Abstract
The reported dissatisfaction rate after primary total knee arthroplasty (TKA) ranges between 15% and 25%. The purpose of this article is to perform a narrative review of the literature with the aim of answering the following question: What are the main factors contributing to patient dissatisfaction after TKA? A review of the literature was performed on patient satisfaction after TKA. The search engines used were MedLine (PubMed) and the Cochrane Library. The keywords used were “TKA” and “satisfaction”. The main reported preoperative factors positively contributing to patient satisfaction were the following: fulfilment of preoperative expectations, preoperative complete joint space collapse, increasing patellar and lateral compartment osteophyte size, and TKA communication checklist. The principal preoperative factors negatively contributing to patient satisfaction included female sex, comorbidities, and Hispanic race. The chief perioperative factor positively contributing to patient satisfaction was cosmetic closure, whereas the fundamental perioperative factors negatively contributing to patient satisfaction included joint laxity, anterior tibial component slope, and greater femoral component valgus angle. The principal postoperative factors positively contributing to patient satisfaction were the following: ameliorated walking distance, improved range of motion, and improvements in pain. The most important postoperative factors negatively contributing to patient satisfaction included poor postoperative knee stability and soft-tissue balance, functional limitation, surgical complication and reoperation, staff or quality of care issues, and increased stiffness.
Key Words: Arthroplasty, Knee, Patient satisfaction, Total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is one of the most commonly performed surgical procedures in the United States, with approximately 2% of the population having had a primary TKA, and soon to be well above 1 million procedures performed annually. Some studies have reported the rate of satisfied patients following their primary TKA to range from 85% to 90%, but with considerable variability.
The capability to identify patients at risk for dissatisfaction would be paramount to counsel, educate, and possibly diminish the overall rate of dissatisfied patients (1). TKA is a treatment alternative for severe osteoarthritis (OA), and most patients profit from this surgical procedure by experiencing reduced knee pain, ameliorated function, and augmented quality of life. Despite these factual improvements, a high dissatisfaction rate after TKA has been reported (15%–25% of patients) (2).
Materials and Methods
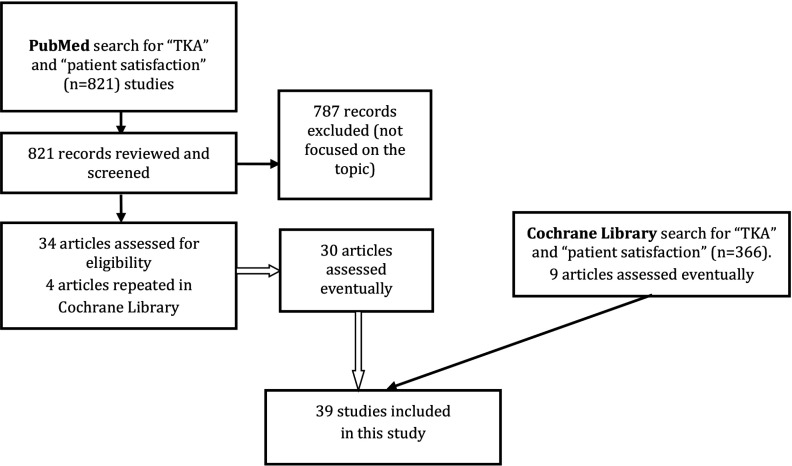
A review of the literature was performed on patient satisfaction after TKA. The search engines used were MedLine (PubMed) and the Cochrane Library. The keywords used were “TKA” and “satisfaction.” The time period searched included all available literature on the Internet up to January 16, 2020. Of the 1187 articles found (821 in PubMed, 366 in the Cochrane Library), 39 were selected and reviewed because they were especially focused on the topic (inclusion criteria). In other words I reviewed those articles on the subject that I found particularly important. Figure 1 shows our search strategies.
Figure 1.
