Abstract
Introduction
Public health achievements throughout the last century have resulted in a steady increase in life expectancy. An emergent subset has distinguished themselves, living well beyond the ninth decade by avoiding or delaying the onset of most age-related diseases, including bone diseases and fractures. In this study, we evaluated the bone health of the oldest community-dwelling individuals living in rural Arkansas.
Methods
299 patients aged ≥90 years were retrospectively reviewed for recorded fractures within 12 years prior to the investigation period. Records were also examined for medications and test results pertinent to bone health, including thyroid stimulating hormone, vitamin D levels, hematocrit, hemoglobin, body mass index, and bone densitometric values.
Results
68 patients (23%) had at least one fracture documented, and 15 had >1 fracture. 40% of patients with fractures had osteoporosis and 28% had osteopenia, respectively. 232 patients (78%) had no documented fractures, and of these, only 18% had osteoporosis and 16% had osteopenia. No significant clinical markers were found among the very old to explain the relatively low occurrence of fractures.
Conclusions
Patients over 90 years of age had an overall low prevalence of fractures and relative preservation of bone health, suggesting a preserved bone molecular profile in these individuals. Epigenetic factors and activity levels might also have favorably affected bone health. The low percentage of osteoporosis and fractures likely reduced the morbidity and mortality in this population, potentially contributing to their overall longevity.
Keywords: longevity, bone health, aging, osteoporosis
Introduction
Public health achievements throughout the last century have resulted in a steady increase in life expectancy for the average American. The risk of dying between the ages of 60 and 80 years has been decreasing each year by 1.7% and 1.5% for women and men, respectively.1 Improvements in technology, safety measures, education, and healthcare availability have resulted in an approximate 30-year increase in life expectancy over the course of the last century.2 From 2016 to 2040, life expectancy is predicted to rise a further 4.4 years for both men and women.3 As of 2018, the average life expectancy in the United States was 78.6 years.4,5 As life expectancy has increased, the leading causes of death among Americans have changed to reflect changes in healthcare and socioeconomic conditions.3,6 Non-communicable diseases, such as cardiovascular disease and cancer, are currently the leading causes of death for Americans.4 Additionally, a subset of the world’s population has emerged, avoiding or delaying the onset of these age-related diseases and further distinguishing themselves by living beyond 100 years of age.
As a demographic group, those ≥100 years of age have been approximately doubling in number over the last few decades.7.These very elderly individuals tend to display exceptional health throughout their life before experiencing a sudden rapid decline at the end.8,9 The certified causes of death among this demographic group are most likely to be associated with “acute decline” due to frailty and pneumonia, conditions which are often the result of hospitalization.10,11 It is the unique ability of these very old to defer experiencing debilitating health issues until their 80s and 90s, which make them an important population to study for further understanding the aging process.12
Certain comorbid conditions occur more frequently with aging, including dementia, cardiovascular disease, cancers, and an increased risk of fractures due to declining bone health. Beginning around the fifth decade of life, maintaining bone health becomes a major health concern due to an increased risk of developing osteoporosis and hence an increased risk of fractures.13 Osteoporosis is characterized by loss of bone density due to deterioration of bone tissue, which is a result of biological changes related to aging. This architectural change in bone tissue results in an increased risk of fractures. Among the elderly population, particularly individuals ≥100 years old, hip fracture is the leading cause of hospitalization and is often accompanied by a high mortality rate.14,15 The hip fracture incidence among this group of very old is 23 per 1000 individuals per year.14,16 Females 85 years of age and older are ∼19 times more likely to sustain a hip fracture than their 65 to 69-year-old counterparts, while men of the same age are approximately 33 times more likely.17 Fracture risk has been shown to have a positive correlation with age in both women and men.18,19
The oldest of the old population’s ability to deter morbid health outcomes may be the result of superior environmental conditions, lifestyle choices, socioeconomic status, physicality, hormonal and nutritional factors, and/or epigenetics. By using the ≥90-year-old population as a study cohort, we can strive to identify which, if any, of these factors contribute to the longevity of this population. This study will use bone health as a specific marker for aging as it is a significant comorbidity in this population and is one of the leading contributors to functional impairment and mortality in those with exceptional longevity.
