Abstract
Increasing evidence suggests that females are more vulnerable to the harmful effects of drugs of abuse, including opioids. Additionally, rates of heroin-related deaths substantially increased in females from 1999 to 2017 [1], underscoring the need to evaluate sex differences in heroin vulnerability. Moreover, the neurobiological substrates underlying sexually dimorphic responding to heroin are not fully defined. Thus, we evaluated male and female Long Evans rats on acquisition, dose-responsiveness, and seeking for heroin self-administration (SA) as well as using a long access model to assess escalation of intake at low and high doses of heroin, 0.025 and 0.1 mg/kg/inf, respectively. We paired this with ex vivo fast-scan cyclic voltammetry (FSCV) in the medial nucleus accumbens (NAc) shell and quantification of mu-opioid receptor (MOR) protein in the ventral tegmental area (VTA) and NAc. While males and females had similar heroin SA acquisition rates, females displayed increased responding and intake across doses, seeking for heroin, and escalation on long access. However, we found that males and females had similar expression levels of MORs in the VTA and NAc, regardless of heroin exposure. FSCV results revealed that heroin exposure did not change single-pulse elicited dopamine release, but caused an increase in dopamine transporter activity in both males and females compared to their naïve counterparts. Phasic-like stimulations elicited robust increases in dopamine release in heroin-exposed females compared to heroin-naïve females, with no differences seen in males. Together, our results suggest that differential adaptations of dopamine terminals may underlie the increased heroin SA behaviors seen in females.
Subject terms: Reward, Addiction
Introduction
Within the last decade, rates of opioid abuse and opioid-related overdoses have increased to epidemic levels [2], underscoring the need to understand the neurobiological bases of vulnerabilities to opioid use disorder (OUD). A large body of clinical literature clearly demonstrates that men display more opioid-related overdoses and negative outcomes when compared to women [3–9]. However, recent studies have suggested that rates of heroin use and overdose are rapidly increasing in women [1]. In addition, female heroin users progressed to meet the criteria for OUD faster than men [10], suggesting that females may be more vulnerable to particular aspects of heroin abuse, such as escalation of use, than men. Therefore, it is important to evaluate sex-dependent heroin self-administration behaviors and attempt to define the neurobiology that may drive female vulnerability to heroin abuse.
Preclinical rodent models of heroin self-administration have shown conflicting results regarding sex differences, with some studies reporting that female rats exhibit greater intake of opioids, including heroin [11–14], and others reporting no differences between sexes [15–22]. However, these studies varied widely in the behavioral outcomes measured, the species and strain of rodents utilized, and the dose(s) of heroin used, making it difficult to determine if sex differences are in fact present in heroin self-administration. Moreover, many studies have also found that differences in dopamine system function may be responsible for the increased responding for psychostimulants and other drugs of abuse seen in female rodents [23–25] (for review [26]).
While previous studies suggested that heroin reinforcement escaped involvement of the dopamine system [27–29], more recently, circuit-level studies have demonstrated that the dopamine system plays a substantial role in the reinforcing properties of heroin [30, 31]. Currently, it is thought that heroin drives reinforcement by activating mu opioid receptors (MORs) located on GABA-containing interneurons in the ventral tegmental area (VTA). Activation of MORs causes disinhibition of dopamine cell bodies by removing inhibitory GABAergic influence and results in increased cell firing as well as increased release from dopamine terminals in the nucleus accumbens (NAc) [32]. Furthermore, it has been proposed that the increased dopamine release, particularly the medial shell region of the NAc, is the primary driver of heroin reinforcement [30]. Because sex differences have been found in both dopamine system function and opioid reinforcement, it is possible that the dopamine system plays a central role in regulating sex differences in heroin self-administration.
The present study evaluated sex differences in acquisition, dose-responsiveness, seeking behavior, and escalation of heroin self-administration. We assessed MOR protein expression levels in the NAc and VTA of drug-naïve and heroin-exposed rats and used fast-scan cyclic voltammetry in medial NAc shell-containing brain slices to measure dopamine terminal alterations following heroin self-administration.
Methods and materials
Animals
Male and female Long Evans rats (Envigo, Indianapolis, IN), weighing 200–350 g, were maintained on a 12:12 h light/dark cycle (0300 h lights off; 1500 h lights on) with food and water ad libitum. All animals were maintained according to the National Institutes of Health guidelines in Association for Assessment and Accreditation of Laboratory Animal Care accredited facilities. The experimental protocol was approved by the Institutional Animal Care and Use Committee at Wake Forest School of Medicine.
Drugs
Heroin (diamorphine) HCl was provided by the National Institute on Drug Abuse (NIDA) Drug Supply Program (Research Triangle Park, NC, USA). Heroin HCl was dissolved in 0.9% physiological saline and filtered prior to experimental use. All drug concentrations are represented as the weight of the salt.
Self-administration surgery and training
Rats were anesthetized with ketamine (100 mg/kg) and xylazine (10 mg/kg) and implanted with chronic indwelling jugular catheters as previously described [33]. At the completion of surgery, rats were given an injection of ketoprofen (2 mg/kg s.c.) as a postsurgical anesthetic and singly housed in cages that served as both housing cages and self-administration chambers. All sessions took place during the active/dark cycle (0900–1500 h). Following a two-day post-surgical recovery period, all rats were given access to heroin (0.025 or 0.1 mg/kg/inf) on a fixed ratio one (FR1) schedule by a lever. These doses were chosen because previous studies have shown they represent low and high doses of heroin [31], respectively, and maintain long-term stable responding [34]. Training sessions (acquisition) were initiated by extension of the lever into the chamber and were terminated after 20 infusions or 6 h, whichever occurred first. During training, each lever response resulted in a 20-s time-out period in which the lever retracted and light was illuminated. Following the training period, the time-out period was equivalent to the length of the infusion. Acquisition was considered complete when rats responded for 20 infusions per session across 5 consecutive daily sessions.
FR1 dose–response curve and seeking probe test
Following acquisition, a heroin dose–response curve (0.00781–0.05000 mg/kg/inf) was generated for each rat during daily 3 h sessions; this session length was chosen to prevent escalation of intake across days [35–37]. Doses were presented in a pseudo-randomized order in which no two doses were ascending or descending, as previously described [38]. Only one dose was tested per daily session and all rats received the same pattern of doses. Following the final dose–response session, heroin was replaced with saline and rats were tested for cue-reactivity during a single 3-h session.
Long access
Rats were given unlimited access to heroin (0.025 or 0.1 mg/kg/inf) during 6 h sessions for 10 consecutive days. Self-administration session were conducted 7 days a week.
