Abstract
Background
Food allergy is a major health problem that significantly impacts quality of life (QoL). There is growing focus to evaluate food allergy‐related QoL and treatment options’ value beyond the clinical effectiveness perspective by engaging patients and caregivers. We aimed to identify and prioritize outcomes important to food allergy parents of children and patients allergic to milk, egg, and/or peanut, to guide comparative effectiveness research (CER) that focuses on evaluating food allergy treatment decisions.
Methods
We conducted a modified 3‐round Delphi study to identify and derive consensus on priority treatment outcomes for parents of children and adult patients with diagnosed allergies to at least one of three major allergenic foods (milk, egg, and peanut) from across the United States.
Results
Round 1 yielded 44 statements for round 2, and 39 statements reached the agreement level for round 3 ranking. Statements were organized under 4 sections: 1) food allergy problems, 2) treatment experiences, 3) important treatment outcomes, and 4) value of different treatment options.
Conclusion
Food allergy parents and patients face several social, psychological, medical, healthcare, financial, food selection, and awareness challenges. The areas of consensus on important treatment outcomes revealed shared priority for reducing the risk of potentially fatal allergic reactions and having reliable treatments. The most valued treatment options reflect hope for permanent cure and fear of serious allergic reactions.
Keywords: caregivers, comparative effectiveness research, delphi technique, food allergy, food hypersensitivity, quality of life
Key Message.
We identified and prioritized: 1) food allergy treatment outcomes and 2) value of different treatment options to food allergy patients and parents. Our results inform comparative effectiveness research that evaluates food allergy treatment outcomes and value. Further research should also compare sub‐groups of children caregivers and patients categorized by their relation to food allergy, that is, caregivers vs. patients, food allergy type, and duration and severity of the condition.
1. INTRODUCTION
Food allergy is a global health problem affecting about 8% of children and 5% of adults worldwide with higher and steadily rising prevalence in developed countries.1 In the United States (US), it is estimated that 7.6% of children and 10.8% of adults have food allergy.2, 3 Among the American children, the most prevalent food allergens are peanut (2.2%) followed by milk (1.9%) and shellfish (1.3%), while egg allergy affects 0.9%. About 39.9% of children with food allergy have multiple allergies to different types of food. Around 42.0% of allergic American children experienced a severe food allergy reaction at least once in their life, and 19.0% visited the emergency department due to a life‐threatening allergic reaction in the prior year.2
Food allergy is a chronic condition that significantly impacts quality of life (QoL) and can be fatal.4 The impact of food allergy on young children is higher than other age groups with repercussions on 1) the child's own perception of the condition, 2) parents’ proxy perception of their child's illness, 3) the child caregiver experience, and 4) parents’ and families’ day‐to‐day life.5 Thus, the societal, psychological, and economic burdens of food allergy impact multiple stakeholders including patients, parents and caregivers, schools and childcare facilities, workplaces, healthcare systems, and the food industry.6
On comparing food allergy QoL in the United States vs. Europe, a population‐based study used the Food Allergy Quality of Life Questionnaire‐Parent Form (FAQLQ‐PF) found that American parents of food‐allergic children had higher clinical impact and lower QoL in comparison to their European counterparts. In both groups, the impact increased with the child's age and the number of food allergies.7
The benefit of food allergy treatments does not come without financial costs and adverse events. For example, the Institute for Clinical and Economic Review found in 2019 satisfactory desensitization effectiveness of two oral immunotherapies (OIT) for peanut allergy. However, the annual cost‐effectiveness limits of these two therapies were $1,508 and $2,369, and their adverse events included systematic allergic reactions, need for epinephrine, and other side effects leading to discontinuation of therapy.8
Universally, there is a growing focus on Patient‐Centered Outcomes Research (PCOR) that helps patients and caregivers make informed healthcare decisions and incorporates their opinions in assessing healthcare options’ value. To support this research direction, the US Patient‐Centered Outcomes Research Institute (PCORI) funds more research investigating comparative effectiveness research (CER) from the patients and caregivers’ perspectives.9 Particularly for food allergy, there is an urgent need to evaluate QoL and treatment value beyond the clinical effectiveness perspective via engaging patients and caregivers to add their insights of the psychological, societal, and economic aspects of the problem.10 Food allergy QoL assessment tools have been using food allergy QoL surveys7, 11, 12; however, there are no specific food allergy treatment value measures guided by food allergy patients and caregivers’ experiences, challenges, needs, and desired outcomes.5, 10 To develop these guided food allergy‐specific measures, PCOR is needed to evaluate and prioritize outcomes important to patients and caregivers.13 In turn, the prioritized treatment outcomes can guide CER that generates evidence on comparing the benefits and harms of alternative food allergy treatments for better informed individual‐ and population‐level decisions.14
In order to guide CER that evaluates food allergy treatment decisions, we conducted a modified 3‐round Delphi study to identify and derive consensus on priority treatment outcomes and value of different treatment options.
