycemia status decreased, SMBG measurement frequency increased by an average of 2.87-3.48 times/day. Eating disorders dropped from 35% at the beginning of 20% to 11% -5%. The care teams had more self - confidence in supplying patients and families with support and touch. Health care support encourages regular contact and interaction with patients, families, and providers in health care in order to facilitate better management results.
Holistic care based on technology
Technology is essential due to era 4.0. Based on the two articles, technology can minimize risk, maximize benefit, effective and efficient for users, and also help poor conditions. The study of Young, Thabit[11] showed closed-loop technology has a significant impact by experience to patients with type 1 Diabetes. Vargas-Lombardo, Jipsion,[12] also give substantial effects related to technology with patient diabetes with lowly economic status.
Young, Thabit[11] examined the holistic impact of closed-loop technology on the home environment. Closed-loop technology is a control system that regulates electronic devices automatically that regulate process variables to the desired state or situation. In this study, three case studies constructed to explore the impact, benefits, and challenges faced by adults at home for one month. The first man, 33 years old, to experience like “changing lives”. Its system gives users a sense of security and trust so that they feel like “a better version of themselves”. Major problems such as hypoglycemia at night were perceived as decreased to none. Feeling safe and comfortable using this tool, study participants felt they were missing something when it ended using this tool. This experience was in line with other participants who did not experience nighttime hypoglycemia and improved sleep quality, which had an impact on improving diabetes control to provide better peace of mind. For 32-year-old women, participants explained that this tool enhances work performance and flexibility. She described his experience in using this tool as “the best control I have ever had,” even though she needed to adapt to it. For 30-year-old men, these participants had difficulty using “very annoying” tools. He explained that this tool puts a burden on the mind. All of the participants reported technical barriers and challenges such as system portability, repeated alarms, and weak device connectivity.
Vargas-Lombardo, Jipsion[12] found in his work that there was clear evidence in the HiPAPD model experiments. HiPAPD is an information technology that helps to reduce adverse health conditions in diabetic patients. The HiPAPD model provides diabetes health training, regular health evaluations, continuous self – care, and social inclusion of thousands of people who suffer from diabetes. HiPAPD serves poor people who stay in areas far from primary health centers, rendering access to essential health services impossible for them.
Complementary and Alternative Medicine (CAM)
Holistic care using complementary and alternative therapies started a long time ago. Study of Popoola[13] and Sachdeva, Khalique[14] got patients with diabetes used alternative food to control their blood sugar. They used herbs or local food to control their blood sugar. The other studies said researcher should develop herbal medicine to reduce diabetes complication[15,16]
Popoola,[13] in this study, the spiritual experience and encouragement of their loved ones have become life 's hope. The holistic balance is their way of looking at their problems, and their coping strategies enable them to live with this disease for years. They actively participate in activities outside the home, go to church, socialize, to find work. Economic drive and fear of losing limbs or vision often make Africans (Americans and Nigerians) focus on holistic health, especially spirituality. The participants explain the way to believe in faith and hope in God to survive. In addition, participants used simple daily CAM therapy to address their needs. They know the types and amounts of foods that raising or reducing blood sugar, understand the needs and changes of their own body, and use simple common sense. They know the benefits of workout and losing weight are alternatives treatments that have a significant impact. They understand the time to use traditional healers or herbal approaches that useful with diseases that would get a better life.
Chawla, Thakur[15] mentions that lack of awareness causes diabetes that suddenly raises the risk of ketoacidosis and diabetic coma. If this is not handled correctly, it will lead to complicated chronic diabetes. This multi-organ dysfunction syndrome that arises through this metabolic disorder can be reduced/postponed by using a holistic approach to herbal medicine. More studies are needed to ensure the development of a practical framework for the standardization of herbal drugs, accompanied by recommendations for regulatory standards for future research efforts.