Ex vivo fast-scan cyclic voltammetry (FSCV)
FSCV was used to characterize presynaptic dopamine system function and dopamine release under single pulse “tonic-like” stimulations and trains of stimuli (10 pulses at 10–60 Hz; multi-pulse “phasic-like” stimulation). Approximately 18 h after their final long access session, at the time when the rats would normally begin their heroin session (0900), they were deeply anesthetized with isoflurane and rapidly decapitated. The brain was removed and immersed in oxygenated artificial cerebrospinal fluid (aCSF) containing (in mM): NaCl (126), KCl (2.5), NaH2PO4 (1.2), CaCl2 (2.4), MgCl2 (1.2), NaHCO3 (25), glucose (11), l-ascorbic acid (0.4). A vibrating tissue slicer (Leica VT1200S, Leica Biosystems, Wetzler, Germany) was used to prepare 400 µm thick coronal brain slices containing the medial NAc shell. Slices were transferred to a recording chamber and submerged in a bath of oxygenated aCSF (32 °C) perfused at a rate of 1 mL/min. A carbon fiber microelectrode (CFE; 100–200 μM length, 7 μm diameter and bipolar stimulating electrode (MS303–3-B-SPC, Plastics One, Roanoke, VA) were placed in the medial NAc shell. Endogenous dopamine release was evoked by a single electrical pulse (750 μA, 4 ms, monophasic) applied to the slice every 3 min. Extracellular dopamine was measured by applying a triangular waveform (−0.4 to +1.2 to −0.4 V vs Ag/AgCl, 400 V/s) to the CFE. Once the extracellular dopamine response was stable for three successive collections, the effects of different stimulation patterns on dopamine release were tested. More specifically, a frequency–response curve was obtained using 10 pulse stimulations at sequential 10, 20, 40, and 60 Hz frequencies with 5 min interstimulus intervals.
Western blot hybridization
In rats that were self-administering the highest heroin dose, 0.1 mg/kg/infusion, the morning following the last long access session, brain tissue punches containing the NAc and VTA were collected, flash-frozen in isopentane, and stored at −80 °C until processing. Tissue was similarly collected and stored from a separate group of age- and size-matched drug-naïve rats to serve as controls. Tissue punches were homogenized in lysis buffer (20 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid pH 7.4, 5 mM ethylenediaminetetraacetic acid pH 8.0, and Halt, a protease and phosphatase inhibitor cocktail (Thermo Fisher Scientific, Waltham, MA) and centrifuged at 14,000 g for 25 min at 4 °C. The supernatant was collected and protein concentrations were determined with a commercially available BCA protein assay kit (23225; ThermoScientific). 50 µg of protein was separated on 10% reducing SDS-PAGE gels at transferred to 0.2 µm nitrocellulose membrane overnight. Nonspecific binding was blocked using a solution of 5% nonfat milk in tris-buffered saline with 0.1% Tween-20 (TBST-0.1%) for 1 h, before incubation in blocking buffer with the primary antibodies: rabbit anti-mu opioid receptor (1:1000, Abcam, AB5511) and mouse anti-actin (1:10 000, Sigma, A1978) overnight at 4 °C. Membranes were rinsed in TBST-0.1%, incubated in fluorescence-conjugated secondary antibodies (1:4000, LI-COR, AF680, and AF800), and imaged on a LICOR Odyssey imaging system. Image Studio Lite and ImageJ (National Institutes of Health) were used for densitometry analyses of proteins and preparation of representative images, respectively.
Data analysis
Demon Voltammetry and Analysis software [39] was used to analyze all FSCV data. Recording electrodes were calibrated at the end of every experiment by washing 3 μM dopamine over the CFE using a flow-injection system and measuring the resulting current, which was then converted to an individualized experiment calibration factor (in nA/μM DA). The calibration factor of each electrode was used to convert the electrical current measured during experiments to dopamine concentration. Michaelis-Menten modeling was used to determine the concentration and maximal rate of dopamine uptake (Vmax) of evoked dopamine responses.
Statistics
GraphPad Prism 7 (La Jolla, CA, USA) was used to statistically analyze all datasets and create graphs. Behavioral data and frequency response curves were analyzed using either a Student’s t test or two-way repeated-measures ANOVA followed by Bonferroni’s posthoc tests when significant main effects were observed. Baseline voltammetry release and reuptake data, before and after drug perfusion, were compared using a one-way or three-way ANOVA, with group differences being tested using Tukey’s posthoc tests where noted. Phasic/tonic ratios and all western blot hybridization data were analyzed using a two-tailed Student’s t test. All data are reported as mean ± SEM. All p values of <0.05 were considered to be statistically significant.
Results
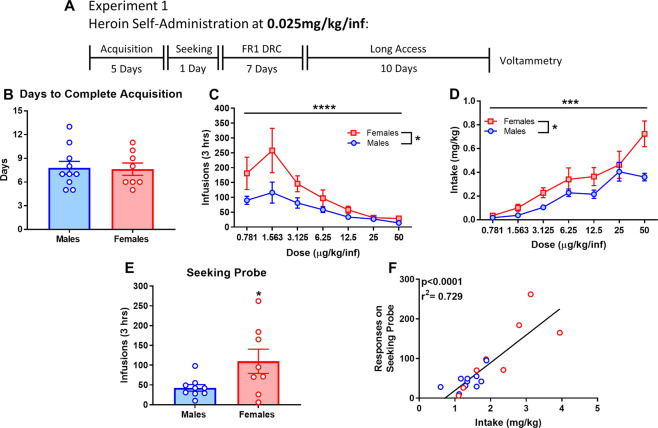
Females show increased responding, intake, and seeking for heroin across doses, but similar rates of acquisition
A group of male and female rats was given access to heroin (0.025 mg/kg/inf) on an FR1 schedule of reinforcement during 6 h sessions without prior operant training (acquisition). During acquisition, female and male rats did not differ in the number of days taken to complete 5 sessions of 20 lever presses (Fig. 1B), nor the number of days to reach the first day of 20 lever presses or the length of time to complete 20 lever presses in each of the 5 sessions (data not shown). After meeting acquisition criteria, rats were tested for responding to heroin across several doses (0.0781–50 µg/kg/inf). Males and females showed a main effect of dose-dependent responding (Fig. 1C, F(2.109,33.74) = 13.48, p = 0.000038) and intake (Fig. 1D, F(2.603,41.64) = 28.27, p = 0.0000000016), and sex with female rats responding more overall (Fig. 1C, F(1,16) = 5.376, p = 0.0339) and taking more heroin (Fig. 1D, F(1,16) = 6.952, p = 0.0179) than males. There was also a significant interaction of Dose × Sex for the intake of heroin (Fig. 1D, F(6,96) = 2.603, p = 0.0221). Following dose–response curves, rats were tested on seeking probe test by substituting saline for heroin during a single 3-h session. Female rats displayed increased responding on the seeking probe compared to males (Fig. 1E, t15 = 2.23, p = 0.0414). Responding during the seeking probe and total heroin intake during the dose–response curve were positively correlated (Fig. 1F, correlation: r2 = 0.729, p = 0.000007; linear regression: β = 69.94 ± 10.66).
Fig. 1. Females show increased responding, intake, and seeking for heroin across doses, but similar rates of acquisition.
A Experimental timeline of behavioral procedure. B Female and male rats did not differ in total number of days to reach acquisition criteria. C Comparison of dose-responsivity for heroin revealed that females have greater responding for and D intake of heroin across various doses. E Responding during a seeking probe test was greater in female rats. F Correlation of responding during the seeking probe and total intake during the dose–response curve demonstrates a positive interaction between the two measures. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. n = 8–10 per group.
