Abstract
Background:
Standardized criteria are lacking to guide patient return to sport (RTS) after rotator cuff surgery (RCS) or shoulder stabilization surgery (SSS).
Purpose:
To describe RTS criteria used after RCS and SSS in athletic populations.
Study Design:
Scoping review; Level of evidence, 4.
Methods:
This scoping review was based on the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Scoping Review) guidelines. A total of 5 electronic databases (MEDLINE, Scopus, SPORTDiscus, Embase, Google Scholar Advanced search) and the gray literature were searched for English-language studies that reported at least 1 RTS criterion in athletes after shoulder surgery. Studies were assigned to the RCS or SSS subgroup based on the primary procedure performed. Data were extracted and summarized as frequencies or arithmetic mean and standard deviation.
Results:
Included were 52 studies and 2706 athletes (2206 male, 500 female, with a mean age of 28.8 ± 1.8 years). The RCS group consisted of 14 studies and the SSS group consisted of 38 studies. Time from surgery was the most common RTS criterion reported overall (37/52 studies; 71%) as well as within the RCS (93%) and SSS (63%) subgroups. Muscle strength (25/52 studies; 48%) and range of motion (23/52; 44%) were used by almost half of the included articles. RTS criteria reported less often were absence of pain, successful completion of sport-specific or position-specific test, proprioception, radiographic evaluation, patient-surgeon agreement, minimum time required to participate in pain-free throwing, and satisfactory scapulothoracic mechanics. All studies used 1 to 3 of the above RTS criteria; however, the definition of each criterion differed among the included articles.
Conclusion:
Time from surgery was the most commonly reported RTS criterion after RCS or SSS in athletes, whereas muscle strength and range of motion were used by almost half of the articles. There was high heterogeneity in the definition of each RTS criterion used among the included studies, which also used different combinations of 1 to 3 RTS criteria. These results suggest the need to better define quantitative and qualitative RTS criteria in athletes undergoing rotator cuff and shoulder stabilization procedures in order to safely return athletes to sport.
Keywords: scoping; review, return to sport, criteria, rotator cuff, shoulder, instability, athletes
A successful return to sport (RTS) after shoulder surgery in the competitive athlete requires a multidisciplinary approach and a coordinated effort between the injured athlete, the athletic training staff, and members of the medical team. Unfortunately, a significant knowledge gap exists regarding the understanding of rehabilitation factors that dictate a safe return to the athlete’s preinjury level of performance. Furthermore, significant variation exists among the postoperative protocols used for athletes undergoing shoulder surgery, and this discrepancy may play a role in the rate of reinjury and successful return.
Currently, no consensus is available regarding the subjective and objective criteria that inform whether an athlete can safely return to sport after a shoulder procedure. Most of the existing research and consensus statements focus on RTS guidelines after shoulder dislocation and/or shoulder stabilization procedures; however, there is lack of evidence supporting the use of clearly defined metrics to guide decision making.22,35 Fewer studies have examined the rate of RTS after rotator cuff repair in athletes given the decreased incidence of the procedure in this population.24,46,49,59 Similar to RTS criteria after shoulder stabilization surgery (SSS), the RTS criteria after rotator cuff repair are not validated. Although shoulder instability is often the primary indication for shoulder arthroscopy in athletes, preexisting rotator cuff lesions may be corrected during the same procedure.40 However, this is not a common scenario, and most of the studies reporting the RTS rate after rotator cuff repair include physically active patients who are younger than 65 years.10,33,46,55 Furthermore, no data are available to suggest that these heterogeneous criteria are utilized in either preventing recurrent injury or optimizing athletic performance. In a systematic review of RTS criteria after anterior stabilization surgery, Ciccotti et al16 found that time from surgery to RTS was the only criterion explicitly used. That study, however, included patients at all levels of sport-related or occupation-related activities and did not exclusively focus on athletes. In addition, the authors included only patients who had traumatic shoulder instability events.
The primary purpose of the current scoping review was to describe the reported RTS criteria after rotator cuff surgery (RCS) or anterior, posterior, or multidirectional SSS in the athletic population. The secondary aim was to evaluate the need for internationally recognized guidelines and clearly defined RTS criteria for athletes who undergo these procedures.
Methods
Due to significant heterogeneity among studies reporting RTS criteria after RCS or SSS in athletes, we elected to proceed with a scoping review. Scoping reviews are appropriate to present an overview of the existing evidence on a topic in order to identify gaps and designate areas for future study.60 We conducted this scoping review by adhering to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Scoping Review) guidelines (http://www.prisma-statement.org/Extensions/ScopingReviews).
Study Identification
We queried 5 electronic databases (MEDLINE, Scopus, SPORTDiscus, Embase, Google Scholar Advanced search) and the gray literature for studies reporting 1 or more RTS criteria in recreational and high-level athletes undergoing RCS or SSS of any type. The search included studies published from the inception time of each database until August 4, 2020. Multiple combinations of the following terms (linked by “AND” or by “OR”) were used to retrieve potentially eligible articles: rotator cuff, instability, labrum, labral, superior labral anterior-posterior, anterior, posterior, multidirectional, dislocation, debridement, repair, reconstruction, tendon transfer, Bristow, Latarjet, coracoid, Bankart, Hill-Sachs, lesion, instability, capsule, capsular, shift, open, mini-open, arthroscopic, arthroscopically assisted, rehabilitation, return to sport, criterion, criteria, athlete, recreational, high-level, professional, outcome, outcomes, shoulder, tear, surgery, clear, clearance. The search was restricted to peer-reviewed articles published in the English language, without a limitation in the year of publication.
Study Criteria and Definitions
Inclusion in this review was based on the following 6 criteria:
Study design: Included were (1) prospective or retrospective studies that included a population of ≥6 athletes (all ages and levels of competition) who underwent surgical treatment for rotator cuff tear or shoulder instability (anterior, posterior, multidirectional) and that reported 1 or more criteria that were used to clear the athletes to return to their sport and (2) articles published in the English language in peer-reviewed journals. Exclusion criteria were as follows: (1) studies reporting the RTS rate after RCS and/or SSS in athletes without mentioning at least 1 RTS criterion; (2) studies reporting the criteria to return to occupational activities after RCS or SSS in patients who were not classified as athletes; (3) studies not reported in the English language; (4) non–peer reviewed articles; (5) case studies and case series with a sample size of <6; and (6) studies that did not designate RCS or SSS as the primary surgical procedure.
Participants: Studies that described any participant as an “athlete,” regardless of age or level of competition (recreational, high school, collegiate, professional). Studies including a mixed patient population (athletes and nonathletes) were excluded if the results in the athletic subgroup were not clearly stated (ie, were not reported separately from the nonathletes). Studies that did not describe any participants as athletes were excluded.
Procedures: Studies in which all athletes underwent RCS or SSS (primary or revision) with or without concomitant procedures. If additional procedures were performed at the time of RCS or SSS, studies were excluded if neither RCS nor SSS was reported as the primary surgical procedure. Studies including patients who underwent surgery for traumatic/acute or nontraumatic/chronic shoulder problems were included. Studies were divided into 2 groups (RCS group or SSS group) based on the primary procedure performed.
