Abstract
Background
In 2010, the American Heart Association introduced a new concept of ideal cardiovascular health (CVH) defined as the simultaneous presence of 7 favorable CVH metrics (smoking, diet, physical activity, body mass index, blood pressure, total cholesterol, and fasting blood glucose). The objective of this study was to conduct a systematic literature review and meta-analysis of studies examining the prevalence of ideal CVH, and each of the ideal CVH metrics as well as the relationship between socio-demographic determinants and ideal CVH.
Methods
A comprehensive literature search was conducted in Medline and Scopus databases for studies published between 1 January 2010 and 30 June 2020. A total of 50 studies including 2,148,470 participants were analyzed. Associations were estimated using DerSimonian-Laird random-effect models. Heterogeneity was investigated through subgroup analyses, Q-test, and I2 statistics.
Results
This study showed a low prevalence of ideal CVH defining as 6 and 7 ideal metrics (3.3%). Among seven ideal CVH metrics, smoking was the best metric (71%), while the poorest CVH metric was a healthy diet (5.8%). Gender was a statistically significant moderator of ideal smoking (81% in females and 60% in males) and ideal blood pressure (42% in females and 30% in males). Females and young adults had better CVH status compared to males and older adults. Also, more educated and better-off individuals had a greater number of ideal CVH metrics.
Conclusions
To the best of our knowledge, this is the first systematic review on the relationship between participants’ socioeconomic status and ideal CVH. The results suggest that the prevalence of ideal CVH and most metrics was unsatisfactory. In order to achieve the improvement of the CVH metrics and the overall ideal CVH, nationwide prevention efforts at the population and individual levels are urgently needed.
Introduction
In 2010, the American Heart Association (AHA) introduced a new concept of ideal cardiovascular health (CVH) as part of its efforts to improve the CVH of all Americans while reducing deaths from cardiovascular disease (CVD) [1]. This concept is defined as the simultaneous presence of 7 favorable CVH metrics or “Life’s Simple 7”: 4 health behaviors (smoking, diet, physical activity, and body mass index) and 3 health factors (blood pressure, total cholesterol, and fasting blood glucose) in the absence of CVD.
Since that time, many population-based studies have examined the prevalence of AHA’s ideal CVH, ideal CVH metrics, and their distribution by socio-demographic characteristics [2–10]. To examine associations between ideal CVH metrics and CVD events and non-CVD endpoints, several prospective cohort studies [2, 11–14], systematic review and meta-analyses [15–18] were conducted. Their results showed that ideal CVH metrics are inversely associated with the risk of CVD events [2, 13, 14, 16, 17], and both all-cause and CVD-related mortality [11–14, 16–18]. Studies suggested that ideal CVH status and even modest improvements in CVH metrics are beneficial for substantial reductions in the risk of CVD events [17] and CVD-related mortality [17, 18].
Therefore, evaluating associations between socio-demographic characteristics and ideal CVH metrics would be a valuable resource for communities to develop public health and clinical interventions and policies to improve ideal CVH and consequently prevent CVD events. However, studies that synthesize data on the prevalence of 7 ideal CVH metrics, ideal CVH, and their distribution by socio-demographic characteristics are lacking. To the best of our knowledge, there is only one systematic review [15] and one meta-analysis [19] on this topic. Accordingly, we conducted a comprehensive systematic review and meta-analysis with the aim to synthesize data on the prevalence of ideal CVH, and each of the ideal CVH metrics. What is new in our review compared to the previous reviews, is the updating of the population’s ideal CVH due to the significant number of recently published studies, and the fact that we examined the relationship between social determinants such as education and income and ideal CVH.
Method
Search strategy for identification of studies
We performed a comprehensive electronic search of published studies from their inception to June 2020 by searching Medline (via PubMed) and Scopus databases with the following terms: "cardiovascular health", "Life’s simple 7", and "ideal" in English. The search string used for the review in PubMed was: ((cardiovascular health[Title]) OR (Life’s simple 7[Title])) AND (ideal) AND ("2010"[Date—Publication]: "2020/06/30"[Date—Publication]) AND (English[Language]), while for Scopus: (TITLE ("cardiovascular health") OR TITLE ("Life’s simple 7")) AND ALL (ideal) AND LANGUAGE (English) AND PUBYEAR > 2009.
To identify any articles missed through the database search, we manually reviewed the reference lists of the selected studies.
Data collection and analysis
Selection of studies
As a first step of the study selection process, two members of the research team (MD and JJ) screened independently the titles and abstracts of the identified articles and excluded duplicates and articles not relevant to the topic. The process between two researchers was compared, and any uncertainties were discussed and solved by the third researcher (SJ). If any key information was missing, we contacted the study authors to provide additional information. If this was not possible or ineffective, the study was rejected.
We documented the study selection process in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart [20].
Eligibility criteria
Articles were eligible for inclusion if written in English, peer-reviewed, and published between January 1, 2010 and June 30, 2020. To be included in the review process, studies had to assess the prevalence of ideal CVH metrics (smoking, physical activity, healthy diet, BMI, blood pressure, total cholesterol, and fasting blood glucose) as defined by the AHA [1]. The AHA criteria for the definition of ideal, intermediate, and poor CVH metrics are presented in S1 Table. Furthermore, studies were included if they enrolled participants 18 years or older who were free of CVD. Review articles, meta-analyses, commentaries and discussions, editorials, letters to editors (except when all relevant data was available), conference papers, books or book chapters were excluded.
Data extraction and quality assessment
Two review authors (MD and JJ) independently extracted and entered data from all included studies into the Characteristics of included studies table. A third review author (SJ) checked the extracted data. The information included the following: first author and year of publication; country where the study was conducted; study design; study date; number of participants enrolled; percentage of male; age/range and mean years (SD) of participants; and main outcome measures. The main outcome measures of this review are prevalence (%) and 95% confidence intervals (CI) of ideal CVH metrics and ideal CVH, ideal health behaviors and ideal health factors, odds ratio (OR) and 95% CI, prevalence ratio (PR) and 95% CI or relative predicted score differences (RPS) and 95% CI of having ideal CVH.
For studies with more than one publication, we considered the first publication as the primary reference.
The quality of each study was evaluated using a standardized 14-item National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (NIH-QAT) [21]. Each study was rated as good (most methodological criteria met, low risk of bias), fair (some criteria met, low risk of bias), or poor (few criteria met, high risk of bias).
Since almost half of the NIH-QAT items are not applicable to the studies included in our analysis, we additionally used the risk of bias tool specifically designed for prevalence studies [22]. It consists of 10 items addressing four domains of bias plus a summary risk of bias assessment. The response options for each item were either yes or no. Studies with yes answered for 0 to 3, 4 to 6, and 7 to 10 items were regarded as having overall high, moderate and low risk of bias, respectively.
Two researchers (JJ and SJ) independently appraised each study meeting inclusion criteria and subsequently, disagreements were discussed and solved by consensus on the final rating of the quality for each study. The reliability of the quality assessment between researchers was calculated using the kappa (k) statistic.
Our study followed all PRISMA guidelines, as applicable, in the design, data collection, analysis and reporting of this systematic review and meta-analysis (S2 Table).
Statistical analysis
The meta-analysis was carried out using the proportion or the double arcsine transformed proportion (in the case of proportions between 0 and 0.2) as the outcome measure. Both a fixed and random-effects model were fitted to the data and the amount of heterogeneity (i.e., τ2) was estimated using the DerSimonian-Laird estimator [23]. In addition, the Q-test for heterogeneity [24] and the I2 statistic [25] were reported. Studentized residuals and Cook’s distances were used to examine whether studies may be outliers and/or influential in the context of the model [26]. In subgroup analysis, for all ideal CVH metrics, and the presence of 5, 6, and 7 ideal CVH metrics and for ideal CVH, proportions were stratified into two groups based on gender (female and male). For ideal CVH proportions were stratified by age into old, middle, and young groups. Mixed-effects models were used to test whether the proportions across these subgroups vary significantly from each other, and the Q (QM) statistic was used to check whether the two or three groups have significantly different outcomes [25]. The analysis was carried out using R Programming Language and Environment for Statistical Computing (version 4.0.2) [27] and the metafor package (version 2.4.0) [28].
This review was registered in the PROSPERO (CRD42020152644) on 28 April 2020.
Results
Description of studies
Results of the search
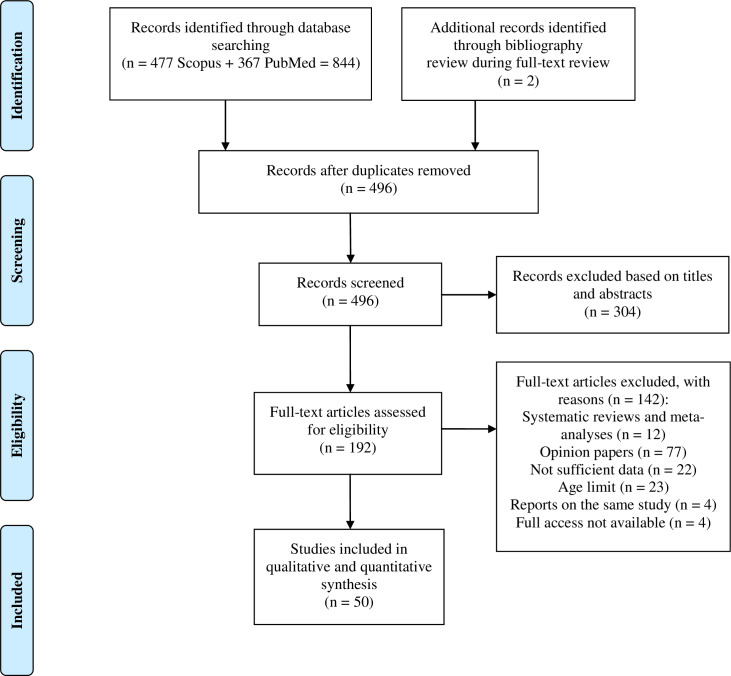
The initial database search yielded 844 records, and two records were obtained from other sources (reference lists of articles identified through database searching). We screened the titles and abstracts of a total of 496 non-duplicate records and excluded 304 articles not relevant to the topic. A total of 192 full-text articles were reviewed for eligibility, and 50 studies that met our search criteria were included in the analysis. Detailed results of our search are presented in Fig 1 as a PRISMA flowchart.
