Abstract
Objective
The COVID-19 pandemic has brought unprecedented changes to young adults’ lives, resulting in mental health difficulties for many; however, some individuals are particularly prone to heightened anxiety. Little is known about the early life predictors of anxiety during the pandemic. We examined a developmental pathway from behavioral inhibition (BI), a temperament characterized by fearful responses toward novelty, to changes in young adults’ anxiety during the initial period of the pandemic. We hypothesized that a stable pattern of BI across early childhood would predict greater adolescent worry dysregulation, which in turn would predict increases in young adult anxiety during a stressful phase of the pandemic.
Method
Participants (N = 291; 54% female) were followed from toddlerhood to young adulthood. BI was observed at ages 2 and 3 years. Social wariness was observed at age 7 years. Participants rated their worry dysregulation in adolescence (age 15) and anxiety in young adulthood (age 18) at 2 assessments during the COVID-19 pandemic, 1 month apart.
Results
A significant moderated mediation, in which a stable pattern of BI from toddlerhood to childhood, as compared to the absence of this pattern, predicted greater worry dysregulation in adolescence. Worry dysregulation predicted elevated young adult anxiety in the second assessment during COVID-19, even after accounting for the first assessment.
Conclusion
This study identifies a developmental pathway from toddlerhood BI to young adults’ elevated anxiety during the COVID-19 pandemic. Findings have implications for early identification of individuals at risk for dysregulated worry and the prevention of anxiety during stressful life events in young adulthood.
Key words: behavioral inhibition, temperament, worry, anxiety, COVID-19 pandemic
The current study leveraged a prospective longitudinal sample to characterize developmental pathways from early temperamental risk to elevated young adult anxiety during the COVID-19 pandemic. The rapid spread of COVID-19 has led governments to implement measures such as home quarantine, school closures, and social distancing. These measures have caused significant changes in everyday social life and educational routines.1,2 Although these changes have been associated with heightened anxiety1 for the population in general, some individuals are more prone to experiencing heightened anxiety during stressful life events than are others.3 As such, examining specific developmental pathways from childhood temperament to heightened anxiety during the COVID-19 pandemic is critical for advancing our understanding of the mechanistic pathways that contribute to elevated anxiety during stressful life events.
The current study leveraged a prospective longitudinal sample to characterize developmental pathways from early temperamental risk to elevated young adult anxiety during the COVID-19 pandemic. The rapid spread of COVID-19 has led governments to implement measures such as home quarantine, school closures, and social distancing. These measures have caused significant changes in everyday social life and educational routines.1 , 2 Although these changes have been associated with heightened anxiety1 for the population in general, some individuals are more prone to experiencing heightened anxiety during stressful life events than are others.3 As such, examining specific developmental pathways from childhood temperament to heightened anxiety during the COVID-19 pandemic is critical for advancing our understanding of the mechanistic pathways that contribute to elevated anxiety during stressful life events.
One of the best childhood predictors of later anxiety is behavioral inhibition (BI), an early childhood temperament characterized by high levels of cautious, fearful, and avoidant responses to unfamiliar people, objects, and situations.4 BI is predictive of a 3- to 4-fold increased risk of developing anxiety disorders, and approximately 40% of children high in BI will develop clinical levels of anxiety.5 , 6 Although BI is most often assessed in infancy and toddlerhood, when it is assessed in social situations (eg, with unfamiliar peers) later in childhood, it is often referred to as “social wariness.”7 Although BI is relatively stable across childhood, not all children high in early BI continue to display shy and socially wary behaviors.8 It is those who demonstrate a stable pattern of BI and social wariness from 2 to 7 years of age who demonstrate higher rates of anxiety disorders in adolescence.9 Although a stable pattern of BI in childhood has been associated with later anxiety, specific mechanisms by which a stable pattern of BI in childhood is linked to changes in anxiety during stressful life events in young adulthood remain underinvestigated.
One mechanism by which a stable pattern of BI across childhood may lead to heightened anxiety in young adulthood is difficulty regulating worry and negative emotions during adolescence. Worry regulation problems in adolescence have been associated with greater anxiety.10 There is also evidence suggesting that emotion dysregulation mediates the relation between early BI and later socioemotional problems.11 , 12 Children who demonstrate a stable pattern of BI may be at a greater risk for later difficulties managing worry and displaying inappropriate expressions of worry (ie, worry dysregulation). This would lead them not only to respond to novel or stressful events in more fearful ways but also to inadequately manage their worry about possible threats, placing them at greater risk for anxiety during stressful events. Limited evidence suggests that children high in BI may express high levels of negative worry,13 , 14 suggestive of worry dysregulation. However, to our knowledge, no research has examined whether BI during childhood predicts worry dysregulation in adolescence.
