Abstract
Background:
Based on previous studies, it is difficult to discern whether patients who have femoroacetabular impingement (FAI) with borderline developmental dysplasia of the hip (BDDH) would benefit from arthroscopy when compared with patients without BDDH.
Purpose:
To evaluate the existing comparative literature on arthroscopic findings, procedures, patient-reported outcomes (PROs), and failures in patients who have FAI with BDDH compared with those without BDDH.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
The PubMed, Embase, and Ovid databases were searched for studies published up to August 31, 2019, that reported outcomes after arthroscopy to treat patients who had FAI with BDDH. Included studies were required to have patients diagnosed with FAI and BDDH who were treated arthroscopically and compared with control patients (FAI without BDDH). Arthroscopic findings, PROs, and revision or total hip arthroplasty (THA) conversion rates were compared between groups.
Results:
Included in the review were 4 articles (933 patients). Patients who had FAI with BDDH were defined as having a lateral center-edge angle (LCEA) of either 18° to 25° or 20° to 25°; for control patients, the maximum LCEA was 40°. Across the studies, there were 224 patients who had FAI with BDDH compared with 709 control patients; the mean follow-up time ranged from 21.6 to 31.3 months among the groups. Improvements were shown across all PROs in each study. Random-effects meta-analysis indicated no statistically significant differences in postoperative PROs, the risk for revision surgery, or conversion to THA between the patients who had FAI with versus without BDDH.
Conclusion:
The results of the current review indicated that hip arthroscopy produced similar short-term outcomes between patients who had FAI with versus without BDDH.
Keywords: borderline developmental dysplasia of the hip, BDDH; femoroacetabular impingement, FAI; hip arthroscopy; systematic review; meta-analysis
Hip arthroscopy is an evolving tool for diagnosing and treating hip pathologies, such as femoroacetabular impingement (FAI), chondral defects, and labral tears.1,15 The use of arthroscopic surgery in the management of hip pathologies appears to provide good clinical outcomes across patient populations, including athletes.10,11,17 However, some articles have suggested factors that result in poor clinical outcomes. One of the most important factors demonstrating poor clinical outcomes is hip instability, a characteristic associated with developmental dysplasia of the hip (DDH).8,22,24
DDH is a musculoskeletal condition in newborns and is considered a precursor to osteoarthritis (OA).21 This condition is characterized by a shallow or an abnormally vertical acetabulum that may result in hip joint instability, unexplained hip dysfunction, pain in young patients, and possible tearing of the labrum.23 DDH can be further defined as borderline based on the coverage the acetabulum provides to the femoral head, the classic measure of which is the lateral center-edge angle (LCEA), ranging anywhere from 18° to 27°.30 Patients with borderline DDH (BDDH) may be evaluated with increased capsular laxity and, as a result, may have a higher risk of poor outcomes after arthroscopic surgery.30 Hip arthroscopic surgery without proper capsule repair may result in increased capsular laxity and thus exacerbate this risk factor in patients with BDDH.30
The treatment of DDH using hip arthroscopy has less support than does treatment using the standard of periacetabular osteotomy and has been associated with less successful outcomes and a likelihood DDH will advance to OA.13,14,20 Studies have shown that clinical results of arthroscopic FAI surgery, including labral repair and/or debridement and capsular closure for BDDH, are relatively favorable.7,18 Conversely, Hatakeyama et al9 reported poor outcomes and identified certain risk factors associated with poorer outcomes when treating patients with BDDH using hip arthroscopy. However, we believe the sample sizes of the aforementioned studies are not large enough to establish the effectiveness and risk factors of hip arthroscopy for patients who have FAI with BDDH as surgical candidates for arthroscopy. Ding et al5 performed a systematic review and concluded that hip arthroscopy for patients with FAI and BDDH brings significant improvement of patient-reported outcomes (PROs), including the modified Harris Hip Score (mHHS), the visual analog scale (VAS) for pain, and patient satisfaction score. However, they did not compare the ability of the procedure to correct the condition or the failures after hip arthroscopy between patients who had FAI with BDDH and patients with normal coverage.5
The purpose of this study was to evaluate the existing comparative literature on arthroscopic findings, procedures, PROs, and failures in patients who have FAI with BDDH as compared with patients who have FAI without BDDH.
Methods
Study Identification and Search Strategy
Using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist, articles were searched using PubMed, Embase, and Ovid MEDLINE databases. The search terms included “borderline developmental dysplasia of the hip,” “arthroscopy,” and “clinical outcome”; no additional Medical Subject Headings or search strategies were used. Two reviewers (Y.M., R.S.) performed the search and data extraction until August 31, 2019, and came to a consensus on the eligibility of relevant studies. Criteria to resolve differences included reading the articles again independently and together, making sure the studies met the inclusion criteria (Table 1). If a study met the criteria after consensus, it was included. In addition, the reference lists from relevant articles were retrieved to identify additional studies.
Table 1.
