Abstract
The Charcot knee is a progressive, degenerative disease of the joint that may represent a diagnostic challenge; at the moment, poorly controlled diabetes mellitus is the main cause of this condition. We describe here a case of a man presenting with an end stage joint arthropathy who was diagnosed with neurosyphilis. Tabetic arthropathy is currently a very rare disease, but in the past represented the main cause of joint arthropathy. Finally, we discussed the different surgical options of Charcot arthropathy, our choice of megaprosthesis implant and the failure of such procedure mainly due to patient’s unreliability to care leading to infective complications and peri-prosthesis fracture.
Key Words: Arthroplasty, Charcot, Knee, Syphilis, Tabetic arthropaty
Introduction
Neuropathic arthropathy is a progressive and degenerative process that leads to destruction and collapse of the weight-bearing surface of joints, of the sub-chondral bone and to the development of large effusions that stretch and damage supporting soft-tissue structures (1,2). In the past, tabetic arthropathy, described by Jean Martin Charcot in 1868, was the most common cause of neuropathic arthropathy; currently, it is an unusual finding because of the early diagnosis and treatment of syphilis,and the most common cause of Charcot arthropathy is represented by poorly controlled diabetes mellitus an early detection of Charcot arthropathy is mandatory for these patients to prevent cartilage injuries and avoid disease progression with deformity and joints destruction (3-5).
The surgical treatment of Charcot knee remains controversial; in the past, it was considered an absolute contraindication for implant of total knee arthroplasty TKA due to the less favorable outcome secondary to unstable neurologic status, development of ataxia, severe joints destruction, bone defects, and deformities (6-9). However, this reports had usually a short follow-up, did not included homogeneous patients, and used different type of prostheses. Nevertheless, despite the technical challenges of the procedure and the high rate of complications reported including peri-prosthetic joint infection, tibiofemoral dislocation and periprosthetic fractures,other authors reported satisfactory results with the use of increased constraint, stems, augments, and revision-type TKA components (10-12).
We report here a case of a patients presenting with a severe Charcot arthropathy who was finally diagnosed with an end stage neurosyphilis; the patient was initially treated with a knee’s megaprosthesis but developed major complications during follow-up leading to amputation.
Case Report
