Abstract
Objective:
To investigate the long-term influence of fixed lingual retainers on the development of mandibular gingival recession and to compare the prevalence with untreated individuals.
Materials and Methods:
The material consisted of 144 subjects: 96 orthodontically treated patients followed for 5 years after therapy and 48 untreated age-matched subjects. The treated patients were divided in two groups: one receiving a fixed mandibular retainer (n = 48) and one receiving no form of retention in the mandible (n = 48). The presence or absence of gingival recession and calculus accumulation were scored before treatment (T0), after debonding (T1), and 5 years after debonding (T5) for each tooth in the mandibular intercanine region using plaster models and intraoral photographs. The chi-square test, one-way ANOVA, and Cochran's Q test were used to evaluate inter- and intragroup differences.
Results:
The prevalence of patients with recession increased gradually and significantly throughout the observation periods in all groups, but the intergroup differences at T5 were not significant. Significantly more calculus accumulation was observed at T5 in the retainer group compared with the group without retainers.
Conclusions:
Long-term presence of fixed lingual retainers does not seem to increase the development of mandibular gingival recession, but does increase calculus accumulation.
Keywords: Gingival recession, Orthodontic retainers, Orthodontics, Calculus
INTRODUCTION
Gingival recession is described as the displacement of the marginal tissue apical to the cementoenamel junction, which leads to exposure of the root surface.1 The etiology is not completely clarified, since both predisposing and precipitating factors are involved. In orthodontically treated patients, the prevalence, severity, and extent of recession have been reported to be higher than in untreated controls,2–4 and the prevalence increased during the posttreatment period.5 It has been indicated that orthodontic treatment combined with fixed lingual retainers promotes gingival recession.2,6 However, other studies have found that fixed retainers have no negative effects on periodontal health.7,8
Mandibular central incisors have been shown to be particularly susceptible to the development of gingival recession.5,9 Compared with untreated controls, the prevalence of gingival recession in mandibular incisors was found to be higher in patients 5 years after orthodontic treatment.3 It is unclear whether orthodontic treatment per se, proclination of incisors,10 or the presence of fixed retention has more influence on the development of gingival recession,3,11 but the type of fixed retainer did not seem to play a significant role.5,12
Previous studies have not resolved the question of whether fixed lingual retainers cause gingival recession. To our knowledge, no studies have investigated the isolated influence of fixed lingual retainers on gingival recession by comparing orthodontically treated patients with and without fixed mandibular retainers. Therefore, the aim of this study was to compare the prevalence of mandibular gingival recession in orthodontically treated patients with and without fixed lingual retainers 5 years after debonding and in a group of untreated, control subjects.
The null hypotheses
The prevalence of mandibular gingival recession in orthodontically treated patients with fixed lingual retainers is not significantly different from those without retainers 5 years after therapy.
The prevalence of mandibular gingival recession in orthodontically treated patients with fixed lingual retainers 5 years after therapy is not significantly different from that in untreated subjects.
MATERIALS AND METHODS
A cohort of 298 consecutively treated orthodontic patients who underwent routine retention control 5 years after orthodontic treatment between 2008 and 2015 were selected from the archives of the Department of Orthodontics, University of Oslo, Norway. These orthodontic patients were selected according to the following inclusion criteria: treated with full fixed appliances; orthodontic treatment started before age 18; and existence of good quality dental casts and intraoral photographs before treatment (T0), 4 to 6 weeks after debonding (T1), and 5 years after debonding (T5). Exclusion criteria were missing or extracted anterior teeth in the mandibular jaw, restorative treatment due to caries or trauma, and orthognathic surgery treatment. From this cohort, 48 patients who had not received any form of retention in the mandible comprised the T without R experimental group. After identifying and excluding these patients, a T with R experimental group of the same size (n = 48) was randomly drawn from the rest of the patient pool. Randomization was performed by computer-generated codes.
