Abstract
Background
The use of eHealth, which has accelerated in the wake of the COVID‐19 pandemic, could contribute to the access to tailor‐made psychological interventions for people with intellectual disabilities.
Method
A scoping review was conducted on peer‐reviewed studies between 1996–2019.
Results
Thirty‐three studies reported on the use of psychological eHealth interventions focused on mental health problems and/or challenging behaviour. The vast majority of these studies reported on interventions that were delivered at the individual level. The context in which these interventions were delivered varied, primarily ranging from the home setting to residential settings, as well as day or activity centres and schools. The studies described various types of interventions: telehealth interventions, computerized cognitive behavioural therapy, and interventions focused on (social) learning principles targeting challenging behaviour.
Conclusions
eHealth provides new opportunities for both therapists and lay‐therapists to deliver psychological interventions. Future studies should focus on the effectiveness of psychological eHealth interventions.
Keywords: eHealth, intellectual disabilities, psychological interventions, therapy
1. INTRODUCTION
In recent years, health services and information that is either wholly delivered or enhanced by the Internet or related technologies (i.e. eHealth; Eysenbach, 2001) are increasingly being used in the field of intellectual disabilities (e.g. Oudshoorn et al., 2020). The use of eHealth has accelerated even more rapidly in the wake of the current coronavirus (COVID‐19) pandemic (Courtenay & Perera, 2020). In an attempt to prevent the proliferation of COVID‐19, manifold preventive measures have been adopted by countries across the globe, such as enjoining their citizens to stay at home and engage in social distancing, closing public places (e.g. restaurants, schools and sport facilities) and significantly reducing the use of public transport. In addition to these measures, work and day services for people with intellectual disabilities have been closed. Moreover, mainstream healthcare facilities, community care and specialized mental health organizations providing services to people with intellectual disabilities have introduced strict measures for on‐site support, face‐to‐face therapy and face‐to‐face mental health provision (VGN, 2020; World Health Organization, 2020). This means that, in most cases, mental health support for people with intellectual disabilities was not in operation during the initial stage of the COVID‐19 pandemic. People with intellectual disabilities are more vulnerable to develop mental health problems and expose challenging behaviour compared to the general population (Cooper, Smiley, Finlayson, et al., 2007). Prevalence studies show a large number of people with intellectual disabilities suffering from mental health problems (30–50%; Einfeld et al., 2011) and/or exposing challenging behaviour (5.5%–18.1%; Bowring et al., 2017; Lowe et al., 2007). They experience more challenging life events, trauma, stigmatizing and discrimination, lack of meaningful relationships and have to deal with less abilities to cope with stressful situations effectively (Taylor et al., 2013). Given their vulnerability for mental health problems and reduced capacity to cope with stress, which may have increased during the pandemic and resulting lockdowns (Courtenay, 2020; Embregts et al., 2020), ensuring the continuation of mental health support for people with intellectual disabilities is of paramount importance (Cooper, Smiley, Finlayson, et al., 2007; Taylor et al., 2013). In this respect, eHealth may represent an valuable alternative. eMental Health interventions in the general population demonstrated positive effects for depression, anxiety, substance use of alcohol and unspecified mental health disorders compared to a waiting list condition (Bennett et al., 2020). Research among the general population has reported on the feasibility of delivering effective psychological interventions via video conferencing with individuals, dyads and groups, and found similar outcomes to interventions delivered on‐site (Banburry et al., 2018). In light of the various governmental measures introduced to stop the proliferation of the COVID‐19 virus, telehealth, such as video conferencing, represents therefore an interesting adjunct to in‐person services (Torous et al., 2020). Hence, it might be possible that people with intellectual disabilities may also profit from remote and digital interventions to support mental health.
Mental health support or psychological interventions can be defined as ‘attempts to make changes in people, their behaviour, the systems around them or their interpersonal relationships, using methods derived from a psychological knowledge and understanding of individuals and their world’ (British Psychological Society, 2004, p. 69). Numerous studies have examined the opportunities and benefits of psychological interventions for people with intellectual disabilities (e.g. Brown et al., 2011; Kok et al., 2016; Koslowski et al., 2016; Osugo & Cooper, 2016; Ramsden et al., 2016), for example based on their meta‐analysis of psychological interventions for adults with various levels of intellectual disabilities. Depression and anger in adults with mild to moderate intellectual disabilities could effectively be treated through cognitive behavioural therapy (CBT) or variants of CBT that have been adapted for working with people with intellectual disabilities (Vereenooghe & Langdon, 2013) and challenging behaviour through behavioural and psychological interventions for people with mild intellectual disabilities (Didden et al., 2006). Moreover, in their systematic review of interventions targeted towards people with severe intellectual disabilities who also had mental health problems, Vereenooghe et al. (2018) also included several studies about psychological interventions. Specifically, they proposed that, while the urgency for mental health intervention programmes with this target group appears to be underestimated (cf. Poppes et al., 2014), psychological interventions may also be beneficial for people with more severe intellectual disabilities.
Historically, psychological interventions have predominantly been provided on‐site, and, in this respect, eHealth significantly expands the opportunities (Wanglin et al., 2016) by, for example, allowing the provision of psychological interventions to continue remotely during the current COVID‐19 pandemic. As well as being expedient during a pandemic, in ordinary circumstances eHealth can potentially lower the threshold for participating in a psychological intervention (e.g. by eliminating the travel time and costs of public transport), while, simultaneously, reducing the fear of stigmatization and shame due to the fact that service users can receive the psychological intervention at home as opposed to visiting mental health services (Proudfoot et al., 2011). In addition, eHealth can contribute towards the designing of bespoke interventions more closely attuned to the personal abilities, wishes, needs and personal contexts of the target group (van Gemert‐Pijnen et al., 2018). Although eHealth interventions among people with intellectual disabilities are routinely used in daily practice, psychological eHealth interventions specifically focused on mental health have hitherto not been extensively studied. The current COVID‐19 pandemic accelerates the urgency for a review of extent knowledge on this topic, which can contribute towards research as well as clinical practice (Wind et al., 2020). The present authors therefore conducted a scoping review specifically focused on psychological eHealth interventions among people with intellectual disabilities. The scoping review was underpinned by the following research question: What are the characteristics of the interventions, participants and persons delivering the intervention, and the content of the studies reporting about psychological eHealth interventions for people with intellectual disabilities?
2. METHOD
To answer the above research question, we conducted a scoping review (Arksey & O’Malley, 2005). For the current review, it was imperative to adopt an iterative approach as psychological eHealth interventions for people with intellectual disabilities is an area of inquiry that is as yet not well‐defined and relatively new. Hence, if a rigid, a priori design was used, then relevant literature might have been omitted. As a result, while we developed a search strategy and inclusion and exclusion criteria at the initial stages of the scoping review, we continually adapted them as the study proceeded.
2.1. Search strategy
A systematic search was conducted within seven bibliographic databases (CINAHL (EBSCO), Cochrane, Embase, Google Scholar, Medline (Ovid), PsycINFO (Ovid) and Web of Science) with the help of an experienced information specialist. These databases, which include both medical and psychologically oriented databases, were selected for their specialism on research in the fields of behavioural sciences, mental health, allied health and nursing. Using this combination of databases maximized, the number of relevant studies found on this topic. Studies had to have been published in peer‐reviewed journals in English from January 1996 until 6 September 2019. The 1996–2019 period was chosen on the grounds that the Internet was first introduced in 1995 within healthcare practice, thus increasing the likelihood of including relevant studies (Kelders & Howard, 2018).
The PICO approach was used, which comprises Population, Intervention/exposure, Comparison and Outcome (Liberati et al., 2009), in order to compose the search string and define the inclusion and exclusion criteria. The Population was specified as people with intellectual disabilities, irrespective of their level of intellectual functioning (i.e. people with all levels of intellectual disabilities were included in this review). According to the American Association of Intellectual and Developmental Disabilities (AAIDD, 2012), an intellectual disability originates prior to the age of 18 and is often characterized by significant limitations in both intellectual functioning and adaptive behaviour, which encompasses a wide variety of everyday social and practical skills. Regarding the Intervention, the studies needed to include a psychological intervention that corresponded to the definition of the British Psychological Society (2004), include an eHealth application (e.g. tablet, wearables, sensor technology or videoconferencing technology) and be carried out under the responsibility of a qualified professional (e.g. clinical psychologist, therapist or a trained research assistant). Next, the Comparison component was not specified as eHealth was regarded as being in its embryonic stages with respect to healthcare provision for people with intellectual disabilities, and, as such, all information about eHealth in the context of psychological interventions was considered to be of interest for the current study. The Outcome component was also not specified in the initial search strategy, in order to ensure that no relevant study in this novel and emerging research area was overlooked.
Table 1 provides an overview of the search terms and strategy that were employed in the Medline (Ovid) database, using MeSH terms (i.e. a controlled vocabulary thesaurus used for indexing papers) and additional text words for ‘intellectual disability’, ‘eHealth’ and ‘psychological intervention’. The other databases use similar thesauri systems (e.g. Embase uses Emtree terms). The ‘eHealth’ terms and synonyms were embedded in ‘psychological intervention’ terms used in the search strategy, as we were interested in sourcing all of the studies that applied eHealth in psychological interventions, and were combined with search words related to ‘intellectual disability’ (Bramer et al., 2017).
TABLE 1.
Search strategy for Medline (Ovid) database
| Medline (Ovid) final search strategy |
|---|
| (exp "Telemedicine"/ OR "Self‐Help Devices"/ OR "Therapy, Computer‐Assisted"/ OR Microcomputers/ OR "Electronic Mail"/ OR "Internet"/ OR "Social Media"/ OR exp "Cell Phones"/ OR Multimedia/ OR "Educational Technology"/ OR "Computer‐Assisted Instruction"/ OR (Telehealth* OR Telecare* OR telemedicine* OR teleconsultat* OR telepsychiatr* OR telemonitor* OR teletherap* OR telerehab* OR ((Tele OR telephone) ADJ3 (health* OR medicine* OR consultat* OR psychiatr* OR therap* OR rehab* OR monitor*)) OR e‐health OR ehealth OR mHealth OR (((assist* OR therap* OR aided OR treat* OR deliver* OR application* OR support* OR training OR education* OR learning OR surveillan* OR counsel* OR cbt OR intervent* OR rehabilitat* OR assessment* OR feedback OR support OR care OR help OR service OR assistance OR self‐help) ADJ3 (technolog* OR media OR computer* OR Web‐based OR Web‐site* OR web‐interface* OR webinterface* OR web‐page* OR web‐resource* OR webpage* OR website* OR email OR online OR Internet OR computer*‐program* OR software OR cyber* OR Remote OR virtual* OR device* OR "text messaging" OR sms OR whatsapp OR skype)) NOT assist*‐reproduct*‐technol*) OR (((e OR electronic*) ADJ (mail* OR health)) NOT electronic‐health‐record*) OR "social media" OR ((mobile OR cell*) ADJ phone*) OR smartphone* OR microcomputer OR ipad OR ipads OR (tablet* ADJ3 ("use" OR usage)) OR "information technology" OR multimedia OR domotic*).ab,ti.) AND ("Mentally Disabled Persons"/ OR exp "Intellectual Disability"/ OR "Learning Disorders"/ OR "Developmental Disabilities"/ OR "Neurodevelopmental Disorders"/ OR (((mental* OR intellect* OR learning OR developmental* OR neurodevelopmental*) ADJ3 (retard* OR impair* OR deficien* OR disab* OR handicap* OR difficult* OR limitation* OR delay*)) OR multipl*‐disab* OR cognitive‐disabilit* OR learning‐disorder* OR (cognitive‐impairment* NOT (dement* OR alzheimer* OR parkinson OR psychiatr* OR older OR aged OR elderly OR injur*)) OR development*‐disorder* OR retarded OR (down* ADJ3 (syndrome*))).ab,ti.) NOT (exp animals/ NOT humans/) NOT (letter OR news OR comment OR editorial OR congresses OR abstracts).pt. AND english.la. |
The initial search was deliberately broad so as to cover as many relevant studies as possible related to eHealth, including not only those studies on psychological interventions, but also those studies that used eHealth in support. The use of eHealth in supporting people with mild intellectual disabilities in daily life is reported in a systematic review (Oudshoorn et al., 2020). This scoping review instead focused on eHealth within the context of psychological interventions. Moreover, given the iterative nature of this scoping review, subsequent to the initial search strategy and prior to the second screening step (see Study selection for more information), mental health problems and challenging behaviours were ultimately chosen as the outcome measures due to the large number of studies. These outcome measures were also chosen because people with intellectual disabilities are more likely to both present symptoms of mental health disorders and exhibit challenging behaviour, which has a negative impact on the quality of life for people with intellectual disabilities, and, in turn, serves as a burden for themselves, relatives and support staff (Campbell et al., 2014; Cooper, Smiley, Finlayson, et al., 2007; Cooper et al., 2007). In addition, mental health problems and challenging behaviour are often the primary reason for being referred to specialized help and psychological interventions (Carr et al., 2016).