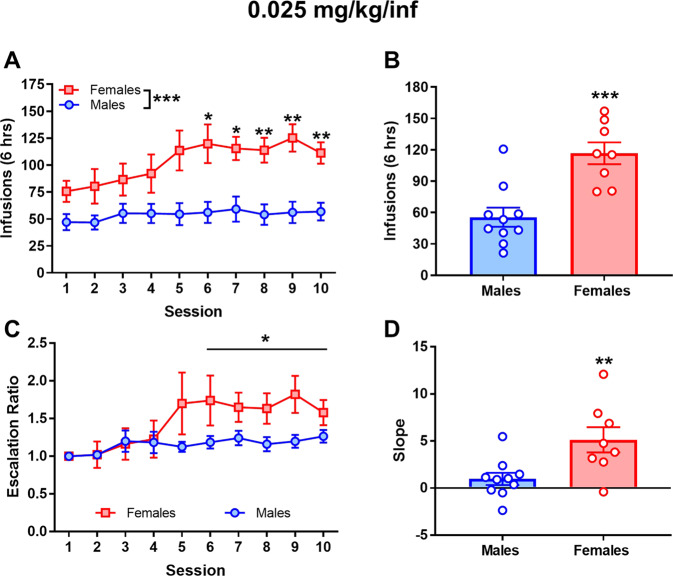
Females exhibit increased responding and escalation for a low dose of heroin during long access
To assess differences in escalation of heroin self-administration, male and female rats were placed on a long access procedure, which has been used to model the transition to excessive drug intake [36, 40, 41]. Comparing session 6–10 of long access, following stabilization of responding, there was a main effect of sex (Fig. 2A, F(1,16) = 16.33, p = 0.0009). Bonferroni post hoc analysis revealed a significant difference in responding at sessions 6–10 (6, p = 0.0498; 7, p = 0.0145, 8, p = 0.0063; 9, 0.0040; 10, p = 0.0041). Averaged responses during the last three long access sessions were increased in females (Fig. 2B, t16 = 4.428 p = 0.000022). Escalation ratios were also determined for each long access session by calculating number of responses in an individual session in comparison to the responding on session 1 of long access. In addition, to evaluate the overall magnitude of escalation across the 10 days of long access, the slope of responding was derived from the difference in responding between session 1 compared to session 10 [42]. A two-way repeated-measures ANOVA of sessions 6–10 revealed a main effect of sex (Fig. 2C, F(1,16)=5.153, p = 0.0374). Females also had increased escalation slope values compared to males (Fig. 2D, t16 = 2.974 p = 0.0089).
Fig. 2. Females exhibit increased responding and escalation for a low dose, 0.025 mg/kg/inf, of heroin during long access.
A Responding for heroin at 0.025 mg/kg/inf was greater in females rats compared to male rats during the second half of long access (sessions 6–10). B Average responding during the final 3 days of long access was increased in females. C Analysis of escalation ratios, responding during individual sessions compared to session 1, during long access demonstrate increased escalation of responding in female rats across sessions 6–10. D The slope of responding during the ten long access sessions was increased in female rats. *p < 0.05; **p < 0.01; ***p < 0.001. n = 8–10 per group.
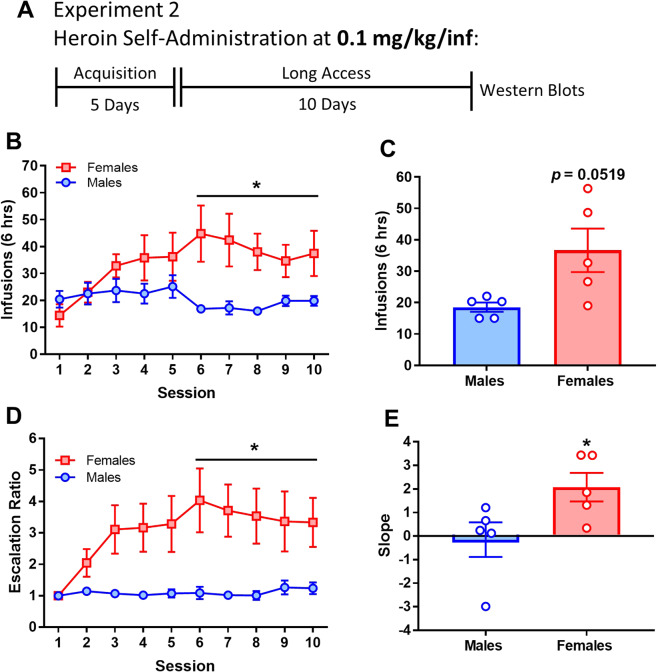
Female rats also have increased responding for a high dose of heroin on long access
To evaluate if sex differences in responding on long access are sensitive to heroin dose, male and female rats were trained on heroin self-administration and placed on long access at a dose of 0.1 mg/kg/infusion. A two-way repeated measures ANOVA of sessions 6–10, when responding stabilized, revealed the main effect of sex (Fig. 3B, F(1,8) = 6.831, p = 0.0310). Comparison of the averaged last three days of long access produced a trend (p = 0.0519) towards increased responding in females (Fig. 3C). Upon comparing escalation ratios from sessions 6–10, a main effect of sex (Fig. 3D, F(1,8) = 7.671, p = 0.0243). The slope of responding for heroin across the ten long access sessions was higher in females (Fig. 3E, t8 = 2.343, p = 0.0472).
Fig. 3. Female rats also have increased responding for a high dose, 0.1 mg/kg/inf, of heroin on long access.
A Experimental timeline of the behavioral procedure. B Female rats display increased lever press responding for heroin during the second half of long access (sessions 6–10). C Females show a trend for increased heroin responding during the final 3 days of long access (p = 0.0519). D Analysis of escalation ratios during long access demonstrate increased escalation of responding in female rats across sessions 6–10. E The slope of responding during the ten long access sessions was increased in female rats. *p < 0.05; **p < 0.01; ****p < 0.0001. n = 5 per group.
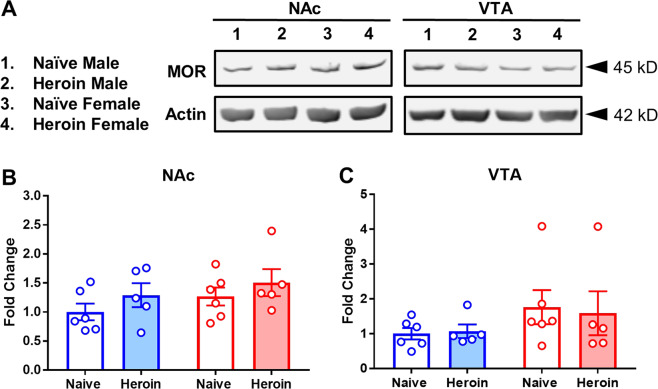
Mu opioid receptor (MOR) protein levels do not differ between drug naïve or heroin-exposed male and female rats in the NAc or VTA
We performed western blot analyses on NAc- and VTA-containing tissue punches from male and female rats after long access, at 0.1 mg/kg/inf, and heroin-naïve controls. There was no effect (p > 0.05) of heroin or sex on MOR protein levels in NAc (p = 0.1656) or VTA (p = 0.5916) (Fig. 4A–C).
Fig. 4. Mu opioid receptor (MOR) protein levels do not differ between drug naïve or heroin-exposed male and female rats in the NAc or VTA.
A Representative blots of all four treatment groups. B MOR expression in the nucleus accumbens (NAc) did not differ between the groups. C No significant difference in MOR expression in the VTA across groups.
