Abstract
Objective:
To determine the effects of extraction and the number of teeth extracted on changes in occlusal function by measuring occlusal contact area and force before and after orthodontic treatment with a fixed appliance.
Materials and Methods:
Female patients treated with a fixed appliance were divided into nonextraction (n = 36), two maxillary premolar extraction (n = 31), and four premolar extraction (n = 18) groups. Bite pressure-sensitive films were used to analyze the occlusal contact area and force. Measurements were performed before treatment (Pre-Tx), immediately afterward (After-Tx), and 2 years later (2Y After-Tx). The data were analyzed using a linear mixed model and the post hoc Bonferroni test.
Results:
The occlusal contact area and force after treatment decreased significantly compared with Pre-Tx values but were increased 2 years later in all groups. There were no significant differences in occlusal contact area or force during the entire observation period among the three groups (P > .05). The occlusal contact area and force in the nonextraction and two maxillary premolar extraction groups recovered to Pre-Tx levels 2 years later (P > .05). The occlusal contact area in the four premolar extraction group was significantly lower than the Pre-Tx level after 2 years of retention (P < .05).
Conclusions:
The occlusal contact area and force showed a tendency to decrease immediately after treatment and then gradually increase to pretreatment levels during the observation period. However, the occlusal contact area did not recover fully after 2 years in the four premolar extraction group.
Keywords: Premolar extraction, Long-term retention, Occlusal contact area, Occlusal force
INTRODUCTION
The goal of orthodontic treatment is to achieve functional occlusion, an esthetic profile, and stable results in the long term.1 For patients with severe crowding or lip protrusion, the orthodontist may include an extraction protocol in the treatment plan. Although a decision to include extractions and about which teeth to be extracted may differ depending on the patient,2,3 the most common choice is first premolars. Extractions are often unavoidable, and the procedure used and number of teeth extracted have substantial effects on the duration of treatment and outcome, including final esthetics and occlusion.4
Masticatory performance is primarily determined by the teeth, masticatory muscles, and jaw movement.5 Orthodontists can play a role in improving masticatory function by aligning the teeth. Recovery of such function can be evaluated by assessing factors affecting occlusal contact, such as occlusal contact points, occlusal contact area, and distribution of occlusal contact.6 According to Owens et al.,7 a wider occlusal contact area helps with grinding of food, and a wider posterior contact area is crucial for masticatory function.
Occlusal function in patients treated by extraction of varying numbers of teeth has been investigated using dental casts.8 However, this method, combined with the peer assessment rating index and the American Board of Orthodontics objective grading system, is only useful for static evaluation.9 One study suggested possible discrepancies between results from dental casts and the actual occlusal contact during functional occlusion.10
The Dental Prescale system (Fuji Film Corp, Tokyo, Japan) has been widely used to evaluate occlusal contact area and force due to its simplicity and objectivity,11–13 but the scope of the research using this system has been limited to posttreatment changes during short-term follow-up over 1 year without consideration of pretreatment records.14 Similar studies included either patients treated with extraction alone15 or a small number of patients.16
The purpose of this 2-year follow-up study was to evaluate changes in occlusal contact area and force in nonextraction, two maxillary premolar extraction, and four premolar extraction cases. Measurements were taken before, immediately after, and 2 years after treatment with a fixed orthodontic appliance. The effects of premolar extractions on changes in occlusal function were assessed.
MATERIALS AND METHODS
Subjects
Patients treated with a fixed appliance in the Department of Orthodontics at Gangnam Severance Dental Hospital between June 2008 and September 2013 were considered for the study. The subjects were included if they met the following criteria: female sex; age <40 years; eruption of second molars completed to occlusion before treatment; no missing teeth; no previous extractions except for third molars, two maxillary premolar extractions, or four premolar extractions, with one premolar extraction per quadrant; and no temporomandibular joint disorder or record of orthognathic surgery.