Inclusion and Exclusion Criteria for Studies Included in This Reviewa
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Human patients of both sexes and all ages Reporting surgical outcomes of isolated hip All included patients having the diagnosis of FAI with BDDH Treatment using hip arthroscopy for correction of FAI with BDDH (ie, no periacetabular osteotomy or additional surgical interventions) Comparative studies |
Review articles Diagnostic studies Case reports Technique reports Opinion articles Non–English language articles Inclusion of patients with other hip pathologies (eg, Legg-Calves-Perthes, avascular necrosis) |
aBDDH, borderline developmental dysplasia of the hip; FAI, femoroacetabular impingement.
A full-text review of the chosen articles was performed in order to determine the following for extraction: patient data, arthroscopic findings, PROs, and the number of patients who underwent revision hip arthroscopy or converted to total hip arthroplasty (THA) after hip arthroscopy with reported mean times to these conversions.
Quality Assessment
Quality assessment of the studies was performed independently by 2 reviewers (Y.M., M.M.) using the Coleman Methodology Score.3
Quantitative Synthesis
Meta-analyses were conducted to compare patients who had FAI with BDDH versus without BDDH with respect to postoperative subjective outcome scales (mHHS, Hip Outcome Score–Activities of Daily Living [HOS-ADL], Hip Outcome Score–Sport Specific Subscale [HOS-SSS], and patient satisfaction), revision rate, and conversion to THA. For continuous endpoints, group differences are expressed using weighted mean differences (WMDs) and are presented with 95% confidence intervals (CIs). For binary endpoints, log odds are reported to compare risk between groups. Random-effects models, estimated using the DerSimonian-Laird method, were chosen to combine studies because formal heterogeneity tests are known to have low statistical power when few studies are combined. P values for the between-group comparison were derived via a z-test within the context of the random-effects models. Heterogeneity among studies was assessed using the I 2 metric and are reported with 95% CIs. R statistical software Version 3.6.2 (R Foundation for Statistical Computing with additional package metafor) was used for all analyses and to produce forest plot figures.
Results
Study Identification and Characteristics
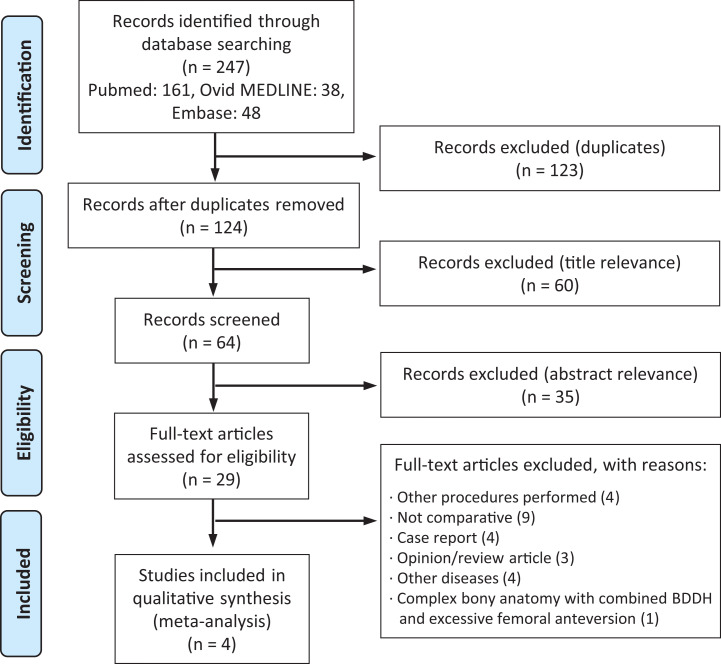
The initial literature search yielded 247 articles that underwent duplicate removal, title exclusion, abstract exclusion, and a final full-text review. After reading the full texts of the 29 articles remaining after the initial exclusions, 25 were excluded based on the following criteria specifically: other procedures performed (n = 4), not comparative (n = 9), case report (n = 4), opinion/review article (n = 3), other diseases (n = 4), and complex bony anatomy with combined BDDH and excessive femoral anteversion (n = 1). The results of the screening process are described in the PRISMA flowchart16 (Figure 1).
Figure 1.
Flowchart of search strategy. BDDH, borderline developmental dysplasia of the hip.
Study Characteristics
Patient characteristics and basic study characteristics of the included articles are noted in Table 2.2,4,6,18 Across the studies there were a total of 224 patients with FAI and BDDH compared with 709 control patients (FAI without BDDH).
Table 2.