Flow chart of our search strategy regarding patient satisfaction following total knee arthroplasty (TKA)
Results
In this article, the following issues relating to patient satisfaction after primary TKA will be reviewed: prevalence, factors contributing to patient satisfaction, differences between OA and rheumatoid arthritis (RA), satisfaction changes over time, predictors of patient satisfaction for the second TKA (6 weeks apart or more) in bilateral primary asynchronous TKA, and predictive models for satisfaction after primary TKA.
Prevalence
In 2017, Huang et al retrospectively analyzed 46 patients who experienced simultaneous bilateral TKA. They stated that up to 20% of Asian patients who underwent TKA reported dissatisfaction with the surgical result. Minimum duration of follow-up was 2 years, with an overall patient satisfaction rate of 91.3% (3). In a systematic review published by Gunaratne et al in 2017, approximately 20% of patients reported dissatisfaction following primary TKA (4).
In 2018, Alosh et al reviewed a consecutive series of primary TKAs carried out by a single surgeon with a minimum 2-year follow-up (5). They analyzed 151 TKAs with a minimum 2.3 years’ follow-up. Eleven (7.28%) were not satisfied, 9 (5.96%) were satisfied, with minor objections, and 131 (86.75%) were fully satisfied after TKA. In a retrospective cohort of 2589 patients who had undergone a primary TKA, at 1 year, Walker at al found 1740 (67.5%) patients very satisfied, 572 (22.2%) satisfied, 190 (7.4%) dissatisfied, and 76 (2.9%) very dissatisfied (6).
Factors contributing to patient satisfaction
There are a number of preoperative, perioperative, and postoperative factors contributing to patient satisfaction.
Preoperative factors
According to the systematic review of Gunaratne et al, patient expectation before surgery is the principal preoperative factor of patient dissatisfaction (4). They searched six literature databases published between 2005 and 1 January 2016. In a study of 3069 TKAs, the most important preoperative factors for dissatisfaction were female sex and lesser improvement in knee flexion (3).
Alosh et al found that the augmenting size of patellar and lateral compartment osteophytes, specifically, greater than 5 mm, was significantly associated with amelioration in Knee Society Score (KSS). Patient satisfaction was also clearly associated with these parameters and seemed independent of mechanical axis alignment (5).
In the study by Hasegawa et al, patient satisfaction after TKA correlated negatively with old age (7). They analyzed 109 patients (130 knees) with knee osteoarthritis who experienced primary TKA with navigation. However, Lange et al found that satisfaction with TKA was 86% among younger patients and 91% among older patients. Distribution of satisfaction answers was shifted toward greater satisfaction in older patients (8). Patient-reported outcomes were recorded before surgery and 2 years after surgery.
According to Clement et al, overall satisfaction was influenced by diabetes, depression, back pain, and short form 12 (SF-12) physical and mental components (9, 10). A retrospective cohort of 2521 patients undergoing a primary unilateral TKA were identified from an established regional arthroplasty database. Walker et al had encountered that patients with lung disease, diabetes, gastric ulcer, kidney disease, liver disease, depression, back pain, and those with poorer preoperative functional scores [WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) and SF-12] had a significantly lower level of satisfaction (6, 11). A retrospective cohort consisting of 2589 patients undergoing a primary TKA were identified from an established arthroplasty database.
In 2019, in a prospective cohort study, Gautreau et al reported that the use of a TKA communication checklist augmented patient satisfaction. In this study, 60 patients had received the checklist in TKA appointments with orthopedic surgeons between 6 weeks and 6 months postoperatively, and their satisfaction ratings were compared with 67 patients who had received the standard of care communication (12).
Halawi et al performed a satisfaction survey. They analyzed 551 patients undergoing TKAs and total hip arthroplasties with a minimum of 1-year follow-up, who responded to a satisfaction survey. Hispanic race was found to be the most significant predictor of dissatisfaction (13). A study by Deakin et al showed a clear correlation between achievement of preoperative expectancies and patient satisfaction after TKA (14). It was a prospective analysis of 200 patients.