Fig 1. Study flow diagram.
A PRISMA flow diagram that details the inclusion and exclusion of studies considered for this systematic review. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of included studies
All 50 studies [2, 4, 8–10, 29–73] included in the review were primarily cross-sectional or cross-sectional nested in a longitudinal study (Table 1). Of all included studies, 17 originated from the USA, 11 from China (one of them from Hong Kong), three from Brazil, two from France, one from Latin America (Argentina, Chile, Uruguay), and one study from each of the following countries: Canada, Australia, Nepal, Korea, Iran, Peru, Venezuela, Ecuador, India, Ghana, Spain, Finland, BH (Republic of Srpska), Serbia, Czech Republic, and Poland (Table 1).
Table 1. Characteristics of included studies.
| First author, year | Country | Study design | Study date | No of population (% male) | Age range; mean age (SD) | Main outcome measures |
|---|---|---|---|---|---|---|
| Bambs CE et al. 2011 [29] | USA | Cross-sectional study | Heart SCORE study 2003 | 1933 (34%) | 45–75; 59 (7.5) | Prevalence of ideal CVH, CVH metrics, ideal health behaviors, and health factors |
| Benziger CP et al. 2018 [30] | Peru | Cross-sectional study | CHRONICAS 2010 | 3058 (48.7%) | ≥35; 55.6 (12.7) | Prevalence of ideal CVH and CVH metrics, PRs of ideal CVH for education and Wealth index |
| Bi Y et al. 2015 [31] | China | Cross-sectional study | 2010 | 96121 (45.7%) | ≥20 | Prevalence of ideal CVH and CVH metrics, ideal health behaviors, and health factors |
| Bundy JD et al. 2020 [32] | USA | Cross-sectional nested in cohort study | 1985–2016 | 30447 (39.4%) | 55.0 (13.9) | Prevalence of ideal CVH and CVH metrics |
| Chang Y et al. 2016 [33] | China | Cross-sectional study | 2012–2013 | 11113 (46.2%) | ≥35; 53.8 (10.6) | Prevalence of ideal CVH, CVH metrics, ideal health behaviors, and health factors, ORs of ideal CVH for education and family income |
| Chung JWY et al. 2018 [34] | Hong Kong, China | Cross-sectional study | 2014–2016 | 626 (9.2%) | >20 | Prevalence of ideal CVH and CVH metrics |
| De Moraes ACF et al. 2019 [10] | USA | Cross-sectional study | 2000–2002 | 6792 (47.2%) | 45–84; 62.2 | Prevalence of ideal CVH and CVH metrics |
| Del Brutto OH et al. 2013 [35] | Ecuador | Cross-sectional study | Atahualpa 2012; | 616 (40.6%) | 40–99; 59.0 (13.0) | Prevalence of ideal CVH and CVH metrics |
| USA | NOMAS 1993–2001 | 1617 (36.7%) | 40–107; 66.0 (9.0) | |||
| Djousse L et al. 2015 [36] | USA | Cross-sectional nested in cohort study | JHS 2000–2004 (baseline visit) | 5301 (36.5%) | 55.3 (12.7) | Prevalence of ideal CVH metrics, ideal health behaviors, and health factors, and number of ideal CVH metrics |
| Fan C et al. 2020 [37] | USA | Cross-sectional nested in cohort study | APAC 2012 | 3475 (56.5%) | 45–75 | Prevalence of ideal CVH and CVH metrics |
| Fang J et al. 2019 [38] | USA | Cross-sectional study | NHANES 2011–2016 | 6764 (46.5%) | ≥20 | Prevalence of ideal CVH and CVH metrics |
| 5278 NHW (49.4) | 49.9 (0.5) | |||||
| 1486 NHAA (47.6) | 44.5 (0.8) | |||||
| Folsom AR et al. 2011 [2] | USA | Cross-sectional nested in cohort study | ARIC 1987–1989 (baseline visit) | 12744 (43.9%) | 45–64; 54.0 | Prevalence of ideal CVH and CVH metrics |
| Foraker RE et al. 2019 [39] | USA | Cross-sectional nested in cohort study | JHS 2000–2004 (baseline examination) | 3667 (35.6%) | 35–84; 55.1 | Prevalence of ideal CVH metrics; EEs of ideal CVH score for income and education |
| Gao B et al, 2020 [40] | China | Cross-sectional nested in cohort study | National survey 2007–2010 | 45984 (50.4%) | ≥18; 49.2 (15.1) | Prevalence of 5 ideal CVH metrics |
| Gaye B et al. 2020 [41] | France | Cross-sectional study | 2007–2011 | 68318 (57.7%) | 43.3 (13.6) | Prevalence of 6 ideal CVH metrics |
| Ghimire U et al. 2020 [42] | Nepal | Cross-sectional study | 2013 | 3238 (31.5%) | 15–69 | Prevalence of ideal CVH and CVH metrics, ideal CVH factors and health behaviors, number of ideal CVH metrics, OR of ideal CVH for education |
| Gonzalez HM et al. 2016 [43] | USA | Cross-sectional nested in cohort study | HCHS/SOL 2008–2011 (baseline) | 15825 (47.8%) | 18–74 | Prevalence of ideal CVH, CVH metrics and number of ideal CVH metrics |
| Gonzalez-Rivas JP et al. 2019 [44] | Venezuela | Cross-sectional study | 2014–2017 | 2992 (47%) | ≥20; 41.4 (15.8) | Prevalence of ideal CVH metrics and number of ideal CVH metrics |
| Graciani A et al. 2013 [4] | Spain | Cross-sectional study | ENRICA 2008–2010 | 11408 (49%) | ≥18 | Prevalence of ideal CVH metrics, ideal health factors and behaviours, number of ideal CVH metrics, OR of ideal CVH for education |
| Gupta B et al. 2017 [45] | India | Cross-sectional study | 2006–2010 | 6198 (55.3%) | 20–75 | Prevalence of ideal CVH and CVH metrics |
| Harrison S et al. 2019 [46] | Canada | Cross-sectional study | 2015–2017 | 777 (49.8%) | 18–65; 41.9 (0.1) | Prevalence of ideal CVH and ideal LS7 metrics and distribution of the LS7 score (0–7) |
| Isiozor NM et al. 2020 [47] | Finland | Cross-sectional nested in cohort study | KIHD 1984 (baseline) | 2577 (100%) | 42–60; 53.1 (5.1) | Prevalence of ideal CVH, ideal CVH metrics, ideal health behaviors, and health factors |
| Jankovic J et al. 2019 [48] | Serbia | Cross-sectional study | NHS 2013 | 11746 (46%) | ≥20; 51.0 (17.4) | Prevalence of ideal CVH metrics, ideal health factors and health behaviors, ORs of ideal CVH for education and Wealth index |
| Jankovic S et al. 2014 [49] | Republic of Srpska, BH | Cross-sectional study | 2010 NHS | 4020 (46%) | ≥18; 50.2 (17.6) | Prevalence of ideal CVH and CVH metrics, ideal health factors and health behaviors, OR of ideal CVH for education |
| Kim JI et al. 2013 [50] | USA | Cross-sectional study | HONU project 2009 and 2011 | 4754 (41.7%) | ≥18; 52.1 (16.0) | Prevalence of ideal CVH metrics and number of ideal CVH metrics |
| Kim JY et al. 2013 [51] | Korea | Cross-sectional nested in cohort study | Seoul Male Cohort Study 1993 | 12538 (100%) | 40–59; 50.0 (5.2) | Prevalence of ideal CVH and CVH metrics |
| Kulshreshtha A et al. 2013 [52] | USA | Cross-sectional nested in cohort study | REGARDS study 2003–2007 (baseline) | 22914 (42.0%) | ≥45.0 (65.0) | Prevalence of ideal CVH and CVH metrics |
| Lawrence EM et al. 2018 [53] | USA | Cross-sectional study | NHANES 2005–2010 | 689 | 24–34 | Prevalence of ideal CVH and CVH metrics, OR of ideal CVH for education |
| Add Health 2007–2008 | 11200 (51%) | |||||
| Liu Y et al. 2014 [54] | China | Cross-sectional nested in cohort study | Kailuan Sudy 2006–2007 (baseline) | 95429 (79.7%) | ≥18–98; 51.5 (12.5) | Prevalence of ideal CVH and CVH metrics |
| Lu Y et al. 2015 [8] | China | Cross-sectional study | 2013 | 11996 (64.7%) | ≥19; 46.8 (13.0) | Prevalence of ideal CVH and CVH metrics |
| Machado LBM et al. 2018 [55] | Brasil | Cross-sectional study | 2008–2010 | 13356 (45.3%) | 35–74 51.7 (8.9) | Prevalence of ideal CVH and CVH metrics, rPSD of ideal CVH for education and income |
