Abstract
Objective:
The role of simultaneous alcohol and marijuana (SAM) use in the experience of blackouts among college students is unclear. To clarify discrepancies, the current study evaluated whether the association between SAM user status and blackouts was moderated by high-intensity drinking (HID).
Participants and Methods:
College students (N = 1,224; 63.7% female) reported on their past year experiences of blackout, marijuana use, SAM use, and HID (i.e., drinking at least twice the binge threshold).
Results:
SAM users had more past year blackouts than non-SAM users, but this effect was only significant among SAM users who had engaged in HID in the past year (non-binge: F(5,37) = 0.50, p = 0.49; binge: F(5,138) = 0.23, p = 0.63; HID: F(5,328) = 4.52, p = 0.03).
Conclusions:
Effects of SAM user status on the experience of alcohol-related blackouts may be limited to individuals who engage in HID.
Keywords: blackout, high intensity drinking, marijuana use, alcohol use, simultaneous alcohol and marijuana use
Introduction
Alcohol-induced blackouts refer to periods of impaired memory formation during a drinking episode1. While in a blackout state, individuals may appear relatively normal and engage in tasks, despite not encoding these events into long-term memory2,3. About half of individuals who drink socially will experience a blackout in their lifetime4,5. Blackouts are arguably one of the more serious acute consequences of alcohol use and are associated with various negative outcomes, including sexual victimization6,7 and injury8,9. Blackouts may also serve as behavioral indicators of the impact of alcohol use on the brain10.
As would be expected, level of alcohol consumption is one important predictor of blackout, with heavy alcohol consumption often preceding these experiences11,12. An extreme form of binge drinking, known as high-intensity drinking (HID; i.e., drinking at least twice the binge threshold of 4+/5+ drinks for women/men, respectively), is particularly associated with risk for experiencing acute physiological consequences of alcohol use, including blackouts13. While twice the binge threshold is the typical cutoff for HID, some studies have explored the possible utility of an additional HID-3 cutoff (i.e., drinking at least three times the binge threshold13–17). The distinction between HID-2 and HID-3 may be particularly useful for more severe alcohol-related consequences like blackout. For example, in one study of adult Australians, individuals who drank to HID-3 levels were significantly more likely to report blackouts compared to those who drank to HID-2 levels13.
Other factors, such as simultaneous alcohol and marijuana (SAM) use, may also play a role in the experience of alcohol-related consequences, including blackouts. Two recent studies comparing individuals who use alcohol and marijuana simultaneously to those who use the two substances concurrently (i.e., non-simultaneously) found that SAM users reported higher rates of alcohol-induced blackouts than concurrent users18,19. Other research using daily diary reports has found increased rates of alcohol consequences on SAM use days compared to alcohol only days, despite no differences in level of consumption or subjective intoxication20. These findings suggest that using marijuana simultaneously with alcohol confers added risk.
However, some studies have cast doubt on the role of SAM use in blackouts. In an ecological momentary assessment study of college students, SAM use did not increase the likelihood of experiencing a blackout at the event-level11. Similarly, another event-level study found that binge drinking occasions did not differ from binge drinking plus marijuana use occasions in terms of consequences experienced, suggesting that adding marijuana posed no additional risk for consequences (including blackouts) beyond that already posed by binge drinking21. Some of these conflicting findings may be due to simultaneous marijuana use only conferring additional risk for blackout under certain drinking conditions. Given that HID is strongly associated with blackouts13, those who engage in HID may be especially vulnerable to risk associated with SAM use.
Present Study
In a large college student sample (n = 1,234), we assessed the prevalence of HID, marijuana use, SAM use, and blackout. Potential interactive effects of HID and SAM use on blackout occurrence and frequency were explored among the subset of college students who had consumed alcohol in the past year (n = 997). We hypothesized that the effects of SAM use on blackout would be stronger among those who consumed alcohol at the high-intensity level than those who consumed at the binge or non-binge levels. We further hypothesized that this effect would be detected in a step-wise fashion across levels of drinking (i.e., non-binge, binge, HID-2, and HID-3).
Materials and Methods
Participants
Study procedures were approved by the University of Missouri Institutional Review Board. Participants were 1,234 students who completed an online survey for course extra credit. 63.9% of participants were female, and most were college freshmen (81.3%; see Table 1). Participants were about 18 years old on average (M = 18.42, SD = 1.07, range = 17–31). The sample was representative of the state population, with the exception that there was a higher proportion of individuals of mixed race/ethnicity in the current sample as compared to the state (2.3%)22; 77.1% were white, 10.3% were of mixed race/ethnicity, 6.6% were Black/African American, 3.2% were Asian/Pacific Islander, 1.6% were Hispanic/Latino, < 1% were Native American or “other”.
Table 1.