An untreated control group (n = 48) consisted of healthy subjects randomly drawn from the archives of the Nittedal Growth Material, a longitudinal study conducted by the Department of Orthodontics, University of Oslo, Norway,13 and consisting of records (models, panoramic radiographs, and cephalometric radiographs) from subjects born between 1958 and 1972 and recalled for dental examination at the ages of 6, 9, 12, 15, 18, and 21. None of the participants had undergone orthodontic treatment.
A sample-size analysis was performed before the study onset using MedCalc 14.8.1 (MedCalc Software BVBA, Ostend, Belgium). For α = 0.05, 1−β = 80, and hypothetical prevalence of recession of 44% in the retainer and 15% in the untreated groups, the established sample size was 45. The study protocol was approved by the Regional Committee for Medical and Health Research Ethics in Norway (2015/2368).
Demographic data, including gender, ages at T0, T1, and T5, and type of orthodontic treatment (extraction vs nonextraction), were obtained from the patient files. Angle classification was determined on plaster models at three assessment periods. The overjet, overbite, and Little's irregularity index (LII)14 were measured at T0, T1, and T5 on plaster models using calipers. At T0, T1, and T5, the presence or absence of gingival recession was scored for each tooth in the mandibular intercanine region on plaster models for all three groups. Recession was noted as present (yes) if the cementoenamel junction was exposed. Intraoral photographs were used to confirm the presence of gingival recession in the experimental groups but no intraoral color photographs were available for the control group. Calculus accumulation (yes/no) was evaluated on intraoral photographs only for the experimental groups. Calculus was noted as present (yes) if calculus accumulation was present on at least two teeth in the intercanine region.
Statistical Analysis
Means, standard deviations, and percentages were used to describe the groups at all assessment points. The chi-square test was used to compare groups by gender, Angle classification, treatment type, and number of patients with gingival recession, and calculus at T0, T1, and T5. One-way ANOVA with the Tukey post hoc test was used to evaluate the difference in age, LII, overjet, and overbite between groups. Related samples Cochran's Q test was used to investigate whether a difference in prevalence of subjects with gingival recession and calculus was present within groups between the three assessment periods, and logistic regression analysis was performed to evaluate the effect of orthodontic treatment, type of treatment (extraction vs nonextraction), presence of a fixed lingual retainer, gender, age, LII, overjet, overbite, and Angle classification on the development of gingival recession at T5.
The level of statistical significance was set at P ≤ .05. Statistical analyses were done using SPSS (IBM SPSS Version 21, Armonk, NY).
Error of the Method
Twenty dental casts were remeasured and intraclass correlation coefficients (ICCs) were used to determine intrarater reliability for LII, overjet, and overbite, while Cohen's kappa statistics were calculated to assess the strength of agreement for scoring the presence of recession and calculus accumulation. Both ICC (0.985 for LII, 0.977 for overjet, and 0.974 for overbite) and Cohen's kappa statistics (0.896 for recession per tooth and 0.814 for calculus accumulation) showed very good agreement between measurements.
RESULTS
The main characteristics of all investigated groups at all three assessment periods are given in Table 1. There were no statistically significant differences between the experimental groups regarding gender, age, observation periods, Angle classification, treatment type or overjet at any point. LII was significantly smaller at T0 and significantly greater at T5 in the treatment without retention group compared with the treatment with retention group. The untreated control group displayed traits characteristic of subjects with normal occlusion, and most of them were significantly different from the experimental groups. No differences were detected in gender, age at T1, or overjet at T5.
Table 1.