2.2. Study selection
In accordance with the PRISMA guidelines (Liberati et al., 2009), the selection process contained four stages: (1) identification, (2) screening title and abstract, (3) eligibility and (4) inclusion (see Figure 1). First, in the identification phase, peer‐reviewed studies were identified in the aforementioned databases, which resulted in 10,405 studies. Second, the screening of the records based on title and abstract was performed in two steps due to the broad focus on eHealth within the core domains of health care: assessment, support and psychological interventions. In the first step of the screening phase, 5,693 studies remained after removing 3,991 duplicates and 721 studies that were conducted prior to the publication date limit (1996). Title and abstract selection was carried out by two independent reviewers (CO and NF) based on the inclusion and exclusion criteria (Table 2). Reviews, dissertations, essays and book chapters were excluded. In the second screening step, studies containing results of eHealth within a psychological intervention targeted at people with intellectual disabilities and focused on mental health problems and challenging behaviours were selected. The two reviewers were in agreement over 90% of their respective decisions; disagreements were discussed with the last author (PE). After discussion, the in‐ or exclusion of a study was made by a shared decision of all reviewers.
FIGURE 1.
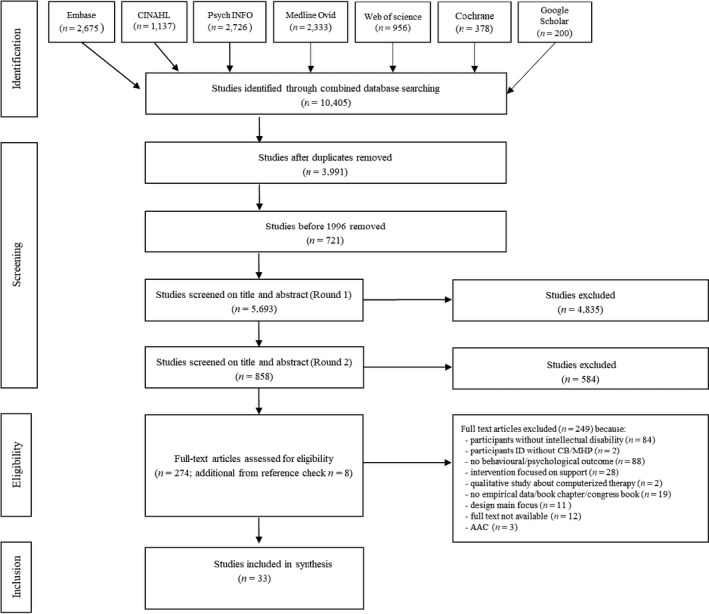
Flowchart of study selection for scoping review
TABLE 2.
Inclusion and exclusion criteria
| Inclusion criteria |
| Participants of the study were people with an intellectual disability (IQ <70, deficits in adaptive functioning resulting in support needs to meet developmental and sociocultural standards for personal independence and social responsibility, and the onset of deficits occur during the developmental period). |
| Participants of the study were reported to have challenging behaviour or a mental health disorder. |
| Studies about a psychological intervention or therapy intended to improve emotional, or psychological well‐being, or behavioural change provided or supervised by a professional (e.g. psychologist, therapist, certificated interventionist). |
| Studies focusing on using technology for the (remote) provision of therapy, or psychological, or behavioural intervention. |
| Studies focusing on individual, psychological or behavioural outcomes (e.g. emotional and psychological well‐being, challenging behaviour, mental health problems or specific behaviour due to psychiatric disorder such as, for example, anxiety, depression). |
| Exclusion criteria |
| Participants: |
| Studies focusing on people with cognitive disabilities/impairments due to traumatic brain injury, stroke, cancer treatment or (early) dementiaa. |
| Intervention: |
| Studies focusing on design of eHealth without application in a psychological or behavioural treatment or a therapy context. |
| Studies focusing only on physical health outcomes (e.g. weight management, drinking, smoking, physical fitness). |
| Studies focusing on parents of children with intellectual disabilities and outcomes on parental behaviour only. |
| General: |
| Studies without empirical data (e.g. policy documents, conference papers, proposal clinical trial) or opinion papers, qualitative studies and grey literature). |
| Studies presenting only psychometric data (i.e. validity and reliability of a specific instrument). |
Several studies reporting about eHealth and mild cognitive impairment to detect early dementia. Because a few studies used the term ‘mild cognitive impairment’ also for people with mild intellectual disabilities, we decided to include ‘(early) dementia’ as an exclusion criteria.
Third, in the eligibility phase, the 274 full texts were read by the first author (PE), with a particular focus on the presence of the inclusion and exclusion criteria (see Table 2). This step led to the exclusion of 249 studies, and the retainment of 25 eligible studies. In the case of doubt, a second researcher (PE) was consulted. In addition, the reference lists of these 25 studies were screened for eligible studies, resulting in the identification of eight additional studies. As the objective of a scoping review is to provide an overview of relevant studies about a specific topic, rather than assessing the quality of the studies included, no quality appraisal was conducted (Arksey & O’Malley, 2005).
2.3. Charting data and analysis
Information on the following items was extracted from the included studies in the present review: the country of origin, the period of publication, the general characteristics of the participants and the design of the included studies. In addition, we extracted data pertaining to the characteristics of the psychological interventions, the participants, the people delivering the intervention and the content of the studies reporting on psychological eHealth interventions for people with intellectual disabilities. The characteristics of the 33 studies included in the scoping review are presented in Table 3.
TABLE 3.
Characteristics of the studies included
| Author#year#country | Study design | Participants | Diagnosis (DSM or ICD) | Treatment context | Model of change/therapeutic | Therapy conditions | eHealth application | Outcome measures | Target behaviour |
|---|---|---|---|---|---|---|---|---|---|
| Individual interventions | |||||||||
| 1. Lancioni et al. (1997), IT | ABABAB (I), ABABABAB (II) | N = 2, 1F 1M, Age 24 and 60 | I. activity centre; II. community home | Not explicated, but BT principles | Sessions 30 min (I), 40 min (II). I. 2–4 times a day, 2 hrs a day device available, 3–4 days a week. II. 2–4 times a week, device available 1–3 hrs a day, sessions 3–5 day/p/week | Battery‐powered electronic unit worn at the chest and connected to an earpiece. The electronic unit consisted of a miniature electret microphone and a two‐stage low frequency amplifier, with dials for setting the loudness limit. | Observation (momentary time interval sampling) | Vocal loudness | |
| 2. Lancioni et al. (1998), IT | ABABABAB | N = 1, M Age 20 | Autistic‐like behaviour | Activity centre | Prompts, reminders, rewards, positive comments are mentioned, but no theoretical framework. | 30 min per session, 5.5 months of duration study | Portable wearable device at the wrist providing visual and auditory feedback | Observation (6 moments during therapy programme) | Vocal loudness |
| 3. Lancioni et al. (1999), IT | ABABAB | N = 1, 1 F Age 56 | Activity centre | Not explicated, but BT principles | 5 months of 30‐min sessions, no further details | Battery‐powered electronic unit worn at the chest and connected to an earpiece. The electronic unit consisted of a miniature electret microphone and a two‐stage low frequency amplifier, with dials for setting the loudness limit. | Recording of talking and vocal loudness (momentary time interval sampling) | Vocal loudness | |
| 4. Lancioni, O’Reilly, et al. (2006), IT | Multiple probe across responses design. Postintervention checks 1,2 and 3 months after intervention | N = 1, 1M Age 12.5 yrs | Congenital cerebropathy with spasticity, minimal residual vision, epilepsy | n.r. | Not explicated, but BT principles | n.r. | Microswitch clusters | Microswitch recorded data movement, sensor monitoring finger mouthing. | Foot and head movements and finger mouthing |
| 5. Lancioni, Singh, et al. (2006), IT | ABAB1B2 | N = 7, 1 F 6M Age 7.9–20.7 (M = 14.3) | Sensory impairments, 5 diagnosed with epilepsy | Home or educational context | Not explicated, but BT principles | 5–10 min (advice parents/professionals) with a microswitch‐based and a stimulation programme (separated and alternating condition) in a variable amount of sessions | Microswitches (pressure device) were linked to an electronic control system. This was a portable, battery‐powered case connected to a variety of preferred stimuli selected for the study | Microswitch activation responses were recorded directly during the sessions. Observation (partial interval system) of indices of happiness from videotapes | Microswitch activation responses and indices of happiness |
| 6. Lancioni, Smaldone, et al. (2006), IT | ABB1AB1 | N = 1, 1 F Age 41 | DS, passive and sedentary | Quited activity room | Not explicated, but BT principles | 5 min, 3–9 times a day | Microswitch clusters (pressure and mercury devices) | Microswitch activation responses were recorded | Handpushing and face hiding |
| 7. Lancioni et al. (2007), IT | ABB1AB1 design | N = 1, M Age 12.8 | Congenital cerebropathy with spastic tetraparesis, minimal residual vision, seizure disorder | Quiet room in a educational context | Not explicated, but BT principles | 5 min sessions 3–9 times a day on participant's availability. Intervention sessions 122, 44 and 50 sessions, respectively. Postintervention check 15 sessions. | Microswitch cluster (optical), light wires attached to a headband | Microswitch activation responses were recorded and target behaviour was measured by activation of sensor | Hand mouthing, eye poking and foot movements |
| 8. Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al. (2008), IT | ABAB with 3 month postintervention | N = 1, 1M Age 29 | Congenital encephalopathy, seizure disorder | n.r. | Not explicated, but BT principles | 5 min, 3–7 times a day; 47–104 sessions | Microswitch cluster | Microswitch activation responses were recorded and target behaviour was measured by activation of sensor | Object‐contact responses without hand stereotypy |
| 9. Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al. (2008), IT | ABAB with 3 month postintervention | N = 1, 1 F Age 12.2 | Seizure disorder (Lennox–Gastaut), visual impairment, MD | n.r. | A section about case conceptualization | 10 min a day, 3–8 times a day. Treatment phases included 86 and 105 sessions | Microswitch cluster | Microswitch +optic and minitilt sensors recorded data +observation indices of happiness (partial interval) on videotapes | Object manipulation and hand mouthing |
| 10. Lancioni et al. (2011), IT | Non‐concurrent multiple baseline design across participants | N = 2, congenital encephalopathy 1 F, 1M Age 34 and 31 | Motor, sensory disabilities | Care and rehabilitation centre | 304 and 129 sessions | Microswitch (pressure) + computer system for stimuli | Computer system automatically recorded responses +observation of indices of happiness on videotapes | Microswitch activation responses and indices of happiness | |
| 11. Gaskin et al. (2012); USA | Multiple probe design across skills | N = 1; IQ 66 verbal and 72 performance (WAIS); 1 F 23 yrs | at home | PII module (parent–infant interaction); part of SafeCare® intervention. Social learning is assumed, but not reported explicitly. | Visits home visitor (certified trainer) weekly at home. Five training sessions with a structured approach towards how physical and non physical skills were trained. A booster session was delivered (2 month FU) focused on underutilized skills. | Digital picture frame | Observation of PII skills by the Planned Activities Training checklist, infant version (PAT‐VI) recording demonstration of PII skills +consumer satisfaction by a 10‐question survey | Physical and nonphysical PII target skills | |
| 12. Lancioni, O’Reilly, et al. (2013), IT | ABB1AB1 design | N = 2, 1 F, 1M. Age 19 and 20 | Visual impairment, non‐ambulatory, one had epilepsy, | Quiet room in the attended centre the persons attended | Not explicated, but BT principles | I. 5 min, 2–6 times a day II. 30 min, once a day. | Microswitch (optic) detected I. hand mouthing and an optical‐touch screen computer monitor activated by the touch response II. Napkin with sensors/microswitches, microprocessor and MP3 device | Observation of frequencies of touch responses, total amount of session time with the presence of hand mouthing were automatically recorded via the computer system | Touch responses, wiping/cleaning and hand mouthing |
| 13. Lancioni, Singh, et al. (2013), IT | I. ABB1AB1 design, II. ABB1AB1B2 design | N = 3, 1 F 2M, Age 10*, 27 and 64 * included | Congenital encephalopathy with spastic tetraparesis | n.r. | Not explicated, but BT principles | I. 10 min, 3 to 6/7 times a day. (Intervention sessions 46, 28 sessions and 84 sessions). II. 15 min, 2–4 times a day | I. a) tilt and optic microswitches connected with the objects react by touching b)microswitch (optic) attached to the wheelchair +headrest was activated with head c) computer control system for preferred stimuli activation. | Observation target responses automatically recorded by computer system, and observation by RA | I. adaptive behaviour (touching objects) and inappropriate posture. II. adaptive behaviour (mouth‐cleaning +object assembling) and drooling |