Sample characteristics and substance use behaviors.
| Mean (SD) or % (N) | χ2 difference | |||
|---|---|---|---|---|
| Full Sample (N=1234) |
Men 35.71 (n=436) |
Women 63.88 (n=780) |
||
| Age | 18.42 (1.07) | 18.68 (1.40) | 18.28 (0.79) | 48.42* |
| Year in school | % (n) | % (n) | % (n) | 25.64* |
| Freshman | 81.33 (989) | 75.00 (324) | 85.20 (662) | - |
| Sophomore | 12.58 (153) | 15.05 (65) | 11.07 (86) | - |
| Junior | 3.95 (48) | 6.25 (27) | 2.57 (20) | - |
| Senior and above | 2.14 (26) | 3.71 (16) | 1.16 (9) | - |
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age of first alcohol use | 16.07 (1.57) | 15.95 (1.85) | 16.16 (1.35) | 33.00* |
| Age of first marijuana use | 16.42 (1.68) | 16.29 (1.87) | 16.52 (1.51) | 27.58 |
| Lifetime Measures | % (n) | % (n) | % (n) | |
| Blackout | 39.47 (461) | 42.44 (174) | 37.72 (281) | 2.47 |
| Marijuana use | 55.34 (637) | 60.45 (243) | 52.51 (387) | 6.63 |
| SAM use | 40.46 (462) | 43.78 (176) | 38.60 (281) | 2.89 |
| Blackout after SAM use | 20.40 (225) | 24.10 (94) | 17.95 (126) | 5.90 |
| Past Year Measures | % (n) | % (n) | % (n) | |
| Any HID | 43.72 (508) | 55.53 (226) | 36.98 (274) | 36.78* |
| Blackout | 32.79 (383) | 37.56 (154) | 30.20 (225) | 6.50 |
| Marijuana use | 44.81 (553) | 50.00 (218) | 42.18 (329) | 6.91 |
| SAM use | 32.84 (375) | 36.57 (147) | 30.77 (224) | 3.95 |
| Blackout after SAM use | 9.25 (102) | 11.79 (46) | 7.55 (53) | 5.48 |
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Number of blackouts | 3.55 (2.76) | 3.85 (3.04) | 3.29 (2.46) | 15.15 |
Note:
indicates significance at a Bonferroni-adjusted p-value of 0.0036. SAM = simultaneous alcohol and marijuana, HID = high-intensity drinking. Number of blackouts were recoded such that ‘never/none’ = 0, ‘1’ = 1, ‘2–5’ = 3.5, ‘6–10’ = 8, and ‘more than 10’ = 10.
Measures
Quantity and Frequency of Alcohol Use.
Typical quantity of alcohol use was assessed by asking, “During the last 12 months, how many alcoholic drinks did you have on a typical day when you drank alcohol?” Response options ranged from ‘1 drink’ to ‘25 or more drinks,’ with an additional option for individuals who had not consumed alcohol in the past year. Typical frequency of use was assessed with the question: “During the last 12 months, how often did you usually have any kind of drink containing alcohol?” Response options ranged from ‘Never’ to ‘every day.’ Participants who had consumed alcohol provided the age at which they had their first drink.
High-Intensity Drinking.
In the current study, two levels of HID were assessed: HID-2 (i.e., drinking twice the binge threshold; 8–11/10–14 drinks for females/males) and HID-3 (i.e., drinking 3 times the binge threshold; 12+/15+ drinks for females/males). HID-2 was assessed with the question: “During the last 12 months, how often did you have 8 to 11 (for females) or 10 to 14 (for males) drinks containing any kind of alcohol on the same occasion?” HID-3 was assessed with a similar question but substituting the 12+/15+ cutoff. Participants were also asked about the frequency with which they engage in binge drinking (women: 4–7 drinks, men: 5–9 drinks). Response options for these items ranged from ‘never’ to ‘every day.’ Three-level (non-binge, binge, any HID) and four-level (non-binge, binge, HID-2, HID-3) past year HID status variables were created based on the peak drinking level reported by a participant.
Marijuana Use.
Participants reported frequency of marijuana use, age of initiation, and SAM use. To assess frequency of use, participants were asked, “During the last 12 months, how often did you usually use marijuana?” Response options ranged from ‘1 or 2 times in the past year’ to ‘every day.’ Participants could also indicate they had not used marijuana in the past year or that they had never used marijuana. Next, participants completed questions regarding SAM use. Participants were asked, “During the last 12 months, have you used marijuana at the same time as alcohol?” Participants could indicate yes; that they had not used the two substances together in the past year, but had before; or that they had never done so. Individuals who reported past year SAM use were considered SAM users, while those who had not done so in the past year were considered non-SAM users.
Participants also provided some indirect information on their frequency of SAM use. In the interest of exploring the temporality of alcohol and marijuana use within a substance using episode, participants were asked how often they consumed marijuana after drinking (never, almost never, less than half the time, about half the time, more than half the time, almost always, always) and how often they drank alcohol after using marijuana (same response options).
Blackouts.