| Matozinhos FP et al. 2017 [56] | Brasil | Cross-sectional study | 2012 | 41134 (48.4%) | ≥18; 41 (0.15) | Prevalence of ideal 6 CVH metrics, PR of ideal CVH for education |
| Medina-Inojosa JR et al. 2020 [57] | Czech Republic | Cross-sectional nested in cohort study | 2014 | 2074 (47.0%) | 25–64; 47.3 (11.3) | Prevalence of ideal CVH and CVH metrics |
| Moghaddam MM et al. 2014 [58] | Iran | Cross-sectional nested in cohort study | TLGS 2009–2011 | 4865 (41.2%) | ≥20; 41.4 (13.6) | Prevalence of ideal CVH and CVH metrics |
| Nowicki GJ et al. 2018 [59] | Poland | Cross-sectional study | 2015–2016 | 3901 (41.1%) | 35–64; 52.1 (8.2) | Prevalence of ideal CVH and number of ideal CVH metrics |
| Ogunmoroti O et al. 2017 [60] | USA | Cross-sectional study | BHSF 2014 | 9056 (26.0%) | 43.0 (12.0) | Prevalence of ideal CVH, ideal CVH metrics and number of ideal CVH metrics, OR of ideal CVH for education. |
| Ommerborn MJ et al. 2016 [61] | USA | Cross-sectional nested in cohort study | JHS 2000–2004 (baseline) | 4702 | 35–84 | Prevalence of ideal CVH and numbers of ideal CVH metrics |
| Patel N et al. 2019 [62] | USA | Cross-sectional study | NHANES 2007–2010 | 4369 (48.6%) | ≥20; 45.0 | Prevalence of ideal CVH and number of ideal CVH metrics |
| Peng Y and Wang Z 2018 [63] | Australia | Cross-sectional study | AHS 2011–2012 | 7499 (44.4%) | ≥18 | Prevalence of ideal CVH and ideal health factors and health behaviors |
| Pilkerton CS et al. 2015 [64] | USA | Cross-sectional nested in cohort study | BRFSS 2011 | 341659 (47.9) | ≥18; 51.1 (0.1) | Prevalence of ideal CVH and CVH metrics |
| Ren J et al. 2016 [65] | China | Cross-sectional study | SMASH 2011–2015 | 15350 (50.05%) | 18–69; 41.4 | Prevalence of ideal CVH and CVH metrics, ORs of ideal CVH for income and education |
| Seron P et al. 2018 [66] | Latin Americaa | Cross-sectional nested in cohort study | CESCAS I 2011–2012 | 5458 (41,1%) | 35–74; 54.8 (10.8) | Prevalence of ideal CVH and CVH metrics |
| Shay et al. 2012 [67] | USA | Cross-sectional study | NHANES 2003–2008 | 14515 (50.7%) | ≥20 | Prevalence of ideal CVH and CVH metrics |
| Simon M et al. 2017 [9] | France | Cross-sectional study | Paris Prospective Study 3 2008–2012 | 9012 (61.5%) | 50–75; 59.5 (6.3) | Prevalence of ideal CVH and CVH metrics, OR of ideal CVH for education |
| van Nieuwenhuizen B et al. 2018 [68] | Ghanab | Cross-sectional study | Multi-centre RODAM study 2012–2015 | 3510 (38.0%) | 18–70; 47.0 (12.0) | Prevalence of ideal CVH and CVH metrics |
| Velasquez-Melendez G et al. 2015 [69] | Brasil | Cross-sectional study | NHS 2013 | 34362 (48.7%) | ≥18; 43.8 (0.2) | Prevalence of ideal CVH metrics |
| Wu HY et al. 2013 [70] | China | Cross-sectional study | CHED 2010 | 1012418 (45.0%) | 20–65; 42.7 (6.4) | Prevalence of ideal CVH and CVH metrics |
| Wu S et al. 2012 [71] | China | Cross-sectional nested in cohort study | Kailuan Study 2006–2007 | 91698 (79.4%) | 18–98; 51.5 (12.4) | Prevalence of ideal CVH and CVH metrics |
| Zeng Q et al. 2013 [72] | China | Cross-sectional study | DREHM 2009–2012 | 9962 (55.8%) | 20–83; 47.1 | Prevalence of ideal CVH and CVH metrics |
| Zhao Y et al. 2016 [73] | China | Cross-sectional study | 2010 | 2693 (33.4%) | 20–80; 51.4 (11.5) | Prevalence of ideal CVH and CVH metrics, ORs of ideal CVH for education and income |
Add Health = National Longitudinal Study of Adolescent to Adult Health; AHS = Australian Health Survey; APAC = Asymptomatic Polyvascular Abnormalities Community study; ARIC = Atherosclerosis Risk in Communities; BHSF = Baptist Health South Florida Employee Study; BRFSS = Behavioral Risk Factor Surveillance System; CHED = Chinese Health Examination Database; CHRONICAS = Center of Excellence in Chronic Diseases; CVH = Cardiovascular health; DREHM = Disease Risk Evaluation and Health Management study; ENRICA = Study on Nutrition and Cardio-vascular Risk; Heart SCORE = Heart Strategies Concentrating on Risk Evaluation study; HCHS/SOL = Hispanic Community Health Study/Study of Latinos; HONU = Heart of New Ulm Screening Participants; JHS = Jackson Heart Study; EE = Effect estimate; KIHD = Kuopio Ischemic Heart Disease study; LS7 = Life’s Simple 7; NHAA = non-Hispanic Asian Americans; NHANES = National Health and Nutrition Examination Survey; NHS = National Health Survey; NHW = non-Hispanic white; NOMAS = Northern Manhattan Study; OR = Odds ratio; PR = Prevalence ratio; REGARDS = The Reasons for Geographic And Racial Differences in Stroke; rPSD = Relative predicted score differences; RODAM = Research on Obesity and Diabetes among African Migrants; SMASH = The Shandong province and the Chinese Ministry of Health collaborative Action on Salt reduction and Hypertension; TLGS = Tehran Lipid and Glucose Study; Wealth index = an aggregation of assets and household facilities.
aArgentina, Chile, and Uruguay
bGhanian population in Amsterdam, London and Berlin.
Studies included a total of 2,148,470 participants. Sаmple sizes ranged from 616 to 1,012,418. Two studies [47, 51] included only males. Participants, were adults 18 years and older with an age range from 18 to 107 years. The survey years of the studies included in our review ranged from 1984 to 2017 (33 year period).
Prevalence of ideal CVH metrics and ideal CVH
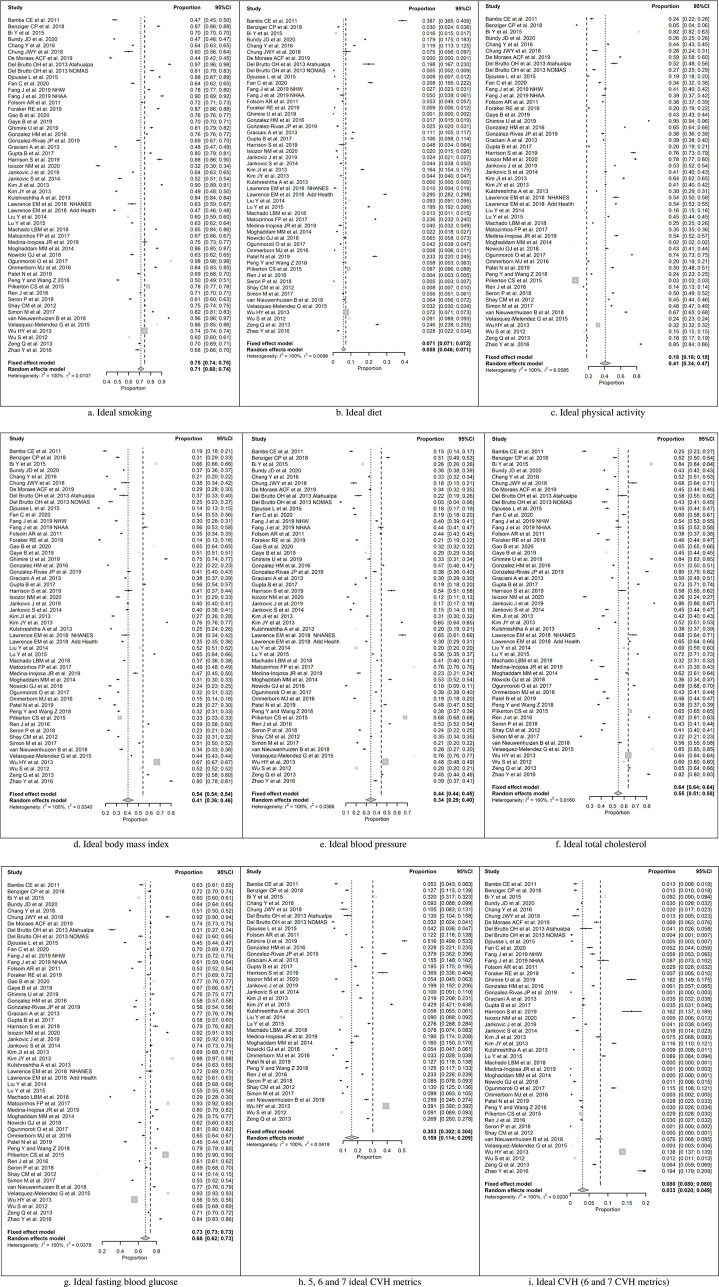
Meta-analyses of each of seven ideal CVH metrics are presented in Fig 2.
Fig 2. Forest plots showing proportions of ideal cardiovascular health metrics and ideal cardiovascular health.
Ideal smoking (A), Ideal diet (B), Ideal physical activity (C), Ideal body mass index (D), Ideal blood pressure (E), Ideal total cholesterol (F), Ideal fasting blood glucose (G), 5, 6 and 7 ideal CVH metrics (H), Ideal CVH (6 and 7 CVH metrics) (I). CVH, Cardiovascular health; CI, confidence interval.
The observed proportions for ideal smoking (Fig 2A) ranged from 0.32 to 0.98, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.68 to 0.74). For ideal diet (Fig 2B) the observed double arcsine transformed proportions ranged from 0.003 to 0.569, and the estimated pooled double arcsine transformed proportion based on the random-effects model was (95% CI: 0.194 to 0.274). The back-transformed summary proportion was 0.058 (95% CI: 0.040 to 0.080). The observed proportions for ideal physical activity (Fig 2C) ranged from 0.02 to 0.95, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.34 to 0.47). For ideal body mass index (Fig 2D), the observed proportions ranged from 0.14 to 0.80, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.36 to 0.45). The observed proportions for ideal blood pressure (Fig 2E) ranged from 0.05 to 0.76, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.29 to 0.39). For ideal total cholesterol (Fig 2F), the observed proportions ranged from 0.22 to 0.86, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.51 to 0.59). The observed proportions for ideal fasting blood glucose (Fig 2G) ranged from 0.14 to 0.97, and the estimated pooled proportion based on the random-effects model was (95% CI: 0.62 to 0.73).
