Abstract
Health disparities and inequities are explained by the conditions of places where people live, learn, work and play. In fact, the health of an individual is partially related to access and quality of health care and mainly associated to his behaviours, socioeconomic conditions and other community related factors that are often challenging to address by health care organizations. To meet the need for information about local social services organizations and the ability to offer resource referrals, a number of platforms have been proposed that provide electronic social resource directories and facilitate referrals to social service agencies. However, these platforms show limitations with regards to their dependancy to health care organizations, application portability, service availability, and user engaging interactions such as tracking, monitoring and notification. Moreover, existing social resource referral platforms suffer from a fragmentation of services and a disconnection between individuals in need and service providers. In this paper, we introduce Smart Community Health (SCH), a novel independent platform that prioritizes connecting people in need with local community resources. SCH is a full-service, end-to-end community service provider recommendation platform designed to help address pressing social, environmental, and health needs within our communities. The platform is composed of a mobile application for individuals looking for services and a web application dashboard for the management of community service providers and health care organizations.
Keywords: Social Determinants of Health, Informatics, Mobile Application Development, Software Engineering
1. INTRODUCTION
The Social Determinants of Health (SDOH), defined as conditions of places where people live, learn, work and play, are known to affect health. SDOH explain, in part, why health disparities and health inequities exist (McGowan et al., 2019). In fact, only 20 percent of what influences the health of a group of patients is related to access and quality of health care. The other 80 percent—commonly known as the social determinants of health—is found in patients’ behaviors, socioeconomic conditions and other factors that are often challenging to address in clinical visits (Smith et al., 2019). For patients and families with complex health issues (e.g., chronic disease, substance abuse, mental health issues), effectively managing care is increasingly complex (Koh et al., 2011).
Racial and ethnic minorities—populations who are more likely to be poor, have lower educational levels, or both—are fundamentally at greater risk of ill health than their non-minority, non-poor, better educated peers (Smith et al., 2007). Multiple factors, both within and outside the health care delivery system, probably explain these disparities. Health care and social factors associated with such disparities relate directly to access to care, and access to care is important because it is believed to lead to better health (Lurie and Dubowitz, 2007). It is widely acknowledged that addressing social risk factors is crucial when comes the time to improve care quality and reduce costs, particularly for low-income patients.
The health care sector’s interest in addressing patients’ social and economic needs has grown dramatically over the past few years (Cartier et al., 2019). For example, health care organizations are interested in diminishing food insecurity to improve outcomes for patients with diabetes and other nutrition-related chronic diseases (Gundersen and Ziliak, 2015). Moreover, they are showing curiosity in reducing housing insecurity and homelessness to lower health care utilization among high-frequency users of emergency health care services (Kushel et al., 2006). In addition, they are engaging in improving access to transportation as a way to reduce no-show rates and to improve specialty care access (Molfenter, 2013).
Health care organizations are also particularly interested in referring their patients to local community-based social service providers that can assist with non-medical needs (Cartier et al., 2019).
For example, health care staff may want to refer patients to food banks, benefits enrolment programs, emergency housing services, or multi-need social service agencies, depending on the patients’ social risks. The health care sector have traditionally relied on informal approaches such as hard-copy or electronic lists of local or community service providers or the experiential knowledge of social or community health workers to determine where to refer patients for non-medical needs. Community service providers’ listings are rarely kept up-to-date and are not always available organization-wide. Furthermore, ad hoc approaches do not enable efficient tracking of referral outcomes, which is increasingly a need as health care organizations seek to systematically address patients’ social risk factors and assess the impacts of these activities. As health care organizations’ interest in addressing patients’ social risks has grown however, many have found these informal approaches insufficient and inefficient to effectively facilitate systematic social risk referrals.
To meet the health care sector’s need for information about local social services organizations and the ability to make electronic referrals, a number of new technology platforms that provide electronic community resource directories and facilitate referrals to social service agencies. However, these technology platforms show several critical limitations. First, these platforms use web technology and do not use the valuable advantages of mobile applications (Han Rebekah Wong, 2012). These advantages include a better response time, a better service availability (off-line and on-line), a full exploitation of the mobile device resources (i.e. camera and localization services). Moreover, mobile applications enable push notifications, instant updates and interactive engagement to name a few. Second, these platforms rely on key words or labels to search social service providers directory ignoring two key factors: needs and locations. The social service referrals suggested by existing technology platforms suffer from a fragmentation of services and a disconnect between individuals in need and service providers. Finally, the coordination between health care organizations or social services agencies in one side and the patient in the other side is systematically not supported in existing service resource referral platforms.
In this paper, we present Smart Community Health (SCH), an end-to-end platform that exists outside the domain of any organization. SCH prioritizes connecting people in need with local community resources. Smart Community Health is a full-service, end-to-end community service provider recommendation platform designed to help address pressing social, environmental, and health needs within our communities.
The paper is organized as follows. In Section 2, we provide an overview of existing resource referral systems. We highlight our motivations to use mobile application technology and more precisely mobile applications over web-based applications to emphasize the portability of our platform. We also offer a comprehensive technical discussion of the introduced existing resource referral systems from a software functional and non-functional requirements perspective. Next, in Section 3, we detail the requirement engineering, the software architecture along with an overview of the two main components of our Smart Community Health platform: the mobile application and the web application dashboard. Finally, in Section 4, we conclude this paper with a synthesis of the main contributions and we share the key elements of our future work.
2. RELATED WORK
In this section, we first provide a short overview on existing local resource referral platforms. Second, we highlight our motivations behind choosing mobile application development over web technology. Finally, we provide a discussion that summarizes the main findings and outline the key functionalities that are needed in a comprehensive, independent, end-to-end community resource recommendation platform.
2.1. Overview on Community Resource Referral Systems
Nine platforms currently dominate the field of community resource referral services; Aunt Bertha (Aunt, 2019), CharityTracker (Charity, 2019), CrossTx (Cross, 2019), Healthify (Healthify, 2019), NowPow (Now, 2019), One Degree (One Degree, 2019), Pieces Iris (Pieces Iris, 2019), TAVConnect (TAVHealth) (TAVHealth, 2019) and Unite Us (Unite Us, 2019). Cartier et al. studied the existing resource referral technology platforms and provided a comprehensive guide for health care organizations (Cartier et al., 2019). Authors in (Cartier et al., 2019) have identified four groups of such technology platforms; (1) Platforms designed for health care-centred social service referrals; (2) Platforms designed for health care-coordination; (3) Platforms designed for individual social service referrals; and (4) Platforms designed for health care professionals.
Healthify, NowPow, and Pieces Iris were developed specifically for health care sector users for the purpose of fostering referrals to social services organizations as part of efforts to improve health by addressing patients’ social needs. As a result, they have a strong focus on providing comprehensive community-wide resource directories and referral management. CrossTx and TAVConnect were also originally developed specifically for health care users but with a greater focus on care coordination and less on the resource directory, though TAV- Connect has recently shifted its focus to become a tool primarily for social service organizations.
In contrast, Aunt Bertha, CharityTracker, One Degree, and Unite Us were not originally developed for health care users. Therefore, they tend to emphasize a community collaboration or patient-focused model of platform implementation rather than a health-care centric approach. Aunt Bertha and One Degree are the only platforms developed to be used by individuals seeking help for themselves; they are the only two that offer a free public-facing online community resource directory that is accessible without logging in. CharityTracker and Unite Us were both originally developed for use by social service organizations and approach referral management more from a community perspective than from a health-care organization perspective. For instance, CharityTracker is the only platform that provides the ability to have unstructured back and forth conversations with a number of organizations through its bulletin board feature. Unite Us stresses in its pitch to users that it approaches implementation from a community wide perspective, rather than only from a health care organization perspective.