Participants were asked the number of times they had experienced blackouts with the following item: “During the last 12 months, approximately how many times have you had an alcohol-related blackout where you forgot parts of a drinking episode (e.g., not remembering how you got home, forgetting something you said to others while drinking, etc.)?” Responses were used to code dichotomous indicators of lifetime and past year occurrence of blackout, as well as frequency in the past year. Blackout frequency was coded such that never/none = 0, ‘1’ = 1, ‘2–5’ = 3.5, ‘6–10’ = 8, and ‘more than 10’ = 10. Participants also reported on whether they had experienced a blackout in their lifetime or in the past year following SAM use.
Data Analysis
Descriptive analyses were conducted within SAS 9.4 to examine the prevalence and frequency of blackouts, HID, marijuana use, and SAM use, along with sample characteristics (see Table 1). When testing for sex differences in substance use behaviors and consequences, a Bonferroni adjusted significance threshold of 0.0036 was used (0.05/14 comparisons = 0.0036). Remaining analyses were conducted among the subset of past year drinkers (n = 997). Binary logistic regressions were used to predict blackout occurrence, and general linear models were used to predict the frequency of blackouts. All models controlled for gender and past-year quantity and frequency of alcohol use. Models examining SAM user status as a predictor controlled for frequency of marijuana use as well. To investigate whether effects of SAM use varied as a function of HID status, models were fit including interaction terms between SAM user status and past year HID status (i.e., a participant’s peak drinking level in the past year: HID, binge, or non-binge) to predict blackout.
Results
Prevalence of Substance Use Behaviors
Descriptive statistics are presented in Table 1. The majority of the sample reported using alcohol in their lifetime (84.9%) and the past year (80.0%), with average drinking onset around age 16 (M = 16.07, SD = 1.57). Of those who had consumed alcohol in the past year (n = 997), three-quarters of male alcohol users (74.14%) and half of female alcohol users (49.81%) had engaged in HID-2 drinking. Over half of men (61.03%) and 29.68% of women had consumed alcohol to HID-3 levels. Over a third of participants who drank in the past year reported they had experienced a blackout (38.82%). Among individuals with a history of HID-2 drinking (but not HID-3 drinking) in the past year, 44.81% reported experiencing a blackout, and among those who drank to HID-3 levels, 65.31% had experienced a blackout. On average, individuals who had experienced a blackout reported having 2 to 5 blackouts in the past year (M = 3.55, SD = 2.76).
Lifetime marijuana use was reported by over half (55.3%) the sample, with first use typically occurring at age 16 (M = 16.42, SD = 1.68; see Table 1). Rates were even higher among the subset of those who had consumed alcohol in the past year, with almost three-quarters endorsing lifetime marijuana use (71.53%). Most of those who had ever used marijuana in their lifetime had also used it in the past year (86.8%), on average 2 to 3 times a month (M = 3.89, SD = 2.66).
SAM use was very common. Of those who had used marijuana, 76.09% reported lifetime and 67.15% reported past-year SAM use. Among lifetime SAM users, using marijuana after drinking alcohol appeared to be slightly more common (M = 1.86, where ‘2’ corresponds to using marijuana less than half the time after using alcohol, SD = 1.39) than the alternate of drinking alcohol after using marijuana (M = 1.43, where ‘1’ corresponds to using alcohol almost never after marijuana use, SD = 1.10). Just over half of lifetime SAM users said they had experienced a blackout following SAM use (51.65%), and about a quarter had experienced a blackout after SAM use in the past year (23.58%).
Independent Associations of High Intensity Drinking and Simultaneous Alcohol and Marijuana Use with Blackout
Any past year HID (i.e., either HID-2 or HID-3) was associated with greater odds of experiencing a blackout (OR = 2.69 [1.86 – 3.89]) and higher frequency of blackout (F1,954 = 15.36, p < 0.0001, model R2 = .30). Gender was not related to blackout occurrence (OR = 0.68 [0.47 – 0.97]) or frequency (F1,954 = 0.76, p = 0.39). As expected, greater quantity and frequency of past year alcohol use was associated with increased likelihood of experiencing a blackout (quantity: OR = 1.15 [1.07 – 1.24]; frequency: OR = 1.60 [1.44 – 1.76]) and with more frequent blackouts (quantity: F1,954 = 38.96, p < 0.0001; frequency: F1,954 = 94.30, p < 0.0001).
After controlling for self-reported past year quantity and frequency of alcohol use, engaging in more frequent HID-2 drinking was associated with increased odds of experiencing a blackout (OR = 1.15 [1.01 – 1.29]) and with experiencing a greater number of past-year blackouts (F1,955 = 44.49, p < 0.0001; model R2 = 0.32). HID-3 drinking frequency was not significantly associated with blackout occurrence after accounting for quantity and frequency of past year drinking (OR = 1.05 [0.94 – 1.19]), but HID-3 frequency was associated with a greater number of past-year blackouts (F1,954 = 38.69, p < 0.0001; model R2 = 0.32).
