Abstract
Objective:
To determine whether, in Class I borderline cases, experienced orthodontists choose nonextraction treatment more frequently than do orthodontists with less experience. A secondary aim was to evaluate whether clinicians' gender and place of education play a role in extraction decision making.
Materials and Methods:
An online survey was developed using three Class I borderline patient cases. The survey included questions about clinicians' demographics as well as questions about the selected cases. The survey was distributed to approximately 2000 clinicians through the American Association of Orthodontics.
Results:
Of the 253 responses collected, a trend was observed wherein clinicians with more than 15 years of experience preferred an extraction treatment option more frequently than did clinicians with less than 5 years of experience. There was no association between gender and place of education and the decision to extract in the selected borderline cases. Crowding, patient's profile, and mandibular incisor inclination were among the top three reasons chosen by clinicians for both the extraction and nonextraction treatment decisions.
Conclusions:
A trend was observed in which clinicians with more experience chose an extraction treatment option more frequently in borderline cases than did those with less experience. Clinicians' gender did not play a role in extraction decision making.
Keywords: Extraction, Experience, Gender
INTRODUCTION
Extraction vs nonextraction orthodontic treatment for Class I borderline patients has been a subject of debate. Borderline cases have been described in different ways. Some studies focus on crowding and consider cases with 4–8 mm of crowding to be borderline.1 However, other variables such as facial profile, Bolton discrepancy, and lip prominence also influence the extraction decision. Therefore, others define borderline in broader terms as cases in which orthodontists cannot agree on whether to extract or not.2 It has been shown that, when presented with the same patient records, some clinicians choose to extract while others opt for nonextraction treatment.3,4 While different philosophies have developed over the years, the reason behind the inconsistencies in treatment plans for borderline cases is unclear.
Multiple studies have been conducted to determine why orthodontists choose extraction vs nonextraction in borderline cases. Clearly, patients' characteristics such as crowding, facial profile, lip prominence, and curve of Spee play a significant role in the decision-making process. However, clinicians' traits and experiences may also influence diagnosis and treatment planning. The significance of clinicians' traits becomes apparent when different orthodontists are given the same patient scenario. Studies show that the degree of agreement on treatment decisions is very low.3,4
Literature on which orthodontist characteristics affect treatment decisions is limited. The few studies that have looked at which clinicians' traits influence treatment decisions have usually been part of larger studies focusing on patient differences, and the data from these few studies are conflicting. Some report an association between clinicians' traits such as gender or experience while others found no relationship.5–7 Kay and Nuttall attributed the differences among clinicians to either judgmental or perceptual variations. They reported that perceptual differences result from two people interpreting the same thing differently while judgmental variations are seen when two people agree on what they see but disagree on the treatment.8 Clinicians' past experiences can influence both the perceptual as well as the judgmental aspects of the decision-making process.
The purpose of this study was to determine whether, in Class I borderline cases, experienced orthodontists choose nonextraction treatment more frequently than do orthodontists with less experience. Some patient traits will also be evaluated. A secondary aim was to evaluate the influence of other clinician characteristics such as gender and place of education to determine whether these factors were associated with the treatment decision.
MATERIALS AND METHODS
Selection of Borderline Cases
The study was approved by the institutional review board. Cases were selected from the orthodontic department graduate clinic. Inclusion criteria were orthognathic profile, Class I molar and canine classification, crowding of 4–8 mm, complete records (intraoral and extraoral photographs, lateral cephalogram, panoramic radiograph, initial models), and full permanent dentition. Cases with the following were excluded: missing teeth, abnormal tooth morphology, major dental work (endodontically treated teeth), severe caries, periodontal disease, and ankylosed teeth.
After an initial screening of 15 cases, 8 met the inclusion criteria and were selected for a pilot survey. The survey was developed using SurveyMonkey and was distributed to 16 orthodontic faculty members and 15 orthodontic residents. Questions in the pilot and final study surveys were identical. Three versions of the survey with different order of patient cases were developed to minimize order effect.
After the initial pilot survey, three patients were selected for the final study survey. These were cases in which extraction and nonextraction treatment options were distributed equally among the participating clinicians. Since clinicians with varying levels of experience could not agree on extraction vs nonextraction, it was concluded that they were borderline. These three cases were used in the survey study described. The order of their presentation in the final survey was chosen randomly (draw) and cases were presented in the same order for all participants.