Eligible subjects were divided into a nonextraction group (non-ext, n = 36), a two maxillary premolar extraction group (2 ext, n = 18), and a four premolar extraction group (4 ext, n = 31). Cephalometric measurements for all subjects before and after treatment are shown in Table 1. The subjects were randomly assigned to three orthodontists who each had at least 10 years of clinical experience.
Table 1.
Subject Number, Age and Cephalometric Measurements Before and After Treatmenta
|
|
Non-ext (n = 36) |
4-ext (n = 31) |
2-ext (n = 18) |
P Value |
||||
| Pre-Tx |
Post-Tx |
Pre-Tx |
Post-Tx |
Pre-Tx |
Post-Tx |
Pre-Tx |
Post-Tx |
|
| Age (y) | 20.3 ± 8.1 | 22.2 ± 7.9 | 20.2 ± 6.0 | 22.5 ± 6.0 | 19.0 ± 5.2 | 21.3 ± 5.1 | .808 | .818 |
| Treatment period (mo) | 23.0 ± 7.1w | 28.1 ± 7.5x | 27.7 ± 7.8 | .012* | ||||
| SNA (°) | 81.0 ± 2.7 | 81.1 ± 2.7 | 81.0 ± 3.4 | 80.9 ± 3.5 | 81.5 ± 2.5 | 81.1 ± 2.3 | .79 | .788 |
| SNB (°) | 78.3 ± 3.5 | 78.4 ± 3.6 | 77.4 ± 4.2 | 77.1 ± 4.2 | 76.0 ± 2.6 | 75.8 ± 2.5 | .09 | .051 |
| ANB (°) | 2.6 ± 2.5w | 2.6 ± 2.5y | 3.5 ± 2.4 | 3.8 ± 2.2 | 5.5 ± 2.5x | 5.3 ± 2.3z | .001** | .001** |
| APDI | 84.7 ± 6.5 | 84.4 ± 6.3 | 82.3 ± 5.4 | 81.4 ± 4.8 | 80.9 ± 7.2 | 80.5 ± 6.5 | .083 | .033* |
| SN to MP (°) | 35.1 ± 6.2 | 35.1 ± 6.8 | 38.9 ± 8.4 | 38.6 ± 8.7 | 38.7 ± 6.1 | 39.6 ± 6.4 | .063 | .063 |
| Gonial angle (°) | 119.6 ± 7.8 | 119.6 ± 8.5 | 121.7 ± 7.2 | 120.8 ± 7.2 | 122.5 ± 6.6 | 122.1 ± 6.8 | .34 | .485 |
| Bjork sum (°) | 395.1 ± 6.2 | 395.8 ± 6.9 | 398.9 ± 8.4 | 398.6 ± 8.7 | 398.7 ± 6.1 | 399.5 ± 6.4 | .063 | .148 |
| ODI | 72.6 ± 8.6 | 71.9 ± 10.0 | 69.1 ± 5.4w | 71.6 ± 6.5 | 76.0 ± 10.1x | 74.2 ± 8.6 | .016* | .557 |
non-ext indicates nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars; APDI, anteroposterior dysplasia index; ODI, overbite depth index.
P < .05; ** P < .01; Scheffe post hoc test, w < x, y < z
Ethical approval for this study was obtained from the Institutional Review Board of Gangnam Severance Dental Hospital, Yonsei University (IRB No. 3-2016-0203).
Measurement of Occlusal Contact Area and Force
Occlusal contact area and force were determined before treatment (Pre-Tx), immediately after the fixed appliance was removed (After-Tx), and 2 years later (2Y After-Tx). Out of four different-sized pressure-sensitive films (Dental Prescale 50H, type R), the one best fitting the arch of each subject was selected to ensure complete coverage of the contact area. The subjects were asked to bite the film with a maximal clenching force for 5 seconds while maintaining a natural head position. The films were read with a CCD camera (Occluzer FPT 707, Fuji Film Corp.) to determine the occlusal contact area and force with a resolution of 0.1 mm2 and 0.1 N, respectively.
