Abstract
Objectives:
Occult spinal dysraphism is a congenital failure of fusion of the posterior vertebral arches with intact skin overlying the defect. Lumbosacral cutaneous manifestations are associated with a variable risk of occult spinal dysraphism. Tethered cord syndrome is a type of occult spinal dysraphism that puts abnormal traction on the spinal cord. This study analyzed neonates and infants who were referred to our pediatric urology practice and had evidence of lumbosacral cutaneous manifestation on physical examination.
Methods:
We reviewed the presence of lumbosacral cutaneous manifestations in neonates and infants evaluated in our pediatric urology clinic at our Institution over a 6-year period (1 March, 2015–28 February, 2021) with no prior diagnosis of lumbosacral cutaneous manifestation. All patients underwent a spinal ultrasound.
Results:
The most common lumbosacral cutaneous manifestations were bifurcated/duplicated gluteal folds (33%), gluteal asymmetry (19%), and sacral dimples (14%). A total of 34 (24%) patients had an abnormal spinal ultrasound; 15 (44%) of these infants underwent a lumbar magnetic resonance imaging. A coccygeal pit was statistically marginally higher in abnormal versus normal spinal ultrasound (p = 0.07). Patients with only one lumbosacral cutaneous manifestation (N = 121) were significantly more likely to have a normal spinal ultrasound compared to those with two or more lumbosacral cutaneous manifestation (N = 17) (79% vs 53%, p = 0.03).
Conclusion:
Due to the varying risk of certain lumbosacral cutaneous manifestations with occult spinal dysraphism, all patients with a lumbosacral cutaneous manifestation should undergo spinal ultrasound. This study also highlights the importance of urodynamic studies when there are abnormal cutaneous findings. Routine physical examinations of the lumbar region for cutaneous manifestations of occult spinal dysraphism are vital to ensure prompt management of tethered cord syndrome and avoid potentially devastating consequences.
Keywords: Pediatrics, pediatric urology, cutaneous, occult spinal dysraphism, ultrasound
Introduction
Spinal dysraphism refers to a group of congenital spinal anomalies resulting from incomplete closure of the neural tube early in fetal life.1 The incidence of spinal dysraphism is 0.5–0.8 cases per 1000 live births.1 An occult spinal dysraphism (OSD) is covered by normal or near-normal skin, usually delaying diagnosis of OSDs compared with the more obvious open spinal defects. In children with OSDs, lumbosacral cutaneous manifestations (LsCMs) are observed in 51%–100% patients.1–5
One type of OSD, tethered cord syndrome (TCS), may lead to neurological, gastrointestinal, musculoskeletal, and urinary dysfunction due to spinal cord traction.6–9 Timely diagnosis and treatment of TCS may mitigate the devastating sequelae that may ensue. A controversy exists as to the association between certain LsCMs and the risk of OSD.2 Studies generally concur that an infant with >1 LsCM increases the likelihood of OSD.3,10–12
We previously reported a 3 ½-year study (1 March 2015–30 September 2018) of 67 infants with at least one LsCM who were evaluated in our pediatric urology clinic.13 The most common LsCMs were duplicated or bifurcated gluteal folds (46%) and gluteal asymmetry (16%).
The current 6-year study expands upon our previous study by increasing the number of patients and statistically analyzing which LsCMs may be higher risk for OSD. We also present the criteria utilized to refer patients for neurosurgical evaluation, perform further testing such as lumbar magnetic resonance imaging (MRI) and urodynamic studies (UDS), and undergo a tethered cord release (TCR).
Materials and methods
Under an Institutional Review Board–approved protocol, we retrospectively reviewed the presence of LsCMs in all neonates and infants evaluated in our pediatric urology clinic at our Institution over a 6-year period (1 March 2015–28 February 2021). As our study focused on observational data, our sample size was comprised of the entire available population who qualified for the inclusion criteria set forth in our study. The calculation and justification of the sample size selected in this study were as follows: at alpha = 0.05, power = 0.8, and 34/141 (24.11%) abnormal spinal ultrasounds (US), we would have been able to detect an effect size of 15.5%. Alternatively, we would have been able to detect an effect size of 15.7% if the three patients whose spinal US were too limited to interpret (34/138 (24.64%) were excluded. The inclusion criteria consisted of all neonates and infants who were evaluated by their pediatrician and subsequently referred to our office for a urological concern unrelated to OSD. The inclusion criteria were comprised of neonates and infants who had not been diagnosed with OSD prior to the pediatric urological evaluation, and the LsCM was first noted in the medical record on routine physical examination by the pediatric urologist. The exclusion criteria included patients who had been previously diagnosed with an LsCM either at birth or by their pediatrician before referral to our pediatric urology office. In addition, the exclusion criteria also encompassed neonates and infants who had any symptoms suggestive of neurogenic bladder dysfunction.