Worry dysregulation also has been identified as 1 of the central mechanisms contributing to anxiety.15 , 16 Individuals who experience difficulties regulating their worries exaggerate both the likelihood and magnitude of potential negative consequences of events,17 , 18 which in turn increases experiences of negative affect and anxiety.19 Children and adults diagnosed with anxiety disorders display higher levels of dysregulated expressions of worry.20 In adolescents, the intensity of daily worry predicted increases in daily anxiety,15 suggesting that worry dysregulation may predict increases in anxiety. In light of these previous findings, given that the COVID-19 pandemic is a multifaceted stressful life event that has brought unprecedented changes and uncertainty to individuals’ lives, adolescents with maladaptive expressions of worry, or dysregulated worry, might be particularly prone to increases in anxiety during the COVID-19 pandemic, as they may experience difficulties in managing their worries and may catastrophize the uncertainty and threats during the COVID-19 pandemic.
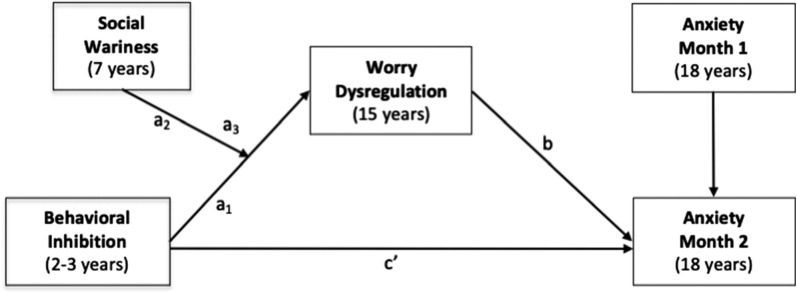
This study examined whether a stable pattern of BI in early childhood predicted greater worry dysregulation in adolescence, and whether greater adolescent worry dysregulation, in turn, predicted increases in young adults’ anxiety during the initial phase of the COVID-19 pandemic. Using a moderated mediation model (Figure 1 ), we examined 3 questions. First, do observed measures of toddlerhood BI and childhood social wariness interact to predict worry dysregulation in adolescence? Toddlerhood BI was observed in novel social and nonsocial situations, whereas childhood BI was assessed in a novel social situation involving an unfamiliar peer (referred to as “social wariness”). Based on the idea that a stable pattern of BI would predict greater worry dysregulation, we hypothesized that higher toddlerhood BI would predict greater adolescent worry dysregulation, particularly among children who displayed greater social wariness in childhood. Second, does worry dysregulation in adolescence predict increases in anxiety in young adulthood during the acute phase of the COVID-19 pandemic? We hypothesized that greater adolescent worry dysregulation would predict relative increases in young adults’ anxiety over 2 consecutive months of the COVID-19 pandemic. Finally, does worry dysregulation in adolescence mediate the relation between stable BI and increases in young adults’ anxiety during the pandemic among individuals demonstrating high levels of childhood social wariness? We hypothesized that stable high BI in childhood would predict greater worry dysregulation in adolescence, which in turn would predict increases in young adults’ anxiety during the initial phase of the pandemic.
Figure 1.
Conceptual Diagram Illustrating the Moderated Mediation Model Tested in the Current Study
Note:Anxiety month 1 and anxiety month 2 represent the first and second anxiety assessments during the COVID-19 pandemic, respectively.
Method
Participants
Participants were involved in an ongoing prospective longitudinal, multi-method study of temperament and socioemotional development conducted in a large metropolitan mid-Atlantic region of the United States. A total of 291 families with a 4-month-old infant (156 female infants) were selected based on displays of positive and negative affect and motor reactivity to novel stimuli.21 Based on maternal report in infancy, mothers were 69.4% White, 16.5% African American, 7.2% Hispanic, 3.1% Asian, 3.4% other, and 0.3% missing. Mothers in the sample were highly educated with 35.7% as graduate school graduates, 41.9% as college graduates, 16.2% as high school graduates, 5.5% with other forms of education, and 0.7% were missing.
Table 1 includes detailed information regarding the sample characteristics in terms of race/ethnicity, sex, and maternal education for each wave of assessment. Of the original sample (N = 291), 248 had data on observed BI at the 2- and 3-year visits; 175 had data on observed social wariness behaviors at the 7-year visit, 163 had data on worry at the 15-year visit, 158 had data on anxiety at the first assessment during the pandemic, and 155 had data on the second assessment during the pandemic. Among the 168 participants who provided data during the pandemic, 147 were residing in mid-Atlantic states (84% in Maryland), 10 were residing in southeastern states, and 10 were residing in other US states, and one participant resided in England, United Kingdom.
Table 1.