Material and Methods
Institutional Review Board approval was obtained for this retrospective study. Patients were identified via a data warehouse search for electronic medical record (EMR) at the University of Arkansas for Medical Sciences (UAMS). Patient records were included if they were over 90 years of age and had been seen at the Thomas and Lyon Longevity Clinic or hospitalized at UAMS between January 2011 and December 2013. Patient ages were determined by their last documented encounter with a healthcare provider through UAMS.
After removal of duplicates and incomplete records, 299 charts were available for review. Demographic data were collected on gender, race, ethnicity, and age, as well as most recent body mass index (BMI) measurements. Due to the retrospective nature of this study, information on study subjects was limited to information provided in their charts.
All imaging documentation and outside records were reviewed for notation of previous and/or existing fractures up to 12 years prior to the investigation period. In all instances, imaging had been obtained on the patients during clinic visits or hospitalization because of complaints of pain in different regions of the body, disability or evaluation of a recent fall-related injury. The documentation was reviewed for location and diagnosis of all acute and chronic fractures. 50 patients had presented to the clinic or hospital with a new fracture over the period reviewed prior to their baseline clinic visit; 18 patients presented to clinic with an old fracture with no known date of occurrence. Radiological evidence of osteoporosis and osteopenia was also noted and bone densitometry T and Z values were recorded for all patients, regardless of documented fractures or bone disease. The most recent laboratory values for thyroid stimulating hormone (TSH), calcium, vitamin D, hemoglobin, and hematocrit levels were also recorded.
Patient medication lists from the most recent visit to UAMS were evaluated for medications that are commonly associated with an increased or decreased risk for fractures. Major medication categories that reduced fracture risk included beta blockers, angiotensin receptor blockers, angiotensin-converting enzyme inhibitors, thiazide diuretic, bisphosphates, vitamin D supplements, and calcium supplements. Drug categories that increased fracture risk included calcium channel blockers, loop diuretics, benzodiazepines, steroids, thyroid, and epileptic medications.20
A standard T test was performed to compare data from patients with documented fractures to those without documented fractures. If the dataset was too small, a non-parametric Mann–Whitney U test was performed instead. Medication prevalence among patients was compared between patients with documented factures and those without. Comparisons were also made among patients with and without documented bone disease, such as osteopenia or osteoporosis. A P-value <.05 was considered statistically significant.
Results
Of the 299 patients, 83.6% were female and 16.4% were male. The demographic characteristics of patients are detailed in Table 1. The majority of patients were between the ages of 90 and 99 years, accounting for 74.2% of the study’s population. The remaining quarter of the study’s population were over the age of 100 years. A majority of the subjects identified as Caucasian (73.9%), while 23.7% identified as Black or African American and only one identified as Hispanic. Seven subjects (2.3%) were not ethnically identified within their charts. Average BMI was 24.3 (±5.1) for the patients included in this study (Table 1). Patients with and without documented fractures had similar BMI (fracture group, 24.6 ± 3.9; non-fracture group, 24.3 ± 5.4). The calculated P-value (P = .49) indicates there was no significant difference between the groups.
Table 1.
Demographics of Study Participants Separated by Fracture/No Fracture.
| Parameter | With fractures | Without fractures | Total N (%) |
|---|---|---|---|
| Age, N (%) | |||
| 90–99 | 46 (67.6) | 176 (76.2) | 222(74.2) |
| ≥100 | 22 (32.4) | 55 (23.8) | 77 (25.8) |
| Gender, N (%) | |||
| Female | 59 (86.8) | 191 (82.7) | 250(83.6) |
| Male | 9 (13.2) | 40 (17.3) | 49(16.4) |
| Race, N (%) | |||
| Caucasian | 48 (70.6) | 172 (74.4) | 220(73.6) |
| African American | 20 (29.4) | 51 (22.1) | 71 (23.7) |
| Hispanic or Latino | 0 (0.0) | 1 (0.43) | 1 (0.33) |
| Unknown | 0 (0.0) | 7 (3.03) | 7 (2.34) |
| BMI | |||
| Mean ± SD | 24.6 ± 3.9 | 24.2 ± 5.4 | 24.3 ± 5.1 |
BMI, body mass index.
A total of 92 separate fractures were identified in our cohort of 299 patients. 68 patients were noted to have at least one fracture, accounting for 22.7% of our study’s population. This resulted in a fracture incidence rate of 1.9% per year in our elderly subjects. Table 2 details the distribution of fractures by location. The most common location for fractures was the spine, followed by hip and femur. 40.3% of those with at least one fracture were also noted to have an osteoporosis diagnosis. A further 28.4% had a diagnosis of osteopenia in addition to their documented fracture. Only 31.3% of those with a documented fracture had no additional bone health diagnosis.