Characteristics of the Included Studiesa
| Lead Author (Year) | Study Type (LOE) | Definition of BDDH | Definition of Control Group | Participants, n | Age, y | Follow-up | Outcome Measures |
|---|---|---|---|---|---|---|---|
| Nawabi (2016)18 | Cohort (3) | LCEA, 18°-25° | LCEA, >25° and ≤40°; age- and sex-matched | BDDH: 46 Control: 131 |
BDDH: 29.8 ± 9.4 Control: 29.6 ± 10.3 |
Unrevised: 31.3 ± 7.6 mo (23.1-67.3 mo) Revised: 21.6 ± 13.3 mo (4.7-40.6 mo) |
mHHS, HOS-ADL, HOS-SSS, iHOT-33 |
| Beck (2019)2 | Cohort (3) | LCEA, 20°-25° | LCEA, 25°-40°; matched 1:2 by age, sex, and BMI | BDDH: 112 Control: 224 |
BDDH: 33.6 ± 12.7 Control: 33.7 ± 12.6 |
Minimum 2 y | mHHS, HOS-ADL, HOS-SSS, iHOT-12, VAS, satisfaction |
| Evans (2017)6 | Therapeutic (4) | LCEA, between 20° and 25° | LCEA, ≥25°; match-paired on age <18 y, sex, femoroplasty, capsular plication, and labral treatment | BDDH: 21 Control: 21 |
BDDH: 15.7 (15.5-15.9) Control: 16.0 (15.9-16.2) |
BDDH: 28.6 mo (27.4-29.8 mo) Control: 27.2 mo (26.7-27.8 mo) |
mHHS, HOS-ADL, HOS-SSS, NAHS, VAS, satisfaction |
| Cvetanovich (2017)4 | Cohort (3) | LCEA, 18°-25° | LCEA, 25.1°-40° | BDDH: 36 Control: 312 |
BDDH: 31.5 ± 11.8 Control: 32.9 ± 12.0 |
2.6 ± 0.6 y | mHHS, HOS-ADL, HOS-SSS, VAS, satisfaction |
aMean values are reported as mean ± SD or mean (95% CI) unless otherwise indicated. BDDH, borderline developmental dysplasia of the hip; BMI, body mass index; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport Specific Subscale; iHOT-12, 12-Item international Hip Outcome Tool; iHOT-33, 33-Item international Hip Outcome Tool; LCEA, lateral center-edge angle; LOE, level of evidence; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; VAS, visual analog scale for pain.
Of note, 2 articles4,18 included patients with an LCEA between 18° and 25°, while the remaining 2 studies2,6 included LCEAs between 20° and 25°. The youngest reported participant inclusion was in the study by Evans et al,6 with a restriction of <18 years of age, while the other 3 studies did not report age restrictions. All 4 studies2,4,6,18 included control patients with LCEAs >25°, and the maximum LCEA was 40° in 3 studies2,4,18 and not specified in 1 article.6
Quality Assessment
The results of the Coleman Methodology Score measuring the quality of the included studies can be found in Table 3. All of the articles included in this review were retrospectively designed studies reporting on prospectively collected data. The highest score was 71 out of a possible 100 points,2 while the lowest score for the purposes of this review was 61 out of 100.6,18
Table 3.
Quality Assessment (Coleman Methodology Score)
| Coleman Methodology Score Item | Nawabi18 | Beck2 | Evans6 | Cvetanovich4 |
|---|---|---|---|---|
| Study size | 10 | 10 | 4 | 10 |
| Mean duration of follow-up | 0 | 0 | 0 | 0 |
| Percentage of patients with follow-up | 0 | 5 | 3 | 3 |
| Number of interventions per group | 10 | 10 | 10 | 10 |
| Study type | 0 | 0 | 0 | 0 |
| Diagnostic certainty | 5 | 5 | 5 | 5 |
| Description of surgical technique | 5 | 5 | 5 | 5 |
| Description of postoperative rehabilitation | 0 | 5 | 3 | 3 |
| Outcome criteria | 10 | 10 | 10 | 10 |
| Procedure for assessing outcomes | 6 | 6 | 6 | 6 |
| Description of participant selection process | 15 | 15 | 15 | 15 |
| Total score (out of 100 points) | 61 | 71 | 61 | 67 |
Arthroscopic Procedures
The concomitant arthroscopic procedures performed are outlined in Table 4, identifying the number and percentage of both groups that underwent each additional procedure. Of note, only 1 article18 reported values for several types of possible decompressive procedures, osteochondroplasty, and capsular shift. All 4 studies2,4,6,18 reported values for capsular plication and labral repair, while only 1 study4 reported iliotibial band procedure values of 4 and 1 for control and BDDH groups, respectively. Beck et al2 reported the least number of concomitant procedures with a total of 4, with the next lowest number reported as 8 procedures by Cvetanovich et al.4 The BDDH group had a lower rate of acetabular rim trimming compared with a control group.4
Table 4.