Skeletal Pattern Analysis
A lateral cephalometric radiograph in the maximum intercuspal position was recorded using PMPROMAX (Planmeca, Helsinki, Finland) for each subject at her first visit. One orthodontist carried out all measurements using V-ceph 3.5 (CyberMed, Seoul, Korea) with a resolution of 0.01° (angular) and 0.01 mm (linear). The measurements were repeated in 20 randomly selected subjects by an examiner, and the intraexaminer correlation coefficient was used for the analysis of the method error. The criteria for classification of malocclusion were determined according to a previous study.17
Statistical Analysis
We determined that a sample size of 18 participants in each group was sufficient to detect an effect size of 0.2 and a correlation between repeated measures of 0.5 at a significance level of .05 with 80% power. Mean (± standard deviation) cephalometric measurements were calculated before and after treatment. One-way analysis of variance was used to test the statistical significance of the cephalometric measurements, treatment time, and objective grading system score of casts after treatment, and post hoc tests were performed using Scheffe's method. Classification of malocclusion in each group was analyzed using the χ2. A linear mixed model was used to test the variations in occlusal contact area and force in each group during the study period and to compare them among the groups. The mandibular plane and gonial angles, which have been shown to affect occlusal contact area and force in previous studies, were designated as covariates.18 The post hoc test for the linear mixed model was performed using the Bonferroni test. Statistical analysis was conducted using SPSS version 21.0 (IBM Corp, Armonk, NY).
RESULTS
The intraexaminer correlation coefficient of skeletal pattern analysis was 0.89 (95% confidence interval, 0.87–0.91), indicating high repeatability of the measurements. The classification of malocclusion before treatment (P > .05, Table 2) and objective grading system scores of casts after treatment (P = .855) were not significantly different among groups.
Table 2.
Classification of Malocclusion in Each Group Before Treatmenta
|
|
Non-ext (n = 36) |
4-ext (n = 31) |
2-ext (n = 18) |
P Value |
| Crowdingb | 29 | 21 | 15 | .347 |
| Open bitec | 1 | 4 | 1 | .567 |
non-ext indicates nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars;
Crowding indicates that the subject had more than four dislocated teeth on each maxillary and mandibular arch;
Open bite indicates that the subject had over –3 mm overbite at centric occlusion.
There was no significant difference in occlusal contact area or force among the three groups before treatment (P > .05, Tables 3 and 4).
Table 3.
Time-Dependent Estimated Mean, Standard Error, and P Value for Occlusal Contact Area Using a Linear Mixed Model (mm2)a
| Group Time |
Estimated meanb (SE) |
Overall P Value |
||
| Non-ext |
4-ext |
2-ext |
||
| Pre-Tx | 11.5(1.0)x | 12.9(1.1)x | 10.6(1.6)x | Group: .451 |
| Post-Tx | 6.4(0.5)y | 4.8(0.6)y | 5.0(0.8)y | Time: <.001*** |
| 2Y after Tx | 10.7(0.8)x | 9.4(0.8)z | 8.9(1.4)x | Group × time: .397 |
SE indicates standard error; non-ext, nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars; Tx, treatment.
Estimated means with different superscript letters are significantly different in each group (P < .05).
P < .05; ** P < .01; *** P < .001.
Table 4.
Time-Dependent Estimated Mean, Standard Error, and P Value for Occlusal Force Using a Linear Mixed Model (N)a
| Group Time |
Estimated meanb (SE) |
Overall P Value |
||
| Non-ext |
4-ext |
2-ext |
||
| Pre-Tx | 434.1 (35.0)y | 462.8 (37.8)y | 409.2 (54.0)y | Group: .671 |
| Post-Tx | 289.5 (23.6)z | 229.5 (25.5)z | 250.8 (33.4)z | Time: <.001*** |
| 2Y after Tx | 425.2 (30.8)y | 384.3 (33.2)y | 405.0 (56.5)y | Group × time: .582 |
SE indicates standard error; non-ext, nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars; Tx, treatment.
Estimated means with different superscript letters are significantly different in each group (P < .05).
P < .05; ** P < .01; *** P < .001.