2.2. Mobile Application Development
Most of the existing community resource referral systems we introduced in sub-section 2.1 use web technology (desktop or mobile websites) to enable user interactions. However, we believe that web technology is not enough to power user engagement or to optimize users’ interaction with community resource referral platforms. In 2018, 51% of the time spent online in the US is on mobile devices. Moreover, 90% of the time people spend on mobile devices is spent in apps (BroadBandSearch, 2018). Mobile apps have higher engagement rates than mobile-optimized websites or desktop web viewing.
Existing community resource referral will soon need to consider mobile app development to meet users’ needs and expectations. The key question here is; why should community resource referral platforms be built as mobile apps? And what are the key benefits of mobile applications over mobile websites? In the following, we present the key advantages mobile apps have over web technology (desktop or mobile websites) that motivated the software architecture of our Smart Community Health platform.
Response Time.
Mobile applications are usually 1.5 times faster than mobile websites and they perform actions much faster too. Mobile applications store data locally on the mobile device. In web technology, data needs to be fetched from web servers which can can be a time consuming task depending upon the network speed and data size (Baby, 2019).
Personalized Content.
With respect to the user ’s interest, location, preferences, mobile apps make it easy to personalize content and enable a user-centred experiences (Pinpin et al., 2019).
Instant Online & Offline Access.
All mobile apps offer instant access by a tap. They allow users to consume their content quickly offering seamless experience via storing vital data that can be accessed offline too. Web technology rely on pre-defined URLs that need to be typed in a web browser (Cupala et al., 2019).
Leveraging Mobile Devices' Capabilities.
Mobile apps have a unique advantage where access and utilize features from the mobile device such as camera, NFC, GPS, fingerprint scanner for authentication and other apps such as calendar, payment, or QR reader, etc (Sen et al., 2019).
Push Notifications.
Push notifications are received on mobile devices regardless a user opens an app or not. Notifications are valuable to maintain an open reliable communication channels with users. These notifications could express updates, reminders, warnings, etc (Pang and Teh, 2019).
Usability.
Unlike web technology that relies on web browsers to support functions, mobile applications support a wide range of functions enabling various interactions and swipe gestures like a drag, pinch, hold, tap, double tap and more, each performing a certain action that increases user friendliness (Kaya et al., 2019).
2.3. Synthesis
In most existing platforms, users can either browse for services or search based on keywords, usually based on a program, organization, service, need, or geographic area. Another limitation that characterize most of existing platforms is preventing users to search for multiple needs simultaneously. All platforms, except CrossTx, offer the possibility to initiate a community resource referral. This referral is either directly to the community service provider or through the individual. With CrossTx, users cannot provide referrals to the individual, instead all referrals are made directly to the community service provider.
In addition, all the existing platforms enable referral information to be sent directly to a social service organization. These platforms do not offer community service providers to securely access a dedicate platform in order to view and act on referrals, to communicate with the individual, and potentially the ability to accept or decline a referral.
Moreover, a critical functionality that is missing in most of existing platforms is closed-loop referral tracking. The goal of closed-loop referral tracking is to find out what happened after a referral is made. Notifications about services are an important part of a community resource referral system. For example, when information about a service is entered by a community service provider, it should ideally trigger a notification to individuals who are expressing needs that match that service. Similarly, a notification would ideally be sent to the community service provider is an individual is seeking help with a certain need. Other useful features to facilitate referrals included appointment scheduling and built-in web forms that enable patients to apply for specific services at the time of the referral.
Finally, most of existing platforms do not match the assessment results with community service providers. In fact, assessment results should automatically trigger platform actions, for example, recommendation of a list of service providers that address identified needs filtered with respect to criteria such as distance, business hours, service quality rating, supported languages and ethnicities.
3. SMART COMMUNITY HEALTH
The main purpose of the Smart Community Health is to provide an end-to-end platform that exists outside the domain of any organization that prioritizes connecting people in need with community resources in their area. Smart Community Health (SCH) is a full-service, end-to-end community service provider recommendation platform designed to help address pressing social, environmental, and health needs within our communities. The platform is composed of a mobile application for individuals looking for services and a web application for service providers to register and list their services and relavant information about their respective organizations.
In the following section, we detail the followed steps to support the Software Development Life-Cycle (SDLC). (Mahalakshmi and Sundararajan, 2013). First, we present the requirement engineering process and highlight the key system requirements. Next, we provide an overview on the system design and architecture.
3.1. System Requirements Engineering
Smart Community Health has been designed to meet specific requirements that aim to to help address pressing social, environmental, and health needs within our communities. Therefore, three key actors have been identified; (1) Community Service Provider User, (2) Individual User and (3) Health Care Professional User. Moreover, with respect to the size and scale of community service organizations, several units or entities of such an organization need to independently and autonomously set up and control their instance of the community dashboard by managing its users and associated credentials and resources. Hence a third actor has been added ton the list; (3) Community Service Provider Administrator. Figure 2 presents the use case diagram of the Smart Community Health platform.
Figure 2:
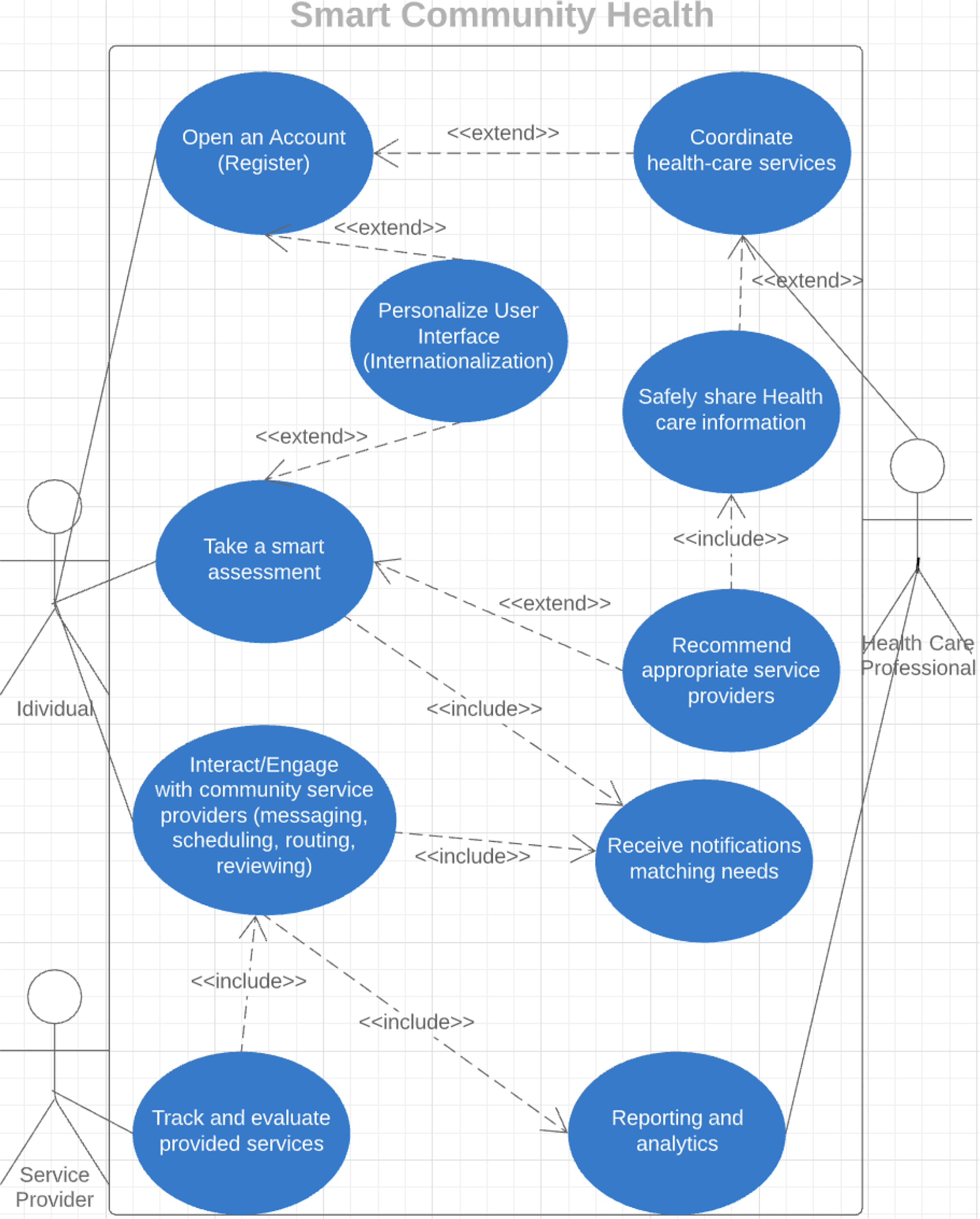
Use Case Diagram of the Smart Community Health platform.