In a meta-analysis of 37 studies, for the simultaneous presence of 5, 6, and 7 ideal CVH metrics (Fig 2H), the observed double arcsine transformed proportions ranged from 0.181 to 0.801, and the estimated pooled double arcsine transformed proportion based on the random-effects model was (95% CI: 0.360 to 0.471). The back-transformed summary proportion was 0.159 (95% CI: 0.124 to 0.197).
The prevalence of ideal CVH (defined here as achieving 6 and 7 ideal CVH metrics), intermediate CVH (defined as achieving 2 to 5 ideal CVH metrics), and poor CVH (defined as 0 to 1 ideal CVH metrics) in selected countries are presented in S1 Fig. The prevalence of ideal CVH was low in all observed countries and ranged from 0.5% in the USA Jackson Heart Study [36] to 15% in the Chinese Health Examination Database study [70]. As many as 15 out of the 21 studies conducted worldwide reported less than 5% prevalence of ideal CVH. Most participants had intermediate CVH with the prevalence ranging from 70% in the USA Heart SCORE study [29] to 93% in the Serbian Health Survey [48]. The prevalence of poor CVH ranged from 1% in the Korean Seoul Male Cohort Study [51] to 29% in the USA Heart SCORE study [29].
The prevalence of ideal health behaviors and the prevalence of ideal health factors from 10 studies with available data are presented in S2 Fig. The percentage of subjects who achieved the 4 ideal behaviors or lifestyles (smoking, diet, physical activity, and BMI) was lower than the percentage of those with the 4 ideal health or biological factors (blood pressure, total cholesterol, fasting blood glucose, and smoking) in all observed studies, except one [29]. As defined by the AHA, given the importance of abstinence from smoking and smoking cessation to health promotion, this metric appears in both health behaviors and health factors [1].
For the ideal CVH (6 and 7 CVH metrics) a total of 44 studies were included in the meta-analysis (Fig 2I), and the observed double arcsine transformed proportions ranged from 0.015 to 0.415. The estimated pooled double arcsine transformed proportion based on the random-effects model was (95% CI: 0.154 to 0.220). The back-transformed summary proportion was 0.033 (95% CI: 0.022 to 0.046).
For all ideal CVH metrics, as well as for the presence of 5 and more ideal CVH metrics and ideal CVH, the true outcomes (proportions) appear to be heterogeneous indicating the need for moderator (subgroup) analysis.
Prevalence of ideal CVH metrics and ideal CVH according to gender and age
Where data was available, participants were stratified by gender (female and male) and moderator analysis was performed for each of 7 ideal CVH metrics, for the presence of 5 and more ideal CVH metrics, and for ideal CVH (6 and 7 ideal CVH metrics) (Table 2). Gender was a statistically significant moderator of ideal smoking (proportion of 0.81 in females and 0.60 in males; QM = 22.12, p < 0.001), and ideal blood pressure (proportion of 0.42 in females and 0.30 in males; QM = 8.94, p = 0.003). Gender was also a statistically significant moderator of ideal CVH with the proportion of 0.06 in females and 0.03 in males (QM = 4.61, p = 0.032), and for the simultaneous presence of 5, 6 and 7 CVH metrics with the proportion of 0.21 in females and 0.13 in males (QM = 6.44, p = 0.011).
Table 2. Moderator (subgroup) analyses of ideal cardiovascular health metrics by gender.
| Ideal CVH metric | Gender | No. of studies | Heterogeneity | Meta-analysis | Test of moderators | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Population | P-valuea | I2 | Model | Proportion | 95% CI | P-value | QM | P-valueb | |||
| Smoking | F | 33 | 710,944 | <0.001 | 99.99% | Random | 0.814 | 0.746, 0.881 | <0.001 | 22.121 | <0.001 |
| M | 35 | 829,878 | <0.001 | 99.94% | Random | 0.601 | 0.543, 0.658 | <0.001 | |||
| Diet | F | 32 | 684,598 | <0.001 | 99.95% | Random | 0.069 | 0.043, 0.101 | <0.001 | 1.131 | 0.288 |
| M | 34 | 811,803 | <0.001 | 99.94% | Random | 0.050 | 0.031, 0.074 | <0.001 | |||
| Physical activity | F | 32 | 684,598 | <0.001 | 99.98% | Random | 0.382 | 0.294, 0.470 | <0.001 | 1.319 | 0.251 |
| M | 34 | 811,803 | <0.001 | 99.97% | Random | 0.451 | 0.374, 0.528 | <0.001 | |||
| Body mass index | F | 33 | 710,944 | <0.001 | 99.95% | Random | 0.465 | 0.401, 0.530 | <0.001 | 1.129 | 0.288 |
| M | 34 | 827,301 | <0.001 | 99.95% | Random | 0.417 | 0.357, 0.478 | <0.001 | |||
| Blood pressure | F | 33 | 710,944 | <0.001 | 99.93% | Random | 0.420 | 0.365, 0.474 | <0.001 | 8.944 | 0.003 |
| M | 35 | 829,878 | <0.001 | 99.96% | Random | 0.297 | 0.239, 0.356 | <0.001 | |||
| Total cholesterol | F | 32 | 689,719 | <0.001 | 99.96% | Random | 0.569 | 0.502, 0.636 | <0.001 | 0.054 | 0.817 |
| M | 34 | 809,969 | <0.001 | 99.95% | Random | 0.580 | 0.519, 0.640 | <0.001 | |||
| Fasting blood glucose | F | 33 | 710,944 | <0.001 | 99.92% | Random | 0.733 | 0.690, 0.776 | <0.001 | 1.910 | 0.167 |
| M | 35 | 829,878 | <0.001 | 99.96% | Random | 0.684 | 0.629, 0.739 | <0.001 | |||
| 5, 6, and 7 metrics | F | 27 | 648,071 | <0.001 | 99.95% | Random | 0.213 | 0.159, 0.272 | <0.001 | 6.442 | 0.011 |
| M | 29 | 837,000 | <0.001 | 99.93% | Random | 0.127 | 0.092, 0.166 | <0.001 | |||
| Ideal CVH (6 and 7) | F | 21 | 620,728 | <0.001 | 99.95% | Random | 0.055 | 0.032, 0.083 | <0.001 | 4.607 | 0.032 |
| M | 23 | 754,906 | <0.001 | 99.83% | Random | 0.026 | 0.015, 0.039 | <0.001 | |||
CVH = Cardiovascular health; F = Female; M = Male
aTest for heterogeneity (Q)
bTest of moderators (QM)
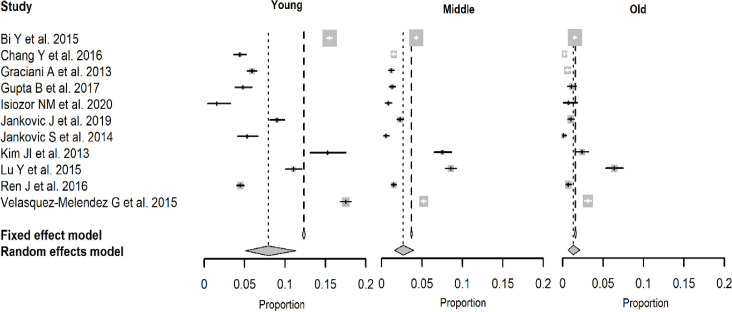
A total of 11 studies had available data and were included in the analysis of age and ideal CVH (6 and 7 ideal CVH metrics) (Fig 3). The back-transformed summary proportions were: 0.08 (95% CI: 0.05 to 0.11) for the young age group, 0.03 (95% CI: 0.01 to 0.04) for the middle age group, and 0.01 (95% CI: 0.01 to 0.02) for the older age group. Test of moderators revealed that the difference between the three subgroups is significant (QM = 24.24, DF = 2, p < 0.001). The better CVH was seen in younger and middle-aged adults compared to older participants.
Fig 3. Forest plots depicting proportions with their confidence intervals of ideal cardiovascular health by age group.
Ideal CVH according to socioeconomic characteristics
The results of 14 studies describing the association between socioeconomic variables (education, income, and Wealth index), and the prevalence of ideal CVH are presented in Table 3.
