Abstract
Background:
The basis of prevention of non-communicable diseases is the identification of primary risk factors and the prevention and control of these factors. The purpose is to prevent the spread of the disease and to control it as much as possible. If population growth continues at this rate, by 2030, 52 million people will die from these diseases each year. The aim of this study was to evaluate the challenges of preventing non-communicable diseases.
Methods:
The present study was a systematic review that conducted in July 2020 and the articles related to prevention of non-communicable diseases on databases of web of science, PubMed, Scopus, science direct, Ovid, Pro Quest and Google Scholar. Strategy for searching and selecting the articles was PRISMA Guidelines.
Results:
Challenges of non-communicable disease prevention, in 4 main codes, including infrastructure, economic, demographic and management and 12 sub-codes that include, lack of preventive infrastructure, restrictions on access to medicine, restrictions on primary health care, restrictions on access to Technology, disease-oriented disease, unsustainable financial resources, failure to implement poverty reduction projects, increase in aging population, migration, rapid and unplanned urban planning, hasty planning and lack of internal and external coordination were classified.
Conclusions:
To reduce non-communicable diseases, strengthen global capacities, reduce risk factors for NCDs and place social determinants by creating health-promoting environments, strengthen health systems to implement prevention and control of NCDs, and place determinants Social can play an effective role through people-centered primary health care.
Keywords: Iran, NCD, non-communicable disease, prevention
Introduction
Non-communicable diseases (NCDs), also known as chronic diseases, are not transmitted from person to person. These diseases persist for a long time and are generally slow to progress.[1] Non-communicable diseases are known as lifestyle diseases because many of them are preventable diseases. The main causes of non-communicable diseases include smoking, alcohol consumption, poor nutrition (excessive use of sugar, salt, saturated fats and trans fatty acids) and physical inactivity. Non-communicable diseases kill 38 million people annually, accounting for 68% of all deaths worldwide.[2]
Primary NCDs (CVD, cancers, CRD, and diabetes) are among the top 10 causes of death.[3] In many countries, the prevalence of non-communicable and chronic diseases has been on the rise and is expected to continue.[4] One of the reasons for this increase can be the increase in life expectancy in many countries, which results in an increase in the number of older people and, as a result, the possibility of contracting various non-communicable and chronic diseases.[3,5]
About three-quarters of non-communicable disease deaths (28 million) occur in low- and middle-income countries. Sixteen million deaths from non-communicable diseases occur before the age of 70, with 82% of these premature deaths coming from low- and middle-income countries. The leading cause of death from non-communicable diseases is cardiovascular disease, which causes 17.5 million deaths a year. It is followed by cancer with 8.2 million deaths, respiratory disease with 4 million deaths, and diabetes with 1.5 million deaths.[6,7]
These four groups of diseases account for 82% of all non-communicable disease deaths. Non-communicable diseases are both specific goals of the SDG (reducing premature mortality from non-communicable diseases to one-third) and are part of several other health goals.[8]
These four groups of diseases account for 82% of all non-communicable disease deaths. Non-communicable diseases are both specific goals of the SDG (reducing premature mortality from non-communicable diseases to one-third) and are part of several other health goals. More than 76% of the total disease burden in Iran is allocated to non-communicable diseases. The basis of prevention of non-communicable diseases is to identify the primary and major risk factors and to prevent and control these factors.[3]
The purpose is to prevent the spread of the disease and to control it as much as possible. If population growth continues at the same rate, non-communicable diseases will cause 7 out of 10 deaths by 2020, and by 2030, 52 million people will die from these diseases each year. This worrying statistic has prompted international organizations, including the World Health Organization, the World Bank's Human Development Network, to raise the issue of non-communicable disease prevention and control as an increasingly important issue.[9] Given the importance of the above and the growing trend of non-communicable diseases in Iran, it seems necessary to study the challenges and achievements of the country to control these diseases.
Methods
The present study was a systematize review of publications relating to non-communicable disease. systematize review attempt to include elements of systematic review process while stopping short of systematic review.[10] The study was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and Critical Appraisal Skills Program (CASP) for articles and AACODS (Authority, Accuracy, Coverage, Objectivity, Date, Significance) for grey literature (provides five criteria for judging the quality of grey information).[11,12]
Information sources
This study was conducted during July 2020 review English and Persian language published papers in the field of non-communicable disease. In addition, as well to the published articles, reports, programs, and the documents that considered in unpublished cases have been included in the study, which are called gray studies. For this purpose, we studied database including ISI web of science, PubMed, Scopus, science direct, Ovid, ProQuest.