Arthroscopic Procedures of the Included Studiesa
| Nawabi18 | Beck2 | Evans6 | Cvetanovich4 | |||||
|---|---|---|---|---|---|---|---|---|
| Control (n = 152) | BDDH (n = 55) | Control (n = 224) | BDDH (n = 112) |
Control (n = 21) | BDDH (n = 21) | Control (n = 312) | BDDH (n = 36) | |
| Labral debridement | 34 (22) | 17 (31) | NR | NR | 8 (38) | 8 (38) | NR | NR |
| Labral repair | 115 (76) | 38 (69) | 224 (100) | 112 (100) | 13 (62) | 13 (62) | 296 (95) | 33 (92) |
| Labral reconstruction | NR | NR | NR | NR | NR | NR | NR | NR |
| Cam decompression | 151 (99) | 54 (98) | NR | NR | NR | NR | NR | NR |
| Isolated cam decompression | 23 (15) | 14 (25) | NR | NR | NR | NR | NR | NR |
| Femoroplasty | NR | NR | 224 (100) | 112 (100) | 15 (71) | 15 (71) | NR | NR |
| Femoral osteoplasty | NR | NR | NR | NR | NR | NR | 308 (99) | 36 (100) |
| Osteochondroplasty | 128 (84) | 40 (73) | NR | NR | NR | NR | NR | NR |
| Rim decompression | 60 (39) | 15 (27) | NR | NR | NR | NR | NR | NR |
| Rim trimming | NR | NR | NR | NR | NR | NR | 165 (53) | 4 (11) |
| Acetabuloplasty | NR | NR | NR | NR | NR | NR | NR | NR |
| Acetabular rim trimming | NR | NR | 203 (91) | 95 (85) | NR | NR | NR | NR |
| Acetabular chondroplasty | NR | NR | NR | NR | 3 (14) | 0 (0) | NR | NR |
| Subspine decompression | 105 (69) | 35 (64) | NR | NR | NR | NR | NR | NR |
| Cam and rim decompression | 24 (16) | 5 (9) | NR | NR | NR | NR | NR | NR |
| Cam and subspine decompression | 68 (45) | 25 (45) | NR | NR | NR | NR | NR | NR |
| Cam, rim, and subspine decompression | 36 (24) | 10 (18) | NR | NR | NR | NR | NR | NR |
| Capsular shift | 1 (1) | 3 (5) | NR | NR | NR | NR | NR | NR |
| Capsular plication | 152 (100) | 55 (100) | 224 (100) | 112 (100) | 21 (100) | 21 (100) | 312 (100) | 36 (100) |
| Microfracture | NR | NR | NR | NR | NR | NR | 5 (2) | 0 (0) |
| Iliopsoas fractional lengthening | NR | NR | NR | NR | NR | NR | NR | NR |
| Iliopsoas release | NR | NR | NR | NR | 19 (90) | 15 (71) | 1 (0.3) | 0 (0) |
| Iliopsoas bursectomy | NR | NR | NR | NR | 4 (19) | 3 (14) | NR | NR |
| Trochanteric bursectomy | NR | NR | NR | NR | NR | NR | 7 (2) | 1 (3) |
| Notchplasty | NR | NR | NR | NR | NR | NR | NR | NR |
| Synovectomy | NR | NR | NR | NR | 2 (10) | 3 (14) | NR | NR |
| LT debridement | 9 (6) | 13 (24) | NR | NR | 5 (24) | 3 (14) | NR | NR |
| Iliotibial band release | NR | NR | NR | NR | NR | NR | 4 (1) | 1 (3) |
aData are reported as n (%). BDDH, borderline developmental dysplasia of the hip; LT, ligamentum teres; NR, not reported.
PRO Scores
Pre- and postoperative PROs were recorded for mHHS, HOS-ADL, HOS-SSS, Nonarthritic Hip Score (NAHS), VAS for pain, and overall patient satisfaction (Table 5). Noticeably, 1 study18 did not measure NAHS, VAS for pain, or patient satisfaction, and 2 studies2,4 did not measure NAHS. Evans et al6 was the only study included that accounted for all PROs reported in this review.
Table 5.
Patient-Reported Outcome Scores of the Included Studiesa
| Nawabi18 | Beck2 | Evans6 | Cvetanovich4 | |