All infants with an LsCM were referred for a spinal US. The determination of an abnormal US was based on either a conus medullaris (CM) that terminated at or below the L2-3 intervertebral disk level or an echogenic filum terminale (FT). As an US does not image the entire spine and instead uses the lowest “lumbar-looking” vertebrae as L5, the US can miscount the vertebral levels. The US can both falsely find a low conus that is actually within normal limits as well as by mislabeling a low conus as normal. All patients with an abnormal spinal US were referred to a pediatric neurosurgeon who determined whether a lumbar MRI would be performed. UDS were conducted in certain infants when clinically indicated, whether or not the lumbar MRI revealed abnormal findings suspicious for TCS. A pediatric radiologist reviewed all of the spinal US and lumbar MRIs.
Statistical analysis
Differences between gender, reasons for pediatric visit, and LsCM percentages were compared between normal and abnormal spinal US using the Fisher’s exact test, while the non-normally distributed ages at the 1st visit and spinal US were compared using the Mann–Whitney U-test. Multiple logistic regression evaluated the relationship between having only one LsCM versus two or more abnormalities on the spinal US while adjusting for age and other variables if the model fit indicated an average improvement in Somers’ D across 100 cross-validations. R (4.0.0) statistical software performed the analysis using basic commands along with the rms package to perform the logistic regression and cross-validations.
Results
Patient demographics and reason for pediatric urological referral
Of the 141 infants who had at least one LsCM observed by the pediatric urologist, 128 (91%) were male and 13 (9%) were female with a mean age of 5.6 weeks at the initial pediatric urology evaluation (Tables 1–3). The most common reasons for a pediatric urology consultation were circumcision, hypospadias, and hydronephrosis (Table 1).
Table 1.
Characteristics of patients with cutaneous findings suggestive of occult spinal dysraphism in our pediatric urology clinic at our institution (1 March 2015–28 February 2021).
| Patient characteristics | Number of patients (N = 141) |
|---|---|
| Gender | |
| Male | 128 (91%) |
| Female | 13 (9%) |
| Mean age at pediatric urology evaluation | 5.6 weeks (1 day–20 weeks) |
| Reason for pediatric urology evaluation | |
| Circumcision | 64 (45%) |
| Hydronephrosis | 23 (16%) |
| Hypospadias | 23 (16%) |
| Pelviectasis | 4 (3%) |
| Undescended testes | 4 (3%) |
| Hydrocele | 3 (2%) |
| Penile torsion | 2 (1%) |
| Vesicoureteral reflux | 2 (1%) |
| Micropenis | 2 (1%) |
| Other* | 9 (6%) |
| Combination** | 5 (4%) |
| Cutaneous finding | |
| Bifurcated/duplicated gluteal fold | 46 (33%) |
| Gluteal asymmetry | 27 (19%) |
| Sacral dimple | 20 (14%) |
| Lumbar hair | 14 (10%) |
| Coccygeal pit | 10 (7%) |
| Mongolian spot | 7 (5%) |
| Lumbar hemangioma | 1 (1%) |
| Combination*** | 16 (11%) |
| Mean age at spinal ultrasound | 6.0 weeks (1 day–16 weeks) |
| Spinal ultrasound findings | |
| Normal | 104 (74%) |
| Abnormal | 34 (24%) |
| Examination limited by spinal ossification | 2 (1%) |
| Examination limited by patient size and motion | 1 (1%) |
| Lumbar MRI following abnormal spinal US | 15/34 (44%) [two additional lumbar MRIs performed for patients who had normal spinal US] |
| Evaluated by neurosurgery of all patients | 25/141 (18%) |
| Evaluated by neurosurgery of patients with abnormal spinal US | 24/34 (71%) |
US: ultrasound; MRI: magnetic resonance imaging.