Table 2.
Distribution of Fractures Among the Oldest of the Old. A Total of 68 Patients had One or More Fractures Recorded.
| Location | N | % |
|---|---|---|
| Spine | 21 | 22.8 |
| Hip | 18 | 19.5 |
| Femur | 17 | 18.5 |
| Humerus | 11 | 11.9 |
| Ribs | 9 | 9.8 |
| Clavicle | 4 | 4.3 |
| Ankle | 3 | 3.3 |
| Radius | 2 | 2.2 |
| Facial | 2 | 2.2 |
| Ulna | 2 | 2.2 |
| Elbow | 1 | 1.1 |
| Toe | 1 | 1.1 |
| Finger | 1 | 1.1 |
| Total | 92 | 100 |
232 patients (77.6%) had no fractures documented in their medical records. 80 participants (26.8% of the study population) who had no documented fractures did have diagnoses of osteopenia or osteoporosis. The remaining 152 study participants with no documented fractures (50.8% of the study population) also did not have any diagnosis of bone disease (Figure 1). In addition to bone health diagnoses, bone densitometry values were reviewed for insight into bone health for this study population. Table 3 shows the P-values of for each bone densitometry location between patients with and without fractures. Interestingly, there were no significant differences between the t-scores of patients with fractures as compared to those without.
Figure 1.
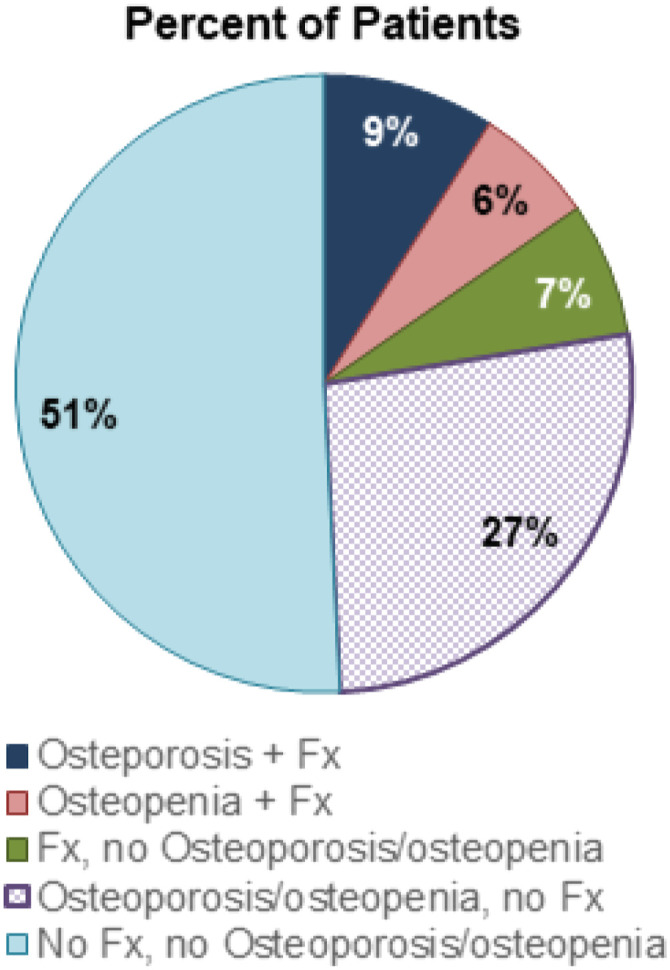
Correlation between incidence of fractures (Fx) and diagnosis of osteoporosis or osteopenia based on imaging.
Table 3.
Various Health Factors Contributable to Bone Health. Bone Density Measurements are Included for Available Dexa Scans. No Significant Difference was Found Between those with Fractures and those without at any of the Measurement Locations or Among the Blood Chemistry Measures.
