Abstract
Background
Sleep problems and cumulative risk factors (e.g., caregiver depression, socioeconomic disadvantage) have independently been linked to adverse child development, but few studies have examined the interplay of these factors. We examined whether cumulative risk exposure moderated the link between sleep problems, including insomnia and poor sleep health, and child psychological outcomes.
Methods
205 caregiver-child dyads (child Mage = 3.3 years; 53.7% girls; 62.9% Black, 22.4% non-Latinx White, and 4.4% Latinx; 85.4% maternal caregiver reporter) completed child sleep, family sociodemographic, and child psychological functioning (internalizing, externalizing, and executive functioning) questionnaires. Indexes of cumulative risk exposure, insomnia symptoms, and poor sleep health were created.
Results
Ninety percent of children had ≥1 cumulative risks, 62.9% had ≥1 insomnia symptom, and 84.5% had ≥1 poor sleep health behavior. Increased insomnia symptoms were significantly associated with increased child internalizing, externalizing, and global executive functioning impairments controlling for child age, race/ethnicity, and sex. Poor sleep health behaviors were associated with internalizing concerns. Cumulative risk exposure was not associated with outcomes but moderated the association between insomnia symptoms and all psychological outcomes, such that children with higher cumulative risk exposure and insomnia symptoms had the greatest impairments. Children with the poorest sleep health behaviors and highest cumulative risks had the greatest internalizing concerns.
Conclusions
Insomnia symptoms in particular are associated with poor child outcomes, which are exacerbated when accompanied by greater cumulative risk exposure. Clinicians should assess sleep when treating early psychological concerns, especially within the context of increased cumulative risks.
Keywords: behavior problems, health behavior, mental health, sleep
Introduction
Insomnia symptoms (difficulty falling/staying asleep) and poor sleep health behaviors (insufficient sleep, bedtime electronics usage, and caffeine consumption) are common in early childhood, impacting up to 20–30% of toddlers and preschoolers (Byars, Yolton, Rausch, Lanphear, & Beebe, 2012; Meltzer, Williamson, & Mindell, 2021; Mindell, Meltzer, Carskadon, & Chervin, 2009). A growing body of research demonstrates that in early childhood, poor sleep is associated with critical psychological outcomes, including internalizing and externalizing problems (Armstrong, Ruttle, Klein, Essex, & Benca, 2014; Conway, Miller, & Modrek, 2017; Quach, Nguyen, Williams, & Sciberras, 2018; Sivertsen et al., 2015; Williams, Berthelsen, Walker, & Nicholson, 2017) and executive functioning concerns (Bruni et al., 2020; Mäkelä et al., 2020; Nelson, Nelson, Kidwell, James, & Espy, 2015; Taveras, Rifas-Shiman, Bub, Gillman, & Oken, 2017). However, there are salient gaps in this work. In terms of insomnia symptoms, meta-analytic research indicates that most early childhood studies have assessed individual aspects of insomnia, rather than a combination of insomnia symptoms, in relation to psychological outcomes (Reynaud, Vecchierini, Heude, Charles, & Plancoulaine, 2018). For instance, difficulty falling asleep and bedtime resistance, both of which are symptoms of insomnia, have been linked to internalizing and externalizing problems in toddlers (Conway et al., 2017). Frequent night awakenings, another common insomnia symptom in young children, have also been associated with worse performance on an executive functioning task in early development (Mäkelä et al., 2020).
Understanding how an array of insomnia symptoms, which better aligns with pediatric insomnia diagnostic criteria (American Academy of Sleep Medicine, 2014; American Psychiatric Association, 2013), may be linked to child psychological functioning is especially important in early childhood, when social-emotional and executive functioning skills are rapidly developing (Reynaud et al., 2018; Turnbull, Reid, & Morton, 2013). Several previous longitudinal studies have examined broadly assessed early childhood behavioral sleep problems, some of which map on to an insomnia diagnosis, in relation to different psychological outcomes (Nelson et al., 2015; Quach et al., 2018; Williams et al., 2017). One study found that insomnia symptom ratings at age 4.5 years were associated with increased externalizing behaviors, both concurrently and age 9 years (Armstrong et al., 2014). Another study found that preschoolers with diagnosed insomnia had worse executive functioning than controls, but this study was limited to children with insomnia recruited from a sleep clinic, reflecting a specific sample of families who have sought sleep care (Bruni et al., 2020).
Similar to pediatric insomnia symptoms, few studies have examined associations among multiple sleep health behaviors and early childhood psychological functioning. A meta-review of 39 meta-analytic studies of child sleep and health outcomes across ages found that the majority of this work has focused on sleep duration or insufficient sleep, that is, sleeping less than age-based 24-hr sleep duration recommendations (Matricciani, Paquet, Galland, Short, & Olds, 2019). Insufficient early childhood sleep is associated with poor executive functioning longitudinally (Taveras et al., 2017) and with greater internalizing and externalizing concerns (Matricciani et al., 2019; Reynaud et al., 2018). However, little is known about whether adherence to commonly recommended sleep health behaviors, such as having an early bedtime, following a bedtime routine, limiting exposure to bedtime electronics devices, and avoiding caffeine, are also related to child psychological outcomes (Allen, Howlett, Coulombe, & Corkum, 2016; Meltzer et al., 2021). Examining these associations can inform whether early childhood sleep health promotion efforts could potentially enhance key social-emotional and executive functioning skills by focusing on multiple sleep behaviors.
It is also notable that despite a large body of literature showing an increased prevalence of sleep problems and poor sleep health in socioeconomically disadvantaged youth (El-Sheikh, Shimizu, Philbrook, Erath, & Buckhalt, 2020; Smith, Hardy, Hale, & Gazmararian, 2019), there is a paucity of research examining associations among sleep, socioeconomic indicators, and psychological functioning in young children. In one study of preschoolers, lower family socioeconomic status (SES) moderated the association between poorer caregiver-rated child sleep quality and diminished caregiver-rated child working memory (Wetter, Fuhs, & Goodnight, 2020), but no moderation effect was found for other executive functioning skills. Additional research is available in older youth. For instance, in school-aged children, poor actigraphy-derived sleep quality was similarly associated with poor working memory skills, but only in children of lower SES (Buckhalt, El‐Sheikh, & Keller, 2007). In a recent study of adolescents, lower family SES moderated the link between sleep problems and psychological concerns, such that youth with sleep problems from lower SES families showed the greatest internalizing and externalizing problems (El-Sheikh et al., 2020).
Studying interrelations among sleep problems, socioeconomic adversity, and psychological outcomes in young children is critical given the growth in social-emotional and executive functioning skills during this developmental period (Black et al., 2017; Turnbull et al., 2013), the high prevalence and persistence of sleep problems in toddlers and preschoolers (Byars et al., 2012; Williamson, Mindell, Hiscock, & Quach, 2019), and the adverse effects of sleep concerns on psychological functioning longitudinally (Matricciani et al., 2019; Sivertsen et al., 2015). This research can also guide whether targeted sleep screening and tailored intervention efforts are needed to address poor sleep, as well as psychological concerns, in children from lower-SES contexts. At the same time, from a cumulative risk perspective, it also necessary to explore other SES-related risks that may accumulate across socioecological domains and worsen child outcomes (Evans, 2004; Evans, Li, & Whipple, 2013). A number of studies have shown that cumulative risk exposure, typically modeled by dichotomizing and summing caregiver (e.g., lower educational attainment; depressive symptoms), family (e.g., household overcrowding; single-caregiver structure), and environmental (e.g., lower neighborhood SES) risk factors, is associated with worse child psychological outcomes (Appleyard, Egeland, Dulmen, & Alan Sroufe, 2005; Atkinson et al., 2015; Evans et al., 2013). Research also indicates that cumulative risk exposure is especially deleterious when it occurs earlier in development (Appleyard et al., 2005). In addition, studies have found that young children exposed to increased cumulative risks show greater sleep problems (Hash et al., 2019). Specifically, in our previous research using the present study’s early childhood sample, we found that cumulative sociodemographic risk factors were associated with a greater odds of pediatric insomnia symptoms and poor sleep health behaviors (Williamson & Mindell, 2020).