Other: One each of the following: ectopic kidney, horseshoe kidney, renal cysts, penile edema, periurethral cyst, redundant foreskin, scrotal hematoma, single kidney, and testicular torsion.
Combination: One each of the following: circumcision/pelviectasis, circumcision/undescended testes, hydronephrosis/circumcision, hypospadias/undescended testes, and pelviectasis/undescended testes.
Combination: Coccygeal pit/lumbar hair (3); Sacral dimple/lumbar hair (2); gluteal asymmetry/coccygeal pit (2); Duplicated gluteal fold/lumbar hair (2); One each of the following: bifurcated gluteal fold/coccygeal pit; coccygeal pit/birth mark on buttock; duplicated gluteal fold/coccygeal pit; duplicated gluteal fold/gluteal asymmetry; gluteal asymmetry/lumbar hair; coccygeal pit/Mongolian spot; duplicated gluteal fold/sacral dimple/Mongolian spot.
Table 3.
Abnormal spinal ultrasounds of patients with cutaneous findings of occult spinal dysraphism at our pediatric urology clinic at our institution (1 March 2015–28 February 2021).
| Patient characteristics | Overall N = 138* | Spinal ultrasound | p value | |
|---|---|---|---|---|
| Abnormal N = 34 | Normal N = 104 | |||
| Gender = Male | 125 (91%) | 32 (94%) | 93 (89%) | 0.52 |
| Age at 1st pediatric urology visit (median (IQR)) (weeks) | 4.6 [2.7, 7.8] | 4.9 [2.6, 9.8] | 4.4 [2.7, 7.4] | 0.40 |
| Age at spinal ultrasound (median (IQR)) (weeks) | 5.9 [3.5, 9.2] | 7.0 [2.9, 10.8] | 5.9 [4.0, 8.8] | 0.81 |
| Reason for pediatric urology visit | ||||
| Circumcision = Yes | 67 (49%) | 14 (41%) | 53 (51%) | 0.33 |
| Hydronephrosis = Yes | 24 (17%) | 7 (21%) | 17 (16%) | 0.61 |
| Hypospadias = Yes | 24 (17%) | 7 (21%) | 17 (16%) | 0.61 |
| Undescended testes = Yes | 7 (5%) | 3 (9%) | 4 (4%) | 0.36 |
| Cutaneous manifestation | ||||
| Bifurcated/duplicated gluteal fold = Yes | 52 (38%) | 11 (32%) | 41 (39%) | 0.54 |
| Gluteal asymmetry = Yes | 31 (22%) | 9 (26%) | 22 (21%) | 0.64 |
| Coccygeal pit = Yes | 18 (13%) | 8 (24%) | 10 (10%) | 0.07 |
| Sacral dimple = Yes | 23 (17%) | 5 (15%) | 18 (17%) | 1.00 |
| Lumbar hair = Yes | 22 (16%) | 5 (15%) | 17 (16%) | 1.00 |
Excludes 3 patients whose spinal ultrasounds were too limited to interpret (two due to spinal ossification and one due to patient size and motion).The bold value represents that a coccygeal pit was statistically marginally higher in abnormal versus normal spinal ultrasounds.
Cutaneous manifestations of OSD
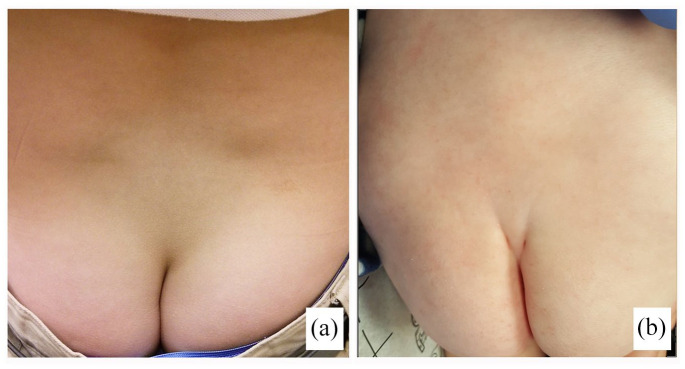
The most frequent LsCM were bifurcated/duplicated gluteal folds, gluteal asymmetry, and a sacral dimple (Tables 1 and 3; Figure 1(a) and (b)). Fifteen (11%) patients had two LsCMs, while one (1%) patient presented with three LsCMs (Table 1).