2. METHODS
2.1. Study design
We conducted a modified 3‐round Delphi study to identify and derive consensus on priority treatment outcomes and value of different treatment options for parents of children and adults with food allergy to milk, egg, and/or peanut. The Delphi technique is a multi‐round survey process used to seek opinions and develop consensus among a defined group of subject matter experts about controversial or limited evidence topics.15 Specifically, rank‐ordering techniques have been identified as one of the most reliable and valid instruments for measuring food allergy‐related QoL.5
2.2. Study participants
For purposes of this study, patient and caregiver experience with food allergy was considered the primary inclusion criteria as panelists were considered experts based on real‐world experience.16 The Asthma and Allergy Foundation of America (AAFA), a national non‐profit patient advocacy organization, identified and assembled a panel of parents of children with food allergy and adult patients from its national advocacy and support national network across the United States. The panelists were assembled from 3 major food allergy groups: milk, egg, and peanut, to capture a wide range of experiences and opinions. Panelists were invited and communicated via emails throughout the Delphi process. We aimed to recruit 10‐15 panelists from each of the 3 allergy groups to capture a wide range of opinions and judgments and balance group dynamics. We targeted a response rate of at least 80% for each round, and thus, a round was not considered complete for analysis until the 80% threshold was reached.
2.3. Data collection
Between January and March 2020, we used Qualtrics® software (Qualtrics, Provo, UT, USA) to collect the panelists’ anonymous responses to the 3‐round survey. Round 1 included a brief demographic survey followed by open‐ended questions on 1) problems encountered by food allergy patients or parents, 2) food allergy treatment experience, 3) important food allergy treatment outcomes, and 4) value of effective food allergy treatment.
2.4. Data analysis
We analyzed round 1 using NVivo 12® software following the grounded theory and a stepwise thematic analysis. Two researchers (JM and MA) independently coded the responses then grouped them into conceptual themes to develop round 2 statements supported with examples from the panelists’ round 1 responses. Round 2 statement was provided against 4‐point Likert‐scale agreement rating in addition to a space for general comments. We sought an agreement (Agree and Strongly Agree) percentage of ≥75 to be determined a consensus for inclusion in the final round. Round 3 asked the panelists to rank consensus statements according to their importance. We assessed round 3 mean rankings and levels of agreement among the panelists using Kendall's coefficient of concordance in Microsoft Excel®.
3. RESULTS
Forty‐five panelists participated in the first round of our survey (Table 1). Forty of these panelists responded to each of the second and third rounds (88.9%). An overview of the Delphi process is presented in Figure 1.
TABLE 1.
Characteristics of participants in a delphi panel on the value of treatment for food allergy (n = 45)
| Mean age* (±SD) | 40.93 (±7.13) | ||
|---|---|---|---|
| Variable | Level | Frequency | Percentage |
| State of Residency | Massachusetts | 5 | 11.1% |
| California | 4 | 8.9% | |
| North Carolina | 4 | 8.9% | |
| Florida | 3 | 6.7% | |
| Pennsylvania | 3 | 6.7% | |
| District of Columbia | 2 | 4.4% | |
| Maryland | 2 | 4.4% | |
| Missouri | 2 | 4.4% | |
| New York | 2 | 4.4% | |
| Ohio | 2 | 4.4% | |
| Texas | 2 | 4.4% | |
| Virginia | 2 | 4.4% | |
| Arkansas | 1 | 2.2% | |
| Alabama | 1 | 2.2% | |
| Connecticut | 1 | 2.2% | |
| Illinois | 1 | 2.2% | |
| Minnesota | 1 | 2.2% | |
| Nebraska | 1 | 2.2% | |
| New Jersey | 1 | 2.2% | |
| Nevada | 1 | 2.2% | |
| Oregon | 1 | 2.2% | |
| Tennessee | 1 | 2.2% | |
| Washington | 1 | 2.2% | |
| Wisconsin | 1 | 2.2% | |
| Gender | Female | 42 | 93.3% |
| Male | 3 | 6.7% | |
| Relation to food allergy | Parent of a child with food allergy | 37 | 82.2% |
| Both Patient and Parent of a child with food allergy | 5 | 11.1% | |
| Patient with food allergy | 3 | 6.7% | |
| Type of food allergy | Peanut allergy | 13 | 28.9% |
| Milk allergy | 2 | 4.4% | |
| Egg allergy | 3 | 6.7% | |
| Peanut and milk allergy | 2 | 4.4% | |
| Peanut and egg allergy | 9 | 20.0% | |
| Milk and egg allergy | 5 | 11.1% | |
| Peanut, milk, and egg allergy | 11 | 24.4% | |
One participant did not report her age.