Survey
The electronic survey was developed using SurveyMonkey and distributed through the American Association of Orthodontists Partners in Research program to all active AAO members who agreed to participate.
The survey consisted of two portions. Section 1: practitioner demographics (years of experience, gender, place of education, treatment philosophy, and so forth [Appendix 1]). Section 2: patients' records (initial intraoral and extraoral photographs, photos of study models, lateral cephalogram, cephalometric analysis, and panoramic radiograph). Each clinician was required to answer whether he or she preferred an extraction or nonextraction treatment for each case. If nonextraction was chosen, a follow-up question asked how space would be created for alignment. If extraction was chosen, the clinicians were asked which teeth they chose to extract (Appendix 1).
Statistical Analysis
Sample size calculation determined that to detect a difference of 40% vs 60% in the three different experience-level groups (less than 5 years, 5 to 15 years, and more than 15 years of experience) with a 0.05 significance level, 60 orthodontists would be needed in each group.
Descriptive analyses were used initially to visualize the general trends in the data. The nonparametric chi-square test was then used to determine the extraction decision association with level of experience, gender, and location of orthodontic training based on members' AAO constituency. The levels of significance were defined as 0.05.
The reasons clinicians chose a particular treatment for each case was categorized based on extraction vs nonextraction, and descriptive analysis was used to examine any trends.
Statistical analyses were performed with R statistical package (Version 2.11.1).
RESULTS
Clinicians' Demographics
The survey was distributed to 2005 clinicians. A total 253 responses were collected (13% response rate). Distribution of experience among the respondents was 28% for <5 years of experience, 32% for 5–15 years, and 40% for >15 years (Table 1), with 25% being female (Table 1). Gender was not equally distributed based on experience. In the <5-year group, 33% were female, while in the >15-year group, 16% were female. This difference in female clinicians based on experience was statistically significant (X2 = 7.08, P = .03) (Table 2).
Table 1.
Clinicians' Demographics
|
|
Respondents | Recipients |
| n (%) |
n (%) |
|
| Experience level | ||
| < 5 y | 72 (28) | 185 (9) |
| 5–15 y | 80 (32) | 803 (40) |
| >15 y | 101 (40) | 1017 (51) |
| Gender | ||
| Female | 60 (25) | 554 (28) |
| Male | 183 (75) | 1451 (72) |
| Total | 253 | 2005 |
Table 2.
Gender vs Experience
|
|
< 5 Y | >15 Y |
| Respondent Recipient | Respondent Recipient | |
| n (%) n (%) |
n(%) n(%) |
|
| Female | 23 (33) 74 (40) | 15 (16) 210 (20) |
| Male | 47 (67) 111 (60) | 80 (84) 807 (80) |
| P Value: .03 |
The demographic information for all clinicians who received the survey was obtained from the AAO. Comparing the demographics of the respondents to the entire group of the survey recipients indicated that they were relatively similar (Table 1). The main difference was that more clinicians in the <5-year experience group responded to the survey (28% respondents vs 9% of all recipients). Clinicians with >15 years of experience were less likely to respond to the survey (40% respondents vs 51% of recipients). Overall gender distribution and gender distribution with regard to experience was similar between both groups (Tables 1 and 2).
The number of responses for each case decreased from case A to B and C. Two hundred twenty-six people completed case A, but that number dropped to 195 for case B and 186 for case C. Therefore, two sets of analyses were completed: one with all the responses and one with responses only from those clinicians completing the entire survey. Gender and experience distribution was similar in both groups.
Case Analysis
Overall extraction vs nonextraction rates for each case are listed in Table 3. Most clinicians preferred nonextraction treatment. The percentage of extraction vs nonextraction decisions were similar for cases A and C; however, the number of extraction decisions was higher in case B.
Table 3.