Characteristics of All Investigated Groups at All Three Assessment Periods With Statistical Analysis
|
|
T with Ra (n = 48) |
T without R (n = 48) |
UnT (n = 48) |
Statistical Test Done |
|||
| Gender, n (%) | |||||||
| Male | 24 (50.00%) | A | 25 (52.08%) | A | 16 (33.33%) | A | Chi-square test; P = .129 |
| Female | 24 (50.00%) | 23 (47.92%) | 32 (66.67%) | ||||
| Age, mean ± SDb, y | |||||||
| T0 | 12.78 ± 1.36 | A | 12.39 ± 1.52 | A | 11.73 ± 0.36 | B | ANOVA; P = .000, Tukey post hoc test |
| T1 | 14.98 ± 1.41 | A | 14.61 ± 1.67 | A | 14.71 ± 0.34 | A | ANOVA; P = .348, Tukey post hoc test |
| T5 | 20.27 ± 1.47 | A | 19.93 ± 1.65 | A | 21.18 ± 0.46 | B | ANOVA; P = .000, Tukey post hoc test |
| Duration of treatment/observation period, mean ± SD, y | 2.17 ± 0.65 | A | 2.18 ± 0.77 | A | 2.98 ± 0.11 | B | ANOVA; P = .000, Tukey post hoc test |
| Retention/observation period, mean ± SD, y | 5.24 ± 0.66 | A | 5.28 ± 0.53 | A | 6.47 ± 0.31 | B | ANOVA; P = .000, Tukey post hoc test |
| Angle classification T0 | |||||||
| Class I, n (%) | 23 (47.92%) | A | 24 (50.00%) | A | 37 (77.08%) | B | Chi-square test; P = .029 |
| Class II, n (%) | 24 (50.00%) | 23 (47.92%) | 11 (22.92%) | ||||
| Class III, n (%) | 1 (2.08%) | 1 (2.08%) | 0 (0%) | ||||
| Treatment type | |||||||
| Extraction | 17 (35.4%) | A | 11 (22.92%) | A | 0 (0%) | B | Chi-square test; P = .000 |
| Nonextraction | 31 (64.6%) | 37 (77.08%) | 48 (100%) | ||||
| Little irregularity index, mean ± SD, mm | |||||||
| T0 | 5.52 ± 4.13 | A | 2.46 ± 2.26 | B | 1.56 ± 1.55 | B | ANOVA; P = .000, Tukey post hoc test |
| T1 | 0.15 ± 0.42 | A | 0.36 ± 0.76 | A | 2.06 ± 1.83 | B | ANOVA; P = .000, Tukey post hoc test |
| T5 | 0.36 ± 0.76 | A | 1.57 ± 1.29 | B | 2.60 ± 2.20 | C | ANOVA; P = .000, Tukey post hoc test |
| Overjet, mean ± SD, mm | |||||||
| T0 | 4.30 ± 2.38 | A | 4.87 ± 2.53 | A | 3.26 ± 1.05 | B | ANOVA; P = .001, Tukey post hoc test |
| T1 | 2.57 ± 0.83 | A | 2.31 ± 0.68 | A | 3.01 ± 0.99 | B | ANOVA; P = .000, Tukey post hoc test |
| T5 | 2.40 ± 0.90 | A | 2.70 ± 1.07 | A | 2.52 ± 0.88 | A | ANOVA; P = .317, Tukey post hoc test |
| Overbite, mean ± SD, mm | |||||||
| T0 | 3.80 ± 1.62 | A | 3.04 ± 1.61 | B | 3.37 ± 0.92 | AB | ANOVA; P = .036, Tukey post hoc test |
| T1 | 2.17 ± 0.88 | A | 1.94 ± 0.80 | A | 3.19 ± 1.09 | B | ANOVA; P = .000, Tukey post hoc test |
| T5 | 2.19 ± 1.06 | A | 2.21 ± 1.09 | A | 2.81 ± 1.32 | B | ANOVA; P = .015, Tukey post hoc test |
T with R indicates treatment with retention experimental group (orthodontically treated patients with fixed lingual retainer); T without R, treatment without retention experimental group (orthodontically treated patients without fixed lingual retainer); UnT, control group of healthy untreated patients.
SD indicates standard deviation; T0, before treatment; T1, after debonding; T5, 5 years after debonding; same letters, that no statistically significant differences were present between the groups; different letters, statistically significant differences.
The prevalence of subjects with gingival recession increased gradually throughout the observation periods in all groups (Table 2). The prevalence of patients with gingival recession at T5 was significantly higher compared with T0 and T1 in both experimental groups, but there were no significant intergroup differences. In the untreated group, the prevalence also increased and was significantly higher at T5 than at T0. Significantly more calculus accumulation was observed on the lingual side in the group with retainers at T5 (Table 2).