FIGURE 1.

Overview of delphi process
Round 1 yielded 44 statements for round 2 organized under 4 sections: 1) food allergy problems, 2) treatment experiences, 3) important treatment outcomes, and 4) value of treatment and the quantitative value of different treatment options.
Thirty‐nine statements reached the targeted agreement level ranging between 77.5% and 100% (Table 2). On quantifying the value of different treatment options, the order of these options according to their average scores is 1) permanently cures food allergy, 2) reduces the risk of serious anaphylaxis, 3) reduces the risk of accidental exposure to small quantities of the allergen, 4) increases food options for patients, 5) allows a food allergy patient to participate in social activities with less fear, 6) allows a food allergy patient to have less anxiety about food, and 7) reduces the risk of mild or moderate allergic reactions (Table 3).
TABLE 2.
Levels of agreement on round 2 statements of a delphi panel on the value of treatment for food allergy
| Topic | Statement and examples* | Agreement percentage |
|---|---|---|
|
Social Activities Patients with food allergy experience problems with… |
…travel.” (Examples include extra planning required, barriers or limitations to travel, difficulty finding travel options that can cater to a food allergy patient's needs.) |
97.50% |
|
… eating or dining at restaurants.” (Examples include restricted eating options, inability to eat full ingredients of offered meals, cross contamination during food handling, restaurants hosting social events do not allow outside food.) |
97.50% | |
|
… social isolation.” (Examples include child feeling ‘left out’ of group activities, inability to attend birthday parties or other activities with friends like ball games or movies at movie theaters, unable to attend summer camps, forced to eat at a separate table from friends.) |
87.50% | |
|
… support from school or childcare services.” (Examples include inadequate supervision and attention to allergic children.) |
80.00% | |
| Psychological Problems |
“Parents of children with food allergy experience anxiety on daily basis.” (Examples include fear of child having allergic reactions; preparing safe food alternatives; and responding to allergic children questions about allergy consequences.) |
97.40% |
|
“Patients with food allergy experience anxiety on daily basis.” (Examples include fear of allergic reactions, accidental exposure, and cross contamination; preparing safe food alternatives.) |
89.70% | |
|
“Parents of children with food allergy experience the feeling of guilt.” (Examples include wondering if taking antibiotics during late pregnancy that lead to the child food allergy.) |
56.4%** | |
|
Medical Problems Patients with food allergy experience problems… |
… as moderate allergic reactions.” (Examples include skin rashes and blisters, itchiness, running nose, sore throat, swelling of the eyes and lips, nausea, diarrhea, sleeplessness.) |
92.50% |
|
… as severe anaphylaxis reactions.” (Examples include delayed or unexpected anaphylactic reaction; rapid shortness of breath; severe tongue or throat swelling.) |
90.00% | |
|
… with growth.” (Examples include: A child with small stature as a result of food allergy and food avoidance.) |
67.5%** | |
|
… with eating disorders.” (Examples include: Potential anorexia after a traumatic experience with food.) |
47.5%** | |
|
Healthcare Problems Patients with food allergy experience problems with… |
… providers not being adequately trained or educated on food allergy.” (Examples include prescribing medications that contain allergens, lack of awareness about advanced or curative treatments for allergy, non‐specialists who delay allergy diagnosis.) |
87.50% |
|
… ensuring an epinephrine autoinjector or other necessary medication or device is available.” (Examples include finding epinephrine autoinjector for children, properly stored epinephrine autoinjector.) |
82.50% | |
|
… scheduling, accessing an appropriately trained provider, or managing all appointments.” (Examples include keeping current on all appointments, securing free time for OIT weekly treatment, scheduling appointments after each other like pediatrician before allergy specialists, preparing medical records for school.) |
67.5%** | |
|
… providers not taking their allergy seriously.” (Examples include emergency room providers prescribe Benadryl instead of Epinephrine autoinjector for severe reactions.) |
65.0%** | |
|
Financial Problems Patients with food allergy experience problems with… |
… pharmacy costs.” (Examples include costs for epinephrine autoinjectors, OIT, antihistamines.) |
92.50% |
|
… food costs.” (Examples include expensive allergen friendly food in grocery stores and restaurants.) |
90.00% | |
|
… medical costs.” (Examples include doctor's appointments, emergency room visits, urgent care.) |
87.50% | |
|
… non‐health care costs.” (Examples include extra expenses relating to vacations, child‐care.) |
77.50% | |
|
Food Selection Patients with food allergy experience problems with… |
… finding safe food.” (Examples include need to call the manufacturer to see if product is safe.) |
95.00% |
|
… impacting the rest of the family's diet.” (Examples include balancing the needs of the patient with his or her siblings.) |