Overall, there is a dearth of studies examining how these specific sleep symptoms and behaviors and cumulative sociodemographic risks may interact and associate with child psychological outcomes, including internalizing/externalizing problems and executive functioning skills. As previously described, understanding these associations is especially valuable during early childhood, a sensitive period for psychological development, and can inform preventive, targeted screening and intervention. This study addresses the aforementioned research gaps and extends previous research by examining the interplay of multiple insomnia symptoms, poor sleep health behaviors, and cumulative risks in relation to early childhood psychological functioning. Based on previous research on pediatric sleep, socioeconomic adversity, and child outcomes (Buckhalt et al., 2007; El-Sheikh et al., 2020; Wetter et al., 2020), we hypothesized that increased cumulative risk exposure would moderate the link between poor sleep and psychological outcomes, such that young children with increased cumulative risks and insomnia symptoms or poor sleep health behaviors would show the greatest psychological impairments in internalizing, externalizing, and executive functioning behaviors.
Methods
Participants
A total of 205 caregivers (87.3% mothers) of preschool-aged children (child Mage = 3.3 years) recruited from primary care waiting rooms were included in this study (Table I). Fifteen additional dyads consented to this study but either did not complete all of the study questionnaires (n = 11) or discontinued before beginning questionnaires (n = 4) due to lack of time. We found no significant differences between those who completed study measures and those with missing data for any participant sociodemographic variables (cumulative risk exposure, child age, sex, racial/ethnic background, urban versus suburban care site). Eligibility criteria were: (a) child age 2–5 years; (b) absence of child acute (e.g., influenza; cold) or chronic medical condition (e.g., epilepsy) that could impact sleep; (c) absence of a diagnosed neurodevelopmental (e.g., autism) or behavioral health condition (attention-deficit/hyperactivity disorder); (d) absence of a diagnosed sleep disorder (e.g., obstructive sleep apnea); and (e) no current use of medications impacting sleep (e.g., clonidine).
Table I.
Sociodemographic Information and Descriptive Statistics
| Variables | Caregivers, mean (SD)/% | Children, mean (SD)/% |
|---|---|---|
| Female sex | 87.4% | 53.7 |
| Race: Black or African American | 57.6% | 62.9% |
| White | 22.4% | 27.3% |
| Other or multiple races | 4.8% | 7.4% |
| Asian | 4.9% | 2.9% |
| Ethnicity: Hispanic/Latinx | 5.4% | 4.4% |
| Age | 3.3 years (1.1 years) | |
| 18–24 years | 16.6% | |
| 25–29 years | 25.4% | |
| 30–39 years | 45.9% | |
| 40–49 years | 9.1% | |
| ≥50 years | 3.0% | |
|
| ||
| Cumulative risk factors | % | |
|
| ||
| Single caregiver household | 49.8 | |
| Distressed neighborhood | 43.9 | |
| U.S. poverty level: ≤125% | 42.4 | |
| Caregiver ≤high school education | 36.1 | |
| ≥1 moves in the last year | 34.1 | |
| ≥3 children in the household | 29.3 | |
| ≥5 total in the household | 29.3 | |
| Caregiver clinically significant depressive symptoms | 19.5 | |
| Caregiver unemployment | 11.7 | |
|
| ||
| Poor sleep health behaviors | % | |
|
| ||
| One or more electronics item in bedroom | 62.9 | |
| Bedtime later than 9:00 p.m. | 48.3 | |
| Inconsistent bedtime routine (≤4 nights/week) | 40.0 | |
| Insufficient sleep | 35.9 | |
| Consumes caffeine daily | 21.1 | |
|
| ||
| Insomnia symptoms | % | |
|
| ||
| Sleep onset latency ≥30 min | 46.1 | |
| Bedtime resistance | 28.3 | |
| Night awakenings ≥3 times/week | 22.9 | |
| Difficulty falling asleep | 20.5 | |
| Sleep problem | 15.1 | |
|
| ||
| Child psychological functioning | T-score, M (SD) | |
|
| ||
| Internalizing problems | 45.82 (10.66) | |
| Externalizing problems | 46.27 (11.37) | |
| Global executive functioning problems | 47.82 (12.53) | |
Procedure
Caregiver–child dyads attending a well-child or follow-up visit were recruited from primary care clinic waiting rooms operated by a large tertiary-care children’s hospital in southeast Pennsylvania. All caregiver-child dyads present in the waiting room who were potentially eligible based on medical chart review were approached for recruitment. A mix of urban (three sites; 74.1% of sample) and suburban (two sites; 25.9% of sample) clinics were selected to include a sample of families that represented a broad socioeconomic and sociodemographic risk spectrum. The characteristics of the study sample were closely aligned with the larger primary care sites from which participants were recruited, with patients of Black racial/ethnic backgrounds and/or lower SES-families more likely to be seen in the urban (i.e., large metropolitan) practices, which were located in lower-SES zip codes, and patients of non-Latinx White backgrounds more likely to be seen in the suburban practices (Pediatric Research Consortium, 2017). This study was approved by the Children’s Hospital Institutional Review Board and consent was provided by the child’s legal guardian who accompanied the child to the visit. Families received a $25.00 gift card following completion of study procedures.
Measures
Sociodemographic Variables
Child demographic information was extracted from the child’s electronic medical record. Extracted data included child age, sex, race/ethnicity, prematurity (< 37 weeks gestation, as noted in birth history), presence of developmental delays (e.g., speech, motor, language, as noted in problem list), and zip code, which was used to obtain the Economic Innovation Group’s Distressed Communities Index (DCI) (https://eig.org/dci) included in the cumulative risk index (see below). Caregivers reported their age, sex, racial/ethnic background, current employment status, marital status, and educational level, number of adults and children in the family home, number of times family moved within the last year, and family income. Family income, total family household size, and U.S. federal poverty guidelines were used to identify families living ≤125% of the federal poverty level (United States Department of Health and Human Services, 2018). Caregivers also reported depressive symptoms using the 10-item Center for Epidemiological Studies Depression Scale (CES-D-10) (Andresen, Malmgren, Carter, & Patrick, 1994; Cheng, Chan, & Fung, 2006), which has shown good reliability and validity in diverse community samples (Cheng et al., 2006; Cheung, Liu, & Yip, 2007). A score of 10 indicates clinically significant depressive symptoms.