| 14. Stasolla and O’Caffò (2013), IT | Multiple probe design across behaviours for each participant | N = 2, 2 F Age 12 and 17 | Rett's syndrome, withdrawal, stereotyped behaviours, motor problems and epilepsy | At home | Not explicated, but BT principles | 5 min 3–4 times a day, 4 days a wk. The intervention programme lasted approximately 6 months. (Intervention I = 50 sessions, Intervention II = 50 sessions) | A wobble microswitch in the first phase, adopted microswitch = two optic sensors (photocells fixed to the lateral panels of the walker device) | Frequencies of responses of object manipulation (automatically count by device) + observation (partial interval and event) of indices of happiness and stereotype behaviour | Hand washing, body rocking (stereotypies), access to preferred stimuli and step responses |
| 15. Stasolla et al. (2013), IT | ABAB sequence with a postintervention check after 15 days | N = 3, 3M Age 6–9 | Cerebral palsy and MD | At home | Based on learning principles | 10 min sessions, 2–4 times a day, 3 days a week. The intervention programme lasted approximately 6 months. (Intervention I 40 sessions, Intervention II 60 sessions). | Laptop computer equipped with a Clicker 5 software package, microswitch (pressure) + a connecting interface +mouse (Intervention II) | Observation of happiness signs (partial interval) and number of requested item | Independent choice behaviour and mood |
| 16. Kim et al. (2014); KR | Multiple probe design across participants | N = 3; IQ < 55 (KISE‐KIT) severe ID, adaptive scores 49–76 (KISE‐SAB), 1 F, 2M Age 17 | Separated room in school | ABA Antecedent‐based intervention; providing alternative behavioural strategies by using Social Stories | Before school starts the teacher provided the intervention (7–17 sessions; varied to participant involved) | Galaxy Tap smart tablet with Social Story created on Prezi and accessed via QR | Observation of disruptive behaviour and academic engagement | Disruptive behaviour and academic engagement | |
| 17. Lancioni, Singh, O’Reilly, Green, et al. (2014), IT | ABAB design | N = 2; MID/MoID, 2M Age 43 (I) and 34 (II)only data II included, I focused on support | II. total blindness, severe hearing disability | Living room of the centre | Not explicated, but BT principles | Sessions 20–30 min, 34 and 47 intervention sessions (3 introduction sessions before start of intervention) | Battery‐powered sound‐detecting unit fixed at the chest and connected with a throat microphone, an airborne microphone, a vibration box fixed at the shoulder. Sound‐detecting unit was triggered when signals conveyed at about 85 dB. | Observation of speaking and vocal loudness by momentary time sampling procedure | Vocal loudness |
| 18. Lancioni, Singh, O’Reilly, Sigafoos, et al. (2014), IT | ABAB design (MPD across settings was used for participant 1). | N = 2; MoID and SID, 2M, Age 33 and 42 | Blind; and one participant suffered from epilepsy; both congenital encephalopathy | Activity area and large dining room for participant 1 (MoID/SID); activity room, corridor and 2 small rooms for participant 2 (SID/PMID). | Not explicated, but BT principles | One or two sessions per day, 3–5 days a week and 10 practical sessions to introduce the technology. | Orientation technology included a sound source at each of the destinations, a mini radio‐coded device worn by participants on the shirt or belt, and a portable control device to activate such source. Short sentences from the apparatus encourage orientation in the right direction | Observation of anxiety‐related behaviour (partial interval) | Anxiety‐related behaviour |
| 19. Stasolla, Damiani, et al. (2014), IT | Non‐concurrent multiple baseline design across participants | N = 2, 2M Age 8–9 | FXS, motor and speech disabilities | at home | Matching behavioural responses to environmental consequences, DRO +self‐determination | 10 min sessions, 2–4 sessions a day, 4 days per wk. Study lasted approximately 5 months. | Optic sensors connected with battery‐powered control system unit. | Observation of stereotypic behaviour +indices of happiness +control system unit counts of performance of target behaviour | Occupation and choice opportunities, stereotyped behaviour and happiness |
| 20. Stasolla, Perilli, et al. (2014), IT | ABB1AB1 | N = 3, 3M Age 8.4–10.2 (M = 9.36) | ASD, motor and speech disabilities | Quiet room at home | Not explicated, but BT principles | 5 min, 3–5 times a day, 4 days per week. 125 sessions. Duration study: 3 months. | Microswitch clusters programme | Recording adaptive response device, hand mouthing was detected by activation of optic sensor fixed with an adapted frame on the chin. Observation of indices of happiness (video) | Object manipulation, hand mouthing and happiness |
| 21. Jonker et al. (2015); NL | Pre‐experimental, quantitative approach | N = 1; MoID IQ = 47; 1M Age 27 | Visual impairment | Residential group home in care for ID and VI | Safe haven and secure base attachment intervention | First phase automatic responses received from a computer on the emotion message send by participant, second phase caregiver response on distance and conversation between person with ID and caregiver about the exchanged messages according a protocol based on the Circle of Security when reunited in person. | iPhone with app | ABCL, BSI, frequency and intensity of behaviour at work and at home. Frequency of messages. Social Validity questionnaire caregivers and client. | Separation anxiety and challenging behaviour |
| 22. Stasolla et al. (2015), IT | Multiple probe design across responses for each participant | N = 3, 3 F Age 9–12 | Rett's syndrome, withdrawal, isolation, passivity, motor disabilities, stereotyped behaviours | At home | Not explicated, but BT principles | 10 min. 2–4 times per day, 4 days per week. Duration study: approximately 6 months. 225 sessions for each participants. | Containers with photocells +laptop equipped with a Clicker 5 software package and a connecting interface | Observation of mood signs +percentage of interval stereotyped behaviour +computer counting inserted objects | Choice strategies, stereotyped behaviour and happiness |
| 23. Singh et al. (2017); USA | Multiple baseline design across participants with a 12 month follow‐up | N = 3 teachers and N = 3 students; mild intellectual disability no IQ scores reported 3M, Age 10–11 | School | Mindfulness | Week 1 daily 30 min recognize precursor of anger +aggression and use SoF procedure to effectively control his anger, week 2 daily 15 min sessions reviewing SoF procedure. Week 3 reminding the student to use the SoF procedure. Teacher recorded the SoF instruction on an iPad for self‐instruction at school and at home. | iPad for recording mindfulness exercises for students. iPad and Google Hangout for treatment fidelity training SoF and check. iPhone and app for recording target behaviour of participants. | Observation of frequency of physical and verbal aggression tapped on iPhone by 2 teacher aides independently | Physical and verbal aggression | |
| 24. Cooney et al. (2017); UK | A 2 * 3 RCT | N = 24 (cCBTG); 12 MID, 12 MoID, 16 F 8M Age 42 (12.85); N = 25 (TAU); 8 MID, 17 MoID, 14 F 11M Age 39.24 (9.14). | Anxiety, depression, comorbid anxiety and depression, or recurring anxiety or depression (DSM IV) | MHID team, a specialist secondary care service for non‐crisis mental health services for adults with ID and mental health needs | CBT | 7 consecutive weekly sessions, therapist guided during sessions | PeskyGnats: TheFeelGoodIsland prototype CBT computer game | Primary: GAS‐ID, GDS‐LD. Secondary: CORE‐LD. | Mood (anxiety/depression) |
| 25. Hoffman et al.(2017); NL | Pre‐experimental within‐group design with multiple baselines and staggered intervention start‐points | N = 6; MID and MoID (IQ scores n.r)with visual impairment, 1 F, 5M; Age 27–56 | Separation anxiety | Group homes at an organization | Safe haven and secure base attachment intervention | Messages sent by automatic response of a computer. Messages by caregiver. Discussion about the exchanged message | iPhone with app | ABCL anxiety subscale, BSI, PIMRA, IDQOL, frequency of each type of message. Frequency and intensity of behaviour at home and at work. | Separation anxiety and challenging behaviour |
| 26. Stasolla, Perilli, Damiani, et al. (2017), IT | ABCAC experimental sequence, 3 month FU | N = 6, 6M, Age 6.4–10.5 (M = 8.2) | ASD (severe conditions due to CARS score), isolated, passive and withdrawn, motor an communicative disabilities | At home | Results can be comparable to a procedure of differential reinforcement of incompatible behaviours. | 5 min, 5 sessions a day, 5 days a week. Duration of study: 5 months 205 sessions per participant. | 2 microswitches (optic sensors) connected to battery‐powered control unit system. | Recording of adaptive behaviour by sensors fixed within the containers +recording challenging behaviour by sensor embedded in a specific frame fixed on the chin. Observation of indices of happiness (partial interval with 20 observation per session) | Adaptive behaviour and hand/object mouthing |
| 27. Stasolla, Perilli, Caffò, et al. (2017), IT | Single‐subject reversal experimental design (included two BL and two intervention phases). Follow‐up phase after 3 months. | N = 3, 3M Age 8–10 | FXS, quite passive and isolated, exhibiting withdrawal and stereotyped behaviours (hand mouthing and flapping), motor and communicative disabilities | At home | Not explicated, but BT principles | Sessions of 5 min, 4–6 sessions a day, 4 days a week. Study lasted approximately 5 months. 150 sessions per participant. Before start 6 familiarization sessions. | Optic sensors connected with an interface, to a laptop. The laptop automatically record a behavioural response, automatically ignored a new behavioural response within the stimulation period and providing participants with positive stimulation during the intervention and follow‐up | Adaptive response was recorded by the computer +Observation of stereotyped behaviour, hand mouthing and indices of happiness | Adaptive response, hand mouthing and happiness |
| 28. Perilli et al. (2019), IT | ABB1AB1 design | N = 6; 6M, Age 13–19 | FXS | Individually at participants’ homes | Not explicated, but BT principles | BL 5 sessions within 2 days; B 30 sessions within 3 wks; B1 30 session within 3 wks. BL2 5 sessions within 2 days. FU (after 1 yr) 30 sessions within 3 wks. Sessions lasted 10 min | Micro switch cluster technology | Computer system automatically recorded responses +Observation of positive participation (video) | Adaptive response, hand biting and positive participation |
| Countries: ABCL, Adult behaviour checklist; BSI, Brief Symptom Inventory; BT, behavioural therapeutic; CARS, Childhood Autism Rating Scale; CB, challenging behaviour; cCBTG, computerized Cognitive Behavior Therapy Group; cg, care giver; CORE‐LD, Clinical Outcomes in Routine Evaluation ‐ Learning Disability; DMT, dance and movement therapy; DSM IV, Diagnostic and Statistical Manual of Mental Disorders; F, female; FXS, fragile X syndrome; GAS‐ID, Glasgow Anxiety Scale for people with Intellectual Disability; GDS‐LD, Glasgow Depression Scale for people with Learning Disability; ID, intellectual Disability; IDQOL, Intellectual Disability Quality of Life; IQ, intelligence quotient; IT, Italy; KISE‐KIT, Korea Institute for Special Education‐Korea Intelligence Test for Children; KISE‐SAB, Korea Institute for Special Education‐Scales of Adaptive Behavior; KR, Korea; M, male; M, mean; MARA, Movement Assessment and Reporting App; MD, multiple disabilities; MHID, Mental Health of Intellectual Disability team; MoID, moderate intellectual disability; n.r., not reported; NC, not clear; NL, the Netherlands; PII, parent–infant interactions; PIMRA, Psychopathology Instrument for Mentally Retarded Adults; PMID, profound multiple intellectual disability; QR, quick response; RA, research assistant; RA2, second research assistant; RCT, randomized controlled trial; SD, standard deviation; SID, severe intellectual disability; SoF, Soles of Feet mindfulness training; TAU, treatment as usual; TBI, traumatic brain injured; UK, United Kingdom; USA, United States of America; WAIS, Wechsler Adult Intelligence Scale. | |||||||||
| Group interventions (with individual elements) | |||||||||
