Abstract
Objective:
To quantify treatment-related changes in peridental bone height and thickness in orthodontic patients.
Materials and Methods:
Cone-beam computed tomographs (CBCTs) of 43 patients (24 female, 19 male; mean age: 25 years, 5 months) who underwent orthodontic treatment with multibracket appliances for at least 1 year were chosen for retrospective evaluation. Dehiscence depth and changes in bone width and tooth inclination were determined for 954 teeth.
Results:
There was a significant decrease in peridental bone height (dehiscence; −0.82 ± 1.47 mm) and bone thickness (−0.56 ± 0.7 and −0.69 ± 0.9 mm at 5 mm and 10 mm apical to the CEJ, respectively) during treatment (P < .001). A significantly greater dehiscence depth with increased vertical bone loss occurred in patients older than 30 years. In patients <30 years old, approximately 20% of the teeth showed defect depths >2 mm before treatment. In 90% of these patients, at least one tooth was affected. The maxillary canines and all mandibular teeth showed a higher risk for vestibular bone loss. Treatment changes in tooth inclination were correlated with horizontal bone loss.
Conclusions:
Based on these results, it seems reasonable to recommend that peridental bone in orthodontic patients older than 30 be evaluated on a routine basis due to the risk of increased vertical bone loss. Ninety percent of patients younger than 30 showed reduced bone height (dehiscence) of the periodontium of at least one tooth.
Keywords: Peridental bone, Cone-beam computed tomography, Multibracket
INTRODUCTION
Despite contemporary orthodontic treatment methods, the occurrence of gingival recession is still a negative side effect. There is widespread agreement that the thickness of the anterior alveolus should be considered a limiting factor for orthodontic treatment.1 Crossing these anatomical boundaries is clearly associated with an increased risk of treatment-related bone loss and the formation of alveolar defects.2 It is important to distinguish between fenestrations and dehiscences. A fenestration occurs when bone covers the root coronally; if the defect is not limited by bone coronally, it is a dehiscence.3 However, alveolar defects are not solely orthodontic issues because they can be detected in many untreated patients as well.4 The prevalence of alveolar defects increases with age.5,6 Studies have determined that there are no differences in prevalence between women and men,7 whereas other authors have detected an increased frequency of these defects in men.8 There is a similar disagreement concerning different prevalences in the maxilla and mandible. Most authors have documented an increased prevalence of dehiscences in the mandible, while fenestrations were detected predominantly in the maxilla.4,9,10
Visualization of three-dimensional structures of the hard and soft tissues with conventional imaging techniques is inadequate because problems such as superimposition and distortion limit a precise reproduction of periodontal information.11 Special three-dimensional recording methods, such as computed tomography (CT), may be used to image these structures. To overcome the limited capacity of conventional imaging methods while minimizing costs and radiation exposure for patients, cone-beam computed tomography (CBCT) may be the method of choice.12
Linear measurements, particularly with respect to quantitatively evaluating bony dehiscences, have been demonstrated using CBCT.13,14 However, others have claimed there is a significant overestimation of dehiscences and fenestrations by CBCT imaging.15
CBCT scanners are not all the same and can vary substantially with regard to the applied radiation dose.16 Depending on the field of view, recording protocol, and manufacturer, the effective dose ranges between 13 and 498 μSv, with most CBCT scans resulting in 30–80 μSv.12,16,17 With indication-dependent dose reduction concepts, the claim of minimal radiation exposure can be met.
Recent findings have documented a high subject-related prevalence of alveolar defects before orthodontic treatment,4 whereas the available data on bone loss during contemporary orthodontic treatment is either outdated or includes only a small and limited patient population, selected by type of malocclusion18 or growth pattern,9 or it is restricted solely to the anterior region.19 The aim of this study was to evaluate the treatment-related bone loss of explicitly unselected patients during modern orthodontic treatment. A quantitative evaluation of treatment-related changes in bone height and width was conducted.
