Abstract
Background
Previous computer-generated splints were designed and produced without modification than the traditional occlusal splints, which did not facilitate surgeon's intraoperative judgment in the single-splint two-jaw orthognathic surgery. Modifications of the digital occlusal splint can be achieved using computer-aided design and computer-aided manufacturing (CAD/CAM) software. This study reported the design, clinical application and validation of a novel CAD/CAM occlusal splint.
Methods
The maxillary and mandibular segments were fixed into the final occlusal splint and moved to the planned position according to the 3-dimensional simulation. The composite occlusal splint has 4 orthogonal bars to facilitate intraoperative assessment of the dental and skeletal midline, facial soft tissue midline, occlusal plane, upper tooth show, facial symmetry and facial bone position. To validate the surgical outcome, 5 parameters including pitch, roll and yaw rotations, midline deviation and chin position were measured on the virtual plan and the postoperative cone-beam computed tomography images to quantify the difference.
Results
The results showed no significant differences in the 5 parameters between the simulation and postoperative images. The root-mean-square difference between the conventional splints and CAD/CAM surgical splint ranged from 0.18 to 0.31 mm by superimposition of the two image models. All patients were satisfied with the treatment outcomes. Overall, this novel occlusal splint is ideal for verification of the maxillomandibular position during surgery.
Conclusion
The novel composite occlusal splint provided useful and informative check to verify the maxillomandibular complex (MMC) position and facial appearance in single-splint two-jaw orthognathic surgery.
Keywords: Occlusal splints, Composite occlusal splint, Single-splint two-jaw orthognathic surgery, Computer-aided design and computer-aided manufacturing (CAD/CAM), Intraoperative assessment
At a glance commentary.
Scientific background on the subject
The composite occlusal splint was designed from the initial digital occlusal splint which contained four mutually orthogonal bars using CAD software, and fabricated using a 3D printer. The CAD/CAM composite occlusal splint was transparentand classified as “surface devices” for guiding the translation and rotation of the maxillomandibular complex.
What this study adds to the field
The surgeons felt the ease of using the CAD/CAM composite occlusal splint without interference. The extended bars provided useful information for positioning the maxillomandibular complex (MMC) position during the surgery without the need of retracting lips for inspection in the surgery.
With the recent advance in three-dimensional (3D) imaging, computer-assisted surgical planning and simulation are popularly used in orthognathic surgery for comprehensive analysis of craniofacial complex and enhanced predictability of surgical outcomes [[1], [2], [3], [4], [5], [6]]. Surgical splints and guides can be generated by using computer-aided design and computer-aided manufacturing (CAD/CAM) technique based on the virtual planning to facilitate orthognathic surgery [[7], [8], [9], [10]]. In recent studies, researchers have proposed the use of CAD/CAM surgical splint as an alternative to conquer possible defects from the laboratory-based method, including the non-controllable errors, inter-laboratory difference and time-consuming problem. Gateno et al. first accessed the precision of computer-generated surgical splints by comparing them with the conventional surgical splints and considered that the plaster dental model surgery may not be required [1]. Lauren et al. proposed the CAD/CAM flat-plane and full-coverage occlusal splints with guidance ramps, and the fabricated splints have been commercially available since 2007 [11]. Metzger et al., Choi et al., Uribe et al., Scolozzi et al. and Francisco et al. introduced case studies of virtual reposition of the jaws and production of surgical splints from the composite skull model obtained by integrating cone-beam computed tomography (CBCT) model and 3D digital dental casts [6,[12], [13], [14], [15]]. Dahan et al., Aboul-Hosn Centenero et al. and Shqaidef et al. reported comparative studies of the accuracy between CAD/CAM and conventional surgical wafers [[16], [17], [18]]. Hernández-Alfaro et al. comprised an in vitro and a prospective in vivo study using an intraoral digital scanner instead of dental impression to obtain the surface images of dental arches, and then fused with CBCT image for virtual surgery and CAD/CAM intermediate splint fabrication. The protocol revealed high accuracy and reliability [19]. Schouman et al. proposed a cadaveric study to evaluate the accuracy of CAD/CAM maxillary cutting guides and intermediate splint in orthognathic surgery [20]. Ying et al. reported a prospective study to investigate the efficacy of combined guiding templates and splints fabricated by rapid prototyping technique for correction of facial asymmetry associated with vertical maxillary excess and mandibular prognathism [21]. The traditional plaster dental model surgery may no longer be required in the future, and evidences have shown that some of the treatment plan could be transferred from the computer to the intraoperative patient by means of the CAD/CAM surgical splints [[19], [20], [21], [22], [23]]. This study was intended to develop a novel dental occlusal splint that served to guide and verify the planned position of the maxillomandibular skeletal object during the orthognathic surgery.