Table 3. Studies describing the association between socioeconomic variables and prevalence of ideal cardiovascular health.
| First author, year | Outcome | Adjustment for potential confounding | Measure of socioeconomic status (95% CI) |
|---|---|---|---|
| Benziger CP et al. 2018 [30] | Ideal CVH metrics (5–7) | Age, sex, site | Education PRa 0.96 (0.68, 1.35) |
| Wealth index PRa 0.75 (0.55, 1.01) | |||
| Wealth index PRb 0.73 (0.56, 0.95) | |||
| Chang Y et al. 2016 [33] | Ideal CVH metrics (5–7 vs. 0–4) | Age, sex, marital status | Education ORa 1.95 (1.70, 2.25) |
| Family income ORa 1.70 (1.30, 2.20) | |||
| Foraker RE et al. 2019 [39] | CVH score: sum of 7 ideal CVH metrics ranging from 0 (worst) to 14 (best) points | Age, sex, neighborhood income or education where appropriate | Individual income EEac 0.31 (0.24, 0.37) |
| Neighborhood income EEac 0.19 (0.09, 0.28) | |||
| Education (bachelor) EEac 0.67 (0.43, 0.91) | |||
| Education (graduate) EEac 0.93 (0.69, 1.16) | |||
| Ghimire U et al. 2019 [42] | Ideal CVH metrics (5–7) | Age, sex, marital status, residence, ethnicity | Education ORa 0.74 (0.44, 1.25) |
| Graciani A et al. 2013 [4] | Ideal CVH metrics (>6 vs. <1) | Age, sex, self-rated health, and use of health care system | Education ORa 2.60 (1.45, 4.64) |
| Jankovic J et al. 2019 [48] | Ideal CVH metrics (6–7 vs. 0–5) | Age, sex, type of settlement, marital status | Education ORa 3.57 (2.36, 5.40) |
| Wealth index ORa 1.43 (1.08, 1.88) | |||
| Wealth index ORb 1.22 (0.91, 1.63) | |||
| Jankovic S et al. 2014 [49] | Ideal CVH metrics (5–7 vs. 0–4) | Age, sex, type of settlement, marital status, employment | Education ORa 2.3 (1.5, 3.5) |
| Lawrence EM et al. 2018 [53] | CVH (ideal vs.poor) | Age, sex | Education ORa 4.98 (3.41, 7.28) |
| Machado LBM et al. 2018 [55] | CVH score: sum of 7 ideal CVH metrics ranging from 0 to 7 | Age, sex, race, educational, family income and study site effect | Education rPSDd −17.2 (−20.0, −14.2) |
| Age, sex, race, educational level, and study site effect | Family incomed rPSD − 4.4 (−7.2, −1.6) | ||
| Matozinhos FP et al. 2017 [56] | Ideal CVH metrics (5–6) | Education women PRd 0.28 (0.23, 0.33) | |
| Education men PRd 0.27 (0.21, 0.33) | |||
| Ogunmoroti O et al. 2017 [60] | Ideal CVH metrics (6–7) | Age, sex, ethnicity | Education ORa 0.29 (0.19, 0.44) |
| Ren J et al. 2016 [65] | Ideal CVH metrics (≥5 vs. ≤4) | Age, sex | Personal income + education ORa 1.85 (1.40,2.45) |
| Simon M et al. 2017 [9] | CVH (ideal vs. poor) | Education ORae 5.20 (4.07, 6.77) | |
| Zhao Y et al. 2016 [73] | Ideal CVH (7 ideal CVH metrics) | History of hypertension, diabetes, dyslipidemia, and CVD | Education ORf 1.33 (0.64, 2.74) |
| Family income ORf 0.93 (0.59, 1.48) |
CI = Confidence intervals; CVH = Cardiovascular health; EE = Effect estimate; PR = Prevalence ratio; rPSD = Relative predicted score differences; OR = Odds ratio; Wealth index = an aggregation of assets and household facilities.
ahighest compared to lowest
bmiddle compared to lowest
cper category increase
dlowest compared to highest
ewomen vs. men
fhighest vs. moderate.
Results from most studies showed that participants with the highest education had a greater number of ideal CVH metrics, i.e. better CVH in comparison with those with the lowest education [4, 9, 33, 39, 48, 49, 53, 56, 73]. In a study by Foraker et al. [39] individuals with a bachelor’s degree, had on average, a CVH score of 0.67 points higher compared with those with high school or less education. Similarly, persons with graduate/professional degrees had on average a CVH score of 0.93 points higher than their less-than-high educated school counterparts. Machado et al. [55] found that individuals with less than high school education had lower ideal CVH scores than college-educated individuals. In a study by Matozinhos et al. [56] lower levels of education were associated with a lower prevalence of ideal CVH, regardless of gender, compared to those with a higher level of education. In contrast, Ongunmoroti et al. [60] found that lower education was associated with better CVH, while Benziger et al. [30] and Zhao et al. [73] did not find any statistically significant association between education and ideal CVH (Table 3).
Only a few studies assessed the relationship between income and CVH. Foraker et al. [39] found that those with higher individual and neighborhood levels of income had higher CVH scores, i.e. better CVH. There was an average increase in CVH score of 0.31, and 0.19 points associated with each 1-category increase in individual income, and neighborhood income, respectively. Better results, considering the number of ideal CVH metrics were also achieved in persons with more family income living in Hong Kong [33]. Machado et al. [55] demonstrated that low (<1245 USD) family income was associated with lower ideal CVH scores compared to those with high (≥3320 USD) family income. In contrast, in a rural area of Northwest China, no associations were found between family income and ideal CVH [73] (Table 3).
In one study conducted in China, higher socioeconomic status (defined according to both personal income and years of education) was associated with an increasing prevalence of meeting 5 or more ideal CVH metrics in women but not in men [65]. Only two studies included in our review assessed the association between Wealth index (an aggregation of assets and household facilities) and ideal CVH. While Jankovic et al. [48] noted a statistically positive association between Wealth index and ideal CVH, Benziger et al. [30] found the opposite (Table 3).
Quality assessment
According to both applied quality assessment tools (NIH-QAT and tool specifically designed for prevalence studies), almost all included studies were regarded as having a low risk of bias (S3 and S4 Tables). Agreement on the quality assessment between the two reviewers was high.
Discussion
Our study is the second meta-analysis ever done that calculated the pooled prevalence estimates of the seven ideal CVH metrics and overall ideal CVH according to the AHA’s guideline, and the first systematic review that examined the association between socioeconomic status (SES) and ideal CVH. Since a considerable number of studies on the prevalence of ideal CVH have been published in the last few years our study provides up-to-date information that could be useful for policymakers, clinicians, researchers, communities, and other stakeholders to understand and implement the most effective approaches to improve CVH in populations.
This study showed a low prevalence of ideal CVH defined as 6 and 7 ideal metrics (3.3%) that is in line with a previous systematic review [15]. When a less strict definition of ideal CVH was applied (5 to 7 ideal metrics) about 16% of our participants had an overall ideal CVH like in recent meta-analysis [19]. In most countries poor CVH (0–1 ideal metrics) was more frequent than ideal CVH (6 and 7 ideal metrics), while intermediate CVH (2–5 ideal metrics) was the most prevalent. Except in one study [29], we also observed a lower prevalence of ideal health behaviors (ranged from 0.1% to 2%) compared with the prevalence of ideal health factors (ranged from 1.4% to 16.4%).
Among seven ideal CVH metrics, smoking was the best metric (71%), followed by fasting blood glucose (68%), total cholesterol (55%), physical activity (41%), BMI (41%), and blood pressure (34%), while the poorest CVH metric was healthy diet (5.8%).
The results of our meta-analyses are summary proportions of ideal CVH and ideal CVH metrics from studies conducted during different study periods, ranging from 1984 to 2017. We are aware that the CVH status has changed during the observed period and several cohort studies assessing trends in ideal CVH and CVH metrics documented that finding. Patel et al. [62] examined the trends in ideal CVH during economic recession (2007–2010) and subsequent economic recovery (2011–2016) among American adults and noted a decline in ideal CVH score that was primarily driven by the increased prevalence of obesity and poor fasting glucose. A Danish study [5], using data from six cross-sectional studies conducted in an adult population aged 30–64 years in Denmark from 1978 to 2006, reported an increasing trend in ideal CVH. Huffman et al. [74] analyzed CVH behavior and health factor changes from 1988 to 2008 and showed modest, further declines in tobacco consumption, high cholesterol, and high blood pressure, offset by increases in obesity and dysglycemia. The high proportions of people with favorable smoking status in this study (71%) could be a reflection of comprehensive tobacco control policies and a significant decrease of smoking worldwide [74]. The prevalence of ideal fasting blood glucose metric (68%) like in reviews by Younus et al. [15] and Peng et al. [19] was also high but trend results suggest its decline [62, 74]. This high optimal prevalence of fasting blood glucose may partly be explained by the slight improvement of physical activity and dietary pattern [74–76], which were found to be risk factors for elevated fasting blood glucose and diabetes [77]. In our review, 55% of participants had ideal total cholesterol that is in line with the recent meta-analysis [19]. Total cholesterol levels were decreasing, partly due to the increasing use of lipid-lowering drugs [78, 79]. We reported that 41% of participants had ideal blood pressure that is consistent with findings from the recent US nationally representative survey (42.3%) [80], but higher in comparison with results of a recent meta-analysis (34.6%) [19] and the China national hypertension survey (35.5%) [81]. Our results of ideal physical activity (41%), and ideal BMI (41%) are also in accordance with a previous meta-analysis by Peng et al. [19]. In our study, the poorest CVH metric was a healthy diet (5.8%) like in both previous reviews [15, 19] and almost all individual studies that examined ideal CVH. Although the prevalence of a healthy diet is extremely low, the question of its relevance to ideal CVH does not arise. A healthy diet is one of 7 CVH metrics proposed by AHA, essential for keeping people healthy across the lifespan which could be successfully improved [1]. Unfortunately, physical activity levels and low diet quality scores changed minimally during the observed time [74]. Hence, successful prevention efforts for improvement of healthy diet and physical activity are needed. This should result in improvement in BMI, blood pressure, fasting blood glucose, and overall CVH status and reducing the related CVD burden.
In this study, women had twice higher ideal CVH (6%) than men (3%) and a higher percentage of 5 and more ideal CVH metrics (21% in women vs. 13% in men) that is in line with findings from a recent meta-analysis [19]. Several studies have specifically investigated gender disparities in the distribution of ideal CVH and discussed the potential reasons behind that [7, 9, 31]. There is evidence that women attended primary care (general practitioner/family physician) and preventive services more often than men [82–84]. Simon et al. [9] hypothesized that more frequent contact of women with the health care system throughout their life (e.g. concerning contraception, pregnancy, and child care) is an opportunity to be more sensitive to health promotion and prevention, contributing to a greater willingness to follow public health and medical recommendations. Subgroup analysis also revealed that gender was a statistically significant moderator of ideal smoking, with a higher percentage in females (81%) compared to males (60%). It could partly be explained by less frequent smoking in women than men. However, epidemiological evidence suggests that smoking is a stronger cardiovascular risk factor in women [85, 86]. This finding and increasing trend in female smoking point out that tobacco control policies should include items specifically targeted at women. Also, there was a statistically significant difference in ideal blood pressure between females (42%) and males (30%) which is in concert with a higher prevalence of raised blood pressure in men compared to women worldwide, but this difference was only statistically significant in the Region of the Americas and the European Region [87].