Demographic Information Across Assessments
| Demographic information | Behavioral inhibition (age 2-3 y) n = 248 | Social wariness (age 7 y) n = 175 | Worry dysregulation (age 15 y) n = 163 | Anxiety month 1 (age 18 y) n = 155 | Anxiety month 2 (age 18 y) n = 153 |
|---|---|---|---|---|---|
| Child sex (%) | |||||
| Male | 47.6 | 44.6 | 42.3 | 41.9 | 41.2 |
| Female | 52.4 | 55.4 | 57.7 | 58.1 | 58.8 |
| Race/ethnicity (%) | |||||
| African American | 14.9 | 15.4 | 15.3 | 11.6 | 11.1 |
| Asian | 2.8 | 2.9 | 3.1 | 3.9 | 2.6 |
| Hispanic | 6.5 | 5.7 | 4.9 | 7.1 | 7.2 |
| White | 71.8 | 73.1 | 73.6 | 73.5 | 75.2 |
| Other | 3.6 | 2.9 | 3.1 | 3.2 | 3.3 |
| Not answered | .4 | .0 | .0 | .6 | .7 |
| Maternal education (%) | |||||
| High school graduate | 16.5 | 14.9 | 16.0 | 13.5 | 15.0 |
| College graduate | 41.5 | 42.3 | 44.2 | 40.0 | 41.2 |
| Graduate school graduate | 37.7 | 37.7 | 36.2 | 40.6 | 37.9 |
| Other | 5.2 | 5.1 | 3.7 | 5.8 | 5.9 |
Examining the patterns of missing data revealed that mother’s race was associated with missing data on the second assessment during the pandemic [χ2 (1) = 5.58, p = .018], such that children with data on these measures were more likely to have White mothers. Because of this, maternal race was included as a covariate in the SEM analyses. Missing data on all other variables was not associated with children’s sex, mother’s race, maternal education, BI, social wariness, or worry dysregulation (p values >.05).
Procedure
BI was measured at ages 2 and 3 years using observational measures of children’s behavior during the presentation of novel stimuli.4 At the 7-year assessment, children’s social wariness was observed in the laboratory during a novel social situation involving an unfamiliar, same-age, same-sex peer recruited from the community.7 At the 15-year assessment, participants reported on their expression and regulation of worries. Finally, between April 20 and May 15, 2020, approximately 1 month (mean = 29.67 days, SD = 6.01 days) after a stay-at-home order was implemented in Maryland on March 30, 2020, young adults completed the first assessment (month 1) of online questionnaires measuring anxiety. Approximately 1 month later (m = 26.48 days, sd = 7.31 days), participants completed a second assessment (month 2) after the mandatory stay-at-home order was lifted and gradual reopening started in the state of Maryland. Participants were on average 18 years of age during these 2 months of the pandemic (mean = 18.26, SD = 0.66 years). The time between assessments, the date of assessment since the stay-at-home order, and the participants’ age were included as covariates in the SEM analyses. The Institutional Review Board of the University of Maryland approved all study protocols, and all participants were compensated for their time.
Behavioral Inhibition
BI was assessed at ages 2 and 3 years using behavioral observations of children’s response to novel toys and interaction with unfamiliar adults.22 BI was coded based on children’s proximity to their caregiver and latency to approach or to vocalize during these novel situations. Consistent with other work investigating pathways linking BI and later social anxiety symptoms, standardized BI scores were computed for the 2- and 3-year assessments and then combined into a composite BI measure averaging scores across the 2 assessments.23 Higher scores indicated higher levels of BI. In addition, we also examined results with a BI composite including behavioral observations and parent reports that has been used in previous studies from this sample.24 Results from these sensitivity analyses showed similar results (see Table S1, available online). Although early BI alone did not predict adolescent worry dysregulation, a stable pattern of childhood BI characterized as high early BI and high childhood social wariness predicted greater dysregulated worry in adolescence. Moreover, the conditional indirect effects also showed the same results as the main analyses, leading to the same conclusions, suggesting that measurement of the BI construct (observation versus observation and parent report) does not significantly affect the results or their interpretation (see Supplement 1, available online).
Social Wariness
Child social wariness was observed during an unstructured free play task with an unfamiliar peer when children were 7 years of age.7 Trained coders rated children’s wariness reflecting a hesitance to play and fearful behavior toward the peer, and unfocused/disengaged behaviors on a scale of 1 to 7 with good interrater reliability.25 These scores were averaged, and higher values indicated greater social wariness in an unfamiliar peer context.
Worry Dysregulation
Worry dysregulation was assessed at 15 years via children’s self-report on the Dysregulation subscale of the Children’s Worry Management Scale.26 This subscale captures maladaptive worry expression and consists of 3 items (eg, “I can't stop myself from acting really worried”). In addition, children were asked to rate how indicative each statement was on a scale of 1 to 3, such that higher scores indicated greater worry dysregulation. This subscale has been shown to have good concurrent validity and internal reliability.27 Because this scale showed suboptimal reliability in our sample (α = .55), we performed a principal component analysis, which suggested that a fourth item be included in this composite (“I show my worried feelings”), improving its reliability to acceptable levels (α = .61). Here in the main article, we report the results with the validated 3-item scale. However, in Table S2, available online, we show results with the 4-item scale with higher reliability, finding the same results and confirming that the way of calculating the worry dysregulation scale does not affect the results and their interpretations (see Supplement 1, available online).