Cumulative Risks
Nine variables based on previous cumulative risk and pediatric sleep research were included in this construct (Appleyard et al., 2005; Atkinson et al., 2015; Bagley & El-Sheikh, 2013; Bagley, Kelly, Buckhalt, & El-Sheikh, 2015; Evans et al., 2013; Hash et al., 2019), consistent with a previous study utilizing this sample (Williamson & Mindell, 2020). The following items were coded dichotomously and summed, with higher scores indicating greater cumulative risk exposure: caregiver unemployment (=1; employed full- or part-time, stay-at-home caregiver or on maternity leave, and student= 0); caregiver high school level education or less (=1; diploma/pre-university/junior college, college/university, and postgraduate= 0); single caregiver household (=1; married and unmarried, living with a partner categories= 0); caregiver clinically significant depressive symptoms (CES-D-10 score of ≥ 10 = 1); household includes ≥3 children (=1); household includes ≥5 people total (=1); family moved ≥1 time in the last year (= 1); family income ≤125% of the U.S. federal poverty guidelines (=1); and family living in a distressed community (=1), based on zip-code level DCI score category quintiles. The DCI score is generated by combining the following seven U.S. Census Bureau’s American Community Survey 5-Year Estimates for 2010–2014: (a) the percent of the population 25 years or older without a high school diploma; (b) the percent housing vacancy rate; (c) the percent of the population ages 25–64 who are without work; (d) the percent of the population living under the poverty line; (e) the median income ratio as a percentage of the state’s median income; (f) the percent change in the number of jobs from the previous Census period; and (g) the percent change in the number of business establishments from the previous Census period. DCI scores are based on geographical ranks which are then averaged and normalized, with scores ranging from 0 to 100 and higher scores indicating more distress.
Insomnia Symptoms
Caregivers completed the Brief Child Sleep Questionnaire (BCSQ), the preschool-aged version of the Brief Infant Sleep Questionnaire. These measures are widely used to assess early childhood sleep, with evidence of strong test-retest reliability and validity for sleep schedule parameters, but potential underestimation of number and duration of nighttime awakenings compared to actigraphy (Kushnir & Sadeh, 2013; Sadeh, 2004; Sadeh, Mindell, Luedtke, & Wiegand, 2009). As in previous research (Daniel et al., 2020), five BCSQ items were selected based on diagnostic criteria for pediatric insomnia, which includes difficulty initiating sleep (typically >30 min), difficulty maintaining sleep, resistance to going to bed, and caregiver concerns about or dissatisfaction with the child’s sleep, with symptoms occurring ≥3 nights per week (AASM, 2014; APA, 2013). To conform with these diagnostic criteria, and in line with previous research (Bruni et al., 2020; Williamson & Mindell, 2020), the following items were coded dichotomously and summed, with higher scores indicating greater insomnia symptoms: bedtime resistance (somewhat difficult, difficult, or very difficult = 1; not difficult = 0); difficulty falling asleep ≥3 nights per week (= 1); sleep onset latency of ≥ 30 min (= 1); night awakenings ≥ 3 nights per week (= 1); and caregiver-perceived sleep problem (small problem, moderate problem, or severe problem = 1, no problem or very small problem = 0; Sadeh, Mindell, & Rivera, 2011).
Poor Sleep Health Behaviors
Five BCSQ items were used to generate a sleep health index based on early childhood sleep recommendations (Allen et al., 2016; Mindell et al., 2009) and in line with previous research (Daniel et al., 2020; Williamson & Mindell, 2020). The following items were dichotomously scored and summed, with higher scores indicating worse sleep health behaviors: bedtime routine implemented ≤4 nights per week (=1); bedtime later than 9:00 p.m. (=1); any electronics items in the child’s bedroom (=1); insufficient sleep (caregiver-reported total [24-hr] sleep duration ≤ the recommended 11 hr total [24-hr] duration for 2-year-olds and 10 hr total [24-hr] duration for 3–5-year-olds = 1); and child consumption of ≥1 caffeinated beverages per day (=1).
Internalizing Problems
Caregiver-reported child internalizing problems were assessed using the internalizing problems composite T-score from the 99-item Child Behavioral Checklist (CBCL) for ages 1.5–5 years, a commonly used measure of child behavior with strong psychometric properties (Achenbach, 2009). Although the CBCL contains a subscale for sleep problems, none of the sleep-related items are included in the internalizing and externalizing scores (Achenbach, 2009). Caregivers were asked to respond to each CBCL on a 3-point Likert scale (not true = 0, somewhat or sometimes true = 1, very true or often true = 2) based on their child’s behavior over the past 6 months. The internalizing problems composite score consists of the emotionally reactive (e.g., sulks), anxiety/depression (e.g., sad mood; fearful), withdrawn (e.g., avoidance of eye contact), and somatic complaints (e.g., stomachaches) subscales. The T-score is generated based on the conversion of raw scores to norm-referenced scores and has a mean of 50 and standard deviation of 10. Clinically significant scores are ≥65.
Externalizing Problems
Caregiver-reported externalizing problems were assessed using the CBCL/1.5–5 years externalizing composite T-score (Achenbach, 2009). Caregivers responded to the CBCL attention problems (e.g., can’t sit still) and aggressive behavior (e.g., fights; is defiant) that comprise the externalizing composite using the Likert scale described above. The mean, standard deviation, and clinical cut-off are as described above.
Global Executive Functioning Problems
Caregivers completed the Behavior Rating Inventory of Executive Functioning—Preschool Version (BRIEF-P) which is a well-validated, 63-item measure consisting of 5 subscales reflecting child inhibition, emotional control, working memory, planning and organization, and ability to shift among tasks (Gioia, Isquith, Guy, & Kenworthy, 2013). The Global Executive Functioning (GEC) score, which consists of these five subscales, was used as the outcome, with raw scores converted to T-score (mean = 50; standard deviation = 10) based on age- and sex-based norms. Clinically significant scores are ≥65.
Statistical Analyses
IBM SPSS v 24 was used to conduct all analyses. Means for continuous variables, proportions for categorical variables, and bivariate correlations were used to generate descriptive statistics. We tested moderation hypotheses using hierarchical linear regression and the PROCESS Macro for SPSS, a tool that automates ordinary least squares regression steps, computation of interaction terms, and probing of interaction effects (Hayes, 2017). Model building followed two steps. First, we fit regression models predicting each outcome variable (child internalizing, externalizing, and global executive functioning T-scores) from both the cumulative risk index and one of the sleep problem indexes (separate sets of models were run for the poor sleep health and insomnia indexes). Using PROCESS we then examined whether there was a change in variance explained (ΔR2) with the addition of the cumulative risk by sleep problem index (insomnia or poor sleep health) interaction term, computed automatically via PROCESS with uncentered variables (Hayes, 2017). We then used PROCESS to plot the interaction terms at low, average, and high values of cumulative risk exposure and sleep problems (−1 SD, mean, +1 SD) and to conduct simple slopes analysis to probe whether each of these effects were significantly different from zero. PROCESS is automatically set to probe all interaction terms with a p-value of <.10; we retained this setting to conserve power given our small sample size and low power for testing interactions and our a priori rationale for examining these effects (Durand, 2013). We used a p-value of <.05 to determine the statistical significance of simple slopes. Covariates in all models included child sex, age, and racial/ethnic background (non-Latinx White = 1), and history of prematurity or developmental delays.