| 29. Hetzroni and Banin (2017); IL | Single‐subject multiple baseline design across situations | N = 5; mild ID (IQ scores n.r.), 5M Age 11–15 | Axenfeld‐Rieger syndrome, psycho‐motor behaviour disorder and epilepsy | School | Social information processing theory and social modelling and simulation | Small group activities (50 min): observation of video clips (adequate and non‐adequate behaviours), followed by discussions related to the demonstrated behaviours. Participation in simulations of the social skill learned. At the end of each session students played the educational computer games. Group sessions included one participant and 5–6 other school peers | Computer, video modelling clips | Observation of socially adequate behaviour (before, during and after intervention in three situations). A observation form was developed with information about the participant, activity and what behaviour was exposed in what situation | Action, verbal and non‐verbal behaviour in three social situations |
| 30. Dunphy and Hens (2018); AUS | Mixed method: Observational data and interviews and focus groups with participants, centre staff, managers and parents | N = 12; MoID and MID, IQ scores, gender and age n.r. | Day centre for people with ID | Dance and movement therapy | 16 weekly sessions | MARA app with iPad | Observation scores on behaviour linked to 2 objectives DMT in six sessions (beginning, mid and final sessions) + interviews participants on experiences DMT and reviewing video clips and therapist scores of DMT sessions | Exposing behaviour on objectives (physical domain and interpersonal domain) | |
| 31. Hronis et al. (2019); AUS | Feasibility study by case series design | N = 21: 2 groups juniors N = 10 MoID/MID, 10 F Age 13–15; seniors N = 11 MoID/MID 11 F Age 14–18 | SAS‐TR school anxiety, SUDS and ID | All‐girls school supporting children with special needs | CBT | 10 face‐to‐face group sessions twice weekly and an online programme | FearlessMe! Online programme with exercises related to CBT | Scores on SUDS of participants, SAS‐TR reported by teachers. Parents outcome measures were not reported due to low response rate | Anxiety |
| Countries: AUS, Australia; CBT, Cognitive Behavior Therapy; IL, Israel; MID, mild intellectual disability; MoID, moderate intellectual disability; SAS‐TR, Social Anxiety Scale‐Teacher Report; SUDS, subjective units of distress score. | |||||||||
| Dyad interventions | |||||||||
| 32. Simacek et al. (2017); USA | Single‐case experimental designs; MPD and ABAB design embedded | N = 3; IQ n.r., low adaptive range VABS; 2 ASD and 1 Rett's syndrome. 3 F Age 3.5–4 yrs | ASD, Rett's disorder (severe neurodevelopmental disability) | At home | ABA | Functional communication training delivered by parents up to 7 daily sessions with a 5 min/3 trial block with a prior functional assessment and psycho‐education of parents supported a certified coach via telehealth | Screen‐recording software on computer, headset, secure internet and storage of data. Videoconferencing software (Google Hangout) and webcam. | Observation of idiographic responses and requests using PECS cards/microswitch for requests and problem behaviour. Treatment Acceptability Rating Scale‐Revised parents | Adaptive request to parents and yelling, tantrum, and hitting object |
| 33. Monlux et al.(2019); USA | Not reported | N = 10 parent–child dyads with eight dyads completed the treatment.; IQ n.r. mean adaptive behaviour composite standard score 62.1 (SD = 8.3, range = 50–73). Age 3–10 | FXS | at home | ABA | 12‐weeks 1‐h telehealth‐supported to implement a functional communication plus extinction training on a daily basis delivered by parent | Apple iPad Air® with a built‐in webcam, a Bluetooth® earpiece and a HIPAA compliant videoconferencing programme | Observation of the rate of problem behaviour and functional communication response during 1 h telehealth session. Treatment Acceptability Rating Scale‐Revised parents | Problem behaviour and child minds |
| Country: ABA, Applied Behavior Analysis; ASD, autism spectrum disorder; BIF, borderline intellectual functioning; F, female; FXS, fragile X syndrome; HIPAA, Health Insurance Portability and Accountability Act; M, male; MID, mild intellectual disability; MoID, moderate intellectual disability; PECS, Picture Exchange Communication System; USA, United States of America; VABS, Vineland Adaptive Behavior Scale. | |||||||||
In line with scoping review recommendations (Levac et al., 2010), two reviewers (CO and NF) independently piloted the utility of the developed coding scheme, by randomly selecting and reviewing five of the 33 studies (18.2%). The first author selected five studies manually by using the Excel number table and pointed studies randomly. Disagreements stemming from ambiguity in the description of the codes were discussed and refined by both reviewers. Next, one reviewer (PE) extracted the data from the remaining 28 studies and any ambiguities were discussed with the second reviewer (PE) until an overall consensus was reached. The final content of the coding scheme was discussed with all authors.
3. RESULTS
After a brief description of the country of origin, the period of publication, the general characteristics of the participants and the designs of the 33 included studies, the data from the studies will be mapped, charted and described in narrative form on: 1) the characteristics of the psychological eHealth interventions, 2) the characteristics of the participants with intellectual disabilities, 3) the characteristics of the people delivering the psychological eHealth intervention and 4) the content of the studies reporting on psychological eHealth interventions for people with intellectual disabilities. The vast majority of the studies were conducted by two research groups from Italy (n = 22), while the remainder of the studies were conducted in the United States (n = 4), Australia (n = 2), the Netherlands (n = 2), Israel (n = 1), Korea (n = 1) and the United Kingdom (n = 1). Most of the studies were published in the last decade (n = 24); the remaining studies were published between 1997 and 2010. In 29 studies, a single case design was used (Dunphy & Hens, 2018; Gaskin et al., 2012; Hetzroni & Banin, 2017; Hronis et al., 2019; Kim et al., 2014; ; Lancioni, O’Reilly, et al., ,2006, 2013; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, et al., 2006, 2013; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni, Smaldone, et al., 2006; Perilli et al., 2019; Simacek et al., 2017; Singh et al., 2017; Stasolla, Damiani, et al., 2014; Stasolla & O’Caffò, 2013; Stasolla et al., 2013, 2015, 2017a; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, et al., 2014). In addition, two studies used a pre‐experimental design (Hoffman et al., 2017; Jonker et al., 2015) and one study used a randomized control trial (Cooney et al., 2017), while one study did not report about the study design (Monlux et al., 2019). Further details of the included studies are reported in Table 3.
3.1. Characteristics of the psychological eHealth interventions
The vast majority of the studies (n = 29) reported on interventions that were delivered at the individual level (Cooney et al., 2017; Dunphy & Hens, 2018; Gaskin et al., 2012; Hoffman et al., 2017; Jonker et al., 2015; Kim et al., 2014; ; Lancioni, O’Reilly, et al., 2013, 2006; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, et al., 2006, 2013; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni, Smaldone, et al., 2006; Perilli et al., 2019; Singh et al., 2017; Stasolla, Damiani, et al., 2014; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017; Stasolla, Perilli, et al., 2014; Stasolla et al., 2015). In addition, two interventions were delivered to a dyad comprising a child with an intellectual disability and his/her parent (Monlux et al., 2019; Simacek et al., 2017), while two studies reported on a combination of a group intervention with individual elements, such as a group discussion combined with playing video games individually (Hetzroni & Banin, 2017; Hronis et al., 2019).
3.1.1. The types of interventions
The types of interventions used within the studies varied. The majority of the studies (n = 24) included applied behaviour analysis or behaviour therapeutic principles as the basis for the intervention (Lancioni et al., 1998, 1999, 2011, 2007, 1997; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni, O’Reilly, et al., 2013, 2006; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, et al., 2006, 2013; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni, Smaldone, et al., 2006; Monlux et al., 2019; Perilli et al., 2019; Simacek et al., 2017; Stasolla, Damiani, et al., 2014; Stasolla & O’Caffò, 2013; Stasolla et al., 2013, 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017; Stasolla, Perilli, et al., 2014), for example prompt fading, extinction and differential reinforcement. In addition, two studies used a practice‐based programme, which was originally developed for a specific centre or target group and subsequently adapted for the participants within the study (Gaskin et al., 2012; Kim et al., 2014). Moreover, two studies reported on using Cognitive Behavioural Therapy (CBT) in their interventions (Cooney et al., 2017; Hronis et al., 2019). CBT is a form of therapy helping people to reduce distress by becoming aware of and changing unhelpful thoughts, underlying thinking schemes and practicing other ways of thinking and applying new skills in daily life (Jahoda et al., 2017). Furthermore, the Circle of Security intervention for developing secure attachment with primary caregivers was used in two studies (Hoffman et al., 2017; Jonker et al., 2015). Finally, two studies reported on interventions that used a systemic approach (Dunphy & Hens, 2018; Hetzroni & Banin, 2017), while one study focused on mindfulness (Singh et al., 2017).
3.1.2. Context of intervention delivery
Eleven studies reported that the intervention was deployed at home (Gaskin et al., 2012; Monlux et al., 2019; Perilli et al., 2019; Simacek et al., 2017; Stasolla, Damiani, et al., 2014; Stasolla & O’Caffò, 2013; Stasolla et al., 2013, 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017; Stasolla, Perilli, et al., 2014). In five studies, the intervention was delivered in a residential setting (Hoffman et al., 2017; Jonker et al., 2015; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni et al., 1997). In addition, a day or activity centre served as the intervention context for five studies (Dunphy & Hens, 2018; Lancioni et al., ,1998, 1999, 1997; Lancioni, O’Reilly, et al., 2013), and a school context for four studies (Hetzroni & Banin, 2017; Kim et al., 2014; Lancioni et al., 2007; Singh et al., 2017). Furthermore, one study combined a school context with the use of online information and practicing of elements of CBT at home (Hronis et al., 2019), while one study delivered the intervention in an educational context for some of the participants and at home for others (Lancioni, Singh, et al., 2006). A clinical mental health setting served as the context for one study, with a specialist team delivering secondary care service (Cooney et al., 2017), while another study was carried out in the context of a care and rehabilitation centre (Lancioni et al., 2011). Finally, four studies did not report the context in which the intervention occurred (Lancioni, O’Reilly, et al., 2006; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni, Singh, et al., 2013).
3.2. Characteristics of the participants with intellectual disabilities
In total, the 33 studies contained 168 participants with intellectual disabilities (75 males, 68 females); two studies did not report about the gender of their 25 participants (Dunphy & Hens, 2018; Monlux et al., 2019). In 16 studies, the participants were children with intellectual disabilities aged between 3 and 18 years old (Hetzroni & Banin, 2017; Hronis et al., 2019; Kim et al., 2014; Lancioni, O’Reilly, et al., 2006; Lancioni et al., 2007; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Monlux et al., 2019; Simacek et al., 2017; Singh et al., 2017; Stasolla, Damiani, et al., 2014; Stasolla & O’Caffò, 2013; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017; Stasolla, Perilli, et al., 2014; Stasolla et al., 2015). Adults with intellectual disabilities participated in 14 studies (Cooney et al., 2017; Dunphy & Hens, 2018; Gaskin et al., 2012; Hoffman et al., 2017; Jonker et al., 2015; Lancioni Markus, & Behrendt, 1998, 1999; Lancioni, O’Reilly, et al., 2013; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni et al., 2011; Lancioni, Smaldone, et al., 2006; Lancioni Van Houten et al., 1997), while in three studies, both a child and an adult with intellectual disabilities were included as participants (Lancioni, Singh, et al., 2006, 2013; Perilli et al., 2019).