In the study by Felix et al they analyzed a German prospective cohort study. They found that 61% of the patients reported satisfactory outcomes; patients were mainly satisfied with the results if postoperative WOMAC was ≥82.49 and the postoperative EuroQol 5-dimension visual analog scale (EQ-5D VAS) was ≥75. In particular, patients with high absolute preoperative patient related outcome (PRO) scores were more likely to remain dissatisfied (15).
Liebensteiner et al found that patient satisfaction after TKA was better in patients with preoperative complete joint space collapse. Patients with preoperative complete joint space collapse (0- to 1-mm minimal joint space width - mJSW) attained a significantly better WOMAC result from TKA than did those with an mJSW equal to or greater than 2 mm. From these findings, it was advised that “complete joint space collapse” could especially be used as an indication for TKA (16). It was a retrospective comparative analysis.
Johnson et al, in a randomized study, compared 3 education methods in the informed consent and their association with patient satisfaction (17). No difference in satisfaction with the consent process between the 3 groups was found; 92%–97% of the patients considered the consent process as good to excellent. Satisfaction was not influenced by reinforcement approaches, such as video or nurse education; they might hence not be necessary (17).
According to Jain et al (prospective multicenter study), greater patient expectations anticipate greater PROs, but not satisfaction, in TKA patients (18). Higher Hospital for Special Surgery Knee Replacement Fulfillment of Expectations Survey scores predicted greater satisfaction at 6 months and 1 year. In TKA patients, preoperative expectations were not affected by patient demographics or preoperative function. Greater preoperative expectations anticipated higher postoperative amelioration in PROs and accomplishment of expectations. The findings of this paper emphasized the significance of preoperative patient expectations on postoperative results. Table 1 summarizes the main preoperative factors contributing to patient satisfaction.
Table 1.
Preoperative factors contributing to patient satisfaction positively (+) or negatively (-).
| AUTHORS | YEAR | PREOPERATIVE FACTORS |
|---|---|---|
| Gunaratne et al (4) | 2017 | Excessive patient expectations prior to surgery (-) |
| Huang et al (3) | 2017 | Female sex (-) |
| Huang et al (3) | 2017 | Better knee flexion (-) |
| Alosh et al (5) | 2018 | Increasing size of patella and lateral compartment osteophytes, particularly greater than 5 mm (+) |
| Hasegawa et al (7) | 2018 | Old age (-) |
| Lange et al (8) | 2018 | Old age (+) |
| Clement et al (10) | 2018 | Diabetes, depression, back pain, SF-12 physical and mental components (-) |
| Walker et al (6) | 2018 | Lung disease, diabetes, gastric ulcer, kidney disease, liver disease, depression, back pain, with worse pre-operative functional scores (WOMAC and SF-12) (-) |
| Gautreau et al (12) | 2019 | TKA communication checklist (+) |
| Halawi et al (13) | 2019 | Hispanic race (-) |
| Deakin et al (14) | 2019 | Fulfilment of preoperative expectations (+) |
| Felix et al (15) | 2019 | High absolute preoperative PRO scores (-) |
| Liebensteiner et al (16) | 2019 | Preoperative complete joint space collapse (+) |
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; SF-12 = Short-form 12; PRO = patient related outcome
Perioperative factors
In simultaneous bilateral TKA Huang et al evaluated whether patients have different satisfaction levels between the first and second knee in the early stage after simultaneous bilateral TKA. They found that there was better patient satisfaction with the second knee in the early stage (first, third, and seventh postoperative days) (3).
In a case series, Tsukiyama et al found that medial rather than lateral knee instability correlated with lower patient satisfaction. Knee laxity was measured with postoperative stress X-rays in flexion and extension, and patient satisfaction and knee function were assessed by the 2011 Knee Society Knee Scoring System. The scores for satisfaction were significantly better in medially tight than in medially loose knees (19). In computer-assisted TKA (case series), Hasegawa et al had found that midflexion instability was associated with poorer expectations and satisfaction (7). In 2018, Azukizawa (case series) had reported that excessive intraoperative medial joint laxity of ≥4 mm at 90° flexion progressively decreased patient satisfaction for 1 year (20).