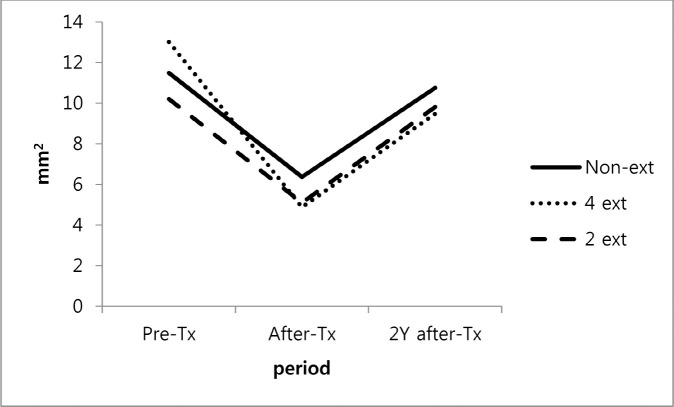
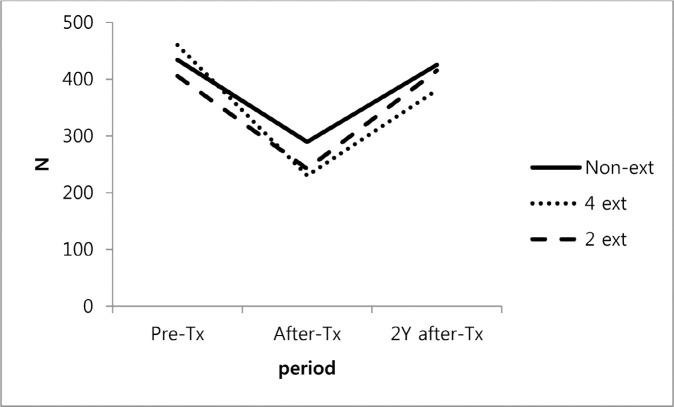
In all groups, the After-Tx occlusal contact area and force were significantly lower than the Pre-Tx values but increased 2 years later (Figures 1 and 2). There was no significant difference in measurements among the three groups for any period of observation, and the tendency to recover occlusal contact area and force was similar during the 2 years (P > .05, Tables 3 and 4).
Figure 1.
Changes in occlusal contact area: Non-ext indicates nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars; Tx, treatment.
Figure 2.
Changes in bite force. Non-ext indicates nonextraction group; 4-ext, extraction of two maxillary and two mandibular premolars; 2-ext, extraction of two maxillary premolars; Tx, treatment.
In all three groups, the After-Tx occlusal contact areas were significantly smaller than the corresponding Pre-Tx values (P < .05). However, after 2 years, the occlusal contact area had increased significantly (P < .05) and there was no significant difference between the Pre-Tx and 2Y after-Tx values (P > .05), except in the 4-ext group, in which the occlusal contact area failed to reach the Pre-Tx level even 2 years later (P < .05, Table 3).
Like the occlusal contact area, the occlusal force increased significantly during 2 years of follow-up (P < .05) after an initial posttreatment decrease (P < .05), and no significant differences were found between Pre-Tx and 2Y After-Tx in any of the three groups (P > .05, Table 4).
DISCUSSION
The Dental Prescale system assesses occlusal contact area and force and has been widely used to evaluate occlusal function. This system uses a flexible pressure-sensitive film of 97-μm thickness, and contact marks created by the patient's teeth in occlusion are scanned for analysis. The system is not affected by intraoral temperature or humidity, nor is it affected by the velocity or duration of pressure.19 Moreover, its performance is not dependent on the proficiency of the examiner, and it is simple to use for objective evaluation of occlusal function.12
In a previous study, occlusal contact area and force were reported to be greater in male patients than in female patients. Further, the occlusal contact area was reported to be larger in patients aged ≥40 years, while there was no statistically significant difference in the occlusal contact area among the three age groups (11–20, 21–30, and 31–40 years).18 Therefore, the current study only included female patients younger than 40 years. In addition, taking into account studies suggesting a correlation between vertical skeletal pattern, occlusal force, and occlusal contact area, the mandibular plane and gonial angles were incorporated into the linear mixed model as covariates.17,18 Patients with a temporomandibular joint disorder often have poor masticatory function.20 Therefore, patients diagnosed with temporomandibular joint disorders based on the questionnaires administered at the first visit or clinical and radiographic examination were excluded from the study.