Requirements describe the characteristics that a system must have to meet the needs of the stakeholders. These requirements are typically divided into functional and non-functional requirements. Functional Requirements [FR] describe how a software must behave and what are its features and functions (Shah and Rogers, 1988). Non-Functional Requirements [NFR] describe the general characteristics of a system (Glinz, 2007) They are also known as software quality attributes (Kim and Kim, 2019).
The following is a selection of functional requirements:
[FR1] The system shall allow Community Service Provider User, Community Service Provider Administrator and Health Care Professional User to create (register), view and edit accounts to be allowed secure access to the platform;
[FR2] The system shall allow to Health Care Professional User to list and coordinate health care services;
[FR3] The system shall allow users to support multiple languages (Internationalization);
[FR4] The system shall allow Health Care Professional User to safely share Health care information;
[FR4] The system shall allow Individual User to take a smart assessment;
[FR5] The system shall provide Individual User with recommended and appropriate service providers with respect to multiple criteria (i.e. location, review, health network, etc.);
[FR6] The system shall allow actors to interact through reliable and synchronous communication channels such as instant messaging, internal emails, routing services, appointment scheduling, and review of services;
[FR7] The system shall allow Individual User to subscribe for a notification service matching needs of interest;
[FR8] The system shall allow to track and evaluate provided services;
[FR9] The system shall allow to provide Community Service Provider User, Community Service Provider Administrator and Health Care Professional users with reporting and analytics;
The above listed functional requirements have been analyzed and validated with stakeholders and the following set of quality attributes (non-functional requirement) has been derived:
[NFR1] Availability: the system shall be available 24/7/365;
[NFR2] Scalability: the system shall be capable to scale in order to address large number of users connecting and interacting with the platform.
[NFR3] Portability: the system shall support common iOS and Android-based mobile devices.
[NFR4] Security: user access and access control as well as data management and sharing must support security best practices and techniques and comply with standard protocols;
3.2. System Architecture
The Smart Community Health platform architecture is a the cloud-based architecture detailed in Figure 3. The architecture uses the well-established infrastructure offered by Amazon Web Services (AWS) (Kovalcik and Altman, 2019). The main motivation behind the use of AWS is the non-functional requirements validated with our stakeholders with regards to availability (NFR1), scalability (NFR2) and security (NFR4).
Figure 3:
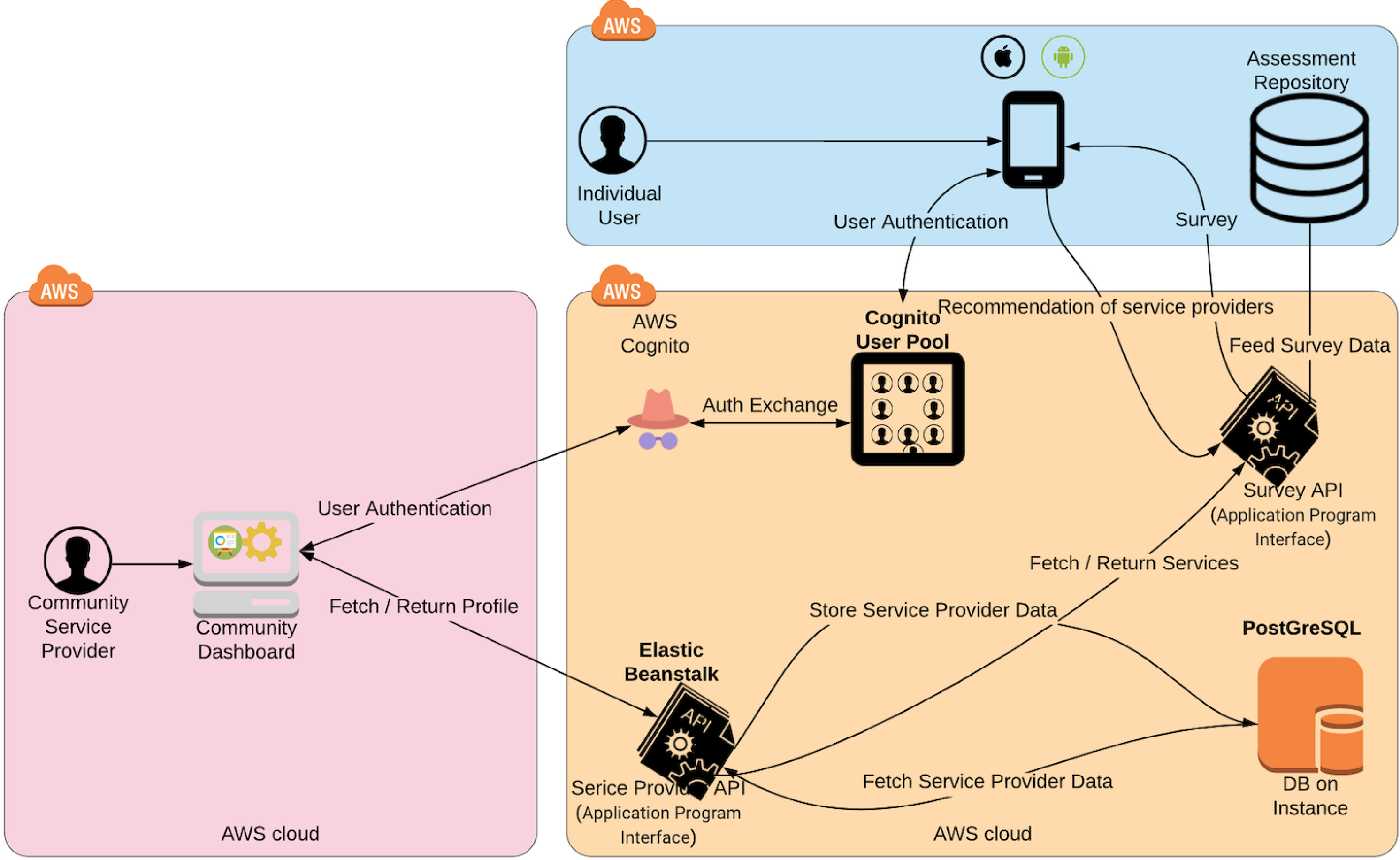
The Smart Community Health architecture.