RTS rate: Studies that reported the percentage of athletes or shoulders that returned to sport (regardless of the level of competition), based on the definition provided by each of the included studies.
Outcomes: Studies that reported at least 1 RTS criterion.
Study timeline: From database (MEDLINE, Scopus, SPORTDiscus, Embase, Google, gray literature) inception to August 1, 2020.
Study Screening
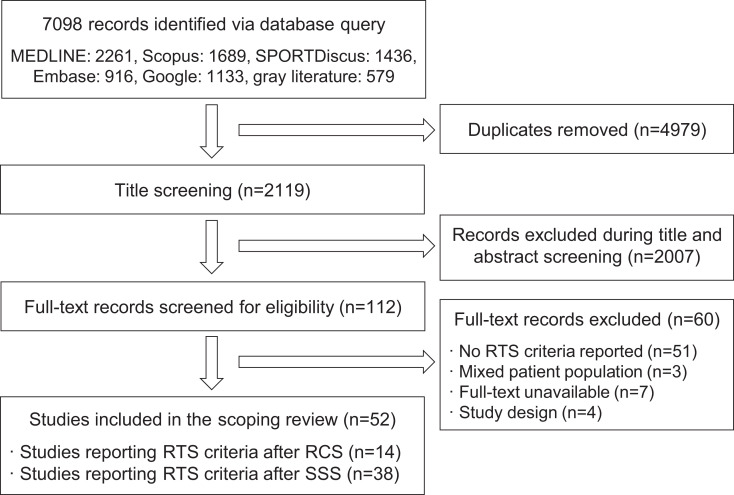
All references were imported to the EndNoteX9 citation manager system (Endnote X9.3.3, Clarivate Analytics). After duplicate removal, 2 independent reviewers (I.K.B., N.F.) completed the title, abstract, and full-text screen. During the title and abstract screening, if at least 1 reviewer was indecisive as to whether a study met the inclusion criteria, the study was included. Discrepancies between the 2 independent reviewers at all 3 screening stages were resolved by a third reviewer (R.G.). The reference list of each of the included studies was searched manually for potentially eligible articles (cross-reference). Figure 1 presents the study identification and screening process in detail.
Figure 1.
Flow diagram of study identification and screening process. RCS, rotator cuff surgery; RTS, return to sport; SSS, shoulder stabilization surgery.
Data Extraction
Data were collected independently from the included articles by 2 reviewers (R.G., I.K.B.) using prearranged Excel sheets (Microsoft). Data included publication year, type of procedure performed (primary only), patient age, number of athletes or shoulders analyzed, number of athletes or shoulders that returned to sport, RTS rate (%), mean RTS time, and reported RTS criteria. The data elements were discussed between the 2 reviewers, and any disagreements were resolved by consulting a third reviewer (F.A.P.).
Results
Study Identification
The initial literature review yielded 5386 studies, of which 52 met the inclusion criteria for this scoping review. The interrater agreement among reviewers was excellent in title-abstract screening (percentage agreement was 93%) and full-text screening (percentage agreement was 91%). Of the 52 included articles, 14 studies (27%)∥ comprised the RCS group and 38 studies (73%)¶ comprised the SSS group.
Study Population
This study entailed 2706 athletes (2206 male, 500 female) with a mean age of 28.8 ± 1.8 years (range, 16.1-73 years). All studies (52/52; 100%) reported the mean patient age and the sex distribution among the study population. Table 1 presents the characteristics of the included patients based on the primary shoulder procedure performed (RCS or SSS).
TABLE 1.
Patient Characteristics and Study Distribution Based on the Primary Procedure Performeda
| Variable | RCS Group | SSS Group | Entire Study Group |
|---|---|---|---|
| Patients (male/female), n | 440 (293/147) | 2266 (1913/353) | 2706 (2206/500) |
| Shoulders or patients with available RTS follow-up, n | 414 | 2047 | 2461 |
| Age at surgery, y, mean ± SD | 43.1 ± 4.4 | 23.5 ± 0.8 | 28.8 ± 1.8 |
| Studies reporting at least 1 RTS criterion, n | 14 | 38 | 52 |
aRCS, rotator cuff surgery; RTS, return to sport; SSS, shoulder stabilization surgery.
Procedures Performed
In the RCS group, the majority of studies included patients who underwent arthroscopic rotator cuff repair (11/14; 79%), 2 studies (14%) included patients who had mini–open rotator cuff repair, and 1 study (1/14; 7%) included patients who underwent open rotator cuff repair. In the SSS group, open shoulder stabilization procedures were reported in 12 studies (12/38; 32%) and arthroscopic procedures were reported in 26 studies (26/38; 68%). Table 2 presents the different procedures performed among the studies included in the SSS group, as reported by the authors of those studies. The majority of SSS studies that reported at least 1 criterion for RTS entailed arthroscopic Bankart repair surgeries (8/38; 21%), followed by open Latarjet procedures (7/38; 18%) and arthroscopic capsulolabral repairs (7/38; 18%).
TABLE 2.
Type of Procedures Performed and Frequency Among the Included Articlesa
| Reported Procedure | No. of Studies |
|---|---|
| Arthroscopic Bankart repair | 8 |
| Open Latarjet | 7 |
| Arthroscopic capsulolabral repair | 7 |
| Arthroscopic labral repair | 4 |
| Arthroscopic capsulolabral reconstruction | 3 |
| Arthroscopic shoulder stabilization | 3 |
| Arthroscopic capsular plication | 1 |
| Arthroscopic pancapsular capsulorrhaphy | 1 |
| Arthroscopic remplissage | 1 |
| Arthroscopic HAGL repair | 1 |
| Bristow procedure | 1 |
| Open shoulder stabilization | 1 |
| Open Bankart repair | 1 |
| Inferior capsular shift | 1 |
aHAGL, humeral avulsion of the glenohumeral ligament.
RTS Rates and Times
Information on RTS rates and/or times was available in 2461 patients: 414 patients in the RCS group and 2047 patients in the SSS group. All but 1 study18 (51/52; 98%) reported RTS rates. In the RCS group, the rate of RTS was >70% in 11 studies (11/14; 79%), whereas 3 studies21,33,59 (3/14; 21%) reported RTS rates <60%. In the SSS group, only 6 studies11,36,43,48,51,64 (6/38; 16%) reported RTS rates <80%, whereas most studies (32/38; 84%) reported rates ≥80%.
The mean RTS time was reported in 67% of the included articles (35/52) (Appendix Tables A1 and A2); the mean RTS time for all of the studies combined was 5.9 ± 0.3 months. The mean time to RTS was reported in 9 of 14 (64%) RCS studies and 21 of 38 (55%) SSS studies. Athletes who underwent RCS returned to sport at a mean time of 6.1 ± 0.7 months (range, 2.2-8.7 months), whereas athletes who had SSS returned at a mean time of 5.9 ± 0.3 months (range, 3-8.8 months).