| Parameter | With fracturemean ± SD | Without fracturemean ± SD | P-value |
|---|---|---|---|
| Densitometry location | |||
| Radial diaphysis | −3.7 (±0.9) | −2.8 (±1.6) | 0.171 |
| Ultradistal radius | −3.0 (±1.2) | −2.5 (±1.3) | 0.347 |
| L1-4 | −2.6 (±1.6) | −2.2 (±1.6) | 0.596 |
| Volumetric lumbar | −4.2 (±1.1) | −3.6 (±1.3) | 0.438 |
| Femoral neck | −2.9 (±1.0) | −2.3 (±0.8) | 0.226 |
| Femoral trochanter | −2.9 (±1.0) | −2.3 (±0.8) | 0.184 |
| Total proximal femur | −1.3 (±2.1) | −1.8 (±1.3) | 0.575 |
| Blood chemistry values | |||
| Calcium | 8.7 (±0.7) | 8.8 (±0.9) | 0.201 |
| TSH | 1.4 (±3.8) | 2.2 (±3.4) | 0.484 |
| Vitamin D | 32.0 (±16.1) | 33.1 (±13.1) | 0.569 |
| Hemoglobin | 11.4 (±1.7) | 11.7 (±2.0) | 0.174 |
| Hematocrit | 35.8 (±5.0) | 36.0 (±5.8) | 0.569 |
TSH, thyroid-stimulating hormone.
Table 3 also details the blood chemistry values of study participants with and without documented fractures. P-values indicate that TSH (1.4 ± 3.8 vs 2.2 ± 3.4), calcium (8.7 ± 0.7 vs 8.8 ± 0.9), vitamin D (32.0 ± 16.1 vs 33.1 ± 13.1), hematocrit (35.8 ± 5.0 vs 36.0 ± 5.8), and hemoglobin (11.4 ± 1.7 vs 11.7 ± 2.0) levels were not significantly different between individuals with documented fractures and those without documented fractures.
Of the 68 participants with fractures, 16.4% were taking medications that might induce osteoporosis, while 26.9% had prescriptions known to prevent osteoporosis development (Table 4). 30% of these participants were prescribed both osteoporosis-inducing and osteoporosis-preventative medications. Among the 232 participants without documented fractures, 12.5% were taking prescriptions known to induce osteoporosis, while 24.1% were taking osteoporosis-preventative medications. 25.9% of the non-fracture participants were prescribed both osteoporosis-inducing and osteoporosis-preventative medications. Of the 125 participants diagnosed with osteopenia or osteoporosis, 12% were prescribed only osteoporosis-inducing medications (Table 5). Furthermore, 31.2% of participants were taking only osteoporosis-preventative medications, while 30.4% were on a combination of these medication categories.
Table 4.
Distribution of Medication and its Correlation with Fracture Incidence. Medications are Categorized Based on their Effect on Bone, Including Medications that Increase Risk of Developing Osteoporosis and those that Act as Preventative Medications.
| Parameter | Fracture | No fractures | Total N (%) |
|---|---|---|---|
| Types of medications prescribed | |||
| Medications that induce bone loss N (%) | 11 (27.5) | 29 (72.5) | 40 (13.4) |
| Medications that prevent bone loss N (%) | 18 (24.3) | 56 (75.7) | 74 (24.7) |
| Both types N (%) | 20 (25.0) | 60 (75.0) | 80 (26.8) |
| Neither type N (%) | 18 (17.1) | 87 (82.9) | 105 (35.1) |
Table 5.
Distribution of Medication and its Effect on Bone Health Outcomes. Medications are Categorized Based on its Effect on Bones, Including Medications that Increase Risk of Developing Osteoporosis and those that act as Preventative Medications.
| Parameter | Osteoporosis or osteopenia diagnosis | No diagnosis | Total N (%) |
|---|---|---|---|
| Types of medications prescribed | |||
| Medications that induce bone loss N (%) | 15 (37.5) | 25 (62.5) | 40 (13.4) |
| Medications that prevent bone loss N (%) | 39 (53.4) | 34 (46.6) | 73 (24.4) |
| Both types N (%) | 38 (47.5) | 42 (52.5) | 80 (26.8) |
| Neither type N (%) | 33 (31.1) | 73 (68.9) | 106 (35.4) |
There were 174 participants who were not diagnosed with osteopenia or osteoporosis. 42% had either no medications listed in their medical file or had medications prescribed that were not known to affect their bone health. 14.4% of the participants without osteopenia or osteoporosis were taking osteoporosis-inducing medications, while 19.5% were prescribed osteoporosis-preventative drugs.
Discussion
The goal of this study was to investigate whether various aspects of bone health among the very elderly could provide insight into the aging process in this unique population. Our study investigated the prominence of fractures, osteopenia, and osteoporosis among our study population and made comparative analyses specifically looking at metabolic values and blood indices characteristic of bone health as well as the impact of prescribed medication therapies.