Case Summary
|
|
Extraction | Nonextraction |
| n % |
n % |
|
| Case A | 34 15 | 192 85 |
| Case B | 58 30 | 137 70 |
| Case C | 37 20 | 149 80 |
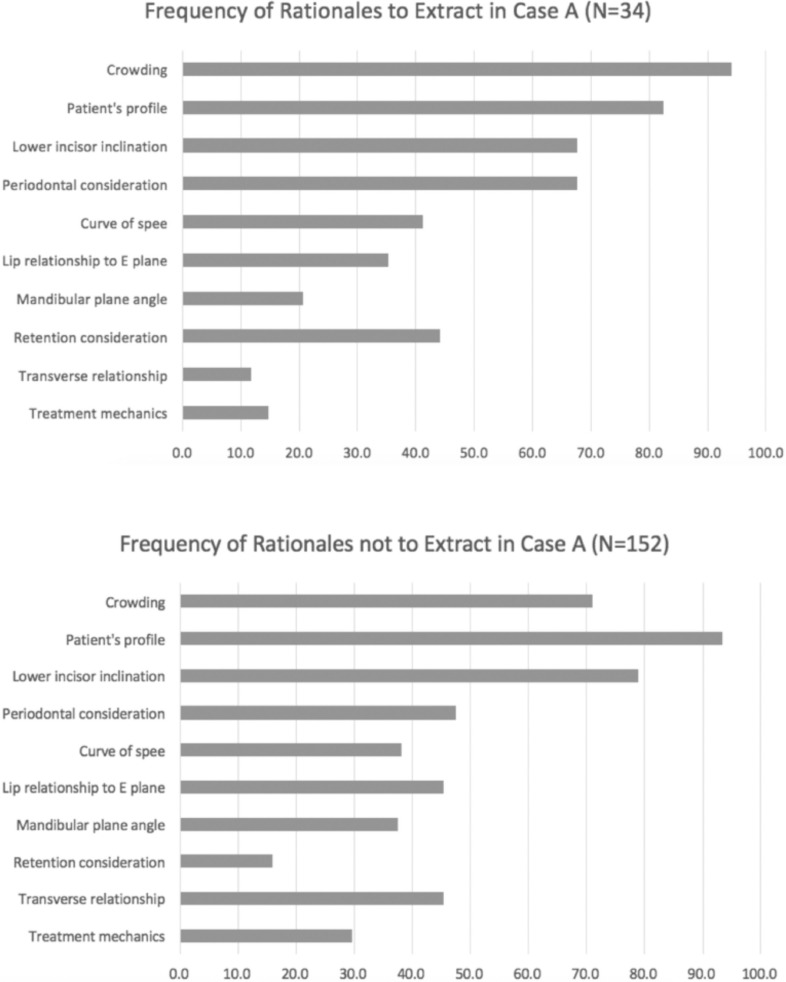
For case A, 85% of the participants preferred nonextraction (Table 3). In the <5-year experience group, only 10% of the participants preferred extraction (Table 4). In the >15-year group, 21% preferred extractions. However, this difference was not statistically significant (X2 = 3.49, P = .06). A second set of analyses compared clinicians with <15 years of experience with those with >15 years of experience. Similar to the initial analysis, only 11% of clinicians with <15 years of experience preferred extractions vs 21% having >15 years of experience (X2 = 4.09, P = .04). A comparable percentage of female (14%) and male (16%) participants preferred extraction in this case (Table 4). The difference in extraction based on gender was not statistically significant (X2 = 0.01, P = .90). The main two reasons provided for extractions were crowding and patient's profile; the top two reasons for nonextraction were patient's profile and mandibular incisor inclination (Figure 1).
Table 4.
Extraction vs Nonextraction Based on Experience and Gender (All Surveys)a
|
|
Case A |
Case B |
Case C |
|||
| Extraction | Nonextraction | Extraction | Nonextraction | Extraction | Nonextraction | |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
|
| Experience | ||||||
| <5 y | 6 (10) | 55 (90) | 9 (20) | 35 (80) | 6 (14) | 36 (86) |
| >15 y | 20 (21) | 74 (79) | 33 (37) | 56 (63) | 22 (26) | 63 (74) |
| P value: .06 | P value: .04 | P value: .14 | ||||
| Experience | ||||||
| <15 y | 14 (11) | 118(89) | 25 (24) | 81 (76) | 15 (15) | 86 (85) |
| >15 y | 20 (21) | 74 (79) | 33 (37) | 56 (63) | 22 (26) | 63 (74) |
| P value: .04 | P value: .06 | P value: .14 | ||||
| Gender | ||||||
| Female | 8 (14) | 48 (86) | 15 (33) | 30 (67) | 4 (10) | 37 (90) |
| Male | 26 (16) | 141 (84) | 43 (29) | 107 (71) | 33 (23) | 112 (77) |
| P value: .90 | P value: .70 | P value: .09 | ||||
Level of statistical significance set at P < .05; nonparametric chi-square test.