The Smart Community Health platform architecture is composed of three layers; the mobile application, the web application and the back-end cloud-based modules hosted by AWS. The use of mobile and web applications aims to address the portability quality attribute supported by the non-functional requirement NFR3.
The platform also heavily rely on Application Program Interface (API). In fact, traditional web application design, centred on client server architecture and scripting languages to ensure dynamic rendering, has delivered significant improvements in web development. But when facing the advanced characteristics of interactive content with multiple channels such as the Smart Community Health platform, the client-server request-driven model alone hits its limits. Applications become harder to scale and the web application harder to manage, leading to ever-more tightly coupled systems. To move beyond the client server architecture, and to enable more scalable, contextual and responsive systems, we integrated and implemented a fully event-driven architecture (EDA) within the core of our SCH platform and design capabilities.
3.3. SCH Mobile Application
The SCH mobile application supports the common iOs and Android mobile operating systems. It aims to target a large panel of mobile devices and hence reach out to a large community of potential users (see Figure 4a). The SCH mobile application allows users to securely register or simply to use the mobile application without registration (see Figure 4b). Obviously, registered users have access to personalized account-based services such as scheduling, instant messaging and internal mailing (see Figure 4c). In addition, registered users have the possibility to share individual contact information cards with community service providers. Sharing contact information allow individuals and community service providers to engage in a secure and interactive collaboration to initiate, execute, track and follow up on services. The SCH mobile app allows for individual interaction tracking and monitoring.
Figure 4:
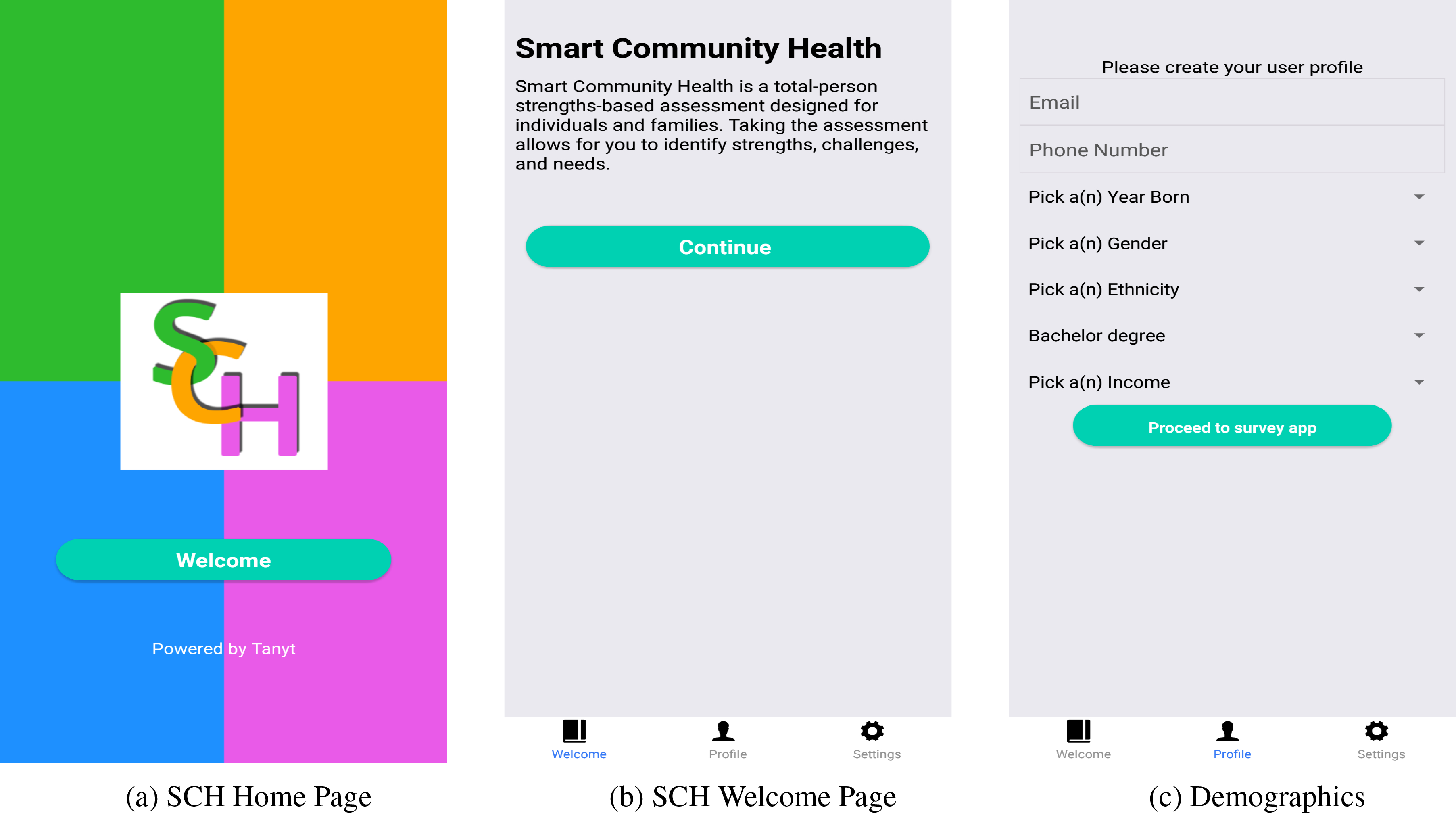
Examples of the Smart Community Health mobile application graphic user interfaces.
The main goal of the SCH mobile application is to match individual needs to available services listed by community service providers. This mobile application uses a smart assessment tool that allows to self-identify health strengths, challenges and needs. This SCH mobile application integrate MyStrengths MyHealth™ (MSMH), a whole-person strengths-based consumer-facing tool designed for individuals, families, and communities to self-identify strengths, challenges, and needs. This SCH mobile application leverages the rigour of the Omaha System (Martin and Scheet, 1992), a multi-disciplinary standardized health terminology and valid, reliable instrument that addresses all of health across four domains with 42 discrete concepts.
Surveys for each of the 42 concepts are embedded using expert- and community-validated plain language terms. In this SCH mobile application, the Omaha System domains, Environmental, Psychosocial, Physiological, and Health-related behaviors, are called My Living, My Mind, Network, My Body, and My Self-care (see Figures 5a). In the SCH mobile application, signs/symptoms associated with the 42 concepts were renamed Challenges (see Figure 5b), and interventions are called Needs (see Figure 5c).