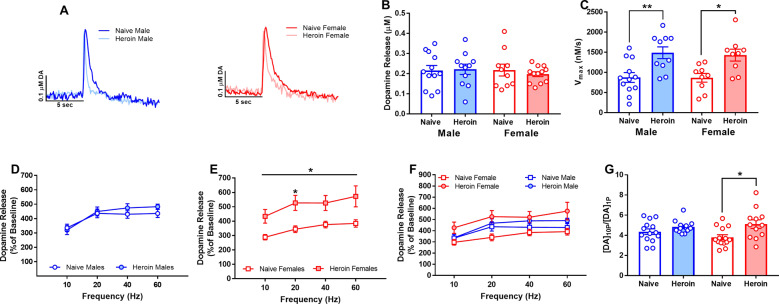
Heroin self-administration increased the rate of dopamine reuptake in both sexes and phasic-like dopamine release in the medial NAc shell of female rats
Dopamine neurons exhibit two different patterns of firing: a pacemaker pattern which is thought to give rise to low “tonic” levels of dopamine [43] and a more variable burst-like pattern, typically in response to environmental stimuli, which gives rise to higher “phasic” release of dopamine [44, 45]. Using FSCV, we measured dopamine kinetics in medial NAc shell-containing brain slices to evaluate the effects of heroin self-administration (0.025 mg/kg/infusion) on “tonic-like” single-pulse stimulated dopamine release and subsequent uptake. We found that single-pulse stimulated dopamine release did not differ by sex or drug condition (Fig. 5B). However, a one-way ANOVA of the maximal rate of dopamine uptake, Vmax, indicated the main effect of drug condition (Fig. 5C, F(1,36) = 19.56, p = 0.000086). Tukey’s post hoc comparisons revealed significant differences between heroin-exposed males and females relative to their naïve counterparts, although there were no sex-dependent differences. These alterations in dopamine transporter kinetics suggest that heroin self-administration increased DAT function, regardless of sex. To evaluate how heroin self-administration alters phasic dopamine release, we used a “multi-pulse” stimulation train (ten pulses) protocol across a range of frequencies (10–60 Hz) to model burst-like patterns of dopamine neuron firing. Female rats that were exposed to heroin self-administration exhibited increased phasic dopamine release following multi-pulse stimulations, across frequencies, compared to their female naïve counterparts (Fig. 5E). There was no difference seen in males (Fig. 5D). A two-way mixed ANOVA revealed a main effect of frequency (Fig. 5E, F(1.144,20.59) = 4.287, p = 0.0466) and drug condition (Fig. 5E, F(1,18) = 7.863 p = 0.0117). Bonferroni comparisons indicated there were significant differences at the 20 Hz (p = 0.0394) frequency. To directly compare males and females, a three-way ANOVA was conducted, which revealed a main effect of condition (Fig. 5F, F(1,148) = 21.08, p = 0.000009) and a significant interaction between sex and condition (Fig. 5F, F(1,148) = 7.827, p = 0.0058). To quantify this finding and account for variable release amounts at different sites, a phasic/tonic ratio was calculated, which divides maximal release at the ten pulses, 60 Hz stimulation by the baseline 1 pulse stimulation amplitude in each slice. A two-way ANOVA revealed a main effect of drug condition (Fig. 5G, F(1,49) = 9.405 p = 0.0035), but not sex. Bonferroni’s post hoc analysis revealed significant differences between naïve females and heroin females (p = 0.0165).
Fig. 5. Heroin self-administration increased the rate of dopamine reuptake in both sexes and phasic-like dopamine release in the medial NAc shell of female rats.
A Representative traces of electrically-evoked dopamine demonstrating increased uptake in heroin-exposed males and females compared to their respective heroin-naïve counterparts. B Stimulated dopamine release did not differ between any treatment groups. C The maximal rate of dopamine uptake (Vmax) was increased in heroin-exposed males and females. D Heroin-exposed and heroin-naïve males did not differ in dopamine elicited by multi-pulse stimulation trains at increasing frequencies; however, heroin females have greater dopamine release across frequencies than heroin-naïve females (E). F A comparison of both sexes and conditions reveal that the increase in phasic dopamine release is specific to female rats after heroin. G Comparison of average phasic/tonic ratios was increased in heroin females compared to their naïve counterparts, as depicted by the concentration of stimulated dopamine release at ten pulses over one pulse. *p < 0.05; **p < 0.01. n = 5–6 rats per group.
Discussion
Here, we document greater vulnerability of females to heroin, which is congruent with published reports evaluating sex differences in other drugs of abuse. Importantly, we thoroughly evaluate multiple aspects of self-administration behaviors at two different training doses. Furthermore, we have identified a neurobiological correlate that may underlie the heightened propensity of females to self-administer opioids. Our results indicate that female and male rats do not differ in rates of acquisition; however, females showed increased responding for and intake of heroin across several doses, increased seeking behavior when heroin was replaced with saline and increased intake and escalation during a long access procedure at both low and high doses. Additionally, although heroin self-administration did not alter the magnitude of tonic-like, single-pulse dopamine release we found enhanced phasic-like, multi-pulse release in heroin-exposed females, but not males. In addition, maximal dopamine uptake rates were increased in both sexes, suggesting increased DAT functionality and/or expression after heroin self-administration.
The lack of sex differences in the acquisition of heroin self-administration in the present study agrees with some previous findings [15], however, it contradicts others that showed females acquired heroin self-administration more rapidly than males [13, 14]. It is important to note that these studies differed significantly from the present study, in that the prior studies used an auto-shaping procedure to train rats to lever press, while rats in this study had no prior operant experience and were allowed to acquire self-administration on their own. In addition, the previous studies used a lower dose of heroin, 0.015 mg/kg/infusion, compared to the 0.025 or 0.1 mg/kg/infusion doses used in this study. These factors may alter the rate of acquisition of drug self-administration [46]. Therefore, additional studies evaluating the effects of self-administration environments and doses will aid in understanding sex differences in acquisition of heroin self-administration.
We documented a vertical shift in the dose–response curve for heroin in females compared to males. It has been suggested that an upward shift in dose–response curves for drugs of abuse is indicative of an increase in drug efficacy rather than increased drug potency, which would be indicated by a leftward shift [47]. Piazza and colleagues stated that individual subjects who display increased responding for drugs across a range of doses represent a more “vulnerable” population and would be more likely to develop drug abuse when higher doses of the drug are present [47]. Moreover, responding during the seeking probe positively correlated with total heroin intake during the dose–response curve, making it difficult to disentangle the two behaviors. Separating intake from seeking in a procedure that limits the number of infusions available per day, thereby standardizing intake prior to assessing seeking, would be helpful in this regard. As has been shown with other drugs of abuse [26, 48, 49], inherent sex differences may have led to both increased heroin responding and seeking, suggesting that biological sex is a factor contributing to vulnerable phenotypes related to heroin abuse.
The greater escalation of heroin self-administration during long access in females is consistent with a previous study showing increased responding for heroin under a long access procedure in female mice [12], yet it contradicts other studies that suggest there are no sex differences in the maintenance or escalation phase of self-administration [17–22]. A major difference is that, in the current study, rats were housed in boxes that served as both the operant and housing chambers. This experimental setup has been shown to increase the saliency of drug-paired cues [50], which has been shown to elicit greater responses in female heroin users [51]. It has been previously shown that male rats housed in their testing chambers self-administered more heroin than those who lived in separate housing chambers [52]. Thus, it is possible that these environmental variables may have driven the increased responding seen in females in the current study. The escalation of responding seen here in females is profound (nearly two- and fourfold higher at 0.025 and 0.1 mg/kg/inf doses, respectively), especially when compared to the lack of escalation exhibited by males. However, it is important to note that escalation during long access heroin self-administration in male rats has been shown to be more prominent in session lengths greater than 6 h [53]. The increased responding of females in most of the measured self-administration behaviors could be explained by either heightened or lowered sensitivity to heroin’s reinforcing properties. Alternatively, it is possible that the rate of tolerance to the sedative effects of heroin may be different between males and females [54]. Taken together, the present study demonstrates divergent heroin self-administration behaviors between males and females; however, it is unknown whether these results would be applicable to self-administration of other opioids, such as oxycodone or morphine.