The single-splint technique fixes the maxillary and mandibular segments into the final occlusal splint, forming a maxillomandibular complex (MMC). The MMC is moved according to surgical plan and confirmed with the intraoperative checkpoints for facial symmetry and aesthetics, in addition to the dental midline and occlusal line. This method has been reported as a practical alternative to the classic two-splint technique for the two-jaw surgery, particularly in patients with facial asymmetry [24]. When the MMC position and facial soft tissue appearance are verified, the maxillary LeFort I and mandibular ramus osteotomies are fixed in sequence. Intraoperative checking of skeletal and soft tissues is technically demanding and could subject to errors. We believed that the occlusal splint with attached auxiliary labels or markers could provide surgeons better intraoperative guidance and surgical information of the underlying MMC. Although previous studies have validated the use of a CAD/CAM occlusal splint as a reliable substitute for the conventional splint [1,[19], [20], [21], [22], [23]]. These computer-generated splints were designed and produced without further modification than the traditional occlusal splint, which did not facilitate surgeon's intraoperative judgment in the single-splint two-jaw orthognathic surgery. Modifications of the digital occlusal splint can be achieved using CAD/CAM software.
Therefore, The aims of this study is to propose a novel occlusal splint for intraoperative confirmation of the soft and hard tissue results during the single-splint two-jaw orthognathic surgery, and to report the accuracy of our design and experience in clinical application.
Material and methods
Patients and study design
Patients with facial bone deformity and malocclusion scheduled for two-jaw orthognathic surgery were included in this prospective study. Exclusion criteria were a history of facial trauma, degenerative or inflammatory conditions, or inadequate imaging. In total, 105 patients were recruited who received single-splint two-jaw orthognathic surgery, including LeFort I osteotomy and bilateral sagittal split osteotomy (BSSO) for correction of dentofacial deformity between May 2015 and September 2017. All surgeries were conducted by the senior author (L.J.L.). The primary outcome assessment was comparison of the differences between the surgical simulation and 1-month postoperative CBCT images. The secondary outcome assessment was the patients' satisfaction with the dental and facial appearance.
Image acquisition and surgical planning
The 3D maxillofacial imaging was performed within one month before the surgery using i-CAT® CBCT scanner (Imaging Sciences International, Hatfield, PA), with the patients' teeth in light-contact condition. An initial surgical planning was made based on 2-dimensional cephalometric analysis, dental model study and 3D representation of the anatomy. The plaster casts were scanned by 3Shape dental scanner (Copenhagen, Denmark), and the digitized images were used for replacing the rough dentition on a CBCT scan to provide a reliable occlusal relationship between maxilla and mandible. The conventional occlusal splint was hand-made from laboratory-processed acrylic resin according to the planned maxilla and mandibular cast position for comparison with CAD/CAM occlusal splint.
3D surgical simulation
All patients' data were stored in Digital Imaging and Communications in Medicine (DICOM) file format. Preoperative digital dental models were incorporated into 3D CBCT bone model to create a composite skull model. The virtual surgical simulation was carried out by Dolphin Imaging® software (Dolphin Imaging and Management Solutions, Chatsworth, California) on the composite skull model. The surgical simulation began with the establishment of the FH plane passing through the midpoint between left and right porion, right orbitale, and left orbitale. Virtual LeFort I osteotomy and BSSO were performed. The distal mandibular segment was moved to fit the final occlusion to the maxilla, forming the MMC image object. The MMC was mobilized based on the initial surgical plan. Modifications of the initial plan were made when the MMC position was not ideal by evaluating the facial symmetry, dental and skeletal midline, pitch, roll and yaw rotations, and facial profile [24,25]. Genioplasty simulation was performed if indicated. When the virtual 3D planning achieved the ideal position and was approved by the treatment team, the simulation object data was exported in a stereolithography (STL) file format.
CAD/CAM composite occlusal splint
Initial occlusal splint
The initial occlusal splint was created from virtual simulation object by Dolphin Imaging® software. First, the upper and lower occlusal planes including cusps of all teeth was made [Fig. 1A]. The contouring function was performed in the top and bottom view to define the vertical thickness and arch boundary of the splint [Fig. 1B]. The shape of occlusal splint and the indentation of the occlusal surfaces combining the upper and lower teeth were repeatedly previewed and adjusted until the ideal final form of initial occlusal splint was achieved [Fig. 1C]. The initial occlusal splint was combined with the virtual simulation object and exported in a STL file format for subsequent design of the final occlusal splint.
Fig. 1.
(A) The upper and lower occlusal planes around cusps of all the teeth was made. (B) The contouring function was performed in the top and bottom view to define the vertical thickness and arch boundary of the splint. (C) Repeated preview the shape of occlusal splint and the indentation of the occlusal surfaces combined with upper and lower teeth, and adjust the shape until the ideal final situation of initial occlusal splint was achieved. (D) The offset operation with average internal distance of 0.2 mm was executed on the combined model of initial occlusal splint and virtual simulation object to provide the ideal fit between the occlusal splint and the MMC.