Figure 5:
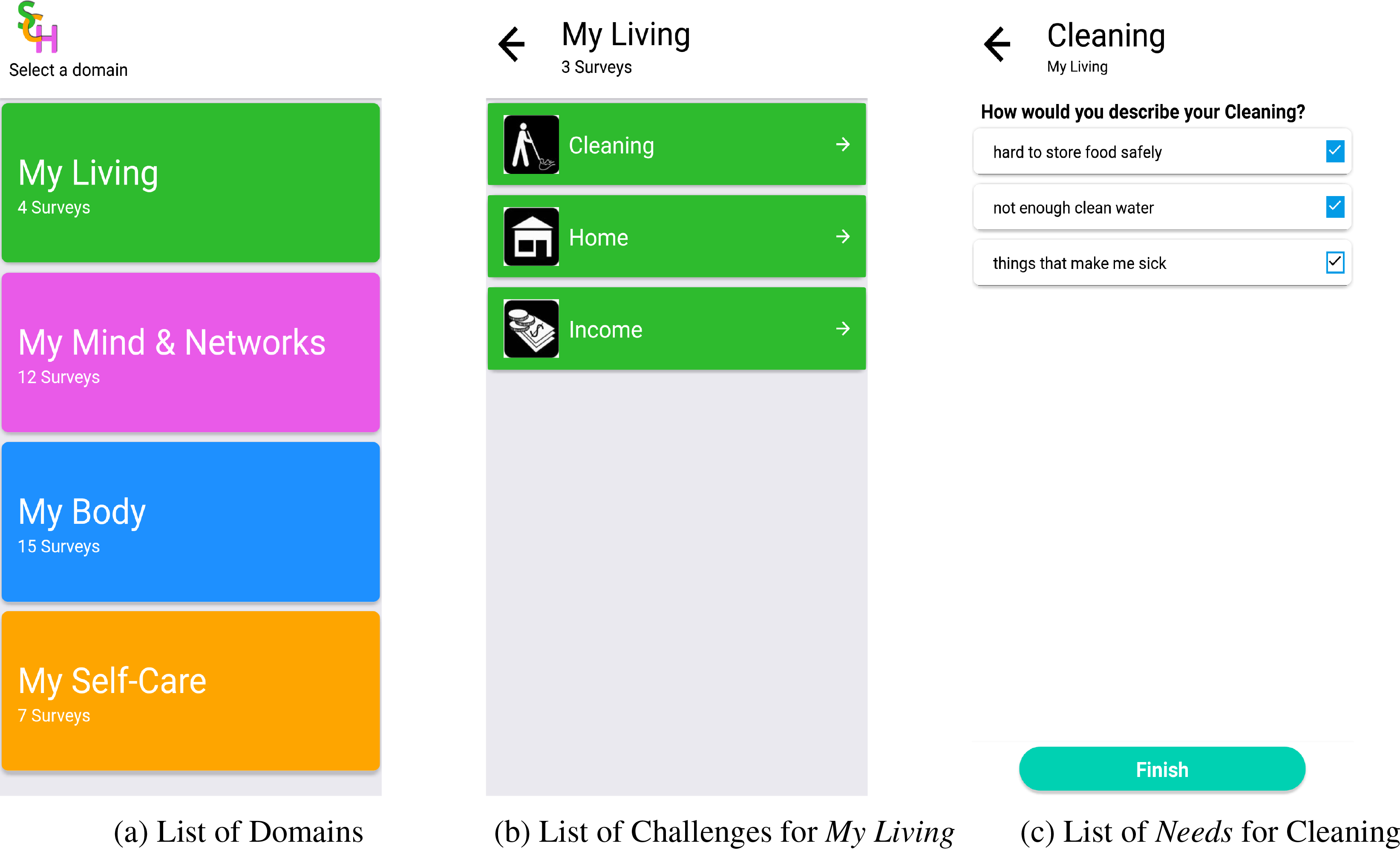
The Smart Community Health mobile application component. Sub-Figures 5a, 5b, 5c describe the smart assessment process. The illustrated challenges in Sub-Figure 5b are associated with the domain ”My Living”. The proposed screening questions in Sub-Figure 5c are associated to the challenge ”Cleaning”.
This community-friendly, consumer-facing instrument generates data for community service providers, health care organizations, education, and research. Once an individual completes the assessment, the SCH mobile application provide a selection of recommended community service providers that match the expressed needs (see Figure 6).
Figure 6:
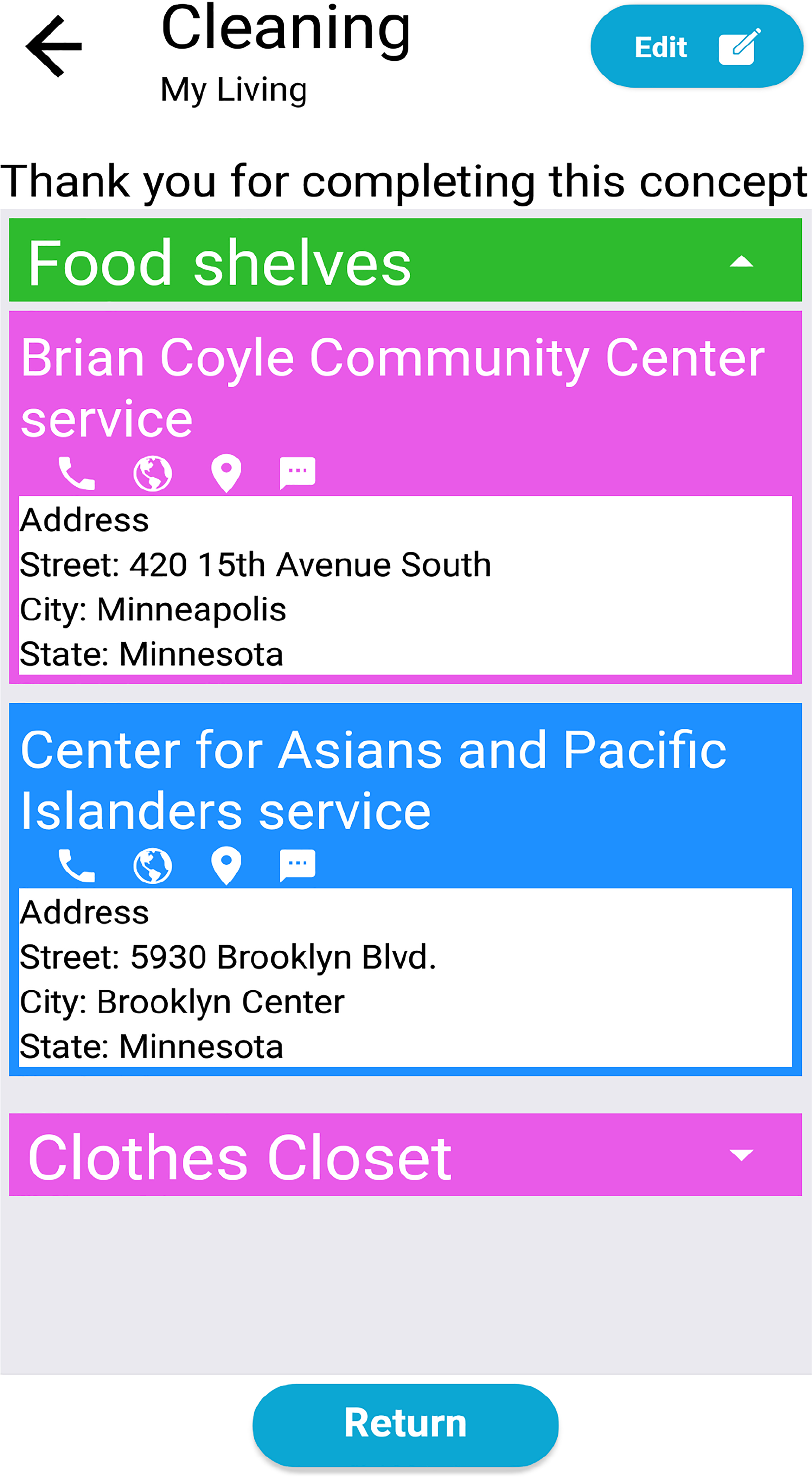
The recommended community service providers grouped by service category for the ”Cleaning” need. Note the user engagement interactive anchors to useful services including phone call, web browsing, routing and instant messaging.