Table 2.
Prevalence of Subjects With Gingival Recession and Calculus Accumulation for All Investigated Groups in the Three Assessment Periods With Statistical Analysis
|
|
T with Ra (n = 48) |
T without R (n = 48) |
UnT (n = 48) |
Statistical Test Done |
|
| Uppercase Letters |
Lowercase Letters |
||||
| Recessions: 43–33, n (%) | |||||
| T0b | 5 (10.42%) Ac a | 3 (6.25%) A a | 0 (0%) a | Chi-square test; P = .081 | Related samples Cochrane's Q test; T with R, P = .001; T without R, P = .000; UnT, P = .001 |
| T1 | 9 (18.75%) A a | 5 (10.42%) A a | 5 (10.42%) A ab | Chi-square test, P = .379 | |
| T5 | 18 (37.50%) A b | 16 (33.33%) A b | 10 (20.83%) A b | Chi-square test, P = .182 | |
| Calculus lingual: 43–33, n (%) | |||||
| T0 | 0 (0%) a | 0 (0%) a | No data | Related samples Cochrane's Q test; T with R, P = .000; T without R, P = .000 | |
| T1 | 0 (0%) A a | 1 (2.08%) A a | Chi-square test, P = .365 | ||
| T5 | 19 (39.58%) A b | 10 (20.83%) B b | Chi-square test, P = .000 | ||
T with R indicates treatment with retention experimental group (orthodontically treated patients with fixed lingual retainer); T without R,= treatment without retention experimental group (orthodontically treated patients without fixed lingual retainer); UnT, control group of healthy untreated patients.
T0 indicates before treatment; T1, after debonding; T5, 5 years after debonding.
Uppercase letters represent the difference between groups at each assessment period; lowercase letters, intragroup difference between different assessment periods; same letters, no statistically significant differences were present; different letters, statistically significant differences.
In both experimental groups and in the control group, most of the patients had one or two teeth with recession at all assessment times. Only a couple of patients had three or more teeth having recession in the intercanine region (Table 3).
Table 3.
Prevalence of Subjects With Gingival Recession in the Intercanine Region (43–33) Before Treatment (T0), After Debonding (T1), and 5 Years After Debonding (T5)
| Subjects |
T with Ra (n = 48) |
T without R (n = 48) |
UnT (n = 48) |
||||||
| T0 |
T1 |
T5 |
T0 |
T1 |
T5 |
T0 |
T1 |
T5 |
|
| Without recessions, % | 43 89.58 | 39 81.25 | 30 62.50 | 45 93.75 | 43 89.58 | 32 66.67 | 48 100 | 43 89.58 | 38 79.17 |
| With recessions, % | 5 10.42 | 9 18.75 | 18 37.50 | 3 6.25 | 5 10.42 | 16 33.33 | 0 (0) | 5 10.42 | 10 20.83 |
| With 1 recession, n | 4 | 6 | 11 | 1 | 4 | 8 | – | 3 | 6 |
| With 2 recessions, n | 1 | 2 | 5 | 2 | 1 | 6 | – | 1 | 4 |
| With 3 recessions, n | – | – | 2 | – | – | 2 | – | – | – |
| With 4 recessions, n | – | 1 | – | – | – | – | – | – | – |
| With 5 recessions, n | – | – | – | – | – | – | – | 1 | – |
| With 6 recessions n | – | – | – | – | – | – | – | – | – |
| Total recessions n | 6 | 14 | 27 | 5 | 6 | 26 | 0 | 10 | 14 |
T with R indicates treatment with retention, experimental group (orthodontically treated patients with fixed lingual retainer); T without R, treatment without retention, experimental group (orthodontically treated patients without fixed lingual retainer); UnT, control group of healthy untreated patients.
The frequencies of gingival recession on each tooth at T0, T1 and T5, in all three groups are displayed in Figure 1. The mandibular left central incisor was significantly more affected in the treatment with retention group than in the other groups, both before treatment, after debonding, and at the 5-year follow-up period. None of the mandibular central incisors in the treatment without retention group had recession at any assessment period. The recession found on the mandibular lateral incisors was similar in all groups. On the other hand, canines in the treatment without retention group were more frequently affected than were the other groups, particularly at T5.