Composite occlusal splint
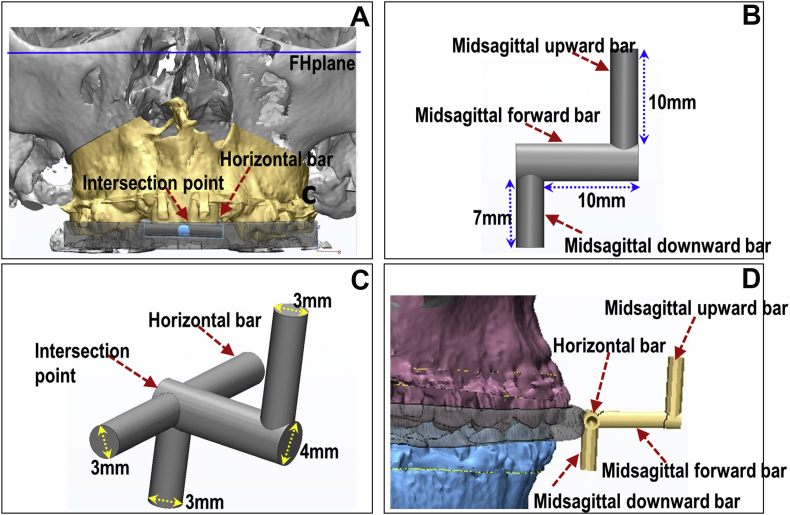
The finial occlusal splint with bars was designed using 3-matic (CAD software, Materialise, Belgium). An offset operation with average internal distance of 0.2 mm was carried out on the combined model to provide the ideal fit between the occlusal splint and the MMC, and ensure convenient and accurate placement in the operating room [Fig. 1D]. Four mutually orthogonal bars were created and attached to the outer surface of the initial occlusal splint, which were horizontal, midsagittal forward, midsagittal downward and midsagittal upward bars. First, the horizontal bar was constructed passing the intersection point of outer surface of occlusal splint and midsagittal plane, and parallel to the FH plane [Fig. 2A]. Next, 3 joined orthogonal bars was created including midsagittal forward (with a length of 10 mm and a diameter of 4 mm), midsagittal upward (with a length of 10 mm and a diameter of 3 mm) and midsagittal downward (with a length of 7 mm and a diameter of 3 mm) bars [Fig. 2B]. Then, the 3 joined bars was connected to the intersection point on the horizontal bar [Fig. 2C], and ensure that midsagittal forward and downward bars were perpendicular to the horizontal bar [Fig. 2D]. In addition, we could design some markers (holes) on the surface of occlusal splint as the validation points when intraoperative navigation system was to be used [26]. The size of the hole was matching with the tracking probe [Fig. 3].
Fig. 2.
(A) The horizontal bar was constructed passing the intersection point of outer surface of occlusal splint and midsagittal plane, and parallel to the FH plane. (B) 3 joined orthogonal bars was created including midsagittal forward, midsagittal downward and midsagittal upward bars. (C) The 3 joined bars was connected to the intersection point on the horizontal bar. (D) The midsagittal forward and downward bars were perpendicular to the horizontal bar.
Fig. 3.
Some markers (holes) on the surface of occlusal splint as the validation points were designed when intraoperative navigation system was used.
When the finial occlusal splint design was complete, a rapid prototype splint was fabricated (3D printing) by using the Objet30 OrthoDesk 3D Printer (Stratasys Ltd. Nasdaq: SSYS) with the biocompatible PolyJet photopolymer (MED610) medical materials. The CAD/CAM composite occlusal splint was transparent [Fig. 4B] and classified as “surface devices” [20]. The medical material has been regularly used to produce the MMC positioning guides for single-splint two-jaw orthognathic surgery in our center [27].
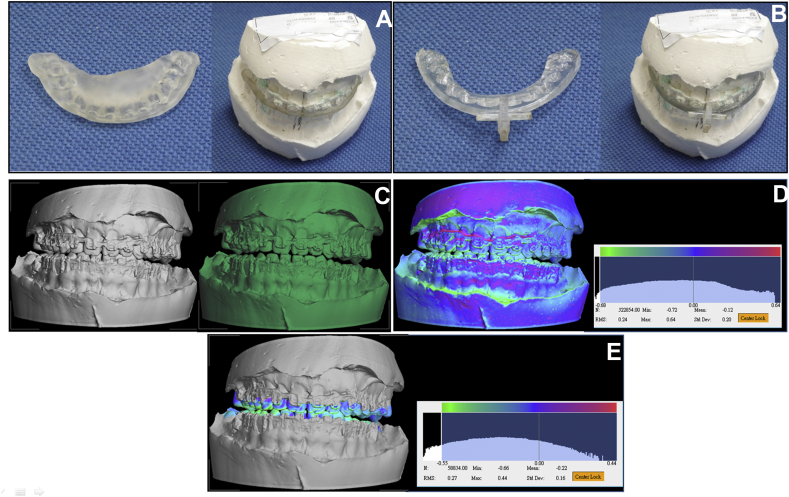
Fig. 4.