In 18 studies, people with severe and profound intellectual disabilities participated in psychological eHealth interventions (Kim et al., 2014; Lancioni, O’Reilly, et al., 2006; Lancioni, Singh, et al., 2006; Lancioni, Smaldone, et al., 2006; Lancioni et al., 2007; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni et al., 2011; Lancioni, O’Reilly, et al., 2013; Lancioni, Singh, et al., 2013; Stasolla & O’Caffò, 2013; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Perilli et al., 2019; Stasolla, Damiani, et al., 2014; Stasolla, Perilli, et al., 2014; Stasolla et al., 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017. In addition, people with moderate intellectual disabilities participated in five studies (Jonker et al., 2015; Lancioni et al., 1997; Lancioni et al., 1998; Lancioni et al., 1999; Stasolla et al., 2013) and a mixed group of people with mild to moderate intellectual disabilities participated in five studies (Cooney et al. 2017; Dunphy & Hens, 2018; Hoffman et al., 2017; Hronis et al., 2019; Lancioni, Singh, O’Reilly, Green, et al., 2014), while three studies only reported the results for participants with mild intellectual disabilities (Gaskin et al., 2012; Hetzroni & Banin, 2017; Singh et al., 2017). Two studies did not report the level of intellectual functioning, but reported the results on the Vineland Adaptive Behaviour Scale with scores in the low adaptive range (Monlux et al., 2019; Simacek et al., 2017). It is noteworthy that only one study reported detailed information about IQ scores based on standardized testing of the participants (Gaskin et al., 2012); all other studies merely reported a description of the level of intellectual functioning of the participants.
3.2.1. Type of challenging behaviour and mental health problems
In 23 studies, the rationale for the intervention was that the participants were exhibiting various types of challenging behaviour. First, self‐injurious and stereotypic behaviour, such as finger biting and hand mouthing, eye poking and body rocking, were reported in 15 studies (Lancioni, O’Reilly, et al., 2006; Lancioni, Smaldone, et al., 2006, Lancioni et al., 2007, Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni et al., 2011, Lancioni, O’Reilly, et al., 2013; Lancioni, Singh, et al., 2013; Perilli et al., 2019; Stasolla & O’Caffò, 2013, Stasolla, Damiani, et al., 2014; Stasolla, Perilli, et al., 2014, Stasolla et al., 2015, Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017). Next, vocal loudness was reported in four studies (Lancioni Markus, & Behrendt, 1998, 1999; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni Van Houten et al., 1997), aggressive behaviour in two studies (Monlux et al., 2019; Singh et al., 2017), disruptive behaviour in one study (Kim et al., 2014), and tantrums, crying and whining in one study (Simacek et al., 2017), while one study reported on the harmful parental behaviour of a mother who had a mild intellectual disability (Gaskin et al., 2012).
Of the remaining studies, ten studies focused on the mental health problems of the participants; in five of these, the main mental health problem was a type of anxiety: general anxiety (Hronis et al., 2019), anxiety with comorbid depression (Cooney et al., 2017), separation anxiety (Hoffman et al., 2017; Jonker et al., 2015) and travel‐related anxiety (Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014). Five studies focused on the combination of mood problems and self‐injurious behaviour (Stasolla, Damiani, et al., 2014; Stasolla et al., 2013, 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017; Stasolla, Perilli, et al., 2014).
3.3. Characteristics of the people delivering the psychological eHealth intervention
The interventions reported in the studies were delivered by a wide variety of people. Two interventions were delivered by parents at home who were being coached remotely by professionals qualified in Applied Behaviour Analysis and early interventions (Monlux et al., 2019; Simacek et al., 2017). Other interventions were delivered by support staff (n = 2) (Hoffman et al. 2017; Jonker et al. 2015) or teachers (n = 3) (Hetzroni & Banin, 2017; Kim et al., 2014; Singh et al. 2017). Therapists delivered the intervention in three studies: a clinical psychologist (Cooney et al., 2017), a dance and movement therapist supported by support staff from the day centre (Dunphy & Hens, 2018) and a psychologist working in collaboration with the class teacher and teaching assistant (Hronis et al., 2019). One study was delivered by a SafeCare® home visitor (Gaskin et al., 2012). Research assistants supported people with severe intellectual disabilities and motor disabilities during the intervention through a combination of verbal and physical prompting (n = 15) (Lancioni, O’Reilly, et al., 2013, 2006; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, et al., 2006; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni et al., 1998,1999,1997; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni, Smaldone, et al., 2006; Stasolla & O’Caffò, 2013; Stasolla et al., 2013, 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017). Parents and support staff were involved to provide information about the personal preferences of people with severe and profound intellectual disabilities. Seven studies failed to report who delivered the intervention (Lancioni, Singh, et al., 2013; Lancioni et al., ,2007, 2011; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Perilli et al., 2019; Stasolla, Damiani, et al., 2014; Stasolla, Perilli, et al., 2014).
3.4. Content of the studies reporting on psychological eHealth interventions
Overall, the content of the included studies reporting on psychological eHealth intervention can be classified into four types, which are not mutually exclusive and combining different types of content (e.g. the use of a video clip within a cognitive behavioural therapy). First, five studies used pictures and video clips of the participants with intellectual disabilities or the person who delivered the intervention (e.g. the teacher) to enable communication about the target behaviour (e.g. discuss about objectives and therapy progress) and to facilitate learning the desired skills rather than exhibiting challenging behaviour (Dunphy & Hens, 2018; Gaskin et al., 2012; Hetzroni & Banin, 2017; Kim et al., 2014; Singh et al., 2017). With respect to the latter, the participants were for example stimulated to display the behaviour learned in the intervention through using the eHealth application. By showing pictures of the participants involved displaying the desired behaviour on a digital screen, the application works as a primer prior to the school day beginning (Kim et al., 2014) or as a reminder (Gaskin et al., 2012), ultimately helping a mother with a mild intellectual disability to repeat the positive parental behaviour she had learned in between the sessions with the home visitor. Three other studies used video‐modelling clips of the participants to show good examples or the process of therapy progress (Dunphy & Hens, 2018; Hetzroni & Banin, 2017; Singh et al., 2017). In an intervention designed to encourage self‐management of aggression in three boys with mild intellectual disabilities, the boys learned to apply a mindfulness‐based procedure (Soles of Feet). More specific, the teacher recorded the Soles of Feet exercises on an iPad, so that they could use the exercises as an alternative to regulate their stress at both school and home (Singh et al., 2017). Another study reported on a programme that used video‐modelling clips of the participants themselves interacting with peers via a computer programme to recognize adequate and non‐adequate social behaviours, in combination with group discussions held in a classroom which involved practicing social skills in pairs under the instruction of a teacher (Hetzroni & Banin, 2017). Finally, the study of Dunphy and Hens (2018) reported on the use of the MARA app as a tool for monitoring the progress of participants in Dance and Movement Therapy (DMT) in line with specific objectives (e.g. movement and interpersonal functioning). This intervention also used video clips of the participants from six different sessions at the beginning, halfway point and end of the therapy to both discuss the progress of the therapy along with the participants and to share the results with relatives, staff and managers.
Second, in order to enable communication about the target behaviour and facilitate learning the desired skills rather than exhibiting challenging behaviour, four studies used a remote, mediated approach (Hoffman et al. 2017; Jonker et al. 2015; Monlux et al., 2019; Simacek et al., 2017). Two of these studies reported on interventions delivered by parents at home who were simultaneously being coached remotely by professionals via video telecommunication. They conducted a functional analysis of the problem behaviour of the child displaying challenging behaviour. The functional analysis was deployed together with the parent and supported the application of a subsequent tailor‐made behavioural programme. The parents received an instruction manual prior to the intervention with information, tips and supporting materials (e.g. red and green cards), and were given specific feedback via email after the session (Monlux et al., 2019; Simacek et al., 2017). In two other studies, support staff delivered a blended (i.e. combination of offline and online components) eHealth intervention for people with mild to moderate intellectual disabilities and visual impairments. Both studies reported on an intervention focused on separation anxiety, which was based on the ‘safe base, safe haven’ principle. Once they were separated during the intervention, the ‘safe base’ consisted of a reply from the support staff member confirming the emotion that the client had shared in the text message sent from their mobile phone (an adapted iPhone touch was provided to the visually impaired person). After the person with an intellectual disability and the person with a visual impairment were reunited with support staff, they both discussed the content of the messages to encourage the person to dare to express emotions while the support staff provided ‘a safe haven’ (Hoffman et al. 2017; Jonker et al. 2015).
Third, a computerized CBT approach was used in two studies (Cooney et al., 2017; Hronis et al., 2019). In Hronis et al. (2019) study, a psychologist delivered a group CBT intervention focused on anxiety, in collaboration with the class teacher and teacher's assistant, to a group of adolescents with intellectual disabilities. These face‐to‐face sessions led by the psychologist and the teacher comprised group and individual activities combined with an online programme to practise relevant CBT skills. Another CBT intervention was delivered by a clinical psychologist, who sat next to the person with an intellectual disability during the session. The person followed a computer‐based programme, which used social stories with avatars in a computer game to explain the cognitive mediated model. This computer‐based programme was combined with digital mindfulness and relaxation exercises at the end of each session. In addition, a workbook was used between the sessions to support the transfer of the skills they had learned in therapy into their daily lives (Cooney et al., 2017).
Fourth, in 22 studies, sensor technology detected the exposure of the target behaviour, such as touching objects without hand mouthing, followed by activation of an aversive1 or preferred stimulus (Lancioni et al., 1997, 1998, 1999, 2007, 2011; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Oliva, et al., 2008; Lancioni, Singh, O’Reilly, Sigafoos, Didden, Smaldone, et al., 2008; Lancioni, O’Reilly, et al., 2013, 2006; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni, Singh, O’Reilly, Sigafoos, et al., 2014; Lancioni, Singh, et al., 2013; Lancioni, Smaldone, et al., 2006; Perilli et al., 2019; Stasolla & O’Caffò, 2013; Stasolla et al., 2013, 2015; Stasolla, Perilli, Caffò, et al., 2017; Stasolla, Perilli, Damiani, et al., 2017). The vast majority of these studies included people with severe to profound intellectual disabilities with additional disabilities (e.g. motor and sensor disability) and used principles of behaviour modification that involved reinforcement schedules without any explicit prior functional assessment to identify the variables causing or maintaining the challenging behaviour. The conclusion of the researchers involved in these studies, nevertheless, was that the behaviour was not socially reinforced or related to specific events without providing any further details. A small number of the studies (n = 5) (Lancioni Markus et al., 1998, 1999; Lancioni, Singh, O’Reilly, Green, et al., 2014; Lancioni Van Houten et al., 1997; Stasolla et al., 2013) investigated the use of sensor technology which provided verbal feedback among people with mild to moderate intellectual disabilities. For example, in one study, a participant with an estimated moderate intellectual disability and severe motor and communication disabilities found sensor technology to be helpful for expressing his preferences, which, in turn, contributed to happiness (Stasolla et al., 2013).
4. DISCUSSION
In recent years, eHealth has increasingly been used in the field of intellectual disabilities, a shift which has been accelerated even more rapidly over the last few months due to the COVID‐19 pandemic. Although psychological eHealth interventions for people with intellectual disabilities are routinely being applied in daily practice, there is a relative dearth of knowledge in this area to inform both research and clinical practice. To address this scarcity of knowledge, this scoping review identified and summarized literature about psychological eHealth interventions among people with intellectual disabilities who also have mental health problems and/or exhibit challenging behaviour. The authors explored the characteristics of interventions, the participants, the people delivering the intervention and the content of 33 studies reporting on psychological eHealth interventions for people with intellectual disabilities.