Search Protocol
The search strategies include: (#1. (NCD OR non-communicable disease)), #2. (prevent* OR control OR manage)), (#3. (health system OR healthcare system)), (#4. (#1 AND #2)), (#5. (#1 AND #2 AND #3)) All synonyms of the keywords were searched using MESH strategies. Filters: Publication date from 2010/11/30 to 2020/05/30.
Selection of articles and document
Independent reviewers (MH and EM) screened abstracts and titles for eligibility. When the reviewers felt that the abstract or title was potentially useful, full copies of the article were retrieved and considered for eligibility. If discrepancies occurred between reviewers, the reasons were identified and a final decision was made based on the third reviewer (AJ) agreement. Two authors (MH and EM) assessed the methodological quality and grade of evidence of included studies with the CASP tools. The CASP tools use a systematic approach to appraise different study designs from the following domains: study validity, methodology quality, presentation of results, and external validity and all the items from the checklists were judged with yes (low risk of bias, score 1), no (high risk of bias), or cannot tell (unclear or unknown risk of bias, score 0). Total scores were used to grade the methodological quality of each study assessed.[11]
Eligibility criteria
We searched papers that (1) mentioned non-communicable disease and based on it the evaluation of CASP criteria and ACCODS criteria were corrected, 2) mentioned one of the challenges of preventing non-communicable diseases, 3) papers in English or Persian language, 4) papers that have a perfect structure, 5) Internal article that has been printed in scientific and research journals, and 6) published paper in the year 2010 and after.
Study quality assessment
Quality assessment of the included studies was done using the (CASP) and (ACCODS) tools. The score of quantitative studies ranged from two to nine. The majority of quantitative studies did not provide any ethical statement, study design, sampling, and reflexivity related to the research process.
Results
Database search
The initial electronic database search of the literature resulted in a total of documents. In the next step, duplicate documents were eliminated and the number decreased to 1066 articles. Using systematic screening, the titles were reviewed to find those related to non-communicable disease and 621 documents were selected. In the next step, abstracts of the documents were studied and 220 documents were selected to be fully reviewed. In this step, 210 documents were excluded. After that, all of the selected documents were completely read and based on the inclusion criteria, only 11 documents were selected. Figure 1 shows the strategy for searching and selecting the documents.
Figure 1.
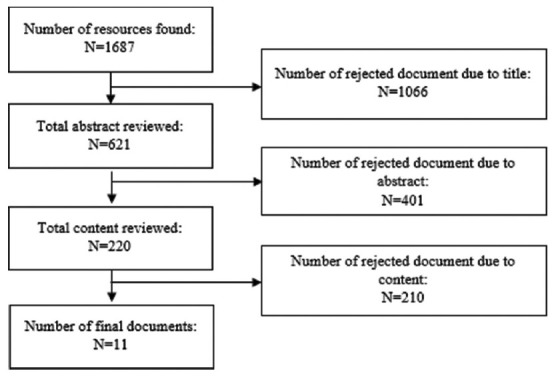
Search strategy
Main finding
According to the findings, the challenges of preventing non-communicable diseases were classified into 4 main codes, including infrastructure, economic, demographic, and managerial. Each of the mentioned codes had sub-codes that are listed in Table 1.
Table 1.