|---|---|---|---|---|
| mHHS | ||||
| Preoperative | ||||
| Control | 63.3 ± 13.0 | 58.5 ± 14.3 | 59.0 (57.0-61.1) | 56.0 ± 13.5 |
| BDDH | 61.7 ± 10.9 | 55.6 ± 14.5 | 59.7 (57.0-62.4) | 57.2 ± 12.3 |
| Postoperative | ||||
| Control | 84.7 ± 16.5 | 81.4 ± 17.2 | 85.5 (83.9-87.1) | 76.3 ± 16.1 |
| BDDH | 86.2 ± 14.6 | 78.6 ± 18.1 | 88.0 (86.2-89.9) | 79.9 ± 13.8 |
| HOS-ADL | ||||
| Preoperative | ||||
| Control | 74.5 ± 17.0 | 66.7 ± 18.2 | 58.5 (54.6-60.5) | 65.9 ± 17.8 |
| BDDH | 76.0 ± 14.4 | 63.8 ± 18.7 | 62.9 (59.7-62.1) | 65.4 ± 16.0 |
| Postoperative | ||||
| Control | 90.7 ± 13.3 | 85.8 ± 17.9 | 93.9 (92.4-95.4) | 85.5 ± 17.0 |
| BDDH | 93.2 ± 11.3 | 85.5 ± 17.4 | 94.7 (93.0-96.5) | 88.6 ± 15.2 |
| HOS-SSS | ||||
| Preoperative | ||||
| Control | 53.3 ± 23.7 | 43.9 ± 22.8 | 40.0 (36.3-42.7) | 42.8 ± 23.3 |
| BDDH | 54.6 ± 23.0 | 41.7 ± 20.5 | 42.1 (38.6-45.6) | 44.5 ± 20.9 |
| Postoperative | ||||
| Control | 78.8 ± 25.2 | 74.7 ± 26.1 | 72.0 (68.2-75.8) | 73.1 ± 27.1 |
| BDDH | 85.4 ± 22.1 | 72.6 ± 27.1 | 81.6 (77.2-85.9) | 73.6 ± 26.7 |
| NAHS | ||||
| Preoperative | ||||
| Control | NR | NR | 58.0 (55.5-60.5) | NR |
| BDDH | NR | NR | 62.8 (60.1-65.4) | NR |
| Postoperative | ||||
| Control | NR | NR | 89.6 (88.3-90.9) | NR |
| BDDH | NR | NR | 91.9 (90.4-93.5) | NR |
| VAS | ||||
| Preoperative | ||||
| Control | NR | 6.8. ± 1.9 | 6.6 (6.3-6.9) | 7.5 ± 1.6 |
| BDDH | NR | 6.7 ± 1.8 | 6.3 (5.6-6.6) | 7.6 ± 2.4 |
| Postoperative | ||||
| Control | NR | 2.0 ± 2.4 | 1.9 (1.6-2.2) | 2.1 ± 2.4 |
| BDDH | NR | 1.9 ± 2.2 | 1.3 (0.9 -1.7) | 1.4 ± 1.6 |
| Satisfaction | ||||
| Postoperative | ||||
| Control | NR | 78.4 ± 29.4 | 8.5 (8.2-8.7) | 78.3 ± 27.2 |
| BDDH | NR | 77.1 ± 28.5 | 7.9 (7.4-8.4) | 81.8 ± 22.3 |
aAll outcome scores are shown as mean ± SD or mean (95% CI). The VAS scores from Beck were converted from a 0-100 scale to a 0-10 scale. BDDH, borderline developmental dysplasia of the hip; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; NR, not reported; VAS, visual analog scale for pain.
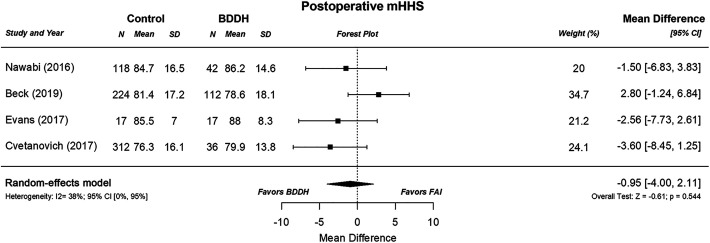
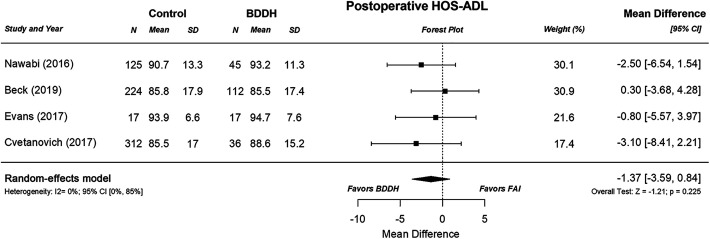
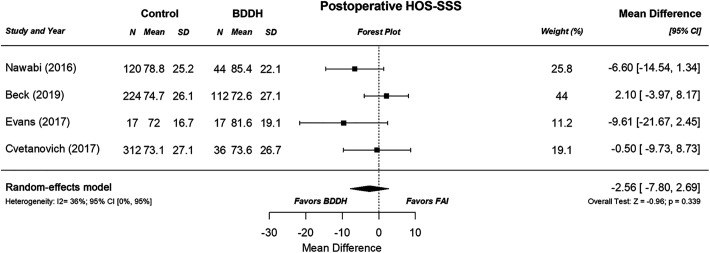
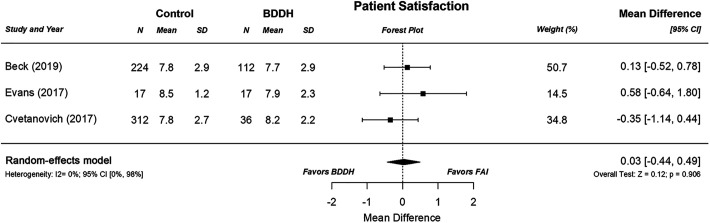
Random-effects meta-analysis showed no statistically significant difference in postoperative mHHS scores between the 2 groups (WMD, –0.95 [95% CI, –4.00 to 2.11]; P = .544; heterogeneity: I 2 = 38% [95% CI, 0% to 95%]) (Figure 2). Similarly, no significant group difference was found for postoperative HOS-ADL (WMD, –1.37 [95% CI, –3.59 to 0.84]; P = .225; heterogeneity: I 2 = 0% [95% CI, 0% to 85%]), HOS-SSS (WMD, –2.56 [95% CI, –7.80 to 2.69]; P = 0.339; heterogeneity: I 2= 36% [95% CI, 0% to 95%]), and patient satisfaction (WMD, 0.03 [95% CI, –0.44 to 0.49]; P = .906; heterogeneity: I 2 = 0% [95% CI, 0% to 98%]) (Figures 3 –5).
Figure 2.
Random-effects weighted mean difference in postoperative modified Harris Hip Score (mHHS) between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement.