Overall, we found a low rate of fractures in our group of patients over 90 years of age. The distribution of fractures found in our study correlates with the expected distribution of fractures for an elderly cohort, with the most common occurring at the spine and hip, and the third and fourth most common being humeral and radial fractures.21 Additionally, there was a trend toward lower incidence of fracture among the oldest Arkansans, as compared to the general very old population in the United States. The incidence for hip fractures in the ≥100-year-old population has been estimated to be 23.1 per 1000 individuals per year (2.3% per year), whereas our study found a fracture incidence of 1.9% per year among our population of very elderly individuals.14 This indicates that our population of nonagenarian and older Arkansans may have characteristics that contributed to the preservation of bone health even into extreme old age.
Fracture risk has been shown to increase in osteoporotic individuals. Osteoporosis prevalence in the ≥90 -year-old population was determined to be 64% in women and 27% in men, while in those over 100 years of age have a slightly increased prevalence at 72% and 28% in women and men, respectively.18,22 The overall incidence of osteoporosis in our study’s population was 40.4%, with 88.8% in women and 11.2% occurring in men. Lower bone mineral density (BMD) is indicative of structural deficiencies in the bone, and the more severe the osteoporosis, the greater the risk of fracture.23,24 This is supported by the fracture group in our study bearing the burden of osteoporosis and osteopenia, with nearly 70% of this group having been diagnosed with one or the other. Only 27% of the non-fracture group had been diagnosed with either osteoporosis or osteopenia. However, while studies have shown that lower BMD, when serving as a measurement for the severity of osteoporosis, does indicate an increased risk for fractures, neither BMD nor a diagnosis of osteoporosis the only factors that increase fracture risk.18,23,24
We found no significant difference in calcium, vitamin D, or TSH levels between subjects with fractures compared to those without. This indicates that while these values may play a significant role in maintaining bone health in the aging population, in the very elderly, there does not appear to be a correlation between fracture occurrence and these nutritional and hormonal factors.25,26 This could also indicate that there may be additional factors contributing to these exceptional individuals’ longevity in bone health. However, it should also be noted that the normal laboratory ranges for the elderly, and especially for nonagenarians and centenarians, have yet to be determined.
In our study population, we found that a majority of both cohorts were not prescribed osteoporosis-inducing medications. Only 17% of those within the fracture cohort and 12% of those within the non-fracture cohort had a documented prescription for medications considered osteoporosis-inducing. While patients with fractures had a higher percentage of osteoporosis-inducing medications, they were also taking a higher percentage of osteoporosis-preventative medications. Both groups were prescribed a mixture of preventative and inducing medications at similar rates. This indicates that patients with fractures were slightly more likely to be consuming some form of bone-affecting medication of any type compared to individuals who did not have documented fractures. Thus, those with fractures were likely to be experiencing other medical conditions requiring medical intervention, were more likely to seek out medical attention, or had medical care more readily available.
A significant number of medications prescribed to the oldest of old may influence bone health by inducing bone loss or bone formation. One of the most common drug classes used by patients 90 years old and older are medications related to heart failure and hypertension, more than half of which are loop diuretics or thiazide diuretics. Such medications may contribute to an increased risk of fractures.27-29 Additionally, this population is often less likely to be prescribed ACE inhibitors or beta blockers, even though they may be protective against fractures.27-29 Hence, prescribing trends may be a contributing factor in the development of fractures among the individuals in this age demographic.