MATERIALS AND METHODS
After approval by the ethics committee of the Charité-Universitätsmedizin Berlin, volumetric patient images were recruited retrospectively from the EU-certified, long-term archive of the national 3D-Röntgennetzwerk MESANTIS. Permission to view and analyze the images involved in this study was obtained. Each indication for a CBCT image was individually justified by a dentist with the appropriate professional qualification and was performed independently of the present retrospective study. Therefore, no patient was exposed to radiation for the specific purpose of this study. Scans were performed with the i-CAT Next Generation (Imaging Sciences International, Hatfield, Pa), with a field of view of 13 × 16 cm and an image resolution of 0.25-mm voxel size. Each patient was treated with the straight-wire technique having an 0.022-inch slot size and MBT prescription. The radiological status of the selected patients was documented before (T0) and after orthodontic treatment (T1) with CBCT imaging. Patients who underwent orthognathic surgery, had severe crowding, suffered from periodontitis, or had teeth with carious lesions or restorations near the cementoenamel junction (CEJ) were excluded. Because of the retrospective character of this study, there were no data on the periodontal sulcus depth before or after treatment, but professional oral hygiene was performed and patients were instructed on a standardized oral hygiene protocol before and during treatment on a regular basis.
The sample was composed of 43 patients treated between August 2007 and March 2012, including 19 men and 24 women with a mean age of 25 years, 5 months (Table 1). The patient population was divided into three age groups. Analysis was done separately for patients aged 10–15 years, 15–30 years, and subjects >30 years. In this study, all fully erupted permanent teeth up to and including the first molars were examined (n = 954).
Table 1.
Patient Population —Age And Sex Distribution
| Age Group |
Total | Male | Female | Mean Age | SD | Agemin | Agemax |
| N (%) |
(Y, Mo) |
||||||
| Male | 19 (44.2) | – | – | 24.0 | 11.11 | 13.6 | 49.10 |
| Female | 24 (55.8) | – | – | 26.7 | 14.8 | 10.2 | 56.9 |
| 10–15 y | 13 (30.2) | 4 (30.8) | 9 (69.2) | 13.7 | 1.5 | 10.2 | 14.11 |
| 15–30 y | 16 (37.2) | 9 (56.2) | 7 (43.8) | 19.9 | 3.9 | 15.8 | 28.3 |
| >30 y | 14 (32.6) | 6 (42.9) | 8 (57.1) | 43.0 | 7.4 | 31.7 | 56.9 |
| Totals | 43 (100) | 19 (44.2) | 24 (55.8) | 25.5 | 13.5 | 10.2 | 56.9 |
The period between the first and second CBCT imaging was 20 ± 8 months (12–45 months). Between the evaluation of pre- and posttreatment CBCTs, an interval of at least 6 months was maintained, and measurements were performed blind.
All measurements were performed by a single calibrated examiner who was trained for 10 days by a senior employee of the radiological institute MESANTIS before data collection. The measurement methodology was based on the research of Fuhrmann.20 Two measurement parameters were gathered that provided information on the peridental bone. The dehiscence depth was measured parallel to the tooth axis as the distance between the CEJ and the cervical bone margin (Figure 1). Bone thickness was measured as the linear distance between the buccal and lingual tooth boundaries and the extreme bone edge perpendicular to the tooth axis at 5 mm and 10 mm, respectively, apical to the CEJ (Figure 2). Additionally, the changes in bone were assessed with a parameter that quantified orthodontic tooth tipping by evaluating the vestibulo-oral inclination of the tooth axis in relation to the occlusal plane (Figure 3). All measurements were made in the multiplanar view.
Figure 1.
Example measurement of dehiscence depth of tooth 25.
Figure 2.
Example measurement of bone thickness at 5 and 10 mm apical to the CEJ of tooth 25 on the vestibular and lingual aspects.
Figure 3.

Example measurement of the vestibulo-oral inclination of tooth 25.
