Abstract
Objective
Previous literature finds an increase in depressive symptoms, substance use, and suicidal ideation following the COVID-19 pandemic in the US – suicides do not appear to increase. We examine whether 1) state lockdown policies in the US precede an increase in mental health symptoms; and 2) the extent to which using substances amplifies or attenuates the relation.
Methods
We specified, as our exposure variable, the timing of state-level lockdown orders. We used, as the outcome variable, the 4-item Patient Health Questionnaire (PHQ-4) that measures anxiety and depression symptoms. We utilized the Understanding America Study (UAS), a nationally representative sample of 7,597 adults across 50 states in the US, surveyed biweekly between March 10, 2020 and November 11, 2020. Linear fixed effect analyses controlled for time-invariant individual factors, as well as employment status, household income, and previous mental health diagnosis.
Results
Regression results indicate an increase in PHQ-4 scores of approximately 1.70 during lockdown, relative to no lockdown (p < 0.05). Relative to no lockdown, an increase in alcohol use corresponds with a 0.08 unit decrease in PHQ-4 scores during lockdown (p < 0.05).
Conclusion
State lockdown policies precede greater mental health symptoms. Increases in consuming alcohol attenuates the relation between state lockdown policies and mental health symptoms. Results may portend greater addiction following the pandemic warranting further investigation into utilization of substance use treatment.
Keywords: Depression, Anxiety, Lockdown, COVID, Substance, Alcohol
1. Introduction
The COVID-19 pandemic spurred state lockdown policies and stay-at-home orders in 43 of the 50 states in the US (Moreland, 2020). Implemented between March and April 2020, these policies aimed to restrict community activities and decrease the spread of COVID-19 by reducing population movement and contact with persons outside of the home (Moreland, 2020). Concerns of economic strain and significant changes to daily life such as social isolation, possible virus contraction, losing a loved-one, and home-schooling children may have exacerbated feelings of uncertainty and fear (COVID-19 to Plunge Global Economy into Worst Recession since World War II, 2020). These factors have led scholars to speculate on the potential mental health consequences of viral outbreaks, such as COVID-19, as a ‘parallel pandemic.’ (Vigo et al., 2020).
Large, cross-sectional studies report an increase in depression, substance use, and suicidal ideation following the COVID-19 pandemic in the US (Czeisler et al., 2020, Ettman et al., 2020). However, overall suicide rates do not appear to rise in the US and even show a decrease in other countries (Czeisler et al., 2020, Differences and in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease, 2019, Radeloff et al., 2020, Tanaka and Okamoto, 2020). Concerns about the psychological fallout from the pandemic prompted urgent calls to examine the relation between mental health and substance use to better inform public policy, practice, and recommendations (Holmes et al., 2020).
Within the self-medication hypothesis of addictive disorders, substances may temporarily relieve painful feelings or control emotions when absent or confusing (Khantzian, 1997). The hypothesis complements other bio-genetic and sociocultural theories on the etiology of substance use disorders. It aims to address the emotional and psychological dimensions of addiction (Khantzian, 1997). The hypothesis posits that 1) substance abuse may relieve psychological suffering; and 2) individuals may prefer particular substances depending on their psychoactive properties (Khantzian, 1997).
The cross-sectional literature finds greater adverse mental health symptoms and substance use after state lockdown orders relative to before the order. A nationally representative study in the US, for instance, finds a three-fold increase in depressive symptoms (Ettman et al., 2020). Studies examining state lockdown policies report greater depressive symptoms following policy implementation (Adams-Prassl et al., 2021, Marroquín et al., 2020). Researchers also report greater alcohol consumption following adoption of social distancing mandates (Kim et al., 2020, McPhee et al., 2020, Pollard et al., 2020, The Lancet Gastroenterology & Hepatology, 2020, Wardell and Karli, 2020). Others report a positive association between psychological distress and substance use (Dawson and Golijani-Moghaddam, 2020, Rodriguez et al., 2020, Skapinakis et al., 2020).
The above work, while suggestive, has three key limitations. First, cross-sectional studies do not follow individuals over time and therefore cannot track the time course of symptoms and substance use behaviors among individuals who newly experience the lockdown. To the extent that survey respondents before and after the lockdown differ systematically in ways that affect mental health and substance use, serial cross-sectional surveys may suffer from selection bias. Cross-sectional work may also be confounded by fundamental differences, across states, in mental health resources and other structural factors that could affect mental health symptoms. Additionally, prior work cannot address the important policy question of whether state-level changes to lockdown policies precede changes in mental health symptoms. The above work ignores the fact that state lockdown policies have changed over time, including cases in which many states have since lifted their policies (Status of lockdown and stay-at-home orders. Ballotpedia, 2020).
Second, although some research focuses on consuming alcohol during COVID-19, literature on using different substances remains scarce. In addition to reports of increased alcohol consumption, cannabis sales increased dramatically at the beginning of the COVID-19 pandemic (McPhee et al., 2020, State of the Cannabis Industry, 2020, Wardell and Karli, 2020). Sales then stabilized at figures 40% higher than 2019 numbers (Sate of the Cannabis Industry, 2020). Previous literature has also grouped substance use with other avoidant or maladaptive behaviors – such as disengagement – masking their individual influence on mental health symptoms. Given that substance use can become addictive, (Is, 2020) examining them individually may uncover potential disorders that follow.
Third, previous research does not examine whether, and to what extent, substance use may amplify or attenuate the relation between COVID-19 related stressors and mental health symptoms. Scholars report increases in substance use and mental health following the state lockdown policies and a positive relation between psychological distress and substance use. However, substance use may affect the relation between stress and psychopathology. It may buffer the relation or destabilize psychological adjustment to stress.
We address these limitations and analyze whether 1) state lockdown policies in the US precede an increase in mental health symptoms; and 2) the extent to which using substances amplify or attenuate any discovered relation between state lockdown policies and mental health symptoms. We examine the Understanding America Study (UAS), a nationally representative sample of adults across 50 states in the US, surveyed biweekly (over 16 waves), between March 10, 2020 and November 11, 2020. Importantly, these individuals provide continual participation over a long study period, which permits a rigorous longitudinal analysis of the evolution of mental health symptoms and substance use behaviors. Results from our study may hold particular relevance to understanding how state lockdown policies and using substances relate to mental health symptoms in the US.