Engaging in past year SAM use was associated with an 82% increase in the likelihood of experiencing a blackout (OR = 1.82 [1.20 – 2.78]), even after accounting for the quantity and frequency of past-year alcohol use and frequency of marijuana use. Among participants who had used alcohol and marijuana in the past year (n = 540), those who engaged in SAM use were more likely to report experiencing a blackout compared to those who used the two substances concurrently (61.86% vs. 36.49%, respectively; t(500)= −5.34, p < 0.0001). SAM users also reported a greater number of past year blackouts than those who used alcohol and marijuana concurrently (2.50 vs. 1.20, respectively; t(500) = −4.71, p < 0.0001).
Does the Effect of Simultaneous Alcohol and Marijuana Use Depend on High Intensity Drinking Status?
Among participants who used alcohol and marijuana in the past year (n = 540), there was a significant interaction between SAM user status and past-year HID on blackout frequency (F(1,508) = 10.49, p = 0.001; see Figure 1). Among college students who consumed alcohol at the non-binge and binge levels, SAM user status was not associated with an increase in the number of past year blackouts (non-binge: F(5,37) = 0.50, p = 0.49; binge: F(5,138) = 0.23, p = 0.63). For participants who had engaged in any form of HID in the past year, however, SAM user status was associated with a greater number of blackouts (F(5,328) = 4.52, p = 0.03).
Figure 1.
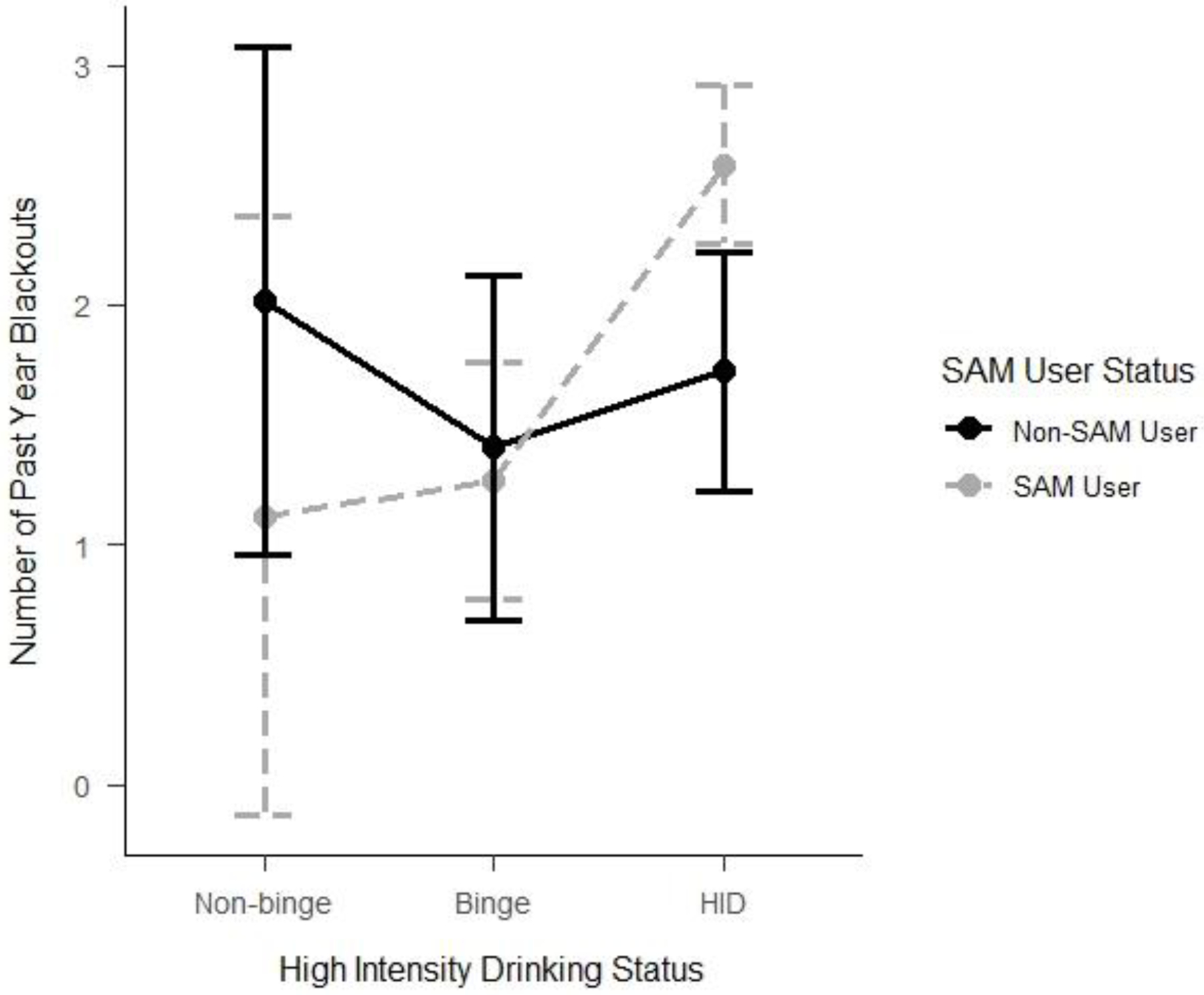
Interaction between high-intensity drinking status and simultaneous alcohol and marijuana user status on past year experiences of blackout among participants who used alcohol and marijuana in the past year (n = 540).