In a case series of cruciate-retaining TKA, postoperative medial stability had an important positive influence over patient satisfaction at 1 year (21). In a prospective, single-arm audit, Agarwala et al stated that concealed cosmetic closure was an efficacious method for skin closure in TKA, producing superior cosmetic healing with minimal complications, leading to ameliorated long-term patient satisfaction (22). Meanwhile, in a prospective trial Sundaram et al reported that skin closure with 2-octyl cyanoacrylate and polyester mesh after primary TKA offered better cosmetic results and patient satisfaction than skin closure with staples (23).
In a prospective multicenter investigation by Khlopas et al, at 4 to 6 weeks postoperatively, patients who had undergone robotic-arm-assisted TKA were found to have a greater satisfaction score than those who had undergone manual TKA (24). In 2019, Reimann et al compared patient-specific implants (PSIs) and conventional TKA. The PSI TKA achieved higher global patient satisfaction (25).
In a case series, a significant improvement in patient satisfaction was shown by Smith et al when they compared robotic-assisted TKA with TKA using conventional manual jig-based instruments (26). In 2020, Galea et al found that anterior (vs neutral or posterior) tibial component slope, greater femoral component valgus angle, less severe OA, and lower preoperative health state were related to inferior levels of satisfaction (27). Data were sourced from 2 prospective international, multicenter studies. In a randomized clinical trial, local infiltration analgesia has been demonstrated to be an efficacious technique for pain mitigation and patient satisfaction in the early postoperative period after TKA (28).
In a case series, Hitt et al found that the use of a flexible intramedullary rod influenced patient satisfaction and femoral size in TKA (29). Those patients who had undergone TKA using a flexible IM rod had better ameliorations in their PROs and diminished risk of oversizing the femoral component. The use of such a rod was not detrimental to outcomes and could have a positive effect on results. Table 2 summarizes the main perioperative factors contributing to patient satisfaction.
Table 2.
Perioperative factors contributing to patient satisfaction positively (+) or negatively (-)
| AUTHORS | YEAR | PERIOPERATIVE FACTORS |
|---|---|---|
| Moghtadaei et al (28) | 2013 | Local infiltration analgesia (+) |
| Hitt et al (29) | 2015 | Use of a flexible intramedullary rod (+) |
| Huang et al (3) | 2017 | First-side TKA in simultaneous bilateral TKA (-) |
| Tsukiyama et al (19) | 2017 | Medial rather than lateral joint laxity (-) |
| Hasegawa et al (7) | 2018 | Midflexion instability (-) |
| Azukizawa et al (20) | 2018 | Excessive intraoperative medial joint laxity of ≥4 mm at 90° flexion (-) |
| Kamenaga et al (21) | 2018 | Medial stability and lateral laxity (-) |
| Agarwala et al (22) | 2019 | Concealed cosmetic closure (+) |
| Khlopas et al (24) | 2019 | Robotic-arm-assisted TKA (+) |
| Reimann et al (25) | 2019 | Patient-specific implants (+) |
| Sundaram et al (23) | 2019 | Skin closure with 2-octyl cyanoacrylate and polyester mesh (+) |
| Smith et al (26) | 2019 | Robotic-assisted TKA (+) |
| Galea et al (27) | 2020 | Anterior (vs neutral or posterior) tibial component slope, greater femoral component valgus angle, less severe OA, and lower preoperative health state (-) |
TKA = Total knee arthroplasty; OA = Osteoarthritis
Postoperative factors
In 2017, in a regional registry study Shannak et al reported that the principal reason for continued dissatisfaction was persistent pain (30). According to Kamenaga et al, postoperative knee stability and soft-tissue balance affected patient satisfaction after cruciate-retaining TKA (21). In 2018, in a case series Van Onsem et al observed that ameliorated walking distance and range of motion (ROM) foretell patient satisfaction after TKA. In their study, male patients improved on the 6-min walk test by 50 m or more and had an augmented ROM of 5° or more, compared with the preoperative situation, and were 6–8 times more likely to be satisfied after TKA (31).