NCDs prevention challenges
| Theme | Sub-theme |
|---|---|
| Infrastructure challenges | Lack of preventive infrastructure |
| Restrictions on access to medicine | |
| Restrictions on the implementation of primary health care | |
| Restrictions on access to technology | |
| Economic challenges | Profitability of the disease |
| Instability of financial resources | |
| Failure to implement poverty reduction plans | |
| Demographic challenges | Increasing elderly population |
| Migration | |
| Managerial challenges | Fast urban planning without a plan |
| Haste in planning | |
| Lack of internal and external coordination |
Infrastructure challenges
According to studies, while political attention to NCDs has increased, in many countries there is still insufficient attention to this issue. For example, according to a 2015 World Health Organization survey of countries' capacity, only 45% of countries reported having an NCD policy.[13] In cases where there are infrastructure policies or programs, there are often still serious budget problems.[7] Infrastructure problems can be classified into categories including lack of preventive infrastructure, restrictions on access to medicine, restrictions on primary health care, and restrictions on access to technology.[3,7,14]
Economic challenges
Non-communicable diseases cause 35 million deaths worldwide each year and are a major obstacle to the development of countries.[2] These diseases have severely affected the poor and vulnerable people of the society and are dragging them into the abyss of poverty.[1] Dealing with these diseases is possible by controlling their risk factors and using the experiences of other countries and the expert advice of international organizations. On the other hand, many products that increase NCDs are profitable for companies.[6] According to studies, economic challenges can be divided into profit-oriented, financial instability and unsuccessful implementation of poverty reduction plans.[15,16,17]
Demographic challenges
Migration has a great impact on the pattern of life.[7] The villager breathes in the polluted air, eats fast food and his health is endangered. On the other hand, the change of the age pyramid has changed to the middle-aged population.[4] In fact, the population aging index in the country has increased from 14.8% to 39.5%. That is, for every 100 people under the age of 15 in the country, about 40 elderly people live in Iran. 73.3% of the elderly live in urban areas and 26.7% in rural areas.[7] According to studies, demographic challenges can be classified into the categories of aging population and migration.[6,7]
Management challenges
Improperly or poorly managed urban planning carries many risks that have an impact on NCD incidence and mortality.[18] For example, it brings a significant increase in air pollution and sedentary living. In 2012, approximately 75% of the world's population was exposed to certain particles at concentrations higher than those specified in World Health Organization guidelines. In many high-income countries, such as Europe and North America, air pollution has declined in recent decades due to extensive efforts to reduce greenhouse gases and particulate matter.[19] Management challenges can be classified according to studies in the categories of rapid and unplanned urban planning, haste in planning and lack of coordination within and outside the sector.[3,4,7]
Discussion
Despite the reduction in NCD-related deaths, current plans will not be sufficient to meet the NCD mortality target (a 25% reduction in early deaths from the four major NCDs by 2050). But it could be an important step in achieving the SDG goal of reducing NCD-related deaths by a third by 2030.[9] In this study, the challenges of prevention in non-communicable diseases were classified into 4 categories: infrastructure, economic, demographic and management. In the field of infrastructure, lack of preventive infrastructure, restrictions on access to medicine, restrictions on the implementation of primary health care, restrictions on access to technology are the main challenges in this area.
In many countries, especially those with limited resources, funding, administration, labor, health information, medical products, and services are needed to meet NCD epidemic demand.[20] In a study conducted by Galambos, the findings show that primary health care services are not sufficient for NCDs and need to be strengthened, and that models should be adopted for the management of chronic diseases.[16]
While political attention to NCDs has increased, insufficient attention continues to be paid in many countries. For example, according to a 2015 World Health Organization survey of country capacity, only 54% of countries reported having a national operational policy with a budget allocated to implement the NCD.[1] The Atun study found that only 37% of countries had NCD policies or programs that covered four major NCDs and four major risk factors for behavior. In cases where there are policies or programs, there are still serious budget problems. Inadequate promotion or prevention effects are reflected in an increase in body mass index.
In the economic sphere, the profitability of the disease, the instability of financial resources and the failure to implement poverty reduction projects were mentioned as the most important challenges.[21]
Many products that increase NCDs are profitable for companies. In a study by Moodie, the findings show that the globalization of marketing and commerce offers many opportunities for companies to expand products that lead to tobacco use, alcohol abuse, consumption of high-fat foods, especially saturated fats. Trans, sugar and salt, and sedentary lifestyles are given, and often benefit from poor regulatory frameworks in many low-income countries.[2]
In a study conducted by Etemad, the findings showed that the instability of financial resources and economic sanctions are among the challenges of implementing the package of essential non-communicable disease interventions.[7]