(A) The laboratory-fabricated occlusal splint. (B) CAD/CAM composite occlusal splint. (C) The splint-stone objects were scanned using 3Shape dental scanner to obtain the digitized images. (D) The images were registered using manual superimposition based on whole surface of models. (E) The final superimposition was automatically performed to quantify the difference between the images on the region of interest (ROI), which was the occlusal relationships of the teeth.
Comparison of occlusal relationship between conventional and CAD/CAM occlusal splint
The conventional and CAD/CAM composite occlusal splints were separately articulated with the upper and lower dental stone model forming a splint-stone object respectively [Fig. 4A]. The splint-stone objects were scanned using 3Shape dental scanner to obtain the digitized images and the images were superimposed to quantify the shell-to-shell difference of occlusal relationship between the splint-stone objects [Fig. 4C]. The images were first registered using manual superimposition based on whole surface of models to shorten the time taken for the subsequent automatic superimposition [Fig. 4D]. After pairs of models were oriented and manually registered, the final superimposition was automatically performed to quantify the difference between the images on the region of interest (ROI). In this study, the occlusal relationship of the teeth was selected as the ROI [Fig. 4E]. The 3dMD Vultus software (3dMD, Atlanta, Georgia) was used for model superimposition and automatically displaying of magnitude, direction, and location of disagreement among the models in a color-scale plot. The precision of the surface superimposition was calculated in terms of the root-mean-square deviation (RMSD) of distance between the superimposed models, with RMSD ≤0.5 mm considered acceptable [28,29]. Before surgery, the splint fitting test was performed on the dental cast and on the patients, for all conventional and CAD/CAM composite occlusal splints.
Surgical procedures
Patients was under general anesthesia and nasotracheal intubation. Draping was performed to expose the whole face from eyebrow to neck. All patients received two-jaw orthognathic surgery using single occlusal splint method. The maxilla and mandible were mobilized after LeFort I and BSSO procedures. The maxillary and mandibular segments were placed in the intermaxillary fixation using the manufactured composite occlusal splint, forming the MMC. The MMC was moved as a unit to the final position according to the simulation plan. A temporary fixation could be done, or the bones were hold in the position with hands. Patient's head was positioned with the FH plane perpendicular to the ground level [Fig. 5]. The facial skin was released for inspection of the facial appearance as well as checking the position of the underlying maxillary and mandibular segments by using the joined orthogonal bars on the occlusal splint [Fig. 6]. First, checking the yaw direction was made by aligning the horizontal bar which should parallel with the ground floor. Next, the pitch direction was confirmed by using the midsagittal upward bar, which should be perpendicular to the FH plane, and parallel to the ground floor. Then, the dental midline, skeletal midline and facial midline were checked by using midsagittal forward bar and a face-bow. Finally, upper tooth show below upper lip, symmetry and facial proportion were repeatedly evaluated to ensure satisfactory appearance. The sequence of steps could be changed and repeated. After the maxillomandibular complex position was confirmed, plate and screw fixation was applied to the LeFort I, followed by the fixation of the mandibular ramus region. Genioplasty was performed when required, and the downward bar used for checking the midline position of the chin bone.
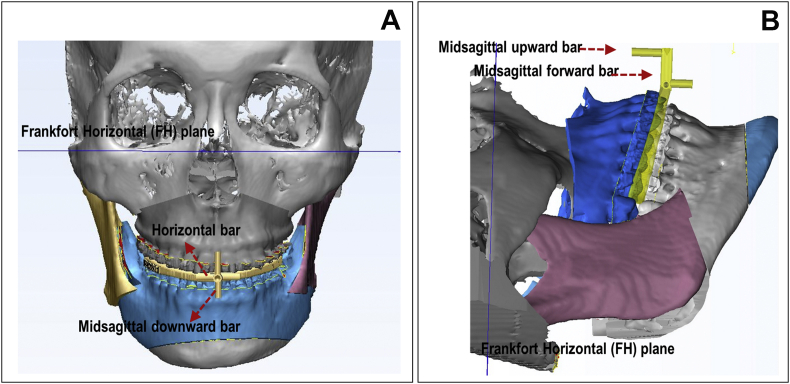
Fig. 5.
(A) The horizontal bar is used to position patient's face in the Frankfort Horizontal (FH) plane, and the midsagittal downward bar is used to check the lower dental and chin midline. (B) In the single-splint two-jaw surgery, the midsagittal forward bar is perpendicular to and the midsagittal upward bar parallel to the ground floor for controlling the pitch rotation of the maxillomandibular complex.
Fig. 6.
The intraoperative inspection of the facial appearance by using the cylinders on the occlusal splint and face-bow.