Generalized Anxiety Disorder 7-Item Scale
Generalized anxiety was measured using the Generalized Anxiety Disorder 7-Item Scale28 at 2 assessments (month 1 and month 2) during the COVID-19 pandemic when participants were 18 years of age. The items consisted of various anxiety symptoms and were summed to create an overall score. Higher scores indicated greater anxiety, with scores ≥10 considered to be in the clinical range. This scale has been shown to have high test−retest reliability and good convergent validity.28 The scale showed excellent internal consistency at both time points (α values >.92) and good test−retest reliability (r = 0.81). Based on the clinical diagnostic interviews conducted at the 15-year assessment, 20 of 151 participants met criteria for generalized anxiety disorder. Participants’ diagnostic status for generalized anxiety disorder (1 = yes, 0 = no) was positively associated with worry dysregulation at age 15 years (r = 0.30, p = .001) and anxiety assessed at the 2 assessments during the COVID-19 pandemic (r = 0.17, p = .077 at month 1; r = 0.30, p = .001 at month 2).
Data Analysis
To test the study’s aims, a moderated mediation path model was conducted using structural equation modeling with lavaan 29 in R, version 3.6. Figure 1 depicts the conceptual model. To test the moderating effect of childhood social wariness on the relation between early BI and adolescent worry dysregulation, paths from BI, social wariness, and their interaction to worry dysregulation were tested. Direct paths from BI and adolescent worry dysregulation to anxiety at month 2 during the pandemic were also added. Finally, to formally test the moderated mediation, we examined the indirect effects from the BI and social wariness interaction to anxiety at month 2 as mediated by worry dysregulation at high (+1 SD) and low (−1 SD) levels of social wariness. This procedure is akin to examining simple slopes when probing the effects of an interaction with a continuous independent variable and moderator in a regression model.30
Based on the preliminary analyses described below with covariates and missing patterns and in line with previous studies with this sample,31 we controlled for maternal education, maternal race, and sex on the main outcomes and any variable that showed a zero-order correlation with these covariates. In addition, we included anxiety at the first COVID-19 assessment, the time between assessments during the pandemic, the date of assessment since the stay-at-home order, and the age of the participants during the pandemic as covariates. Our model used full information maximum likelihood estimation to handle missing data to reduce potential bias in the parameter estimates.32 This permitted the inclusion of all participants with data on 1 or more variables. Moreover, because of the missing data and potential departures from multivariate normality, the model was estimated using a robust maximum likelihood estimator and a scaled test χ2 statistic.33 Finally, to test indirect effects, we used a bias-corrected bootstrapping procedure (5,000 draws), as it has been shown to increase accuracy in estimating effects, reducing type I error rates.34
Results
Descriptive Statistics
Descriptive statistics and the correlations among all study variables are presented in Table 2 . Both BI and social wariness were positively related to adolescent worry dysregulation. Adolescent worry dysregulation was positively related to anxiety during the first and second assessments during the COVID-19 pandemic. Compared to male participants, female participants displayed higher levels of social wariness at age 7 years, reported increased worry dysregulation at 15 years and anxiety at month 1 during the pandemic (18 years). As such, sex was included as a covariate in the path model examining our main hypotheses.
Table 2.
Means, Standard Deviations, and Correlations Among All Study Variables
| Variable (age of assessment) | n | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|---|
|
291 | |||||||||
|
290 | –0.05 | ||||||||
|
273 | 1.21 | 0.72 | 0.01 | 0.19∗ | |||||
|
248 | –0.01 | 0.47 | –0.02 | –0.01 | 0.01 | ||||
|
175 | 1.92 | 0.65 | –0.22∗ | –0.11 | –0.13 | 0.06 | |||
|
163 | 1.45 | 0.47 | –0.31∗ | 0.00 | 0.08 | 0.24∗ | 0.19∗ | ||
|
155 | 5.69 | 5.62 | –0.16∗ | 0.05 | 0.16 | –0.05 | 0.02 | 0.18∗ | |
|
153 | 5.07 | 5.06 | –0.10 | 0.14 | 0.08 | 0.05 | 0.08 | 0.26∗ | 0.81∗ |
Note: Anxiety month 1 and anxiety month 2 represent the first and second anxiety assessments during the COVID-19 pandemic, respectively.
1 = Male participants and 0 = female participants.
1 = White and 0 = other race/ethnicity.
p < .05.
Change in Anxiety During the COVID-19 Pandemic
At month 1, 20% of the participants reported moderate levels of anxiety symptoms considered to be in the clinical range (ie, scores ≥10). At month 2, 18.3% of participants reported clinical levels of anxiety. In line with this and contrary to our expectations, results from a paired-samples t test indicated a significant decrease in anxiety [t(145) = 2.79, p = .006] from month 1 to month 2. As such, to capture those individuals who continued to experience elevated levels of anxiety, our main outcome of interest was anxiety during the second assessment (month 2) relative to the first assessment (month 1).