From the beginning of this century, considerable efforts have been made to improve understanding of the sex/gender differences in CVD and to heighten awareness of heart disease in women [7]. Policy and prevention efforts, to be successful, need to be investigated and targeted within genders. A better understanding of sex differences in CVD is needed to prevent and treat CVD more efficiently in both gender. Continued efforts are required to unravel the belief that CVD is a man’s disease [88].
Like in themeta-analysis by Peng et al. [19] our results showed that younger adults had higher overall CVH than older counterparts. We found statistically significant differences in the summary prevalence of ideal CVH among younger (8%), middle-aged (3%), and older participants (1%). The highest prevalence of ideal CVH observed in younger subjects could be explained mostly by their better ideal health factors, although this is in contrast to the poor results on health behaviors reported elsewhere [4, 89]. Comparing to other two groups, the oldest participants had lower levels of almost all ideal CVH metrics except for smoking and diet [4, 49]. Nevertheless, the young people should be a priority objective for primordial prevention that may prevent worsening of their current CVH in the future.
Although literature data highlights the relevance of SES as determinants of health in both high- income and low- and middle-income countries [90–92], only a few studies have examined the association between ideal CVH and SES. Accumulating evidence supports the notion that social environment (SES and social networks) shape the personal lifestyle choices such as physical activity, nutritional choices, and smoking which profoundly influence CVH risk factors. However, the cumulative impact of the environment on CVD risk has been difficult to assess and the mechanisms by which some environment factors influence CVD remain obscure [93]. Education, income or aggregation of assets and household facilities known as the Wealth index [94, 95] are most commonly used as proxies for SES. Results from many studies included in our systematic review showed that participants with higher education had a greater number of ideal CVH metrics, i.e. better CVH in comparison with those with lower education. Olsen et al. [5] reported an increasing trend in ideal CVH with a more unfavorable risk profile among persons with low educational levels. Another study [96] found that additional years of education are associated with better CVH. The Tromso study [97] demonstrated the most unfavorable CVD risk factors in the lowest educational group. Our results are also in accordance with the results from the world’s largest population-based cross-sectional study performed in the 50 states of the USA [3]. Only two studies [30, 48] included in our review assessed the association between Wealth index and ideal CVH. Jankovic et al. [48] found a positive association, while the opposite results were noted in the study by Benziger et al. [30]. Several previous studies failed to find any significant association between the Wealth index and CVH score [98, 99]. Overall, the results of this review suggest that those with higher levels of SES have better CVH and a possible explanation could be the fact that people with higher education or income are more prone to afford healthier foods and exercise more compared with those with lower education or income. Also, better-off people compared with those worse-off are more likely to afford high-quality health care.
The strength of our study is that we calculated the pooled prevalence estimates for the 7 ideal CVH metrics and overall CVH according to age and sex on a large sample size (over 2 million people). Besides, this is the first systematic review on the relationship between participants’ SES and ideal CVH. However, several limitations should be briefly stressed. First, the results of meta-analyses of ideal CVH metrics and ideal CVH showed a great heterogeneity across studies and it could be explained by the variance in the measurements of ideal CVH metrics in assessed studies, differences in the study populations in terms of gender, age, SES, geographic distribution, lifestyle patterns, and a difference in survey years for each of the included studies. Second, some CVH metrics (smoking, dietary intake, and physical activity) were self-reported measures, which carried an inherent degree of bias. Third, not all studies followed the metric definitions of AHA, especially for a healthy diet or physical activity which may preclude comparisons between studies. To address heterogeneity at least a part, we performed subgroup analyses of each of the 7 ideal CVH metrics and their clustering (6 and 7; and 5 and more ideal metrics) by gender and age groups.
Conclusion
Our systematic review and meta-analysis provided evidence that ideal CVH is low worldwide. We found that gender was a statistically significant moderator of ideal CVH, cluster of 5 and more ideal CVH metrics, ideal smoking, and ideal blood pressure (the better values were observed in females). Also, younger, more educated and better-off individuals had a greater number of ideal CVH metrics, i.e. better ideal CVH in comparison with middle or old age participants, less educated and worse-off. To achieve the improvement of the CVH metrics and the overall ideal CVH, nationwide primordial prevention efforts at the population and individual levels are urgently needed and should focus on the diet, as well as those components which showed gender inequalities, such as smoking and blood pressure. Targeting public health interventions to improve CVH status among less educated and more disadvantaged individuals may have substantial societal implications.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The study was funded by the Ministry of Education, Science and Technological Development of the Republic of Serbia (project No. 200110). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The american heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121: 586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 2.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the american heart association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57: 1690–1696. doi: 10.1016/j.jacc.2010.11.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 States and the District of Columbia, 2009. J Am Heart Assoc. 2012;1: 1–13. doi: 10.1161/JAHA.111.000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graciani A, León-Muñoz LM, Guallar-Castillón P, Rodríguez-Artalejo F, Banegas JR. Cardiovascular health in a southern mediterranean european country a nationwide population-based study. Circ Cardiovasc Qual Outcomes. 2013;6: 90–98. doi: 10.1161/CIRCOUTCOMES.112.967893 [DOI] [PubMed] [Google Scholar]
- 5.Olsen GS, Holm ASS, Jørgensen T, Borglykke A. Distribution of ideal cardiovascular health by educational levels from 1978 to 2006: A time trend study from the capital region of Denmark. Eur J Prev Cardiol. 2014;21: 1145–1152. doi: 10.1177/2047487313485513 [DOI] [PubMed] [Google Scholar]
- 6.Janković J, Erić M, Stojisavljević D, Marinković J, Janković S. Socio-Economic Differences in Cardiovascular Health: Findings from a Cross-Sectional Study in a Middle-Income Country. PLoS One. 2015;10: e0141731. doi: 10.1371/journal.pone.0141731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janković J, Marinković J, Stojisavljević D, Erić M, Vasiljević N, Janković S. Sex inequalities in cardiovascular health: a cross-sectional study. Eur J Public Health. 2016;26: 152–158. doi: 10.1093/eurpub/ckv161 [DOI] [PubMed] [Google Scholar]
- 8.Lu Y, Shen S, Qi H, Fang N, Li F, Wang L, et al. Prevalence of ideal cardiovascular health in southeast Chinese adults. Int J Cardiol. 2015;184: 385–387. doi: 10.1016/j.ijcard.2015.02.104 [DOI] [PubMed] [Google Scholar]
- 9.Simon M, Boutouyrie P, Narayanan K, Gaye B, Tafflet M, Thomas F, et al. Sex disparities in ideal cardiovascular health. Heart. 2017;103: 1595–1601. doi: 10.1136/heartjnl-2017-311311 [DOI] [PubMed] [Google Scholar]
- 10.De Moraes ACF, Carvalho HB, McClelland RL, Diez-Roux A V, Szklo M. Sex and ethnicity modify the associations between individual and contextual socioeconomic indicators and ideal cardiovascular health: MESA study. J Public Health (Oxf). 2019;41: e237–e244. doi: 10.1093/pubmed/fdy145 [DOI] [PubMed] [Google Scholar]
- 11.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125: 987–995. doi: 10.1161/CIRCULATIONAHA.111.049122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang Q, Cogswell ME, Dana Flanders W, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among us adults. JAMA—J Am Med Assoc. 2012;307: 1273–1283. doi: 10.1001/jama.2012.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang X, Wang A, Liu X, An S, Chen S, Wang Y, et al. Positive changes in ideal CVH metrics reduce the incidence of stroke. Sci Rep. 2016;6: 1–7. doi: 10.1038/s41598-016-0001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaye B, Tajeu GS, Vasan RS, Lassale C, Allen NB, Singh-Manoux A, et al. Association of Changes in Cardiovascular Health Metrics and Risk of Subsequent Cardiovascular Disease and Mortality. J Am Heart Assoc. 2020;9: e017458. doi: 10.1161/JAHA.120.017458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Younus A, Aneni EC, Spatz ES, Osondu CU, Roberson L, Ogunmoroti O, et al. A Systematic Review of the Prevalence and Outcomes of Ideal Cardiovascular Health in US and Non-US Populations. Mayo Clin Proc. 2016;91: 649–670. doi: 10.1016/j.mayocp.2016.01.019 [DOI] [PubMed] [Google Scholar]
- 16.Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: A meta-analysis. Int J Cardiol. 2016;214: 279–283. doi: 10.1016/j.ijcard.2016.03.210 [DOI] [PubMed] [Google Scholar]