A 67-years old man attended to the Emergency Department for progressive swelling of the right knee with edema and worsening pain of the entire right leg [Figure 1]. A color Doppler ultrasound excluded deep venous thrombosis. X-ray and CT scan of the knee showed deformity of the femoral-tibial joint with erosion of the medial femoral condyle and significant intra-articular swelling, with local contrast-enhancement; MRN confirmed severe joint erosion, diffused calcifications and inhomogeneus contrast enhancement of the bone at the femoral condyle and at tibial plateau, compatible with osteomyelitis [Figure 2-5]. Arthrocentesis was negative for septic arthritis findings; finally, scintigraphy with marked leucocytes confirmed an uneven hyper-captation of the right knee. Autoimmunity pattern and blood tests were normal, including C-reactive protein and procalcitonin; blood and urine cultures were negative for bacteria and fungi. A bone biopsy showed aspecific lymphoplasmacellular infiltrate. Charcot arthropathy was suspected but the patient had persistently normal glucose levels and glycated hemoglobin levels of 36 mmol/mol (normal value < 42 mmol/mol). Finally, syphilis was suspected and rapid plasma reagin (RPR) and TPHA were done, resulting positive at significant titers in both plasma and cefalorachidian liquor. Intravenous ceftriaxon (2 grams/daily) was then administered (patient had a past history of allergy to penicillin) for 14 days before surgery.
Figure 1.
Pre-operative swelling and varus deviation
Figure 2.
X-ray lateral view in emergency room
Figure 5.
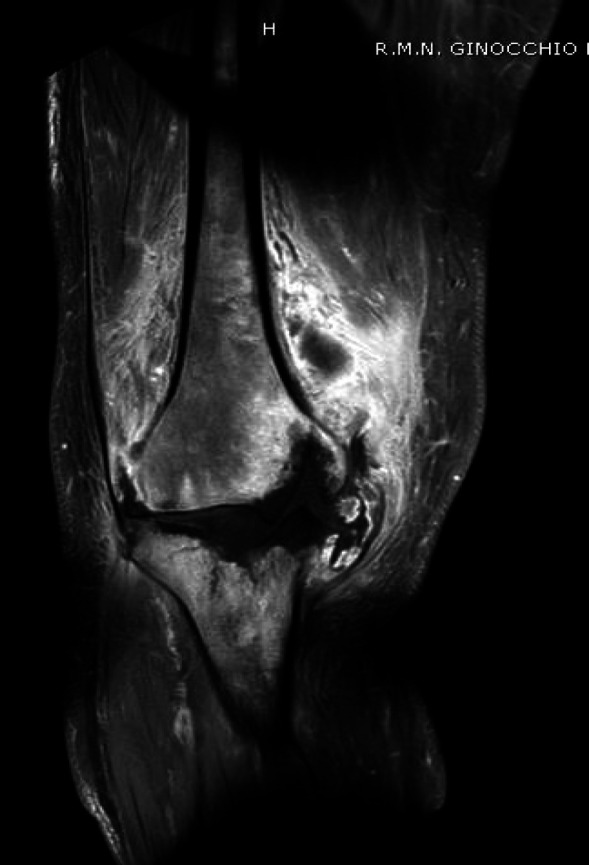
Erosion of the medial femoral condyle and significant bone edema and swelling
Due to the rapid joint and bone destruction occurred in three months from admission, an implant of knee megaprosthesis was planned; two weeks after surgery, the patient had an accidental trauma with damage of the knee extensor system and lateral dislocation of the patella [Figure 6-12]. In the next few days, a delayed healing of the surgical wound was observed and meticillyn-resistant Staphylococcus aureus was isolated from culture. Daptomycin was then started associated with local VAC therapy leading to a progressive improvement of the surgical wound. After 4 weeks of intravenous daptomycin, antibiotic treatment was shifted, according to antibiogram, to trimethoprim/sulfamethoxazole and doxycicline and the patient was finally discharged from the hospital. Two weeks later, the patient had an accidental fall that resulted in a peri-prosthetic, open fracture b3 type Vancouver [Figure 13; 14]. Further, the patients revealed that he had taken antibiotic therapy only occasionally and rejected to continue the treatment. Meticillyn-resistant Staphylococcus aureus was isolated again from surgical wound. As a consequence , considering the severity of the fracture, the persistence of meticillyn-resistant Staphylococcus aureus and the patient’s unreliability to care, we decided to amputate the leg [Figure 15; 16].
Figure 6-7.