3.4. SCH Community Dashboard
The SCH Community Dashboard is a web application platform that serves community partners including community service providers and health care organizations. It allows organizations to create an account and securely access and manage their profile (see Figure 7a and 7b). Once logged in, an organization representative can define a geospatial service area where this organization offer services (see Figure 8a). Each defined geospatial service area is characterized with a set of services and ethnicities targeted by these services (See Figures 8b and 9a).
Figure 7:
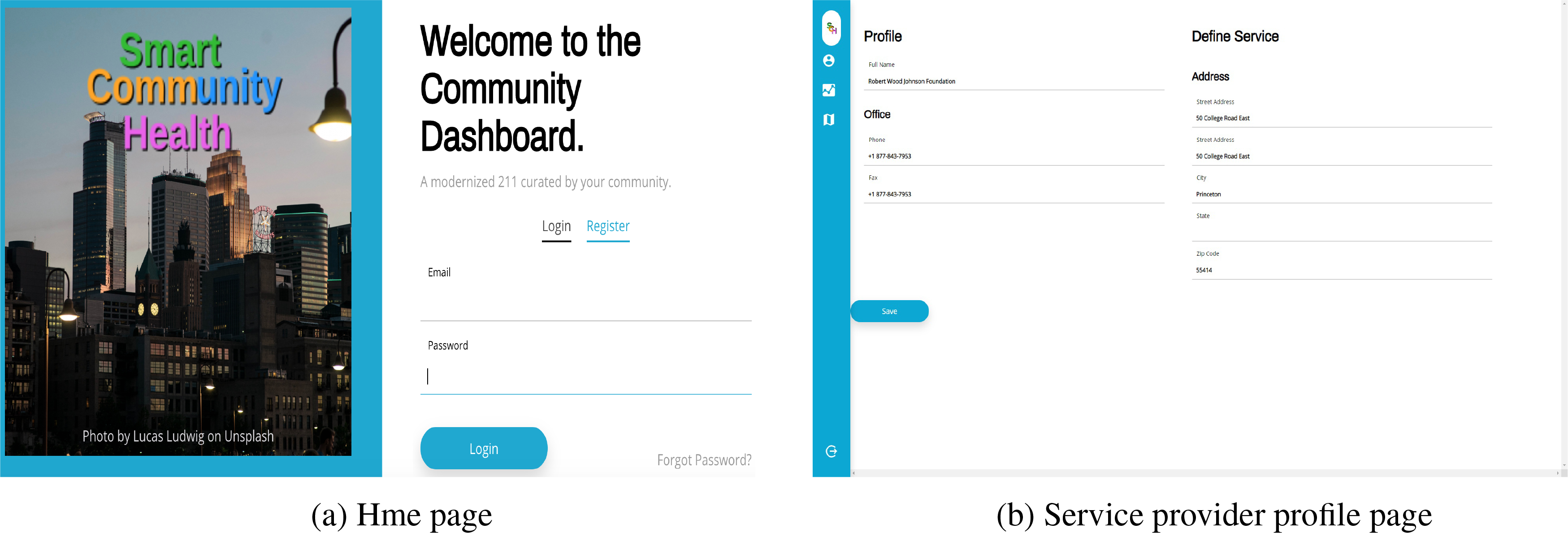
The Smart Community Health web app Community Dashboard component. Community service providers securely register and access this platform.
Figure 8:
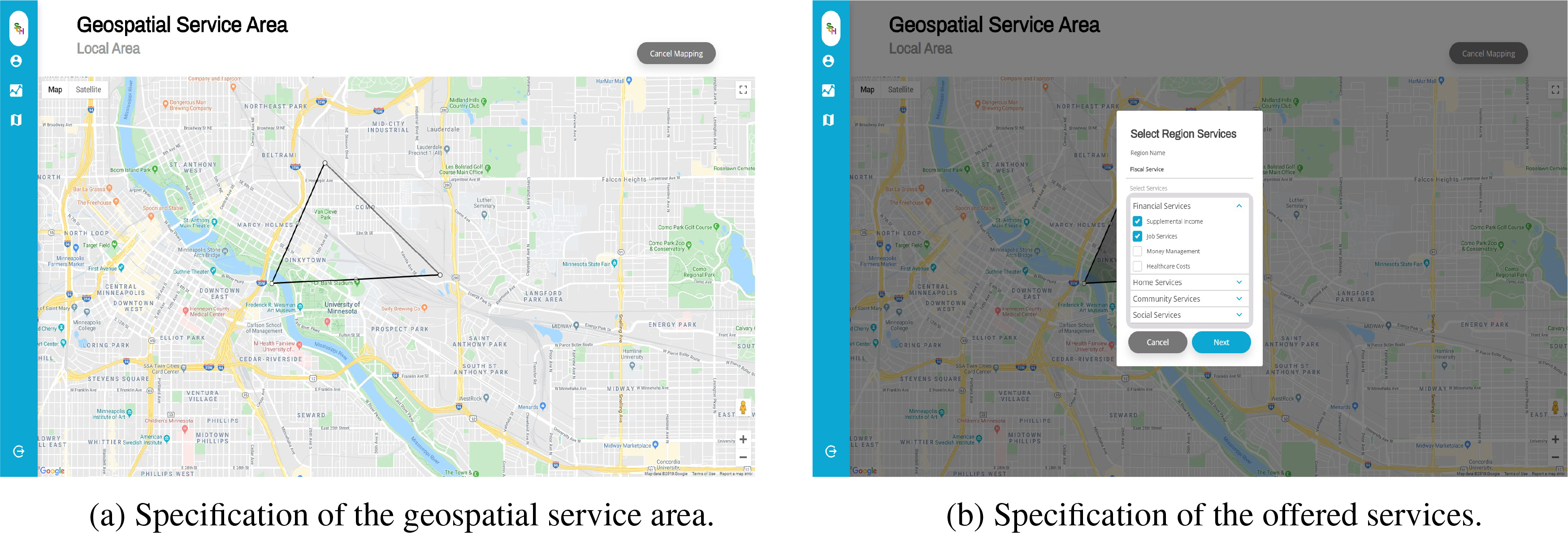
The Smart Community Health web app Community Dashboard component. Community Dashboard offers an interactive map allowing for polygon drawing.