Prior studies have shown that chronic exposure to opioids results in reduced MOR function (for review [55]) which is thought to play a significant role in tolerance to opioids [56]. Therefore, we hypothesized that intrinsic differences in MOR expression or differences in heroin-induced adaptations may underlie the divergent responding seen between males and females. However, we did not find any significant differences in MOR immunoreactivity between sexes or heroin conditions, in either NAc or VTA. While we did not see a change in total protein levels of MOR, this does not exclude the possibility that MORs may have altered functioning and/or signaling capabilities. Some studies have indicated increased activity of MORs on GABAergic neurons in the VTA after heroin self-administration [57–60]. This suggests that augmented heroin responding and phasic-like dopamine release in females is probably not due to differences in MOR levels but may be due to altered MOR activity or sex-dependent regulation of dopamine terminals.
Somewhat surprisingly, we did not see a difference in single-pulse electrically-stimulated (tonic) dopamine release following long access heroin exposure in male or female rats. The present study evaluated dopamine terminal alterations after 10 days of long access and during acute withdrawal (~18 h), which we have found is an optimal time point for assessing terminal alterations following exposure to several other drugs of abuse [61–65]. However, it is unknown if longer exposure to heroin or a longer withdrawal period would yield different changes in dopamine dynamics. While we did not observe differences in single pulse evoked dopamine release, we did see increases in dopamine uptake rate, a measure of DAT function, following heroin exposure, although this change was not sex-dependent. This finding was unexpected, as heroin exposure resulted in decreased DAT mRNA expression [66], binding availability [67], and protein levels [68] in the NAc of human heroin users. However, this discrepancy may be explained by the differences between total levels of static markers and DAT activity at the plasma membrane, as well as the fact that the entire NAc was evaluated in humans, rather than just the medial shell of the NAc as in the current study. Our group has also found increased DAT function with chronic alcohol exposure [69, 70] and methylphenidate [64, 71], but not cocaine or amphetamine self-administration [72, 73], suggesting that elevations of extracellular dopamine alone cannot explain functional DAT changes. In the case of stimulants, the characteristics of drug-DAT interactions may determine activity changes. Methylphenidate self-administration produced large increases in dopamine uptake rates, which led to increased effects of DAT substrates/releasers, most likely due to greater intracellular accumulation of drug, without changing the effects of blockers [73]. Therefore, it would be interesting to evaluate if heroin self-administration would show a similar pattern of altered stimulant effects.
The DAT is a major regulator of dopamine terminal function, and it is a primary determinant of extracellular dopamine levels in the NAc [74]. Thus, we hypothesize that the increased uptake seen here would lead to lower extracellular dopamine levels, as seen in previous studies using microdialysis [75–77]. To our knowledge, this is the first preclinical report evaluating DAT activity following exposure to heroin in rats. These data support the conclusion that neural adaptions to downregulate dopamine activity occur in response to repeated exposure to heroin, as they do with other drugs of abuse [61, 78, 79]. It is thought that drug-mediated compensatory alterations in presynaptic dopamine terminals result in a state of hypodopaminergia [78–81], which may engender anhedonia and/or dysphoria and thereby promote increased drug-taking and relapse [80–84].
In addition to alterations in dopamine uptake kinetics, we also observed a robust increase in phasic dopamine release under burst-like stimulation patterns in heroin-exposed females, but not males, without changes in single-pulse evoked release. Increases in phasic firing of VTA dopamine neurons occur in response to salient stimuli, such as drugs of abuse or drug-related cues, and are thought to drive drug seeking [85–88]. In addition, in freely behaving rats, the peak concentration of phasic dopamine release events evoked by reward cues is directly related to the magnitude of the expected reward [89]. One possible explanation for our finding that only multipulse-evoked release in females is increased is that after heroin self-administration, MOR activity is increased in on GABAergic neurons in the VTA [57–60], selectively in heroin exposed females. This would lead to increased disinhibition of dopamine neurons in the VTA and thereby, prime dopamine terminals in the NAc to release more dopamine during stimulation trains [90, 91]. Another possibility is that in females, increased phasic dopamine release is due to altered activity of cholinergic interneurons in the NAc that also contain MOR [92, 93]. Dopamine release is highly regulated by cholinergic activity, with activation of nicotinic receptors on dopamine terminals increasing single pulse release and decreasing phasic, multipulse release. If females have increased MOR activity in cholinergic interneurons in the NAc, acetylcholine levels and nicotinic receptor activity would be reduced, resulting in the enhanced phasic dopamine release seen in heroin exposed females. Similarly, lower acetylcholine levels would reduce dopamine tone and autoreceptor-mediated inhibition of phasic dopamine release, thus leading to augmented phasic dopamine release [94].
Conclusions
Taken together, this study provides insights into potential neurobiological mechanisms underlying sexually dimorphic heroin self-administration behaviors. These data suggest that increased heroin self-administration and seeking in females may be linked to an enhancement of phasic dopamine release in the NAc; however, the exact mechanism has yet to be identified. Nevertheless, these changes could lead to increases in the saliency of drug-related stimuli [43]. Therefore, it is tempting to speculate that heroin-induced dopamine changes may lead to greater positive reinforcing value and drug cue reactivity underlying heightened female vulnerability to heroin abuse and addiction.
Funding and disclosure
This work was supported by NIH grants F31 DA049504 (BEG), T32 DA041349 (BEG, SHB), R01 DA048490 (SRJ), P50 DA006634 (SRJ), T32 AA007565 (KMH), R01 AA023999 (KMH and SRJ), U01 AA014091 (KMH and SRJ), NS105005 (KFR-G) and DoD grant USAMRMC W81XWH-14-1-0061 (KFR-G). The authors declare no competing interests.