Walker et al observed that patients with less improvement in the WOMAC and SF-12 scores had a significantly inferior level of satisfaction (6). In 2018, in a retrospective cohort Bryan et al had stated that the patient will be less satisfied if the TKA does not produce ameliorations in pain and physical health (32). According to Halawi et al (satisfaction survey), the most common reasons for dissatisfaction after TKA were unceasing pain (41%), functional limitation (26%), surgical adverse event and reoperation (17%), staff or quality of care issues (11%), and unmet expectations (4%) (13). In 2019, in a retrospective study Clement et al reported that augmented symptoms of stiffness 1 year after TKA were related to an inferior rate of patient satisfaction (33).
In a randomized controlled trial Moffet et al compared the degree of patient satisfaction following in-home telerehabilitation after TKA with that of patients following a usual face-to-face home visit rehabilitation (34). The satisfaction degree of both groups was similar and was very high (over 85%). Satisfaction was rather found to be associated with walking and stair-climbing ability. Moffet et al firmly supported the use of telerehabilitation to ameliorate access to rehabilitation services and effectiveness of service delivery after TKA. Table 3 summarizes the main postoperative factors contributing to patient satisfaction.
Table 3.
Postoperative factors contributing to patient satisfaction positively (+) or negatively (-)
| AUTHORS | YEAR | POSTOPERATIVE FACTORS |
|---|---|---|
| Shannak et al (30) | 2017 | Persistent pain (-) |
| Kamenaga et al (21) | 2018 | Poor postoperative knee stability and soft-tissue balance (-) |
| Van Onsem et al (31) | 2018 | Improved walking distance and range of motion (+) |
| Walker et al (6) | 2018 | Poor improvement in WOMAC and SF-12 (-) |
| Bryan et al (32) | 2018 | Improvements in pain, mental health, and physical health from 6 to 12 months, predicted improvements in satisfaction (+). |
| Halawi et al (13) | 2019 | Persistent pain, functional limitation, surgical complication and reoperation, staff or quality of care issues, and unmet expectations (-) |
| Clement et al (33) | 2019 | Increased stiffness (-) |
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; SF-12 = Short-form 12
In a case series Kobayashi et al showed that patient satisfaction was better but functional activity was lower in RA than in OA (35). In a regional registry study Shannak et al found that patient satisfaction after TKA changed over a period of 5 to 20 years. The main conclusion was that half of the patients who stated that they were not satisfied with their TKA at 1 year went on to be satisfied with their knee (30). In 2020, Galea et al found that patients with anterior tibial component slope improved in satisfaction level over time (27). In a prospective randomized study Lützner et al stated that fulfillment of expectations influences patient satisfaction 5 years after TKA (36).
Clement et al had analyzed a retrospective cohort of 454 patients undergoing an asynchronous (6 weeks apart or more) bilateral primary TKA. They had observed that amelioration of pain and function was less with the second TKA, but the rate of satisfaction remained much the same. Patients who were dissatisfied with their first TKA were more likely to be dissatisfied with their second TKA (37).
Predictive models for satisfaction after primary TKA
Tools designed to predict patient satisfaction following TKA have the potential to guide patient selection.
In 2019, in a case series Kunze et al internally validated a predictive model for postoperative patient satisfaction after TKA analyzing 484 TKAs. This knee survey showed a 97.5% sensitivity and 95.7% negative predictive value in identifying at-risk patients for postoperative dissatisfaction after primary TKA (38).
Zabawa et al aimed to validate a model that predicts patient satisfaction following TKA. Phone surveys were administered to 203 patients who underwent TKA. The satisfaction in their study was 65%. Comparing satisfied and dissatisfied groups, there was a significant difference with respect to pain before TKA and body mass index (39).
Calkins et al aimed to determine the external validity of a prediction model for patient satisfaction (PMPS), with the hypothesis that it would achieve similar predictive success in their study group. They found that their prediction model was incapable to anticipate patient satisfaction after TKA (1).