Note: SAM = Simultaneous alcohol and marijuana; HID = high-intensity drinking. Analysis controls for gender, typical frequency of marijuana use, and quantity-frequency of alcohol use.
Following up on this finding, we explored whether SAM user status conferred differential risk for experiencing a blackout across levels of HID (i.e., HID-2 and HID-3). Among high-intensity drinkers (n = 340), the level of HID was related to blackout frequency, such that HID-3 drinkers experienced more blackouts than HID-2 drinkers (F(6,327) = 6.64, p = 0.01). On average, those who drank to HID-2 levels reported experiencing between one and two past-year blackouts (M = 1.5, SD = 2.22), while those who drank to HID-3 levels experienced more than double that number of blackouts in the past year (M = 3.26, SD = 3.33).
Finally, we compared rates of post-SAM blackouts between HID-SAM users (individuals who endorsed SAM use and had also drank to the high intensity level in the past year; n = 276) and non-HID SAM users (individuals who reported past year SAM use but had engaged in only binge or non-binge drinking; n = 138). Whereas a third of HID-SAM users (32.70%) reported experiencing a past-year blackout following SAM use, only about one in ten non-HID SAM users (11.57%) reported a post-SAM use blackout (t(1) = 19.21, p < 0.0001).
Discussion
As expected, high-intensity drinkers had elevated odds of experiencing alcohol-induced blackouts. HID was relatively common in this sample (43.7%), and previous research has suggested HID may be especially prevalent among college students23, which may make this population uniquely vulnerable to harmful effects of drinking, including memory impairments. For example, in the current study, 59.04% of those who engaged in HID in the past year reported experiencing a past year blackout, compared to 25.26% of individuals with a past year history of binge drinking (but no HID), and just 3.45% of those without a past year history of binge or HID.
Of particular interest was the finding that SAM users experienced more frequent blackouts than non-SAM users, but only if they had engaged in HID in the past year. Additionally, compared to non-HID SAM users, SAM users who had drank to high-intensity levels in the past year were more likely to experience a blackout on a SAM use occasion (32.70% vs. 11.57%, respectively). These findings could help explain discrepant results from the blackout literature on the effects of marijuana use11,24,25. SAM use may be a risk factor for more frequent blackouts, but only among those engaging in particularly heavy drinking. Among individuals without a history of HID, there was virtually no added risk for blackout associated with SAM use. Therefore, for individuals engaging in light drinking or even binge drinking, simultaneous use of marijuana may pose no additional risk for the experience of blackouts, consistent with recent event-level research21. Given that Mallett and colleagues (2019) defined heavy drinking occasions based on binge criteria (4+/5+ drinks), both binge drinking and HID were lumped together, which may have obscured their ability to detect effects of SAM use during HID occasions. Future research should continue to explore interactions between marijuana and alcohol use patterns, with particular attention to HID.
Findings suggest that targeting HID may help reduce college students’ experiences of harmful consequences following alcohol use. In addition to acute consequences like blackouts, this hazardous form of drinking could also have long-lasting impacts on brain development and maturation among underage drinkers, such as the majority of college students. Heavy drinking during adolescence has been linked to alterations in normal brain development 26,27. In addition to increasing college student awareness of the harms associated with HID, college students should be educated on the risks associated with blackouts, which include sexual victimization6, neurological disruptions10, and risk of injury or overdose8. Though associated with various negative outcomes, many college students (46.6%) do not view blackout experiences negatively28, suggesting they may not be aware of these deleterious effects; therefore, education and feedback may be critical for increasing student perceptions of blackout-related risk.
Blackout prevention and intervention efforts would benefit from informing students of risk factors that increase their likelihood of experiencing a blackout, with particular attention to the potential role of HID and SAM use. Toward this aim, for college students using marijuana and alcohol, interventions may focus on more responsible use of the two substances by moderating alcohol consumption. While education on the harms of heavy drinking may be useful for some college students, these approaches alone are unlikely to be sufficient29–31. Instead, such efforts may be more effective if combined with harm reduction approaches, which focus on motivating college students to reduce risky substance use behaviors32. One widely-used harm reduction approach for alcohol use on college campuses is the Brief Alcohol Screening and Intervention for College Students (BASICS)33,34, which has been shown to produce long-term reductions in both alcohol consumption and negative consequences among heavy drinking college students35,36. BASICS’s efficacy may be due in part to its multi-pronged approach, (1) using motivational interviewing, with the goal of exploring and resolving ambivalence about change37, (2) providing education and personalized feedback on alcohol use and consequences (e.g., blood alcohol levels, normative comparisons), and (3) helping students develop protective behavioral strategies to minimize their experience of deleterious consequences38,39.