Results
Descriptive Statistics
Table I provides sociodemographic information and descriptive statistics for study variables. Additional information about BCSQ-derived child sleep patterns and environment are shown in Supplementary Table 1. Over ninety percent (90.7%) of children had been exposed to at least one cumulative risk factor, with 15.6% exposed to one risk, 17.6% exposed to two risks, 18.5% exposed to three risks, 16.6% exposed to four risks, 15.1% exposed to five risks, 3.9% exposed to six risks, 2.9% exposed to seven risks, and 0.5% exposed to eight risks. No children experienced all nine risks. Insomnia symptoms were common, with 62.9% of children experiencing at least one symptom. Over one-quarter (28.8%) experienced one symptom, while 12.2% experienced two symptoms, 10.7% experienced three symptoms, 6.3% experienced four symptoms, and 4.4% experienced all five symptoms. With regard to poor sleep health behaviors, 84.5% of caregivers reported ≥1 poor child sleep health behavior; 20% engaged in one unhealthy behavior, 26.2% in two unhealthy behaviors, 24.1% in three unhealthy behaviors, 12.8% in four unhealthy behaviors, and 1.6% engaged in all 5 unhealthy behaviors. Table I shows the prevalence of each cumulative risk factor, insomnia symptom, and poor sleep health behavior, along with descriptive information for child psychological functioning outcomes. The prevalence of clinically significant (≥65) T-scores in the sample was 4.0% for internalizing problems, 7.4% for externalizing problems, and 8.8% for global executive functioning problems. Preliminary bivariate correlations among study variables are shown in Supplementary Table 2.
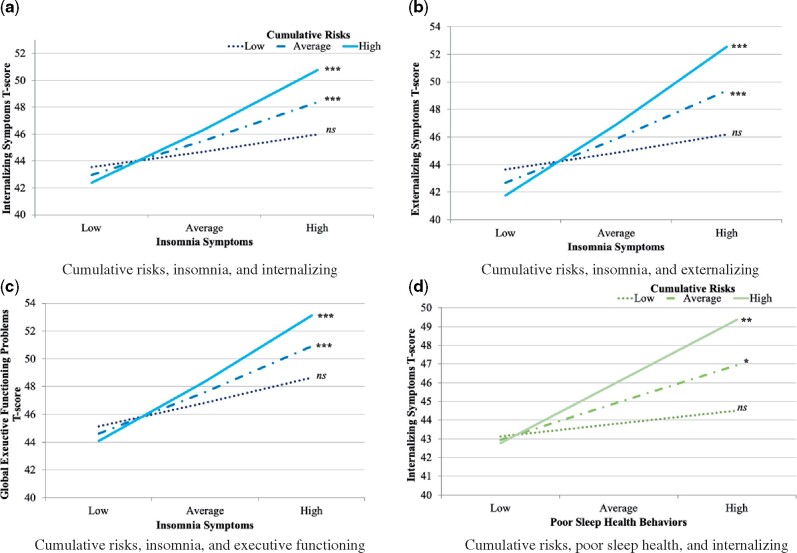
Cumulative Risks, Insomnia Symptoms and Psychological Functioning
Hierarchical regression models for associations among cumulative risks, insomnia symptoms, and child psychological outcomes are provided in Table II. For internalizing problems, in the first step greater insomnia symptoms were significantly linked with greater internalizing problems, whereas cumulative risks were not associated with this outcome. In the second step, insomnia symptoms were no longer significantly associated with the outcome. However, there was a significant interaction effect (Figure 1a). Simple slopes analyses showed that children with average cumulative risk exposure had more internalizing problems in the context of increased insomnia symptoms (b = 3.06 [95% CI 1.78–4.34], SE = 0.65, t = 4.71, p <.001). Those with the highest levels of cumulative risk exposure and the most insomnia symptoms experienced the greatest internalizing problems (b = 4.95 [95% CI 3.22–6.68], SE = 0.87, t = 5.64, p <.001). At lower levels of cumulative risk exposure, insomnia was not significantly associated with internalizing problems.
Table II.
Models for Cumulative Risks, Sleep Problem Indexes, and Child Functioning
| Insomnia symptoms models | Internalizing problems | |||
|---|---|---|---|---|
| Step 1: R2 = .16, F = 6.03, p <.001 |
b (95% CI) |
SE
|
p
|
|
| Child non-White background | 1.65 (−2.13, 5.42) | 1.92 | .390 | |
| Child female sex | 2.91(0.10, 5.71) | 1.42 | .042* | |
| Child age | −1.08(−2.38, 0.21) | 0.66 | .102 | |
| Prematurity and/or developmental delays | 0.43 (−4.04, 4.90) | 2.27 | .851 | |
| Cumulative risks | 0.54 (−0.30, 1.37) | 0.43 | .208 | |
| Insomnia symptoms | 2.29 (1.30, 3.29) | 0.53 | <.001*** | |
| Step 2: ΔR2 =.024, F = 5.55, p =.020 | ||||
| Child non-White background | 1.52 (−2.27, 5.31) | 1.92 | .430 | |
| Child female sex | 3.04 (0.23, 5.84) | 1.42 | .034* | |
| Child age | −1.26 (−2.56, 0.04) | 0.66 | .058+ | |
| Prematurity and/or developmental delays | 0.35 (−4.13, 4.84) | 2.27 | .876 | |
| Cumulative risks | −0.32 (−1.43, 0.80) | 0.57 | .578 | |
| Insomnia symptoms | 0.25 (−2.00, 2.50) | 1.14 | .827 | |
| Cumulative risks × insomnia symptoms | 0.75 (0.12, 1.37) | 0.32 | .020* | |
|
| ||||
| Externalizing problems | ||||
|
| ||||
| Step 1: R2 =.21, F = 8.82, p <.001 | b (95% CI) | SE | p | |
| Child non-White background | −0.31 (−4.20, 3.57) | 1.97 | .874 | |
| Child female sex | 1.20 (−1.68, 4.09) | 1.46 | .412 | |
| Child age | −1.70 (−3.03, −0.37) | 0.68 | .013* | |
| Prematurity and/or developmental delays | 5.36 (0.76, 9.97) | 2.33 | .023* | |
| Cumulative risks | 0.67 (−0.20, 1.53) | 0.44 | .133 | |
| Insomnia symptoms | 2.91 (1.99, 3.93) | 0.52 | <.001*** | |
| Step 2: ΔR2 = .041, F = 10.07, p =.002 | ||||
| Child non-White background | −0.53 (−4.42, 3.37) | 1.98 | .790 | |
| Child female sex | 1.37 (−1.52, 4.26) | 1.46 | .351 | |
| Child age | −1.95 (−3.29, −0.61) | 0.68 | .005* | |
| Prematurity and/or developmental delays | 5.24 (0.63, 9.84) | 2.35 | .026* | |
| Cumulative risks | −0.51 (−1.66, 0.64) | 0.58 | .383 | |
| Insomnia symptoms | 0.03 (−2.35, 2.29) | 1.18 | .978 | |
| Cumulative risks × insomnia symptoms | 1.04 (0.39, 1.68) | 0.33 | .002** | |
|
| ||||
| Global executive functioning problems | ||||
|
| ||||
| Step 1: R2 =.13, F = 5.04, p <.001 | b (95% CI) | SE | p | |
| Child non-White background | 3.29 (−1.13, 7.70) | 2.24 | .144 | |