Figure 1.
(a) Gluteal asymmetry and (b) gluteal bifurcation.
Lumbar spinal US
The mean age of the infants at the time of the lumbar spinal US was 6 weeks (Table 1). The spinal US was normal in 104 (74%) cases. Of the 34 abnormal spinal US, a low-lying CM was noted in 33 (97%) patients, and an echogenic FT was observed in 1 (3%) patient. The US examination was too limited to interpret in three patients: in two due to spinal ossification and in one due to patient size and motion.
A coccygeal pit was statistically marginally higher in abnormal versus normal spine US (24% vs 10%, p = 0.07) (Table 3). Patients with only one LsCM (N = 121) were significantly more likely to have a normal spinal US compared to those with two or more LsCM (N = 17) (79% vs 53%, p = 0.03). Furthermore, patients with >1 LsCM were 3.2 (odds ratio (OR) = 3.24, 95% confidence interval (CI) = (1.14–9.23), age at US adjusted) times more likely to have an abnormal US compared to those with only one LsCM.
Lumbar MRI imaging
Of the 34 patients who had an abnormal spinal US, 15 (44%) underwent a lumbar MRI which confirmed that the CM terminated at L2-3. Two patients had a lumbar MRI despite negative findings on the spinal US. One of these patients underwent a lumbar MRI as part of a complete evaluation for abusive head trauma at the age of 5 months; there was no evidence of TCS. The correlation between the reason for pediatric urology evaluation, cutaneous findings of OSD, abnormal spinal US, lumbar MRI, and pediatric neurosurgery consultation are presented in Table 2.
Table 2.
Correlation between reason for pediatric urology evaluation, cutaneous findings suggestive of OSD, abnormal spinal US, lumbar MRI, and neurosurgery consultation at our institution (1 March 2015–28 February 2021) (n = 34).
| Gender/age at spinal US (Weeks) | Reason for urology evaluation | Cutaneous findings of OSD | Spinal US | Lumbar MRI | Neurosurgery evaluation |
|---|---|---|---|---|---|
| Male/8.29 | Hydrocele | Bifurcated gluteal fold | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT |
| Male/10.71 | Penile edema | Lumbar hair, coccygeal pit | FT appears echogenic | Not performed | None |
| Male/2.86 | Penile torsion | Gluteal asymmetry | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT; constipation |
| Male/10.86 | Hydronephrosis | Lumbar hair | CM ends at L2-3 | CM ends at L2-3, filar fibrolipoma | 2 UDS; PT; TCR |
| Male/7.57 | Hydronephrosis | Gluteal asymmetry | CM ends at L2-3 | Not performed | No clinical TCS |
| Male/8.57 | Penile torsion | Gluteal symmetry | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT |
| Male/0.29 | Undescended testes | Lumbar hair | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT; constipation |
| Male/13.29 | Hypospadias | Coccygeal pit | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT |
| Male/4.71 | Hypospadias | Duplicated gluteal fold | CM ends at L2-3 | Not performed | No clinical TCS |
| Male/0.29 | Hypospadias | Bifurcated gluteal fold, coccygeal pit | CM ends at L2-3 | Not performed | No clinical TCS; PT |
| Male/3.71 | Circumcision | Duplicated gluteal fold | CM ends at L2-3 | Not performed | No clinical TCS; PT |
| Male/3.29 | Circumcision | Gluteal aymmetry | CM ends at L2-3 | Not performed | No clinical TCS |
| Female/10.86 | Single kidney | Coccygeal pit, Mongolian spot | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; 1 UDS |