92.50% | |
|
… food preparation.” (Examples include: Spending additional time to prepare all meals, additional time learning new recipes, planning meals.) |
89.70% | |
|
Food Allergy Awareness Patients with food allergy experience problems with… |
… family and friends being aware of their needs.” (Examples include others not taking allergy seriously, not understanding cross contamination, not aware how to use Epinephrine autoinjector or other allergy medications.) |
95.00% |
|
… school or childcare employees being aware of their needs.” (Examples include providing allergic food to children, lack of training on how to use epinephrine autoinjector when needed.) |
85.00% | |
|
Food Allergy Diagnosis Patients with food allergy experience problems with… |
… food allergy diagnostic tests.” (Examples include limited tests that patients can't do due to contraindications, inaccurate tests, tests that cause delayed allergic reactions.) |
80.00% |
|
… reaching definite allergy diagnosis.” (Examples include babies with allergy who don't have typical symptoms, some physicians don't allow babies to take some tests below certain ages, allergy diagnosis takes long time.) |
77.50% | |
|
Food Allergy Treatment Patients with food allergy experience… |
… inconvenient treatment experience.” (Examples include carrying epinephrine autoinjector and inhalers all time, rest periods required for OIT.) |
90.0% |
|
… limited treatment options.” (Examples include ineffective treatments for infants and young children, having Eosinophilic esophagitis (EoE) makes patients ineligible to take OIT, better treatments are not located everywhere.) |
90.0% | |
|
… unsatisfactory treatments.” (Examples include there is no preventive treatment and avoidance is the only way for prevention, treatments respond only to allergic reaction and there is no curative treatment available.) |
85.0% | |
| Important Treatment Outcomes | “Treatments that lessen the risk of anaphylaxis (a potentially life‐threatening allergic reaction) are important to food allergy patients.” | 100.00% |
| “Treatments that lessen the risk of moderate allergic reactions (like skin rash, itching, and sore throat) are important to food allergy patients.” | 100.00% | |
| “Treatments that lessen the risk of cross contamination or accidental exposure to little amounts of allergens are important to food allergy patients.” | 97.50% | |
|
“Treatments that have been thoroughly investigated in clinical trials are important to food allergy patients.” (Examples include OIT that have been well‐investigated without drop‐outs due to side‐effects during the clinical trial.) |
97.50% | |
| “Convenient treatments are important to food allergy patients.” (Examples include treatments that does not cause pain, easy to administer by anyone like a family member or a caregiver, doesn't require rest period.) | 97.50% | |
| “Reliable treatments (work every time without doubt) are important to food allergy patients.” | 97.50% | |
|
“Treatments that improves tolerance to allergic food are important to food allergy patients.” (Examples include ability to eat small amounts of egg or milk, make small amounts of allergic food not life‐threatening, enables more dietary options.) |
95.00% | |
| “Treatments with less side‐effects are important to food allergy patients.” | 95.00% | |
| Value of Different Treatments | reduce the risk of serious anaphylaxis (a potentially life‐threatening allergic reaction) | 97.50% |
| increases the food options for food allergy patients | 97.50% | |
| would allow food allergy patients to participate in social activities with less fear | 97.50% | |
| permanently cures the allergy | 95.00% | |
| reduce the risk of mild or moderate allergic reactions (eg, skin rash, itching, runny nose, mild swelling) | 95.00% | |
| reduce the risk of a reaction to accidental exposure of small quantities of the allergen | 95.00% | |
| does not cure the allergy but allows food allergy patients to have less anxiety about food | 92.50% |
Round 2 examples were rephrased from the panelists’ responses in round 1.
Failed to reach agreement, which was defined as a concurrence of 75% or more for the responses agree or strongly agree (5 statements out of 44 statements).
TABLE 3.
Rating of round 2 statements on different food allergy treatment values (0 = No value at all, 100 = Maximum value or priceless)
| Mean value (± SD) | |
|---|---|
| Food allergy treatment that… | |
| … permanently cures food allergy | 98.2 (±5.82) |
| … reduces the risk of serious anaphylaxis | 96.0 (±10.98) |
| … reduces the risk of accidental exposure to small quantities of the allergen | 88.3 (±15.08) |
| … increases the food options for a patient | 85.7 (±19.17) |
| … would allow food allergy patient to participate in social activities with less fear | 84.0 (±20.16) |
| … allows food allergy patient to have less anxiety about food | 82.8 (±17.82) |
| … reduces the risk of mild or moderate allergic reactions | 81.2 (±19.01) |
In round 3, concordance assessment showed that the ranking for food allergy treatment values had the highest level of consensus (W = 0.4), while the lowest consensus was found in ranking the two statements on food allergy awareness (W = 0.002) (Table 4).
TABLE 4.