| Child female sex | 3.63 (0.31, 6.94) | 1.68 | .032* | |
| Child age | 0.13 (−1.41, 1.68) | 0.78 | .866 | |
| Prematurity and/or developmental delays | 2.80 (−2.52, 8.12) | 2.70 | .300 | |
| Cumulative risks | 0.55 (−0.44, 1.54) | 0.50 | .274 | |
| Insomnia symptoms | 2.43 (1.28, 3.59) | 0.59 | <.001*** | |
| Step 2: ΔR2 = .016, F = 3.53, p =.062 | ||||
| Child non-White background | 3.32 (−1.11, 7.74) | 2.24 | .141 | |
| Child female sex | 3.79 (0.46, 7.11) | 1.68 | .026* | |
| Child age | −0.05 (−1.60, 1.50) | 0.78 | .951 | |
| Prematurity and/or developmental delays | 2.70 (−2.63, 8.04) | 2.71 | .319 | |
| Cumulative risks | −0.29 (−1.62, 1.03) | 0.67 | .664 | |
| Insomnia symptoms | 0.79 (−1.75, 3.33) | 1.29 | .541 | |
| Cumulative risks × insomnia symptoms | 0.69 (−0.03, 1.41) | 0.36 | .062+ | |
|
| ||||
| Poor sleep health behaviors models | Internalizing problems | |||
|
| ||||
| Step 1: R2 = 0.10, F = 3.19, p = .005 | b (95% CI) | SE | p | |
| Child non-White background | −1.28 (−5.46, 2.91) | 2.12 | .548 | |
| Child female sex | 3.41 (0.34, 6.48) | 1.56 | .030* | |
| Child age | −1.04 (−2.43, 0.34) | 0.70 | .139 | |
| Prematurity and/or developmental delays | −0.64 (−5.57, 4.30) | 2.50 | .800 | |
| Cumulative risks | 0.62 (−0.34, 1.57) | 0.48 | .205 | |
| Poor sleep health behaviors | 1.63 (0.29, 2.97) | 0.68 | .018* | |
| Step 2: ΔR2 = .015, F = 3.01, p = .084 | ||||
| Child non-White background | −0.64 (−4.86, 3.58) | 2.14 | .764 | |
| Child female sex | 3.67 (0.60, 6.74) | 1.56 | .020* | |
| Child age | −1.00 (−2.38, 0.37) | 0.69 | .152 | |
| Prematurity and/or developmental delays | −0.17 (−5.11, 4.76) | 2.50 | .944 | |
| Cumulative risks | −0.51 (−2.09 1.08) | 0.80 | .531 | |
| Poor sleep health behaviors | −0.10 (−2.48, 2.28) | 1.20 | .934 | |
| Cumulative risks × poor sleep health behaviors | 0.55 (−0.07, 1.17) | 0.31 | .084+ | |
|
| ||||
| Externalizing problems | ||||
|
| ||||
| Step 1: R2 = 0.10, F = 3.11, p = .006 | b (95% CI) | SE | p | |
| Child non-White background | −3.20 (−7.69, 1.29) | 2.28 | .162 | |
| Child female sex | 1.59 (−1.71, 4.89) | 1.67 | .343 | |
| Child age | −1.83 (−3.32, −0.35) | 0.75 | .016* | |
| Prematurity and/or developmental delays | 3.65 (−1.66, 8.95) | 2.69 | .176 | |
| Cumulative risks | 0.91 (−0.11, 1.93) | 0.52 | .081+ | |
| Poor sleep health behaviors | 1.42 (−0.02, 2.86) | 0.73 | .054+ | |
| Step 2: ΔR2 = 0.001, F = 0.16, p = .688 | ||||
| Child non-White background | −3.03 (−7.61, 1.52) | 2.31 | .191 | |
| Child female sex | 1.65 (−1.74, 4.88) | 1.68 | .328 | |
| Child age | −1.82 (−3.31, −0.33) | 0.75 | .017* | |
| Prematurity and/or developmental delays | 3.76 (−1.58, 9.11) | 2.71 | .167 | |
| Cumulative risks | 0.63 (−1.09, 2.35) | 0.87 | .470 | |
| Poor sleep health behaviors | 0.99 (−1.59, 3.56) | 1.30 | .451 | |
| Cumulative risks × poor sleep health behaviors | 0.14 (−0.54, 0.81) | 0.40 | .688 | |
|
| ||||
| Global executive functioning problems | ||||
|
| ||||
| Step 1: R2 = 0.07, F = 2.16, p = .049 | b (95% CI) | SE | p | |
| Child non-White background | 1.16 (−3.84, 6.16) | 2.53 | .647 | |
| Child female sex | 3.93 (0.23, 7.63) | 1.87 | .037* | |
| Child age | 0.05 (−1.62, 1.72) | 0.85 | .953 | |
| Prematurity and/or developmental delays | 1.27 (−0.4.71, 7.26) | 3.03 | .675 | |
| Cumulative risks | 0.62 (−0.52, 1.76) | 0.58 | .285 | |
| Poor sleep health behaviors | 1.17 (−0.46, 2.80) | 0.83 | .159 | |
| Step 2: ΔR2 = 0.003, F = 0.56, p = .456 | ||||
| Child non-White background | 1.46 (−3.61, 6.53) | 2.57 | .570 | |
| Child female sex | 4.03 (0.32, 7.75) | 1.88 | .033* | |
| Child age | 0.08 (−1.60, 1.75) | 0.85 | .929 | |
| Prematurity and/or developmental delays | 1.52 (−4.50, 7.55) | 3.05 | .619 | |
| Cumulative risks | 0.05 (−1.86, 1.95) | 0.97 | .963 | |
| Poor sleep health behaviors | 0.27 (−2.63, 3.16) | 1.47 | .857 | |
| Cumulative risks × poor sleep health behaviors | 0.29 (−0.47, 1.04) | 0.38 | .456 | |
Note. CI = confidence interval; SE = standard error. + p<.10 * p<.05, ** p<.01, *** p<.001.
Figure 1.
Moderation effects. (a) Cumulative risks, insomnia, and internalizing. (b) Cumulative risks, insomnia, and externalizing. (c) Cumulative risks, insomnia, and executive functioning. (d) Cumulative risks, poor sleep health, and internalizing.
Insomnia symptoms were similarly associated with increased externalizing problems, with no significant effect for cumulative risk exposure in step 1 (Table II). At step 2, insomnia symptoms were no longer significantly linked to the outcome, but cumulative risk exposure significantly moderated the association between insomnia and externalizing problems (Figure 1b), such that children with the highest levels of cumulative risk exposure and insomnia symptoms had the highest externalizing T-scores (b = 4.94 [95% CI 3.22–6.68], SE = 0.88, t = 5.64, p <.001). Children with average levels of cumulative risk exposure also had higher externalizing scores in the context of increased insomnia symptoms (b = 3.06 [95% CI 1.78–4.34], SE = 0.65, t = 4.71, p <.001). The slope for children with less cumulative risk exposure across the range of insomnia symptoms was not significant.