Author contributions
BEG, RTL, and SRJ were responsible for the study concept and design. BEG conducted all of the behavioral and voltammetry experiments and analyzed these data under the guidance of LBK and KMH. SHB conducted western blotting experiments and analyzed this data under the guidance of KRG, BEG, and SRJ drafted the manuscript. All authors provided critical revision of the manuscript for important intellectual content. All authors critically reviewed content and approved final version for publication.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.VanHouten J, Rudd R, Ballesteros M, Mack K. Drug overdose deaths among women aged 30–64 years—United States, 1999–2017. Morb Mortal Wkly Rep. 2019;68:1–5. doi: 10.15585/mmwr.mm6801a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154–63. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powis B, Griffiths P, Gossop M, Strang J. The differences between male and female drug users: community samples of heroin and cocaine users compared. Subst Use Misuse. 1996;31:529–43. doi: 10.3109/10826089609045825. [DOI] [PubMed] [Google Scholar]
- 4.Hickman M, et al. Drug-related mortality and fatal overdose risk: pilot cohort study of heroin users recruited from specialist drug treatment sites in London. J Urban Health. 2003;80:274–87. doi: 10.1093/jurban/jtg030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roxburgh A, et al. Trends in heroin and pharmaceutical opioid overdose deaths in Australia. Drug Alcohol Depend. 2017;179:291–8. doi: 10.1016/j.drugalcdep.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–14. Morb Mortal Wkly Rep. 2016;64:1378–82. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 7.Marsh JC, Park K, Lin YA, Bersamira C. Gender differences in trends for heroin use and nonmedical prescription opioid use, 2007–14. J Subst Abus Treat. 2018;87:79–85. doi: 10.1016/j.jsat.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zacny JP. Morphine responses in humans: a retrospective analysis of sex differences. Drug Alcohol Depend. 2001;63:23–28. doi: 10.1016/s0376-8716(00)00186-1. [DOI] [PubMed] [Google Scholar]
- 9.Zun LS, Downey LVA, Gossman W, Rosenbaum J, Sussman G. Gender differences in narcotic-induced emesis in the ED. Am J Emerg Med. 2002;20:151–4. doi: 10.1053/ajem.2002.32631. [DOI] [PubMed] [Google Scholar]
- 10.Hser YI, Anglin MD, Booth MW. Sex differences in addict careers. 3. Addiction. Am J Drug Alcohol Abus. 1987;13:231–51. doi: 10.3109/00952998709001512. [DOI] [PubMed] [Google Scholar]
- 11.Cicero TJ, Aylward SC, Meyer ER. Gender differences in the intravenous self-administration of mu opiate agonists. Pharm Biochem Behav. 2003;74:541–9. doi: 10.1016/s0091-3057(02)01039-0. [DOI] [PubMed] [Google Scholar]
- 12.Towers EB, Tunstall BJ, McCracken ML, Vendruscolo LF, Koob GF. Male and female mice develop escalation of heroin intake and dependence following extended access. Neuropharmacology. 2019;151:189–94. doi: 10.1016/j.neuropharm.2019.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carroll ME, Morgan AD, Lynch WJ, Campbell UC, Dess NK. Intravenous cocaine and heroin self-administration in rats selectively bred for differential saccharin intake: phenotype and sex differences. Psychopharmacology. 2002;161:304–13. doi: 10.1007/s00213-002-1030-5. [DOI] [PubMed] [Google Scholar]
- 14.Lynch WJ, Carroll ME. Sex differences in the acquisition of intravenously self-administered cocaine and heroin in rats. Psychopharmacology. 1999;144:77–82. doi: 10.1007/s002130050979. [DOI] [PubMed] [Google Scholar]
- 15.Stewart J, Woodside B, Shaham Y. Ovarian hormones do not affect the initiation and maintenance of intravenous self-administration of heroin in the female rat. Psychobiology. 1996;24:154–9. [Google Scholar]
- 16.Zhang Y, et al. Mouse model of the OPRM1 (A118G) polymorphism: differential heroin self-administration behavior compared with wild-type mice. Neuropsychopharmacology. 2015;40:1091–1100. doi: 10.1038/npp.2014.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vazquez M, Frazier JH, Reichel CM, Peters J. Acute ovarian hormone treatment in freely cycling female rats regulates distinct aspects of heroin seeking. Learn Mem. 2020;27:6–11. doi: 10.1101/lm.050187.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Venniro M, Zhang M, Shaham Y, Caprioli D. Incubation of methamphetamine but not heroin craving after voluntary abstinence in male and female rats. Neuropsychopharmacology. 2017;42:1126–35. doi: 10.1038/npp.2016.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Venniro M, Russell TI, Zhang M, Shaham Y. Operant social reward decreases incubation of heroin craving in male and female rats. Biol Psychiatry. 2019;86:848–56. doi: 10.1016/j.biopsych.2019.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bossert JM, et al. In a rat model of opioid maintenance, the G protein-biased MU opioid receptor agonist TRV130 decreases relapse to oxycodone seeking and taking and prevents oxycodone-induced brain hypoxia. Biol Psychiatry. 2020;88:935–44. doi: 10.1016/j.biopsych.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fredriksson I, et al. Effect of the dopamine stabilizer (-)-OSU6162 on potentiated incubation of opioid craving after electric barrier-induced voluntary abstinence. Neuropsychopharmacology. 2020;45:770–9. doi: 10.1038/s41386-020-0602-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reiner DJ, et al. Role of projections between piriform cortex and orbitofrontal cortex in relapse to fentanyl seeking after palatable food choice-induced voluntary abstinence. J Neurosci. 2020;40:2485–97. doi: 10.1523/JNEUROSCI.2693-19.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calipari ES, et al. Dopaminergic dynamics underlying sex-specific cocaine reward. Nat Commun. 2017;8:13877. doi: 10.1038/ncomms13877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blanchard BA, Steindorf S, Wang S, Glick SD. Sex differences in ethanol-induced dopamine release in nucleus accumbens and in ethanol consumption in rats. Alcohol Clin Exp Res. 1993;17:968–73. doi: 10.1111/j.1530-0277.1993.tb05650.x. [DOI] [PubMed] [Google Scholar]
- 25.Velásquez VB, et al. Programming of dopaminergic neurons by early exposure to sex hormones: effects on morphine-induced accumbens dopamine release, reward, and locomotor behavior in male and female rats. Front Pharm. 2019;10:295–295. doi: 10.3389/fphar.2019.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Becker JB, Hu M. Sex differences in drug abuse. Front Neuroendocrinol. 2008;29:36–47. doi: 10.1016/j.yfrne.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ettenberg A, Pettit HO, Bloom FE, Koob GF. Heroin and cocaine intravenous self-administration in rats: Mediation by separate neural systems. Psychopharmacology. 1982;78:204–9. doi: 10.1007/BF00428151. [DOI] [PubMed] [Google Scholar]
- 28.Gerrits MAFM, Ramsey NF, Wolterink G, van Ree JM. Lack of evidence for an involvement of nucleus accumbens dopamine D1 receptors in the initiation of heroin self-administration in the rat. Psychopharmacology. 1994;114:486–94. doi: 10.1007/BF02249340. [DOI] [PubMed] [Google Scholar]
- 29.Van Ree JM, Ramsey N. The dopamine hypothesis of opiate reward challenged. Eur J Pharmacol. 1987;134:239–43. doi: 10.1016/0014-2999(87)90172-5. [DOI] [PubMed] [Google Scholar]
- 30.Corre, J et al. Dopamine neurons projecting to medial shell of the nucleus accumbens drive heroin reinforcement. Elife. 2018;7. 10.7554/eLife.39945 [DOI] [PMC free article] [PubMed]