Final rankings of statements of a delphi panel on the value of treatment for food allergy
| Topic | Item/Characteristic | Rank | Mean (±SD) | W * |
|---|---|---|---|---|
| Social Activities | Eating or dining at restaurants | 1 | 2.2 (±1.02) | 0.07 |
| Support from school or childcare services | 2 | 2.2 (±1.2) | ||
| Social Isolation | 3 | 2.5 (±1.09) | ||
| Travel | 4 | 3.0 (±0.97) | ||
| Psychological | Parent's anxiety | 1 | 1.2 (±0.42) | 0.3 |
| Patient's anxiety | 2 | 1.8 (±0.42) | ||
| Medical | Severe anaphylaxis reactions | 1 | 1.4 (±0.49) | 0.02 |
| Moderate allergic reactions | 2 | 1.6 (±0.49) | ||
| Healthcare | Providers’ inadequate training on food allergy | 1 | 1.3 (±0.46) | 0.2 |
| Availability of necessary food allergy medications or devices | 2 | 1.7 (±0.46) | ||
| Financial | Food costs | 1 | 1.9 (± 0.96) | 0.2 |
| Pharmacy costs | 2 | 2.4 (± 1.12) | ||
| Medical costs | 3 | 2.5 (±1.03) | ||
| Non‐health care costs | 4 | 3.3 (± 0.90) | ||
| Food Selection | Finding safe food | 1 | 1.4 (± 0.66) | 0.3 |
| Food preparation | 2 | 2.2 (± 0.63) | ||
| Impacting the rest of the family's diet | 3 | 2.4 (± 0.77) | ||
| Food Allergy Awareness | School or childcare employees | 1 | 1.5 (± 0.50) | 0.002 |
| Family and friends | 2 | 1.5 (± 0.50) | ||
| Food Allergy Diagnosis | Diagnostic tests | 1 | 1.4 (± 0.48) | 0.09 |
| Reaching definite allergy diagnosis | 2 | 1.7 (± 48) | ||
| Food Allergy Treatment | Unsatisfactory treatments | 1 | 1.9 (± 0.75) | 0.02 |
| Limited treatment options | 2 | 2.0 (± 84) | ||
| Inconvenient treatment experience | 3 | 2.2 (± 83) | ||
| Important Treatment Outcomes | Reducing the risk of anaphylaxis (a potentially life‐threatening allergic reaction) | 1 | 2.0 (± 1.41) | 0.3 |
| Reliable treatments | 2 | 4.0 (± 2.42) | ||
| Reducing the risk of mild or moderate allergic reactions | 3 | 4.3 (± 1.85) | ||
| Reducing the risk of cross contamination or accidental exposure to small quantities of the allergen | 4 | 4.4 (± 1.93) | ||
| Improving tolerance to allergic food | 5 | 4.6 (± 2.07) | ||
| Reducing side‐effects | 6 | 5.4 (± 1.80) | ||
| Thoroughly investigated in clinical trials | 7 | 5.4 (± 2.00) | ||
| Convenient treatments | 8 | 6.1 (± 2.15) | ||
| Value of Different Treatments | Permanently cures the allergy | 1 | 2,0 (± 1.82) | 0.4 |
| Reducing the risk of serious anaphylaxis | 2 | 2.4 (± 1.24) | ||
| Reducing anxiety about food | 3 | 3.8 (± 1.53) | ||
| Reducing the risk of a reaction to accidental exposure of small quantities of the allergen | 4 | 4.6 (± 1.58) | ||
| Reducing the risk of mild or moderate allergic reactions | 5 | 4.6 (± 1.61) | ||
| Increasing food options for food allergy patients | 6 | 5.2 (± 1.56) | ||
| Allowing food allergy patients to participate in social activities with less fear | 7 | 5.6 (± 1.43) |
Kendall's coefficient (W) calculated to evaluate confidence in ranks.
4. DISCUSSION
We engaged parents of children with food allergy and adult patients in a 3‐round Delphi panel survey to identify and prioritize important food allergy outcomes and valued treatments to guide future CER (Figure 2). Two key findings emerged from this study. First, food allergy parents and patients face several challenges revolving around social, psychological, medical, healthcare, financial, food selection, and awareness problems. Second, our panel agreed that the current treatments for food allergy are unsatisfactory, offer limited options, and are inconvenient. The areas of consensus and ranking of important treatment outcomes revealed are reducing the risk of fatal allergic reactions and having reliable treatments. The most valued treatment options reflect hope for permanent cure and fear of serious allergic reactions.
FIGURE 2.