- 17.Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: A meta-analysis of prospective studies. Clin Cardiol. 2017;40: 1339–1346. doi: 10.1002/clc.22836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aneni EC, Crippa A, Osondu CU, Valero-Elizondo J, Younus A, Nasir K, et al. Estimates of mortality benefit from ideal cardiovascular health metrics: A dose response meta-analysis. J Am Heart Assoc. 2017;6. doi: 10.1161/JAHA.117.006904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peng Y, Cao S, Yao Z, Wang Z. Prevalence of the cardiovascular health status in adults: A systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2018;28: 1197–1207. doi: 10.1016/j.numecd.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institutes of Health. National Heart Lung and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, vol. 2015. Bethesda, MD; 2014 [cited 21 Nov 2020]. Available: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 22.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012Sep;65(9):934–9. doi: 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7: 177–188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 24.Cochran WG. The Combination of Estimates from Different Experiments Author(s): William G. Cochran Source: Biometrics. 1954;10: 101–129. [Google Scholar]
- 25.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21: 1539–1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 26.Viechtbauer W, Cheung MW-L. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1: 112–125. doi: 10.1002/jrsm.11 [DOI] [PubMed] [Google Scholar]
- 27.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. Available: https://www.r-project.org/ [Google Scholar]
- 28.Viechtbauer W. Conducting meta-analyses in R with the metafor. J Stat Softw. 2010;36: 1–48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 29.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of ideal cardiovascular health in a community-based population: The heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011;123: 850–857. doi: 10.1161/CIRCULATIONAHA.110.980151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benziger CP, Zavala-Loayza JA, Bernabe-Ortiz A, Gilman RH, Checkley W, Smeeth L, et al. Low prevalence of ideal cardiovascular health in Peru. Heart. 2018;104: 1251–1256. doi: 10.1136/heartjnl-2017-312255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bi Y, Jiang Y, He J, Xu Y, Wang L, Xu M, et al. Status of cardiovascular health in Chinese adults. J Am Coll Cardiol. 2015;65: 1013–1025. doi: 10.1016/j.jacc.2014.12.044 [DOI] [PubMed] [Google Scholar]
- 32.Bundy JD, Ning H, Zhong VW, Paluch AE, Lloyd-Jones DM, Wilkins JT, et al. Cardiovascular Health Score and Lifetime Risk of Cardiovascular Disease. Circ Cardiovasc Qual Outcomes. 2020;13: 1–11. doi: 10.1161/CIRCOUTCOMES.119.006450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang Y, Guo X, Chen Y, Guo L, Li Z, Yu S, et al. Prevalence and Metrics Distribution of Ideal Cardiovascular Health: A Population-based, Cross-sectional Study in Rural China. Hear Lung Circ. 2016;25: 982–992. doi: 10.1016/j.hlc.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 34.Chung JWY, Wong BYM, Yan VCM, Chung LMY, So HCF, Chan A. Cardiovascular health of construction workers in Hong Kong: A cross-sectional study. Int J Environ Res Public Health. 2018;15: 1251. doi: 10.3390/ijerph15061251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Del Brutto OH, Dong C, Rundek T, Elkind MSV, Del Brutto VJ, Sacco RL. Cardiovascular health status among Caribbean Hispanics living in northern Manhattan and Ecuadorian natives/mestizos in rural coastal Ecuador: A comparative study. J Community Health. 2013;38: 634–641. doi: 10.1007/s10900-013-9658-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Djoussé L, Petrone AB, Blackshear C, Griswold M, Harman JL, Clark CR, et al. Prevalence and changes over time of ideal cardiovascular health metrics among African-Americans: The Jackson Heart Study. Prev Med (Baltim). 2015;74: 111–116. doi: 10.1016/j.ypmed.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fan C, Zhang Q, Zhang S, Wang A, Bi X, Chen S, et al. Association of Newly Found Asymptomatic Intracranial Artery Stenosis and Ideal Cardiovascular Health Metrics in Chinese Community Population. Sci Rep. 2020;10: 1–9. doi: 10.1038/s41598-019-56847-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fang J, Zhang Z, Ayala C, Thompson-Paul AM, Loustalot F. Cardiovascular health among non-Hispanic Asian Americans: NHANES, 2011–2016. J Am Heart Assoc. 2019;8: 2011–2016. doi: 10.1161/JAHA.118.011324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Foraker RE, Bush C, Greiner MA, Sims M, Henderson K, Smith S, et al. Distribution of Cardiovascular Health by Individual- and Neighborhood-Level Socioeconomic Status: Findings From the Jackson Heart Study. Glob Heart. 2019;14: 241–250. doi: 10.1016/j.gheart.2019.04.007 [DOI] [PubMed] [Google Scholar]
- 40.Gao B, Wang F, Zhu M, Wang J, Zhou M, Zhang L, et al. Cardiovascular health metrics and all-cause mortality and mortality from major non-communicable chronic diseases among Chinese adult population. Int J Cardiol. 2020;313: 123–128. doi: 10.1016/j.ijcard.2020.04.048 [DOI] [PubMed] [Google Scholar]
- 41.Gaye B, Tajeu GS, Offredo L, Vignac M, Johnson S, Thomas F, et al. Temporal trends of cardiovascular health factors among 366 270 French adults. Eur Hear J—Qual Care Clin Outcomes. 2020;6: 138–146. doi: 10.1093/ehjqcco/qcz038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghimire U, Shrestha N, Gyawali B, Pradhan PMS, Mishra SR. Prevalence of American Heart Association defined ideal cardiovascular health metrics in Nepal: findings from a nationally representative cross-sectional study. Int Health. 2020;12: 325–331. doi: 10.1093/inthealth/ihz088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.González HM, Tarraf W, Rodríguez CJ, Gallo LC, Sacco RL, Talavera GA, et al. Cardiovascular health among diverse Hispanics/Latinos: Hispanic Community Health Study/Study of Latinos (HCHS/SOL) results. Am Heart J. 2016;176: 134–144. doi: 10.1016/j.ahj.2016.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.González-Rivas JP, Mechanick JI, Ugel E, Marulanda MI, Duran M, Nieto-Martínez R. Cardiovascular Health in a National Sample of Venezuelan Subjects Assessed According to the AHA Score: The EVESCAM. Glob Heart. 2019;14: 285–293. doi: 10.1016/j.gheart.2019.06.006 [DOI] [PubMed] [Google Scholar]
- 45.Gupta B, Gupta R, Sharma KK, Gupta A, Mahanta TG, Deedwania PC. Low Prevalence of AHA-Defined Ideal Cardiovascular Health Factors: A Study of Urban Indian Men and Women. Glob Heart. 2017;12: 219–225. doi: 10.1016/j.gheart.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 46.Harrison S, Couillard C, Robitaille J, Vohl MC, Bélanger M, Desroches S, et al. Assessment of the American Heart Association’s “Life’s simple 7” score in French-speaking adults from Québec. Nutr Metab Cardiovasc Dis. 2019;29: 684–691. doi: 10.1016/j.numecd.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 47.Isiozor NM, Kunutsor SK, Voutilainen A, Kurl S, Kauhanen J, Laukkanen JA. Association between ideal cardiovascular health and risk of sudden cardiac death and all-cause mortality among middle-aged men in Finland. Eur J Prev Cardiol. 2020; 204748732091533. doi: 10.1177/2047487320915338 [DOI] [PubMed] [Google Scholar]
- 48.Janković J, Davidović M, Bjegović-Mikanović V, Janković S. Status of cardiovascular health in the Republic of Serbia: Results from the National Health Survey. Manfrini O, editor. PLoS One. 2019;14: e0214505. doi: 10.1371/journal.pone.0214505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Janković S, Stojisavljević D, Janković J, Erić M, Marinković J. Status of cardiovascular health in a transition European country: findings from a population-based cross-sectional study. Int J Public Health. 2014;59: 769–778. doi: 10.1007/s00038-014-0579-1 [DOI] [PubMed] [Google Scholar]
- 50.Kim JI, Sillah A, Boucher JL, Sidebottom AC, Knickelbine T. Prevalence of the American heart association’s “ideal cardiovascularhealth” metrics in a rural, cross-sectional, community-based study: The heart of new ulm project. J Am Heart Assoc. 2013;2: 1–11. doi: 10.1161/JAHA.113.000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JY, Ko YJ, Rhee CW, Park BJ, Kim DH, Bae JM, et al. Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: The seoul male cohort study. J Prev Med Public Heal. 2013;46: 319–328. doi: 10.3961/jpmph.2013.46.6.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kulshreshtha A, Vaccarino V, Judd SE, Howard VJ, McClellan WM, Muntner P, et al. Life’s simple 7 and risk of incident stroke: The reasons for geographic and racial differences in stroke study. Stroke. 2013;44: 1909–1914. doi: 10.1161/STROKEAHA.111.000352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lawrence EM, Hummer RA, Domingue BW, Harris KM. Wide educational disparities in young adult cardiovascular health. SSM—Popul Heal. 2018;5: 249–256. doi: 10.1016/j.ssmph.2018.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu Y, Chi HJ, Cui LF, Yang XC, Wu YT, Huang Z, et al. The ideal cardiovascular health metrics associated inversely with mortality from all causes and from cardiovascular diseases among adults in a Northern Chinese industrial city. PLoS One. 2014;9: 1–7. doi: 10.1371/journal.pone.0089161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Machado LBM, Silva BLS, Garcia AP, Oliveira RAM, Barreto SM, Fonseca M de JM, et al. Ideal cardiovascular health score at the ELSA-Brasil baseline and its association with sociodemographic characteristics. Int J Cardiol. 2018;254: 333–337. doi: 10.1016/j.ijcard.2017.12.037 [DOI] [PubMed] [Google Scholar]
- 56.Matozinhos FP, Felisbino-Mendes MS, Gomes CS, Jansen AK, Machado ÍE, Lana FCF, et al. Saúde cardiovascular em população residente nas capitais brasileiras. Rev Lat Am Enfermagem. 2017;25. doi: 10.1590/1518-8345.1327.2843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Medina-Inojosa JR, Vinciguerra M, Maugeri A, Kunzova S, Sochor O, Movsisyan N, et al. Prevalence of ideal cardiovascular health in a Central European community: results from the Kardiovize Brno 2030 Project. Eur J Prev Cardiol. 2020;27: 441–443. doi: 10.1177/2047487319834875 [DOI] [PubMed] [Google Scholar]