Statistical analyses including exploratory data analysis and nonparametric tests, as well as the generation of charts, were conducted using the statistical software SPSS Statistics (Statistical Package of Social Science, Version 20, Chicago, Ill). Post hoc analyses were executed for the respective n. To calculate the power 1–β, a significance level of α = .05 was used, and the effect size was d = 0.5. According to the Kolmogorov-Smirnov test, no parameter except the inclination of the teeth showed a normal distribution. Therefore, nonparametric tests were performed in addition to the t test for paired samples. Repeated measurements of 50 randomly selected teeth from 10 CBCTs of different patients were made to ascertain the errors in measurement by means of the Dahlberg formula and the Houston reliability coefficient. The interval between repeated measurements was at least 24 hours.
RESULTS
The error of measurement was less than 0.1° for inclination and less than 0.01 mm for measures of the peridental bone. The Houston reliability coefficient was 99.8 for all three parameters.
The amount of vertical bone decreased significantly with treatment, both on the facial and lingual sides (P < .01). Of the examined teeth, 79.6% showed an enlargement in vestibular dehiscence depth, with a mean change in all teeth of 0.82 ± 1.47 mm (range, −1.27 to +9.5 mm). A frequency distribution of the treatment-related changes in defect depth is shown for the vestibular side in Figure 4, and for the lingual side in Figure 5. An increase in lingual dehiscence depth occurred in 79.4% of the teeth with the mean change averaging 0.57 ± 0.79 mm (range, −1.84 to 6.07 mm).
Figure 4.
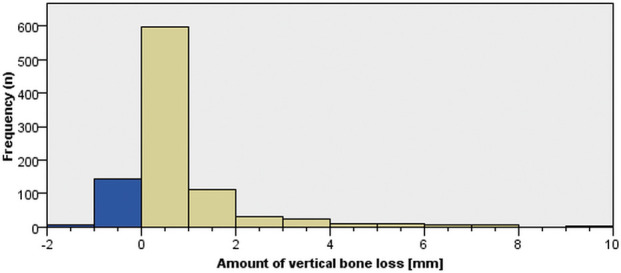
Frequency distribution of the amount of treatment-related vertical bone loss (dehiscence) on the vestibular (buccal) tooth aspect.
Figure 5.
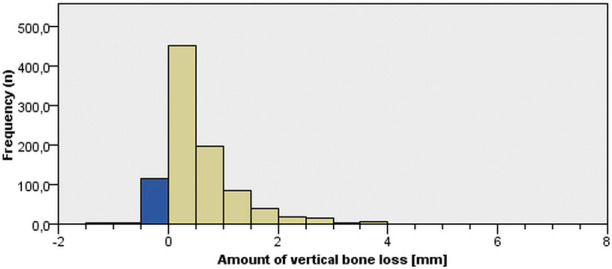
Frequency distribution of the amount of treatment-related vertical bone loss (dehiscence) on the lingual aspect.
During treatment, all measures of bone thickness showed a significant reduction. The combined (facial and lingual) change in bone thickness averaged −0.56 ± 0.7 mm at 5 mm apical to the CEJ, and −0.69 ± 0.9 mm at 10 mm apical to the CEJ. Lingual bone thickness 10 mm apical to the CEJ decreased significantly by an average of −0.4 ± 0.78 mm and was greater than the treatment-related bone thickness decrease observed at other sites. There were no significant differences in treatment-related changes of bone height and thickness between males and females.
Among age groups, there were significant differences in both the pre- and posttreatment defect depths (dehiscences) on the vestibular and lingual aspects (P < .001; Table 2). Of the examined teeth, 21.1% of the <30-year-olds showed pretreatment vestibular defect depths exceeding 2 mm. At least one tooth was affected in 89.7% of these patients (Figures 6 and 7). In this age group, a treatment-related loss of vestibular vertical bone height exceeding 2 mm was found in 8.2% of the examined teeth. In 75.9% of patients in this age group, at least one tooth was affected. Table 3 displays the percentages of teeth and patients affected in each age group.
Table 2.