With respect to the characteristics of the psychological eHealth interventions, the vast majority of the studies reported on interventions that were delivered at the individual level and within the individual's living environment or home of the person with intellectual disabilities. In so doing, such psychological interventions can overcome often cited physical and logistical barriers that hinders the access to mental health care and solve the challenge of transferring learned skill to personal life (Taylor et al., 2013; Whittle et al., 2018). More specifically, the transfer of learned skills from an intervention in the therapist's room to daily life and the recall of relevant situations to discuss in a session are often mentioned as significant barriers for people with an intellectual disability (Taylor et al., 2013). eHealth could overcome those barriers by delivering a psychological intervention in an individual's living environment or home, so a person with intellectual disabilities could benefit optimally from the intervention. An additional advantage of eHealth is that psychological eHealth interventions can be tailored (e.g. use of personal video clips, preferred stimuli as motivators, online homework assignments). Literature about the adaptations of psychological interventions among people with intellectual disabilities emphasizes the importance of adaptation within the provision of psychological therapies, such as using visual tools and the application of technology for monitoring target behaviour and progress (Jahoda et al., 2017; Whitehouse et al., 2006).
A notable finding of the scoping review is that only two studies reported about parents of young children exhibiting challenging behaviour being coached via telecare (i.e. delivering a psychological intervention through the use of video conferencing technology); no studies reported using telecare applications to deliver psychological interventions directly to people with intellectual disabilities. Research among the general population has reported on the feasibility of delivering effective psychological interventions via video conferencing with individuals, dyads and groups, and, in fact, has reported similar outcomes to interventions delivered on‐site (Banburry et al., 2018; Shaffer et al., 2020). The pilot or feasibility nature of studies fits into the early stage of developing effective eHealth interventions. That is, evaluation of the effectiveness of interventions (e.g. Thornicroft et al., 2011) and in particular eHealth interventions (e.g. Bonten et al., 2020) often starts with an initial phase in which the opportunities of eHealth interventions are explored in feasibility/pilot studies. Within those studies, the aim is to provide insight into the possibilities of psychological eHealth interventions rather than conducting these interventions to explore its effectiveness. When more evidence‐based knowledge is available with respect to psychological eHealth interventions, it is likely that other studies will be conducted as well, such as studies focusing on the effectiveness of a psychological eHealth intervention delivered directly to people with intellectual disabilities. Further, potential barriers for delivering psychological interventions directly may be the lack of access to digital devices (e.g. computer, laptop) and Internet, sensory and motor abilities to handle a device, digital literacy and cognitive burden (Lussiers‐Desrochers et al., 2017). Perceived barriers depend on the attitude of professionals, for example by assuming that delivering a psychological intervention to people with intellectual disabilities directly might be too difficult (Parsons et al., 2008). The COVID‐19 pandemic forced therapists to deliver psychological interventions to their clients directly, because on‐site support staff or relatives were not allowed to visit group homes. So, the current situation provides valuable insights into relevant aspects for delivering eHealth interventions to people with intellectual disabilities directly. In a review of telepsychiatry among people with intellectual disabilities in a psychiatric setting, Madhavan (2019) concluded that it constituted an effective means through which to empower people with intellectual disabilities, while, simultaneously, reducing costs.
Regarding the participants that were involved in the psychological eHealth interventions, both children and adults were included in the studies. More than half of the studies included participants with severe to profound intellectual disabilities who were engaged in self‐injurious and stereotypic behaviour and the interventions were focused primarily on learning adaptive behaviour and unlearning challenging behaviour. One‐third of the studies reported on psychological eHealth interventions among people with mild to moderate intellectual disabilities that were focused on anxiety and mood disorders. This latter focus is in accordance with psychological eHealth interventions among the general population suffering from mental health problems, which predominantly address anxiety and depression (Carlbring et al., 2018; Grist et al., 2019). However, psychological eHealth interventions among the general population serve a broader range of mental health problems that also happen to be especially prevalent among people with mild intellectual disabilities (e.g. anger, body dissatisfaction, PTSD and substance abuse). Both the broader range of mental health problems affecting people with intellectual disabilities besides anxiety and depression and the wealth of opportunities afforded by eHealth require further attention from researchers (Berryhill et al., 2018; Carlbring et al., 2018; Mevissen & De Jongh, 2010; Schützwohl et al., 2016). There is a scarcity of studies specifically focusing on psychological eHealth interventions for mental health problems among people with mild intellectual disabilities (n = 3), despite their increased risk of mental health problems (Bowring et al., 2019; Munir, 2016).
Regarding the characteristics of the people delivering psychological eHealth interventions, various persons were identified in this scoping review. All psychological eHealth interventions were either guided or therapist‐led interventions, with only a few interventions delivered by a therapist (e.g. clinical therapist). Support staff and teachers, were often involved as lay therapists along with non‐professionals, such as parents in the delivery of a psychological eHealth intervention. They were supervised by a clinical expert and provided with an instruction manual to increase the reliability of the treatment and the materials. Indeed, the participation of lay therapists is often used as a feasible method through which to deliver psychological interventions among people with intellectual disabilities (Jahoda et al., 2013). Within psychological eHealth interventions among the general population, non‐clinicians often function as lay therapists under the supervision of a psychologist as well (Titov et al., 2010). In general, the addition of human support leads to enhanced adherence to eHealth interventions (Mohr et al., 2011). The applicability and role of lay therapists within psychological eHealth interventions among people with intellectual disabilities requires further exploration. In contrast to a substantial number of eHealth interventions among the general population (Deady et al., 2017), this scoping review did only contain studies that used a guided approach.
There are some limitations of the scoping review that need to be addressed. First, only studies written in English were included, which means that relevant studies published in other languages have potentially been overlooked. Second, the quality of the evidence was not formally evaluated within this scoping review. More than 20% of the studies reported that their intervention was a pilot, trial, or feasibility study, with researchers openly acknowledging that they failed to meet the high‐quality research standards found, for example, in RCTs (e.g. Hronis et al., 2019). Given that the aim of this scoping review was to provide an overview of studies reporting on psychological eHealth interventions rather than assessing the quality of these studies, a quality appraisal was not carried out (Arksey & O’Malley, 2005). Third, similar to our previous systematic review (Oudshoorn et al., 2020), a notable challenge of this scoping review was to determine the concept of ‘eHealth’ itself, as it is regularly used as an umbrella term for a multitude of different ways of delivering and facilitating health care (Oh et al., 2005; Skär & Söderberg, 2017). Hence, it would be beneficial to formulate a clear definition of eHealth, which, in turn, would reduce the risk of misinterpreting what precisely eHealth is. Future research should therefore focus on developing a more concrete definition and rigorous conceptualization of the concept of eHealth.
This scoping review identified various psychological eHealth interventions, and reported on their specific characteristics. Although the current COVID‐19 pandemic has accelerated the use of eHealth with people with intellectual disabilities, unfortunately they have hitherto often been excluded from studies about psychological eHealth interventions targeted at the mainstream population, and in this respect scientific knowledge in this areas has not kept pace with knowledge development of psychological eHealth interventions among the general population (Brown et al., 2011). Hence, further research is needed to contribute to knowledge building about effective psychological eHealth interventions among people with intellectual disabilities who suffer from mental health problems and challenging behaviour. While some recent qualitative studies have shown that people with intellectual disabilities are, in general, interested in and open to eHealth, many obstacles still need to be overcome, including limited access to digital devices or lacking the necessary digital skills to participate in eHealth interventions (Cooney et al., 2018; Frielink et al., 2020; Vereenooghe et al., 2017). Moreover, it would be interesting for future research to explore the value of a blended format, combining face‐to‐face sessions with online sessions, which is now commonly utilized with the general population (Wentzel et al., 2016).
To conclude, this scoping review has demonstrated that eHealth provides an opportunity for therapists and lay therapists to deliver psychological eHealth interventions, which could range from a small component of a multimodal intervention up to a completely computerized, therapist‐led intervention. The inherent variety and flexibility of eHealth provides opportunities to overcome obstacles which are commonly encountered during face‐to‐face psychological interventions, especially as face‐to‐face sessions are impossible because of the COVID‐19 measures. eHealth enables the delivery of different forms of psychological eHealth interventions (e.g. CBT, mindfulness, Circle of Security), which may be helpful to people with intellectual disabilities, but also to their relatives and direct support staff, during the COVID‐19 pandemic (Courtenay & Perera, 2020). eHealth may solve access barriers and bring a therapist and the psychological intervention in the personal situation. The loss of professional care at home is a huge problem and increases anxiety and mental health problems in individuals previously receiving support (Embregts et al., 2020; Willner et al., 2020). The current situation requires patience and is a long‐term process in which eHealth could be ‘the digital bridge’ connecting people with intellectual disabilities who need mental health support and those who could deliver it.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTION
All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author byline.
ACKNOWLEDGEMENTS
The authors would like to thank Wichor Bramer, Information Specialist of Erasmus Medical Center Rotterdam, for his assistance for the literature search.
Funding information
This research was funded by service provider ASVZ. The authors would like to thank Prinsen Geerligs Foundation for their contribution to making this systematic review possible.
Footnotes
The use of aversive stimuli is less widely used in contemporary psychological interventions and could be considered as an unacceptable procedure of punishment.
REFERENCES
*Included studies in the scoping review.