| Male/0.71 | Circumcision | Duplicated gluteal fold, coccygeal pit | CM ends at L2-3 | Not performed | No clinical TCS |
| Male/7.29 | Hydronephrosis | Gluteal asymmetry; lumbar hair | CM ends at L2-3 | Not performed | None |
| Male/11.57 | Circumcision | Duplicated gluteal fold | CM ends at L2-3 | Not performed | None |
| Male/11.0 | Hydronephrosis | Mongolian spot | CM ends at L2-3 | Not performed | No clinical TCS; PT; constipation |
| Male/3.57 | Hypospadias | Duplicated gluteal fold | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT |
| Male/12.14 | Circumcision | Gluteal asymmetry | CM ends at L2-3 | CM ends at L2-3 | No clinical TCS; PT; constipation |
| Male/1.43 | Circumcision | Sacral dimple | CM ends at L2-3 | Not performed | No clinical TCS |
| Male/8.0 | Circumcision | Coccygeal pit, birthmark buttock | CM ends at L2-3 | CM ends at L2-3 | None |
| Male/1.43 | Circumcision | Sacral dimple | CM ends at L2-3 | CM ends at inferior L2 | None |
| Male/2.29 | Hydronephrosis | Sacral dimple | CM ends at L2-3 | CM ends at superior L2 | No clinical TCS; PT |
| Male/12.57 | Hypospadias | Coccygeal pit | CM ends at L2-3 | Not performed | No clinical TCS |
| Male/3.14 | Circumcision | Duplicated gluteal fold | CM ends at L2-3 | Not performed | No clinical TCS; PT |
| Female/3.14 | Hydronephrosis | Gluteal asymmetry | CM ends at L2-3 | Not performed | No clinical TCS; PT |
| Male/6.71 | Circumcision | Coccygeal pit, lumbar hair | CM ends at L2-3 | Not performed | None |
| Male/13.0 | Circumcision | Gluteal asymmetry | CM ends at L2-3 | Not performed | None |
| Male/0.43 | Circumcision | Sacral dimple | CM ends at L2-3 | CM ends at inferior L2 | None |
| Male/9.29 | Hypospadias | Bifurcated gluteal fold | CM ends at L2-3 | Not performed | None |
| Male/5.86 | Circumcision | Lumbar Mongolian spot | CM ends at L2-3 | CM ends at mid L2 | No clinical TCS; PT |
| Male/0.29 | Circumcision | Gluteal asymmetry | CM ends at L2-3 | Not performed | None |
| Male/11.71 | Hydronephrosis | Duplicated gluteal fold | CM ends at L2-3 | Not performed | No clinical TCS; PT |
| Male/9.0 | Hypospadias | Duplicataed gluteal fold, sacral dimple, Mongolian spot | CM ends at L2-3 | CM ends at inferior L2 | No clinical TCS |
US: ultrasound; MRI: magnetic resonance imaging; CM: conus medullaris; FT: filum terminale; TCS: tethered cord syndrome; PT: physical therapy; TCR: tethered cord release.
The bold values represent the only patient with a cutaneous finding of occult spinal dysraphism, abnormal spinal ultrasound, and abnormal lumbar MRI who subsequently underwent a tethered cord release.
Neurosurgical consultation, UDS, and TCR
Of the 34 infants who had an abnormal spinal US, 24 (71%) were evaluated by a pediatric neurosurgeon and had evidence of a low-lying CM (Tables 1 and 2). One additional infant with an LsCM and negative spinal US was also seen by a pediatric neurosurgeon. Of the 25 patients with an LsCM suggestive of OSD and evaluated by a pediatric neurosurgeon, two infants underwent a TCR. One of these infants had an abnormal spinal US, lumbar MRI, UDS, and cutaneous manifestation (lumbar hair), while the other infant had abnormal UDS, clinical findings (tiptoe walking), and cutaneous manifestation (bifurcated gluteal fold) although the spinal US was normal.