Validation of the treatment
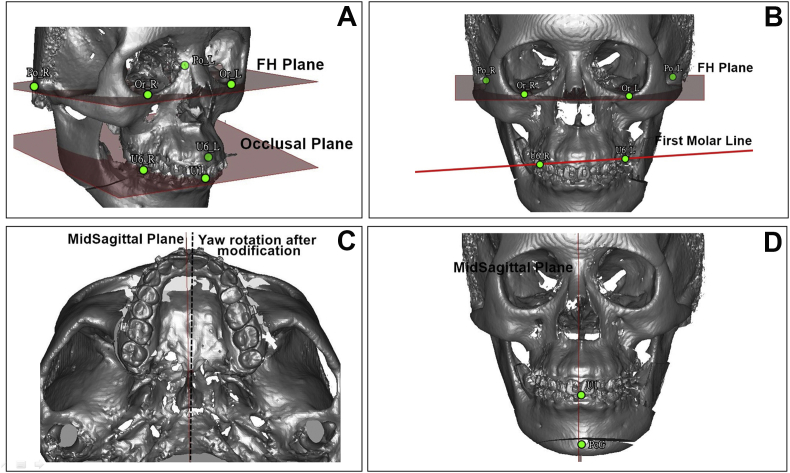
Postoperative CBCT was taken at 1 month using the same condition as for preoperative CBCT. There was no dental treatment in this period. The digital dental images from the stone models were used to replace the teeth in the maxilla and mandible separately in the postoperative CBCT, using the proposed artifact-resistant superimposition technique with high reproducibility and clinically acceptable RMSD [30]. The pitch, roll and yaw rotations, midline deviation and chin position were measured on the integrated postoperative CBCT model and the surgical simulation model respectively, to quantify the difference between the two images for the execution of the 3D plan [Fig. 7] [25].
Fig. 7.
The measurement of pitch, roll and yaw rotation; difference of frontal ramus inclination; midline deviation and chin position on 3D model. (A) Pitch rotation is the angle between lateral occlusal plane to FH plane. (B) Roll rotation is the angle formed by FH plane and bimaxillary first molar line. Frontal ramus inclination is the angle between FH plane and line from lateral condyle point to lateral gonion point. (C) Yaw rotation is the angle between sagittal plane and midpalatal suture. (D) Midline deviation is the distance from the midpoint of molars to the midsagittal plane. Chin position is the distance from the Pogonion to the midsagittal plan.
Postoperative outcome
All patients continued orthodontic treatment and follow-ups in the same treatment team. Intraoperative use of the splint and possible related problems, the postoperative treatment results, and patient satisfaction were evaluated.
Statistical analysis
Each manual superimposition of conventional and CAD/CAM occlusal splint was performed twice by 2 operators to investigate the intraobserver reproducibility and interobserver reliability. The Pearson correlation coefficient was calculated to validate the intraobserver reproducibility; the interobserver reliability was calculated using Cronbach's alpha reliability coefficient, which ranged between 0 and 1, with a higher value indicating a higher correlation or reliability. Statistical analyses were performed using the SPSS software (Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc.).
Results
The surgical simulation, as well as fabrication and intraoperative use of the CAD/CAM composite occlusal splint were performed in 105 patients. In the initial stage, the occlusal splints were designed to facilitate intraoperative assessment of the dental, skeletal and facial soft tissue midlines. The bars were later modified to obtain more convenience and intraoperative information of the MMC rotation. All surgeries were performed according to the 3D plan. The splint fit well in the maxillary and the mandibular teeth, and the bars provided useful information in positioning the MMC. After orthognathic surgery, the patients continued to receive orthodontic treatment in the same center, and were regularly followed up in surgical clinic. There were no complications with regard to using the composite occlusal splint.
Statistical results of the intraobserver reproducibility and interobserver reliability of digital superimposition between the conventional and CAD/CAM occlusal splints were shown in Table 1. The Pearson correlation coefficient and Cronbach's alpha reliability coefficient showed no statistically significant difference within and between operators on image superimposition of conventional and CAD/CAM occlusal splints, indicating desirable intraobserver reproducibility and interobserver reliability.
Table 1.
Statistical results of intraobserver and interobserver measurement for superimposition of conventional and CAD/CAM occlusal splints.
| Intraobserver (operator A) | Mean ± SD | Minimum | Maximum | Pearson correlation coefficient (r) |
|---|---|---|---|---|
| 1st operation | 0.21 ± 0.05 | 0.25 | 0.32 | 0.987 |
| 2nd operation | 0.20 ± 0.07 | 0.27 | 0.31 | |
| Interobserver | Mean ± SD | Minimum | Maximum | Cronbach's alpha |
| 1st operation | 0.21 ± 0.05 | 0.25 | 0.32 | 0.972 |
| Operator B | 0.28 ± 0.11 | 0.22 | 0.38 | |
| 2nd operation | 0.20 ± 0.07 | 0.27 | 0.31 | 0.905 |
| Operator B | 0.28 ± 0.11 | 0.22 | 0.38 | |
Correlation coefficient (r) > 0.8, Cronbach's alpha > 0.8: the degree of linear relationship showed strong correlation.