The pretreatment ANB value was significantly higher in the 2-ext group than in the non-ext group. This implies that extraction in the maxillary arch was more frequently performed in patients with skeletal Class II malocclusion. The lower pretreatment overbite depth index value in the 4-ext group might be associated with lingual tipping of the incisors according to the “drawbridge principle” described by Janson et al.21 However, there was no significant difference in pretreatment occlusal contact area and force among the three groups (non-ext, 2-ext, 4-ext).
The After-Tx occlusal contact area and force were reduced to approximately half the Pre-Tx values in a manner similar to that obtained in a study using a three-dimensional digital model.22 Nonetheless, the After-Tx occlusal contact area and force gradually recovered to Pre-Tx levels by “occlusal settling,” regardless of the extraction procedure used or type of malocclusion present. However, the 2Y After-Tx occlusal contact area and force values in the non-ext group were 10.7 mm2 and 425.2 N, respectively, and were still lower than the average occlusal contact area and force in patients with normal occlusion as reported in a previous study (24.2 mm2 and 744.5 N, respectively).18 The results of the present study indicate that recovery of occlusion may take more than 2 years after treatment, which is longer than the period described previously.18
The occlusal contact area in the 4-ext group did not fully recover to its initial pretreatment state by the end of the 2-year observation period. This is in contrast with a previous study that reported finding no significant difference in occlusal function between four premolar extractions and nonextraction following treatment.14 After comparing the occlusal contact areas of the groups 1 year after treatment, that study concluded that the reduction in occlusal contact area caused by premolar extraction did not have a clinically significant effect on occlusal function.14 However, in the present study, the 2Y After-Tx occlusal contact area in the 4-ext group was significantly reduced compared with the Pre-Tx value. Considering that the occlusal contact area has a larger impact on masticatory performance than occlusal force,5 this finding suggests that four premolar extractions could impair occlusal function. Further, the results of this study support assessment of occlusal contact using the American Board of Orthodontics objective grading system, in which the score for four premolar extractions is lower than that for two maxillary premolar extractions.8
In the 2-ext group, the occlusal contact area was restored to a level equivalent to that in the non-ext group; however, the occlusal force exceeded its Pre-Tx value after 2 years. Although the Pre-Tx occlusal contact area and force in the 2-ext group were lower than that in the 4-ext group, the 2Y After-Tx values were higher in the 2-ext group than in the 4-ext group. The current findings are consistent with those of studies based on the peer assessment rating index and the American Board of Orthodontics objective grading system in which higher scores for occlusal contact were recorded for two maxillary premolar extractions than four premolar extractions in patients with skeletal Class II malocclusion.8 This could be one of the reasons why two maxillary premolar extraction is now becoming a more common orthodontic treatment.3
There are several limitations to the Dental Prescale system that should be taken into consideration. The thickness of the pressure-sensitive film (97 μm) can prevent recording of areas of actual contact (<50 μm) and near contact (50–350 μm) during mastication.7,23–26 Further, a pressure >5 MPa is required to mark contact points on the film, and measurements can deviate from the actual occlusal contact area and force, thereby causing significant errors. This might explain why the occlusal contact area appeared larger than the actual value by 10-fold in a study using a three-dimensional model.22 In addition, given that a spatial resolution of 0.25 × 0.25 mm2 is used in the CCD camera, contact points smaller than the spatial resolution cannot be accurately represented.27
In summary, variation in occlusal function was investigated in a 2-year posttreatment follow-up study by determining occlusal contact area and force. It was found that the occlusal contact area and force decreased immediately after treatment but recovered to initial values after 2 years in the nonextraction and two maxillary premolar extraction groups. In contrast, the occlusal contact area in the four premolar extraction group was not fully recovered after 2 years; this finding suggests a decrease in occlusal function that should be taken into account when planning orthodontic treatment. Long-term studies extending beyond 2 years are necessary to further determine the recovery of occlusion after premolar extraction.