2. Methods
2.1. Study population
Our study comprised respondents from UAS, a probability-based Internet panel of adults in the US. The study drew respondents from the universe of US postal addresses and provided them with internet and/or a tablet, if necessary. Beginning March 10, the UAS issued its first longitudinal survey on COVID-19. UAS then issued subsequent rounds beginning April 1, 2020, and every two weeks thereafter, to the same panel of respondents. UAS compensated panel members $20 for their participation in 30-minute surveys (Understanding America Study, 2021). Additional details regarding methodology appear on the UAS website (Understanding America Study, 2021). We used data from 16 waves of the study between March 10, 2020 and November 11, 2020 from respondents across all 50 states in the US. Of the 7,962 panel members eligible for the survey, our analytic sample comprised 7,597 who provided complete data on the variables of interest (95% completeness).
3. Study measures
We used, as the mental health outcome variable, the 4-item Patient Health Questionnaire (PHQ-4) that measures anxiety and depression (Kroenke et al., 2009, Understanding America Study, 2021). The PHQ-4 asked respondents the number of days in the last two weeks in which they have mental health symptoms (Kroenke et al., 2009). The PHQ-4 total score is calculated across questions and ranges from 0 to 12, in which a higher score indicates more anxiety and depression (Kroenke et al., 2009). Researchers confirm the reliability and measurement validity of the PHQ-4 scale (Kroenke et al., 2009). Within the UAS dataset, the PHQ-4 has high internal consistency and scale reliability (Cronbach’s alpha = 0.910).
We specified, as our exposure variable, the timing and duration of state-level lockdown orders. We retrieved start and end dates for state lockdown and stay-at-home orders, issued by US state governors, from Ballotopedia (Status of lockdown and stay-at-home orders. Ballotpedia, 2020). Ballotopedia, a non-profit organization, provides information on American politics and elections as a digital encyclopedia. With a staff of 100 professional editors, writers, and researchers, Ballotopedia regularly updates articles as new information becomes available (Status of lockdown and stay-at-home orders, 2020). Ballotopedia provided official state lockdown orders outlining mandates and closures, issued by governors in 43 of the 50 states that enacted policies (Status of lockdown and stay-at-home orders. Ballotpedia, 2020). Mandates included information on closure of non-essential businesses, travel restrictions, and public health practices (IHME COVID-19 Forecasting Team, 2020, Status of lockdown and stay-at-home orders. Ballotpedia, 2020). Previous literature also uses these data, thus supporting reliability (Kettl, 2020, McCannon, 2020). We linked these data to the UAS based on whether respondents completed waves of the survey when their state enacted lockdown policies or not. We specified a binary indicator for whether respondents completed each of the 16 surveys during their own state’s lockdown policy or not (binary indicator; 0 = no lockdown; 1 = during lockdown). We categorized respondents in the seven states that did not implement lockdown policies (Arkansas, Iowa, Nebraska, North Dakota, South Dakota, Utah, and Wyoming) as ‘0′ for the entire study period.
We obtained data on substance use from survey questions on the UAS (Understanding America Study, 2021). We measured using alcohol, cannabis, and other recreational drugs with the following question: Out of the past 7 days, what is your best estimate of the number of days that you did each of the following activities? (Understanding America Study, 2021) Responses included 0–7 days for 1) consumed alcohol; 2) used cannabis products such as marijuana; and 3) used recreational drugs other than alcohol or cannabis products (Understanding America Study, 2021).
3.1. Statistical analysis
We first tested whether mental health symptoms increase following state lockdown policies. We used Ordinary Least Squares (OLS) regression with individual-level fixed effects specification to examine whether state lockdown policies correspond with mental health symptoms. Results from the Durbin-Wu-Hausman hypothesis test, commonly used to decide between fixed or random effects analyses in panel data, support the use of a fixed effects model. Our individual-level fixed effects analytic strategy exploits the longitudinal “repeated measures” nature of the survey and compares mental health over time, within the same individual. This approach controls for time-invariant attributes that may correspond with mental health symptoms. Individual features such as preference for help-seeking, and sociodemographic attributes that do not vary over time are controlled using individual fixed-effects (Wooldridge, 2012). This strategy limits confounding from unobserved stable attributes that may influence mental health outcomes after COVID-19. We clustered standard errors by state to account for confounding that may arise from non-independence of individuals within states. Clustered standard errors, also known as the Liang-Zeger standard errors, corrects for possible correlation in modeling residuals.
Employment status and household income that changes over time, within an individual, may confound our analysis in that unemployment and economic strain may worsen mental health symptoms (Goldman-Mellor et al., 2010). To control for this possibility, we utilized questions from the UAS regarding employment status and household income as control variables in our analysis. Additionally, we control for previous mental health diagnosis as that may influence mental health symptomology. We include indicators for month to control for month-specific factors (e.g., seasonality), or exogenous events, such as the George Floyd protests, which may also influence mental health symptoms. As a sensitivity analysis, we estimated whether lockdown corresponded with mental health symptoms after adjusting for outliers. We included PHQ-4 scores within the 5th and 95th percentile for this analysis. We also conduct an exploration of whether duration of lockdown (in weeks), among states that enacted lockdown policies, corresponds with greater mental health symptoms to assess a ‘dose-response’ relationship.
Second, we examined whether using substances (drinking alcohol, using cannabis products, or using recreational drugs) amplifies or attenuates any relation between state lockdown policies and mental health symptoms (separately for each substance). We used the same individual fixed-effects specification as described above, but now added an interaction term (using substances*lockdown policy), on the additive scale, as the key variable to examine the interaction (Knol et al., 2007). This interaction term permits estimation of whether any relation between lockdown levels (i.e., lockdown, no lockdown) and PHQ-4 scores varies depending on the level of substance use. It also measures whether using substances strengthens or changes the relation between state lockdown policies and mental health symptoms. Third, we stratified analyses by heavy and non-heavy drinking to examine whether any relation between lockdown levels and PHQ-4 scores varies depending on the level of alcohol use. We removed all individuals who did not consume alcohol for this analysis.
