Landmark studies have demonstrated that wrist-worn wearable devices (eg, smartwatches, fitness bands) can provide potentially actionable data to improve real-time surveillance of respiratory diseases, such as influenza,1 and facilitate the detection of irregular heart rhythms.2 Although these tools undoubtedly will transform health care and energize scientific research, important ethical, legal, and social issues have been raised and require careful public deliberation.3 We have identified another aspect of the digital health revolution that has not yet received due attention: the unanticipated and potentially negative effects of wearable devices on patients’ psychological health, quality of life, and health care utilization.
Although unlimited access to digital health information can motivate some individuals to engage in healthy behaviors, these data may inadvertently contribute to pathologic symptom monitoring and impaired function in others. Patients with intermittent atrial fibrillation (AF) may be especially susceptible to excessive cardiac monitoring with a wearable device given the transient, unpredictable nature of arrhythmias and the ongoing risk of recurrence despite medical or procedural therapy. Anxiety is prevalent among those with AF and has been associated with a higher AF symptom burden, worse quality of life, and increased health care consumption.4,5 Thus, technologies that heighten awareness and attention to normal and potentially abnormal fluctuations in heart rates may lead to substantial increases in anxiety in predisposed persons and prompt unnecessary medical care.
To illustrate this point, we describe a case from our cardiology clinic of a 70-year-old woman with paroxysmal AF. One year after her initial AF diagnosis, a clinical health psychologist (LR) diagnosed her as having new-onset health anxiety that was primarily triggered by excessive cardiac monitoring with a commercially available smartwatch. No evidence of previous mental health problems was noted in her medical records. She had hypertension, a moderate risk of stroke (CHA2DS2-VASc score 3), and arrhythmia burden <1%, and she was compliant with oral anticoagulation and antihypertensive therapies. Smartwatch data provided by the patient revealed that she had performed 916 electrocardiograms (ECGs) over a 1-year period. Of those ECG recordings, 701 were sinus rhythm, 55 were possible AF, 30 indicated low or high heart rate, and 130 were inconclusive. As shown in Figure 1, smartwatch ECG monitoring increased over time. Acute escalations in ECG-taking behaviors were frequently triggered by smartwatch notifications that were either innocuous (eg, transient exercise-induced elevations in heart rate), inconclusive, or indicative of possible AF. Notably, irregular rhythm notifications and findings of uncertain significance (“inconclusive” ECG) produced a relatively similar behavioral response, suggesting that ambiguous data may have been misinterpreted as actual health threats.
Figure 1.
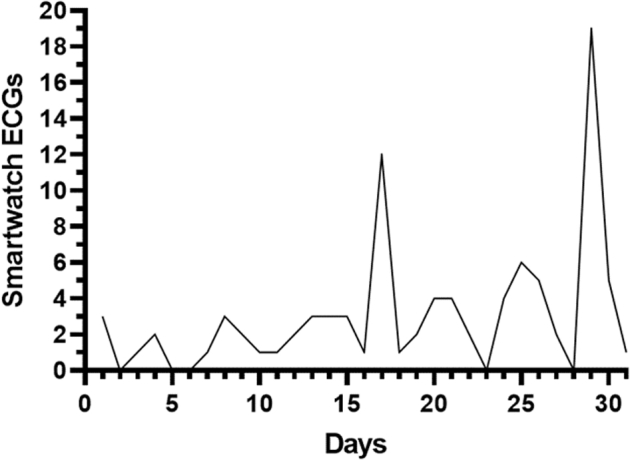
Number of patient-initiated electrocardiographic (ECG) recordings obtained during the first month of device ownership. Note the marked increase in recordings after smartwatch notifications for an “inconclusive” ECG on day 17 and possible atrial fibrillation on day 29. Data obtained from January 2018 to January 2019.
Based on diagnostic interview and validated questionnaires,6,7 it became apparent that our patient had developed an enduring belief that smartwatch notifications were a sign of worsening cardiac function, leading to a vicious cycle of excessive worry, preoccupation with cardiac stimuli and sensations, and compensatory behaviors (eg, habitual cardiac monitoring with the smartwatch and repeatedly seeking reassurance from health care professionals). Despite repeated medical assessment and reassurance, this maladaptive pattern resulted in 12 ambulatory clinic and emergency department visits and numerous telephone calls to health care providers. Because she was asymptomatic and receiving appropriate anticoagulation therapy, none of these clinical encounters led to alterations in medical treatment. Furthermore, her constant worry and frequent health care visits had a profoundly negative impact on her mental health, relationships, and quality of life. The patient was referred to our cardiac psychologist (LR) for further psychological evaluation, and she ultimately was diagnosed with illness anxiety disorder (formerly known as hypochondriasis). The patient subsequently completed 6 sessions of cognitive behavioral therapy to target health anxiety8 associated with AF, which resulted in complete symptom remission.