- American Association of Intellectual and Developmental Disabilities . (2012). https://www.aaidd.org/intellectual‐disability/definition
- Arksey, H., & O’Malley, L. (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Banburry, A., Nancarrow, S., Dart, J., Gray, L., & Parkinson, L. (2018). Telehealth interventions delivering home‐based support group videoconferencing: Systematic review. Journal of Medical Internet Research, 20(2), e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berryhill, M. B., Culmer, N., Williams, N., Halli‐Tierney, A., Betancourt, A., Roberts, H., & King, M. (2018). Videoconferencing psychotherapy and depression: A systematic review. Telemedicine and e‐Health, 25(6), 435–446. 10.1089/tmj.2018.0058 [DOI] [PubMed] [Google Scholar]
- Bennett, C. B., Ruggero, C. J., Sever, A. C., & Yanouri, L. (2020). eHealth to redress psychotherapy access barriers both new and old: A review of reviews and meta‐analyses. Journal of Psychotherapy Integration, 30, 188–207. 10.1037/int0000217 [DOI] [Google Scholar]
- Bonten, T. N., Rauwerdink, A., Wyatt, J. C., Kasteleyn, M. J., Witkamp, L., Riper, H., van Gemert‐Pijnen, L. J., Chavannes, N. H., & Ehealth Evaluation Research Group . (2020). Online guide for electronic health evaluation approaches: Systematic Scoping Review and Concept Mapping Study. Journal of Medical Internet Research. 22(8), e17774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowring, D. L., Painter, J., & Hastings, R. P. (2019). Prevalence of challenging behaviour in adults with intellectual disabilities, correlates, and association with mental health. Current Developmental Disorders Reports, 6, 173–181. 10.1007/s40474-019-00175-9 [DOI] [Google Scholar]
- Bowring, D. L., Totsika, V., Hastings, R. P., Toogood, S., & Griffith, G. M. (2017). Challenging behaviours in adults with an intellectual disability: A total population study and exploration of risk indices. British Journal of Clinical Psychology, 56(1), 16–32. 10.1111/bjc.12118 [DOI] [PubMed] [Google Scholar]
- Bramer, W. M., Rethlefsen, M. L., Kleijnen, J., & Franco, O. H. (2017). Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Systematic Reviews, 6(245), 1–12. 10.1186/s13643-017-0644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Psychological Society . (2004). Challenging behaviours: Psychological interventions for severely challenging behaviours shown by people with learning disabilities. The British Psychological Society. [Google Scholar]
- Brown, M., Duff, H., Karatzias, T., & Horsburgh, D. (2011). A review of the literature relating to psychological interventions and people with intellectual disabilities: Issues for research, policy, education and clinical practice. Journal of Intellectual Disabilities, 15, 31–45. 10.1177/1744629511401166 [DOI] [PubMed] [Google Scholar]
- Campbell, M., Robertson, A., & Jahoda, A. (2014). Psychological therapies for people with intellectual disabilities: comments on a Matrix of evidence for interventions in challenging behaviour. Journal of Intellectual Disability Research, 58, 172–188. [DOI] [PubMed] [Google Scholar]
- Carlbring, P., Andersson, G., Cuijpers, P., Riper, H., & Hedman‐Lagerlöf, E. (2018). Internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta‐analysis. Cognitive Behaviour Therapy, 47, 1–18. 10.1080/16506073.2017.1401115 [DOI] [PubMed] [Google Scholar]
- Carr, A., Linehan, C., O’Reilly, G., Noohan Walsh, P., & Mc Evoy, J. (Eds). (2016). The handbook of intellectual disability and clinical psychology practice, 2nd ed. Routledge. [Google Scholar]
- *Cooney, P., Jackman, C., Coyle, D., & O’Reilly, G. (2017). Computerised cognitive‐behavioural therapy for adults with intellectual disability: Randomised controlled trial. The British Journal of Psychiatry, 211, 95–102. 10.1192/bjp.bp.117.198630 [DOI] [PubMed] [Google Scholar]
- Cooney, P., Jackman, C., Tunney, C., Coyle, D., & O'Reilly, G. (2018). Computer‐assisted cognitive behavioural therapy: The experiences of adults who have an intellectual disability and anxiety or depression. Journal of Applied Research in Intellectual Disability, 31, 1032–1045. 10.1111/jar.12459 [DOI] [PubMed] [Google Scholar]
- Cooper, S.‐A., Smiley, E., Finlayson, J., Jackson, A., Allan, L., Williamson, A., Mantry, D., & Morrison, J. (2007). The prevalence, incidence, and factors predictive of mental ill‐health in adults with profound intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 20, 493–501. 10.1111/j.1468-3148.2007.00401.x [DOI] [Google Scholar]
- Cooper, S.‐A., Smiley, E., Morrison, J., Williamson, A., & Allan, L. (2007). Mental ill‐health in adults with intellectual disabilities: prevalence and associated factors. British Journal of Psychiatry, 190, 27–35. [DOI] [PubMed] [Google Scholar]
- Courtenay, K. (2020). Covid‐19: challenges for people with intellectual disability. British Medical Journal, 369, m1609. [DOI] [PubMed] [Google Scholar]
- Courtenay, K., & Perera, B. (2020). COVID‐19 and people with intellectual disability: Impacts of a pandemic. Irish Journal of Psychological Medicine, 37(3), 231–236. 10.1017/ipm.2020.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deady, M., Choi, I., Calvo, R. A., Glozier, N., Christensen, H., & Harvey, S. B. (2017). eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta‐analysis. BMC Psychiatry, 17, 310. 10.1186/s12888-017-1473-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Didden, R., Korzelius, H., van Oorsouw, W., & Sturmey, P. (2006). Behavioral treatment of challenging behaviors in individuals with mild mental retardation: Meta‐analysis of single‐subject research. American Journal on Mental Retardation, 111, 290–298. [DOI] [PubMed] [Google Scholar]
- *Dunphy, K. F., & Hens, T. (2018). Outcome‐focused dance movement therapy assessment enhanced by iPad app MARA. Frontiers in Psychology, 9, 1–10. 10.3389/fpsyg.2018.02067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einfeld, S. L., Ellis, L. A., & Emerson, E. (2011). Comorbidity of intellectual disability and mental disorder in children and adolescents: A systematic review. Journal of Intellectual & Developmental Disability, 36(2), 137–143. [DOI] [PubMed] [Google Scholar]
- Embregts, P. J. C. M., van den Bogaard, K. H. J. M., Frielink, N., Voermans, M. A. C., Thalen, M., & Jahoda, A. (2020). A thematic analysis into the experiences of people with a mild intellectual disability during the COVID‐19 pandemic in the Netherlands. International Journal of Developmental Disabilities. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach, G. (2001). What is e‐health? Journal of Medical Internet Research, 3(2), E20. 10.2196/jmir.3.2.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frielink, N., Oudshoorn, C. E. M., & Embregts, P. J. C. M. (2020). eHealth in support for daily functioning of people with intellectual disability: Views of service users, relatives, and professionals on both its advantages and disadvantages and its facilitating and impeding factors. Journal of Intellectual & Developmental Disability. 10.3109/13668250.2020.1744878 [DOI] [Google Scholar]
- *Gaskin, E. H., Lutzker, J. R., Crimmins, D. B., & Robinson, L. (2012). Using a digital frame and pictorial information to enhance the SafeCare® Parent‐Infant Interactions module with a mother with intellectual disabilities: Results of a pilot study. Journal of Mental Health Research in Intellectual Disabilities, 5, 187–202. 10.1080/19315864.2012.674871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist, R., Croker, A., Denne, M., & Stallard, P. (2019). Technology Delivered Interventions for depression and anxiety in children and adolescents: A systematic review and meta‐analysis. Clinical Child and Family Psychology Review, 22, 147–171. 10.1007/s10567-018-0271-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hetzroni, O. E., & Banin, I. (2017). The effect of educational software, video modelling and group discussion on social‐skill acquisition among students with mild intellectual disabilities. Journal of Applied Research in Intellectual Disability, 30, 757–773. 10.1111/jar.12271 [DOI] [PubMed] [Google Scholar]
- *Hoffman, N., Sterkenburg, P. S., & Van Rensburg, E. (2017). The effect of technology assisted therapy for intellectually and visually impaired adults suffering from separation anxiety: Conquering the fear. Assistive Technology, 31, 98–105. 10.1080/10400435.2017.1371813 [DOI] [PubMed] [Google Scholar]
- *Hronis, A., Roberts, R., Roberts, L., & Kneeborne, I. (2019). FearlessMe!©: A feasibility case series of cognitive behavioural therapy for adolescents with intellectual disability. Journal of Clinical Psychology, 75, 919–932. 10.1102/jclp.22741 [DOI] [PubMed] [Google Scholar]
- Jahoda, A., Stenfert Kroese, B., & Pert, C. (2017). Cognitive behaviour therapy for people with intellectual disabilities. Thinking creatively. Palgrave Macmillan. [Google Scholar]
- Jahoda, A., Willner, P., Rose, J., Kroese, B. S., Lammie, C., Shead, J., Woodgate, C., Gillespie, D., Townson, J., Felce, D., Stimpson, A., Rose, N., MacMahon, P., Nuttall, J., & Hood, K. (2013). Development of a scale to measure fidelity to manualized group‐based cognitive behavioural interventions for people with intellectual disabilities. Research in Developmental Disabilities, 34, 4210–4221. 10.1016/j.ridd.2013.09.006 [DOI] [PubMed] [Google Scholar]
- *Jonker, D., Sterkenburg, P. S., & Van Rensburg, E. (2015). Caregiver‐mediated therapy for an adult with visual and intellectual impairment suffering from separation anxiety. Research in Developmental Disabilities, 47, 1–13. 10.1016/j.ridd.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Kelders, S. M., & Howard, M. (2018). Opportunities of technology to promote health and well‐being. In Van Gemert‐Pijnen L., Kelders S. M., Kip H., & Sanderman R. (Eds.), eHealth research, theory and development. A multidisciplinary approach (pp. 48–68). Routledge. [Google Scholar]
- *Kim, M., Blair, K.‐S.‐C., & Lim, K. (2014). Using tablet assisted Social Stories™ to improve classroom behaviour for adolescents with intellectual disabilities. Research in Developmental Disabilities, 35, 2241–2251. 10.1016/j.ridd.2014.05.011 [DOI] [PubMed] [Google Scholar]
- Kok, L., Van der Waa, A., Klip, H., & Staal, W. (2016). The effectiveness of psychosocial interventions for children with a psychiatric disorder and mild intellectual disability to borderline intellectual functioning: A systematic literature review and meta‐analysis. Clinical Child Psychology and Psychiatry, 21, 156–171. 10.1177/1359104514567579 [DOI] [PubMed] [Google Scholar]
- Koslowski, N., Klein, K., Arnold, K., Kösters, M., Schützwohl, M., Salize, H. J., & Puschner, B. (2016). Effectiveness of interventions for adults with mild to moderate intellectual disabilities and mental health problems: Systematic review and meta‐analysis. The British Journal of Psychiatry, 209(6), 469–474. [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Markus, S., & Behrendt, M. (1998). A portable vibratory‐feedback device for reducing excessive vocal loudness: A case study. Behavioural and Cognitive Psychotherapy, 26, 371–376. [Google Scholar]
- *Lancioni, G. E., Markus, S., & Behrendt, M. (1999). Vibratory versus auditory feedback for reducing excessive vocal loudness: A case study. Scandinavian Journal of Behaviour Therapy, 28, 150–153. 10.1080/028457199439892 [DOI] [Google Scholar]
- *Lancioni, G. E., O’Reilly, M. F., Singh, N. N., Sigafoos, J., Oliva, D., Alberti, G., Carrella, L., Didden, R., & Lang, R. (2013). Technology‐based programs to support adaptive responding and reduce hand mouthing in two persons with multiple disabilities. Journal of Developmental and Physical Disabilities, 25, 65–77. 10.1007/s10882-012-9303-3 [DOI] [Google Scholar]
- *Lancioni, G. E., O’Reilly, M. F., Singh, N. N., Sigafoos, J., Oliva, D., Baccani, S., & Groeneweg, J. (2006). Microswitch clusters promote adaptive responses and reduce finger mouthing in a boy with multiple disabilities. Behavior Modification, 30, 892–900. 10.1177/0145445505283416 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Green, V. A., Alberti, G., Boccasini, A., Smaldone, A., Oliva, D., & Bosco, A. (2014). Automatic feedback to promote safe walking and speech loudness control in persons with multiple disabilities: Two single‐case studies. Developmental Neurorehabilitation, 17, 224–231. 10.3109/17518423.2012.749953 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Oliva, D., Smaldone, A., Tota, A., Martielli, G., Stasolla, F., Pontiggia, G., & Groeneweg, J. (2006). Assessing the effects of stimulation versus microswitch‐based programmes on indices of happiness of students with multiple disabilities. Journal of Intellectual Disability Research, 50, 739–747. 10.1111/j.1365-2788.2006.00839.x [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Alberti, G., Oliva, D., & Buono, S. (2011). A technology‐aided stimulus choice program for two adults with multiple disabilities: Choice responses and mood. Research in Developmental Disabilities, 32, 2602–2607. 10.1016/j.ridd.2011.06.015 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Boccasini, A., La Martire, M. L., Oliva, D., & Lang, R. (2014). Orientation technology to help persons with blindness and multiple disabilities manage indoor travel and travel‐related anxiety. Journal of Intellectual and Developmental Disability, 39, 198–205. 10.1016/j.ridd.2011.06.015 [DOI] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Didden, R., Oliva, D., & Cingolani, E. (2008). A girl with multiple disabilities increases object manipulation and reduces hand mouthing through a microswitch‐based program. Clinical Case Studies, 7, 238–249. 10.1177/1534650107307478 [DOI] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Didden, R., Smaldone, A., & Oliva, D. (2008). Helping a man with multiple disabilities increase object‐contact responses and reduce hand stereotypy via a microswitch cluster program. Journal of Intellectual & Developmental Disability, 33, 349–353. 10.1080/13668250802441664 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Oliva, D., Boccasini, A., La Martire, M. L., D’Amico, F., & Sasanelli, G. (2013). Persons with multiple disabilities increase adaptive responding and control inadequate posture or behavior through programs based on microswitch‐cluster technology. Research in Developmental Disabilities, 34, 3411–3420. 10.1016/j.ridd.2013.07.014 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Oliva, D., Pidala, S., Piazzolla, G., & Bosco, A. (2007). Promoting adaptive foot movements and reducing hand mouthing and eye poking in a boy with multiple disabilities through microswitch technology. Cognitive Behaviour Therapy, 36, 85–90. 10.1080/16506070601097999 [DOI] [PubMed] [Google Scholar]