The comparison between the conventional and CAD/CAM occlusal splint demonstrated a high degree of similarity. The root-mean-square deviation (RMSD) values of superimposition of the corresponding splint-stone object for traditional and CAD/CAM splint ranged from 0.18 to 0.31 mm (with a mean of 0.27 mm) for the 105 patients. Clinically, there was no perceptible difference in the occlusal fitting between the two types of occlusal splints. The results showed that the conventional acrylic splints could be reliably substituted by the CAD/CAM surgical splint for the surgery.
The later modifications of the CAD/CAM splint were for easier and accurate intraoperative control of the MMC position. 17 patients had available images for the outcome assessment. Five parameters were checked, including pitch, roll and yaw rotations, midline deviation and chin position. The results showed no significant difference in the 5 parameters between the simulation and postoperative CBCT models [Table 2]. The results indicated that the proposed CAD/CAM occlusal splint is a reliable technique for translating the 3D surgical plan in the operating room.
Table 2.
The difference of pitch, roll and yaw rotation; difference of frontal ramus inclination; midline deviation and chin position on the maxillomandibular complex (MMC) between 3D surgical simulation and postoperative images.
| Parameters | 3D simulation |
Postoperative image |
Difference |
p valuea |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Pitch | 14.52 (3.52) | 10.97 (2.38) | 4.32 (2.55) | 0.091 |
| Roll | 1.24 (0.65) | 0.90 (0.60) | 0.65 (0.33) | 0.237 |
| Yaw | 0.78 (0.51) | 1.65 (1.42) | 1.21 (0.95) | 0.128 |
| Chin position | 1.14 (1.08) | 2.76 (2.05) | 2.63 (2.5) | 0.398 |
| Midline deviation | 0.83 (0.50) | 1.52 (1.28) | 1.26 (1.16) | 0.499 |
The pitch, roll and yaw are in degrees. The chin position and midline deviation are in mm.
The difference was considered statistically significant if p < 0.05.
The surgeons felt the ease of using the composite occlusal splint without interference. The extended bars provided information for positioning the MMC position during the surgery without the need of retracting lips for inspection in the surgery. For subjective outcome assessment, an investigation of patient satisfaction revealed that all patients were happy with the surgical outcome, facial appearance, and dental alignment. No patients in this series received secondary procedures for the dentofacial deformity.
Discussion
Most studies reported the use of a CAD/CAM surgical splint without further modification, and concluded that it was a reliable substitute for the laboratory-fabricated occlusal splints with respect to the accuracy of occlusal fitting [11,[20], [21], [22], [23],31]. However, the reported 3D printed splints were little different from the conventional splints, and offered no additional intraoperative information for the single-splint two-jaw orthognathic surgery. Modifications were made in this study. Addition of the extension bars provided useful intraoperative guidance for positioning MMC in single-splint two-jaw orthognathic surgery.
The CAD/CAM composite occlusal splint provided precision, consistency, quantitative control, low cost, and speed over manually produced occlusal splint. The results showed that the conventional occlusal splint could be reliably replaced by the CAD/CAM occlusal splint with a clinically acceptable RMSD of less 0.5 mm in all patients. In the validation of surgical outcome, an accurate superimposition method was used to replace the maxillary and mandibular teeth in the postoperative CBCT. The difference of pitch, roll and yaw rotations, midline deviation and chin position were compared between the simulation and integrated postoperative CBCT images, and showed acceptable accuracy in translating the virtual plan to actual surgery.
The 4 mutually orthogonal bars consisting of two horizontal and two vertical bars were used for intraoperative assessment of dental midline, skeletal midline, occlusal plane, upper tooth show below upper lip, facial skin midline, and symmetry. Because the bars extend outside of oral aperture, the lips and facial tissue do not need to be retracted for the intraoperative inspection. Checking of the midline, horizontal occlusal line (roll), yaw and pitch position of the MMC is straightforward by using the composite occlusal splint. The horizontal bar is used to position patient's face corresponding to the Frankfort Horizontal (FH) plane, and the midsagittal downward bar is used to check the chin midline during genioplasty [Fig. 5A]. In the single-splint two-jaw surgery, control of the pitch rotation of the MMC is important and subjected to surgeon's experience. In our approach, the CAD/CAD composite occlusal splints were designed initially to facilitate intraoperative inspection of the dental and skeletal midline, facial soft tissue midline, and occlusal line. Modifications were made to control the yaw and pitch rotations of the MMC. With patient's head positioned in FH plane, the horizontal bar is parallel to the ground floor for the yaw and midsagittal upward is parallel to the ground floor for the pitch control [Fig. 5B]. The yaw control was satisfactory with a mean difference of 1.21° [Table 2]. We noticed that the pitch control was 4.32° in average, presenting a room for improvement in the future study. Accurate pitch control of the MMC position is an important issue in single-splint two-jaw orthognathic surgery.