The notion that fear and uncertainty may drive some patients with AF to engage in hypervigilant self-monitoring behaviors with a wearable device to “control” or mitigate distress associated with an unpredictable heart rhythm disorder should come as no surprise. Our observations are consistent with established theoretical models (eg, Uncertainty and Anticipation Model of Anxiety [UAMA])9 and are well supported by decades of neurobiological research demonstrating a robust relationship among uncontrollable stress, unpredictable aversive health events, reassurance-seeking behaviors, and the development of health anxiety.9 In this context, wearable health technologies likely fuel the phenomenon. Unlike traditional clinical visits, which can be expensive or infrequent, wearables provide an unprecedented level of access to on-demand health data via affordable, highly engaging, and, in some cases, Food and Drug Administration–approved devices that continuously reinforce somatic preoccupation. In susceptible persons, this may bolster the belief that even those with AF who are at low risk and are receiving appropriate anticoagulation therapy should seek care, even when it is not necessary.
Although the prevalence, clinical course, and associated outcomes of this phenomenon remain unknown, an increasing number of cases have been reported anecdotally by colleagues at our institution and other medical centers nationwide. This suggests that our patient may represent the tip of an iceberg. By highlighting the practical difficulties clinicians may face in managing this phenomenon, we hope to stimulate thoughtful discussion and robust research into the co-occurrence of health anxiety and wearable devices in patients with arrhythmias and other medical conditions.
Important questions warrant further investigation. First, when and in whom is this condition most likely to manifest? Because individuals with underlying anxiety have elevated threat expectancies and heightened responses to uncertainty,9 they may be more likely to develop this maladaptive pattern of behavior. However, more studies are needed to draw firm conclusions in this regard. Second, how does this pathology affect clinical and quality-of-life outcomes; provider burden/workflow; and health care utilization and expenditures? Another consideration is the inevitability of false-positive results. How do patients cope with discrepancies between data obtained from a wearable device compared to that from a clinic visit? How do these findings affect patients’ trust and satisfaction with their providers and the health care system? Further research in these areas will facilitate the adaptation of existing theoretical models of anxiety to address this contemporary clinical phenomenon. In addition, a more nuanced understanding of these issues is essential to educate the public about incidental findings and inform best practices for managing patients’ questions and concerns about wearable health technology.
Wearables can play an important role in promoting patient empowerment and health care engagement. However, this will require active involvement and strong collaboration among all stakeholders—technology companies, behavioral scientists, health care practitioners, researchers, patients, and caregivers—to understand the ways in which diverse segments of society (eg, older adults, individuals with medical and mental health issues) interact with this technology.
Funding Sources
This study was supported by a grant from the National Heart, Lung, and Blood Institute of the National Institutes of Health to Dr Rosman (K23HL141644).
Disclosures
Dr Gehi receives research support from Bristol-Myers Squibb Foundation; consulting fees from Biosense Webster; and speaker’s honoraria from Abbott, Biotronik, and Zoll Medical. Dr Lampert receives research support from Medtronic, Boston Scientific, and Abbott; consulting fees from Medtronic; and honoraria from Medtronic and Abbott. Dr Rosman has reported that she has no conflicts relevant to the contents of this paper to disclose.
References
- 1.Radin J.M., Wineinger N.E., Topol E.J., Steinhubl S.R. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: a population-based study. Lancet Digital Health. 2020;2:E85–E93. doi: 10.1016/S2589-7500(19)30222-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perez M.V., Mahaffey K.W., Hedlin H., et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med. 2019;381:1909–1917. doi: 10.1056/NEJMoa1901183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sim I. Mobile devices and health. N Engl J Med. 2019;381:956–968. doi: 10.1056/NEJMra1806949. [DOI] [PubMed] [Google Scholar]
- 4.Kivimaki M., Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018;15:215–229. doi: 10.1038/nrcardio.2017.189. [DOI] [PubMed] [Google Scholar]
- 5.Baumgartner C., Fan D., Fang M.C., et al. Anxiety, depression, and adverse clinical outcomes in patients with atrial fibrillation starting warfarin: Cardiovascular Research Network WAVE Study. J Am Heart Assoc. 2018;7:e007814. doi: 10.1161/JAHA.117.007814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eifert G.H., Thompson R.N., Zvolensky M.J., et al. The cardiac anxiety questionnaire: development and preliminary validity. Behav Res Ther. 2000;38:1039–1053. doi: 10.1016/s0005-7967(99)00132-1. [DOI] [PubMed] [Google Scholar]
- 7.Rosman L., Whited A., Lampert R., Mosesso V.N., Lawless C., Sears S.F. Cardiac anxiety after sudden cardiac arrest: severity, predictors and clinical implications. Int J Cardiol. 2015;181:73–76. doi: 10.1016/j.ijcard.2014.11.115. [DOI] [PubMed] [Google Scholar]
- 8.Axelsson E., Andersson E., Ljótsson B., Björkander D., Hedman-Lagerlöf M., Hedman-Lagerlöf E. Effect of Internet vs face-to-face cognitive behavior therapy for health anxiety: a randomized noninferiority clinical trial. JAMA Psychiatry. 2020:e200940. doi: 10.1001/jamapsychiatry.2020.0940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grupe D.W., Nitschke J.B. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat Rev Neurosci. 2013;14:488–501. doi: 10.1038/nrn3524. [DOI] [PMC free article] [PubMed] [Google Scholar]