Figure 1.
Rationale to extract vs not to extract for case A.
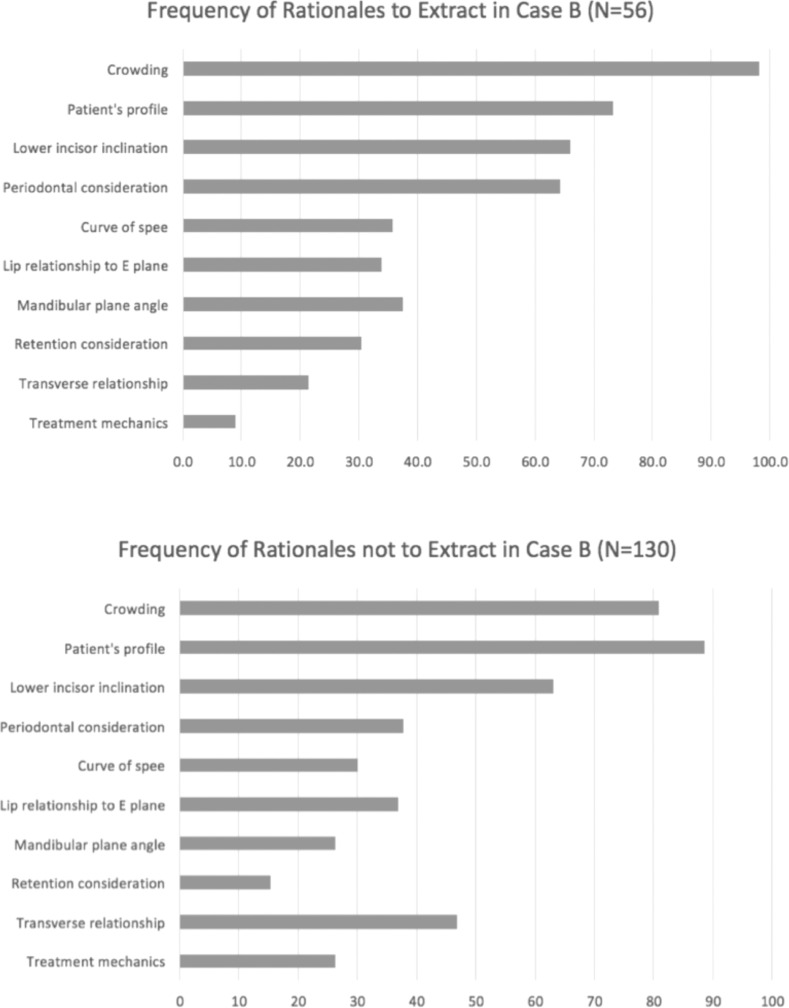
In case B, nonextraction was chosen by 70% (Table 3). In the <5-year experience group, 20% chose extraction while in the >15 year group, 37% chose this option. This difference was statistically significant (X2 = 4.05, P = .04). Comparing the <15-years-of-experience decisions with those of >15 years, a similar trend was observed (24% extraction rate in >15 years vs 37% in <15 years of experience; X2 = 3.59, P = .06) (Table 4). Of the males, 29%, and of the females, 33% preferred extraction, but this was not statistically significantly different (X2 = .04, P = .7) (Table 4). The clinicians' chief two reasons for extraction in this case were crowding and patient's profile. Those who chose nonextraction also selected patient's profile and crowding as reasons not to extract (Figure 2).
Figure 2.
Rationale to extract vs not to extract for case B.