Developmental Pathways From Early BI to Anxiety During the COVID-19 Pandemic
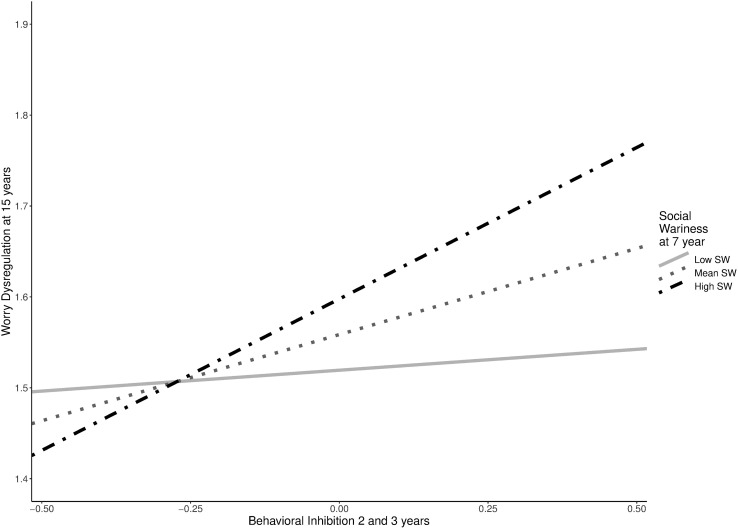
The moderated mediation model examining the hypothesized paths fit the data well (root mean square error of approximation = 0.06, comparative fit index = 0.96). All nonstandardized and standardized path coefficients are reported in Table 3 . Consistent with our first hypothesis, the relation between early BI and adolescent worry dysregulation was moderated by childhood social wariness (b = 0.22, p = .002). As shown in Figure 2 , higher toddlerhood BI predicted more worry dysregulation at age 15 years at high levels of social wariness at 7 years (+1 SD; b = 0.33, p < .001) but not at low levels of social wariness (−1 SD; b = 0.05, p = .625).
Table 3.
Path Analysis Results for the Final Moderated Mediation Model
| Predictors/outcome | β | b | p | CI lower | CI upper |
|---|---|---|---|---|---|
| Anxiety month 2 | |||||
| Anxiety month 1 | 0.81 | 0.72 | .000 | 0.618 | 0.820 |
| BI | 0.04 | 0.48 | .370 | –0.571 | 1.534 |
| Maternal education | –0.05 | –0.32 | .298 | –0.926 | 0.284 |
| Maternal race/ethnicity | 0.11 | 1.17 | .025 | 0.149 | 2.181 |
| Sex | 0.06 | 0.60 | .237 | –0.395 | 1.600 |
| Time between assessments | 0.08 | 0.06 | .135 | –0.017 | 0.127 |
| Age during COVID-19 | 0.01 | 0.06 | .863 | –0.657 | 0.785 |
| Date of assessment | –0.12 | –0.11 | .029 | –0.213 | –0.012 |
| Worry dysregulation | 0.12 | 1.26 | .037 | 0.078 | 2.448 |
| Worry dysregulation | |||||
| BI | 0.81 | 0.19 | .009 | 0.047 | 0.332 |
| Social wariness | 0.04 | 0.06 | .189 | –0.030 | 0.150 |
| BI × social wariness | –0.05 | 0.22 | .002 | 0.080 | 0.362 |
| Sex | 0.11 | –0.25 | .000 | –0.384 | –0.115 |
Note: Anxiety month 1 and anxiety month 2 represent the first and second anxiety assessments during the COVID-19 pandemic, respectively. Boldface type indicates significant paths. Sex is coded as 0 = female participants and 1 = male participants. Maternal race/ethnicity is coded as 1 = White participants and 0 = other race/ethnicity. BI = behavioral inhibition.
Figure 2.
Simple Slopes for the Interaction Between Behavioral Inhibition and Social Wariness Predicting Worry Dysregulation at Age 15 Years
Note:Low social wariness was defined as −1 standard deviation and high social wariness was defined as +1 standard deviation from the mean. SW = social wariness.
As shown in Table 2 and consistent with our second hypothesis, greater worry dysregulation at 15 years predicted greater anxiety at month 2 of the pandemic, accounting for the stability in anxiety from month 1 to month 2 and the direct effects from BI to anxiety at month 2.