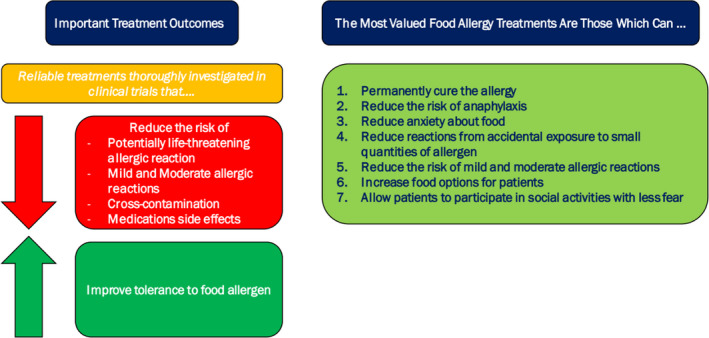
Panelists’ important treatment outcomes and most valued treatments
Overall, our panel identification and enumeration of different social challenges confirm their importance and echo the findings of two previous surveys on the social challenges of food allergy.12, 17 Our panel ranked these social challenges putting “eating at restaurants” on the top of the list. A previous survey supports this prioritization, where 53% of food allergy families reported leaving a restaurant in the middle of dining, and 89% avoided certain restaurants.17 This finding can be relevant to the fact that no formal training on food allergy is required for restaurant employees who learn about the problem during on‐job ad hoc training.18
The second social challenge, school or childcare services, has been found in a previous study as a leading factor for food allergy parents to become a school volunteer or attend a school field trip for close monitoring of their child (61% and 69% of survey respondents), change their child's school (25% of respondents), or even decide to homeschool (18% of respondents).17 Social isolation, our panel's third rank, was discussed in two previous surveys where families in the first survey reported experiencing social isolation and limited social activities in different ways,17 while the second survey identified social limitation was the only consistent factor for food allergy implications according to food allergy caregivers.12 The fourth challenge was travel which was previously reported in different ways: canceling vacation plans (57% of respondents) and avoiding airline travel (43% of respondents).17
Final ranking of psychological challenges put the anxiety experienced by parents of allergic children above the anxiety of adult patients. One interpretation could be the higher percentage of food allergy parents in our panel (93.3% are either parents or both parents and patients). The higher ranking of parents’ anxiety is consistent with a study that revealed mothers of food allergy children have higher anxiety and stress levels in comparison to mothers of asthmatic children and control groups. In that study, anxiety and stress were related to history of anaphylaxis, parents’ continuous stress about their children, and the effects of food allergy on the family relations and financial conditions.19 This finding supports the inclusion of caregiver burden or other spillover effects observed when evaluating the comparative cost‐effectiveness of any interventions in food allergy.
The ranking of medical challenges showed that severe and moderate allergic reactions are agreed on and prioritized and may reflect the adaptation to mild reactions. Providers’ inadequate training on food allergy was ranked first in the healthcare challenges and could be attributed to the first‐round examples of prescribing medication that contain allergens, lack of awareness about advanced or curative treatments for allergy, and delayed diagnosis by non‐specialists. Unavailability of necessary medications such as pediatrics epinephrine autoinjector and properly stored autoinjector also presented significant challenges.
The panel agreed that several costs are challenging to food allergy patients and parents including food, pharmacy, medical, and non‐healthcare costs related to vacations and special childcare. Food costs received the highest rank and confirm previous findings that showed allergy‐safe food is priced higher than regular food resulting in higher financial burden on food allergy families.17 In the same line, our panel agreed on other food‐related challenges including finding and preparing safe food, and interference with the family diet. When considering the economic value of potential interventions for food allergy patients, costs outside of the typical “health system” frequently covered by health insurance may need to be considered.
Our panel agreement on pharmacy and medical costs is not surprising; several qualitative and quantitative studies report higher costs of food allergy medications and added costs of medical visits due to food allergy, including emergency room visits.17, 20 Additionally, it is estimated that the annual direct medical costs attributed to pediatric food allergy are $4.3 billion.21
Food allergy awareness was prioritized by our panel which agreed on the challenges of lack of awareness among school and childcare employees, and family and friends. School personnel awareness is a challenge reported elsewhere; a study conducted with public elementary schools found that 52% relied on parents to educate school personnel on their children food allergy, 16% only had written individual emergency plans for food allergy, 11% had no methods for educating their staff on food allergy, and 9% posted food service notices.22 Educational strategies to improve food allergy awareness may help reduce the fear parents face when they leave their children at school or at daycare, but complex educational interventions may be difficult to assess.
Diagnostic tests and reaching definite allergy diagnosis were agreed upon as major challenges. Panelists elaborated on these challenges by discussing diagnostic tests’ contraindications, inaccurateness, delayed results, and delayed allergic reactions to some of these tests. These findings are not surprising as accurate diagnosis, and consequently prevalence estimates, of food allergies remains a challenge due the nature of the current diagnostic tests.23
Our panel agreed that the current treatments for food allergy are unsatisfactory, offer limited options, and are inconvenient. Agreement and ranking of important treatment outcomes revealed that reducing the risk of anaphylaxis is the top priority followed by the reliability of food allergy treatments. Interestingly, the order of different treatment options’ value in round 2 differed from their final ranking in round 3. However, the two treatment options: “permanently cures the allergy” and “reducing the risk of serious anaphylaxis” had the highest mean values (98.2 ± 5.82, and 96.0 ± 10.98) in round 2 and ranked first and second in round 3.