Discussion
TKA is one of the most frequently performed surgeries in the world. The vast majority of patients profit from primary TKA by experiencing diminished knee pain, ameliorated function, and augmented quality of life. In spite of these fact-based ameliorations, a high dissatisfaction rate after TKA has been reported (15%–25% of patients); however, other studies have stated that the rate of patients satisfied following primary TKA ranges from 85% to 90%.
A number of preoperative, perioperative, and postoperative factors contribute to patient satisfaction. The capacity to recognize patients at risk for dissatisfaction would be valuable to counsel, educate, and potentially diminish the overall rate of dissatisfied patients. Tools (predictive models) intended to anticipate patient satisfaction following TKA have the potential to guide patient selection. Nonetheless, further research is required to develop a simple, but robust questionnaire that consistently foretells patient satisfaction after primary TKA.
Funding:
This paper was not funded.
Declaration of interest:
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
References
- 1.Calkins TE, Culvern C, Nahhas CR, Della Valle CJ, Gerlinger TL, Levine BR, et al. External validity of a new prediction model for patient satisfaction after total knee arthroplasty. J Arthroplasty. 2019;34(8):1677–81. doi: 10.1016/j.arth.2019.04.021. [DOI] [PubMed] [Google Scholar]
- 2.Bierke S, Häner M, Karpinski K, Hees T, Petersen W. Midterm effect of mental factors on pain, function, and patient satisfaction 5 years after uncomplicated total knee arthroplasty. J Arthroplasty. 2020;35(1):105–11. doi: 10.1016/j.arth.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Huang Y, Lee M, Chong HC, Ning Y, Lo NN, Yeo SJ. Reasons and factors behind post-total knee arthroplasty dissatisfaction in an Asian population. Ann Acad Med Singapore. 2017;46(8):303–9. [PubMed] [Google Scholar]
- 4.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: A systematic review of the literature. J Arthroplasty. 2017;32(12):3854–60. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Alosh H, Behery OA, Levine BR. Radiographic predictors of patient satisfaction following primary total knee arthroplasty. Bull Hosp Jt Dis (2013). 2018;76(2):105–11. [PubMed] [Google Scholar]
- 6.Walker LC, Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, et al. The WOMAC score can be reliably used to classify patient satisfaction after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3333–41. doi: 10.1007/s00167-018-4879-5. [DOI] [PubMed] [Google Scholar]
- 7.Hasegawa M, Naito Y, Yamaguchi T, Wakabayashi H, Sudo A. Factors contributing to patient satisfaction and expectations following computer-assisted total Knee arthroplasty. J Knee Surg. 2018;31(5):448–52. doi: 10.1055/s-0037-1604144. [DOI] [PubMed] [Google Scholar]
- 8.Lange JK, Lee YY, Spiro SK, Haas SB. Satisfaction rates and quality of life changes following total knee arthroplasty in age-differentiated cohorts. J Arthroplasty. 2018;33(5):1373–8. doi: 10.1016/j.arth.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 9.Ware J Jr, Kosinski M, Keller S D. A 12-Item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. The rate and predictors of patient satisfaction after total knee arthroplasty are influenced by the focus of the question: a standard satisfaction question is required. Bone Joint J. 2018;100-B(6):740–8. doi: 10.1302/0301-620X.100B6.BJJ-2017-1292.R1. [DOI] [PubMed] [Google Scholar]
- 11.American College of Rheumatology. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [(accessed 12 July 2013)]. http://www.rheumatology.org/practice/clinical/clinicianresearchers/outcomes-instrumentation/WOMAC.asp.