For all analyses, we used robust standard errors to adjust for heteroscedasticity in residuals and clustered standard errors by state. We performed all analyses using Stata SE version 16.0. The University of California, Irvine, Institutional Review Board deemed this study exempt owing to the use of publicly available, de-identified data.
4. Results
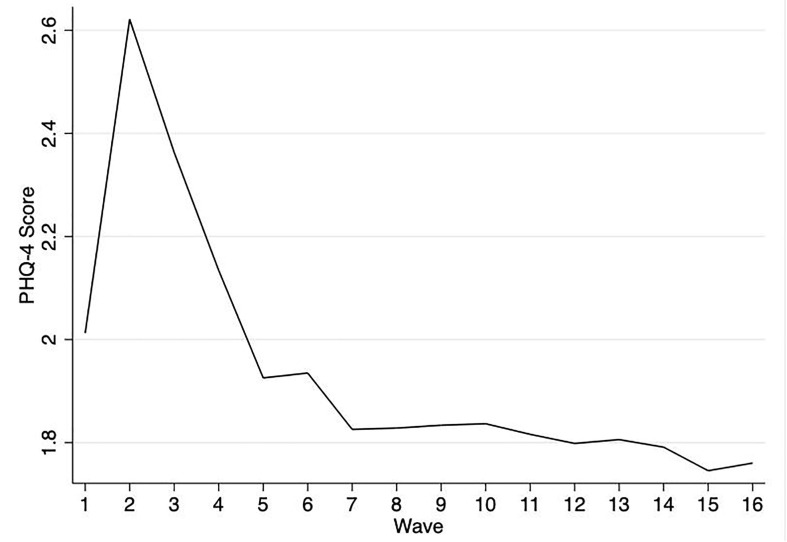
Over the study period, 7,597 respondents participated for the full 16 waves. These respondents reflect the age, gender, racial/ethnic, and socioeconomic diversity of adults in the US (Table 1 ). PHQ-4 scores among survey respondents average 1.94 across 16 waves of the survey (Table 1). Fig. 1 shows average PHQ-4 scores from respondents across each wave of the survey. Scores initially increase after Wave 1 (i.e., greater reported anxiety and/or depression), but steadily decline in the subsequent waves. This general pattern indicates an acute rise in mental health symptoms in late March and an abrupt drop immediately thereafter, to the month of June.
Table 1.
Sociodemographic characteristics and descriptive statistics among 7,597 respondents, over 16 waves of the Understanding America Study, March 10-November 11, 2020.
| Variable | |
|---|---|
| Sociodemographic characteristics | |
| Age (years) | |
| 18–34 | 18.13% |
| 35–44 | 19.45% |
| 45–54 | 18.28% |
| 55–64 | 20.71% |
| 65+ | 23.43% |
| Gender (%) | |
| Male | 41.55% |
| Female | 58.45% |
| Race (%) | |
| Whitea | 66.81% |
| Blacka | 7.58% |
| Hispanic | 15.16% |
| Othera, b | 10.45% |
| Highest Education (%) | |
| Below 12th grade | 4.83% |
| High school diploma | 38.83% |
| Associate’s degree/vocational | 14.32% |
| Bachelor’s degree | 24.73% |
| Graduate degree | 17.29% |
| Study measures | Mean (SD) |
| PHQ-4 Score (0–12) | 1.94 (2.82) |
| Days in the last week consumed alcohol | 1.46 (2.14) |
| Days in the last week used cannabis product | 0.51 (1.64) |
| Days in the last week used recreational drugs other than alcohol and cannabis | 0.12 (0.79) |
Non-Hispanic.
Other includes American Indian/Alaska Native, Asian, Hawaiian/Pacific Islander, and Mixed races.
Fig. 1.
Patient Health Questionnaire-4 (PHQ-4) scores among 7,597 respondents, over 16 survey waves, March 10-November 11, 2020.
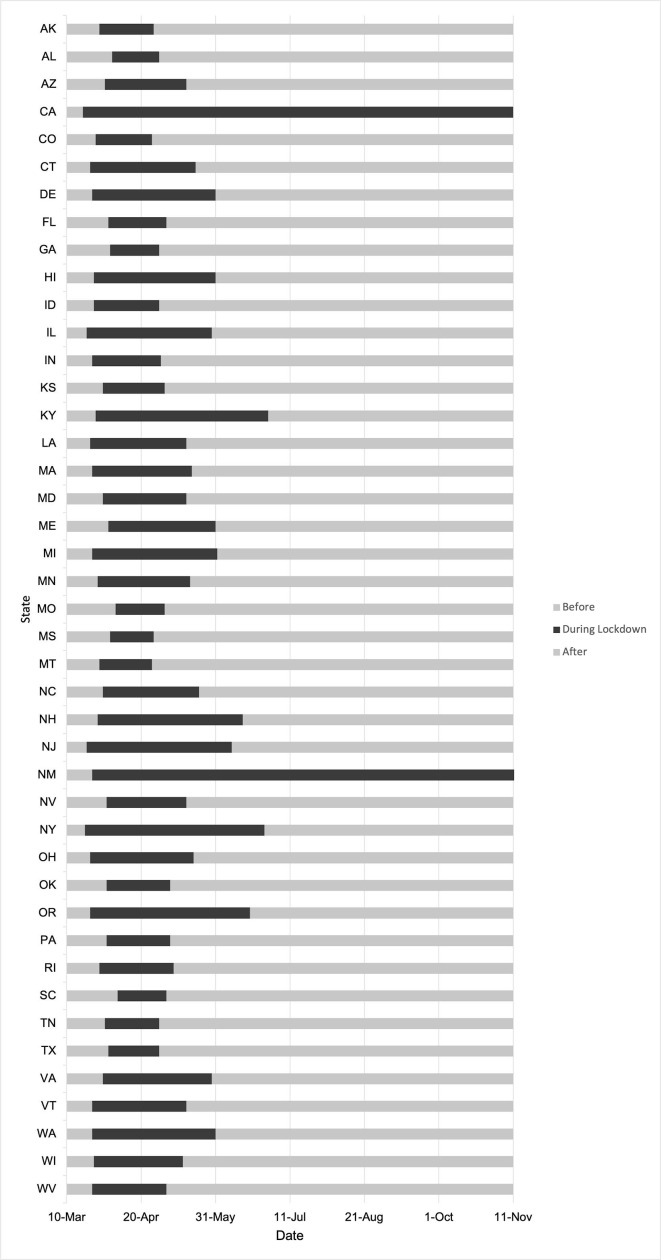
States enacted and lifted lockdown policies at various times (Fig. 2 ). New York and California, for instance, enacted policies relatively early. Texas and Georgia enacted policies later, and the duration of lockdown policies in these two states lasted less than one month. This variation in initiation and termination of lockdown policies provides important spatial–temporal variation in exposure across UAS participants.