This study confirms previous findings that food allergy patients and caregivers experience various health and economic burdens frequently outside standard healthcare services (eg, food, special childcare, travel).21, 24, 25 Our study further demonstrates the potential spillover effects experienced by caregivers of young children with food allergies. In pediatric economic evaluations, incorporating family spillover effects and health outcomes is substantial and makes health interventions more cost‐effective.26 In the case of food allergy, our panel rated parental anxiety as an important psychological consideration. To our knowledge, the economic burden specific to these parental health effects attributable to pediatric food allergy has not been evaluated.
In conclusion, our findings support future research that develops food allergy‐specific measures for evaluating allergy treatment options’ value and desired outcomes. Further research should also compare sub‐groups of children caregivers and patients categorized by their relation to food allergy, that is, caregivers vs. patients, food allergy type, and duration and severity of the condition.
Our study has some limitations. First, since we included mainly parents of allergic children and very few adult patients, the two different experiences may have impacted the homogeneity of our panel. Second, although we included a relatively large and geographically diverse national sample of food allergy patients and caregivers, the Delphi panel selection was purposeful and not intended to be completely representative but rather diverse enough to capture all salient themes. We also acknowledge that some themes may be relevant to the US context, e.g., healthcare economics, access to medical services, availability, and costs of treatments. The third limitation is specific to the Delphi technique which lacks in‐person discussions among the panelists. In‐person discussions may produce more interactive and reassessed ideas and perspectives.
CONFLICTS OF INTEREST
Sanaz Eftekhari, Hannah Jaffee, and Melanie Carver are employed by the Asthma and Allergy Foundation of America (AAFA), a non‐profit patient organization, which has received food allergy‐related funding from Aimmune, DBV Technologies, Genentech, kaléo, Mylan, Pfizer, and PhRMA.
AUTHOR CONTRIBUTION
Moaz Abdelwadoud: Conceptualization (equal); Data curation (equal); Formal analysis (lead); Methodology (equal); Project administration (equal); Resources (lead); Software (lead); Writing‐original draft (lead). Sanaz Eftekhari: Conceptualization (equal); Data curation (equal); Investigation (equal); Project administration (equal); Validation (equal); Writing‐review & editing (equal). Hannah Jaffee: Conceptualization (equal); Investigation (equal); Writing‐review & editing (equal). Melanie Carver: Conceptualization (equal); Investigation (equal); Writing‐review & editing (equal). T. Joseph Mattingly II: Conceptualization (equal); Formal analysis (equal); Project administration (equal); Resources (lead); Supervision (lead); Validation (lead); Writing‐review & editing (equal).
ETHICAL APPROVAL
Our study received exempt approval from The University of Maryland Baltimore Institutional Review Board.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/pai.13464.
ACKNOWLEDGMENT
The authors would like to thank the panelists for their invaluable inputs.
Abdelwadoud M, Eftekhari S, Jaffee H, Carver M, Mattingly TJ II. Food allergy treatment value: Child caregiver and patient perspectives. Pediatr Allergy Immunol. 2021;32:1039–1048. 10.1111/pai.13464
Editor: Motohiro Ebisawa
Funding information
This work was funded by Pharmaceutical Research and Manufacturers of America (PhRMA) Foundation, Washington, DC.
REFERENCES
- 1.Sicherer SH, Sampson HA. Food allergy: epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133(2):291‐307.e5. [DOI] [PubMed] [Google Scholar]
- 2.Gupta RS, Warren CM, Smith BM, et al. The public health impact of parent‐reported childhood food allergies in the United States. Pediatrics. 2018;142(6):e20181235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta RS, Warren CM, Smith BM, et al. Prevalence and severity of food allergies among US adults. JAMA Netw open. 2019;2(1):e185630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010;125(2 SUPPL. 2): 10.1016/j.jaci.2009.08.028 [DOI] [PubMed] [Google Scholar]
- 5.Greenhawt M. Food allergy quality of life and living with food allergy. Curr Opin Allergy Clin Immunol. 2016;16(3):284‐290. 10.1097/ACI.0000000000000271 [DOI] [PubMed] [Google Scholar]
- 6.Dyer A, Negris O, Gupta R, Bilaver L. Food allergy: how expensive are they? Curr Opin Allergy Clin Immunol. 2020;20(2):188‐193. [DOI] [PubMed] [Google Scholar]
- 7.DunnGalvin A, Koman E, Raver E, et al. An examination of the food allergy quality of life questionnaire performance in a countrywide American sample of children: cross‐cultural differences in age and impact in the United States and Europe. J Allergy Clin Immunol Pract. 2017;5(2):363‐368.e2. [DOI] [PubMed] [Google Scholar]
- 8.Tice JA, Guzauskas GF, Hansen RN, et al. The effectiveness and value of oral immunotherapy and Viaskin peanut for peanut allergy a summary from the Institute for Clinical and Economic Review’s California Technology Assessment Forum. J Manag Care Spec Pharm. 2020;26(5):620‐623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patient‐Centered Outcomes Research Institute . Our Programs. https://www.pcori.org/about‐us/our‐programs. Published 2017. Accessed December 20, 2020.