A similarly styled intervention providing personalized feedback on marijuana use and encouraging the use of protective behavioral strategies among college students effectively reduced frequency of marijuana use and increased their use of protective behavioral strategies40. Combining these two efforts (i.e., explicitly targeting both alcohol and marijuana use in interventions) may be needed for co-occurring alcohol and marijuana users, as alcohol interventions alone have not been shown to be effective at reducing marijuana use41,42, and use of marijuana may predict poorer alcohol intervention outcomes43,44. Based on our findings and the findings of others45,46, even a minor reduction in alcohol use (for example, from the HID level to binge level) could produce considerable health benefits. Additionally, interventions that successfully reduce blackout rates on college campuses may lead to institutional savings and fewer alcohol-related injuries9.
Limitations
The current study’s findings should be interpreted in light of several limitations. First, although gender, typical drinking patterns, and frequency of marijuana use were controlled for in analyses, there are a number of other ways in which SAM and non-SAM users (or HID and non-HID drinkers) may differ. For example, one study found that individuals who were higher in sensation seeking were more likely to be simultaneous polysubstance users than concurrent users47. These and other personality differences may partially account for the increased rates of blackouts seen in SAM and HID users. However, it could be difficult to disentangle these personality traits from the resulting substance use behaviors, since they are likely related in a complex fashion. Instead, it may be more feasible to make within-person comparisons using event-level data to understand the direct effects of HID and SAM use occasions on blackout experiences.
Second, the retrospective nature of the study makes it difficult to determine whether blackouts occurred at higher rates among HID-SAM users because of the increased volume of alcohol consumed or because of differences between HID-SAM users and non-HID SAM users that may predispose the former to more risky drinking (e.g., sensation seeking, risk taking, etc.). HID-SAM users were more likely to report experiencing a blackout following SAM use compared to non-HID SAM users (32.70% vs. 11.57%), but it was unclear if those SAM use events that led to a blackout occurred in the context of high-intensity drinking. In the future, event-level data could be used to examine whether SAM users are more likely to experience a blackout after an HID-SAM use occasion compared to an HID/no marijuana use occasion.
Third, the assessment of blackout is inherently complicated by its reliance on self-report, and it is possible that there were drinking occasions in which individuals experienced a blackout but were not aware they had done so. If missing memories are not salient ones (i.e., if an individual is missing memories of a conversation they had with a friend, this may be less salient than missing memories of how one got home), they may be disregarded entirely and never interpreted as a blackout. Fourth, this study used dichotomous (yes/no) indicators of SAM use. It will be important for future studies to take into account the frequency of SAM use. Finally, these findings are based on a sample of predominantly underage college students. Though this population is one of the most at-risk groups for HID48, findings may not generalize to other groups.
Future Directions
An important direction for future research will be to examine these associations using event-level data to further clarify the nature of blackout risk among individuals using alcohol and marijuana simultaneously. Also, given that HID has been studied primarily among college students, research is needed on non-college-attending young adults. Regarding marijuana use, both college students and their same-age non-college attending peers have similar rates of use, though non-college attending young adults are more likely to engage in daily marijuana use49. Given their greater frequency of use, research on the role of SAM use in blackouts should consider including non-college attending young adults. Future research may also benefit from assessing use of specific forms of marijuana. Marijuana products differ in their cannabinoid profiles (i.e., higher or lower levels of delta-9-tetrahydrocannabinol (THC), the main psychoactive component in marijuana), and this may affect the experience of memory-impairing effects like blackouts.
Conclusions
This study found that SAM use may most substantially increase risk for blackouts among college students who also engage in HID. In particular, there appeared to be step-wise effects, such that the impact of SAM use on blackouts was increasingly greater at each successive level of drinking (i.e., from non-binge to binge to HID). Harm reduction strategies that focus on moderating alcohol consumption among individuals engaging in SAM use may produce reductions in rates of blackout and related consequences.
Role of Funding Sources:
Investigator effort was supported by the National Institute on Alcohol Abuse and Alcoholism (K23AA026895, PI Miller; R21AA025175, PI Miller; T32AA013526, PI Sher). The NIH had no role in study design; data collection, analysis, or interpretation; manuscript preparation; or the decision to submit the paper for publication.
Footnotes
Declaration of Interest: The authors have no conflicts of interest to declare.