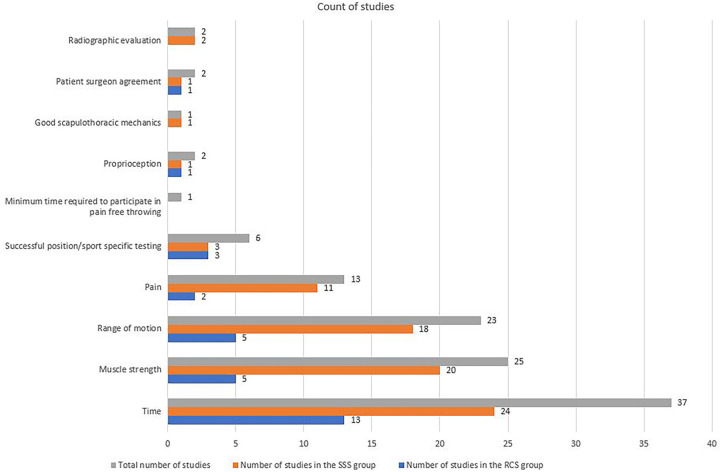
RTS Criteria
We identified 10 RTS criteria used to clear athletes after RCS or SSS; these criteria are described below. The number of RTS criteria used in each of the included articles ranged from 1 to 3. Figure 3 presents the frequency of each of the RTS criteria reported among the included studies. Time from surgery to RTS was the most commonly reported criterion overall (71%), as well as in the RCS (13/14 studies; 93%) and SSS (24/38 studies; 63%) groups. In the RCS group, muscle strength and range of motion (ROM) were used with the same frequency (5/14 studies; 36%). In the SSS group, muscle strength was more commonly used compared with ROM (20/38 studies [53%] vs 18/38 studies [48%]). Appendix Tables A1 and A2 present the individual study data, including the primary procedure performed, patient characteristics, and RTS information.
Figure 3.
Distribution of the return-to-sport criteria used among the included studies (total and based on the primary procedure). RCS, rotator cuff surgery; SSS, shoulder stabilization surgery.
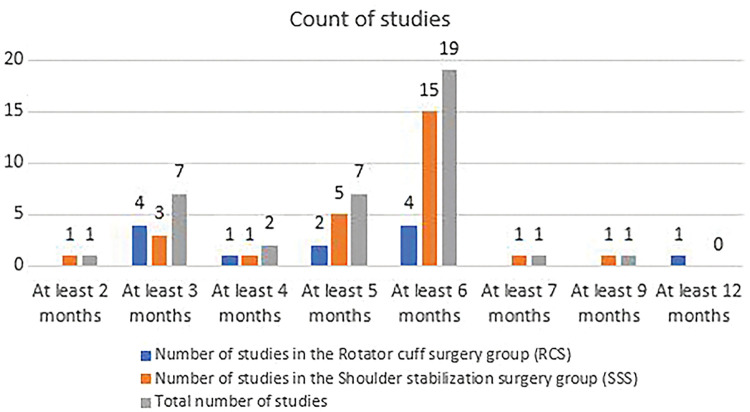
(1) Time
Time from surgery was the most common RTS criterion, used by 37 of 52 (71%) studies. Time alone was used as the RTS criterion in 23 of 52 studies (44%). Figure 2 presents the minimum time required between surgery and return to play, which was used as the RTS criterion among the included articles. The mode (most observed value) for time from surgery to return to play was 6 months, and it was used as an RTS criterion in 19 studies (15/52; 36.5%): 4 studies in the RCS group and 15 studies in the SSS group.
Figure 2.
Count of studies using time from surgery to return to play as a criterion to clear athletes for sport participation based on the primary procedure performed.
(2) Muscle Strength
A total of 25 studies (25/52; 48%) used muscle strength as an RTS criterion, but the definition was variable (Figure 3). The following definitions of muscle strength were reported: full strength; preinjury strength; at least 80% of the strength of the contralateral side; similar strength compared with the contralateral side; symmetrical abduction and external rotation strength with manual testing; grade 5 strength of all intrinsic and extrinsic shoulder muscles; strength equal to or greater than the baseline value.
(3) Range of Motion
We found that 23 studies (23/52; 44%) used shoulder ROM as an RTS criterion, with variable definitions as follows: full ROM; symmetrical ROM compared with the contralateral side; painless ROM; ROM within 20° of the baseline surgical extremity value in all planes.
(4) Pain
A total of 13 studies (13/52; 25%) used pain as an RTS criterion, which was defined as the athletes being pain-free during the physical examination or sport participation before returning to play.
(5) Successful Report-Specific or Position-Specific Testing
We found that 6 studies (6/52; 12%) used sport-specific or player-specific criteria to allow the athletes to return to play. These criteria included baseball pitchers completing a 2-phase interval throwing program (flat-ground program, throwing from the ground); position players completing a flat-ground throwing program; completion of a sport-specific interval training program; successful tackle training, falls training, wrestling, and skills assessment.
(6) Proprioception
Proprioception was used as an RTS criterion in 2 studies (2/52; 4%), with the athlete needing to satisfy proprioceptive criteria before returning to sport.
(7) Patient-Surgeon Agreement on RTS Clearance
In 2 studies (2/52; 4%), a discussion between the patient and the surgeon about the athlete’s readiness or willingness to return was used as the RTS criterion.
(8) Radiographic Healing
In total, 2 studies (2/52; 4%) that included patients who underwent the Latarjet procedure used radiographic evaluation as an RTS criterion, defined as (1) fusion of the coracoid graft on the Bernageau glenoid view at 3 months postoperatively or (2) healed bone graft on radiograph or computed tomography scan at 16 to 24 weeks postoperatively.
(9) Satisfactory Scapulothoracic Mechanics
In 1 study (1/52; 2%), athletes were required to have “good” scapulothoracic mechanics before they could return to play.
(10) Minimum Time Required to Participate in Pain-Free Throwing
One study (1/52; 2%) required that athletes be able to throw without discomfort for 2 weeks before they returned to play.
Discussion
The current scoping review identified 10 RTS criteria after RCS or SSS in athletes competing at any level. Time from surgery was the most common criterion used (71%), followed by muscle strength (48%), ROM (44%), pain (25%), successful sport-specific or position-specific testing (12%), proprioception (4%), patient-surgeon agreement regarding return (4%), radiographic evaluation (4%), scapulothoracic mechanics (2%), and minimum time required to participate in pain-free throwing (2%). Notably, the definition of each of the above criteria was variable among the different studies. Each study used 1 to 3 criteria for RTS; however, there was no consensus on which criteria were used based on the procedure performed or whether some of these criteria were considered more important than the rest when making the decision to clear athletes to return to their sport.