Fig. 2.
Timeline of lockdown policy enactment in 43a of the 50 US states during the study period, March 10-November 11, 2020.
aSeven states that did not enact lockdown policies (AR, IA, ND, NE, SD, UT, WY) not included in figure.
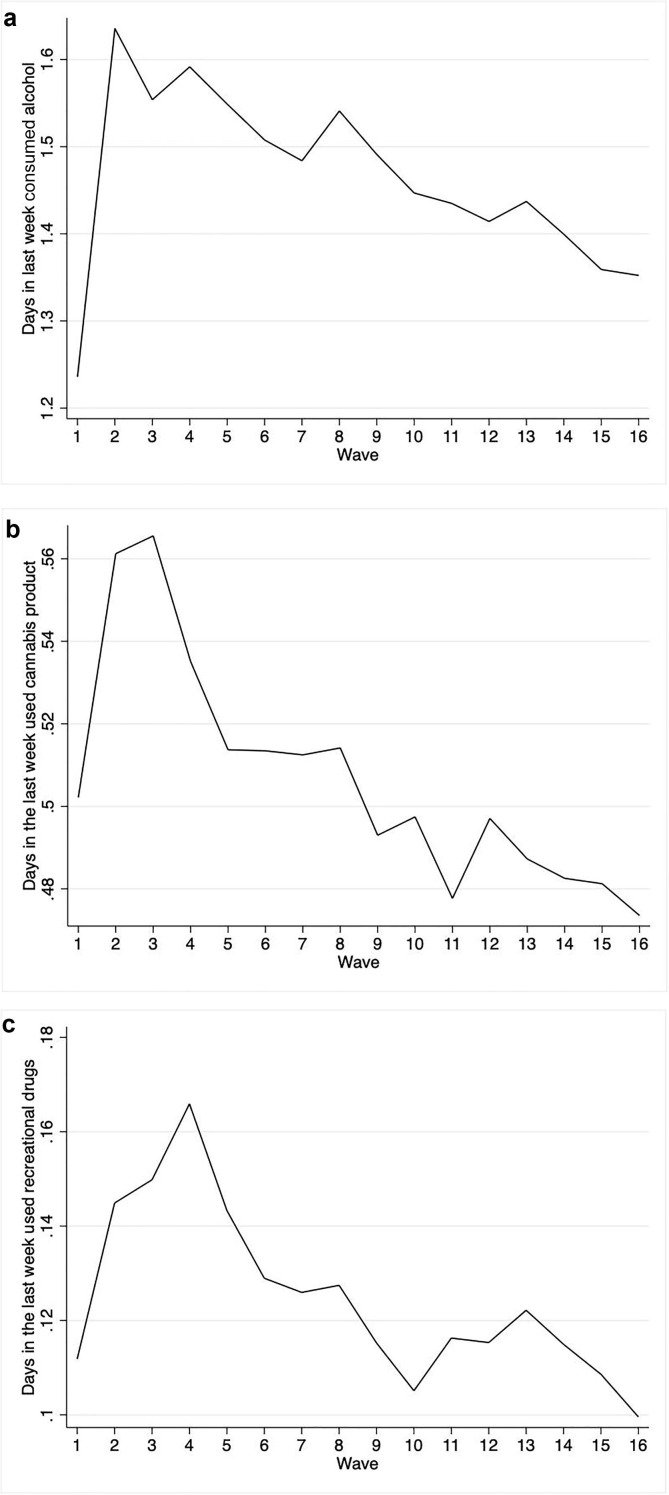
Respondents averaged 1.46 days consuming alcohol, 0.51 days using cannabis products, and 0.12 days using recreational drugs in the past week. Consuming alcohol, cannabis, and recreational drugs initially increases after Wave 1 and declines in later waves (Fig. 3 ).
Fig. 3.
Days in the last week consuming alcohol, using cannabis products, and using recreational drugs (other than alcohol or cannabis) among 7,597 respondents, over 16 survey waves, March 10-November 11, 2020.
Table 2 presents results from OLS fixed effects regression analyses predicting PHQ-4 scores as a function of state lockdown policies. Regression results indicate an increase in PHQ-4 scores of approximately 1.70 during lockdown as opposed to not during lockdown (p < 0.05). This finding indicates that on a scale of 0–12, PHQ-4 scores increase by 1.70 during lockdown as opposed to no lockdown.
Table 2.
Linear fixed effects regression results predicting PHQ-4 score as a function of state lockdown policies among 7,597 respondents, over 16 survey waves, March 10-November 11, 2020.
| Covariatesa | Coefficient | 95% CIb |
|---|---|---|
| Lockdown policy (reference: No lockdown) | ||
| During lockdown | 1.695** | (0.116,3.275) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.257**** | (0.133,0.380) |
| 25 k-50 k | 0.564**** | (0.345,0.782) |
| <25 k | 0.922**** | (0.724,1.120) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.024 | (−0.156,0.108) |
| Previous Mental Health Diagnosis (reference: No) | ||
| Diagnosis | 2.590**** | (2.338,2.844) |
| N | 7,597 | |
*p < 0.1; **p < 0.05; *** p < 0.01; **** p < 0.001.
Time invariant individual and month fixed effects included but not shown.
Robust standard errors.