Size of Dehiscence Depths Pre- (T0) and Posttreatment (T1) and Their Relations in Terms of Age-Specific Differences
| Age Group |
Vestibular Defect Depth ± SD (mm) |
Lingual Defect Depth ± SD (mm) |
||||
| T0 |
T1 |
Change |
T0 |
T1 |
Change |
|
| AG1 (10–15 years) | 1.25 ± 1.71 | 1.99 ± 2.23 | 0.7 ± 0.08 | 0.64 ± 0.75 | 1.18 ± 1.08 | 0.5 ± 0.05 |
| AG2 (15–30 years) | 1.84 ± 1.94 | 2.53 ± 2.24 | 0.7 ± 0.06 | 1.26 ± 1.47 | 1.73 ± 1.69 | 0.5 ± 0.04 |
| AG3 (>30 years) | 2.35 ± 2.08 | 3.38 ± 2.92 | 1 ± 0.1 | 1.88 ± 1.40 | 2.6 ± 1.63 | 0.7 ± 0.05 |
| Significance | <.001 | <.001 | .059 | <.001 | <.001 | <.001 |
Figure 6.
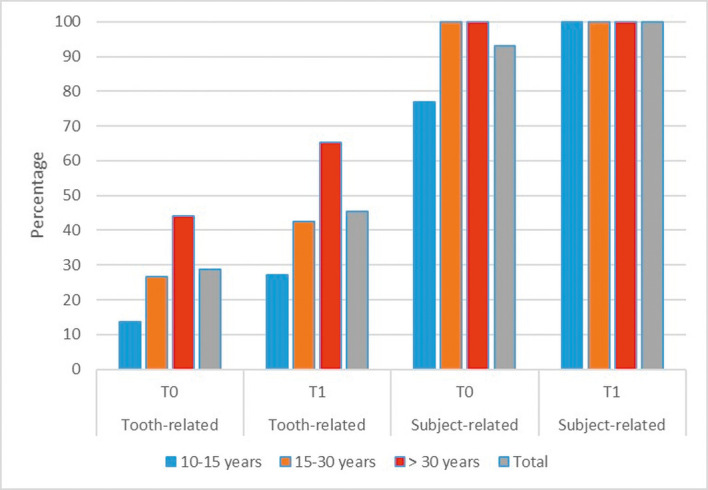
Age-specific prevalence of vestibular dehiscences exceeding 2 mm before (T0) and after (T1) orthodontic treatment.
Figure 7.
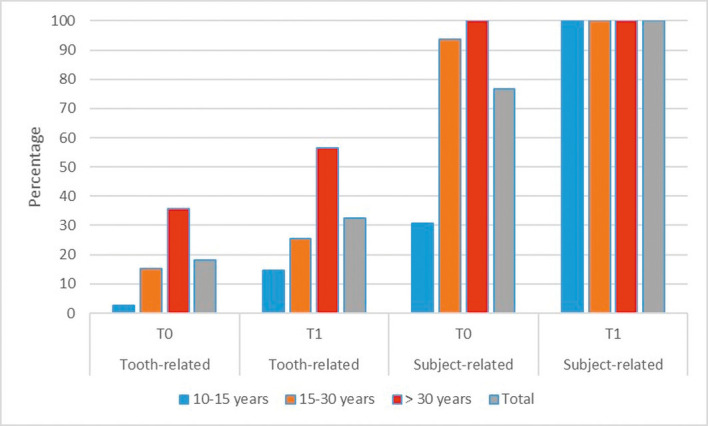
Age-specific prevalence of lingual dehiscences exceeding 2 mm before (T0) and after (T1) orthodontic treatment.
Table 3.
Treatment-Related Vertical Bone Loss Exceeding 2 mm
|
|
10–15 Y |
15–30 Y |
>30 Y |
Total |
||||
| Tooth- Related |
Subject- Relateda |
Tooth- Related |
Subject- Relateda |
Tooth- Related |
Subject- Relateda |
Tooth- Related |
Subject- Relateda |
|
| Vestibular (%) | 8.79 | 84.62 | 7.82 | 68.75 | 12.9 | 71.43 | 9.75 | 74.42 |
| Lingual (%) | 6.59 | 61.54 | 3.23 | 50 | 7.42 | 71.43 | 5.56 | 60.47 |
Indicates patients with at least one tooth affected.