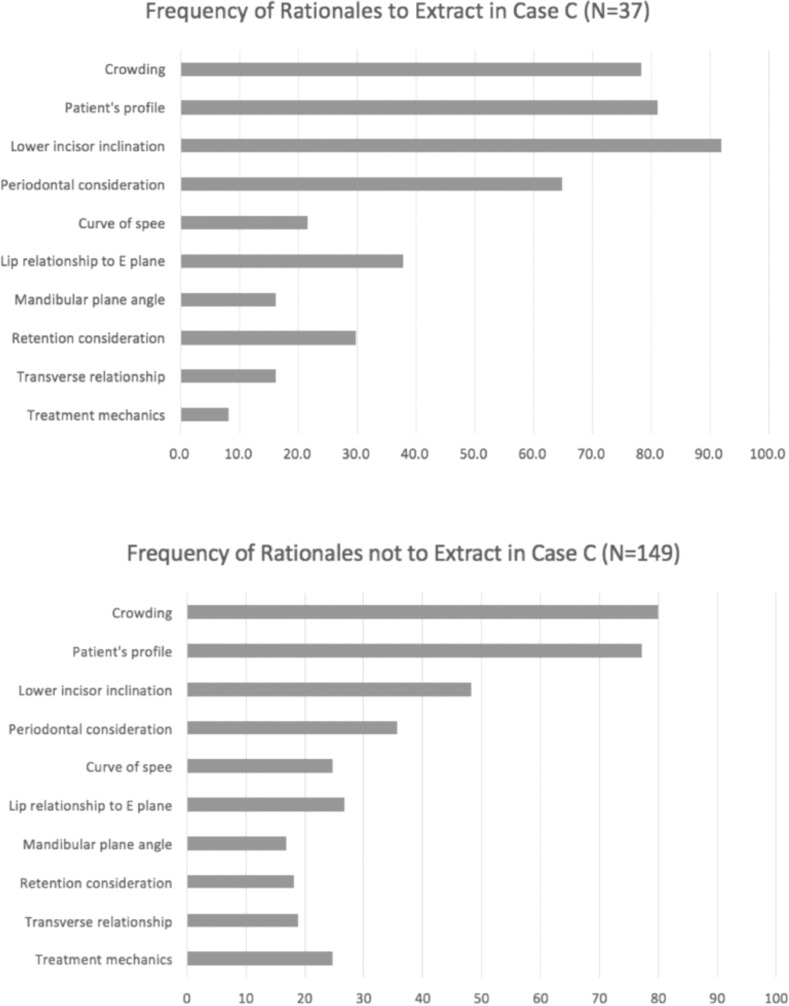
For case C, 80% of the respondents favored nonextraction over extraction (Table 3). In the <5-year experience group, 14% chose extraction compared with 26% of the more experienced group (X2 = 2.20, P = .14) (Table 4). In the group with <15 years of experience, 15% of the clinicians preferred extraction, compared with 26% of clinicians with >15 years' experience (X2 = 2.87, P = .09) (Table 4). Only 10% of the females preferred extraction treatment, whereas 23% of male clinicians chose extraction. This difference was not statistically significant (X2 = 0.15, P = .09) (Table 4). For case C, mandibular incisor inclination and patient's profile were the primary reasons clinicians chose extraction. Crowding and patient's profile were the reasons chosen for nonextraction (Figure 3).
Figure 3.
Rationale to extract vs not to extract for case C.
When all incomplete surveys were eliminated and only completed surveys were analyzed, a similar pattern was detected. For every case, more clinicians with >15 years of experience preferred extraction than clinicians with <5 years of experience. However, since some of the responses had been eliminated, P values decreased for cases A and B, and the differences were not statistically significant (Table 5). The extraction rate difference with respect to gender was not statistically significant.
Table 5.
Extraction vs Nonextraction Based on Experience and Gender (Completed Surveys Only)
|
|
Case A |
Case B |
Case C |
|||
| Extraction | Nonextraction | Extraction | Nonextraction | Extraction | Nonextraction | |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
|
| Experience | ||||||
| <5 y | 6 (14) | 36 (86) | 9 (21) | 33 (79) | 6 (14) | 36 (86) |
| >15 y | 20 (24) | 65 (76) | 32 (38) | 53 (62) | 22 (26) | 63 (74) |
| P value: .2 | P value: .07 | P-value: .14 | ||||
| Gender | ||||||
| Female | 7 (26) | 20 (74) | 8 (30) | 19 (70) | 3 (11) | 24 (89) |
| Male | 17 (18) | 77 (82) | 32 (34) | 62 (66) | 24 (26) | 70 (74) |
| P value: .4 | P value: .7 | P value: .1 | ||||
Level of statistical significance set at P < .05; nonparametric chi-square test.
Twenty-four percent of respondents believed that extraction rates had decreased in their practice over the past 10 years. The majority attributed this to a change in treatment philosophy (48%), aesthetic beliefs (31%), and patient desire (21%).
Clinicians were grouped into their respective AAO constituents based on their place of education. The percentage of extraction vs nonextraction treatment choice for each case was compared between the different constituencies. There was no association between clinicians' AAO constituent and their preference for extraction vs nonextraction (Table 6).