For a sensitivity analysis, we tested our model after removing outliers of PHQ-4 scores below the 5th percentile and above the 95th percentile. We find increases in PHQ-4 scores of 1.20 during lockdown as opposed to no lockdown following outlier adjustment (Appendix, Table A1). We also find attenuation for each category of household income and previous mental health diagnosis (Appendix, Table A1). These results indicate that very high or very low PHQ scores may have driven a portion of the overall effect size of the lockdown coefficient and that of the covariates reported in Table 2.
As an exploration, we measure whether greater duration of lockdown (in weeks) corresponds with increased mental health symptoms. Among individuals living in states that enacted lockdown policies, we find no relation between duration of lockdown (in weeks) and PHQ-4 scores (Appendix, Table A2).
Table 3 (Models A-C) shows results predicting PHQ-4 scores as a function of the interaction between lockdown policies and consuming alcohol (Model A), cannabis products (Model B), and recreational drugs (Model C). Relative to before lockdown, increase in alcohol use corresponds with a 0.08 unit decrease in PHQ-4 scores during lockdown as opposed to no lockdown. This finding indicates that consuming alcohol slightly attenuates the relation between state lockdown policies and mental health symptoms. Although we fail to reject the null for cannabis and recreational drugs, the positive effect sizes indicate that cannabis and recreational drugs amplifies the relation between state lockdown policies and mental health symptoms (Table 3, Model B and C).
Table 3.
Linear fixed effects regression results predicting PHQ-4 score as a function of the interaction of lockdown policies and using substances (consuming alcohol, using cannabis products, and using recreational drugs) among 7,597 respondents, over 16 survey waves, March 10-November 11, 2020.
| Covariatesa | Coefficient | 95% CIb |
|---|---|---|
| Model A - Alcohol | ||
| Lockdown Policy*Consuming Alcohol | ||
| During | −0.078** | (−0.150, −0.006) |
| Lockdown Policy (at Consuming Alcohol = 0) | ||
| During | 1.748** | (0.185,3.311) |
| Consuming Alcohol (at Lockdown Policy = 0) | 0.102*** | (0.031,0.173) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.273**** | (0.150,0.397) |
| 25 k-50 k | 0.589**** | (0.373,0.805) |
| <25 k | 0.957**** | (0.759,1.155) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.028 | (−0.160,0.104) |
| Previous Mental Health Diagnosis (reference: None) | ||
| Diagnosis | 2.596**** | (2.340,2.853) |
| N | 7,597 | |
| Model B - Cannabis | ||
| Lockdown Policy*Using Cannabis | ||
| During | 0.047 | (−0.077,0.170) |
| Lockdown Policy (at Using Cannabis = 0) | ||
| During | 1.626** | (0.250,3.001) |
| Using Cannabis (at Lockdown Policy = 0) | 0.0795 | (−0.0408,0.200) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.244**** | (0.127,0.361) |
| 25 k-50 k | 0.533**** | (0.310,0.755) |
| <25 k | 0.856**** | (0.657,1.055) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.020 | (−0.154,0.113) |
| Previous Mental Health Diagnosis (reference: None) | ||
| Diagnosis | 2.533**** | (2.282,2.784) |
| N | 7,597 | |
| Model C – Recreational Drugs | ||
| Lockdown Policy*Using Recreational Drugs | ||
| During | 0.197 | (−0.150,0.190) |
| Lockdown Policy (at Using Recreational Drugs = 0) | ||
| During | 1.609** | (0.175,3.042) |
| Using Recreational Drugs (at Lockdown Policy = 0) | 0.292*** | (0.132,0.452) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.252**** | (0.130,0.373) |
| 25 k-50 k | 0.540**** | (0.319,0.760) |
| <25 k | 0.861**** | (0.663,1.060) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.019 | (−0.150,0.113) |
| Previous Mental Health Diagnosis (reference: None) | ||
| Diagnosis | 2.583**** | (2.329,2.836) |
| N | 7,597 | |
*p < 0.1; **p < 0.05; *** p < 0.01; **** p < 0.001.
Time-invariant individual and month fixed effects included but not shown.
Robust standard errors.
We then stratified our analyses by heavy and non-heavy alcohol use to gauge whether the “buffering” role of alcohol use during the lockdown varies by the severity of alcohol consumption (Appendix, Table A3). Results suggest that the overall relation between PHQ-4 scores and the lockdown by level of alcohol consumption concentrates among non-heavy alcohol drinkers (Appendix, Table A3).
5. Discussion
State governors issued COVID-19 related lockdown policies in 43 of the 50 states in the US. These policies likely spurred substantial lifestyle changes and economic uncertainty for many. Using substances may relieve painful emotions or exacerbate mental disorder. In this study, we examined 1) whether state lockdown policies preceded increases in mental health symptoms; and 2) the extent to which any relation between state lockdown policies and mental health symptoms varied by the level of substance use. We find that state lockdown policies correspond with an increase in PHQ-4 scores after the lockdown. Our results also indicate that consuming alcohol attenuated this relation. Alcohol consumption offers a very modest but statistically detectable ‘protective effect’ in that increase in frequency of alcohol consumption corresponds with fewer anxiety and depressive symptoms (i.e., lower PHQ-4 score).
The self-medication hypothesis of addictive behaviors offers a plausible explanation for this finding (Khantzian, 1997). Individuals may consume alcohol as a means of regulating negative emotions. This notion is further supported by the observation that the main detectable association concentrates among non-heavy drinkers. We caution against the interpretation that promotion of alcohol use may reduce anxiety and depressive symptoms. Rather, our findings indicate that individuals may consume alcohol to modestly regulate negative mood during state lockdown restrictions. We also note that our analyses describe relatively short-term relations (from March to November 2020) between alcohol consumption and mental health symptoms. These relations may change following prolonged exposure to the underlying stressor (Zeidner & Saklofske, 1996). Additionally, our findings reflect mental health responses to lockdown policies that also appear in other countries such as Italy, United Kingdom, and Austria (Meda et al., 2021, Pieh et al., 2021, Pierce et al., 2020). Studies conducted in these countries report greater adverse mental health during lockdown restrictions, as opposed to before or after lockdown (Meda et al., 2021, Pieh et al., 2021, Pierce et al., 2020).