The thickness of bone decreased significantly during treatment in all age groups. Younger patients had greater bone thickness, especially before orthodontic treatment, and greater treatment-related decreases.
There was a significantly lower bone height and greater treatment-related loss in vestibular vertical bone in the mandible than in the maxilla. However, treatment-related changes in maxillary bone thickness were greater than the changes in lingual bone thickness and overall bone thickness observed in the mandible. Comparing the different groups of teeth, the mandibular incisors displayed an increased treatment-related vertical bone loss. A summary of the changes in defect depth on the vestibular side for each tooth type is illustrated in Figure 8. Average vertical bone loss for each tooth, in each age group on the vestibular and lingual aspects, respectively, are depicted in Figures 9 and 10. The frequency of posttherapeutic vestibular defect depths >2 mm was over 20% in all groups of teeth and was most frequently observed in maxillary canines at 58.67%. In addition, the frequency was greater than 50% in the mandibular premolars, mandibular canines and mandibular incisors. Bone thickness decreased during treatment to a greater extent in the maxillary premolars and molars than in other groups of teeth.
Figure 8.
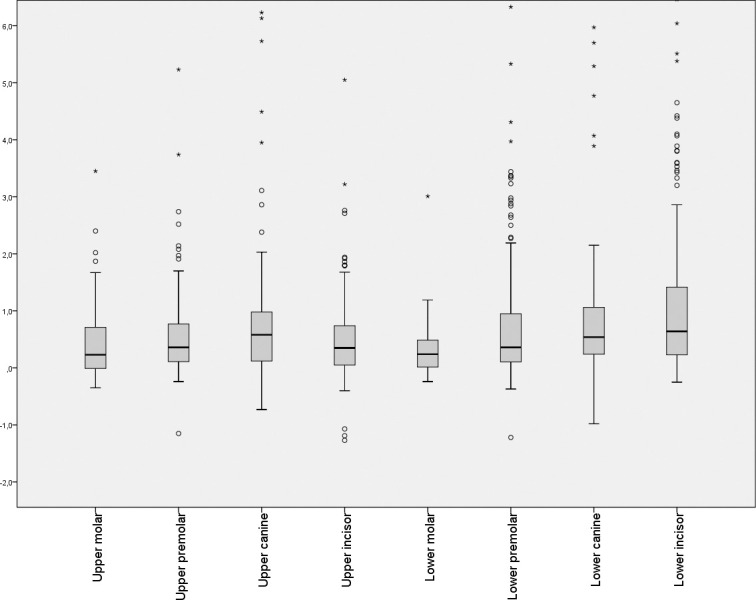
Comparison of treatment-related vestibular vertical bone loss (dehiscence) in mm by tooth type.
Figure 9.
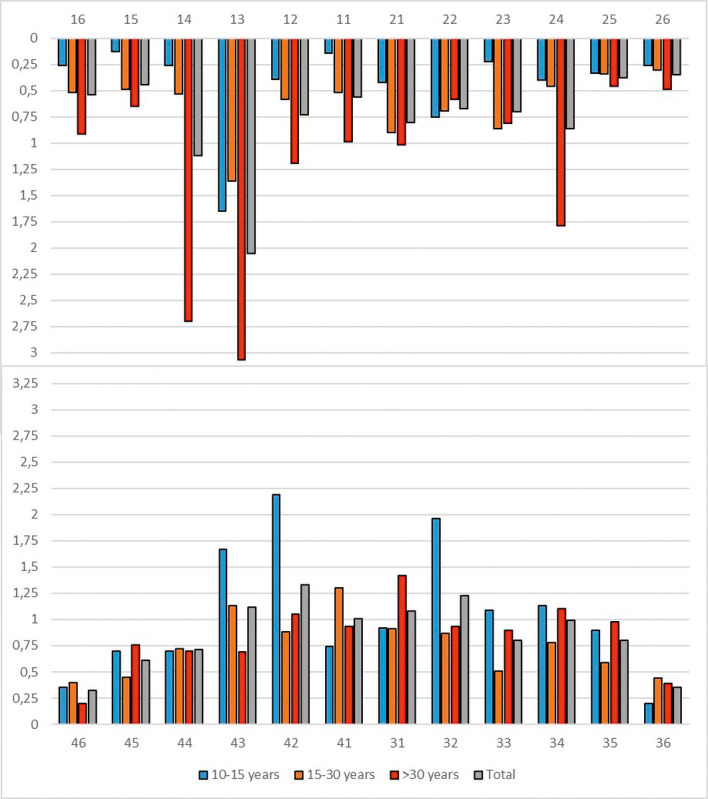
Mean treatment-related vestibular vertical bone loss (dehiscence) for each tooth for the three age groups in mm.