To produce this composite occlusal splint, it requires computer software, a trained personnel and 3D printer, which may currently constitute the limitation on its use. In summary, the CAD/CAM composite occlusal splint transferred the virtual plan to the patient in actual operating theater with satisfactory surgical outcome. There was no related complications. Surgeons felt convenient on its use, and patients were happy with the results.
Conclusions
The novel composite occlusal splint provided useful and informative check to verify the MMC position and facial appearance in single-splint two-jaw orthognathic surgery.
Ethics statement
This prospective study was conducted in Chang Gung Craniofacial Center under the approval of the Institutional Review Board (IRB) of Chang Gung Medical Foundation (IRB No. 102-5354B). Written informed consents were obtained from all patients or guardians of the patients younger than 20 years.
Conflicts of interest
The authors have no financial conflicts of interest.
Acknowledgments
This work was supported by Chang Gung Memorial Hospital under Grant CMRG5F0181-2, and a grant from the Ministry of Science and Technology MOST 106-2314-B-182A-154, MOST 106-2314-B-182-060, MOST 106-2314-B-182-061. The authors are grateful to Betty Pai, DDS, for orthodontic management and initial surgical planning for these patients. The authors declare no other potential conflicts of interest with respect to the authorship and/or publication of this article.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Gateno J., Xia J., Teichgraeber J.F., Rosen A., Hultgren B., Vadnais T. The precision of computer-generated surgical splints. J Oral Maxillofac Surg. 2003;61:814–817. doi: 10.1016/s0278-2391(03)00240-4. [DOI] [PubMed] [Google Scholar]
- 2.Xia J.J., Gateno J., Teichgraeber J.F. Three-dimensional computeraided surgical simulation for maxillofacial surgery. Atlas Oral Maxillofac Surg Clin North Am. 2005;13:25–39. doi: 10.1016/j.cxom.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Swennen G.R., Mollemans W., Schutyser F. Three-dimensional treatment planning of orthognathic surgery in the era of virtual imaging. J Oral Maxillofac Surg. 2009;67:2080–2092. doi: 10.1016/j.joms.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Schendel S.A., Jacobson R. Three-dimensional imaging and computer simulation for office-based surgery. J Oral Maxillofac Surg. 2009;67:2107–2114. doi: 10.1016/j.joms.2009.04.111. [DOI] [PubMed] [Google Scholar]
- 5.Olszewski R. Re: How accurate is model planning for orthognathic surgery? Sharifi A, Jones R, Ayoub A, Moos K, Walker F, Khambay B, McHugh S. Int J Oral Maxillofac Surg 2008;37:1089–1093. Int J Oral Maxillofac Surg. 2009;38:1009–1010. doi: 10.1016/j.ijom.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 6.Choi J.Y., Song K.G., Baek S.H. Virtual model surgery and wafer fabrication for orthognathic surgery. Int J Oral Maxillofac Surg. 2009;38:1306–1310. doi: 10.1016/j.ijom.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Zinser M., Mischkowski R.A., Sailer H.F., Zöller J.E. Computer-assisted orthognathic surgery: feasibility study using multiple CAD/CAM surgical splints. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:673–687. doi: 10.1016/j.oooo.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Shehab M.F., Barakat A.A., AbdElghany K., Mostafa Y., Baur D.A. A novel design of a computer-generated splint for vertical repositioning of the maxilla after Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e16–e25. doi: 10.1016/j.oooo.2011.09.035. [DOI] [PubMed] [Google Scholar]
- 9.Li B., Zhang L., Sun H., Yuan J., Shen S.G., Wang X. A novel method of computer aided orthognathic surgery using individual CAD/CAM templates: a combination of osteotomy and repositioning guides. Br J Oral Maxillofac Surg. 2013;51:e239−44. doi: 10.1016/j.bjoms.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Polley J.W., Figueroa A.A. Orthognathic positioning system: intraoperative system to transfer virtual surgical plan to operating field during orthognathic surgery. J Oral Maxillofac Surg. 2013;71:911–920. doi: 10.1016/j.joms.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Lauren M., McIntyre F. A new computer-assisted method for design and fabrication of occlusal splints. Am J Orthod Dentofacial Orthop. 2008;133:S130−5. doi: 10.1016/j.ajodo.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Metzger M.C., Hohlweg-Majert B., Schwarz U., Teschner M., Hammer B., Schmelzeisen R. Manufacturing splints for orthognathic surgery using a three-dimensional printer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e1–e7. doi: 10.1016/j.tripleo.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 13.Uribe F., Janakiraman N., Shafer D., Nanda R. Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: surgery first approach. Am J Orthod Dentofacial Orthop. 2013;144:748–758. doi: 10.1016/j.ajodo.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 14.Scolozz P., Herzog G. Total mandibular subapical osteotomy and Le Fort I osteotomy using piezosurgery and computer-aided designed and manufactured surgical splints: a favorable combination of three techniques in the management of severe mouth asymmetry in Parry-Romberg syndrome. J Oral Maxillofac Surg. 2014;72:991–999. doi: 10.1016/j.joms.2013.09.044. [DOI] [PubMed] [Google Scholar]