CONCLUSION
-
•
Evaluation of occlusal contact area and force using the Dental Prescale system revealed a tendency for occlusal function to recover to its initial value after 2 years of observation despite premolar extraction.
-
•
The occlusal contact area may not be fully regained during this time if four premolar extraction is performed.
-
•
Long-term occlusal function should be considered when contemplating premolar extraction during orthodontic treatment. A recovery period of more than 2 years may be required to achieve normal occlusal function after treatment.
REFERENCES
- 1.Haydar B, Cier S, Saatçi P. Occlusal contact changes after the active phase of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102:22–28. doi: 10.1016/0889-5406(92)70011-x. [DOI] [PubMed] [Google Scholar]
- 2.Proffit WR. Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthod. 1994;64:407–414. doi: 10.1043/0003-3219(1994)064<0407:FROEFA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Janson G, Maria FRT, Bombonatti R. Frequency evaluation of different extraction protocols in orthodontic treatment during 35 years. Prog Orthod. 2014;15:1. doi: 10.1186/s40510-014-0051-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vig PS, Orth D, Weintraub JA, Brown C, Kowalski CJ. The duration of orthodontic treatment with and without extractions: a pilot study of five selected practices. Am J Orthod Dentofacial Orthop. 1990;97:45–51. doi: 10.1016/S0889-5406(05)81708-1. [DOI] [PubMed] [Google Scholar]
- 5.Lepley CR, Throckmorton GS, Ceen RF, Buschang PH. Relative contributions of occlusion, maximum bite force, and chewing cycle kinematics to masticatory performance. Am J Orthod Dentofacial Orthop. 2011;139:606–613. doi: 10.1016/j.ajodo.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 6.Imamura Y, Sato Y, Kitagawa N, et al. Influence of occlusal loading force on occlusal contacts in natural dentition. J Prosthodont Res. 2015;59:113–120. doi: 10.1016/j.jpor.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Owens S, Buschang PH, Throckmorton GS, Palmer L, English J. Masticatory performance and areas of occlusal contact and near contact in subjects with normal occlusion and malocclusion. Am J Orthod Dentofacial Orthop. 2002;121:602–609. doi: 10.1067/mod.2002.122829. [DOI] [PubMed] [Google Scholar]
- 8.Cansunar HA, Uysal T. Comparison of orthodontic treatment outcomes in nonextraction, 2 maxillary premolar extraction, and 4 premolar extraction protocols with the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2014;145:595–602. doi: 10.1016/j.ajodo.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Lee S-M, Lee J-W. Computerized occlusal analysis: correlation with occlusal indexes to assess the outcome of orthodontic treatment or the severity of malocculusion. Korean J Orthod. 2016;46:27–35. doi: 10.4041/kjod.2016.46.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazit E, Lieberman MA. Occlusal contacts following orthodontic treatment: measured by a photocclusion technique. Angle Orthod. 1985;55:316–320. doi: 10.1043/0003-3219(1985)055<0316:OCFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Okiyama S, Ikebe K, Nokubi T. Association between masticatory performance and maximal occlusal force in young men. J Oral Rehabil. 2003;30:278–282. doi: 10.1046/j.1365-2842.2003.01009.x. [DOI] [PubMed] [Google Scholar]
- 12.Ando K, Fuwa Y, Kurosawa M, Kondo T, Goto S. Bite force measurement system using pressure-sensitive sheet and silicone impression material. Dent Mater J. 2009;28:212–218. doi: 10.4012/dmj.28.212. [DOI] [PubMed] [Google Scholar]