Figure 10.
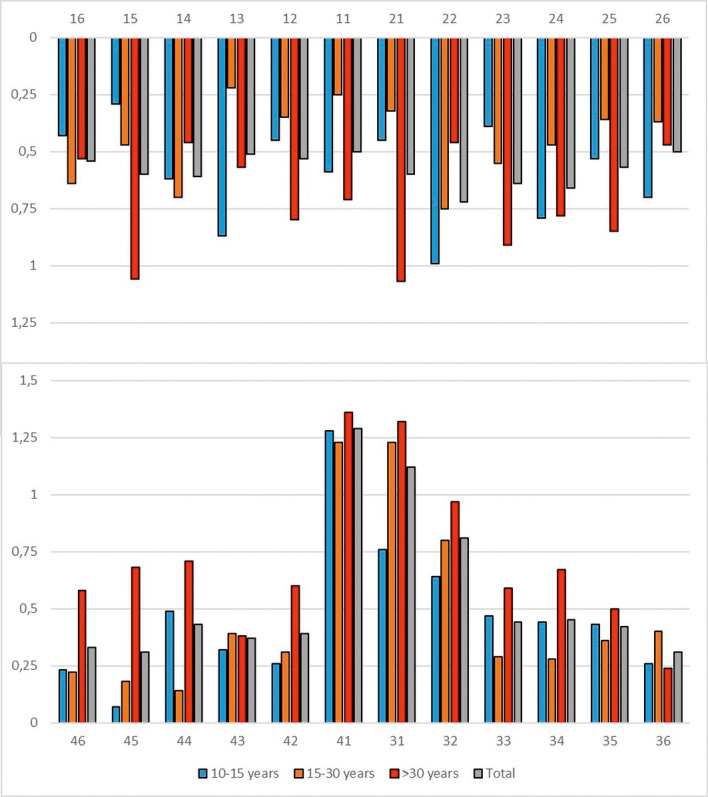
Mean treatment-related lingual vertical bone loss (dehiscence) for each tooth in the three age groups in mm.
There was no significant correlation between the extent of pretreatment vestibular defect depth and the treatment-related change in this measure. Moreover, there were no correlations between the changes in the parameters of bone thickness and the treatment-related loss in vestibular bone height. That said, there was a slight relationship between the change of the lingual defect depth (dehiscence) and changes in bone thickness observed.
There was a significant correlation between the change in inclination and change in bone thickness but no correlation between inclination change and vertical bone loss. Bone thickness decreased in the apical region on the side toward which a root was moving and increased in both the cervical and apical region on the opposite side.
DISCUSSION
Since the population studied consisted of patients who underwent routine orthodontic treatment, the data presented should be considered clinically important. Conversely, the deliberately inhomogeneous patient population, in combination with the application of few exclusion criteria, also restricts the application of the results obtained because there was a wide age range, a lack of assessment of specific periodontal parameters, and unidentified types of tooth movement that were induced due to the wide range of pretreatment malocclusions present. Therefore, it is critical that further studies be conducted to assess the relevance of the present results.
The main criterion of including CBCT data available with a voxel size below 0.25 mm, along with evaluation in the multiplanar view, was meant to improve measurement accuracy. There are fewer false negative results using these methods compared with the volume-rendering view.15 Nevertheless, it should be kept in mind that there is a general risk of overestimating fenestrations and dehiscences in CBCTs.21 Computer-assisted superimposition was considered in evaluating bone levels. Due to the fragility of the structures analyzed and the small treatment-related differences, the expected error of superimposition was considered too large. The calculated reliability of vestibular bone height and width exceeding values reported in the literature22 and a possible bias due to having only one investigator involved in the study has to be considered.