Similarly, studies on COVID-19 lockdown policies in the US also report a modest increase in mental health symptoms. One population-representative study finds a 0.085 standard deviation increase in adverse mental health following lockdown orders, particularly among women (Adams-Prassl et al., 2021). Another study reports a minimal increase in depressive, rather than anxiety, symptoms among college students following Stay-At-Home Orders in Louisiana (Buckner et al., 2021).
Although our study finds no significant differences in whether cannabis and recreational drugs moderate the relation between lockdown policies and mental health symptoms, the positive effect size indicates the potential for amplifying the relation. Previous studies, however, find conflicting results as to whether cannabis use precedes mental health symptoms (Danielsson et al., 2016, Lev-Ran et al., 2014). Our study also indicates that alcohol use modestly attenuates the relation between state lockdown policies and mental health symptoms, specifically among non-heavy drinkers. Prior works also finds that light- or moderate- alcohol users had fewer depressive symptoms in the presence of stress, suggesting that alcohol either attenuated the effect of stress on depression or suppressed the influence of the stressor (Lipton, 1994). Future work may benefit from better understanding differences based on the type of stressors.
Strengths of our study include the use of a nationally representative panel of respondents spanning all 50 states in the US. The longitudinal nature of the data allows for measurement of within-individual changes over time. This study design notably departs from previous COVID-19 and mental health literature which compares different adults over time or provides cross-sectional information. Our analysis, by contrast, controls for selection bias due to individual differences in sampling and measures the evolution of health behaviors of the same individuals during the study period. The analysis also controls for confounding by trend, place, and time. Methods further control for time-varying factors such as household income and employment status, which may influence mental health symptoms. Taken together, our use of high-quality population-based data, longitudinal study design, and fixed effects analytic approach offer strong internal validity.
Limitations include that UAS questions regarding substance use do not specifically capture motive. This would allow for a better understanding of whether individuals use substances for coping, interpersonal conflict, or fewer alternative activities. In addition, substantial macrosocial shocks may provoke or uncover psychiatric conditions by development of new disorders or exacerbation of pre-existing disorders (Catalano & Dooley, 1977). We have controlled for previous mental health diagnosis in our analyses, but cannot differentiate between types of psychiatric diagnosis. Clinic-based studies with detailed medical history information, therefore, would complement population-representative surveys such as the UAS. We encourage such future research if and when more detailed and complete patient-level data become available.
Additionally, our study cannot account for social ties (i.e., friends, family members) that may also influence mental health symptoms during state lockdown restrictions (Kawachi & Berkman, 2001). Further research would benefit from evaluation of how social ties may have influenced substance use and mental health. Although we utilized rigorous methods (i.e., longitudinal data and fixed effects regression analysis), our data do not allow us to rule out the possibility that social networks may have partially accounted for the protective relation between alcohol use and adverse mental health following state lockdown restrictions.
Increased mental health symptoms following lockdown and the attenuation of symptoms consuming alcohol may portend greater addiction following the pandemic (Khantzian, 1997). Although we fail to reject the null for cannabis and recreational drugs, the increase in cannabis sales and opioid-related emergency room visits observed in other studies may contribute to greater substance use disorder (Rodda et al., 2020, State of the Cannabis Industry, 2020). The Affordable Care Act expanded treatment for substance use disorders through insurance coverage, enhanced parity, and opportunities to integrate primary care and psychiatric treatment (Abraham et al., 2017). In addition, rapid expansion of mental health and substance use treatment in Community Health Centers may also have provided low-cost and free care to medically underserved communities most affected by economic hardship (Bruckner et al., 2019). However, punitive drug policies in the US have played a role in the incarceration, rather than treatment, of those with substance use disorders – especially in minority communities (Western & Wildeman, 2009). As the policy landscape changes to include legalized medical and recreational marijuana, (Laws, 2020) this shift may allow for use of expanded substance disorder treatment following the Affordable Care Act. The role of these policies and changes in the federal healthcare landscape warrants further research.
Whereas our study focuses on lockdown policies during COVID-19, examination of specific indicators such as local or regional unemployment rates may help uncover contributing factors that exacerbate mental disorder and/or using substances. In November 2020, unemployment in the US reached 10.7 million (Economic News Releases : U.S. Bureau of Labor Statistics, 2020). With additional economic uncertainty as COVID-19 cases rise and states implement further mandates, unemployment may precede increases in adverse mental health symptoms and suicidal behavior. Literature on this topic forecasts that a 5.7% worldwide unemployment rate would precede a predicted increase in>9000 suicides, globally (Kawohl & Nordt, 2020). This forecast, however, should be reconciled with the somewhat counterintuitive results of fewer (or no change in) suicides than expected following the COVID-19 pandemic (Differences and in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease, 2019, Radeloff et al., 2020, Tanaka and Okamoto, 2020), as well as acute decreases in opioid-related ED visits following economic downturns (Trinh et al., 2021). Examination of potential psychiatric and substance use sequelae of the COVID-19 recession, as well as development of theory regarding collective responses to large societal shifts, need further investigation.
6. Funding
National Institute of Mental Health (1R21MH110815-01A1).
7. Ethics Approval
The University of California, Irvine, institutional review board deemed this study exempt owing to the use of publicly available, deidentified data.
8. Data Availability
The dataset used for the analysis and the statistical code is available from the corresponding author. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
CRediT authorship contribution statement
Abhery Das: Conceptualization, Methodology, Software, Formal analysis, Resources, Data curation, Writing – original draft, Project administration. Parvati Singh: Methodology, Software, Validation, Writing - review & editing, Visualization, Supervision. Tim A. Bruckner: Conceptualization, Methodology, Validation, Visualization, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A
Table A1.
Linear fixed effects regression results (adjusting for outliers) predicting PHQ-4 score as a function of state lockdown policies among 7,501 respondents over 16 survey waves, March 10-November 11, 2020.
| Covariatesa | Coefficient | 95% CIb |
|---|---|---|
| Lockdown policy (reference: No lockdown) | ||
| During lockdown | 1.20** | (0.220,2.178) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.161*** | (0.070,0.252) |
| 25 k-50 k | 0.377**** | (0.243,0.511) |
| <25 k | 0.535**** | (0.408,0.663) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.040 | (−0.132,0.052) |
| Previous Mental Health Diagnosis (reference: None) | ||
| Diagnosis | 1.69**** | (1.497,1.884) |
| N | 7,501 | |
*p < 0.1; **p < 0.05; *** p < 0.01; **** p < 0.001.