References
- 1.White AM. What happened? Alcohol, memory blackouts, and the brain. Alcohol Research & Health. 2003;27(2):186–196. [PMC free article] [PubMed] [Google Scholar]
- 2.Goodwin DW, Crane JB, Guze SB. Phenomenological aspects of the alcoholic “blackout”. The British Journal of Psychiatry. 1969;115(526):1033–1038. [DOI] [PubMed] [Google Scholar]
- 3.White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: Results of an e-mail survey. Journal of American College Health. 2002;51(3):117–131. [DOI] [PubMed] [Google Scholar]
- 4.Barnett NP, Tevyaw TOL, Fromme K, et al. Brief alcohol interventions with mandated or adjudicated college students. Alcoholism: Clinical and Experimental Research. 2004;28(6):966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis CN, Slutske WS, Martin NG, Agrawal A, Lynskey MT. Genetic epidemiology of liability for alcohol-induced blacking and passing out. Alcoholism: Clinical and Experimental Research. 2019;43(6):1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valenstein-Mah H, Larimer M, Zoellner L, Kaysen D. Blackout drinking predicts sexual revictimization in a college sample of binge-drinking women. Journal of Traumatic Stress. 2015;28(5):484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilhite ER, Mallard T, Fromme K. A longitudinal event-level investigation of alcohol intoxication, alcohol-related blackouts, childhood sexual abuse, and sexual victimization among college students. Psychology of Addictive Behaviors. 2018;32(3):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hingson RW, Zha W, Simons-Morton B, White A. Alcohol-induced blackouts as predictors of other drinking related harms among emerging young adults. Alcoholism: Clinical and Experimental Research. 2016;40(4):776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mundt MP, Zakletskaia LI. Prevention for college students who suffer alcohol-induced blackouts could deter high-cost emergency department visits. Health Affairs. 2012;31(4):863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boness CL, Korucuoglu O, Ellingson JM, et al. Twenty-first birthday drinking: Extreme-drinking episodes and white matter microstructural changes in the fornix and corpus callosum. Experimental and Clinical Psychopharmacology. 2019. [DOI] [PMC free article] [PubMed] [Retracted]
- 11.Merrill JE, Boyle HK, Jackson KM, Carey KB. Event-level correlates of drinking events characterized by alcohol-induced blackouts. Alcoholism: Clinical and Experimental Research. 2019;43(12):2599–2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perry PJ, Argo TR, Barnett MJ, et al. The association of alcohol-induced blackouts and grayouts to blood alcohol concentrations. Journal of Forensic Sciences. 2006;51(4):896–899. [DOI] [PubMed] [Google Scholar]
- 13.Dash GF, Davis CN, Martin NG, Statham DJ, Lynskey MT, Slutske WS. High-intensity drinking in adult Australian twins. Alcoholism: Clinical and Experimental Research. 2020;44(2):522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hingson RW, Zha W, White AM. Drinking beyond the binge threshold: predictors, consequences, and changes in the US. American Journal of Preventive Medicine. 2017;52(6):717–727. [DOI] [PubMed] [Google Scholar]
- 15.Jung J, Rosoff DB, Muench C, et al. Adverse childhood experiences are associated with high-intensity binge drinking behavior in adulthood and mediated by psychiatric disorders. Alcohol and Alcoholism. 2020. [DOI] [PMC free article] [PubMed]
- 16.Patrick ME, Schulenberg JE, Martz ME, Maggs JL, O’Malley PM, Johnston LD. Extreme binge drinking among 12th-grade students in the United States: Prevalence and predictors. JAMA Pediatrics. 2013;167(11):1019–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patrick ME, Terry-McElrath YM. High-intensity drinking by underage young adults in the United States. Addiction. 2017;112(1):82–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson KM, Sokolovsky AW, Gunn RL, White HR. Consequences of alcohol and marijuana use among college students: Prevalence rates and attributions to substance-specific versus simultaneous use. Psychology of Addictive Behaviors. 2020. [DOI] [PMC free article] [PubMed]
- 19.Cummings C, Beard C, Habarth JM, Weaver C, Haas A. Is the sum greater than its parts? Variations in substance-related consequences by conjoint alcohol-marijuana use patterns. Journal of Psychoactive Drugs. 2019;51(4):351–359. [DOI] [PubMed] [Google Scholar]
- 20.Linden-Carmichael AN, Van Doren N, Masters LD, Lanza ST. Simultaneous alcohol and marijuana use in daily life: Implications for level of use, subjective intoxication, and positive and negative consequences. Psychology of Addictive Behaviors. 2020;34(3):447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mallett KA, Turrisi R, Trager BM, Sell N, Linden-Carmichael AN. An examination of consequences among college student drinkers on occasions involving alcohol-only, marijuana-only, or combined alcohol and marijuana use. Psychology of Addictive Behaviors. 2019. [DOI] [PMC free article] [PubMed]
- 22.United States Census Bureau. 2013-2017 American Community Survey 5-Year Estimates. In: American Community Survey.; 2018. [Google Scholar]
- 23.Linden-Carmichael AN, Lanza ST. Drinking patterns of college-and non-college-attending young adults: is high-intensity drinking only a college phenomenon? Substance Use & Misuse. 2018;53(13):2157–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schuckit MA, Smith TL, Shafir A, et al. Predictors of patterns of alcohol-related blackouts over time in youth from the collaborative study of the genetics of alcoholism: the roles of genetics and cannabis. Journal of Studies on Alcohol and Drugs. 2017;78(1):39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shillington AM, Clapp JD. Substance use problems reported by college students: Combined marijuana and alcohol use versus alcohol-only use. Substance Use & Misuse. 2001;36(5):663–672. [DOI] [PubMed] [Google Scholar]