Table 6.
Extraction vs Nonextraction Based on AAO Constituency
|
|
X2 |
P
|
| Case A | 4.16 | .65 |
| Case B | 6.97 | .32 |
| Case C | 2.25 | .89 |
DISCUSSION
The purpose of this study was to determine whether clinicians' traits such as gender and experience had an influence on extraction decisions in Class I borderline patients. Three borderline cases were selected, and a survey was distributed to orthodontists through the AAO Partners in Research program. The demographics of the survey respondents was generally similar to all participants of the Partners in Research program. The significant difference in the number of female clinicians with more than 15 years of experience who responded to the survey is reflected in the demographics of all the survey recipients. This study had a larger percentage of clinicians with less than 5 years of experience respond to the survey (29% of respondents vs 9% of the recipients).
There was a clear relationship between extraction decision making and experience. Experienced clinicians preferred extraction treatment in the selected borderline cases more frequently than the less experienced group. A few other studies have evaluated the influence of clinicians' experience on extraction treatment decision making, but this has not been studied using clinical cases. The results of this study indicated that experience may influence clinicians' decision making regarding extraction vs nonextraction in Class I borderline cases. In all three scenarios, clinicians with >15 years of experience chose an extraction option almost twice as often than those with less experience.
Baelum et al.5 found that orthodontic experience was the only factor that could be correlated with differences in treatment plans by different orthodontists. Another study showed that clinicians with more experience lean toward nonextraction treatment.6 Weintraub et al. reported that the rate of self-reported extractions from private orthodontic practices did not correlate with the amount of experience.7
It has been stated that clinicians' past experiences may lead them to categorize a certain facial pattern as a “nonextraction face.” Therefore, they choose nonextraction in those patients regardless of other factors such as crowding.9–11 It can be speculated that, with experience, clinicians become more familiar with borderline cases best treated with extractions and are more comfortable making that decision than clinicians with less experience.
The results of this study suggested that gender does not play a role in the decision between extraction vs nonextraction treatment. In every patient case, almost equal percentages of female and male clinicians preferred extraction. The same results were achieved when the data were stratified based on gender and experience. Another study also showed that gender did not influence treatment decision making.5 Gentry, however, discovered that female practitioners needed more discrepancy from normal values when choosing extraction.6
Most clinicians who participated in this survey preferred nonextraction treatment for the selected borderline cases. Perhaps the selected cases were not truly borderline. They were selected based on a preliminary survey completed by a group of clinicians who either trained at the same institution or had been teaching at the same department for many years, which may have influenced their treatment planning decisions.
Nonextraction has become more popular with clinicians over the past few years. Extraction rates of four premolars were around 10% in the 1950s, increasing to about 50% in the 1960s, then gradually declining to approximately 10% in the '90s. The frequency of extractions in orthodontics has since increased to 27%–30%.12–15 As indicated in the results of the current study, 24% of the participants believed that the extraction rate in their practice had decreased over the past 10 years. Most clinicians attributed this to a change in treatment philosophy, change in aesthetic beliefs, or patient desires.
In this study, patient's profile, crowding, and mandibular incisor inclination were among the top reasons chosen by both the clinicians who preferred extractions and those who chose nonextraction. Baumrind et al. also discovered that crowding was the number one reason cited by most clinicians when they decided to extract.16 Other patient factors affect the clinicians' decisions9,16,17 and may be subject to interpretation and perceptual variation among orthodontists. The current study confirmed that clinicians are choosing the same diagnostic information as reasons to either extract or not extract.
A secondary aim of this study was to determine whether place of education affected a clinician's extraction decision, and it was inconclusive. Research in this area is scarce; however, another study showed that place of education did not influence clinicians' decision making.5
The number of survey respondents decreased from case A to B to C. The reason some participants did not complete the survey was due to fatigue. Two separate sets of analyses were completed to ensure that this decrease in response rate did not affect the outcome. In both analyses, it was evident that clinicians with >15 years of experience preferred to extract more frequently than clinicians with <5 years of experience.
One of the main limitations of this study was that the numbers of extraction vs nonextraction treatment decisions were not equally distributed. Despite the measures taken by developing a pilot survey to ensure that the patients included in the final survey would be truly borderline, the larger population of orthodontists involved in the final survey mostly preferred nonextraction treatment. Although the sample size goal of 60 for each experience group and gender was reached, some of the analyses that were intended to be performed could not be completed since, in most instances, a very small number of participants chose the extraction treatment option.