Insomnia symptoms were also significantly associated with greater executive functioning concerns in the first model step, with no significant association for cumulative risks. Similar to the previous models, insomnia symptoms were no longer significantly associated when the interaction term was included in the model. We probed the interaction effect, which was <.10 (p = .062). Children with average cumulative risk exposure had worse executive functioning in the context of increased insomnia symptoms (Figure 1c; b = 2.84 [95% CI 1.38–4.29], SE = 0.74, t = 3.86, p<.001), while those with the highest levels of both cumulative risk exposure and insomnia symptoms showed the greatest executive functioning impairments (b = 4.09 [95% CI 2.09–6.08], SE = 1.01, t = 4.04, p<.001).
Cumulative Risks, Poor Sleep Health Behaviors, and Psychological Functioning
As shown in Table II, in the initial step of the model examining cumulative risks, poor sleep health, and internalizing problems, poor sleep health, but not cumulative risk exposure, was associated with greater internalizing problems. Poor sleep health was no longer significant with the addition of the interaction term, which was not statistically significant. We conducted post-hoc probing as the term was <.10 (p = .084). Simple slopes analyses revealed that above average cumulative risk exposure and increased poor sleep health behaviors were linked to significantly greater internalizing problems (Figure 1d; b = 1.52 [95% CI 0.18–2.86], SE = 0.68, t = 2.24, p =.027). Those with the highest levels of both cumulative risk exposure and poor sleep health behaviors also had the greatest internalizing problems (b = 2.51 [95% CI 0.84–4.18], SE = 0.84, t = 2.97, p =.003). The slope for those with lower levels of cumulative risk exposure was not statistically significant. Neither poor sleep health nor cumulative risk exposure was significantly associated with externalizing or with global executive functioning outcomes (Table II). Interaction terms were similarly non-significant, with each p>.10 and we did not probe these effects.
Discussion
In the current study, cumulative risks were not independently associated with child psychological functioning, although cumulative risk exposure has been linked to sleep problems in a previous study with this sample (Williamson & Mindell, 2020) and to child outcomes in other research (Appleyard et al., 2005; Atkinson et al., 2015; Evans et al., 2013). Instead, sleep problems were more consistently associated with these outcomes, especially internalizing concerns, beyond cumulative risk and other child sociodemographics. We also found evidence of moderation, such that children with increased cumulative risk exposure and more insomnia symptoms had the greatest internalizing, externalizing, and executive functioning concerns.
The lack of direct association between cumulative risk exposure and child psychological outcomes is surprising, however there is limited research previous research that considers sleep, cumulative risk exposure, and child psychological functioning simultaneously. Thus, it could be that poor sleep serves as a mechanism linking risk exposure and child outcomes (El-Sheikh et al., 2020; Wetter et al., 2020), but longitudinal research is needed to examine this hypothesis. Our finding that increased insomnia symptoms were associated with significantly greater internalizing, externalizing, and global executive functioning impairments does align with previous research (Bruni et al., 2020; El-Sheikh et al., 2020; Matricciani et al., 2019). Beyond commonly investigated sleep parameters (e.g., sleep duration or night awakenings), the current study found that accumulating caregiver-reported insomnia symptoms are linked with impaired early childhood outcomes, adding to the extant literature on sleep and psychological functioning in early childhood (Reynaud et al., 2018). Putative mechanisms linking insomnia symptoms to these outcomes include impairments in emotion regulation and behavioral control due to poor sleep (Miller, Seifer, Crossin, & Lebourgeois, 2015; Turnbull et al., 2013). It also may be that children with sleep problems reflect a subgroup of children with undiagnosed internalizing and externalizing conditions. Additionally, there may be bidirectional linkages between child sleep and psychological functioning (Conway et al., 2017; Quach et al., 2018), particularly given the co-occurrence of insomnia and behavioral health concerns (Van Dyk, Becker, & Byars, 2019).
Moderation findings for insomnia and cumulative risk indicate that the interactive effect of these concerns amplify child psychological functioning impairments. Psychological stress conferred via increased cumulative risk exposure (Evans et al., 2013) may make it more challenging for families to manage child sleep and behavioral concerns. Some qualitative research has elucidated the ways in which increased environmental stress impacts sleep routines and behaviors in early childhood (Caldwell, Ordway, Sadler, & Redeker, 2020). Collectively, the insomnia findings are clinically meaningful. Although few children in the sample evidenced clinically significant T-scores for internalizing, externalizing, and executive functioning concerns, children with more insomnia symptoms and increased exposure to cumulative risks showed psychological functioning scores up to approximately 10 points (1 standard deviation) higher than children with few insomnia symptoms but similarly increased cumulative risk exposure. These findings also have clinical implications given observed racial, ethnic, and socioeconomic disparities in pediatric sleep and behavioral health (Evans et al., 2013; Howell & McFeeters, 2008; Smith et al., 2019). A recent National Institutes of Health report highlighted the need for more culturally and contextually tailored sleep intervention approaches to address persistent sleep health disparities (Jackson, Walker, Brown, Das, & Jones, 2020), which aligns with our findings. While the direct links between insomnia symptoms and early psychological concerns underscore the need for assessment and treatment of insomnia concerns in outpatient settings, the moderation results highlight the importance of addressing early sleep concerns in the context of cumulative risk exposure in particular.
Although poor sleep health behaviors were associated with increased internalizing symptoms, with children showing greater internalizing problems when poor sleep health behaviors and cumulative risk exposure were increased, no direct or moderation effects were found for externalizing or executive functioning outcomes. The results for internalizing are consistent with a systematic review that found nighttime sleep duration and later bedtimes were linked to internalizing concerns in young children (Reynaud et al., 2018). Previous studies focusing only on insufficient sleep duration have found that sleep curtailment is associated with poor psychological functioning throughout childhood, including externalizing and executive functioning concerns (Matricciani et al., 2019). Our null findings in this study for poor sleep health behaviors could be due to differences in our approach to indexing multiple sleep health behaviors or due to our use of caregiver-reported, versus objectively measured, total (24-hr) sleep duration and behaviors. It is also possible that the impacts of poor sleep health behaviors, including inconsistent bedtime routines, insufficient sleep, and electronics items in the bedroom, have not yet begun to erode specific aspects of psychological functioning, such as externalizing concerns and executive functioning, in early childhood. Overall, future research examining sleep health behaviors and their interplay with cumulative risk exposure is needed.
Study findings should be considered in light of several limitations, including the nature of the cross-sectional study, which precludes any causal assumptions. It could be that child psychological concerns are predictive of subsequent sleep problems, although it is notable that a growing body of research suggests that sleep and psychological problems may interact and lead to cascading impairments over time (Williams et al., 2017). However, available research has either focused primarily on less sociodemographically diverse child samples (Quach et al., 2018; Williams et al., 2017) or on diverse, but older, children (Kelly & El-Sheikh, 2014). More research examining interrelations among these factors as well as cumulative risk exposure is needed, especially in preschool-aged and younger children. Additional studies are especially needed given experimental research indicating that nap deprivation can impair toddlers’ self-regulation strategies (Miller et al., 2015). Although insufficient sleep was based on total, 24-hr sleep, future research should further explore the impact of nighttime versus daytime sleep duration on psychosocial outcomes, especially given that there is considerable variability in napping developmentally, between ages 2 and 5 years, as well as according to child racial/ethnic background (Staton et al., 2020).