Pre-operative x ray: rapid joint and bone destruction occurred in three months from admission
Figure 13.

Traumatic tibial peripro-sthetic fracture: antero-posterior view
Figure 15.
Periprosthetic joint infection
Discussion
Currently, the main cause of Charcot knees is diabetes mellitus; destructive tabetic arthropathy has become rare in the course of tertiary syphilis because of early diagnosis and treatment. Tabetic arthropathy occurs in the late stages of the disease, usually 20 to 30 years when primary syphilis is not properly treated. This condition results in loss of perception of pain combined with repeated subclinical micro-trauma leading to significant fragmentation, destruction and collapse of joints that is typical of Charcot arthropathy. Syphilis peripheral neuropathy is not always present, therefore joint changes can precede neurological deficit. In advanced stages, bone destruction with soft tissue changes leads to deformities. Patients usually have very mild symptoms compared to radiological findings that include subchondral sclerosis, osteophytosis, subluxation and soft tissue swelling. Long-standing neuro-arthropaty is characterized by a subversion of joints. It’s really hard to come up to diagnosis during the evolution of the disease; in fact, our patient was not aware of having a tertiary syphilis because he never had symptoms compatible with primary or secondary syphilis. During the diagnostic phase, the patient underwent to rapid and progressive joint destruction with loss of functionality, therefore no chance of conservative treatment was possible. At the early stage of disease, differential diagnosis with osteomyielitis, osteonecrosis, calcium pyrophosphate dihydrate crystal deposition disease, psoriac arthritis and osteoarthritis was difficult because swelling and little pain prevailed on the deformity pattern
Once eradication treatment for tertiary syphilis was completed, the surgical approach was considered. In the early stages of joint involvement, the Charcot’s knee treatment includes local treatment such as joint lavage, local steroid, or synoviorthesis. Palliative reduction of instability by immobilization and weight control are important to reduce micro-traumas that can deteriorate the joints Arthrodesis of the knee has been performed since the early 1900s to treat pain and instability associated with advanced osteoarthritis, post-traumatic arthritis, Charcot arthropathy, infectious arthritis, poliomyelitis, and reconstruction following tumor resection. Massive bone loss may substantially reduce the success rate of arthrodesis (6). Nevertheless, many patients with Charcot arthropathy are choosing to preserve motion with a total knee arthroplasty, considering arthrodesis only in case of failure of this procedure. Arthrodesis is a possible surgical treatment option, but it usually results in poor limb function; on the contrary, total knee arthroplasty could guarantee a better functional outcome (13-15). Some authors suggest that there are distinct stages of neuro-arthropathy based on clinical and imaging patterns. This should be consider when planning surgery because poor outcomes after TKA for Charcot knees are often obtained from unnecessarily early surgery; as a consequence surgical intervention should be considered only in the reconstruction or coalescence stages. Sometimes fragmentation, destruction and coalescence coexisted in the same knee and is not simple choose the perfect timing for surgery. The choice of the type of constraint in Charcot’s knee is still debated. Although most authors consider unconstrained or highly constrained components inappropriate for Charcot knees, others demonstrated that condylar constrained implants are the optimal choice and that hinged components are inappropriate because of the high risk of periprosthetic fractures and aseptic loosening. Strong constraint is likely to increase the stress on the implant–bone interface, leading to a high risk of failure. However constrained condylar and rotating hinge prostheses are used for Charcot joints with bone deficiency and soft tissue imbalance. Further, even if Charcot arthropathy is not an absolute contraindication to total knee replacement, the use of this procedure is associated with a high risk of serious complications. Finally, megaprostheses play a decisive role in rescuing joints that present severe bone loss, when it is necessary to preserve a joint function or when the loss of substance does not allow arthrodesis without significant shortening (16).
In our patient, the metaphyseal involvement of both femur and tibia led us to choose the constrained megaprosthesis, to bridge the bone loss. The choice of megaprosthesis could provide a better functional outcome while preserving the limb but with the awareness of possible systemic and local complications associated with the prosthetic implant. The management of the extensor mechanism was technically performed by the anterior transposition of the tendons of the medial and lateral twins and thanks to the quadriceps tenodesis obtained with non-absorbable high resistance points.
At our knowledge, this is the first case of Charcot knee treated with a modular megaprosthesis implant. Amputation, as an additional surgical option, should be considered only in case of implant failure mainly due to infective complications and periprosthesis fractures related to a low pain perception as occurred in our patient.
The timing and surgery technique and the prosthesis choice should be carefully considering before arthroplasty and these choices should be done according to patient’s clinical condition. Amputation represents a possible alternative in case of implant failure; modern leg prosthesis may guarantee an acceptable quality of life in this specific conditions.
Figure 3.

X-ray Antero-posterior view in emergency room
Figure 4.

pre-operative 3D CTscan
Figure 8.
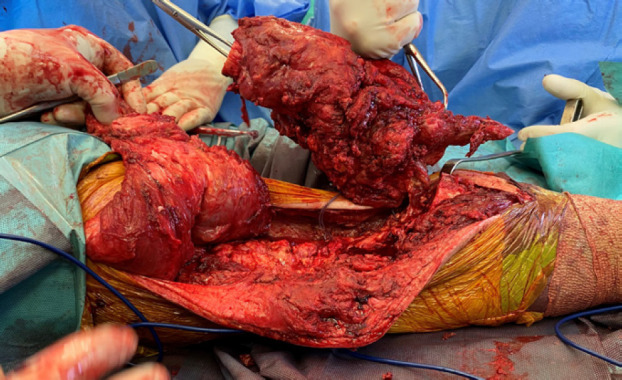
Bone resection
Figure 9.
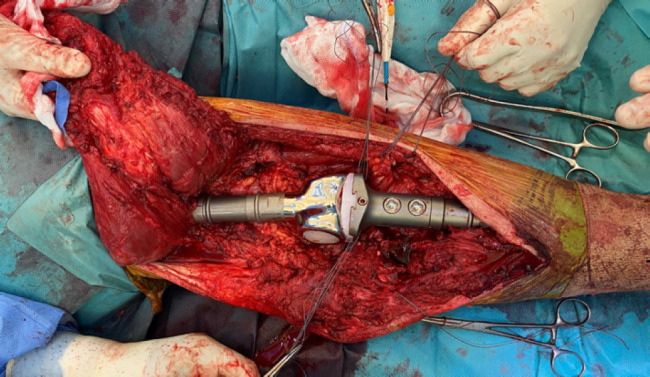
Implant of knee megaprosthesis
Figure 10.