Figure 1.
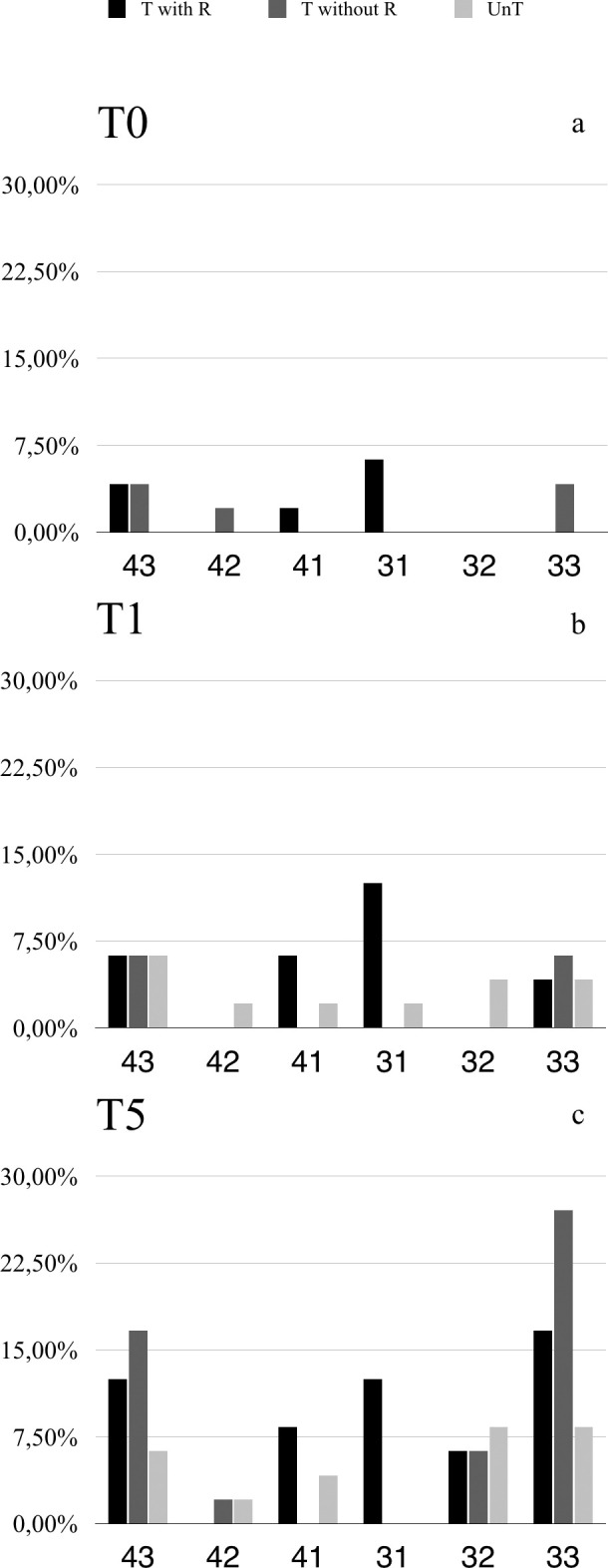
Frequencies (%) of gingival recession in the mandible by tooth type and group. T with R = Treatment with retention group: orthodontically treated patients with fixed lingual retainer; T without R = Treatment without retention group: orthodontically treated patients without fixed lingual retainer; UnT = control group of untreated patients at three assessment times: (a) T0 = before treatment, (b) T1 = after debonding, and (c) T5 = 5 years after debonding.
Stepwise multiple regression analysis showed that the recession at T5 was not influenced by orthodontic treatment, extractions, retainer, age and gender, nor by pretreatment LII, overjet, overbite, and Angle classification when they were added to the model (Table 4).
Table 4.