- 58.Moghaddam MM, Mohebi R, Hosseini F, Lotfaliany M, Azizi F, Saadat N, et al. Distribution of ideal cardiovascular health in a community-based cohort of Middle East population. Ann Saudi Med. 2014;34: 134–142. doi: 10.5144/0256-4947.2014.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nowicki GJ, Ślusarska B, Piasecka H, Bartoszek A, Kocka K, Deluga A. The status of cardiovascular health in rural and urban areas of janów lubelski district in eastern poland: A population-based study. Int J Environ Res Public Health. 2018;15. doi: 10.3390/ijerph15112388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ogunmoroti O, Utuama OA, Michos ED, Valero-Elizondo J, Okunrintemi V, Taleb Z Ben, et al. Does education modify the effect of ethnicity in the expression of ideal cardiovascular health? The Baptist Health South Florida Employee Study. Clin Cardiol. 2017;40: 1000–1007. doi: 10.1002/clc.22757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ommerborn MJ, Blackshear CT, Hickson DMA, Griswold ME, Kwatra J, Djoussé L, et al. Ideal Cardiovascular Health and Incident Cardiovascular Events: The Jackson Heart Study. Am J Prev Med. 2016;51: 502–506. doi: 10.1016/j.amepre.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Patel N, Kalra R, Bhargava A, Arora G, Arora P. Ideal Cardiovascular Health Among American Adults After the Economic Recession of 2008–2009: Insights from NHANES. Am J Med. 2019;132: 1182–1190.e5. doi: 10.1016/j.amjmed.2019.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peng Y, Wang Z. Cardiovascular health status among australian adults. Clin Epidemiol. 2018;10: 167–178. doi: 10.2147/CLEP.S155783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pilkerton CS, Singh SS, Bias TK, Frisbee SJ. Changes in cardiovascular health in the United States, 2003–2011. J Am Heart Assoc. 2015;4: 2003–2011. doi: 10.1161/JAHA.114.001650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ren J, Guo XL, Lu ZL, Zhang JY, Tang JL, Chen X, et al. Ideal cardiovascular health status and its association with socioeconomic factors in Chinese adults in Shandong, China. BMC Public Health. 2016;16: 1–7. doi: 10.1186/s12889-015-2639-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seron P, Irazola V, Rubinstein A, Calandrelli M, Ponzo J, Olivera H, et al. Ideal Cardiovascular Health in the southern cone of Latin America. Public Health. 2018;156: 132–139. doi: 10.1016/j.puhe.2017.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, et al. Status of cardiovascular health in US adults: Prevalence Estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125: 45–56. doi: 10.1161/CIRCULATIONAHA.111.035733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.van Nieuwenhuizen B, Zafarmand MH, Beune E, Meeks K, Aikins A de G, Addo J, et al. Ideal cardiovascular health among Ghanaian populations in three European countries and rural and urban Ghana: the RODAM study. Intern Emerg Med. 2018;13: 845–856. doi: 10.1007/s11739-018-1846-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Velasquez-Melendez G, Felisbino-Mendes MS, Matozinhos FP, Claro R, Gomes CS, Malta DC. Prevalência de saúde cardiovascular ideal na população Brasileira–pesquisa nacional de saúde (2013). Rev Bras Epidemiol. 2015;18: 97–108. doi: 10.1590/1980-5497201500060009 [DOI] [PubMed] [Google Scholar]
- 70.Wu HY, Sun ZH, Cao DP, Wu LX, Zeng Q. Cardiovascular health status in Chinese adults in urban areas: Analysis of the Chinese Health Examination Database 2010. Int J Cardiol. 2013;168: 760–764. doi: 10.1016/j.ijcard.2012.09.235 [DOI] [PubMed] [Google Scholar]
- 71.Wu S, Huang Z, Yang X, Zhou Y, Wang A, Chen L, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a Northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5: 487–493. doi: 10.1161/CIRCOUTCOMES.111.963694 [DOI] [PubMed] [Google Scholar]
- 72.Zeng Q, Dong SY, Song ZY, Zheng YS, Wu HY, Mao LN. Ideal cardiovascular health in Chinese urban population. Int J Cardiol. 2013;167: 2311–2317. doi: 10.1016/j.ijcard.2012.06.022 [DOI] [PubMed] [Google Scholar]
- 73.Zhao Y, Yan H, Yang R, Li Q, Dang S, Liu R, et al. Status of cardiovascular health among adults in a rural area of Northwest China: Results from a cross-sectional study. Med (United States). 2016;95: 1–9. doi: 10.1016/j.ijmedinf.2016.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: Results from the national health and nutrition examination surveys. Circulation. 2012;125: 2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang DD, Leung CW, Li Y, Ding EL, Chiuve SE, Hu FB, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174: 1587–1595. doi: 10.1001/jamainternmed.2014.3422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Devonshire-Gill KR NK. Australian adult physical activity sufficiency trend data: positive, prevalent, and persistent changes 2002–2012. J Phys Act Heal. 2018;15: 117e26. [DOI] [PubMed] [Google Scholar]
- 77.Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: A systematic review for the community preventive services task force. Ann Intern Med. 2015;163: 437–451. doi: 10.7326/M15-0452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cohen JD, Cziraky MJ, Cai Q, Wallace A, Wasser T, Crouse JR, et al. 30-year trends in serum lipids among united states adults: Results from the national health and nutrition examination surveys II, III, and 19992006. Am J Cardiol. 2010;106: 969–975. doi: 10.1016/j.amjcard.2010.05.030 [DOI] [PubMed] [Google Scholar]
- 79.Hopstock LA, Bønaa KH, Eggen AE, Grimsgaard S, Jacobsen BK, Løchen ML, et al. Longitudinal and secular trends in total cholesterol levels and impact of lipid-lowering drug use among Norwegian women and men born in 1905–1977 in the population-based Tromsø Study 1979–2016. BMJ Open. 2017;7: 1–10. doi: 10.1136/bmjopen-2016-015001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, et al. Potential U.S. Population Impact of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Circulation. 2018;137: 109–118. doi: 10.1161/CIRCULATIONAHA.117.032582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018; 2344e56. doi: 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 82.Bertakis KD, Azari R, Jay Helms L, Callahan EJ, Robbins JA, Sacramento M. Gende r D ifferences in th e U tilization of Health Care Services. 2000;49. [PubMed] [Google Scholar]
- 83.Jankovic J, Simic S, Marinkovic J. Inequalities that hurt: demographic, socio-economic and health status inequalities in the utilization of health services in Serbia. Eur J Public Health. 2010;20: 389–396. doi: 10.1093/eurpub/ckp189 [DOI] [PubMed] [Google Scholar]
- 84.Janković J, Šiljak S, Erić M, Marinković J, Janković S. Inequalities in the utilization of health care services in a transition European country: results from the national population health survey. Int J Public Health. 2018;63: 261–272. doi: 10.1007/s00038-017-1009-y [DOI] [PubMed] [Google Scholar]
- 85.Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J. Smoking and risk of myocardial infarction in women and men: Longitudinal population study. Br Med J. 1998;316: 1043–1047. doi: 10.1136/bmj.316.7137.1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: A systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378: 1297–1305. doi: 10.1016/S0140-6736(11)60781-2 [DOI] [PubMed] [Google Scholar]
- 87.WHO. Global status report on noncommunicable diseases 2010. World Health Organization. 2011. pp. 9–31. [Google Scholar]
- 88.Bots SH, Peters SAE, Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health. 2017;2(2):e000298. doi: 10.1136/bmjgh-2017-000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Janković S, Stojisavljević D, Janković J, Erić M, Marinković J. Association of socioeconomic status measured by education, and cardiovascular health: a population-based cross-sectional study. BMJ Open. 2014;4: e005222–e005222. doi: 10.1136/bmjopen-2014-005222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mayén AL, Marques-Vidal P, Paccaud F, Bovet P, Stringhini S. Socioeconomic determinants of dietary patterns in low- and middle-income countries: A systematic review. Am J Clin Nutr. 2014;100: 1520–1531. doi: 10.3945/ajcn.114.089029 [DOI] [PubMed] [Google Scholar]
- 91.Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: A review. Bull World Health Organ. 2004;82: 940–946. doi: /S0042-96862004001200011 [PMC free article] [PubMed] [Google Scholar]
- 92.Leinsalu M, Tekkel M, Kunst AE. Social determinants of ever initiating smoking differ from those of quitting: A cross-sectional study in Estonia. Eur J Public Health. 2007;17: 572–578. doi: 10.1093/eurpub/ckm030 [DOI] [PubMed] [Google Scholar]
- 93.Bhatnagar A. Environmental Determinants of Cardiovascular Disease. Circ Res. 2017;121: 162–180. doi: 10.1161/CIRCRESAHA.117.306458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rutstein SO JK. The DHS Wealth Index. DHS Comparative Reports No. 6. Calverton, Maryland; 2004. Available: http://www.measuredhs.com/pubs/pub_details.cfm?ID¼470
- 95.Jankovic J, Marinkovic J, Simic S. Utility of data from a national health survey: Do socioeconomic inequalities in morbidity exist in Serbia? Scand J Public Health. 2011;39: 230–238. doi: 10.1177/1403494811401477 [DOI] [PubMed] [Google Scholar]
- 96.Kubota Y, Heiss G, Maclehose RF, Roetker NS, Folsom AR. Association of educational attainment with lifetime risk of cardiovascular disease the atherosclerosis risk in communities study. JAMA Intern Med. 2017;177: 1165–1172. doi: 10.1001/jamainternmed.2017.1877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Eggen AE, Mathiesen EB, Wilsgaard T, Jacobsen BK, Njølstad I. Trends in cardiovascular risk factors across levels of education in a general population: Is the educational gap increasing? The Tromsø study 1994–2008. J Epidemiol Community Health. 2014;68: 712–719. doi: 10.1136/jech-2013-203428 [DOI] [PubMed] [Google Scholar]
- 98.Ball K, Crawford D. Socioeconomic status and weight change in adults: A review. Soc Sci Med. 2005;60: 1987–2010. doi: 10.1016/j.socscimed.2004.08.056 [DOI] [PubMed] [Google Scholar]
- 99.Stelmach W, Kaczmarczyk-Chałas K, Bielecki W, Drygas W. How education, income, control over life and life style contribute to risk factors for cardiovascular disease among adults in a post-communist country. Public Health. 2005;119: 498–508. doi: 10.1016/j.puhe.2004.09.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.