A previous systematic review identified 7 return-to-play criteria after surgical stabilization of traumatic anterior shoulder instability.16 As expected, the authors found that time from surgery was the most commonly used RTS criterion, followed by strength and ROM. Ciccotti et al,16 however, included patients who sustained athletic and also occupational injuries to the shoulder that were treated with anterior shoulder stabilization procedures. We focused exclusively on athletes, and we excluded articles that did not designate the participants as athletes. Further, we examined the RTS criteria after RCS and SSS for traumatic and nontraumatic shoulder instability (anterior, posterior, multidirectional). In the RCS group, time from surgery was the most commonly observed (93%) RTS criterion, whereas muscle strength and ROM criteria were used at a same rate (36%). In the SSS group, muscle strength (53%) was more commonly used compared with ROM (48%), but time remained the most frequently reported RTS criterion (63%) in this subgroup as well.
Based on our findings, the variability in the surgical procedures performed was not reflected in the RTS criteria used to clear athletes for sport participation. Although allowing adequate time for tissue healing and regaining shoulder muscle strength and ROM are the most fundamental surgical principles to ensure patient safety when resuming sports, there is a need to establish rigorous, procedure-specific RTS criteria. Such criteria will allow for a more personalized approach to each athlete’s condition, with possible modification of the time required between surgery and resumption of sport based on these findings.
Research on RTS criteria after anterior cruciate ligament reconstruction (ACLR) has evolved significantly during the past 2 decades. A recent scoping review identified time and impairment-based measures (strength and physical examination tests) as the most commonly used criteria for RTS in patients undergoing primary ACLR.14 Other criteria used were hop testing, performance-based criteria, and patient-reported outcome measures (PROMs), and which have not been shown to have good correlation with PROMs.14 Apart from time, muscle strength and ROM were the most commonly used RTS criteria in athletes who underwent shoulder procedures, based on our findings. None of the included studies in this review reported the use of PROMs as an RTS criterion. Given that obtaining PROMs is a relatively easy way to evaluate the progress of postoperative recovery, we suggest the validation of specific cutoff values or specific ranges of values of the most commonly used PROMs in the shoulder literature, to serve as RTS criteria after common shoulder procedures (such as rotator cuff repair or shoulder stabilization) in athletes.
This scoping review did not identify possible reasons why the RTS criteria after RCS or SSS in athletes were underreported. Most of the included studies were prospective or retrospective case series of athletes who underwent the aforementioned procedures. We suspect that clinicians provided only the basic criteria used for RTS clearance after surgery, given that the decision to return to play was made on an individual basis for each participant. Determining the optimal RTS timing after shoulder surgery can be particularly challenging. This decision may be affected by multiple factors including, but not limited to, injury, type of sport, time from injury to surgery, the athlete’s personal goals, intraoperative findings, postoperative rehabilitation and complications, and socioeconomic variables.61 Consequently, it is almost impossible to establish RTS criteria that would apply to all athletes. However, it is critical to identify certain criteria that may significantly affect the surgical outcome, time to return to play, and career longevity in athletes who undergo shoulder procedures. This scoping review verifies the lack of validated RTS criteria after RCS and SSS in the athletic population, and it encourages the development of recovery pathways using quantitative and qualitative metrics to facilitate clinical decision making related to the clearance of athletes to return to play after shoulder surgery.
An abundance of studies have described postoperative rehabilitation protocols and functional tests in athletes who underwent RCS or SSS in order to facilitate successful return to the preinjury level of physical activity.17,25 However, the communication between physical therapists or other health care professionals who apply these protocols and surgeons is not reflected in the existing literature. From a surgical standpoint, there is an urgent need to validate some of the widely acceptable RTS criteria after RCS or SSS in clinical practice. Examples include the time from surgery to RTS, muscle strength, and ROM. By comparing the RTS time, postoperative performance, reinjury, and career longevity in athletes who return to play earlier versus later after surgery, the ideal timing of RTS per procedure could be predicited with more accuracy. In addition, normative and comparative data between the injured and uninjured extremity as well as the dominant and nondominant extremities should be outlined for sports of interest.
The progressive “normalization” of the above-mentioned measures for the operated limb must be outlined, and the required muscle strength and ROM in the operated extremity must be clearly defined. As stated above, sport-specific and procedure-specific criteria should be established in order to facilitate a more personalized approach to determine the best RTS timing in athletes who undergo RCS or SSS. For example, different RTS criteria may apply in contact athletes versus throwing athletes. Ultimately, these criteria must be validated for the individual sports. The validation of procedure-specific and sports-specific criteria is extremely challenging; however, a stepwise approach to the issue may be ideal. We recommend that future studies of surgical series report the outcomes of different procedures by sport type and that the authors describe the rehabilitation protocol and RTS criteria used in detail. The last will lead to accumulation of the data necessary to validate these criteria.
A relatively small percentage (25%) of studies included in this scoping review used pain as an RTS criterion after RCS or SSS in athletes. We believe that this observation does not reflect the reality in clinical practice and is a result of this criterion’s being underreported or not emphasized in clinical papers. The presence of pain during athletic activity must be considered a warning sign in athletes who attempt to return to play after any type of surgical intervention. Surgeons, physical therapists, and the coaching staff must ensure that athletes are pain-free when participating in sports. It is difficult to determine whether certain characteristics of pain are important during the RTS decision-making process, but the presence of pain itself may be a useful RTS criterion, and its clinical value must be assessed.
Radiographic evaluation was used in 2 studies as an RTS criterion in this review.9,43 Both studies included athletes who underwent a Latarjet procedure, and imaging was obtained in order to ensure bone graft healing.9,43 As stated above, procedure-specific RTS criteria would be helpful to provide individualized consultation for athletes. It is important to determine the type of imaging necessary based on the procedure performed as well as the appropriate time for this evaluation during the athlete’s recovery. For example, in cases of rotator cuff repair, ultrasound or magnetic resonance imaging confirmation of rotator cuff healing or normalization of tendon properties may guide the clinical RTS decision making.
Only 2 studies reported that agreement between the patient and the medical team served as an RTS criterion in athletes undergoing RCS or SSS.2,6 We believe that athletes’ insight into their own physical condition and whether they feel ready to return to play are crucial factors in determining medical clearance for RTS. Previous studies in the ACLR literature have addressed this issue by examining the effect of psychological factors on the ability to return to play for athletes undergoing this procedure.38,62 Therefore, the use of PROMs as RTS criteria in athletes who undergo RCS or SSS is highly recommended, given that the subjective nature of these evaluation tools may also account for the psychological component. An honest discussion between the athlete and the medical team is necessary before the athlete is allowed to return to play. We encourage the development of specific questionnaires to assess the readiness of athletes to return to play after RCS or SSS and to determine their expectations in terms of athletic performance and career longevity. Previous studies have shown that surgeons and patients often have different expectations after surgery, and this is particularly important in the athletic population.3,32
In the current review we identified studies that reported any RTS criteria after RCS and SSS. Although all patients in the included studies were physically active individuals, RCS is mostly performed in older adults whereas the patient population undergoing SSS is younger (Appendix Tables A1 and A2). As shown in Table 1, the mean age was 43.1 years in RCS patients compared with 23.5 years in SSS patients. Based on the findings of this broad scoping review, future consideration of the Delphi technique to establish widely accepted RTS criteria is necessary. In addition, because of the different characteristics of physically active patients who undergo RCS versus SSS, the Delphi method and the proposed RTS criteria must be procedure specific.