The magnitude of increases in defect depth (dehiscence) found in this study slightly exceeded that found in previous studies.7,23,24 In agreement with other studies, however, deep dehiscences occurred less frequently on the lingual.4,9,10 A large interindividual variation in vertical bone height was also observed.7 In agreement with previous studies, there was no significant correlation between the extent of the pretreatment dehiscence and the magnitude of change occurring during treatment.25
The correlation between treatment-related changes in tooth inclination and changes in bone thickness found in this study is consistent with findings of previous studies in which it was observed that the greatest treatment-related bone loss was on the side toward which a tooth was moved.2,26,27 On this side, bone loss occurred predominantly in the cervical and middle-root sections.26
The mean treatment-related loss in vertical bone height for the three age groups was consistent with observations from other studies.6 Although a correlation between increased age and increased prevalence and dehiscence depth is described in the literature,5,6 the frequency of patients with at least one tooth with a pretreatment dehiscence and treatment-related bone loss exceeded findings of previous studies for all age groups. The treatment-related changes in bone thickness in the maxilla were greater than the changes in lingual bone thickness and overall bone thickness observed in the mandible. These findings were consistent with results reported by previous authors who described an increased prevalence of fenestrations in the maxilla.4,9,10
The increased incidence of dehiscences in the anterior tooth region was generally consistent with the results of other authors.9,10,19 However, others also detected an increased prevalence of dehiscences in the maxillary molars, which could not be confirmed on the basis of present results.5
Due to the lack of uniformity in the study population evaluated, further research is needed to examine the effect of differences in skeletal characteristics and Angle classification on bony changes during orthodontic treatment, as variations in jaw morphology and mandibular plane inclination influence the morphology of the alveolar process. Moreover, it is necessary to study the influence of different orthodontic appliances and treatment mechanics, as well as the influence of accelerated tooth movement techniques, on bony response.
CONCLUSIONS
-
•
Results suggest that a pretreatment, three-dimensional assessment (using CBCT) may be indicated, especially in patients over 30 years old, when buccal tooth movement during treatment is anticipated.
-
•
There was also a large number of younger subjects with at least one tooth displaying decreased pretreatment vertical bone (dehiscence) and notable treatment-related bone loss.
-
•
In patients with preexisting periodontal damage, less treatment-related bone loss was observed.
REFERENCES
- 1.Garib DG, Yatabe MS, Ozawa TO, Silva Filho OGD. Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dental Press J Orthod. 2010;15(5):192–205. [Google Scholar]
- 2.Mulie RM, Hoeve AT. The limitations of tooth movement within the symphysis, studied with laminagraphy and standardized occlusal films. J Clin Orthod. 1976;10:882–893. [PubMed] [Google Scholar]
- 3.Lindhe J, Karring T, Araújo M. Clinical periodontology and implant dentistry. In: Lindhe J, Karring T, Lang N, editors. Anatomy 4th ed. Copenhagen: Blackwell Munksgaard; 2003. pp. 3–48. [Google Scholar]
- 4.Evangelista K, Vasconcelos KDF, Bumann A, Hirsch E, Nitka M, Silva MAG. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138:133–135. doi: 10.1016/j.ajodo.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 5.Baljoon M, Natto S, Bergstrom J. Occurrence of vertical bone defects in dentally aware individuals. Acta Odontol. 2003;61(1):47–51. doi: 10.1080/ode.61.1.47.51. [DOI] [PubMed] [Google Scholar]
- 6.Harris EF, Baker WC. Loss of root length and crestal bone height before and during treatment in adolescent and adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1990;98:463–469. doi: 10.1016/s0889-5406(05)81656-7. [DOI] [PubMed] [Google Scholar]