Time-invariant individual and month fixed effects included but not shown.
Robust standard errors.
Table A2.
Linear fixed effects regression results predicting PHQ-4 score as a function of duration of state lockdown policies among 7,208 respondents (from 43 states) over 16 survey waves, March 10-November 11, 2020.
| Covariatesa | Coefficient | 95% CIb |
|---|---|---|
| Duration (in weeks) | −0.0006 | (−0.004,0.003) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | 0.261**** | (0.134,0.389) |
| 25 k-50 k | 0.563**** | (0.332,0.793) |
| <25 k | 0.928**** | (0.722,1.132) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.038 | (−0.169,0.093) |
| Mental Health Diagnosis (reference: None) | ||
| Diagnosis | 2.57**** | (2.334,2.808) |
| N | 7,208 | |
*p < 0.1; **p < 0.05; *** p < 0.01; **** p < 0.001.
Time-invariant individual and month fixed effects included but not shown.
Robust standard errors.
Table A3.
Linear fixed effects regression results predicting PHQ-4 score as a function of the interaction of lockdown policies and using substances (non-heavy and heavy drinking) among 7,597 respondents, over 16 survey waves, March 10-November 11, 2020.
| Covariatesa | Coefficient | 95% CIb |
|---|---|---|
| Model A – Non-Heavy Drinking | ||
| Lockdown Policy*Consuming Alcohol | ||
| During | −0.080** | (−0.158, −0.002) |
| Lockdown Policy (at Consuming Alcohol = 0) | ||
| During | −0.271 | (−0.885,0.343) |
| Consuming Alcohol (at Lockdown Policy = 0) | 0.085** | (0.012,0.159) |
| Household Income (reference: >100 k) | ||
| 50 k-100 k | −0.043 | (−0.292,0.206) |
| 25 k-50 k | 0.038 | (−0.358,0.434) |
| <25 k | 0.022 | (−0.428,0.472) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.183* | (−0.380,0.013) |
| N | 4,606 | |
| Model B – Heavy Drinking | ||
| Lockdown Policy*Consuming Alcohol | ||
| During | −0.027 | (−0.193,0.139) |
| Lockdown Policy (at Consuming Alcohol = 0) | ||
| During | −1.372** | (−2.589, −0.154) |
| Consuming Alcohol (at Lockdown Policy = 0) | 0.103 | (−0.058,0.264) |
| Household Income (reference: >100 k) | ||
| 50 k–100 k | 0.113 | (−0.110,0.336) |
| 25 k–50 k | 0.192 | (−0.102,0.486) |
| <25 k | 0.266 | (−0.067,0.599) |
| Employment Status (reference: Employed) | ||
| Unemployed | −0.065 | (−0.230,0.100) |
| N | 6,622 | |
*p < 0.1; **p < 0.05; *** p < 0.01; **** p < 0.001.
Time-invariant individual and month fixed effects included but not shown.
Robust standard errors.
References
- Abraham Amanda J., Andrews Christina M., Grogan Colleen M., D’Aunno Thomas, Humphreys Keith N., Pollack Harold A., et al. The affordable care act transformation of substance use disorder treatment. American Journal of Public Health. 2017;107(1):31–32. doi: 10.2105/AJPH.2016.303558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams-Prassl A, Boneva T, Golin M, Rauh C. The Impact of the Coronavirus Lockdown on Mental Health: Evidence from the US. Published online 2021.
- Bruckner T.A., Singh P., Chakravarthy B., Snowden L., Yoon J. Psychiatric emergency department visits after regional expansion of community health centers. Psychiatric Services (Washington, D. C.) 2019;70(10):901–906. doi: 10.1176/appi.ps.201800553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner Julia D., Abarno Cristina N., Lewis Elizabeth M., Zvolensky Michael J., Garey Lorra. Increases in distress during stay-at-home mandates During the COVID-19 pandemic: A longitudinal study. Psychiatry Research. 2021;298:113821. doi: 10.1016/j.psychres.2021.113821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R., Dooley C.D. Economic predictors of depressed mood and stressful life events in a metropolitan community. Journal of Health and Social Behavior. 1977;18(3):292–307. doi: 10.2307/2136355. [DOI] [PubMed] [Google Scholar]
- COVID-19 to Plunge Global Economy into Worst Recession since World War II. World Bank. Accessed June 18, 2020. https://www.worldbank.org/en/news/press-release/2020/06/08/covid-19-to-plunge-global-economy-into-worst-recession-since-world-war-ii.
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., et al. Mental Health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsson A.-K., Lundin A., Agardh E., Allebeck P., Forsell Y. Cannabis use, depression and anxiety: A 3-year prospective population-based study. Journal of Affective Disorders. 2016;193:103–108. doi: 10.1016/j.jad.2015.12.045. [DOI] [PubMed] [Google Scholar]
- Dawson David L., Golijani-Moghaddam Nima. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What Is Addiction? Accessed December 1, 2020. https://www.psychiatry.org/patients-families/addiction/what-is-addiction.
- Racial Differences in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease 2019 (COVID-19) Pandemic. Published online 2020:3. [DOI] [PMC free article] [PubMed]
- Economic News Releases : U.S. Bureau of Labor Statistics. Accessed December 7, 2020. https://www.bls.gov/bls/newsrels.htm.
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9):e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman-Mellor Sidra J., Saxton Katherine B., Catalano Ralph C. Economic contraction and mental health: A review of the evidence, 1990–2009. International Journal of Mental Health. 2010;39(2):6–31. doi: 10.2753/IMH0020-7411390201. [DOI] [Google Scholar]
- Holmes Emily A, O'Connor Rory C, Perry V Hugh, Tracey Irene, Wessely Simon, Arseneault Louise, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IHME COVID-19 Forecasting Team. Modeling COVID-19 scenarios for the United States. Nat Med. Published online October 23, 2020. doi: 10.1038/s41591-020-1132-9.