Patients who undergo RCS are usually middle-aged adults who wish to return to noncompetitive, recreational activities (Appendix Table A1). In contrast, SSS is mostly performed in younger athletes who wish to return to high-level sport and continue their athletic careers (Appendix Table A2). Not only is it necessary to establish widely accepted criteria, but the validation of these criteria would be helpful. The postoperative athletic performance and longevity of the athletic career may vary based on how quickly the athlete returned to sport and how “conservative” the RTS assessment protocol was. It is imperative that a stepwise approach be developed to establish evidence-based, procedure-specific (and ideally sport-specific) RTS criteria in order to advance the quality of orthopaedic care that athletes receive worldwide.
This study has several limitations. It is possible that some authors reported the RTS criteria used to clear athletes for sport participation but did not describe these criteria in detail due to limitations related to the publication process. In addition, the procedures performed were sometimes different among the athletes included in the same study, and the RTS criteria provided were not procedure specific. This review included both recreational and professional athletes and did not differentiate the RTS criteria used based on the level of competition. We did not examine the association of RTS criteria used in the included studies with the clinical outcome or the postoperative performance of the athletes, which would be helpful to understand the clinical value of each criterion. The last constitutes an area of future research. Overall, the results of this scoping review point toward the need for validation of RTS criteria in athletes undergoing shoulder procedures in order to provide evidence-based medical care to this population.
Conclusion
Time from surgery was the most commonly reported RTS criterion after RCS or SSS in athletes, whereas muscle strength and ROM were used by almost half of the studies reviewed. We noted high heterogeneity in the definition of each RTS criterion used among the included studies, which also used different combinations of 1 to 3 RTS criteria. These results point to a gap in knowledge and the clinical need for further study of RTS criteria in athletes undergoing rotator cuff and shoulder stabilization procedures, with the ultimate goal of minimizing reinjury while improving performance and career longevity.
APPENDIX TABLE A1.
Characteristics and RTS Criteria of the Included Studies on Rotator Cuff Surgerya
| Lead Author (Year) | Mean Patient Age, y | Primary Procedure | Patients Analyzed, n | Patients at Follow-up, n (% of Analyzed) | Mean RTS Time, mo | Reported RTS Criteria |
|---|---|---|---|---|---|---|
| Antoni2 (2016) | 57 | Arthroscopic RCR | 76 | 67 (88) | NR | 1. Time (3 mo) 2. Surgeon-patient discussion-agreement |
| Azaam5 (2018) | 16.1 | Arthroscopic or open RCR | 27 | 25 (94) | NR | 1. Time 2. Completion of sport-specific interval training program |
| Bhatia10 (2015) | 73 | Arthroscopic RCR | 31 | 24 (77) | 1. Time (minimum 3 mo) | |
| Carbone15 (2020) | 40.5 | Single row RCR | 22 | 22 (100) | 8.7 | 1. Time (6 mo) |
| Hawkins21 (1999) | 33.4 | Open RCR | 19 | 8 (50) | NR | 1. Time (4-6 mo) 2. Full symmetric external rotation |
| Ide24 (2005) | 42 | Arthroscopic RCR repair | 6 | 5 (83) | 8.4 | 1. Time (3-6 mo) 2. Restoration of shoulder strength |
| Liem31 (2008) | 58.9 | Arthroscopic RCR | 21 | 21 (100) | 6.3 | 1. Time |
| Mazoue33 (2006) | 29.4 | Mini-open RCR | 16 | 4 (25) | 2.2 | 1. Successful completion of standardized rehabilitation program 2. Full, nonpainful ROM 3. Satisfactory muscle strength 4. Pitchers: completion of 2-phase interval throwing program (flat-ground program, throwing from the ground) 5. Position players: competition of flat ground throwing program |
| Ranalleta46 (2016) | 36.2 | Arthroscopic removal of RC calcifications + RCR | 24 | 23 (96) | 5.3 | 1. Time (3-6 mo) 2. Pain-free 3. Full shoulder ROM 4. Shoulder strength 100% |
| Rossi49 (2019) | 42.2 | Arthroscopic RCR | 72 | 61 (87) | 5.6 | 1. Time 2. Pain-free patient 3. Full shoulder ROM 4. Shoulder strength near to preinjury level |
| Shimada54 (2020) | 65 | Arthroscopic RCR | 32 | 31 (97) | 8 | 1. Time (3 mo for light sport activity, 6 mo for full sport participation) |
| Simon55 (2017) | 55 | Arthroscopic RCR | 12 | 12 (100) | NR | 1. Time (sport-related activities allowed at 12 wk, climbing allowed at 16 wk, full sport participation at 6 mo) |
| Tambe58 (2009) | 25.7 | Arthroscopic RCR | 11 | 11 (100) | 4.8 | 1. Time 2. Satisfactory ROM, strength and isokinetic proprioceptive criteria |
| Tibone59 (1986) | 29 | Open RCR | 45 | 25 (56) | 6 | 1. Time (nonpitcher: 6 mo, pitchers: 12 mo) |
NR, not reported; RCR, rotator cuff repair; ROM, range of motion; RTS, return to sport.
Appendix Table A2.