- 7.Zachrisson BU, Alnaes L. Periodontal condition in orthodontically treated and untreated individuals II. Alveolar bone loss: radiographic findings. Angle Orthod. 1974;44:48–55. doi: 10.1043/0003-3219(1974)044<0048:PCIOTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Wouters FR, Satonen LE, Helldën LB, Frithiof L. Prevalence of interproximal periodontal intrabony defects in an adult population in Sweden. A radiographic study. J Clin Periodontol. 1989;16:144–149. doi: 10.1111/j.1600-051x.1989.tb01631.x. [DOI] [PubMed] [Google Scholar]
- 9.Enhos S, Uysal T, Yagci A, Veli İ, Ucar FI, Ozer T. Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod. 2012;82:868–874. doi: 10.2319/111211-702.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yagci A, Veli I, Uysal T, Ucar FI, Ozer T, Enhos S. Dehiscence and fenestration in skeletal Class I, II, and III malocclusions assessed with cone-beam computed tomography. Angle Orthod. 2011;82:67–74. doi: 10.2319/040811-250.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sitzmann F. Bildgebende Verfahren in der Zahn-, Mund- und Kieferheilkunde. AfCS-Nature Mol. 1988. In. Ketterl, W. (Hrsg.) Grundlagen der Zahn-, Mund- und Kieferheilkunde I. 202.
- 12.Silva MAG, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop. 2008;133:640.e1–640.e5. doi: 10.1016/j.ajodo.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Evans CA. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:238–257. doi: 10.1016/j.oooo.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–1266. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 15.Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137:S109–S119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Ludlow J, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2008;106:106–114. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Loubele M, Bogaerts R, Van Dijck E, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009;71(3):461–468. doi: 10.1016/j.ejrad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y, Park JU, Kook Y-A. Alveolar bone loss around incisors in surgical skeletal Class III patients: a retrospective 3-D CBCT study. Angle Orthod. 2009;79:676–682. doi: 10.2319/070308-341.1. [DOI] [PubMed] [Google Scholar]
- 19.Garlock DT, Buschang PH, Araujo EA, Behrents RG, Kim KB. Evaluation of marginal alveolar bone in the anterior mandible with pretreatment and posttreatment computed tomography in nonextraction patients. Am J Orthod Dentofacial Orthop. 2016;149:192–201. doi: 10.1016/j.ajodo.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 20.Fuhrmann R. Three-dimensional interpretation of periodontal lesions and remodeling during orthodontic treatment. J Orofacial Orthop. Fortschritte der Kieferorthopädie Organ/official J. Dtsch. Gesellschaft für Kieferorthopädie. 1996. 57(4, pt 3):224–237. [DOI] [PubMed]
- 21.Patcas R, Müller L, Ullrich O, Peltomäki T. Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2012;141:41–50. doi: 10.1016/j.ajodo.2011.06.034. [DOI] [PubMed] [Google Scholar]
- 22.Timock AM, Cook V, McDonald T, et al. Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 2011;140:734–744. doi: 10.1016/j.ajodo.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 23.Bollen A, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139:413–422. doi: 10.14219/jada.archive.2008.0184. [DOI] [PubMed] [Google Scholar]
- 24.Janson G, Bombonatti R, Brandão AG, Henriques JFC, de Freitas MR. Comparative radiographic evaluation of the alveolar bone crest after orthodontic treatment. Am J Orthod Dentofacial Orthop. 2003;124:157–164. doi: 10.1016/s0889-5406(03)00392-5. [DOI] [PubMed] [Google Scholar]
- 25.Lindhe J, Haffaiee AD, Socransky SS. Progression of periodontal disease in adult subjects in the absence of periodontal therapy. J Clin Periodontol. 1983;10:433–442. doi: 10.1111/j.1600-051x.1983.tb01292.x. [DOI] [PubMed] [Google Scholar]
- 26.Sarikaya S, Haydar B, Ciǧer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 27.Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone, and symphysis after orthodontic treatment. A retrospective study. Am J Orthod Dentofac Orthop. 1996;110:239–246. doi: 10.1016/s0889-5406(96)80006-0. [DOI] [PubMed] [Google Scholar]