- 31.Wei C, et al. Response dynamics of midbrain dopamine neurons and serotonin neurons to heroin, nicotine, cocaine, and MDMA. Cell Discov. 2018;4:60. doi: 10.1038/s41421-018-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fields HL, Margolis EB. Understanding opioid reward. Trends Neurosci. 2015;38:217–25. doi: 10.1016/j.tins.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y, Morgan D, Roberts DC. Cross-sensitization of the reinforcing effects of cocaine and amphetamine in rats. Psychopharmacology. 2007;195:369–75. doi: 10.1007/s00213-007-0909-6. [DOI] [PubMed] [Google Scholar]
- 34.Zhang F, et al. Motivation of heroin-seeking elicited by drug-associated cues is related to total amount of heroin exposure during self-administration in rats. Pharmacol Biochem Behav. 2004;79:291–8. doi: 10.1016/j.pbb.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 35.Wee S, Specio SE, Koob GF. Effects of dose and session duration on cocaine self-administration in rats. J Pharm Exp Ther. 2007;320:1134–43. doi: 10.1124/jpet.106.113340. [DOI] [PubMed] [Google Scholar]
- 36.Ahmed SH, Koob GF. Transition from moderate to excessive drug intake: change in hedonic set point. Science. 1998;282:298–300. doi: 10.1126/science.282.5387.298. [DOI] [PubMed] [Google Scholar]
- 37.Roth ME, Carroll ME. Sex differences in the escalation of intravenous cocaine intake following long- or short-access to cocaine self-administration. Pharm Biochem Behav. 2004;78:199–207. doi: 10.1016/j.pbb.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 38.Lacy RT, Strickland JC, Feinstein MA, Robinson AM, Smith MA. The effects of sex, estrous cycle, and social contact on cocaine and heroin self-administration in rats. Psychopharmacology. 2016;233:3201–10. doi: 10.1007/s00213-016-4368-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yorgason JT, España RA, Jones SR. Demon voltammetry and analysis software: analysis of cocaine-induced alterations in dopamine signaling using multiple kinetic measures. J Neurosci Methods. 2011;202:158–64. doi: 10.1016/j.jneumeth.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edwards S, Koob GF. Escalation of drug self-administration as a hallmark of persistent addiction liability. Behav Pharm. 2013;24:356–62. doi: 10.1097/FBP.0b013e3283644d15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahmed SH, Walker JR, Koob GF. Persistent increase in the motivation to take heroin in rats with a history of drug escalation. Neuropsychopharmacology. 2000;22:413–21. doi: 10.1016/s0893-133x(99)00133-5. [DOI] [PubMed] [Google Scholar]
- 42.McNamara R, Dalley JW, Robbins TW, Everitt BJ, Belin D. Trait-like impulsivity does not predict escalation of heroin self-administration in the rat. Psychopharmacology. 2010;212:453–64. doi: 10.1007/s00213-010-1974-9. [DOI] [PubMed] [Google Scholar]
- 43.Wanat MJ, Willuhn I, Clark JJ, Phillips PE. Phasic dopamine release in appetitive behaviors and drug addiction. Curr Drug Abus Rev. 2009;2:195–213. doi: 10.2174/1874473710902020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Floresco SB, West AR, Ash B, Moore H, Grace AA. Afferent modulation of dopamine neuron firing differentially regulates tonic and phasic dopamine transmission. Nat Neurosci. 2003;6:968–73. doi: 10.1038/nn1103. [DOI] [PubMed] [Google Scholar]
- 45.Borland LM, Michael AC. Voltammetric study of the control of striatal dopamine release by glutamate. J Neurochem. 2004;91:220–9. doi: 10.1111/j.1471-4159.2004.02708.x. [DOI] [PubMed] [Google Scholar]
- 46.Campbell UC, Carroll ME. Acquisition of drug self-administration: environmental and pharmacological interventions. Exp Clin Psychopharmacol. 2000;8:312–25. doi: 10.1037//1064-1297.8.3.312. [DOI] [PubMed] [Google Scholar]
- 47.Piazza PV, Deroche-Gamonent V, Rouge-Pont F, Le Moal M. Vertical shifts in self-administration dose-response functions predict a drug-vulnerable phenotype predisposed to addiction. J Neurosci. 2000;20:4226–32. doi: 10.1523/jneurosci.20-11-04226.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Becker JB. Sex differences in addiction. Dialogues Clin Neurosci. 2016;18:395–402. doi: 10.31887/DCNS.2016.18.4/jbecker. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Becker JB, Perry AN, Westenbroek C. Sex differences in the neural mechanisms mediating addiction: a new synthesis and hypothesis. Biol Sex Differ. 2012;3:14–14. doi: 10.1186/2042-6410-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson NR, Roberts DC. Progressive ratio schedules in drug self-administration studies in rats: a method to evaluate reinforcing efficacy. J Neurosci Methods. 1996;66:1–11. doi: 10.1016/0165-0270(95)00153-0. [DOI] [PubMed] [Google Scholar]
- 51.Yu J, et al. Gender and stimulus difference in cue-induced responses in abstinent heroin users. Pharmacol Biochem Behav. 2007;86:485–92. doi: 10.1016/j.pbb.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 52.Caprioli D, et al. Opposite environmental regulation of heroin and amphetamine self-administration in the rat. Psychopharmacology. 2008;198:395–404. doi: 10.1007/s00213-008-1154-3. [DOI] [PubMed] [Google Scholar]
- 53.Vendruscolo LF, et al. Escalation patterns of varying periods of heroin access. Pharmacol, Biochem, Behav. 2011;98:570–4. doi: 10.1016/j.pbb.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Craft RM. Sex differences in analgesic, reinforcing, discriminative, and motoric effects of opioids. Exp Clin Psychopharmacol. 2008;16:376–85. doi: 10.1037/a0012931. [DOI] [PubMed] [Google Scholar]
- 55.Williams JT, et al. Regulation of μ-opioid receptors: desensitization, phosphorylation, internalization, and tolerance. Pharm Rev. 2013;65:223–54. doi: 10.1124/pr.112.005942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mazei-Robison MS, et al. Role for mTOR signaling and neuronal activity in morphine-induced adaptations in ventral tegmental area dopamine neurons. Neuron. 2011;72:977–90. doi: 10.1016/j.neuron.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sim-Selley LJ, Selley DE, Vogt LJ, Childers SR, Martin TJ. Chronic heroin self-administration desensitizes mu opioid receptor-activated G-proteins in specific regions of rat brain. J Neurosci. 2000;20:4555–62. doi: 10.1523/jneurosci.20-12-04555.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weber RJ, Gomez-Flores R, Smith JE, Martin TJ. Neuronal adaptations, neuroendocrine and immune correlates of heroin self-administration. Brain Behav Immun. 2009;23:993–1002. doi: 10.1016/j.bbi.2009.05.057. [DOI] [PubMed] [Google Scholar]
- 59.Fattore L, et al. Bidirectional regulation of mu-opioid and CB1-cannabinoid receptor in rats self-administering heroin or WIN 55,212-2. Eur J Neurosci. 2007;25:2191–2200. doi: 10.1111/j.1460-9568.2007.05470.x. [DOI] [PubMed] [Google Scholar]
- 60.Steffensen SC, et al. Contingent and non-contingent effects of heroin on mu-opioid receptor-containing ventral tegmental area GABA neurons. Exp Neurol. 2006;202:139–51. doi: 10.1016/j.expneurol.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 61.Mateo Y, Lack CM, Morgan D, Roberts DCS, Jones SR. Reduced dopamine terminal function and insensitivity to cocaine following cocaine binge self-administration and deprivation. Neuropsychopharmacology. 2005;30:1455–63. doi: 10.1038/sj.npp.1300687. [DOI] [PubMed] [Google Scholar]