- 13.Hidaka O, Iwasaki M, Saito M, Morimoto T. Influence of clenching intensity on bite force balance, occlusal contact area, and average bite pressure. J Dent Res. 1999;78:1336–1344. doi: 10.1177/00220345990780070801. [DOI] [PubMed] [Google Scholar]
- 14.Choi Y-J, Chung CJ, Kim K-H. Changes in occlusal force and occlusal contact area after orthodontic treatment. Korean J Orthod. 2010;40:176–183. [Google Scholar]
- 15.Sultana M, Yamada K, Hanada K. Changes in occlusal force and occlusal contact area after active orthodontic treatment: a pilot study using pressure-sensitive sheets. J Oral Rehabil. 2002;29:484–491. doi: 10.1046/j.1365-2842.2002.00849.x. [DOI] [PubMed] [Google Scholar]
- 16.Makino E, Nomura M, Motegi E, et al. Effect of orthodontic treatment on occlusal condition and masticatory function. Bull Tokyo Dent Coll. 2014;55:185–197. doi: 10.2209/tdcpublication.55.185. [DOI] [PubMed] [Google Scholar]
- 17.Kitafusa Y. Application of “prescale” as an aid to clinical diagnosis in orthodontics. Bull Tokyo Dent Coll. 2004;45:99–108. doi: 10.2209/tdcpublication.45.99. [DOI] [PubMed] [Google Scholar]
- 18.Yoon H-R, Choi Y-J, Kim K-H, Chung C. Comparisons of occlusal force according to occlusal relationship, skeletal pattern, age and gender in Koreans. Korean J Orthod. 2010;40:304–313. [Google Scholar]
- 19.Suzuki T, Watanabe T, Yoshitomi N, Ishinabe S, Kumagai H, Uchida T. Evaluation of a new measuring system for occlusal force with pressure sensitive sheet. J Jpn Prosthodont Soc. 1994;38:966–973. [Google Scholar]
- 20.Sato S, Ohta M, Sawatari M, Kawamura H, Motegi K. Occlusal contact area, occlusal pressure, bite force, and masticatory efficiency in patients with anterior disc displacement of the temporomandibular joint. J Oral Rehabil. 1999;26:906–911. doi: 10.1046/j.1365-2842.1999.00481.x. [DOI] [PubMed] [Google Scholar]
- 21.Janson G, Maria FRT, Barros SEC, de Freitas MR, Henriques JFC. Orthodontic treatment time in 2- and 4-premolar-extraction protocols. Am J Orthod Dentofacial Orthop. 2006;129:666–671. doi: 10.1016/j.ajodo.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 22.Lee H, Kim M, Chun Y-S. Comparison of occlusal contact areas of class I and class II molar relationships at finishing using three-dimensional digital models. Korean J Orthod. 2015;45:113–120. doi: 10.4041/kjod.2015.45.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yurkstas A, Manly R. Measurement of occlusal contact area effective in mastication. Am J Orthod. 1949;35:185–195. doi: 10.1016/0002-9416(49)90028-7. [DOI] [PubMed] [Google Scholar]
- 24.Gurdsapsri W, Ai M, Baba K, Fueki K. Influence of clenching level on intercuspal contact area in various regions of the dental arch. J Oral Rehabil. 2000;27:239–244. doi: 10.1046/j.1365-2842.2000.00527.x. [DOI] [PubMed] [Google Scholar]
- 25.Razdolsky Y, Sadowsky C, BeGole EA. Occlusal contacts following orthodontic treatment: a follow-up study. Angle Orthod. 1989;59:181–185. doi: 10.1043/0003-3219(1989)059<0181:OCFOTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Sakaguchi RL, Anderson GC, DeLong R. Digital imaging of occlusal contacts in the intercuspal position. J Prosthodont. 1994;3:193–197. doi: 10.1111/j.1532-849x.1994.tb00154.x. [DOI] [PubMed] [Google Scholar]
- 27.Kwon HK, Yoo JH, Kwon YS, Kim BI. Comparison of bite force with dental prescale and unilateral bite force recorder in healthy subjects. J Korean Acad Prosthodont. 2006;44:103–111. [Google Scholar]