CONCLUSIONS
-
•
The results of this study indicated that there could be an association between clinicians' experience and the decision to extract. However, further studies are needed to confirm the results.
-
•
Clinicians with >15 years of experience chose an extraction treatment option more frequently than did clinicians with <5 years of experience.
-
•
No association was found between the clinicians' gender or place of education and the extraction-nonextraction treatment choice.
-
•
The reasons orthodontists chose to extract or not extract for each case were similar for both treatment options.
APPENDIX 1
Survey Questions
Clinicians' Demographic Questions:
-
1.
What is your gender?
-
a.
Female
-
b.
Male
-
a.
-
2.
What is your ethnicity? (Please select all that apply.)
-
a.
American Indian or Alaskan Native
-
b.
Asian or Pacific Islander
-
c.
Black or African American
-
d.
Hispanic or Latino
-
e.
White/Caucasian
-
f.
Prefer not to answer
-
g.
Other (please specify)
-
a.
-
3.
How many years have you practiced orthodontics?
-
a.
Less than 5 years
-
b.
5–15 years
-
c.
More than 15 years
-
a.
-
4.
Compared to earlier in your practice, how would you describe the overall extraction rate for your patients in the past 10 years?
-
a.
Increased
-
b.
Decreased
-
c.
Not changed
-
d.
Prefer not to answer
-
a.
-
5.
To what do you attribute the change in extraction rates in your practice?
-
a.
Development of new mechanics such as TADs
-
b.
Change in treatment philosophy
-
c.
Change in aesthetics beliefs
-
d.
Patient's desire
-
e.
Not sure
-
f.
Other (please specify)
-
a.
-
6.
Approximately, how many hours/week do you practice?
-
7.
Did you attend a 2-year or 3-year orthodontic program?
-
a.
2-year
-
b.
3-year
-
c.
Other (please specify)
-
a.
-
8.
What year did you graduate from your orthodontic program?
-
9.
Do you currently teach in a graduate program?
-
a.
Yes
-
b.
No
-
c.
Prefer not to answer
-
a.
-
10.
How many hours/week do you teach?
-
11.
Do you practice based on a certain philosophy
-
a.
Yes
-
b.
No
-
c.
Prefer not to answer
-
a.
-
12.
Please specify which philosophy you follow in your practice:
-
13.
Which orthodontic program did you attend? (optional)
Clinical Cases:
-
1.
Case A is best treated by:
-
a.
Extractions, other than third molars
-
b.
Nonextraction
-
a.
-
2.
Please specify the extraction pattern you prefer: (select all that apply)
-
a.
UR4 (#5)
-
b.
UR5 (#4)
-
c.
UL4 (#12)
-
d.
UL5 (#13)
-
e.
LL4 (#21)
-
f.
LL5 (#20)
-
g.
LR4 (#28)
-
h.
LR5 (#29)
-
i.
One mandibular incisor
-
j.
Prefer not to answer
-
k.
Other (please specify)
-
a.
-
3.
For nonextraction treatment, how will you create space to level/align the teeth? (Please check all that apply)
-
a.
Expansion
-
b.
Proclination of incisors
-
c.
Leveling curve of Spee
-
d.
Leveling curve of Wilson
-
e.
Distalization of molars
-
f.
Interproximal reduction
-
g.
Prefer not to answer
-
h.
Other (please specify)
-
a.
-
4.
Please briefly describe your treatment plan:
-
5.
The decision to extract or not extract is based on the following considerations: (please select all that apply.)
-
a.
Crowding
-
b.
Patient's profile
-
c.
Manibular incisor inclination
-
d.
Curve of Spee
-
e.
Transverse relationship
-
f.
Lip relationship to E-plane
-
g.
Retention consideration
-
h.
Periodontal consideration
-
i.
Mandibular plane angle
-
j.
Treatment mechanics
-
k.
Prefer not to answer
-
l.
Other (please specify)
-
a.
-
6.
Which long-term retention mechanism do you prefer for maxillary teeth?
-
a.
Hawley
-
b.
Essix
-
c.
Fixed retainer
-
d.
Other (please specify)
-
a.
-
7.
Which long-term retention mechanism do you prefer for mandibular teeth?
-
a.
Hawley
-
b.