Characteristics and RTS criteria of the included studies on shoulder stabilization surgery
| Lead Author (Year) | Mean Patient Age, y | Primary Procedure | Patients Analyzed, n | Patients at Follow-up, n (% of Analyzed) | Mean RTS Time, mo | Reported RTS Criteria |
|---|---|---|---|---|---|---|
| Alentrorn Geli1 (2016) | 22 | Arthroscopic capsulolabral repair | 57 | 49 (86) | 4 | 1. Pain-free, full ROM 2. At least 80% of the strength of the contralateral side |
| Arner4 (2015) | 17.9 | Arthroscopic posterior capsulolabral repair | 56 | 52 (93) | 6 | 1. Time (6 mo) 2. Full ROM without pain 3. Full strength and endurance |
| Badge6 (2009) | NR | Arthroscopic posterior labral repair | 11 | 11 (100) | 4.3 | 1. Satisfactory movement, strength, isokinetic, and proprioceptive criteria 2. Discussion between the therapist, surgeon, player, and conditioning coach |
| Bak7 (2000) | 23 | Inferior capsular shift for multidirectional glenohumeral instability | 25 | 21 (84) | 5.5 | 1. Time (minimum 3 mo) 2. Full ROM and good strength |
| Baker8 (2009) | 19.1 | Arthroscopic capsulolabral repair | 36 | 6 (86) | 6 | 1. Painless ROM 2. Strength and endurance comparable with contralateral side |
| Baverel9 (2018) | 21 | Open Latarjet | 106 | 91 (86) | 3 | 1. Physical exam = shoulder pain free and with complete ROM 2. Radiography: fusion of the coracoid graft was achieved on the Bernageau glenoid view at 3 mo 3. Time (minimum 3 mo) |
| Blonna11 (2016) | 31.5 | Arthroscopic Bankart repair vs open Bristow-Latarjet (30/30) | 60 | 52 (87) | NR | 1. Time (noncollision sports 2 mo, collision 6 mo) |
| Bradley12 (2006) | 23.3 | Capsulolabral repair or reconstruction | 100 | 6 (89) | 6 | 1. 80% strength and endurance compared with contralateral side 2. Sport-specific rehabilitation protocol 3. Full, painless ROM 4. Full strength and endurance comparable with the contralateral side |
| Bradley13 (2013) | 24.3 | Arthroscopic capsulolabral reconstruction | 200 | 180 (90) | 6 | 1. Full, painless ROM 2. Full strength and endurance comparable with contralateral side |
| Frantz18 (2020) | 24.5 | Open Latarjet | 65 | NR | NR | 1. ROM within 20° of baseline surgical extremity value in all planes 2. Strength measurement equal to or greater than baseline value |
| Garcia19 (2016) | 29.8 | Arthroscopic remplissage | 44 | 42 (95) | 7.0 | 1. Time (minimum 6 mo) |
| Gerometta20 (2016) | 28.9 | Arthroscopic Bankart repair | 46 | 44 (96) | 6.9 | 1. Time (4-5 mo) |
| Ide23 (2004) | 19 | Arthroscopic Bankart repair | 55 | 44 (80) | NR | 1. Time (4-6 mo) |
| Jones26 (2012) | 19.1 | Arthroscopic capsular plication | 20 | 18 (90) | NR | 1. Time (6 mo) |
| Kasawaki27 (2018) | 18.9 | Bristow procedure | 152 | 142 (93) | 6.3 | 1. Time (5 mo) |
| Kee28 (2018) | 26.5 | Open Latarjet | 56 | 54 (96) | NR | 1. Time (minimum 6 mo) |
| Kercher29 (2019) | 20.5 | Arthroscopic posterior labral repair | 32 | 30 (94) | NR | 1. Adequate strength and ROM 2. Time (6 mo) |
| Kraeutler30 (2018) | 26 | Arthroscopic anterior and/or posterior stabilization | 151 | 109 (72) | 8 | 1. Time (18-24 wk for anterior stabilization, 20-24 wk for posterior stabilization) 2. ROM 3. Strength |
| McClincy34 (2015) | 17.5 | Arthroscopic posterior capsulolabral repair | 96 | 83 (86) | NR | 1. Painless full ROM 2. Full strength and endurance compared to contralateral side |
| Neri36 (2011) | 25 | Arthroscopic repair of type 2 SLAP lesions | 23 | 13 (57) | 8.8 | 1. Time (6 mo) |
| Nevasier37 (2015) | 31 | Open Bankart repair | 23 | 22 (96) | NR | 1. Time (6 mo) |
| Ozturk39 (2013) | 19.5 | Arthroscopic anterior capsulolabral repair | 58 | 40 (87) | NR | 1. Time (6 mo) |
| Pagnani40 (2002) | 18.2 | Open anterior shoulder stabilization | 58 | 52 (90) | NR | 1. Abduction and external rotation strength are symmetrical on manual muscle testing |
| Pennington41 (2010) | 21 | Arthroscopic posterior labral repair | 28 | 27 (93) | NR | 1. Time (6 mo) |
| Plath42 (2015) | 41.2 | Arthroscopic Bankart repair | 44 | 42 (95) | NR | 1. Time (minimum 6 mo) if SLAP, then 7.5 mo |
| Privitera43 (2018) | 25.8 | Open Latarjet | 73 | 46 (63) | 8.1 | 1. Full strength 2. Healed bone graft on radiograph or CT at 16-24 wk |
| Radkowski44 (2008) | 22 | Arthroscopic posterior capsulolabral repair | 98 | 82 (84) | NR | 1. Full ROM 2. Full strength 3. Time 9-12 mo 4. Throwing athletes: able to throw without discomfort for 2 wk |
| Ranalletta47 (2017) | 25.4 | Arthroscopic anterior shoulder stabilization | 20 | 19 (95) | 6.4 | 1. Pain-free 2. Full shoulder ROM 3. Preinjury strength 4. Time 6-8 mo |
| Ranalletta45 (2018) | 22.8 | Modified Latarjet without capsulolabral repair | 50 | 45 (94) | 5.4 | 1. Pain-free 2. Full shoulder ROM 3. Preinjury strength |
| Raynor48 (2016) | 23 | Arthroscopic pancapsular capsulorrhaphy | 30 | 23 (77) | NR | 1. Time (4-6 mo) |
| Rossi50 (2020) | 26.5 | Classic vs congruent arc Latarjet | 135 | 118 (87) | 4.8 | 1. Pain-free 2. Full strength (preinjury) 3. Full ROM |
| Saper51 (2017) | 16.9 | Arthroscopic Bankart repair | 37 | 29 (78) | NR | 1. Time (7 mo) |
| Schmiddem52 (2019) | 24 | Arthroscopic HAGL repair | 9 | 9 (100) | NR | 1. Time (6-9 mo) |
| Shah53 (2018) | 29.7 | Arthroscopic Bankart repair | 22 | 22 (100) | 6 | 1. Satisfactory rehabilitation progression 2. Strength over 80% compared with preinjury 3. Successful tackle training, falls training, wrestling and skills assessment |
| Stein56 (2011) | 26.9 | Arthroscopic Bankart repair | 47 | 47 (100) | 6.5 | 1. Time (minimum 6 mo) 2. Pass sport-specific shoulder test |
| Stirma57 (2020) | 22.9 | Open Latarjet | 10 | 9 (100) | 3 | 1. Time (3 mo) 2. Full painless ROM 3. Strength 5 grade of all intrinsic and extrinsic shoulder muscles |
| Wilson63 (2020) | 18.1 | Arthroscopic anterior or posterior shoulder stabilization | 43 | 5 (11.6) | 6 | 1. Time 2. RTS test performed at 6 mo |
| Wooten64 (2015) | 17 | Arthroscopic posterior capsulolabral reconstruction | 22 | 15 (67) | NR | 1. Full and symmetric ROM 2. Full strength 3. Good scapulothoracic mechanics in the shoulder |
aCT, computed tomography; HAGL, humeral avulsion of the glenohumeral ligament; NR, not reported; ROM, range of motion; RTS, return to sport; SLAP, superior labral anterior-posterior.