Given the support for our first 2 hypotheses, we tested whether the indirect effect from BI to increased anxiety during the pandemic through adolescent worry dysregulation was significant among children with high childhood social wariness. The indirect effect from early BI to anxiety at month 2 via adolescent worry dysregulation was conditional on social wariness (b = 0.28, 95% CI = 0.003, 0.821). As hypothesized, individuals high in early BI, who continued to display high levels of social wariness during childhood reported more worry dysregulation in adolescence, which led to greater anxiety at month 2 of the pandemic (b = 0.42, 95% CI = 0.022, 1.082), when they were 18 years of age. This developmental pathway was not significant for children who displayed low levels of social wariness in childhood (b = 0.06, 95% CI −0.178, 0.422). Finally, in sensitivity analyses, we found that this developmental pathway from early BI to anxiety during the COVID-19 pandemic was specific to worry dysregulation rather than other forms of emotion dysregulation such as anger dysregulation or sadness dysregulation (see Tables S3 and S4, available online).
Discussion
The COVID-19 pandemic is a multifaceted, stressful life event that has posed concern and uncertainty about individuals’ health, future, and disruptions to their social life. Although stressful life events such as this increase mental health problems in adolescents and young adults,3 individuals with a stable pattern of childhood temperament of BI, particularly toddlerhood BI and the later manifestation of social wariness, may be at a greater risk for experiencing heightened anxiety. The current study examined a developmental pathway spanning 16 years from BI observed in toddlerhood to change in self-reported anxiety in young adulthood during 2 stressful months of the COVID-19 pandemic in the United States. As hypothesized, individuals high in toddlerhood BI who continued to display high levels of social wariness in childhood reported experiencing dysregulated worry in adolescence, which ultimately predicted increased anxiety in young adulthood during a critical stage of the pandemic (May−June 2020), relative to anxiety assessed 1 month before. These findings suggest that worry dysregulation in adolescence may be a mechanism by which a stable pattern of BI across childhood puts individuals at risk for experiencing elevated levels of anxiety during stressful life events such as the COVID-19 pandemic.
Our findings extend previous research showing that children high in BI express excessive levels of worry in childhood.13 , 14 Findings from the current study show that not all young children with high early BI report overt expressions of dysregulated worry in adolescence; however, those with high early BI who continue to experience high social wariness in childhood report experiencing greater dysregulated worry in adolescence. These findings suggest that stable BI throughout childhood may be a risk factor for the development of dysregulated worry.
Consistent with previous work showing that worry dysregulation is a core mechanism of generalized anxiety disorder19 that leads to increases in anxiety over time,15 our findings showed that dysregulated worry expression in adolescence predicted elevated levels of anxiety during the initial phase of the COVID-19 pandemic. Notably, we assessed anxiety twice during the pandemic: first, during the stay-at-home orders, and second, approximately 1 month later, shortly after the mandatory stay-at-home order was lifted and gradual reopening began. A large proportion of the sample reported anxiety symptoms in the clinical range (20% and 18.3% at month 1 and month 2, respectively), compared to only ∼11.59% of individuals from a large community sample of adolescents reporting clinical levels of anxiety based on the same criteria.35 Similarly, for this sample at age 15 years, only ∼13% of adolescents reported clinical levels of generalized anxiety based on a clinical interview. Although anxiety decreased from the first to the second month in the overall sample, those who reported dysregulated expressions of worry in adolescence continued to experience relatively elevated anxiety in the second month of assessment. Individuals with maladaptive worry patterns may be more likely to exaggerate threats and negative consequences associated with stressful events (eg, the COVID-19 pandemic), and thus experience elevated levels of anxiety during the pandemic.
Our study has several notable strengths, including a longitudinal sample spanning 16 years as well as the use of a multi-method approach including behavioral measures of temperament and self-report measures of worry and anxiety. In addition, having 2 assessments of anxiety during the COVID-19 pandemic is a notable strength of the study, because this design allowed us to examine changes in young adults’ anxiety during the early phase of the pandemic. However, it is important to note that having an earlier assessment right before the start of the COVID-19 outbreak could have allowed us to capture the purported increases in anxiety. It is also important to note that there were missing data due to the longitudinal design of the study. Importantly, we utilized statistical approaches to use all available data and mitigated bias due to missing data. Furthermore, in sensitivity analyses, we found a comparable pattern of results when examining only participants with complete data (see Table S5, Supplement 1, available online). To examine the role of early temperament in future anxiety, the sample was oversampled for temperamental reactivity in infancy. Thus, when interpreting the results of the current study, is also important to consider this sampling strategy, and caution is warranted when interpreting our results and, in particular, the prevalence of anxiety during the COVID-19 pandemic.
To conclude, this study provides evidence that a stable pattern of BI across childhood is associated with excessive worry dysregulation in adolescence, which in turn leads to relative increases in young adults’ anxiety from 1 month to the next during a stressful life event, the COVID-19 pandemic. Prevention of dysregulated worry and anxiety may be improved by targeting children who demonstrate a stable pattern of fearful temperament across early childhood, as they may show difficulties regulating their worries in adolescence, which may put them at risk for future anxiety. Consistent with findings from previous research, targeting social wariness in childhood and/or dysregulated worry in adolescence may be a viable strategy for the prevention of anxiety disorders.36 Findings from this study suggest that targeting dysregulated worry may particularly be important for preventing increases in anxiety during stressful life events such as the COVID-19 pandemic.