Discussion
Risk of OSD and TCS based on various LsCM
The risk of OSD and TCS depends not only on the particular LsCM but also on its specific features and location in the lumbosacral area. Atypical dimples, lumbar masses, large pedunculated lesions, raised lumbar hemangiomas, dermal sinus track, subcutaneous lipoma, caudal appendage, midline pedunculated swelling, sacral agenesis, and highly unusual hair patterns are generally high-risk for OSD, while a flat hemangioma, non-midline lesion, forked gluteal cleft, coccygeal pit, simple sacral dimple, and asymmetric cleft are often low risk for OSD.2,5,10,14
While coccygeal pits are not considered markers of OSD in the literature, a coccygeal pit was statistically marginally higher in abnormal versus normal spine US in this study. Patients with only one LsCM were significantly more likely to have a normal spinal US compared to those with two or more LsCM. Patients with >1 LsCM are 3.2 times more likely to have an abnormal US compared to those with only one LsCM. Our findings concur with previous studies that >1 LsCM portends a significantly higher risk of OSD than a single LsCM.3,10–12
Spinal imaging, UDS, neurosurgical evaluation, TCR
A spinal US is an effective screening tool for neonates and infants with evidence of LsCM due to its ease of performance, no radiation exposure, no sedation, and low cost.5,15–17 To best visualize the spinal canal contents, it is usually performed prior to 3 months of age at which time ossification of the posterior sacral elements occurs. A lumbar MRI is a better imaging study to detect OSD as it is able to visualize the CM and to assess the thickness of the FT.5,6,17 However, a lumbar MRI requires sedation or general anesthesia, is expensive and time-consuming, and is usually not performed until after 3–6 months of age when images are more free of micro-motion artifact. In Tawfik et al.18 study of the diagnostic value of spinal US compared to MRI for the diagnosis of pediatric spinal anomalies, they determined that spinal US may be used as a first-line screening tool for spinal dysraphism while an MRI is the best diagnostic modality for older pediatric patients. Furthermore, these authors recommended that patients with an abnormal spinal US should undergo a spinal MRI.
UDS are the gold standard for evaluating bladder function and shed light on the bladder mechanics during filling and voiding.5,8 While UDS are valuable in elucidating bladder function, they are invasive tests and are usually recommended when medical treatments are unsuccessful, noninvasive studies are not conclusive, and urological surgery is scheduled.8 A TCR involves surgical untethering through a 1-level lumbar laminotomy which eliminates cord traction imposed by TCS and prevents neurological deficits, often resulting in improved function.6,8
Strengths and limitations
Our 6-year multidisciplinary study of LsCMs suggestive of OSD stresses the importance of conducting a thorough examination of the lumbosacral area and performing a spinal US in patients with an LsCM. We report a large series of patients evaluated at a pediatric urology office with at least one LsCM. While certain LsCM have been associated with a higher risk of OSD in the literature, the significance of our work is that no specific lesion had a higher association with OSD apart from the marginally higher risk of a coccygeal pit. Therefore, all LsCM should raise suspicion, especially when >1 LsCM is observed on the same infant.
Closely observing neonates and infants with LsCM as they age plays a crucial role in detecting potential OSD and TCS. Pediatricians should be alert to the neurological consequences that may ensue in a patient with an LsCM suggestive of OSD and carefully monitor their developmental milestones as they age. A prompt neurosurgical referral is mandatory to mitigate the devastating sequelae that are associated with TCS.
The limitation of our current work is its retrospective nature and few patients who underwent UDS. The neurosurgeons used their judgment to determine whether UDS should be performed, primarily based on whether the patients had evidence of clinical TCS. In addition, less than half of the patients with an abnormal spinal US underwent a lumbar MRI. In several cases, parents of neonates and infants who had an abnormal US did not want to subject them to the MRI-required anesthesia despite a neurosurgeon’s recommendation. Another limitation is that our cohort may not be representative of the “normal” population of neonates and infants. Our study population consists of patients referred to pediatric urologists for a suspected urological condition or procedure. In this respect, the findings in our study may be biased toward a higher proportion of abnormal US.
Conclusion
A multidisciplinary effort involving pediatricians, pediatric urologists, and pediatric neurosurgeons is warranted in the early recognition and diagnosis of OSD to decrease the likelihood of developing permanent deficits from TCS. All LsCM suggestive of OSD should raise the index of suspicion, and a spinal US is necessary to confirm the CM location and FT thickness. Careful monitoring for urological impairment is necessary to prevent severe renal dysfunction. In addition, close observation of infants as they age is imperative to discern gait abnormalities. This study also highlights the importance of UDS when there are abnormal cutaneous findings. Routine physical examinations of the lumbar region for cutaneous manifestations of OSD are imperative to confirm prompt management of TCS and avoid potentially devastating repercussions.
Acknowledgments
The authors acknowledge Norton Healthcare for their continued support.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The Chair/Vice-Chair of The University of Louisville Institutional Review Board (IRB Number 19.1001) determined that our study was exempt according to 45 CFR 46.101(b) under Category 4.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: As the patients in this study were less than 1 year of age, the patients’ mothers provided written consent before the study.