Figure 9:
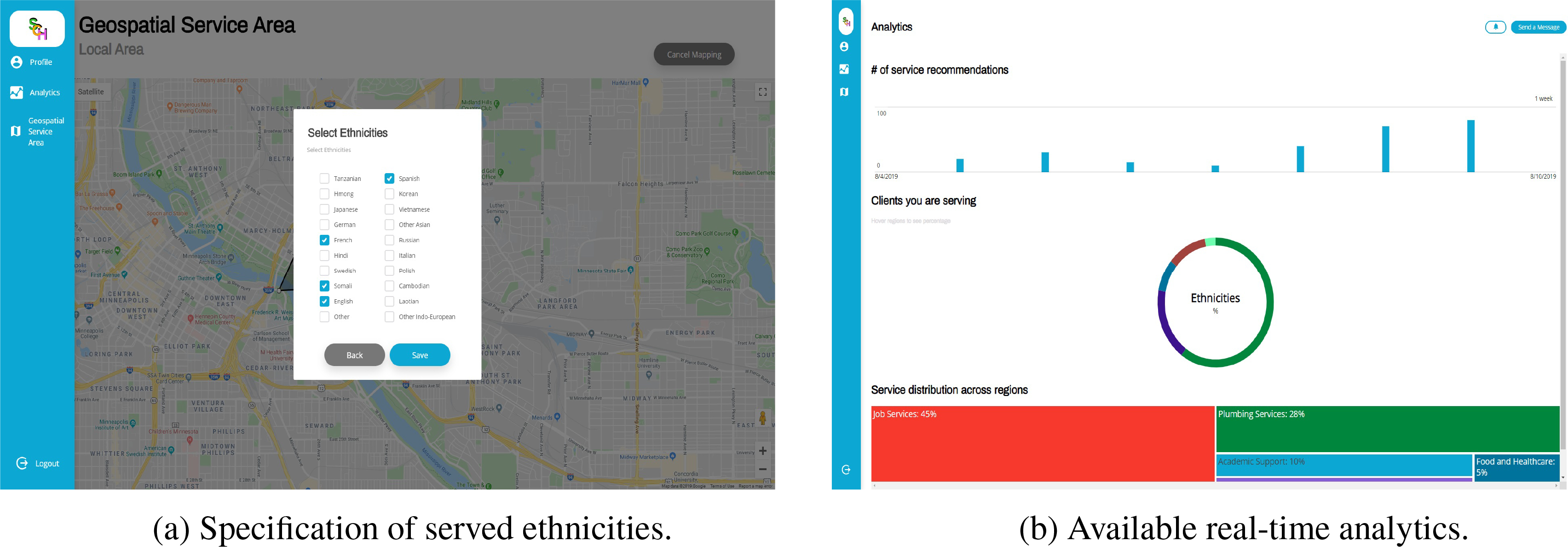
The Smart Community Health web app Community Dashboard component. Community service providers use this platform as a dashboard to track, control and manage their listed services.
The SCH Community Dashboard has been designed to address the needs from small, medium and large scale organizations. Large scale organization can hence define multiple branches, each servicing a specific geospatial area and helping a set of communities or ethnicities. For example, an organization like the Y (YMCA: Young Men’s Christian Association), a worldwide organisation that aims to put communities into practice by developing a healthy ”body, mind, and spirit”. Such a large organization counts 120 national associations worldwide and 2,700 separate local YMCA entities in the USA only. The capability of the SCH Community Dashboard to allow multiple entities management and yet a centralized control tp main entities make it a unique platform.
Using the SCH Community Dashboard, organizations can reach out to individuals who experience needs that can be addressed by their services. Organizations utilize the internal messaging, email and calendar services and benefit from the notification managing services for a closed-loop tracking of referrals. Finally, the SCH Community Dashboard provide organizations with a real-time analytics dashboard enabling full control, management and monitoring of provided services and serviced communities (see Figure 9b).
4. CONCLUSION
In this paper, we presented Smart Community Health, a full-service, end-to-end community service provider recommendation platform designed to help address pressing social, environmental, and health needs within our communities. The platform is composed of a mobile application for individuals looking for services and the Community Dashboard platform for service providers.
The mobile application integrates a health assessment tool that builds on top of an existing validated screening tool, My Strengths My Health. It generates international disease classification (ICD) codes that can be stored within all healthcare systems. Placing the assessment in the mobile app reduces the barrier to accessing services, because the app is freely available to anyone regardless of healthcare status or the organization they belong to. When participants use the assessment and indicate they have a need they are immediately presented with information connecting them to organizations that provide those services.
The Community Dashboard powers the mobile app assessment, by allowing community organizations to register services they provide into our application. It start by providing a suite of curated services from our partnered organizations, then it allows the community to add their “pop-up services”. It also provides community service providers with analytics for informed and meaningful actions. The Dashboard platform provides full-service analytics for organizations, allowing them to understand what is happening in their community. In particular, it focuses on providing a common framework that allows health providers and city planners to understand the spatial and temporal relationships between social determinants of health and health outcomes.
To conclude, the main contribution of Smart Community Health is it community focused design, its community curation, its community engaged approach and its advanced analytics that allow for a greater understanding of community needs.
5. FUTURE WORK
The development of the Smart Community Health platform has not finish yet. Several features and functionalities in the product backlog are still waiting for grooming to be addressed by the coming sprints. The coming steps will include a live pilot with a real community service provider and a representative focus group of actual users.
One of the areas we are interested in investigating is the assessment component. Although the SmartCommunity Health platform integrates a well-established health assessment tool that builds on top of an existing validated screening tool, My Strengths My Health. We believe emerging Artificial Intelligence technologies and more particularly conversational agents could benefit our platform. The term ‘Conversation Agent’ has come to mean a wide variety of systems with varying capabilities and purposes, with the underlying assumption that the agent participates in a human-machine dialog. Licklider’s ‘Man-machine symbiosis’ (Licklider, 1960) was one of the earliest discourses from a Human Computer Interaction (HCI) perspective that visualized humans interacting with machines in a natural manner. Research in conversation agents started with messaging-based chatbots, whose purpose was to maintain a conversation with a human user.
In the last decade, conversational agents started focusing more on utility, with the goal of accomplishing specific tasks. Nowadays, conversational agents range across several modalities, including speech (such as Siri, Alexa, Cortana), text-messaging (such as Domino’s, CNN, Pandorabots, Burberry, etc. found on Messenger, Slack, and/or Skype platform), and as multimodal embodied agents. Table 1 provides a summary of most popular text-messaging based CAs, called chatbots.
Table 1:
Timeline of Chatbot (Bieliauskas and Schreiber, 2017).
| Year | Timeline of Chatbots |
|---|---|
|
| |
| 1950 | Chatbots Revolution Concept of truly intelligent Machine |
| 1966 | Eliza – MIT – Simulate Human Conversation |
| 1972 | Parry- Added Conversational Strategy |
| 1988 | JABBERWACKEY- Simulate natural human Chat with Entertaining and Humorous Manner |
| 1992 | Dr. SBAITSO- Speech Synthesis Program |
| 1995 | Alice- Artificial Linguistic Internet Computer Entity – Heuristic Patten |
| 2001 | SMARTERCHILD- Fun Personalized network; Precursor to Apple’s SIRI |
| 2006 | IBM’s WATSON- Natural Language Processing; Machine Language |
| 2010 | SIRI- Apple’s IOS, Natural Language UI |
| 2012 | Google Now- uses natural language for google search on mobile |
| 2015 | Alexa- Amazon Echo Device; using language processing Algorithms |
| 2015 | CORTANA- Bing Search; Natural Voice; Different Language |
| 2016 | Facebook user bots |
| 2016 | TAY- Microsoft to mimic the speech and habit of teenage girl |
Using chatbots to engage individuals in a natural language based conversation will move our Smart Community Health platform from static assessments towards more dynamic evolutive and learning assessment approach.