Figure 3.
Random-effects weighted mean difference in postoperative Hip Outcome Score–Activities of Daily Living (HOS-ADL) between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement.
Figure 4.
Random-effects weighted mean difference in postoperative Hip Outcome Score–Sport Specific Subscale (HOS-SSS) between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement.
Figure 5.
Random-effects weighted mean difference in patient satisfaction between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement.
Revision Arthroscopy or THA Conversion Rate
Treatment failures resulting in either revision surgery or conversion to THA are reported in Table 6. Evans et al6 is the only study included that reported no conversions or revisions. Only 1 article2 reported on patients with BDDH having to undergo conversion to THA, with an occurrence of 0.8%. On the other hand, the highest revision rates were reported by Nawabi et al18 as 4.6% and 4.3% at 5.8 to 37.3 months and 9.6 to 23.8 months postoperatively for the control and BDDH groups, respectively.
Table 6.
Failure Rate of the Included Studiesa
| Nawabi18 | Beck2 | Evans6 | Cvetanovich4 | |
|---|---|---|---|---|
| Participants | ||||
| Control | 131 | 224 | 21 | 312 |
| BDDH | 46 | 125 | 21 | 36 |
| Revision hip arthroscopy | ||||
| Control | 6 (4.6%) | 0 | 0 | 2 (0.6%) |
| Description | 5.8-37.3 mo postoperatively
|
NR | NR | NR |
| BDDH | 2 (4.3%) | 1 (0.8%) | 0 | 1 (2.8%) |
| Description | 9.6-23.8 mo postoperatively
|
NR | NR | NR |
| Conversion to THA | ||||
| Control | 0 | 0 | 0 | 3 (1.0%) |
| BDDH | 0 | 1 (0.8%) | 0 | 0 |
aData are reported as n (%). BDDH, borderline developmental dysplastic hip; NR, not reported; THA, total hip arthroplasty.
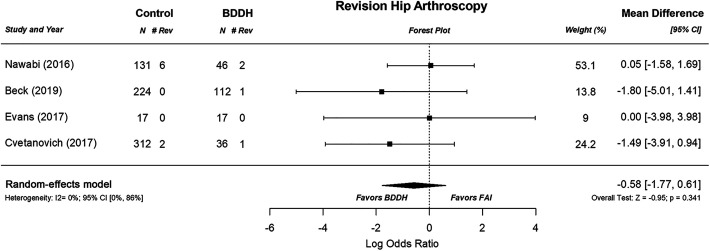
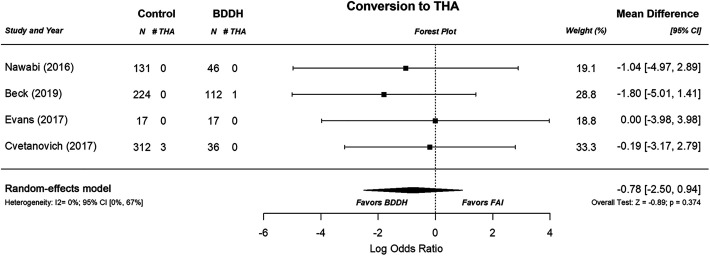
When compared via random-effects meta-analysis, there was no statistical significance in risk for revision surgery (log[odds ratio], –0.58 [95% CI, –1.77 to 0.61]; P = .341; heterogeneity: I 2 = 0% [95% CI, 0% to 86%]) (Figure 6) or conversion to THA (log[odds ratio], –0.78 [95% CI, –2.50 to 0.94]; P = .374; heterogeneity: I 2 = 0% [95% CI, 0% to 67%]) across groups (Figure 7).
Figure 6.
Random-effects weighted mean difference in revision (Rev) hip arthroscopy rates between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement.
Figure 7.
Random-effects weighted mean difference in the conversion rates between the control and borderline developmental dysplasia of the hip (BDDH) groups. FAI, femoroacetabular impingement; THA, total hip arthroplasty.
Discussion
Our search identified 4 comparative outcome studies2,4,6,18 between patients who had FAI with BDDH and patients with normal coverage (patients who had FAI without BDDH). The main findings of this review were as follows: (1) When clinically confirming BDDH, authors only used radiographic parameters. (2) In terms of concomitant procedures, there was a lower rate of acetabular rim trimming in patients who had FAI with BDDH than in patients with normal coverage. (3) As shown through the meta-analysis, there were no differences in postoperative PROs and failure rate (defined as revision arthroscopy and/or conversion to THA) for both groups.
When compared with arthroscopic procedures performed on patients with normal coverage, the procedure for patients who have FAI with BDDH has a different feature: a lower rate of acetabular rim trimming.4 The lower rate of acetabular rim trimming seen in patients who have FAI with BDDH compared with a control group of patients who have FAI without BDDH can be attributed to the anatomic abnormalities that differ between the 2 conditions. Patients with normal coverage diagnosed with FAI may have a pincer deformity, a cam deformity, or both.