Footnotes
Drs. Zeytinoglu and Morales contributed equally to this research
This research was supported by grants MH093349 and HD017899 to NF from the National Institute of Health, the Coronavirus Research Seed Grant from the University of Maryland awarded to NF, and ZIA-MH-002782 project awarded to DP from the Intramural Research Program at the National Institute of Mental Health (NIMH).
Drs. Morales and Zeytinoglu served as the statistical experts for this research.
Author Contributions
Conceptualization: Zeytinoglu, Morales, Lorenzo, Chronis-Tuscano, Degnan, Almas, Henderson, Pine, Fox
Data curation: Zeytinoglu, Morales
Formal analysis: Zeytinoglu, Morales
Funding acquisition: Chronis-Tuscano, Degnan, Almas, Henderson, Pine, Fox
Investigation: Zeytinoglu, Morales, Lorenzo, Henderson, Fox
Methodology: Zeytinoglu, Morales, Degnan, Henderson, Fox
Project administration: Zeytinoglu, Morales, Fox
Supervision: Henderson, Pine, Fox
Visualization: Morales
Writing – original draft: Zeytinoglu, Morales
Writing – review and editing: Zeytinoglu, Morales, Lorenzo, Chronis-Tuscano, Degnan, Almas, Henderson, Pine, Fox
The authors thank the many research assistants involved in collecting and coding the data presented in this manuscript. They also thank the participating families without whom the study would not have been possible.
Disclosure: Dr. Morales has received funding from NIMH (grant U01MH093349-09S1). Dr. Lorenzo has received funding from NIMH (grant R01MH118320–02S1). Dr. Chronis-Tuscano has received royalties from Oxford University Press and research funding from NIMH. Dr. Henderson has received research funding from the Social Sciences and Humanities Research Council of Canada and NIMH. Dr. Fox has received grant support from NIMH, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Science Foundation, the National Institutes of Health Environmental influences on Child Health Outcomes consortium, the Russell Sage Foundation, and the Lumos Foundation. He has received royalties from Guilford Press and Harvard University Press. He has received honoraria for lectures to professional audiences. Drs. Zeytinoglu, Degnan, Almas, and Pine have reported no biomedical financial interests or potential conflicts of interest.
Supplemental Material
References
- 1.Cao W., Fang Z., Hou G., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020:287. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Heal. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLaughlin K.A., Hatzenbuehler M.L. Stressful life events, anxiety sensitivity, and internalizing symptoms in adolescents. J Abnorm Psychol. 2009;118:659–669. doi: 10.1037/a0016499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fox N.A., Henderson H.A., Marshall P.J., Nichols K.E., Ghera M.M. Behavioral inhibition: linking biology and behavior within a developmental framework. Annu Rev Psychol. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- 5.Clauss J.A., Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J Am Acad Child Adolesc Psychiatry. 2012;51:1066–1075. doi: 10.1016/j.jaac.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandstrom A., Uher R., Pavlova B. Prospective association between childhood behavioral inhibition and anxiety: a meta-analysis. J Abnorm Child Psychol. 2020;48:57–66. doi: 10.1007/s10802-019-00588-5. [DOI] [PubMed] [Google Scholar]
- 7.Degnan K.A., Henderson H.A., Fox N.A., Rubin K.H. Predicting social wariness in middle childhood: the moderating roles of child care history, maternal personality and maternal behavior. Soc Dev. 2008;17:471–487. doi: 10.1111/j.1467-9507.2007.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Degnan K.A., Fox N.A. Behavioral inhibition and anxiety disorders: multiple levels of a resilience process. Dev Psychopathol. 2007;19:729–746. doi: 10.1017/S0954579407000363. [DOI] [PubMed] [Google Scholar]
- 9.Chronis-Tuscano A., Degnan K.A., Pine D.S., et al. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. J Am Acad Child Adolesc Psychiatry. 2009;48:928–935. doi: 10.1097/CHI.0b013e3181ae09df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weems C.F., Silverman W.K., La Greca A.M. What do youth referred for anxiety problems worry about? Worry and its relation to anxiety and anxiety disorders in children and adolescents. J Abnorm Child Psychol. 2000;28:63–72. doi: 10.1023/a:1005122101885. [DOI] [PubMed] [Google Scholar]
- 11.Penela E.C., Walker O.L., Degnan K.A., Fox N.A., Henderson H.A. Early behavioral inhibition and emotion regulation: pathways toward social competence in middle childhood. Child Dev. 2015;86:1227–1240. doi: 10.1111/cdev.12384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hipson W.E., Coplan R.J., Séguin D.G. Active emotion regulation mediates links between shyness and social adjustment in preschool. Soc Dev. 2019;28:893–907. [Google Scholar]