Footnotes
Final revision submitted February 22, 2021; accepted March 2, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.E.W. has received educational support from Arthrex, nonconsulting fees from Arthrex, and hospitality payments from Stryker. S.C.G. has received educational support from Arthrex, consulting fees from Zimmer Biomet, and nonconsulting fees from Arthrex. F.A.P. has received consulting fees from Zimmer Biomet, Flexion Therapeutics, Exactech, and Stryker; honoraria from Fidia Pharma and the Musculoskeletal Transplant Foundation; and education payments from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Alentorn-Geli E, Álvarez-Díaz P, Doblas J, et al. Return to sports after arthroscopic capsulolabral repair using knotless suture anchors for anterior shoulder instability in soccer players: minimum 5-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):440–446. [DOI] [PubMed] [Google Scholar]
- 2.Antoni M, Klouche S, Mas V, et al. Return to recreational sport and clinical outcomes with at least 2 years follow-up after arthroscopic repair of rotator cuff tears. Orthop Traumatol Surg Res. 2016;102(5):563–567. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. [DOI] [PubMed] [Google Scholar]
- 4.Arner JW, McClincy MP, Bradley JP. Arthroscopic stabilization of posterior shoulder instability is successful in American football players. Arthroscopy. 2015;31(8):1466–1471. [DOI] [PubMed] [Google Scholar]
- 5.Azzam MG, Dugas JR, Andrews JR, et al. Rotator cuff repair in adolescent athletes. Am J Sports Med. 2018;46(5):1084–1090. [DOI] [PubMed] [Google Scholar]
- 6.Badge R, Tambe A, Funk L. Arthroscopic isolated posterior labral repair in rugby players. Int J Shoulder Surg. 2009;3(1):4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bak K, Spring BJ, Henderson JP. Inferior capsular shift procedure in athletes with multidirectional instability based on isolated capsular and ligamentous redundancy. Am J Sports Med. 2000;28(4):466–471. [DOI] [PubMed] [Google Scholar]
- 8.Baker CL, III, Mascarenhas R, Kline AJ, et al. Arthroscopic treatment of multidirectional shoulder instability in athletes: a retrospective analysis of 2- to 5-year clinical outcomes. Am J Sports Med. 2009;37(9):1712–1720. [DOI] [PubMed] [Google Scholar]
- 9.Baverel L, Colle P-E, Saffarini M, Odri GA, Barth J. Open Latarjet procedures produce better outcomes in competitive athletes compared with recreational athletes: a clinical comparative study of 106 athletes aged under 30 years. Am J Sports Med. 2018;46(6):1408–1415. [DOI] [PubMed] [Google Scholar]
- 10.Bhatia S, Greenspoon JA, Horan MP, Warth RJ, Millett PJ. Two-year outcomes after arthroscopic rotator cuff repair in recreational athletes older than 70 years. Am J Sports Med. 2015;43(7):1737–1742. [DOI] [PubMed] [Google Scholar]
- 11.Blonna D, Bellato E, Caranzano F, et al. Arthroscopic Bankart repair versus open Bristow-Latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med. 2016;44(12):3198–3205. [DOI] [PubMed] [Google Scholar]
- 12.Bradley JP, Baker CL, III, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061–1071. [DOI] [PubMed] [Google Scholar]
- 13.Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005–2014. [DOI] [PubMed] [Google Scholar]
- 14.Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med. 2019;53(18):1154–1161. [DOI] [PubMed] [Google Scholar]
- 15.Carbone S, Candela V, Gumina S. High rate of return to CrossFit training after arthroscopic management of rotator cuff tear. Orthop J Sports Med. 2020;8(4):2325967120911039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ciccotti MC, Syed U, Hoffman R, et al. Return to play criteria following surgical stabilization for traumatic anterior shoulder instability: a systematic review. Arthroscopy. 2018;34(3):903–913. [DOI] [PubMed] [Google Scholar]
- 17.Delvecchio BM, Westgard PE, Bradley H. Rotator cuff physical therapy, rehabilitation and return to sport. In: Arciero RA, Cordasco FA, Provencher MT, eds. Shoulder and Elbow Injuries in Athletes: Prevention, Treatment and Return to Sport. Elsevier: 2017:269–282. [Google Scholar]
- 18.Frantz TL, Everhart JS, Cvetanovich GL, et al. Are patients who undergo the Latarjet procedure ready to return to play at 6 months? A Multicenter Orthopaedic Outcomes Network (MOON) shoulder group cohort study. Am J Sports Med. 2020;48(4):923–930. [DOI] [PubMed] [Google Scholar]
- 19.Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD. Outcomes of the Remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med. 2016;44(5):1124–1130. [DOI] [PubMed] [Google Scholar]
- 20.Gerometta A, Rosso C, Klouche S, Hardy P. Arthroscopic Bankart shoulder stabilization in athletes: return to sports and functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1877–1883. [DOI] [PubMed] [Google Scholar]
- 21.Hawkins RJ, Morin WD, Bonutti PM. Surgical treatment of full-thickness rotator cuff tears in patients 40 years of age or younger. J Shoulder Elbow Surg. 1999;8(3):259–265. [DOI] [PubMed] [Google Scholar]
- 22.Ialenti MN, Mulvihill JD, Feinstein M, Zhang AL, Feeley BT. Return to play following shoulder stabilization: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(9):2325967117726055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ide J, Maeda S, Takagi K. Arthroscopic Bankart repair using suture anchors in athletes: patient selection and postoperative sports activity. Am J Sports Med. 2004;32(8):1899–1905. [DOI] [PubMed] [Google Scholar]
- 24.Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff anatomical and clinical study. Am J Sports Med. 2005;33(11):1672–1679. [DOI] [PubMed] [Google Scholar]
- 25.Johnson M. Rehabilitation following surgery for glenohumeral instability. Sports Med Arthrosc Rev. 2017;25(3):116–122. [DOI] [PubMed] [Google Scholar]
- 26.Jones KJ, Kahlenberg CA, Dodson CC, et al. Arthroscopic capsular plication for microtraumatic anterior shoulder instability in overhead athletes. Am J Sports Med. 2012;40(9):2009–2014. [DOI] [PubMed] [Google Scholar]
- 27.Kawasaki T, Hasegawa Y, Kaketa T, et al. Midterm clinical results in rugby players treated with the Bristow procedure. Am J Sports Med. 2018;46(3):656–662. [DOI] [PubMed] [Google Scholar]
- 28.Kee YM, Kim JY, Kim HJ, Lim CT, Rhee YG. Return to sports after the Latarjet procedure: high return level of non-collision athletes. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):919–925. [DOI] [PubMed] [Google Scholar]
- 29.Kercher JS, Runner RP, McCarthy TP, Duralde XA. Posterior labral repairs of the shoulder among baseball players: results and outcomes with minimum 2-year follow-up. Am J Sports Med. 2019;47(7):1687–1693. [DOI] [PubMed] [Google Scholar]