Relying on one caregiver reporter for study data could have contributed to shared method variance, thus additional reporters of child behavior (e.g., preschool teachers) and objective estimates of child sleep would be beneficial in future research. In addition, while our use of dichotomous items to capture insomnia symptoms conforms with the dichotomous nature of pediatric insomnia diagnostic criteria (AASM, 2014; APA, 2013), this measure does not capture all criteria necessary for a formal diagnosis of chronic pediatric insomnia, such as the stipulation that symptoms have occurred for 3 or more months, nor does it account for nuanced differences across insomnia symptom profiles. The sleep health behaviors index is also limited in that it does not include other aspects of problematic sleep health behaviors, including sleep time variability, which has been linked to poor child outcomes and is an important indicator of broad sleep health (Meltzer et al., 2021). Additional research is needed to replicate our results, especially in larger samples with increased power to detect interaction effects, given our smaller sample size. Although we included available information about child history of prematurity and developmental delays, these characteristics were recorded by clinicians in the medical record and may not reflect a comprehensive assessment. Future studies should also examine unmeasured child, family, and environmental variables, such as difficult child temperament (Cremone et al., 2018), household chaos (Boles et al., 2017), caregiver stress (McQuillan, Bates, Staples, & Deater-Deckard, 2019), sleep-related cultural beliefs/practices, caregiver work and child school/daycare schedules (Caldwell et al., 2020), and aspects of the sleep environment, such as light, noise, and neighborhood violence exposure (Bagley et al., 2015). These factors may impact both child sleep and behavior, and could theoretically account for these findings. It is also highly important to identify protective factors that could buffer against the development of both sleep problems and behavior concerns in early childhood.
Despite these limitations, this study extends previous research by examining the interplay of modifiable sleep problems, cumulative risk exposure, and psychological outcomes in young children. Study findings provide directions for future research and, more importantly, implications for clinical care. Results of this research suggest that continued identification and treatment of sleep problems, and especially insomnia symptoms, is necessary. While further research is needed, treating insomnia early in development is a potentially fruitful method to buffer against the onset or worsening of critical impairments in child psychological functioning for all children, but particularly those exposed to cumulative risks.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Supplementary Material
Acknowledgments
We are indebted to our colleague Carole L. Marcus, MBBCh, FAASM, who provided mentorship on this study’s design and procedures prior to her unexpected passing. We also want to thank the network of primary care clinicians, their patients, and families for their contribution to this project and clinical research facilities through the Pediatric Research Consortium at Children’s Hospital of Philadelphia. We also thank Nicholas Ambrulavage, Esha Bhandari, Julia Krasny, and Kristen Lanzilotta for their contribution to study data collection. We also thank the Economic Innovation Group for the use of the Distressed Communities Index data. The findings expressed in this publication are solely those of the authors and not necessarily those of the Economic Innovation Group. The Economic Innovation Group does not guarantee the accuracy or reliability of, or necessarily agree with, the information provided herein.
Funding
Dr. Williamson was supported during this study by postdoctoral fellowship T32HL007953-17 from the National Heart, Lung, and Blood Institute, a career development award from the Sleep Research Society Foundation, and K23HD094905 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Conflict of interest: None declared.
References
- Achenbach T. M. (2009). Achenbach system of empirically based assessment (ASEBA): Development, findings, theory, and applications. Burlington, VT: Research Center of Children, Youth & Families. [Google Scholar]
- Allen S. L., Howlett M. D., Coulombe J. A., Corkum P. V. (2016). ABCs of sleeping: A review of the evidence behind pediatric sleep practice recommendations. Sleep Medicine Reviews, 29, 1–14. [DOI] [PubMed] [Google Scholar]
- American Academy of Sleep Medicine (2014). International classification of sleep disorders—Third edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine.
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5). Darien, IL: American Psychiatric Publications.
- AndresenE. M., , MalmgrenJ. A., , CarterW. B., & , Patrick D. L. (1994). Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D (center for epidemiologic studies depression scale). American Journal of Preventive Medicine, 10(2), 77–84. [PubMed] [Google Scholar]
- Appleyard K., Egeland B., Dulmen M. H., Alan Sroufe L. (2005). When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry, 46(3), 235–245. [DOI] [PubMed] [Google Scholar]
- Armstrong J. M., Ruttle P. L., Klein M. H., Essex M. J., Benca R. M. (2014). Associations of child insomnia, sleep movement, and their persistence with mental health symptoms in childhood and adolescence. Sleep, 37(5), 901–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson L., Beitchman J., Gonzalez A., Young A., Wilson B., Escobar M., Chisholm V., Brownlie E., Khoury J. E., Ludmer J., Villani V. (2015). Cumulative risk, cumulative outcome: A 20-year longitudinal study. PLoS One, 10(6), e0127650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BagleyE. J., & , El-Sheikh M. (2013). Familial Risk Moderates the Association Between Sleep and zBMI in Children. Journal of Pediatric Psychology, 38(7), 775–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagley E. J., Kelly R. J., Buckhalt J. A., El-Sheikh M. (2015). What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Medicine, 16(4), 496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black M. M., Walker S. P., Fernald L. C. H., Andersen C. T., DiGirolamo A. M., Lu C., McCoy D. C., Fink G., Shawar Y. R., Shiffman J., Devercelli A. E., Wodon Q. T., Vargas-Barón E., Grantham-McGregor S. (2017). Early childhood development coming of age: Science through the life course. The Lancet, 389(10064), 77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boles R. E., Halbower A. C., Daniels S., Gunnarsdottir T., Whitesell N., Johnson S. L. (2017). Family chaos and child functioning in relation to sleep problems among children at risk for obesity. Behavioral Sleep Medicine, 15(2), 114–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni O., Melegari M. G., Esposito A., Sette S., Angriman M., Apicella M., Caravale B., Ferri R. (2020). Executive functions in preschool children with chronic insomnia. Journal of Clinical Sleep Medicine, 16(2), 231–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckhalt J. A., El‐Sheikh M., Keller P. (2007). Children's sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Development, 78(1), 213–231. [DOI] [PubMed] [Google Scholar]
- Byars K. C., Yolton K., Rausch J., Lanphear B., Beebe D. W. (2012). Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics, 129(2), e276–e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell B., Ordway M., Sadler L., Redeker N. (2020). Parent perspectives on sleep and sleep habits among young children living with economic adversity. Journal of Pediatric Health Care, 34(1), 10–22. [DOI] [PubMed] [Google Scholar]
- Cheng S. T., Chan A., Fung H. H. (2006). Factorial structure of a short version of the center for epidemiologic studies depression scale. International Journal of Geriatric Psychiatry, 21(4), 333–336. [DOI] [PubMed] [Google Scholar]
- Cheung Y. B., Liu K. Y., Yip P. S. (2007). Performance of the CES-D and its short forms in screening suicidality and hopelessness in the community. Suicide and Life-Threatening Behavior, 37(1), 79–88. [DOI] [PubMed] [Google Scholar]