Summary of Multiple Stepwise Logistic Regression Analysis for Variables Predicting Gingival Recession Development at T5a
|
|
B |
SE |
P
|
OR |
95% CI |
| Constant | 4.2 | 3.3 | |||
| Orthodontic treatment (yes) | 0.2 | 0.6 | .74 | 1.2 | 0.4–3.7 |
| Treatment type (extraction) | 0.4 | 0.6 | .43 | 1.6 | 0.5–4.5 |
| Fixed lingual retainer (yes) | 0.3 | 0.5 | .61 | 1.3 | 0.5–3.5 |
| Gender (male) | 0.8 | 0.4 | .05 | 2.3 | 1.0–5.3 |
| Age at T5 | −0.3 | 0.2 | .11 | 0.8 | 0.6–1.1 |
| Little irregularity index at T0b | 0.0 | 0.1 | .78 | 1.0 | 0.9–1.2 |
| Overbite at T0 | −0.1 | 0.2 | .70 | 0.9 | 0.7–1.3 |
| Overjet at T0 | −0.2 | 0.1 | .15 | 0.9 | 0.7–1.1 |
| Angle Class II | 0.1 | 0.4 | .75 | 1.2 | 0.5–2.7 |
Negelkerke Pseudo R2 = 0.107; P =.268; 70% correctly classified cases.
T0 indicates before treatment; T5, 5 years after debonding; B, logistic coefficient; SE, standard error; P, significance level; OR, odds ratio; 95% CI, 95% confidence interval.
DISCUSSION
The aim of this investigation was to evaluate the long-term influence of fixed lingual retainers on the development of gingival recession during the retention period in orthodontically treated patients. The present results did not lead to rejection of the first null hypothesis since no significant differences were detected in the prevalence of labial gingival recession in patients with or without fixed lingual retainers 5 years after orthodontic treatment. Hence, fixed lingual retainers per se did not seem to promote development of labial recession in the mandibular intercanine region. They did, however, promote calculus accumulation, as the patients with fixed lingual retainers had significantly more calculus than those without any retention appliance.
The existing evidence on the effect of fixed retainers on gingival health is contradictory. Short- and long-term investigations showed that fixed mandibular lingual retainers had no detrimental effect on periodontal health8,15 or marginal bone,16 while other studies found higher calculus accumulation and increased incidence of gingival recession.2,6 According to a recent systematic review, it was uncertain whether periodontal outcomes and presence of calculus differ between different retainer regimens, but the evidence was of low quality.11 It is important to note that the included studies compared orthodontically treated groups with different retention protocols, but none included a group without any kind of mandibular retention. In the present study, the no-retainer and the fixed-retainer groups showed no differences regarding age, gender, Angle classification, type of treatment, or duration of treatment and retention. In that way, some of the known predisposing factors were eliminated. Excluding confounders such as hygiene and diet regimens that were not evaluated, the only difference between the groups at debonding until the 5-year follow-up was the presence or absence of a fixed lingual retainer. Therefore, the periodontal changes observed at the 5-year follow-up may be attributed mainly to the effects of the retainer.
Cross-sectional and cohort studies clearly show increases of gingival recession with age.17–19 This was evident in all three groups in the present study. The significant increase occurred between debonding and 5-year follow-up in the experimental groups, and between 15 and 21 years of age in the control group; the increase during orthodontic treatment was not significant. It can be argued that the significant increase in gingival recession during retention is a delayed effect of orthodontic treatment. There is weak evidence that slight worsening of periodontal status occurs after orthodontic therapy.20 However, the significant increase in the nontreated, control group during the same time interval can hardly be attributed to the detrimental effect of orthodontic appliances. Despite the tendency for more gingival recession in the experimental groups, no significant differences could be observed between the three groups at T5. Thus, the second null hypothesis was also not rejected. It is probable that the development of recession cannot be solely attributed to orthodontic treatment or the presence of a fixed lingual retainer, but should be regarded as a multifactorial phenomenon.