The articles included in this review also reported capsular plication rates of 100% for both patients with and patients without BDDH. As a result of the shallow acetabulum, the surface area of the femur covered by both the labrum and the acetabulum is lower than that covered in patients with normal acetabular coverage. This reduces the stability of the joint and is associated with capsular laxity and microinstability, therefore requiring additional capsular procedures in patients with BDDH to reduce the chance of instability postoperatively. Even in patients who are treated for FAI arthroscopically and do not have BDDH, inadequate or lack of capsular plication/closure can result in the need for revision arthroscopy. Because the hip capsule is an important stabilizer of the hip joint,27,28 capsular plication should be performed for patients who have FAI with or without BDDH.
Across 2 of the 3 meta-analyzed PROs, the postoperative treatment effect favored patients in the FAI with BDDH groups.2,4,6,18 This is not to infer that arthroscopy is not a favored treatment for patients with FAI without BDDH. However, there was no statistical significance in these results. This indicates that further research is required to establish a larger base of knowledge from which to pull and analyze data for a stronger consensus on outcomes. The sample size of patients who had FAI without BDDH included 688 patients with a total of 8 (1.2%) reported revisions and 3 (0.4%) THAs; the 228 patients who had FAI with BDDH reported 4 (1.8%) revisions and 1 (0.4%) failure. Although there was no statistical significance in these results, there may be a higher rate of failure when using arthroscopic surgery for the treatment of patients who have FAI with BDDH when compared with those patients without BDDH. Given that DDH is a known risk factor for hip OA,21 it is possible that patients with BDDH may have worse results with longer follow-up. The follow-up periods of the included studies were relatively short (all <3 years), and the patients treated were young (mean age, <35 years for all studies).
Limitations
This review has several limitations. First, this review had a risk of publication bias, as cases of clearly diagnosed BDDH were published and listed in medical literature search engines whereas underdiagnosed cases were probably less likely to be published in the medical literature. Second, we included only comparative studies to do the meta-analysis in order to exclude the following confounding factors: country/race, hospital, and procedures. A third limitation was that the diagnostic pathway was not validated. Each diagnostic procedure should be assessed to confirm whether it in fact exhibits test sensitivity. We also did not have information on the selection of patients with FAI and BDDH. It is possible that there were some patients who underwent periacetabular osteotomy rather than arthroscopy depending on surgeon preference and associated pathology. More research should be done on larger sample sizes to determine if the benefits outweigh the risks of arthroscopy for patients with BDDH.
A fourth limitation was that the small size of this systematic review limits the weight of these findings, and more research is still needed to appropriately answer the question at hand. The fifth limitation was that the minimum 2-year follow-up period of most papers included was not ideal for a systematic review assessing outcomes and failure rates for a surgical procedure that seeks to alter the natural history of the underlying disease. It should be noted that given the nature of this review, there was heterogeneity across studies in terms of surgical procedure, terminology, and diagnostic procedure. Each surgeon and each corresponding patient showed variability, as shown in the arthroscopic findings and concomitant procedures summary of each included article. Some of these patients underwent associated procedures not related to FAI (eg, iliopsoas release). Furthermore, this limits how homogeneously findings were able to be summarized. Sixth, the studies had minor differences in the definition of BDDH. BDDH is largely defined solely according to lateral acetabular coverage,31 which is mostly evaluated using the LCEA.29 Recent studies have supported the formerly mentioned study, suggesting that the analysis of the hip based on a single measurement of the LCEA is not substantial to diagnose a patient as having BDDH.19 Wilkin et al30 described that 3-dimensional analysis using computed tomography scans has shown that hip dysplasia has a variety of forms, with acetabular undercoverage being found in the anterior, lateral, and posterior acetabular regions. In other words, we should consider several radiographic features to determine the full area of acetabular coverage, including vertical center anterior angle,12 the acetabular wall indices,25 the Femoral Epiphyseal Acetabular Roof index, and the Tönnis acetabular roof angle.26 These measurements lead to a more thorough classification of BDDH when used in conjunction with each other by evaluating acetabular coverage of the femoral head in >1 dimension.
Conclusion
This study showed that arthroscopic outcomes for patients with FAI and BDDH are similar to those for patients with FAI without BDDH.