- Kawachi I., Berkman L.F. Social ties and mental health. The Journal of Urban Health|New York Academy of Medicine. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawohl W., Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kettl Donald F. States divided: The implications of american federalism for COVID-19. Public Adm Rev. 2020;80(4):595–602. doi: 10.1111/puar.v80.410.1111/puar.13243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian E.J. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kim Jin Un, Majid Amir, Judge Rebekah, Crook Peter, Nathwani Rooshi, Selvapatt Nowlan, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology and Hepatology. 2020;5(10):886–887. doi: 10.1016/S2468-1253(20)30251-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol M.J., van der Tweel I., Grobbee D.E., Numans M.E., Geerlings M.I. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. International Journal of Epidemiology. 2007;36(5):1111–1118. doi: 10.1093/ije/dym157. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1016/S0033-3182(09)70864-3. [DOI] [PubMed] [Google Scholar]
- State Medical Marijuana Laws. Published 2020. Accessed November 20, 2020. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- Lev-Ran S., Roerecke M., Foll B.L., George T.P., McKenzie K., Rehm J. The association between cannabis use and depression: A systematic review and meta-analysis of longitudinal studies. Psychological Medicine. 2014;44(4):797–810. doi: 10.1017/S0033291713001438. [DOI] [PubMed] [Google Scholar]
- Lipton R.I. The effect of moderate alcohol use on the relationship between stress and depression. American Journal of Public Health. 1994;84(12):1913–1917. doi: 10.2105/AJPH.84.12.1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín Brett, Vine Vera, Morgan Reed. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCannon B.C. Stay-at-home orders were issued earlier in economically Unfree States. SSRN Electron J. 2020 doi: 10.2139/ssrn.3589934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhee M.D., Keough M.T., Rundle S., Heath L.M., Wardell J.D., Depression Hendershot CS. Environmental reward, coping motives and alcohol consumption during the COVID-19 Pandemic. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.574676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meda Nicola, Pardini Susanna, Slongo Irene, Bodini Luca, Zordan Mauro Agostino, Rigobello Paolo, et al. Students’ mental health problems before, during, and after COVID-19 lockdown in Italy. Journal of Psychiatric Research. 2021;134:69–77. doi: 10.1016/j.jpsychires.2020.12.045. [DOI] [PubMed] [Google Scholar]
- Moreland A. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement — United States. Morbidity and Mortality Weekly Report. 2020;69 doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Humer E., Probst T. Comparing mental health during the COVID-19 lockdown and 6 months after the lockdown in Austria: A longitudinal study. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.625973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce Matthias, Hope Holly, Ford Tamsin, Hatch Stephani, Hotopf Matthew, John Ann, et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radeloff D., Papsdorf R., Uhlig K., Vasilache A., Putnam K., von Klitzing K. Trends in suicide rates during the COVID-19 pandemic Restrictions in a Major German City. Psychiatry and Clinical Psychology. 2020 doi: 10.1101/2020.10.21.20187419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodda L.N., West K.L., LeSaint K.T. Opioid overdose-related emergency department visits and accidental deaths during the COVID-19 pandemic. Journal of Urban Health. 2020;97(6):808–813. doi: 10.1007/s11524-020-00486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez Lindsey M., Litt Dana M., Stewart Sherry H. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors. 2020;110:106532. doi: 10.1016/j.addbeh.2020.106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skapinakis Petros, Bellos Stefanos, Oikonomou Achilleas, Dimitriadis Georgios, Gkikas Paschalis, Perdikari Evridiki, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: A cross-sectional survey of the population. Depression Research and Treatment. 2020;2020:1–11. doi: 10.1155/2020/3158954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of the Cannabis Industry - 2020 Report. Stateofthecannabis. Accessed November 30, 2020. https://www.stateofthecannabisindustry.com.
- Status of lockdown and stay-at-home orders. Ballotpedia. Published 2020. Accessed November 2, 2020. https://ballotpedia.org/Status_of_lockdown_and_stay-at-home_orders_in_response_to_the_coronavirus_(COVID-19)_pandemic_2020.
- Tanaka T., Okamoto S. Suicide during the COVID-19 Pandemic in Japan. Public and Global Health. 2020 doi: 10.1101/2020.08.30.20184168. [DOI] [Google Scholar]
- The Lancet Gastroenterology & Hepatology Drinking alone: COVID-19, lockdown, and alcohol-related harm. The Lancet Gastroenterology and Hepatology. 2020;5(7):625. doi: 10.1016/S2468-1253(20)30159-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinh Nhung T.H., Singh Parvati, Cerdá Magdalena, Bruckner Tim A. Opioid-related emergencies in New York City after the Great Recession. Journal of Substance Abuse Treatment. 2021;125:108311. doi: 10.1016/j.jsat.2021.108311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Understanding America Study. Published 2021. Accessed December 1, 2020. https://uasdata.usc.edu/index.php.
- Vigo D., Patten S., Pajer K., et al. Mental health of communities during the COVID-19 pandemic. The Canadian Journal of Psychiatry. 2020 doi: 10.1177/0706743720926676. 070674372092667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell J.D., Kempe T., Rapinda K.K., et al. Drinking to cope during COVID‐19 pandemic: The role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcoholism: Clinical and Experimental Research. 2020 doi: 10.1111/acer.14425. acer.14425. [DOI] [PubMed] [Google Scholar]
- Western B., Wildeman C. The black family and mass incarceration. The American Academy of Political and Social Science. 2009;621(1):221–242. doi: 10.1177/0002716208324850. [DOI] [Google Scholar]
- Wooldridge JM 1960-. Introductory Econometrics : A Modern Approach. Fifth edition. Mason, Ohio : South-Western Cengage Learning, [2012] ©2012; 2012. https://search.library.wisc.edu/catalog/9910154038602121.
- Zeidner, M., & Saklofske, D. (1996). Adaptive and maladaptive coping. In Handbook of Coping: Theory, Research, Applications (pp. 505–531). John Wiley & Sons.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used for the analysis and the statistical code is available from the corresponding author. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.