- 15.Vale F., Scherzberg J., Cavaleiro J., Sanz D., Caramelo F., Maló L. 3D virtual planning in orthognathic surgery and CAD/CAM surgical splints generation in one patient with craniofacial microsomia: a case report. Dental Press J Orthod. 2016;21:89–100. doi: 10.1590/2177-6709.21.1.089-100.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahan S., Le Gall M., Julié D., Salvadori A. New protocols for the manufacture of surgical splints in surgical-orthodontic treatment. Int Orthod. 2011;9:42–62. doi: 10.1016/j.ortho.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Aboul-Hosn Centenero S., Hernández-Alfaro F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results - our experience in 16 cases. J Craniomaxillofac Surg. 2012;40:162–168. doi: 10.1016/j.jcms.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 18.Shqaidef A., Ayoub A.F., Khambay B.S. How accurate are rapid prototyped (RP) final orthognathic surgical wafers? A pilot study. Br J Oral Maxillofac Surg. 2014;52:609–614. doi: 10.1016/j.bjoms.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 19.Hernández-Alfaro F., Guijarro-Martínez R. New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: an in vitro and in vivo study. Int J Oral Maxillofac Surg. 2013;42:1547–1556. doi: 10.1016/j.ijom.2013.03.025. [DOI] [PubMed] [Google Scholar]
- 20.Schouman T., Rouch P., Imholz B., Fasel J., Courvoisier D., Scolozzi P. Accuracy evaluation of CAD/CAM generated splints in orthognathic surgery: a cadaveric study. Head Face Med. 2015;11:24. doi: 10.1186/s13005-015-0082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ying B., Ye N., Jiang Y., Liu Y., Hu J., Zhu S. Correction of facial asymmetry associated with vertical maxillary excess and mandibular prognathism by combined orthognathic surgery and guiding templates and splints fabricated by rapid prototyping technique. Int J Oral Maxillofac Surg. 2015;44:1330–1336. doi: 10.1016/j.ijom.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Song K.G., Baek S.H. Comparison of the accuracy of the three-dimensional virtual method and the conventional manual method for model surgery and intermediate wafer fabrication. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:13–21. doi: 10.1016/j.tripleo.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Kim B.C., Lee C.E., Park W., Kim M.K., Zhengguo P., Yu H.S. Clinical experiences of digital model surgery and the rapid-prototyped wafer for maxillary orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:278–285. doi: 10.1016/j.tripleo.2010.04.038. e1. [DOI] [PubMed] [Google Scholar]
- 24.Lonic D., Pai B.C., Yamaguchi K., Chortrakarnkij P., Lin H.H., Lo L.J. Computer-assisted orthognathic surgery for patients with cleft lip/palate: from traditional planning to three-dimensional surgical simulation. PLoS One. 2016;11 doi: 10.1371/journal.pone.0152014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho C.T., Lin H.H., Liou E.J., Lo L.J. Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: a qualitative and quantitative study. Sci Rep. 2017;10:40423. doi: 10.1038/srep40423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang H.W., Lin H.H., Chortrakarnkij P., Kim S.G., Lo L.J. Intraoperative navigation for single-splint two-jaw orthognathic surgery: from model to actual surgery. J Craniomaxillofac Surg. 2015;43:1119–1126. doi: 10.1016/j.jcms.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Lin H.H., Chang H.W., Lo L.J. Development of customized positioning guides using computer aided design and manufacturing technology for orthognathic surgery. Int J Comput Assist Radiol Surg. 2015;10:2021–2033. doi: 10.1007/s11548-015-1223-0. [DOI] [PubMed] [Google Scholar]
- 28.Bholsithi W., Tharanon W., Chintakanon K., Komolpis R., Sinthanayothin C. 3D vs. 2D cephalometric analysis comparisons with repeated measurements from 20 Thai males and 20 Thai females. Biomed Imaging Interv J. 2009;5:e21. doi: 10.2349/biij.5.4.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oh S., Kim C.Y., Hong J. A comparative study between data obtained from conventional lateral cephalometry and reconstructed three-dimensional computed tomography images. J Korean Assoc Oral Maxillofac Surg. 2014;40:123–129. doi: 10.5125/jkaoms.2014.40.3.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin H.H., Chiang W.C., Lo L.J., Hsu S.P., Wang C.H., Wan S.Y. Artifact-resistant superimposition of digital dental models and cone-beam computed tomography images. J Oral Maxillofac Surg. 2013;71:1933–1947. doi: 10.1016/j.joms.2013.06.199. [DOI] [PubMed] [Google Scholar]
- 31.Yu C.C., Bergeron L., Lin C.H., Chu Y.M., Chen Y.R. Single-splint technique in orthognathic surgery: intraoperative checkpoints to control facial symmetry. Plast Reconstr Surg. 2009;124:879–886. doi: 10.1097/PRS.0b013e3181b03842. [DOI] [PubMed] [Google Scholar]