In line with the previous study, Baldi, Choudhary[16] recommended the use of herbal medicines in diabetes therapy. The use of herbal medicine aims to overcome conventional therapy which can result in secondary failure and side effects such as hypoglycemia, liver problems, lactic acidosis, digestive system disorders, diarrhea, hematological disorders, and others. Ayurvedic treatment system recommends several polyherbal formulations with anti-diabetic potential. A large number of plants/plant parts have been investigated for the anti-diabetes potential to date. But the problem associated with polyherbal formulations is the lack of scientific evidence concerning their pharmacological effects and possible actions, difficulties to standardize and control the quality according to Food and Drug Association regulations. Many studies have reported that more than a thousand different botanicals and nutraceuticals have anti-diabetic activity. Fifty-eight studies were conducted in individuals with diabetes, 88% of trials evaluating single botany, and 67% of trials evaluating each vitamin or mineral supplement reported a statistically significant treatment effect. Side effects are only mild and mild such as gastrointestinal irritation and nausea. Some nutraceuticals and herbs are considered complementary therapy approaches diabetes type 2. Herbal treatments with the most persuasive evidence of clinical effects include American ginseng, C. indica, A. vera, T. foenum-graecum, and Opuntia (Nopal). Nutraceutical agents to increase insulin sensitivity and glycemic control are α-lipoic acid, vitamins C and E, and magnesium.
Kutty and Raju[17] revealed a study conducted by Kyizom, Singh[18] reported the beneficial effects of yoga therapy when included together with conventional medical treatment. Blood glucose is effectively controlled when traditional medicine is carried out along with yoga therapy. Other studies also show stable blood sugar in type 2 diabetes in response to yoga therapy. Kyizom, Singh[18] have shown that the practice of yoga for 45 days with conventional medicine effectively improves neurocognitive function. This study has several limitations. There is no correlation between cognitive improvement with stress level and education level. Age of patients with a history of the disease 2–10 years in the range of 35–60. A yoga regimen is carried out for at least six days a week under supervision to get better results. Yoga practice creates an internal atmosphere that is conducive from cellular to system level. This will help to effectively manage stress and anxiety in addition to the role of positive regulation in other systems. Maybe through combination therapy, we can effectively control diabetes, in addition, improve cognitive function and improve the overall quality of life.
Sachdeva, Khalique[14] got the result from their studies that researchers have to think about the cultural factor. Diabetes care requires cultural factors to provide better results. Prevention and care services, diabetes providers are expected to provide interventions that are in line with the patient's culture. Patients' perception is also related to local eating habits. The way to eat or international diet cannot be applied in all regions unless it has a similar family structure in the Euro-American context. The choice of the menu should be made more creative in adjusting to the culture of each region. Biomedical practitioners are expected to work hard to provide guidance related to understand and treat diabetes when there is a public health program for diabetes. Cultural features, such as values, beliefs, structures, behaviors, and family patterns, may be used as a culturally appropriate treatment plan for diabetics. It aims to provide culturally appropriate interventions so that a range of innovative care models for diabetics is effective with multi-disciplinary teams. Culture-specific approaches in accordance with local contexts and needs seem to have a considerable impact on diabetes care. A concept like that still needs to be tested and evaluated, however.
Discussion
Holistic nursing care incorporates the mind, body, and spirit of the patient in a community that fosters a therapeutic nurse/patient relationship, resulting in incompleteness, harmony, and healing. Holistic approach in medicine is patient-led and patient-focused in order to offer individualized care while caring for the patient as a whole rather than in fragmented pieces.[19] Modern science, like nursing and medicine, has been one of the most showing that soul and spirit are important to health. As these advances continue, it is not just our patients who will benefit, but healthcare worker as well.[20] This study founded from basic holistic care (mind, body, and spirit) to holistic care combine with the technology.
Bott, Bott[8] integrated education, experience, and psychosocial program; Chalermsri, Paisansudhi[9] provided a holistic approach consisting of psychological support, lifestyle modification counseling and health education in the clinic; and Likitmaskul, Sahakitrungruang[10] implemented self-management education and skill. Those study showed the results HbA1c controlled, low risk hypoglycemia, and glycemic controlled. Self-management start from the patients and for the patients, it gives meaningful experience to the patients that would give a positive impact to controlled the diabetes.[21,22] Those also give positive impact to the healthcare teams that had more self-confidence in supplying patients and families with support and touch. Health care support encourages regular contact and interaction with patients, families, and providers in health care in order to facilitate better management results.