The control group in this study was chosen from longitudinal growth material with defined 3-year follow-up intervals. Despite attempts to match ages with the experimental groups, the control subjects were significantly older at T5, and the observation period between T1 and T5 was significantly longer. As these were untreated individuals, they had more subjects with Angle Class I occlusion, showed more incisor irregularity at T1 and T5, and had larger overbite than the treated patients. Although statistically significant, the clinical importance of these differences is questionable. On the other hand, according to the regression analysis, none of these factors influenced the development of gingival recession. The results from the regression analysis showed also that neither gender nor treatment with or without extractions was associated with the development of recession. This confirms previous studies,5,6,21 which concluded that extraction is not an independent etiological factor in developing gingival recession.
Some studies have reported distribution of recession sites per tooth type. It was found that mandibular incisors were particularly prone to develop recession.3–6,9,18 In a population of orthodontically treated patients with fixed lingual retainers 5 years after treatment, the highest recession frequency was registered for the central incisors, then for the canines, and least for the mandibular lateral incisors.5 The present study showed that canines in the group without retainers had the highest frequency, followed by canines and central incisors in the retainer group. However, the differences were not statistically significant. A recent study showed large increases in crown length of the canines approximately 7 years after orthodontic treatment.21 Crown length was not measured in the current study, so the results cannot be directly compared. Nevertheless, the increased prevalence of canine recession could be due to lingual tipping in the absence of retainers or it could be an incidental finding, as these canines had the highest recession frequency—also before treatment. The only tooth with a significantly higher frequency of recession was the mandibular left central incisor in the retainer group. As this finding was present before and immediately after treatment and at the 5-year follow-up, it can hardly be attributed to the orthodontic treatment. In view of the aforementioned findings, it was concluded that orthodontically treated patients with bonded fixed lingual retainers are not at a higher risk of developing recession on incisors or canines.
Studies that investigated periodontal health in patients with fixed lingual retainers15,22 found slightly more pronounced plaque accumulation and calculus formation, but no overall negative effect on periodontal health. Also in the current study, calculus accumulation was significantly higher in the retainer group, but professional plaque and calculus removal and maintenance of good oral hygiene could improve the periodontal condition.
Retrospective studies, such as the present one, have drawbacks. The evaluation of recession and calculus accumulation in this study was limited to visual inspection on color photographs and plaster models. Pocket depths and gingival bleeding could not be evaluated, and no information was collected regarding dietary and hygiene regimens from the patients. However, the study has advantages. To our knowledge, this is the first study to assess the prevalence of gingival recession in treated patients with and without fixed lingual retainers 5 years after therapy and compare it with untreated control subjects. All three groups derived from the same population; they were matched as much as possible by age, gender, and occlusal characteristics; and they were treated in the same clinic. Both the advantages and disadvantages must be taken into consideration when interpreting the results.
CONCLUSIONS
-
•
Within the limitations of this study, the long-term presence of fixed lingual retainers did not increase the development of mandibular gingival recession, but did increase the accumulation of calculus.
-
•
The prevalence of gingival recession in patients 5 years after orthodontic treatment, with and without retainers, was similar to the prevalence in untreated individuals of the same age.