- 13.Stevenson-Hinde J., Glover A. Shy girls and boys: a new look. J Child Psychol Psychiatry Allied Discip. 1996;37:181–187. doi: 10.1111/j.1469-7610.1996.tb01389.x. [DOI] [PubMed] [Google Scholar]
- 14.Muris P., Merckelbach H., Wessel I., Van De Ven M. Psychopathological correlates of self-reported behavioural inhibition in normal children. Behav Res Ther. 1999;37:575–584. doi: 10.1016/s0005-7967(98)00155-7. [DOI] [PubMed] [Google Scholar]
- 15.Dickson K.S., Ciesla J.A., Reilly L.C. Rumination, worry, cognitive avoidance, and behavioral avoidance: examination of temporal effects. Behav Ther. 2012;43:629–640. doi: 10.1016/j.beth.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 16.McLaughlin K.A., Mennin D.S., Farach F.J. The contributory role of worry in emotion generation and dysregulation in generalized anxiety disorder. Behav Res Ther. 2007;45:1735–1752. doi: 10.1016/j.brat.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 17.Vasey M.W., Crnic K.A., Carter W.G. Worry in childhood: a developmental perspective. Cognit Ther Res. 1994;18:529–549. [Google Scholar]
- 18.Vasey M.W., Borkovec T.D. A catastrophizing assessment of worrisome thoughts. Cognit Ther Res. 1992;16:505–520. [Google Scholar]
- 19.Newman M.G., Llera S.J., Erickson T.M., Przeworski A., Castonguay L.G. Worry and generalized anxiety disorder: a review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annu Rev Clin Psychol. 2013;9:275–297. doi: 10.1146/annurev-clinpsy-050212-185544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suveg C., Zeman J. Emotion regulation in children with anxiety disorders. J Clin Child Adolesc Psychol. 2004;33:750–759. doi: 10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- 21.Hane A.A., Fox N., Henderson H., Marshall P.J. Behavioral reactivity and approach-withdrawal bias in infancy. Dev Psychol. 2008;44:1491–1496. doi: 10.1037/a0012855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calkins S.D., Fox N.A., Marshall T.R. Behavioral and physiological antecedents of inhibited and uninhibited behavior. Child Dev. 1996;67:523–540. [PubMed] [Google Scholar]
- 23.Pérez-Edgar K., Reeb-Sutherland B.C., McDermott J.M., et al. Attention biases to threat link behavioral inhibition to social withdrawal over time in very young children. J Abnorm Child Psychol. 2011;39:885–895. doi: 10.1007/s10802-011-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Troller-Renfree S.V., Buzzell G.A., Bowers M.E., et al. Development of inhibitory control during childhood and its relations to early temperament and later social anxiety: unique insights provided by latent growth modeling and signal detection theory. J Child Psychol Psychiatry Allied Discip. 2019;60:622–629. doi: 10.1111/jcpp.13025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lamm C., Walker O.L., Degnan K.A., et al. Cognitive control moderates early childhood temperament in predicting social behavior in 7-year-old children: an ERP study. Dev Sci. 2014;17:667–681. doi: 10.1111/desc.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeman J.L., Cassano M., Suveg C., Shipman K. Initial validation of the children’s worry management scale. J Child Fam Stud. 2010;19:381–392. [Google Scholar]
- 27.Folk J.B., Zeman J.L., Poon J.A., Dallaire D.H. A longitudinal examination of emotion regulation: pathways to anxiety and depressive symptoms in urban minority youth. Child Adolesc Ment Health. 2014;19:243–250. doi: 10.1111/camh.12058. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 29.Rosseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36. [Google Scholar]
- 30.Aiken L.S., West S.G., Reno S.S. Sage Publications; Newbury Park, CA: 1991. Multiple Regression: Testing and Interpreting Interactions. [Google Scholar]
- 31.Morales S., Miller N.V., Troller-Renfree S.V., et al. Attention bias to reward predicts behavioral problems and moderates early risk to externalizing and attention problems. Dev Psychopathol. 2020;32:397–409. doi: 10.1017/S0954579419000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Enders C.K., Bandalos D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct Equ Model. 2001;8:430–457. [Google Scholar]
- 33.Satorra A., Bentler P.M. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.MacKinnon D.P., Lockwood C.M., Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tiirikainen K., Haravuori H., Ranta K., Kaltiala-Heino R., Marttunen M. Psychometric properties of the 7-item Generalized Anxiety Disorder Scale (GAD-7) in a large representative sample of Finnish adolescents. Psychiatry Res. 2019;272:30–35. doi: 10.1016/j.psychres.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Topper M., Emmelkamp P.M.G., Watkins E., Ehring T. Prevention of anxiety disorders and depression by targeting excessive worry and rumination in adolescents and young adults: a randomized controlled trial. Behav Res Ther. 2017;90:123–136. doi: 10.1016/j.brat.2016.12.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.