- 12.Gautreau SJ, Gould ON, Allanach WW, Clark AE, Massoeurs SJ, Forsythe ME. Total knee arthroplasty communication checklist increases patient satis-faction. J Arthroplasty. 2019;34(3):456–61. doi: 10.1016/j.arth.2018.11.032. [DOI] [PubMed] [Google Scholar]
- 13.Halawi MJ, Jongbloed W, Baron S, Savoy L, Williams VJ, Cote MP. Patient dissatisfaction after primary total joint arthroplasty: The patient perspective. J Arthroplasty. 2019;34(6):1093–6. doi: 10.1016/j.arth.2019.01.075. [DOI] [PubMed] [Google Scholar]
- 14.Deakin AH, Smith MA, Wallace DT, Smith EJ, Sarungi M. Fulfilment of preoperative expectations and postoperative patient satisfaction after total knee replacement A prospective analysis of 200 patients. The Knee. 2019;26(6):1403–12. doi: 10.1016/j.knee.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Felix J, Becker C, Vogl M, Buschner P, Plötz W, Leidl R. Patient characteristics and valuation changes impact quality of life and satisfaction in total knee arthroplasty - results from a German prospective cohort study. Health Qual Life Outcomes. 2019;17(1):180. doi: 10.1186/s12955-019-1237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liebensteiner M, Wurm A, Gamper D, Oberaigner W, Dammerer D, Krismer M. Patient satisfaction after total knee arthroplasty is better in patients with preoperative complete joint space collapse. Int Orthop. 2019;43(8):1841–7. doi: 10.1007/s00264-018-4185-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson MR, Singh JA, Stewart T, Gioe TJ. Patient understanding and satisfaction in informed consent for total knee arthroplasty: A randomized study. Arthritis Care & Research. 2011;63(7):1048–54. doi: 10.1002/acr.20475. [DOI] [PubMed] [Google Scholar]
- 18.Jain D, Nguyen LCL, Bendich I, Nguyen LL, Lewis CG, Huddleston JI, et al. Higher patient expectations predict higher patient-reported outcomes, but not satisfaction, in total knee arthroplasty patients: A prospective multicenter study. J Arthroplasty. 2017;32(9S):S166–S170. doi: 10.1016/j.arth.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 19.Tsukiyama H, Kuriyama S, Kobayashi M, Nakamura S, Furu M, Ito H, et al. Medial rather than lateral knee instability correlates with inferior patient satisfaction and knee function after total knee arthroplasty. Knee. 2017;24(6):1478–84. doi: 10.1016/j.knee.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y, Furu M et al. Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg. 2018;138(8):1143–50. doi: 10.1007/s00402-018-2965-2. [DOI] [PubMed] [Google Scholar]
- 21.Kamenaga T, Muratsu H, Kanda Y, Miya H, Kuroda R, Matsumoto T. The influence of postoperative knee stability on patient satisfaction in cruciate-retaining total knee arthroplasty. J Arthroplasty. 2018;33(8):2475–9. doi: 10.1016/j.arth.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Agarwala S, Vijayvargiya M. Concealed cosmetic closure in total knee replacement surgery - A prospective audit assessing appearance and patient satisfaction. J Clin Orthop Trauma. 2019;10(1):111–6. doi: 10.1016/j.jcot.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sundaram K, Piuzzi NS, Patterson BM, Stearns KL, Krebs VE, Mont MA. Skin closure with 2-octyl cyanoacrylate and polyester mesh after primary total knee arthroplasty offers superior cosmetic outcomes and patient satisfaction compared to staples: a prospective trial. European Journal of Orthopaedic Surgery & Traumatology. 2020;30(3):447–53. doi: 10.1007/s00590-019-02591-4. [DOI] [PubMed] [Google Scholar]
- 24.Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T, et al. Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. The journal of knee surgery. 2020;33(07):685–90. doi: 10.1055/s-0039-1684014. [DOI] [PubMed] [Google Scholar]
- 25.Reimann P, Brucker M, Arbab D, Lüring C. Patient satisfaction - A comparison between patient-specific implants and conventional total knee arthroplasty. J Orthop. 2019;16(3):273–7. doi: 10.1016/j.jor.2019.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith AF, Eccles CJ, Bhimani SJ, Denehy KM, Bhimani RB, Smith LS, et al. Improved patient satisfaction following robotic-assisted Total knee Arthroplasty. The journal of knee surgery. 2019 doi: 10.1055/s-0039-1700837. [DOI] [PubMed] [Google Scholar]