- 10.Polk BI, Dinakar C. Patient‐centered outcomes in food allergy. Curr Allergy Asthma Rep. 2017;17(6): 10.1007/s11882-017-0708-z [DOI] [PubMed] [Google Scholar]
- 11.Allen CW, Bidarkar MS, Vannunen SA, Campbell DE. Factors impacting parental burden in food‐allergic children. J Paediatr Child Health. 2015;51(7):696‐698. [DOI] [PubMed] [Google Scholar]
- 12.Springston EE, Smith B, Shulruff J, Pongracic J, Holl J, Gupta RS. Variations in quality of life among caregivers of food allergic children. Ann Allergy, Asthma Immunol. 2010;105(4):287–294.e3. [DOI] [PubMed] [Google Scholar]
- 13.Frank L, Basch E, Selby JV. The PCORI perspective on patient‐centered outcomes research. JAMA ‐ J Am Med Assoc. 2014;312(15):1513‐1514. [DOI] [PubMed] [Google Scholar]
- 14.Sox HC. Defining comparative effectiveness research the importance of getting it right. Med Care. 2010;48(6 SUPPL.): 10.1097/MLR.0b013e3181da3709 [DOI] [PubMed] [Google Scholar]
- 15.Jorm AF. Using the Delphi expert consensus method in mental health research. Aust N Z J Psychiatry. 2015;49(10):887‐897. [DOI] [PubMed] [Google Scholar]
- 16.Mattingly TJ, Slejko JF, Perfetto EM, Kottilil S, Mullins CD. What matters most for treatment decisions in hepatitis C: effectiveness, costs, and altruism. Patient. 2019;12(6):631‐638. [DOI] [PubMed] [Google Scholar]
- 17.Asthma and Allergy Foundation of America . My Life With Food Allergy Report. VA: Arlington; 2019. [Google Scholar]
- 18.Bureau of Labor Statistics. Food and Beverage Serving and Related Workers . Occupational Outlook Handbook. https://www.bls.gov/ooh/food‐preparation‐and‐serving/food‐and‐beverage‐serving‐and‐related‐workers.htm. Published 2019. Accessed May 20, 2020.
- 19.Lau GY, Patel N, Umasunthar T, et al. Anxiety and stress in mothers of food‐allergic children. Pediatr Allergy Immunol. 2014;25(3):236‐242. [DOI] [PubMed] [Google Scholar]
- 20.Protudjer JLP, Jansson SA, Heibert Arnlind M, et al. Household costs associated with objectively diagnosed allergy to staple foods in children and adolescents. J Allergy Clin Immunol Pract. 2015;3(1):68‐75. [DOI] [PubMed] [Google Scholar]
- 21.Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167(11):1026‐1031. [DOI] [PubMed] [Google Scholar]
- 22.Rhim GS, McMorris MS. School readiness for children with food allergies. Ann Allergy, Asthma Immunol. 2001;86(2):172‐176. [DOI] [PubMed] [Google Scholar]
- 23.Renz H, Allen KJ, Sicherer SH, et al. Food allergy. Nat Rev Dis Prim. 2018;4: 10.1038/nrdp.2017.98 [DOI] [PubMed] [Google Scholar]
- 24.Bilaver LA, Chadha AS, Doshi P, O’Dwyer L, Gupta RS. Economic burden of food allergy: a systematic review. Ann Allergy, Asthma Immunol. 2019;122(4):373‐380.e1. [DOI] [PubMed] [Google Scholar]
- 25.Cummings AJ, Knibb RC, King RM, Lucas JS. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: a review. Allergy Eur J Allergy Clin Immunol. 2010;65(8):933‐945. [DOI] [PubMed] [Google Scholar]
- 26.Lavelle TA, D’Cruz BN, Mohit B, et al. family spillover effects in pediatric cost‐utility analyses. Appl Health Econ Health Policy. 2019;17(2):163‐174. [DOI] [PubMed] [Google Scholar]