- Conway A., Miller A. L., Modrek A. (2017). Testing reciprocal links between trouble getting to sleep and internalizing behavior problems, and bedtime resistance and externalizing behavior problems in toddlers. Child Psychiatry & Human Development, 48(4), 678–689. [DOI] [PubMed] [Google Scholar]
- Cremone A., de Jong D. M., Kurdziel L. B. F., Desrochers P., Sayer A., LeBourgeois M. K., Spencer R. M. C., McDermott J. M. (2018). Sleep tight, act right: Negative affect, sleep and behavior problems during early childhood. Child Development, 89(2), e42–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel L. C., Childress J. L., Flannery J. L., Weaver-Rogers S., Garcia W. I., Bonilla-Santiago G., Williamson A. A. (2020). Identifying modifiable factors linking parenting and sleep in racial/ethnic minority children. Journal of Pediatric Psychology, 45(8), 867–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand C. P. (2013). Does raising type 1 error rate improve power to detect interactions in linear regression models? A simulation study. PLoS One, 8(8), e71079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M., Shimizu M., Philbrook L. E., Erath S. A., Buckhalt J. A. (2020). Sleep and development in adolescence in the context of socioeconomic disadvantage. Journal of Adolescence, 83, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G. W. (2004). The environment of childhood poverty. American Psychologist, 59(2), 77–92. [DOI] [PubMed] [Google Scholar]
- Evans G. W., Li D., Whipple S. S. (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342–1396. [DOI] [PubMed] [Google Scholar]
- Gioia G. A., Isquith P. K., Guy S. C., Kenworthy L. (2013). Behavior rating inventory of executive function: BRIEF. Psychological Assessment Resources: FL. [Google Scholar]
- Hash J. B., Oxford M. L., Fleming C. B., Ward T. M., Spieker S. J., Lohr M. J. (2019). Impact of a home visiting program on sleep problems among young children experiencing adversity. Child Abuse & Neglect, 89, 143–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Publications. [Google Scholar]
- Howell E., McFeeters J. (2008). Children's mental health care: Differences by race/ethnicity in urban/rural areas. Journal of Health Care for the Poor and Underserved, 19(1), 237–247. [DOI] [PubMed] [Google Scholar]
- Jackson C. L., Walker J. R., Brown M. K., Das R., Jones N. L. (2020). A workshop report on the causes and consequences of sleep health disparities. Sleep, 43(8), zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly R. J., El-Sheikh M. (2014). Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology, 50(4), 1137–1147. [DOI] [PubMed] [Google Scholar]
- Kushnir J., Sadeh A. (2013). Correspondence between reported and actigraphic sleep measures in preschool children: The role of a clinical context. Journal of Clinical Sleep Medicine, 09(11), 1147–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkelä T. E., Peltola M. J., Saarenpää‐Heikkilä O., Himanen S. L., Paunio T., Paavonen E. J., Kylliäinen A. (2020). Night awakening and its association with executive functioning across the first two years of life. Child Development, 91(4), e937–e951. [DOI] [PubMed] [Google Scholar]
- Matricciani L., Paquet C., Galland B., Short M., Olds T. (2019). Children’s sleep and health: A meta-review. Sleep Medicine Reviews, 46, 136–150. [DOI] [PubMed] [Google Scholar]
- McQuillan M., Bates J., Staples A., Deater-Deckard K. (2019). Maternal stress, sleep, and parenting. Journal of Family Psychology, 33(3), 349–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Williamson A. A., Mindell J. (2021). Pediatric sleep health: It matters, and so does how we define it. Sleep Medicine Reviews, 57, 101425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A. L., Seifer R., Crossin R., Lebourgeois M. K. (2015). Toddler's self‐regulation strategies in a challenge context are nap‐dependent. Journal of Sleep Research, 24(3), 279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell J. A., Meltzer L. J., Carskadon M. A., Chervin R. D. (2009). Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America poll. Sleep Medicine, 10(7), 771–779. [DOI] [PubMed] [Google Scholar]
- Nelson T. D., Nelson J. M., Kidwell K. M., James T. D., Espy K. A. (2015). Preschool sleep problems and differential associations with specific aspects of executive control in early elementary school. Developmental Neuropsychology, 40(3), 167–180. [DOI] [PubMed] [Google Scholar]
- Pediatric Research Consortium (2017). CHOP Care Network Information. https://perc.research.chop.edu/sites/default/files/CHOP-Care-Network-Information-for-grants-2017.pdf. Retrieved December 21, 2020.
- Quach J., Nguyen C., Williams K., Sciberras E. (2018). Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatrics, 172(2), e174363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynaud E., Vecchierini M. F., Heude B., Charles M. A., Plancoulaine S. (2018). Sleep and its relation to cognition and behaviour in preschool‐aged children of the general population: A systematic review. Journal of Sleep Research, 27(3), e12636. [DOI] [PubMed] [Google Scholar]
- Sadeh A. (2004). A brief screening questionnaire for infant sleep problems: Validation and findings for an internet sample. Pediatrics, 113(6), e570–e577. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Mindell J. A., Luedtke K., Wiegand B. (2009). Sleep and sleep ecology in the first 3 years: A web-based study. Journal of Sleep Research, 18(1), 60–73. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Mindell J. A., Rivera L. (2011). My child has a sleep problem”: A cross-cultural comparison of parental definitions. Sleep Medicine, 12(5), 478–482. [DOI] [PubMed] [Google Scholar]
- Sivertsen B., Harvey A. G., Reichborn-Kjennerud T., Torgersen L., Ystrom E., Hysing M. (2015). Later emotional and behavioral problems associated with sleep problems in toddlers: A longitudinal study. JAMA Pediatrics, 169(6), 575–582. [DOI] [PubMed] [Google Scholar]
- Smith J. P., Hardy S. T., Hale L. E., Gazmararian J. A. (2019). Racial disparities and sleep among preschool aged children: A systematic review. Sleep Health, 5(1), 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staton S., Rankin P. S., Harding M., Smith S. S., Westwood E., LeBourgeois M. K., Thorpe K. J. (2020). Many naps, one nap, none: A systematic review and meta-analysis of napping patterns in children 0–12 years. Sleep Medicine Reviews, 50, 101247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras E. M., Rifas-Shiman S. L., Bub K. L., Gillman M. W., Oken E. (2017). Prospective study of insufficient sleep and neurobehavioral functioning among school-age children. Academic Pediatrics, 17(6), 625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull K., Reid G. J., Morton J. B. (2013). Behavioral sleep problems and their potential impact on developing executive function in children. Sleep, 36(7), 1077–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (2018). U.S. Federal poverty guidelines used to determine financial eligibility for certain federal programs. https://aspe.hhs.gov/poverty-guidelines. Retrieved August 12, 2020.
- Van Dyk T., Becker S. P., Byars K. C. (2019). Mental health diagnoses and symptoms in preschool and school age youth presenting to insomnia evaluation: Prevalence and associations with sleep disruption. Behavioral Sleep Medicine, 17(6), 790–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter S. E., Fuhs M., Goodnight J. A. (2020). Examining sleep as a protective mechanism for executive functioning in children from low-income homes. Early Child Development and Care, 190(15), 2380–2391. [Google Scholar]
- Williams K., Berthelsen D., Walker S., Nicholson J. (2017). A developmental cascade model of behavioral sleep problems and emotional and attentional self-regulation across early childhood. Behavioral Sleep Medicine, 15(1), 1–21. [DOI] [PubMed] [Google Scholar]
- Williamson A. A., Mindell J. A. (2020). Cumulative socio-demographic risk factors and sleep outcomes in early childhood. Sleep, 43(3), zsz233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson A. A., Mindell J. A., Hiscock H., Quach J. (2019). Sleep problem trajectories and cumulative socio-ecological risks: Birth to school-age. The Journal of Pediatrics, 215, 229–237. e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.