- *Lancioni, G. E., Smaldone, A., O’Reilly, M. F., Singh, N. N., Sigafoos, J., Oliva, D., & Bosco, A. (2006). Promoting adaptive hand responding and reducing face hiding in a woman with profound developmental disabilities using microswitch technology. Behavioural and Cognitive Psychotherapy, 35, 225–230. 10.1017/S1352465806003353 [DOI] [Google Scholar]
- *Lancioni, G. E., Van Houten, K., & Ten Hoopen, G. (1997). Reducing excessive vocal loudness in persons with mental retardation through the use of a portable auditory‐feedback device. Journal of Behavior Therapy and Experimental Psychiatry, 28, 123–128. [DOI] [PubMed] [Google Scholar]
- Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: advancing the methodology. Implementation Science, 5, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. A., Clarke, M., Devereaux, P. J., Kleijnen, J., & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine, 6, 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe, K., Allen, D., Jones, E., Brophy, S., Moore, K., & James, W. (2007). Challenging behaviours: prevalence and topographies. Journal of Intellectual Disability Research, 51, 625–636. 10.1111/j.1365-2788.2006.00948.x [DOI] [PubMed] [Google Scholar]
- Lussier‐Desrochers, D., Norman, C. L., Romero‐Torres, A., Lachapelle, Y., Godin‐Tremblay, V., Dupont, M., … Bilodeau, P. (2007). Bridging the digital divide for people with intellectual disability. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 11(1). 10.5817/CP2017-1-1 [DOI] [Google Scholar]
- Madhavan, G. (2019). Telepsychiatry in intellectual disability psychiatry: Literature review. BJPsych Bulletin, 43, 167–173. 10.1192/bjb.2019.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mevissen, L., & De Jongh, A. (2010). PTSD and its treatment in people with intellectual disabilities: A review of the literature. Clinical Psychology Review, 30, 308–316. [DOI] [PubMed] [Google Scholar]
- Mohr, D. C., Cuijpers, P., & Lehman, K. (2011). Supportive accountability: A model for providing human support to enhance adherence to ehealth interventions. Journal of Medical Internet Research, 13, e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Monlux, K. D., Pollard, J. S., Bujanda Rodriguez, A. Y., & Hall, S. S. (2019). Telehealth delivery of function‐based behavioral treatment for problem behaviors exhibited by boys with Fragile X Syndrome. Journal of Autism and Developmental Disorders, 49, 2461–2475. 10.1007/s10803-019-03963-9 [DOI] [PubMed] [Google Scholar]
- Munir, K. (2016). The co‐occurrence of mental disorders in children and adolescents with intellectual disability/intellectual developmental disorder. Curr Opin Psychiatry, 29(2), 95–102. 10.1097/YCO.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh, H., Rizo, C., Enkin, M., Jadad, A., Powell, J., & Pagliari, C. (2005). What is eHealth (3): A systematic review of published definitions. Journal of Medical Internet Research, 7, 1–12. 10.2196/jmir.7.1.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osugo, M., & Cooper, S.‐A. (2016). Interventions for adults with mild intellectual disabilities and mental ill‐health: a systematic review. Journal of Intellectual Disability Research, 60, 615–622. 10.1111/jir.12285 [DOI] [PubMed] [Google Scholar]
- Oudshoorn, C. E. M., Frielink, N., Nijs, S. L. P., & Embregts, P. J. C. M. (2020). eHealth in the support of people with mild intellectual disability in daily life: A systematic review. Journal of Applied Research in Intellectual Disability, 33(6), 1166–1187. 10.1111/jar.12758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, S., Daniels, H., Porter, J., & Robertson, C. (2008). Resources staff beliefs and organizational culture: Factors in the use of information and communication technology for adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 21, 19–33. [Google Scholar]
- *Perilli, V., Stasolla, F., Caffò, A. O., Albano, V., & D’Amico, F. (2019). Microswitch‐Cluster technology for promoting occupation and reducing hand biting of six adolescents with Fragile X Syndrome: New evidence and social rating. Journal of Developmental and Physical Disabilities, 31, 115–133. 10.1007/s10882-018-9634-9. [DOI] [Google Scholar]
- Poppes, P., Van der Putten, A. A., & Vlaskamp, C. (2014). Addressing challenging behavior in people with profound intellectual and multiple disabilities: Analyzing the effects of daily practice. Journal of Policy and Practice in Intellectual Disabilities, 11(2), 128–136. [Google Scholar]
- Proudfoot, J., Klein, B., Barak, A., Carlbring, P., Cuijpers, P., Lange, A., Ritterband, L., & Andersson, G. (2011). Establishing guidelines for executing and reporting internet intervention research. Cognitive Behavior Therapy, 40(2), 82–97. [DOI] [PubMed] [Google Scholar]
- Ramsden, S., Tickle, A., Dawson, D. L., & Harris, S. (2016). Perceived barriers and facilitators to positive therapeutic change for people with intellectual disabilities: Client, care and clinical psychologist perspectives. Journal of Intellectual Disabilities, 20, 241–262. 10.1177/1744629515612627 [DOI] [PubMed] [Google Scholar]
- Schützwohl, M., Koch, A., Koslowski, N., Puschner, B., Voß, E., Salize, H. J., Pfennig, A., & Vogel, A. (2016). Mental illness, problem behaviour, needs and service use in adults with intellectual disability. Social Psychiatry and Psychiatry Epidemiology, 51, 767–776. 10.1007/s00127-016-1197-4 [DOI] [PubMed] [Google Scholar]
- Shaffer, K. M., Tigershtrom, A., Badr, H., Benvengo, S., Hernandez, M., & Ritterband, L. M. (2020). Dyadic psychosocial eHealth interventions: systematic scoping review. Journal of Medical Internet Research, 22(3), e15509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Simacek, J., Dimian, A. F., & McComas, J. J. (2017). Communication intervention for young children with severe neurodevelopmental disabilities via telehealth. Journal of Autism and Developmental Disorders, 47, 744–767. 10.1007/s10803-016-3006-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Singh, N. N., Chan, J., Karazsia, B. T., McPherson, C. L., & Jackman, M. M. (2017). Tele‐health training of teachers to teach a mindfulness‐based procedure for self‐management of aggressive behavior to students with intellectual and developmental disabilities. International Journal of Developmental Disabilities, 63, 195–203. 10.1080/20473869.2016.12778441 [DOI] [Google Scholar]
- Skär, L., & Söderberg, S. (2017). The importance of ethical aspect when implementing eHealth services in healthcare: A discussion paper. Journal of Advanced Nursing, 74, 1043–1050. [DOI] [PubMed] [Google Scholar]
- *Stasolla, F., Damiani, R., Perilli, V., Di Leone, A., Albano, V., Stella, A., & Damato, C. (2014). Technological supports to promote choice opportunities by two children with fragile X syndrome and severe to profound developmental disabilities. Research in Developmental Disabilities, 35, 2993–3000. 10.1016/j.ridd.2014.07.045 [DOI] [PubMed] [Google Scholar]
- *Stasolla, F., & O’Caffò, A. O. (2013). Promoting adaptive behaviors by two girls with Rett syndrome through a microswitch‐based program. Research in Autism Spectrum Disorders, 7, 1265–1272. 10.1016/j.rasd.2013.07.010 [DOI] [Google Scholar]
- *Stasolla, F., O’Caffò, A. O., Picucci, L., & Bosco, A. (2013). Assistive technology for promoting choice behaviors in three children with cerebral palsy and severe communication impairments. Research in Developmental Disabilities, 34, 2694–2700. 10.1016/j.ridd.2013.05.029 [DOI] [PubMed] [Google Scholar]
- *Stasolla, F., Perilli, V., Caffò, A. O., Boccasini, A., Stella, A., Damiani, R., Albano, V., D’Amico, F., Damato, C., & Albano, A. (2017). Extending microswitch‐cluster programs to promote occupation activities and reduce mouthing by six children with autism spectrum disorders and intellectual disabilities. Journal of Developmental and Physical Disabilities, 29, 307–324. [Google Scholar]
- *Stasolla, F., Perilli, V., Damiani, R., & Albano, V. (2017). Assistive technology to promote occupation and reduce mouthing by three boys with fragile X syndrome. Developmental Neurorehabilitation, 20, 185–193. 10.3109/17518423.2015.1133724 [DOI] [PubMed] [Google Scholar]
- *Stasolla, F., Perilli, V., Damiani, R., O’Caffò, A. O., Di Leone, A., Albano, V., Stella, A., & Damato, C. (2014). A microswitch‐cluster program to enhance object manipulation and to reduce hand mouthing by three boys with autism spectrum disorders and intellectual disabilities. Research in Autism Spectrum Disorders, 8, 1071–1078. 10.1016/j.rasd.2014.05.016 [DOI] [Google Scholar]
- *Stasolla, F., Perilli, V., Di Leone, A., Damiani, R., Albano, V., Stella, A., & Damato, C. (2015). Technological aids to support choice strategies by three girls with Rett syndrome. Research in Developmental Disabilities, 36, 36–44. 10.1016/j.ridd.2014.09.017 [DOI] [PubMed] [Google Scholar]
- Taylor, J. L., Lindsay, W. R., Hastings, R. P., & Hatton, C. (Eds). (2013). Psychological therapies for adults with intellectual disabilities. Wiley‐Blackwell. [Google Scholar]
- Thornicroft, G., Lempp, H., & Tansella, M. (2011). The place of implementation science in the translational medicine continuum. Psychological Medicine, 41, 2015–2021. [DOI] [PubMed] [Google Scholar]
- Titov, N., Andrews, G., Davies, M., McIntyre, K., Robinson, E., & Solley, K. (2010). Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLoS One, 5(6), e10939. 10.1371/journal.pone.0010939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous, J., Myrick, K. J., Rauseo‐Ricupero, N., & Firth, J. (2020). Digital mental health and COVID‐19: Using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health, 7(3), e18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gemert‐Pijnen, L., Kelders, S. M., Kip, H., & Sanderman, R. (Eds). (2018). eHealth research, theory and development. A Multidisciplinary Approach. Routledge. [Google Scholar]
- Vereenooghe, L., Flynn, S., Hastings, R. P., Adams, D., Chauhan, U., Cooper, S.‐A., & Waite, J. (2018). Interventions for mental health problems in children and adults with severe intellectual disabilities: a systematic review. British Medical Journal Open, 8, e021911. 10.1136/bmjopen-2018-021911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vereenooghe, L., Gega, L., & Langdon, P. (2017). Intellectual disability and computers in therapy: Views of service users and clinical psychologists. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 11(1). 10.5817/CP2017-1-11 [DOI] [Google Scholar]
- Vereenooghe, L., & Langdon, P. (2013). Psychological therapies for people with intellectualdisabilities: A systematic review and meta‐analysis. Research in Developmental Disabilities, 34, 4085–4102. [DOI] [PubMed] [Google Scholar]
- VGN . (2020). The effects of COVID‐19 on direct support staff. https://www.vgn.nl/nieuws/laatste‐nieuws‐over‐het‐coronavirus [Google Scholar]
- Wanglin, B. C., Szafranski, D. D., & Gros, D. F. (2016). Telehealth technologies in evidence‐based psychotherapy. In Luiselli J. K., & Fischer A. J. (Eds.), Computer‐assisted and web‐based innovations in psychology, special education, and health (pp. 119–140). Academic Press. [Google Scholar]
- Wentzel, J., van der Vaart, R., Bohlmeijer, E. T., & van‐Gemert‐Pijnen, J. E. (2016). Mixing online and face‐to‐face therapy: how to benefit from blended care in mental health care. JMIR Mental Health, 3(1), e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehouse, R. M., Tudway, J. A., Look, R., & Stenfert Kroese, B. (2006). Adapting individual psychotherapy for adults with intellectual disabilities: A comparative review of the cognitive–behavioural and psychodynamic literature. Journal of Applied Research in Intellectual Disability, 19, 55–65. 10.1111/j.1468-3148.2005.00281.x [DOI] [Google Scholar]
- Whittle, E. L., Fisher, K. R., Reppermund, S., Lenroot, R., & Trollor, J. (2018). Barriers and enablers to accessing mental health services for people with intellectual disability: A scoping review. Journal of Mental Health Research in Intellectual Disabilities, 11, 69–102. 10.1080/19315864.2017.1408724 [DOI] [Google Scholar]
- Willner, P., Rose, J., Stenfert Kroese, B., Murphy, G. H., Langdon, P. E., Clifford, C., Hutchings, H., Watkins, A., Hiles, S., & Cooper, V. (2020). Effect of the COVID‐19 pandemic on the mental health of carers of people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities: JARID, 33(6), 1523–1533. 10.1111/jar.12811 [DOI] [PubMed] [Google Scholar]
- Wind, T. R., Rijkeboer, M., Andersson, G., & Riper, H. (2020). The COVID‐19 pandemic: The ‘black swan’ for mental health care and a turning point for e‐health. Internet Interventions, 20, 100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Mental health and psychosocial considerations during the COVID‐19 outbreak. https://apps.who.int/iris/bitstream/handle/10665/331490/WHO‐2019‐nCoV‐MentalHealth‐2020.1‐eng.pdf [Google Scholar]