In the field of population, increasing aging population and migration were the most important challenges. In a study by Mohan, the findings showed that the incidence of NCD and mortality increased with age, and in both cases the absolute values of the elderly and the percentage of the elderly population were increasing in all areas.[22] A study by Beaglehole found that 58 percent of NCD deaths in 2012 occurred in people over the age of 70, and in the years that followed, an increase in the elderly population led to an increase in NCD-related illnesses and deaths. It will also increase the pressure on health systems.[19]
In the Etemad study, the findings show that changing the age pyramid to aging and migration is one of the challenges of implementing the package of essential non-communicable disease interventions.[7]
In the field of management, rapid and unplanned urban planning, haste in planning and lack of coordination within and outside the sector were mentioned as the most important challenges. In a study by Donkelaar, the findings showed that poorly or poorly managed urban planning has many risks that have an impact on NCD incidence and mortality. For example, it brings a significant increase in air pollution and sedentary living.[17]
Also in the Kontis study, the findings showed that, for non-communicable disease interventions in the various organizations to be involved, there should be a representative who communicates with all organizations and informs all organizations.[23]
Conclusions
NCDs are often characterized by interconnected cause-and-effect chains. So identifying a specific factor that leads to its reduction is very difficult and challenging. Health promotion and disease prevention are important for NCDs that are associated with a number of risk factors that provide an excellent opportunity for intervention at the demographic level. Many of the risk factors for NCDs are related to the air we breathe, the food and drink we eat and drink, and how much we move our bodies. But in general to reduce non-communicable diseases, strengthen global capacities, reduce risk factors for NCDs and place social determinants by creating health-promoting environments, strengthen health systems to implement prevention and control of NCDs, and Giving social determinants through people-centered primary health care can play an effective role.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Organization WH. Assessing national capacity for the prevention and control of noncommunicable diseases: Report of the 2019 global survey. 2020 [Google Scholar]
- 2.Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381:670–9. doi: 10.1016/S0140-6736(12)62089-3. [DOI] [PubMed] [Google Scholar]
- 3.Organization WH. Noncommunicable diseases progress monitor 2015. 2015 [Google Scholar]
- 4.Nugent R, Bertram MY, Jan S, Niessen LW, Sassi F, Jamison DT, et al. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. 2018;391:2029–35. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 5.Juma PA, Mohamed SF, Mwagomba BLM, Ndinda C, Mapa-Tassou C, Oluwasanu M, et al. Non-communicable disease prevention policy process in five African countries authors. BMC Public Health. 2018;18:961. doi: 10.1186/s12889-018-5825-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob Health. 2017;5:e277–89. doi: 10.1016/S2214-109X(17)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Etemad K, Heidari A, Panahi M, Lotfi M, Fallah F, Sadeghi S. A challenges in implementing package of essential noncommunicable diseases interventions in Iran's Healthcare System. J Health Res Community. 2016;2:32–43. [Google Scholar]
- 8.Di Cesare M, Khang Y-H, Asaria P, Blakely T, Cowan MJ, Farzadfar F, et al. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–97. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- 9.Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, et al. NCD countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. 2018;392:1072–88. doi: 10.1016/S0140-6736(18)31992-5. [DOI] [PubMed] [Google Scholar]
- 10.Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 11.CASP U. Critical Appraisal Skills Programme (CASP) Check lists. 2017 [Google Scholar]
- 12.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Inter Med. 2015;162):777–84. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 13.Salinas A, Kones R. Barriers to global action plan for the prevention and control of noncommunicable diseases: Proposal modifications to the voluntary targets. J Prev Med. 2018;3:1–5. [Google Scholar]
- 14.Organization WH. Assessing national capacity for the prevention and control of noncommunicable diseases: Report of the 2017 global survey. 2018 [Google Scholar]
- 15.Organization WH. Global Health Estimates: Deaths, disability-adjusted life year (DALYs), years of life lost (YLL) and years lost due to disability (YLD) by cause, age, and sex: 2000–2012. 2016 [Google Scholar]
- 16.Galambos L, Sturchio JL. Addressing the gaps in global policy and research for non-communicable diseases. Baltimore: Johns Hopkins University; 2012. [Google Scholar]
- 17.Van Donkelaar A, Martin RV, Brauer M, Boys BL. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environm Health Perspect. 2015;123:135–43. doi: 10.1289/ehp.1408646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D. Non-communicable disease syndemics: Poverty, depression, and diabetes among low-income populations. Lancet. 2017;389:951–63. doi: 10.1016/S0140-6736(17)30402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet. 2008;372:940–9. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 20.Organization WH. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 66th Session of the Unites Nations General Assembly. New York: WHO; 2011. [Google Scholar]
- 21.Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, et al. Improving responsiveness of health systems to non-communicable diseases. Lancet. 2013;381:690–7. doi: 10.1016/S0140-6736(13)60063-X. [DOI] [PubMed] [Google Scholar]
- 22.Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast asian and african regions: Need for effective strategies for prevention and control in primary health care settings? Int J Hypertens. 2013;2013:409083. doi: 10.1155/2013/409083. doi: 10.1155/2013/409083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, et al. Contribution of six risk factors to achieving the 25×25 non-communicable disease mortality reduction target: A modelling study. Lancet. 2014;384:427–37. doi: 10.1016/S0140-6736(14)60616-4. [DOI] [PubMed] [Google Scholar]