- 27.Galea VP, Rojanasopondist P, Connelly JW, Bragdon CR, Huddleston JI 3rd, Ingelsrud LH, et al. Changes in patient satisfaction following total joint arthroplasty. J Arthroplasty. 2020;35(1):32–8. doi: 10.1016/j.arth.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Moghtadaei M, Farahini H, Faiz SH, Mokarami F, Safari S. Pain management for total knee arthroplasty: single-injection femoral nerve block versus local infiltration analgesia. Iran Red Crescent Med J. 2014;16(1):e13247. doi: 10.5812/ircmj.13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hitt KD, Pierce TP, Jauregui JJ, Cherian JJ, Elmallah RD, Leibowitz E, et al. Use of a flexible intramedullary rod and its influence on patient satisfaction and femoral size in total knee arthroplasty. J Long Term Eff Med Implants. 2015;25(3):201–8. doi: 10.1615/jlongtermeffmedimplants.2015013275. [DOI] [PubMed] [Google Scholar]
- 30.Shannak O, Palan J, Esler C. A regional registry study of 216 patients investigating if patient satisfaction after total knee arthroplasty changes over a time period of five to 20 years. Knee. 2017;24(4):824–8. doi: 10.1016/j.knee.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Van Onsem S, Verstraete M, Dhont S, Zwaenepoel B, Van Der Straeten C, Victor J. Improved walking distance and range of motion predict patient satisfaction after TKA. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3272–9. doi: 10.1007/s00167-018-4856-z. [DOI] [PubMed] [Google Scholar]
- 32.Bryan S, Goldsmith LJ, Davis JC, Hejazi S, MacDonald V, McAllister P, et al. Revisiting patient satisfaction following total knee arthroplasty: A longitudinal observational study. BMC Musculoskelet Disord. 2018;19(1):423. doi: 10.1186/s12891-018-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clement ND, Bardgett M, Weir D, Holland J, Deehan DJ. Increased symptoms of stiffness 1 year after total knee arthroplasty are associated with a worse functional outcome and lower rate of patient satisfaction. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1196–1203. doi: 10.1007/s00167-018-4979-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, et al. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: Results from a randomized controlled trial. Telemed J E Health. 2017;23(3):80–7. doi: 10.1089/tmj.2016.0060. [DOI] [PubMed] [Google Scholar]
- 35.Kobayashi S, Niki Y, Harato K, Nagura T, Nakamura M, Matsumoto M. Rheumatoid arthritis patients achieve better satisfaction but lower functional activities as compared to osteoarthritis patients after total knee arthroplasty. J Arthroplasty. 2019;34(3):478–482. doi: 10.1016/j.arth.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 36.Lützner C, Postler A, Beyer F, Kirschner S, Lützner J. Fulfillment of expectations influence patient satisfaction 5 years after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2061–70. doi: 10.1007/s00167-018-5320-9. [DOI] [PubMed] [Google Scholar]
- 37.Clement ND, Merrie KL, Weir DJ, Holland JP, Deehan DJ. Asynchronous bilateral total knee arthroplasty: Predictors of the functional outcome and patient satisfaction for the second knee replacement. J Arthroplasty. 2019;34(12):2950–6. doi: 10.1016/j.arth.2019.06.056. [DOI] [PubMed] [Google Scholar]
- 38.Kunze KN, Akram F, Fuller BC, Zabawa L, Sporer SM, Levine BR. Internal validation of a predictive model for satisfaction after primary total knee arthroplasty. J Arthroplasty. 2019;34(4):663–70. doi: 10.1016/j.arth.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 39.Zabawa L, Li K, Chmell S. Patient dissatisfaction following total knee arthroplasty: External validation of a new prediction model. Eur J Orthop Surg Traumatol. 2019;29(4):861–7. doi: 10.1007/s00590-019-02375-w. [DOI] [PubMed] [Google Scholar]