- 26.Pfefferbaum A, Kwon D, Brumback T, et al. Altered brain developmental trajectories in adolescents after initiating drinking. American Journal of Psychiatry. 2018;175(4):370–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Squeglia LM, Tapert SF, Sullivan EV, et al. Brain development in heavy-drinking adolescents. American Journal of Psychiatry. 2015;172(6):531–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mallett KA, Bachrach RL, Turrisi R. Are all negative consequences truly negative? Assessing variations among college students’ perceptions of alcohol related consequences. Addictive Behaviors. 2008;33(10):1375–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dejong W, Larimer ME, Wood MD, Hartman R. NIAAA’s rapid response to college drinking problems initiative: reinforcing the use of evidence-based approaches in college alcohol prevention. Journal of Studies on Alcohol and Drugs, Supplement. 2009(16):5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Larimer ME, Cronce JM. Identification, prevention and treatment: a review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol, Supplement. 2002(14):148–163. [DOI] [PubMed] [Google Scholar]
- 31.Stockings E, Hall WD, Lynskey M, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. The Lancet Psychiatry. 2016;3(3):280–296. [DOI] [PubMed] [Google Scholar]
- 32.Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32(11):2469–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dimeff LA. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. Guilford Press; 1999. [Google Scholar]
- 34.Dimeff L, Baer J, Kivlahan D, Marlatt G. Brief alcohol screening and intervention for college students (BASICS). Substance Abuse. 1999;21(4):283–285. [Google Scholar]
- 35.Fachini A, Aliane PP, Martinez EZ, Furtado EF. Efficacy of brief alcohol screening intervention for college students (BASICS): A meta-analysis of randomized controlled trials. Substance Abuse Treatment, Prevention, and Policy. 2012;7(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DiFulvio GT, Linowski SA, Mazziotti JS, Puleo E. Effectiveness of the Brief Alcohol and Screening Intervention for College Students (BASICS) program with a mandated population. Journal of American College Health. 2012;60(4):269–280. [DOI] [PubMed] [Google Scholar]
- 37.Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford press; 2012. [Google Scholar]
- 38.Martens MP, Taylor KK, Damann KM, Page JC, Mowry ES, Cimini MD. Protective behavioral strategies when drinking alcohol and their relationship to negative alcohol-related consequences in college students. Psychology of Addictive Behaviors. 2004;18(4):390. [DOI] [PubMed] [Google Scholar]
- 39.Benton SL, Schmidt JL, Newton FB, Shin K, Benton SA, Newton DW. College student protective strategies and drinking consequences. Journal of Studies on Alcohol. 2004;65(1):115–121. [DOI] [PubMed] [Google Scholar]
- 40.Riggs NR, Conner BT, Parnes JE, Prince MA, Shillington AM, George MW. Marijuana eCHECKUPTO GO: Effects of a personalized feedback plus protective behavioral strategies intervention for heavy marijuana-using college students. Drug and Alcohol Dependence. 2018;190:13–19. [DOI] [PubMed] [Google Scholar]
- 41.Yurasek AM, Merrill JE, Metrik J, Miller MB, Fernandez AC, Borsari B. Marijuana use in the context of alcohol interventions for mandated college students. Journal of Substance Abuse Treatment. 2017;79:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.White HR, Jiao Y, Ray AE, et al. Are there secondary effects on marijuana use from brief alcohol interventions for college students? Journal of Studies on Alcohol and Drugs. 2015;76(3):367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Subbaraman MS, Metrik J, Patterson D, Swift R. Cannabis use during treatment for alcohol use disorders predicts alcohol treatment outcomes. Addiction. 2017;112(4):685–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mojarrad M, Samet JH, Cheng DM, Winter MR, Saitz R. Marijuana use and achievement of abstinence from alcohol and other drugs among people with substance dependence: A prospective cohort study. Drug and Alcohol Dependence. 2014;142:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. Journal of Studies on Alcohol and Drugs. 2016;77(2):185–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Griswold MG, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2018;392(10152):1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martin CS, Clifford PR, Clapper RL. Patterns and predictors of simultaneous and concurrent use of alcohol, tobacco, marijuana, and hallucinogens in first-year college students. Journal of Substance Abuse. 1992;4(3):319–326. [DOI] [PubMed] [Google Scholar]
- 48.Patrick ME, Terry-McElrath YM, Kloska DD, Schulenberg JE. High-intensity drinking among young adults in the United States: Prevalence, frequency, and developmental change. Alcoholism: Clinical and Experimental Research. 2016;40(9):1905–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schulenberg J, Johnston L, O’Malley P, Bachman J, Miech R, Patrick M. Monitoring the Future national survey results on drug use, 1975–2018: Volume II, college students and adults ages 19–60. In:2019.