This study focused on individuals ≥90 years old living in Arkansas. Despite Arkansas being ranked 48th on the America’s Health Rankings 2019 Annual Report produced by the United Health Foundation, we have a thriving population of very elderly individuals.30 Furthermore, in this unique population of very elderly, bone health appears to be similar to that reported by other parts of the country. According to the 2010 United States Census, people 90–99 years of age made up 0.59% of the Arkansas population, which is equal to the national average for this age group. However, for people 100 years and over, Arkansas has the distinction of having 1.99 centenarians per 10,000 people, which is above the national average of 1.73 per 10,000 people.31 The state was ranked 18th for its population percentage of those 100 years old and older as of 2010, not including Puerto Rico.31
Our study found no significant difference in BMI between those that experienced fractures and those that did not; however, the small size of our study population restricted our ability to look specifically at correlations with fracture sites. BMI has also been noted to play a role in increased fracture risk. Multiple studies have found an inverse relationship between BMI and fracture risk in the hip, spine, and wrist, while Compston et al. (2017) found the risk for ankle fractures had a positive correlation with BMI.16,18,19,32 The inverse relationship between BMI and fracture risk appears to be at its most notable in thin, Caucasian, post-menopausal women.18,33 A number of factors separately contribute to this relationship, including Caucasian ethnicity and post-menopausal status, as well as low muscle mass and the subsequent development of sarcopenia.18,33,34 Furthermore, our population was predominantly Caucasian women, restricting our ability to develop any meaningful conclusions about ethnicity and gender other than further supporting the well-known effect of gender on longevity.18,33
This study, being retrospective in nature, presents us with various limitations including missing data. It is possible that some radiological studies, although indicated, were not done because of patients’ advanced age or other reasons. Furthermore, retrospective collection of fracture data could miss minor fractures. There was also lack of information about diet, lifestyle choices, and activity level. These missing factors could have provided further insight about bone health in this unique population. Additionally, our study included a select group of patients that sought clinical care at a facility that encouraged health monitoring and education provided in a comprehensive geriatric setting. It is possible that these patients are healthier than other groups of 90-year-old patients who do not have access to a clinic that specializes in aging.
Conclusion
This study investigated potential markers of bone health in those over 90 years of age in the South Central United States. Our population of the oldest of old patients in Arkansas appeared to have no significant differences or obvious bone health predictors between those with or without fractures documented in their medical history. Furthermore, medications that have previously been implicated in changes in bone health did not appear to have any significant influence on fracture rates. However, very elderly Arkansans do appear to meet or exceed the average bone health expected of those in their age group, showing a trend toward lower fracture incidence as compared to other studies.
Acknowledgments
We thank Codi English for help with manuscript preparation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partly supported by PHS# AG028718.
ORCID iD
Simon C. Mears https://orcid.org/0000-0002-0068-0283
References
- 1.Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. The Lancet. 2015;385(9967):540-548. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) . Ten great public health achievements--United States, 2001-2010. MMWR. Morbidity and mortality weekly report. 2011;60(19):619-623. [PubMed] [Google Scholar]
- 3.Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. The Lancet. 2018;392(10159):2052-2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017. NCHS Data Brief, no 328. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 5.Arias E, Xu J, Kochanek KD. United States life tables, 2016. Natl Vital Stat Rep. 2019:68(4):1-66, 31112121. [PubMed] [Google Scholar]
- 6.Xu J, Murphy S, Kochanek K, Elizabeth A. Mortality in the United States, 2015. NCHS Data Brief. No. 267. Hyattsville, MD: National Center for Health Statistics; 2016. [Google Scholar]
- 7.Robine JM, Cubaynes S. Worldwide demography of centenarians. Mechanisms of Ageing and Development. 2017;165:59-67. [DOI] [PubMed] [Google Scholar]
- 8.Milman S, Barzilai N. Dissecting the mechanisms underlying unusually successful human health span and life span. Cold Spring Harbor perspectives in medicine. 2016;6(1):a025098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mosfeldt M, Madsen CM, Lauritzen JB, Jørgensen HL. Centenarian hip fracture patients: A nationwide population-based cohort study of 507 patients. Actaorthopaedica. 2019;90(4):342-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doblhammer G, Barth A. Prevalence of morbidity at extreme old age in Germany: An observational study using health claims data. Journal of the American Geriatrics Society. 2018;66(7):1262-1268. [DOI] [PubMed] [Google Scholar]