Implant of knee megaprosthesis
Figure 11.

Post operative X-ray: antero-posterior view
Figure 12.

Post operative x-ray: laterl view
Figure 14.

Traumatic tibial peripro-sthetic fracture: lateral view
Figure 16.
Above the knee amputation
References
- 1.Tibbo ME, Chalmers BP, Berry DJ, Pagnano MW, Lewallen DG, Abdel MP. Primary Total Knee Arthroplasty in Patients With Neuropathic (Charcot) Arthropathy: Contemporary Results. J Arthroplasty. 2018;33(9):2815–2820. doi: 10.1016/j.arth.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Koshino T. Stage classifications, types of joint destruction, and bone scintigraphy in Charcot joint disease. Bull Hosp Jt Dis Orthop Inst. 1991;51(2):205–17. [PubMed] [Google Scholar]
- 3.Allali F, Rahmouni R, Hajjai-Hassouni N. Tabetic arthropathy A report of 43 cases. Clin Rheumatol. 2006;25(6):858–860. doi: 10.1007/s10067-006-0205-6. [DOI] [PubMed] [Google Scholar]
- 4.Kucera T, Urban K, Sponer P. Charcot arthropathy of the knee A case-based review. Clin Rheumatol. 2011;30(3):425–8. doi: 10.1007/s10067-010-1617-x. [DOI] [PubMed] [Google Scholar]
- 5.Bae DK, Song SJ, Yoon KH, Noh JH. Long-Term Outcome of Total Knee Arthroplasty in Charcot Joint A 10- to 22-Year Follow-Up. J Arthroplasty. 2009;24(8):1152–6. doi: 10.1016/j.arth.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Marmor L. The Marmor knee replacement. Orthop Clin North Am. 1982;13(1):55–64. [PubMed] [Google Scholar]
- 7.Ranawat CS, Shine JJ. Duo-condylar total knee arthroplasty. Clin Orthop. 1973;(94):185–95. doi: 10.1097/00003086-197307000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Yasuda M, Inoue K, Ikawa T, Yukioka M, Shichikawa K. A giant thigh mass in a patient with total knee arthroplasty for Charcot joint. Clin Orthop. 1995;(317):159–61. [PubMed] [Google Scholar]
- 9.Kim YH, Kim JS, Oh SW. Total knee arthroplasty in neuropathic arthropathy. J Bone Joint Surg Br .2002;84(2):216–9. doi: 10.1302/0301-620x.84b2.12312. [DOI] [PubMed] [Google Scholar]
- 10.Parvizi J, Marrs J, Morrey BF. Total knee arthroplasty for neuropathic (Charcot) joints. Clin Orthop Relat Res. 2003;(416):145–50. doi: 10.1097/01.blo.0000081937.75404.ed. [DOI] [PubMed] [Google Scholar]
- 11.Zeng M, Xie J, Hu Y. Total knee arthroplasty in patients with Charcot joints. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2672–7. doi: 10.1007/s00167-016-4073-6. [DOI] [PubMed] [Google Scholar]
- 12.Yang JH, Yoon JR, Oh CH, Kim TS. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):517–23. doi: 10.1007/s00167-011-1590-1. [DOI] [PubMed] [Google Scholar]
- 13.DRENNAN DB, FAHEY JJ, MAYLAHN DJ. Important factors in achieving arthrodesis of the Charcot knee. JBJS. 1971;53(6):1180–93. [PubMed] [Google Scholar]
- 14.Gualtieri G, Sudanese A, Toni A, Giunti A. Loosening of a hip prosthesis in a patient affected with tabetic disease. La Chirurgia degli organi di movimento. 1991;76(1):83–5. [PubMed] [Google Scholar]
- 15.Green DP, Parkes JC 2nd, Stinchfield FE. Arthrodesis of the knee A follow up study. J Bone Joint Surg Am. 1967;49(6):1065–78. [PubMed] [Google Scholar]
- 16.Calori GM, Colombo M, Ripamonti C, Malagoli E, Mazza E, Fadigati P, et al. Megaprosthesis in large bone defects: opportunity or chimaera? Injury. 2014;45(2):388–93. doi: 10.1016/j.injury.2013.09.015. [DOI] [PubMed] [Google Scholar]