- 62.Ferris MJ, Mateo Y, Roberts DC, Jones SR. Cocaine-insensitive dopamine transporters with intact substrate transport produced by self-administration. Biol Psychiatry. 2011;69:201–7. doi: 10.1016/j.biopsych.2010.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ferris MJ, et al. Cocaine self-administration produces pharmacodynamic tolerance: differential effects on the potency of dopamine transporter blockers, releasers, and methylphenidate. Neuropsychopharmacology. 2012;37:1708–16. doi: 10.1038/npp.2012.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Calipari ES, et al. Methylphenidate and cocaine self-administration produce distinct dopamine terminal alterations. Addict Biol. 2014;19:145–55. doi: 10.1111/j.1369-1600.2012.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Calipari ES, Beveridge TJR, Jones SR, Porrino LJ. Withdrawal from extended-access cocaine self-administration results in dysregulated functional activity and altered locomotor activity in rats. Eur J Neurosci. 2013;38:3749–57. doi: 10.1111/ejn.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Horvath MC, et al. Heroin abuse is characterized by discrete mesolimbic dopamine and opioid abnormalities and exaggerated nuclear receptor-related 1 transcriptional decline with age. J Neurosci. 2007;27:13371–5. doi: 10.1523/JNEUROSCI.2398-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu Y, et al. Dopamine transporter availability in heroin-dependent subjects and controls: longitudinal changes during abstinence and the effects of Jitai tablets treatment. Psychopharmacology. 2013;230:235–44. doi: 10.1007/s00213-013-3148-z. [DOI] [PubMed] [Google Scholar]
- 68.Yuan J, et al. Comparison of striatal dopamine transporter levels in chronic heroin-dependent and methamphetamine-dependent subjects. Addict Biol. 2017;22:229–34. doi: 10.1111/adb.12271. [DOI] [PubMed] [Google Scholar]
- 69.Karkhanis AN, Rose JH, Huggins KN, Konstantopoulos JK, Jones SR. Chronic intermittent ethanol exposure reduces presynaptic dopamine neurotransmission in the mouse nucleus accumbens. Drug Alcohol Depend. 2015;150:24–30. doi: 10.1016/j.drugalcdep.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Budygin EA, et al. Effects of chronic alcohol exposure on dopamine uptake in rat nucleus accumbens and caudate putamen. Psychopharmacology. 2007;193:495–501. doi: 10.1007/s00213-007-0812-1. [DOI] [PubMed] [Google Scholar]
- 71.Calipari ES, Ferris MJ, Salahpour A, Caron MG, Jones SR. Methylphenidate amplifies the potency and reinforcing effects of amphetamines by increasing dopamine transporter expression. Nat Commun. 2013;4:2720. doi: 10.1038/ncomms3720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Siciliano CA, et al. Amphetamine reverses escalated cocaine intake via restoration of dopamine transporter conformation. J Neurosci. 2018;38:484–97. doi: 10.1523/jneurosci.2604-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Siciliano CA, Calipari ES, Ferris MJ, Jones SR. Adaptations of presynaptic dopamine terminals induced by psychostimulant self-administration. ACS Chem Neurosci. 2015;6:27–36. doi: 10.1021/cn5002705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jones SR, Joseph JD, Barak LS, Caron MG, Wightman RM. Dopamine neuronal transport kinetics and effects of amphetamine. J Neurochem. 1999;73:2406–14. doi: 10.1046/j.1471-4159.1999.0732406.x. [DOI] [PubMed] [Google Scholar]
- 75.Parsons L, Smith A, Justice J., Jr Basal extracellular dopamine is decreased in the rat nucleus accumbens during abstinence from chronic cocaine. Synapse. 1991;9:60–65. doi: 10.1002/syn.890090109. [DOI] [PubMed] [Google Scholar]
- 76.Ng JP, Hubert GW, Justice JB., Jr Increased stimulated release and uptake of dopamine in nucleus accumbens after repeated cocaine administration as measured by in vivo voltammetry. J Neurochem. 1991;56:1485–92. doi: 10.1111/j.1471-4159.1991.tb02042.x. [DOI] [PubMed] [Google Scholar]
- 77.Grace AA. The tonic/phasic model of dopamine system regulation: its relevance for understanding how stimulant abuse can alter basal ganglia function. Drug Alcohol Depend. 1995;37:111–29. doi: 10.1016/0376-8716(94)01066-t. [DOI] [PubMed] [Google Scholar]
- 78.Siciliano CA, et al. Increased presynaptic regulation of dopamine neurotransmission in the nucleus accumbens core following chronic ethanol self-administration in female macaques. Psychopharmacology. 2016;233:1435–43. doi: 10.1007/s00213-016-4239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sulzer D. How addictive drugs disrupt presynaptic dopamine neurotransmission. Neuron. 2011;69:628–49. doi: 10.1016/j.neuron.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Koob GF. Theoretical frameworks and mechanistic aspects of alcohol addiction: alcohol addiction as a reward deficit disorder. Curr Top Behav Neurosci. 2013;13:3–30. doi: 10.1007/7854_2011_129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Melis M, Spiga S, Diana M. The dopamine hypothesis of drug addiction: hypodopaminergic state. Int Rev Neurobiol. 2005;63:101–54. doi: 10.1016/s0074-7742(05)63005-x. [DOI] [PubMed] [Google Scholar]
- 82.Diana M, Pistis M, Muntoni A, Gessa G. Profound decrease of mesolimbic dopaminergic neuronal activity in morphine withdrawn rats. J Pharm Exp Ther. 1995;272:781–5. [PubMed] [Google Scholar]
- 83.Diana M, Muntoni AL, Pistis M, Melis M, Gessa GL. Lasting reduction in mesolimbic dopamine neuronal activity after morphine withdrawal. Eur J Neurosci. 1999;11:1037–41. doi: 10.1046/j.1460-9568.1999.00488.x. [DOI] [PubMed] [Google Scholar]
- 84.Blum K, et al. Hatching the behavioral addiction egg: Reward Deficiency Solution System (RDSS)™ as a function of dopaminergic neurogenetics and brain functional connectivity linking all addictions under a common rubric. J Behav Addict. 2014;3:149–56. doi: 10.1556/JBA.3.2014.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hyland BI, Reynolds JN, Hay J, Perk CG, Miller R. Firing modes of midbrain dopamine cells in the freely moving rat. Neuroscience. 2002;114:475–92. doi: 10.1016/s0306-4522(02)00267-1. [DOI] [PubMed] [Google Scholar]
- 86.Zhang L, Doyon WM, Clark JJ, Phillips PEM, Dani JA. Controls of tonic and phasic dopamine transmission in the dorsal and ventral striatum. Mol Pharm. 2009;76:396–404. doi: 10.1124/mol.109.056317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Grace AA, Bunney BS. The control of firing pattern in nigral dopamine neurons: burst firing. J Neurosci. 1984;4:2877–90. doi: 10.1523/jneurosci.04-11-02877.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Phillips PE, Stamford JA. Differential recruitment of N-, P- and Q-type voltage-operated calcium channels in striatal dopamine release evoked by ‘regular’ and ‘burst’ firing. Brain Res. 2000;884:139–46. doi: 10.1016/s0006-8993(00)02958-9. [DOI] [PubMed] [Google Scholar]
- 89.Tobler PN, Fiorillo CD, Schultz W. Adaptive coding of reward value by dopamine neurons. Science. 2005;307:1642. doi: 10.1126/science.1105370. [DOI] [PubMed] [Google Scholar]
- 90.Cragg SJ. Variable dopamine release probability and short-term plasticity between functional domains of the primate striatum. J Neurosci. 2003;23:4378–85. doi: 10.1523/JNEUROSCI.23-10-04378.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Condon MD, et al. Plasticity in striatal dopamine release is governed by release-independent depression and the dopamine transporter. Nat Commun. 2019;10:4263. doi: 10.1038/s41467-019-12264-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Trovero F, Herve D, Desban M, Glowinski J, Tassin JP. Striatal opiate mu-receptors are not located on dopamine nerve endings in the rat. Neuroscience. 1990;39:313–21. doi: 10.1016/0306-4522(90)90270-e. [DOI] [PubMed] [Google Scholar]
- 93.Svingos AL, Colago EE, Pickel VM. Vesicular acetylcholine transporter in the rat nucleus accumbens shell: subcellular distribution and association with mu-opioid receptors. Synapse. 2001;40:184–92. doi: 10.1002/syn.1041. [DOI] [PubMed] [Google Scholar]
- 94.Cachope R, et al. Selective activation of cholinergic interneurons enhances accumbal phasic dopamine release: setting the tone for reward processing. Cell Rep. 2012;2:33–41. doi: 10.1016/j.celrep.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]