Figure 1:
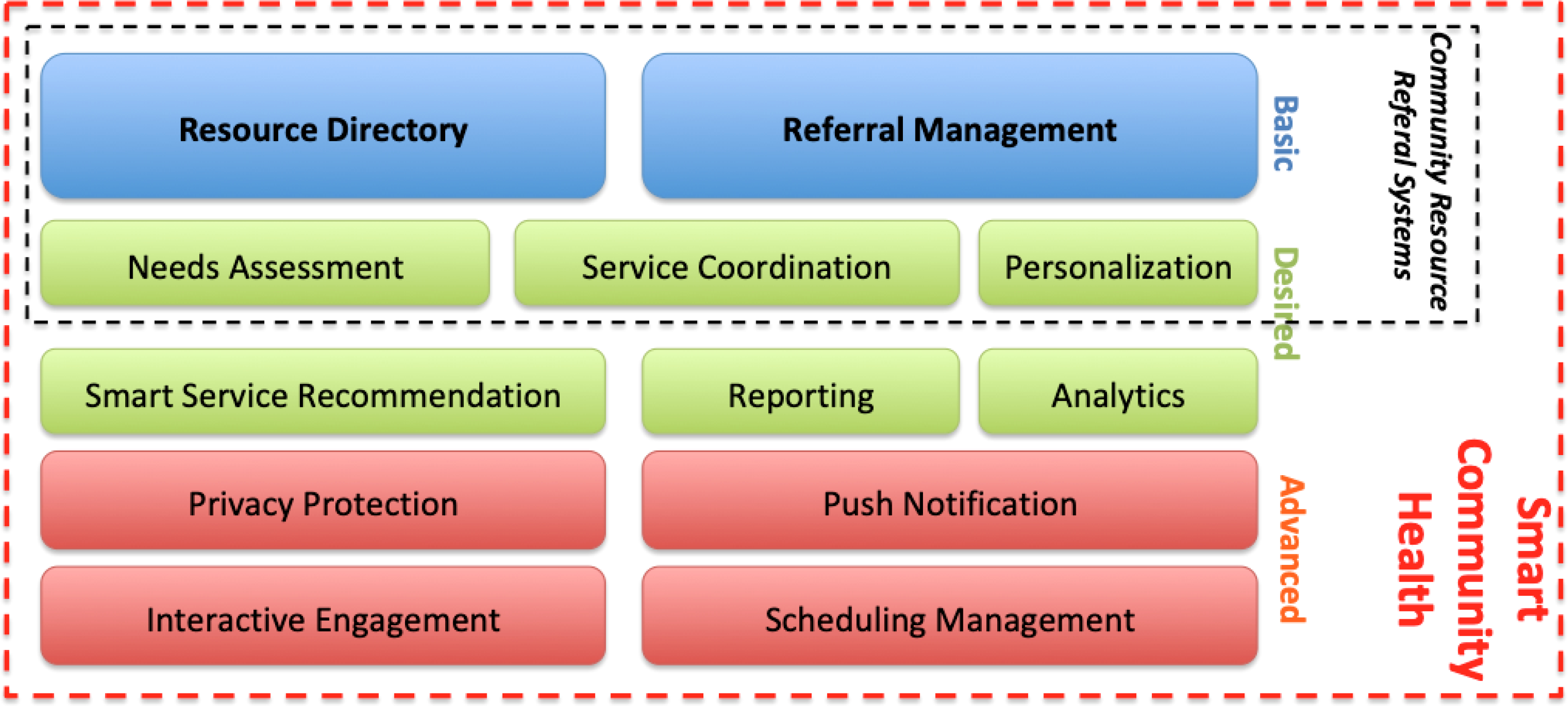
An overview of basic, desired and advanced functionalities of a community resource referral system. Smart Community Health outperforms the traditional platforms and offers advanced innovative features including push notification, interactive user engagement and scheduling functionalities.
REFERENCES
- Baby KT (2019). Generating internal motivation through mobile application technology. In Metacognition in Learning. IntechOpen. [Google Scholar]
- Bieliauskas S and Schreiber A (2017). A conversational user interface for software visualization. In 2017 IEEE Working Conference on Software Visualization (VISSOFT), pages 139–143. IEEE. [Google Scholar]
- BroadBandSearch (2018). Mobile Vs. Desktop Usage.
- Cartier Y, Fichtenberg C, and Gottlieb L (2019). Community resource referral platforms: A guide for health care organizations. Technical report, Social Interventions Research & Evaluation Network (SIREN).
- Cupala SJ, Ye L, and Garg N (2019). Selective update of core mobile device user interface through application marketplace. US Patent App. 10/235,155.
- Glinz M (2007). On non-functional requirements. In 15th IEEE International Requirements Engineering Conference (RE 2007), pages 21–26. IEEE. [Google Scholar]
- Gundersen C and Ziliak JP (2015). Food insecurity and health outcomes. Health affairs, 34(11):1830–1839. [DOI] [PubMed] [Google Scholar]
- Han Rebekah Wong S (2012). Which platform do our users prefer: website or mobile app? Reference Services Review, 40(1):103–115. [Google Scholar]
- Kaya A, Ozturk R, and Gumussoy CA (2019). Usability measurement of mobile applications with system usability scale (sus). In Industrial Engineering in the Big Data Era, pages 389–400. Springer. [Google Scholar]
- Kim S-H and Kim W-J (2019). Evaluation of software quality-in-use attributes based on analysis network process. Cluster Computing, 22(1):2101–2114. [Google Scholar]
- Koh HK, Piotrowski JJ, Kumanyika S, and Fielding JE (2011). Healthy people: a 2020 vision for the social determinants approach. Health Education & Behavior, 38(6_suppl):551–557. [DOI] [PubMed] [Google Scholar]
- Kovalcik J and Altman E (2019). Amazon web services (aws) & digital initiatives.
- Kushel MB, Gupta R, Gee L, and Haas JS (2006). Housing instability and food insecurity as barriers to health care among low-income americans. Journal of general internal medicine, 21(1):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licklider JC (1960). Ire transactions on human factors in electronics. online]. URL https://goo.gl/vndAUs (2017-11-13).
- Lurie N and Dubowitz T (2007). Health Disparities and Access to Health. JAMA, 297(10):1118–1121. [DOI] [PubMed] [Google Scholar]
- Mahalakshmi M and Sundararajan M (2013). Traditional sdlc vs scrum methodology—a comparative study. International Journal of Emerging Technology and Advanced Engineering, 3(6):192–196. [Google Scholar]
- Martin KS and Scheet N (1992). The omaha system. Applications for Community health nursing, page 1992.
- McGowan AK, Kramer K, and Teitelbaum JB (2019). Healthy people: The role of law and policy in the nation’s public health agenda. The Journal of Law, Medicine & Ethics, 47(2_suppl):63–67. [DOI] [PubMed] [Google Scholar]
- Molfenter T (2013). Reducing appointment no-shows: going from theory to practice. Substance use & misuse, 48(9):743–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- One Degree (2019). One Degree.
- Pang KL and Teh HS (2019). Mobile-based access control system. US Patent App. 16/059,537.
- Pieces Iris (2019). Pieces Iris.
- Pinpin MBG, Greathouse WE, Wall JJ, Kendall KL, and Li D (2019). User personalization of third-party webpage images. US Patent App. 10/248,812.
- Sen S, Spatscheck O, Huang J, Mao ZM, and Qian F (2019). Facilitation of mobile device resource optimization. US Patent App. 10/172,041.
- Shah JJ and Rogers MT (1988). Functional requirements and conceptual design of the feature-based modelling system. Computer-Aided Engineering Journal, 5(1):9–15. [Google Scholar]
- Smith T, Mattingly TJ, and Slabaugh L (2019). Improving health determinants outside of the clinic does not mean outside of clinical science. In Healthcare. Elsevier. [DOI] [PubMed] [Google Scholar]
- Smith WR, Betancourt JR, Wynia MK, Bussey-Jones J, Stone VE, Phillips CO, Fernandez A, Jacobs E, and Bowles J (2007). Recommendations for teaching about racial and ethnic disparities in health and health care. Annals of Internal Medicine, 147(9):654–665. [DOI] [PubMed] [Google Scholar]
- TAVHealth (2019). TAVHealth/TAVConnect.
- Unite Us (2019). Unite Us.