Essix
-
c.
Fixed retainer
-
d.
Other (please specify)
-
a.
REFERENCES
- 1.Rody WJ, Jr, Araujo EA. Extraction decision-making wigglegram. J Clin Orthod. 2002;36:510–519. [PubMed] [Google Scholar]
- 2.Baumrind S, Korn EL, Boyd RL, Maxwell R. The decision to extract: Part 1—Interclinician agreement. Am J Orthod Dentofacial Orthop. 1996;109:297–309. doi: 10.1016/s0889-5406(96)70153-1. [DOI] [PubMed] [Google Scholar]
- 3.Brown WA, Harkness EM, Cousins AJ, Isotupa K. Treatment planning from study models: an examiner variability study. Angle Orthod. 1977;47(2):118–122. doi: 10.1043/0003-3219(1977)047<0118:TPFSMA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Lee R, MacFarlane T, O'Brien K. Consistency of orthodontic treatment planning decisions. Clin Orth Res. 1999;2:79–84. doi: 10.1111/ocr.1999.2.2.79. [DOI] [PubMed] [Google Scholar]
- 5.Baelum V, Borchorst E, Buch H, Domgaard P, Harting LE. Inter-examiner variability in orthodontic treatment decisions for Danish children with ‘borderline' treatment need. Eur J Orthod. 2012;34:250–256. doi: 10.1093/ejo/cjq195. [DOI] [PubMed] [Google Scholar]
- 6.Gentry SI. Extraction Decision-Making in Class I Malocclusions: A Survey Identifying Values for Definite Extraction and Non-Extraction Therapy [MSD thesis] St Louis, Mo: Saint Louis University; 2009. [Google Scholar]
- 7.Weintraub JA, Vig PS, Brown C, Kowalski CJ. The prevalence of orthodontic extractions. Am J Orthod Dentofacial Orthop. 1989;96:462–466. doi: 10.1016/0889-5406(89)90112-1. [DOI] [PubMed] [Google Scholar]
- 8.Kay EJ, Nuttal N. Clinical Decision making—an art or science. Part II making sense of treatment decisions. Br Dent J. 1995;180:113–117. doi: 10.1038/sj.bdj.4808664. [DOI] [PubMed] [Google Scholar]
- 9.Patrick JH, Strough J. Everyday problem solving: experience, strategies and behavioral intentions. J Adult Development. 2004;11:9–19. [Google Scholar]
- 10.Hicks EP, Kluemper GT. Heuristic reasoning and cognitive biases: are they hindrances to judgments and decision making in orthodontics? Am J Orthod Dentofacial Orthop. 2011;139(3):297–304. doi: 10.1016/j.ajodo.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Bowman SJ, Johnston LE. The esthetic impact of extraction and nonextraction treatments on Caucasian patients. Angle Orthod. 2000;70(1):3–10. doi: 10.1043/0003-3219(2000)070<0003:TEIOEA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Konstantonis D. The impact of extraction vs nonextraction treatment on soft tissue changes in Class I borderline malocclusions. Angle Orthod. 2012;82(2):209–217. doi: 10.2319/051911-339.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Connor BM. Contemporary trends in orthodontic practice: a national survey. Am J Orthod Dentofacial Orthop. 1993;103:163–170. doi: 10.1016/S0889-5406(05)81766-4. [DOI] [PubMed] [Google Scholar]
- 14.Proffit WR. Forty-year review of extraction frequencies at a university orthodontic clinic. Angle Orthod. 1994;64:407–414. doi: 10.1043/0003-3219(1994)064<0407:FROEFA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Jackson TH, Guez C, Lin F-C, Proffitt WR, Ko C-C. Extraction frequencies at a university orthodontic clinic in the 21st century: demographic and diagnostic factors affecting the likelihood of extraction. Am J Orthod Dentofacial Orthop. 2017;151:456–462. doi: 10.1016/j.ajodo.2016.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baumrind S, Korn EL, Boyd RL, Maxwell R. The decision to extract: Part II. Analysis of clinicians' stated reasons for extraction. Am J Orthod Dentofacial Orthop. 1996;109:393–402. doi: 10.1016/s0889-5406(96)70121-x. [DOI] [PubMed] [Google Scholar]
- 17.Carey CW. Diagnosis and case analysis in orthodontics. Am J Orthod. 1952;38:149–161. [Google Scholar]