Footnotes
Final revision submitted November 2, 2020; accepted December 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.P. has received education payments from Linvatec; has received speaking fees and consulting fees from Smith & Nephew and Synthes GmbH; has received research support from Smith & Nephew and Arthrex; hospitality payments from Siemens Medical Solutions; has received royalties from DJO, Elsevier, SLACK, Conmed, DonJoy, Linvatec, and Smith & Nephew; holds stock in Arthrosurface and MIS; has ownership in TSC Imaging MJP Innovations; and is a shareholder for EffRx. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Amanatullah DF, Antkowiak T, Pillay K, et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics. 2015;38(3):185–199. [DOI] [PubMed] [Google Scholar]
- 2.Beck EC, Nwachukwu BU, Chahla J, et al. Patients with borderline hip dysplasia achieve clinically significant outcome after arthroscopic femoroacetabular impingement surgery: a case-control study with minimum 2-year follow-up. Am J Sports Med. 2019;47(11):2636–2645. [DOI] [PubMed] [Google Scholar]
- 3.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2–11. [DOI] [PubMed] [Google Scholar]
- 4.Cvetanovich GL, Levy DM, Weber AE, et al. Do patients with borderline dysplasia have inferior outcomes after hip arthroscopic surgery for femoroacetabular impingement compared with patients with normal acetabular coverage? Am J Sports Med. 2017;45(9):2116–2124. [DOI] [PubMed] [Google Scholar]
- 5.Ding Z, Sun Y, Liu S, Chen J. Hip Arthroscopic surgery in borderline developmental dysplastic hips: a systematic review. Am J Sports Med. 2019;47(10):2494–2500. [DOI] [PubMed] [Google Scholar]
- 6.Evans PT, Redmond JM, Hammarstedt JE, Liu Y, Chaharbakhshi EO, Domb BG. Arthroscopic treatment of hip pain in adolescent patients with borderline dysplasia of the hip: minimum 2-year follow-up. Arthroscopy. 2017;33(8):1530–1536. [DOI] [PubMed] [Google Scholar]
- 7.Fukui K, Briggs KK, Trindade CAC, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015;31(12):2371–2379. [DOI] [PubMed] [Google Scholar]
- 8.Fukui K, Trindade CAC, Briggs KK, Philippon MJ. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J. 2015;97-B(10):1316–1321. [DOI] [PubMed] [Google Scholar]
- 9.Hatakeyama A, Utsunomiya H, Nishikino S, et al. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med. 2018;46(1):135–143. [DOI] [PubMed] [Google Scholar]
- 10.Ishøi L, Thorborg K, Kraemer O, Hölmich P. Return to sport and performance after hip arthroscopy for femoroacetabular impingement in 18- to 30-year-old athletes: a cross-sectional cohort study of 189 athletes. Am J Sports Med. 2018;46(11):2578–2587. [DOI] [PubMed] [Google Scholar]
- 11.Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lequesne MG, Laredo JD. The faux profile (oblique view) of the hip in the standing position: contribution to the evaluation of osteoarthritis of the adult hip. Ann Rheum Dis. 1998;57(11):676–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuda DK, Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy. 2012;28(11):1738–1743. [DOI] [PubMed] [Google Scholar]
- 14.Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28(3):440–445. [DOI] [PubMed] [Google Scholar]
- 15.Menge TJ, Truex NW. Femoroacetabular impingement: a common cause of hip pain. Phys Sportsmed. 2018;46(2):139–144. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W264. [DOI] [PubMed] [Google Scholar]
- 17.Murata Y, Uchida S, Utsunomiya H, Hatakeyama A, Nakamura E, Sakai A. A comparison of clinical outcome between athletes and nonathletes undergoing hip arthroscopy for femoroacetabular impingement. Clin J Sport Med. 2017;27(4):349–356. [DOI] [PubMed] [Google Scholar]
- 18.Nawabi DH, Degen RM, Fields KG, et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44(4):1017–1023. [DOI] [PubMed] [Google Scholar]
- 19.Nepple JJ, Wells J, Ross JR, Bedi A, Schoenecker PL, Clohisy JC. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res. 2017;475(4):1037–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross JR, Clohisy JC, Baca G, Sink E. Patient and disease characteristics associated with hip arthroscopy failure in acetabular dysplasia. J Arthroplasty. 2014;29(9)(suppl):160–163. [DOI] [PubMed] [Google Scholar]
- 21.Saberi Hosnijeh F, Zuiderwijk ME, Versteeg M, et al. Cam deformity and acetabular dysplasia as risk factors for hip osteoarthritis. Arthritis Rheumatol. 2017;69(1):86–93. [DOI] [PubMed] [Google Scholar]
- 22.Sardana V, Philippon MJ, de Sa D, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31(10):2047–2055. [DOI] [PubMed] [Google Scholar]
- 23.Schmitz MR, Murtha AS, Clohisy JC. Developmental dysplasia of the hip in adolescents and young adults. J Am Acad Orthop Surg. 2020;28(3):91–101. [DOI] [PubMed] [Google Scholar]
- 24.Sharfman ZT, Grundshtein A, Paret M, Amit L, Amar E, Rath E. Surgical technique: arthroscopic osteoplasty of anterior inferior iliac spine for femoroacetabular impingement. Arthrosc Tech. 2016;5(3):e601–e606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siebenrock KA, Kistler L, Schwab JM, Buchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470(12):3355–3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 27.van Arkel RJ, Amis AA, Cobb JP, Jeffers JR. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J. 2015;97-B(4):484–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walters BL, Cooper JH, Rodriguez JA. New findings in hip capsular anatomy: dimensions of capsular thickness and pericapsular contributions. Arthroscopy. 2014;30(10):1235–1245. [DOI] [PubMed] [Google Scholar]
- 29.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83(suppl 58):7–38. [Google Scholar]
- 30.Wilkin GP, Ibrahim MM, Smit KM, Beaule PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty. 2017;32(9)(suppl):S20–S27. [DOI] [PubMed] [Google Scholar]
- 31.Yeung M, Kowalczuk M, Simunovic N, Ayeni OR. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res. 2016;5(6):225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]