ORCID iD: Lisa BE Shields  https://orcid.org/0000-0002-1526-4063
https://orcid.org/0000-0002-1526-4063
References
- 1.Drolet BA, Chamlin SL, Garzon MC, et al. Prospective study of spinal anomalies in children with infantile hemangiomas of the lumbosacral skin. J Pediatr 2010; 157(5): 789–794. [DOI] [PubMed] [Google Scholar]
- 2.Aby J, Kim JL.A cross-sectional assessment of cutaneous lumbosacral and coccygeal physical examination findings in a healthy newborn population. Glob Pediatr Health. Epub ahead of print 8 February 2018. DOI: 10.1177/2333794X18756133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi SJ, Yoon HM, Hwang JS, et al. Incidence of occult spinal dysraphism among infants with cutaneous stigmata and proportion managed with neurosurgery: a systematic review and meta-analysis. JAMA Netw Open 2020; 3(7): e207221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schropp C, Sörensen N, Collmann H, et al. Cutaneous lesions in occult spinal dysraphism—correlation with intraspinal findings. Childs Nerv Syst 2006; 22(2): 125–131. [DOI] [PubMed] [Google Scholar]
- 5.Tuite GF, Thompson DNP, Austin PF, et al. Evaluation and management of tethered cord syndrome in occult spinal dysraphism: recommendations from the international children’s continence society. Neurourol Urodyn 2018; 37(3): 890–903. [DOI] [PubMed] [Google Scholar]
- 6.Bhimani AD, Selner AN, Patel JB, et al. Pediatric tethered cord release: an epidemiological and postoperative complication analysis. J Spine Surg 2019; 5(3): 337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horn S, Moses M, Vasquez-Montes D, et al. Tethered cord syndrome in the United States cluster analysis of presenting anomalies and associated. Bull Hosp Jt Dis 2020; 78(3): 157–162. [PubMed] [Google Scholar]
- 8.Park K.Urological evaluation of tethered cord syndrome. J Korean Neurosurg Soc 2020; 63(3): 358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solakhan M, Oktay K, Guzel E, et al. Course of urological problems in children with spinal dysraphism: long-term follow-up results. Pediatr Neurosurg 2020; 55(2): 101–105. [DOI] [PubMed] [Google Scholar]
- 10.Ausili E, Maresca G, Massimi L, et al. Occult spinal dysraphisms in newborns with skin markers: role of ultrasonography and magnetic resonance imaging. Childs Nerv Syst 2018; 34(2): 285–291. [DOI] [PubMed] [Google Scholar]
- 11.Guggisberg D, Hadj-Rabia S, Viney C, et al. Skin markers of occult spinal dysraphism in children: a review of 54 cases. Arch Dermatol 2004; 140(9): 1109–1115. [DOI] [PubMed] [Google Scholar]
- 12.Sung HJ, Lee HS.Dorsal midline cutaneous stigmata associated with occult spinal dysraphism in pediatric patients. Korean J Pediatr 2019; 62(2): 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shields LBE, Mutchnick IS, Peppas DS, et al. Importance of physical examination and imaging in the detection of tethered cord syndrome. Glob Pediatr Health. 2019; 6: 2333794X19851419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dias M, Partington M.Congenital brain and spinal cord malformations and their associated cutaneous markers. Pediatrics 2015; 136(4): e1105–e1119. [DOI] [PubMed] [Google Scholar]
- 15.Cho HH, Lee SM, You SK.Optimal timing of spinal ultrasound evaluations for sacral dimples in neonates: earlier may not be better. J Ultras Med 2019; 38(5): 1241–1247. [DOI] [PubMed] [Google Scholar]
- 16.Lode HM, Deeg KH, Krauss J.Spinal sonography in infants with cutaneous birth markers in the lumbo—sacral region—an important sign of occult spinal dysrhaphism and tethered cord. Ultraschall Med 2008; 29(suppl. 5): 281–288. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill BR, Gallegos D, Herron A, et al. Use of magnetic resonance imaging to detect occult spinal dysraphism in infants. J Neurosurg Pediatr 2017; 19(2): 217–226. [DOI] [PubMed] [Google Scholar]
- 18.Tawfik NA, Ahmed AT, El-Shafei TE, et al. Diagnostic value of spinal ultrasound compared to MRI for diagnosis of spinal anomalies in pediatrics. Egypt J Radiol Nucl Med 2020; 51: 18. [Google Scholar]