- 11.Evans CJ, Ho Y, Daveson BA, Hall S, Higginson IJ, Gao W. Place and cause of death in centenarians: A population-based observational study in England, 2001 to 2010. PLoS medicine. 2014;11(6):e1001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sebastiani P, Perls TT. The genetics of extreme longevity: Lessons from the new England centenarian study. Frontiers in genetics. 2012;3:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazzola P, Rea F, Merlino L, Bellelli G, Dubner L, Corrao G, et al. Hip fracture surgery and survival in centenarians. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2016;71(11):1514-1518. [DOI] [PubMed] [Google Scholar]
- 15.Moore J, Carmody O, Carey B, Harty JA, Reidy D. The cost and mortality of hip fractures in centenarians. Irish Journal of Medical Science. 2017;186(4):961-964. [DOI] [PubMed] [Google Scholar]
- 16.Aurégan JC, Frison A, Bégué T, Hannouche D, Bosser C, Bensidhoum M, et al. Contra-lateral hip fracture in the elderly: Are decreased body mass index and skin thickness predictive factors? International orthopaedics. 2017;41(2):247-252. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan KJ, Husak LE, Altebarmakian M, Brox WT. Demographic factors in hip fracture incidence and mortality rates in California, 2000–2011. Journal of orthopaedic surgery and research. 2016;11(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Silva AP, Matos A, Ribeiro R, Gil Â, Valente A, Bicho M, et al. Sarcopenia and osteoporosis in Portuguese centenarians. European journal of clinical nutrition. 2017;71(1):56-63. [DOI] [PubMed] [Google Scholar]
- 19.Alonso AC, Goncalves TA, Almeida JK, Machado-Lima A, Ernandes RD, Greve JMDA, et al. Relationship between bone mineral density and body composition in elderly. Actaortopedicabrasileira. 2018;26(1):27-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ilić K, Obradović N, Vujasinović-Stupar N. The relationship among hypertension, antihypertensive medications, and osteoporosis: A narrative review. Calcified tissue international. 2013;92(3):217-227. [DOI] [PubMed] [Google Scholar]
- 21.Southerland LT, Barrie M, Falk J, Menaker J. Fractures in older adults. Emergency Medicine Reports. 2014;35(11):1-13. [Google Scholar]
- 22.Poggiogalle E, Cherry KE, Su LJ, Kim S, Myers L, Welsh DA, et al. Body composition, IGF1 status, and physical functionality in nonagenarians: Implications for osteosarcopenia. Journal of the American Medical Directors Association. 2019;20(1):70-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unnanuntana A, Gladnick BP, Donnelly E, Lane JM. The assessment of fracture risk. The Journal of Bone and Joint Surgery. American volume. 2010;92(3):743-753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomasevic-Todorovic S, Vazic A, Issaka A, Hanna F. Comparative assessment of fracture risk among osteoporosis and osteopenia patients: A cross-sectional study. Open access rheumatology: research and reviews. 2018;10:61-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Azhar G, Abraham RR, Girotra M, Wei JY, Foster SR, Schrader AM. A study of metabolic health in very old individuals residing in central Arkansas. Aging Sci 2015;3:136. [Google Scholar]
- 26.Madrigal-Leer F, Martìnez-Montandòn A, Solìs-Umaña M, Helo-Guzmàn F, Alfaro-Salas K, Barrientos-Calvo I, et al. Clinical, functional, mental and social profile of the Nicoya Peninsula centenarians, Costa Rica, 2017. Aging ClinExp Res. 2020;32:313-321. [DOI] [PubMed] [Google Scholar]
- 27.Hawthorne JL, Warford LJ, Hutchison LC, Pangle AK, Price ET, Wei JY, et al. Prescription medication use in the oldest old of south-central United States. American Research Journal of Geriatrics and Aging 2017;1(1):1-10. [Google Scholar]
- 28.Emeny RT, Chang CH, Skinner J, O’Malley AJ, Smith J, Chakraborti G, et al. Association of receiving multiple, concurrent fracture-associated drugs with hip fracture risk. JAMA network open. 2019;2(11):e1915348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmidt IM, Kreutz R, Dräger D, Zwillich C, Hörter S, Kuhlmey A, et al. Lower prescription rates in centenarians with heart failure and heart failure and kidney disease combined: Findings from a longitudinal cohort study of very old patients. Drugs & Aging. 2018;35(10):907-916. [DOI] [PubMed] [Google Scholar]
- 30.United Health Foundation; American Public Health Association . America's Health Rankings Annual Report, 2019 Edition. Minnetonka, MN: United Health Foundation; 2019. [Google Scholar]
- 31.Meyer J. U.S. Census Bureau, 2010 Census Special Reports, Centenarians: 2010, C2010SR-3. Washington, DC: U.S. Government Printing Office; 2012. [Google Scholar]
- 32.Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Gregson C, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Archives of osteoporosis. 2017;12(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, et al. Major osteoporotic fragility fractures: Risk factor updates and societal impact. World journal of orthopedics. 2016;7(3):171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Locquet M, Beaudart C, Bruyère O, Kanis JA, Delandsheere L, Reginster JY. Bone health assessment in older people with or without muscle health impairment. Osteoporosis International. 2018;29(5):1057-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]