Nowadays, the era of technology 4.0 gives a lot of impact to healthcare. The holistic care approach, not only focus on the mind body spirit but also social, economic, cultural, and whole part human needs including technology. Technology can minimize risk, maximize benefit, effective, and efficient for users, and also help poor conditions. The study of Young, Thabit[11] showed closed-loop technology has a significant impact by experience to patients with type 1 Diabetes. Vargas-Lombardo, Jipsion,[12] also give substantial effects related to technology with patient diabetes with lowly economic status. Those articles showed technological is an integral part of caring competence and robotics is an unavoidable aspect of technological development. While these developments offer noted efficiencies and cost savings opportunities, a greater understanding of the effects of patient engagement, dignified, and empathetic treatment, is vital to ensuring that the application and use of technology aligns with nursing principles and vision for the future.[23]
Holistic care approach integrating with complementary and alternative medicine (CAM) have been used in west country.[24] Kutty and Raju[17] revealed a study conducted by Kyizom, Singh[18] reported the beneficial effects of yoga therapy when combined with conventional medical treatment is effectively controlled of glycemic. Sachdeva, Khalique[14] have a notions about the cultural factor that will provide better results. Cultural features, including values, beliefs, structures, behaviors, and family patterns, it could provide culturally appropriate interventions with local contexts and needs seem to have a considerable impact on diabetes care.
A new idea of diabetic care is use herbal as a medicine. Study of Popoola[13] and Sachdeva, Khalique[14] got patients with diabetes used alternative food to control their blood sugar. They used herbs or local food to control their blood sugar. The other studied said researcher should develop herbal medicine to reduce diabetes complication.[15,16] Those study need empirical study because there is no empirical study have been tried related to herbal medicine for patients with diabetes mellitus.
Conclusions
Management patient with diabetes mellitus by holistic care approach includes psychosocial, psychological support, lifestyle changes, health education, herbal food and medicine, culture, yoga, and technology. Indonesia has a diverse culture. Each island or region has different habits in consuming herbs as food or medicine. In addition, the healthy outlook held by each area is also different. The differences in each region can be a barrier to the treatment of diabetes. That is highly considered for further study by the authors.
However, to improve the effectiveness of diabetes treatment programs that are needed to be integrated with culture, health, and technology. Culture could be a barrier. On the other hand, it must be utilized as supportive therapy for diabetes. Technology helps reach the poor to get the proper care. In addition, technology provides a broader range. In this case, areas that lack health facilities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge Chulalongkorn University for the Second Century Fund (C2F).
References
- 1.WHO. Noncommunicable diseases country profiles 2018. 2018:9241514620. [Google Scholar]
- 2.Cho N, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 3.Prevention CfDC. Diabetes Prevention Recognition Program standards and operating procedures. 2018 [Google Scholar]
- 4.Frisch NC, Rabinowitsch D. What's in a definition. Holistic nursing, integrative health care, and integrative nursing: Report of an integrated literature review? J Holist Nurs. 2019;37:260–72. doi: 10.1177/0898010119860685. [DOI] [PubMed] [Google Scholar]
- 5.Lindquist R, Tracy MF, Snyder M. Complementary and Alternative Therapies in Nursing. Springer Publishing Company. 2018 [Google Scholar]