- 30.Kraeutler MJ, Aberle NS, Brown CC, Ptasinski JJ, McCarty EC. Clinical outcomes and return to sport after arthroscopic anterior, posterior, and combined shoulder stabilization. Orthop J Sports Med. 2018;6(4):2325967118763754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liem D, Lichtenberg S, Magosch P, Habermeyer P. Arthroscopic rotator cuff repair in overhead-throwing athletes. Am J Sports Med. 2008;36(7):1317–1322. [DOI] [PubMed] [Google Scholar]
- 32.Martin RL, Mohtadi NG, Safran MR, et al. Differences in physician and patient ratings of items used to assess hip disorders. Am J Sports Med. 2009;37(8):1508–1512. [DOI] [PubMed] [Google Scholar]
- 33.Mazoué CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182–189. [DOI] [PubMed] [Google Scholar]
- 34.McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31(6):1041–1051. [DOI] [PubMed] [Google Scholar]
- 35.Michener LA, Abrams JS, Bliven KCH, et al. National Athletic Trainers’ Association position statement: evaluation, management, and outcomes of and return-to-play criteria for overhead athletes with superior labral anterior-posterior injuries. J Athl Train. 2018;53(3):209–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes. Am J Sports Med. 2011;39(1):114–120. [DOI] [PubMed] [Google Scholar]
- 37.Neviaser AS, Benke MT, Neviaser RJ. Open Bankart repair for revision of failed prior stabilization: outcome analysis at a mean of more than 10 years. J Shoulder Elbow Surg. 2015;24(6):897–901. [DOI] [PubMed] [Google Scholar]
- 38.Nwachukwu BU, Adjei J, Rauck RC, et al. How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Orthop J Sports Med. 2019;7(5):2325967119845313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ozturk BY, Maak TG, Fabricant P, et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29(12):1922–1931. [DOI] [PubMed] [Google Scholar]
- 40.Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in American football players. J Bone Joint Surg Am. 2002;84(5):711–715. [DOI] [PubMed] [Google Scholar]
- 41.Pennington WT, Sytsma MA, Gibbons DJ, et al. Arthroscopic posterior labral repair in athletes: outcome analysis at 2-year follow-up. Arthroscopy. 2010;26(9):1162–1171. [DOI] [PubMed] [Google Scholar]
- 42.Plath JE, Feucht MJ, Bangoj R, et al. Arthroscopic suture anchor fixation of bony Bankart lesions: clinical outcome, magnetic resonance imaging results, and return to sports. Arthroscopy. 2015;31(8):1472–1481. [DOI] [PubMed] [Google Scholar]
- 43.Privitera DM, Sinz NJ, Miller LR, et al. Clinical outcomes following the Latarjet procedure in contact and collision athletes. J Bone Joint Surg Am. 2018;100(6):459–465. [DOI] [PubMed] [Google Scholar]
- 44.Radkowski CA, Chhabra A, Baker CL, III, Tejwani SG, Bradley JP. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36(4):693–699. [DOI] [PubMed] [Google Scholar]
- 45.Ranalletta M, Rossi LA, Bertona A, et al. Modified Latarjet without capsulolabral repair in rugby players with recurrent anterior glenohumeral instability and significant glenoid bone loss. Am J Sports Med. 2018;46(4):795–800. [DOI] [PubMed] [Google Scholar]
- 46.Ranalletta M, Rossi LA, Sirio A, et al. Return to sports after arthroscopic treatment of rotator cuff calcifications in athletes. Orthop J Sports Med. 2016;4(10):2325967116669310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ranalletta M, Rossi LA, Sirio A, et al. Return to sports and recurrences after arthroscopic anterior shoulder stabilization in martial arts athletes. Orthop J Sports Med. 2017;5(9):2325967117725031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raynor MB, Horan MP, Greenspoon JA, Katthagen JC, Millett PJ. Outcomes after arthroscopic pancapsular capsulorrhaphy with suture anchors for the treatment of multidirectional glenohumeral instability in athletes. Am J Sports Med. 2016;44(12):3188–3197. [DOI] [PubMed] [Google Scholar]
- 49.Rossi LA, Atala N, Bertona A, et al. Return to sports after in situ arthroscopic repair of partial rotator cuff tears. Arthroscopy. 2019;35(1):32–37. [DOI] [PubMed] [Google Scholar]
- 50.Rossi LA, Tanoira I, Gorodischer T, Pasqualini I, Ranalletta M. Similar results in return to sports, recurrences, and healing rates between the classic and congruent arc Latarjet for athletes with recurrent glenohumeral instability and a failed stabilization. Arthroscopy. 2020;36(9):2367–2376. [DOI] [PubMed] [Google Scholar]
- 51.Saper MG, Milchteim C, Zondervan RL, Andrews JR, Ostrander RV, III. Outcomes after arthroscopic Bankart repair in adolescent athletes participating in collision and contact sports. Orthop J Sports Med. 2017;5(3):2325967117697950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schmiddem U, Watson A, Perriman D, Liodakis E, Page R. Arthroscopic repair of HAGL lesions yields good clinical results, but may not allow return to former level of sport. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3246–3253. [DOI] [PubMed] [Google Scholar]
- 53.Shah N, Nadiri MN, Torrance E, Funk L. Arthroscopic repair of bony Bankart lesions in collision athletes. Shoulder Elbow. 2018;10(3):201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shimada Y, Sugaya H, Takahashi N, et al. Return to sport after arthroscopic rotator cuff repair in middle-aged and elderly swimmers. Orthop J Sports Med. 2020;8(6):2325967120922203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Simon M, Popp D, Lutter C, Schöffl V. Functional and sports-specific outcome after surgical repair of rotator cuff tears in rock climbers. Wilderness Environ Med. 2017;28(4):342–347. [DOI] [PubMed] [Google Scholar]
- 56.Stein T, Linke RD, Buckup J, et al. Shoulder sport-specific impairments after arthroscopic Bankart repair: a prospective longitudinal assessment. Am J Sports Med. 2011;39(11):2404–2414. [DOI] [PubMed] [Google Scholar]
- 57.Stirma GA, Lima EBS, Chaves DH, et al. Latarjet procedure on anterior shoulder instability in professional soccer players. Acta Ortop Bras. 2020;28(2):84–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tambe A, Badge R, Funk L. Arthroscopic rotator cuff repair in elite rugby players. Int J Shoulder Surg. 2009;3(1):8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tibone JE, Elrod B, Jobe FW, et al. Surgical treatment of tears of the rotator cuff in athletes. J Bone Joint Surg Am. 1986;68(6):887–891. [PubMed] [Google Scholar]
- 60.Tricco A, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. [DOI] [PubMed] [Google Scholar]
- 61.Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46(7):1545–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilson KW, Popchak A, Li RT, Kane G, Lin A. Return to sport testing at 6 months after arthroscopic shoulder stabilization reveals residual strength and functional deficits. J Shoulder Elbow Surg. 2020;29(7_suppl):S107–S114. [DOI] [PubMed] [Google Scholar]
- 64.Wooten CJ, Krych AJ, Schleck CD, et al. Arthroscopic capsulolabral reconstruction for posterior shoulder instability in patients 18 years old or younger. J Pediatr Orthop. 2015;35(5):462–466. [DOI] [PubMed] [Google Scholar]