REFERENCES
- 1.Wennstrom JL ZG, Pini Prato GP. Mucogingival therapy—periodontal plastic surgery. In: Lindhe J LN, Karring T, editors. Clinical Periodontology and Implant Dentistry Vol 2. Oxford, United Kingdom: Blackwell Munksgaard; 2008. 958. [Google Scholar]
- 2.Levin L, Samorodnitzky-Naveh GR, Machtei EE. The association of orthodontic treatment and fixed retainers with gingival health. J Periodontol. 2008;79:2087–2092. doi: 10.1902/jop.2008.080128. [DOI] [PubMed] [Google Scholar]
- 3.Renkema AM, Fudalej PS, Renkema AA, Abbas F, Bronkhorst E, Katsaros C. Gingival labial recessions in orthodontically treated and untreated individuals: a case-control study. J ClinPeriodontol. 2013;40:631–637. doi: 10.1111/jcpe.12105. [DOI] [PubMed] [Google Scholar]
- 4.Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008;134:652–656. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- 5.Renkema AM, Fudalej PS, Renkema A, Kiekens R, Katsaros C. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofacial Orthop. 2013;143:206–212. doi: 10.1016/j.ajodo.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Pandis N, Vlahopoulos K, Madianos P, Eliades T. Long-term periodontal status of patients with mandibular lingual fixed retention. Eur J Orthod. 2007;29:471–476. doi: 10.1093/ejo/cjm042. [DOI] [PubMed] [Google Scholar]
- 7.Artun J, Spadafora AT, Shapiro PA. A. 3-year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod. 1997;19:501–509. doi: 10.1093/ejo/19.5.501. [DOI] [PubMed] [Google Scholar]
- 8.Booth FA, Edelman JM, Proffit WR. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop. 2008;133:70–76. doi: 10.1016/j.ajodo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 9.Vasconcelos G, Kjellsen K, Preus H, Vandevska-Radunovic V, Hansen BF. Prevalence and severity of vestibular recession in mandibular incisors after orthodontic treatm-ent. Angle Orthod. 2012;82:42–47. doi: 10.2319/021411-108.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joss-Vassali I, Grebenstein C, Topouzelis N, Sculean A, Catsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13:127–141. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 11.Westerlund A, Daxberg EL, Liljegren A, et al. Stability and side effects of orthodontic retainers—a systematic review. Dentistry. 2014;4(9):258. doi: 10.4172/2161-1122.1000258. [DOI] [Google Scholar]
- 12.Corbett AI, Leggitt VL, Angelov N, Olson G, Caruso JM. Periodontal health of anterior teeth with two types of fixed retainers. Angle Orthod. 2015;85:699–705. doi: 10.2319/060314-398.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Axelsson S, Kjaer I, Bjornland T, Storhaug K. Longitudinal cephalometric standards for the neurocranium in Norwegians from 6 to 21 years of age. Eur J Orthod. 2003;25:185–198. doi: 10.1093/ejo/25.2.185. [DOI] [PubMed] [Google Scholar]
- 14.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 15.Heier EE, De Smit AA, Wijgaerts IA, Adriaens PA. Periodontal implications of bonded versus removable retainers. Am J Orthod.Dentofacial.Orthop. 1997;112:607–616. doi: 10.1016/s0889-5406(97)70225-7. [DOI] [PubMed] [Google Scholar]
- 16.Westerlund A, Oikimoui C, Ransjö M, Ekestubbe A, Bresin A, Lund H. Cone-beam computed tomographic evaluation of the long-term effects of orthodontic retainers on marginal bone levels. Am J Orthod Dentofacial Orthop. 2017;151:74–81. doi: 10.1016/j.ajodo.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 17.Loe H, Anerud A, Boysen H. The natural history of periodontal disease in man: prevalence, severity, and extent of gingival recession. J Periodontol. 1992;63:489–495. doi: 10.1902/jop.1992.63.6.489. [DOI] [PubMed] [Google Scholar]
- 18.Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J Periodontol. 2004;75:1377–1386. doi: 10.1902/jop.2004.75.10.1377. [DOI] [PubMed] [Google Scholar]
- 19.Thomson WM, Broadbent JM, Poulton R, Beck JD. Changes in periodontal disease experience from 26 to 32 years of age in a birth cohort. J Periodontol. 2006;77:947–954. doi: 10.1902/jop.2006.050319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139:413–422. doi: 10.14219/jada.archive.2008.0184. [DOI] [PubMed] [Google Scholar]
- 21.Villard NM, Patcas R. Does the decision to extract influence the development of gingival recession? A retrospective long-term evaluation. J Orofac Orthop. 2015;76:476–492. doi: 10.1007/s00056-015-0308-2. [DOI] [PubMed] [Google Scholar]
- 22.Dietrich P, Patcas R, Pandis N, Eliades T. Long-term follow-up of maxillary fixed retention: survival rate and periodontal health. Eur J Orthod. 2015;37:37–42. doi: 10.1093/ejo/cju001. [DOI] [PubMed] [Google Scholar]