- 6.Ilhan M, Demir B, Yüksel S, Çataklı SA, Yıldız RS, Karaman O, et al. The use of complementary medicine in patients with diabetes. North Clin Istanb. 2016;3:34–8. doi: 10.14744/nci.2016.63825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yıldırım Dİ, Marakoğlu K. Complementary and alternative medicine use amongst Turkish type 2 diabetic patients: A cross-sectional study. Complement Ther Med. 2018;41:41–6. doi: 10.1016/j.ctim.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Bott U, Bott S, Hemmann D, Berger M. Evaluation of a holistic treatment and teaching programme for patients with Type 1 diabetes who failed to achieve their therapeutic goals under intensified insulin therapy. Diabet Med. 2000;17:635–43. doi: 10.1046/j.1464-5491.2000.00345.x. [DOI] [PubMed] [Google Scholar]
- 9.Chalermsri C, Paisansudhi S, Kantachuvesiri P, Pramyothin P, Washirasaksiri C, Srivanichakorn W, et al. The effectiveness of holistic diabetic management between Siriraj Continuity of Care clinic and medical out-patient department. J Med Assoc Thai. 2014;97:197–205. [PubMed] [Google Scholar]
- 10.Likitmaskul S, Sahakitrungruang T, Numbenjapon N, Sriussadaporn P, Nitiyanant W. Outcomes of holistic care for patients with type 1 diabetes (T1D) by multidisciplinary teams in Thailand. Diabetes Res Clin Pract. 2016;120:S123–S. [Google Scholar]
- 11.Young AJ, Thabit H, Heller SR, Evans ML, Amiel SA, Hovorka R, et al. Holistic impact of closed-loop technology on people with type 1 diabetes. J Diabetes Sci Technol. 2015;9:932–3. doi: 10.1177/1932296815580162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vargas-Lombardo M, Jipsion A, Vejarano R, Camargo I, Álvarez H, Mora EV, et al. Technologies to better serve the millions of diabetic patients: A holistic, interactive and persuasive ICT model to facilitate self care, in extremely poor rural zones of central America. Journal of Medical Systems. 2012;36:595–600. doi: 10.1007/s10916-010-9523-y. [DOI] [PubMed] [Google Scholar]
- 13.Popoola MM. Living with diabetes: The holistic experiences of Nigerians and African Americans. Holist Nurs Pract. 2005;19:10–6. doi: 10.1097/00004650-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Sachdeva S, Khalique N, Ansari MA, Khan Z, Mishra SK, Sharma G, et al. Cultural determinants: Addressing Journal of Social Health and Diabetes. 2015;3:33–8. [Google Scholar]
- 15.Chawla R, Thakur P, Chowdhry A, Jaiswal S, Sharma A, Goel R, et al. Evidence based herbal drug standardization approach in coping with challenges of holistic management of diabetes: A dreadful lifestyle disorder of 21st century. J Diabetes Metab Disord. 2013;12:35. doi: 10.1186/2251-6581-12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baldi A, Choudhary N, Kumar S. Nutraceuticals as therapeutic agents for holistic treatment of diabetes. 2013;7:278–87. [Google Scholar]
- 17.Kutty BM, Raju TR. New vistas in treating diabetes - Insight into a holistic approach. Indian J Med Res. 2010;131:606–7. [PubMed] [Google Scholar]
- 18.Kyizom T, Singh S, Singh K, Tandon O, Kumar R. Effect of pranayama & yoga-asana on cognitive brain functions in type 2 diabetes-P3 event related evoked potential (ERP) Indian J Med Res. 2010;131:636–40. [PubMed] [Google Scholar]
- 19.McEvoy L, Duffy A. Holistic practice – A concept analysis. Nurse Educ Pract. 2008;8:412–9. doi: 10.1016/j.nepr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Dossey BM, Dossey L. Body-mind-spirit: Attending to holistic care. Am J Nurs. 1998;98:35–8. [PubMed] [Google Scholar]
- 21.Jasemi M, Valizadeh L, Zamanzadeh V, Keogh B. A Concept analysis of holistic care by hybrid model. Indian J Palliat Care. 2017;23:71–80. doi: 10.4103/0973-1075.197960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Modarresi M, Gholami S, Habibi P, Ghadiri-Anari A. Relationship between self care management with glycemic control in type 2 diabetic patients. Int J Prev Med. 2020;11:127. doi: 10.4103/ijpvm.IJPVM_207_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Archibald MM, Barnard A. Futurism in nursing: Technology, robotics and the fundamentals of care. J Clin Nurs. 2018;27:2473–80. doi: 10.1111/jocn.14081. [DOI] [PubMed] [Google Scholar]
- 24.Sharp D, Lorenc A, Little P, Mercer SW, Hollinghurst S, Feder G, et al. Complementary medicine and the NHS: Experiences of integration with UK primary care. Eur J Integr Med. 2018;24:8–16. [Google Scholar]