Abstract
Context
Return to play after sport-related concussion (SRC) requires authorized clearance from a health care provider (HCP). The variability in HCPs and facilities where athletes seek care may influence return time.
Objective
To identify the initial examiner, HCPs who authorize clearance to return to play, and medical facilities that authorize clearance to return to play for high school student-athletes after SRC and compare authorized clearance time by HCPs and medical facilities.
Design
Prospective cohort study.
Setting
High school.
Patients or Other Participants
Student-athletes (n = 16 001) with SRC participating in athletics sponsored by the Michigan High School Athletic Association.
Main Outcome Measure(s)
Frequencies of initial examiner and authorized clearance for each HCP (doctor of osteopathic medicine, medical doctor, nurse practitioner, physician assistant) and medical facility (neurologist's office; team physician, primary care physician or pediatrician's office [PCP]; hospital; urgent/ready care) for each case of SRC. We calculated Kaplan-Meier curves and Peto tests to evaluate differences in the median time to authorized clearance between HCPs and facilities. Only cases with a date on which clearance to return to play was authorized (80.3%; n = 12 856) were included in the authorized clearance and time-to-return analyses.
Results
An athletic trainer was at least 1 of the initial examiners in 71.3% (n = 11 404) of SRC cases; 81.2% (n = 12 990) had only 1 initial examiner. We observed an association between the initial examiner and the medical facility providing clearance for athletic director (χ2 = 52.6, P < .001, V = .06), athletic trainer (χ2 = 172.0, P < .001, V = .12), coach (χ2 = 161.5, P < .001, V = .11), doctor of osteopathic medicine (χ2 = 59.4, P < .001, V = .07), and nurse practitioner (χ2 = 10.0, P = .04, V = .12). Clearance was authorized most frequently by a medical doctor (63.9%, n = 8218) and at a PCP (70.8%, n = 9099). Median (interquartile range) time to authorized clearance varied by facility (urgent/ready care = 7 days [4–11 days], hospital = 9 days [6–14 days], PCP = 10 days [6–14 days], team physician = 12 days [8–16 days], neurologist's office = 13 days [9–20 days]; P < .001). An athletic trainer was the initial examiner more often for males (74.1%) than for females (65.8%). The medical facility where clearance to return to play was authorized also differed between males (PCP = 69.3%, team physician = 11.3%, neurologist's office = 8.4%) and females (PCP = 73.6%, team physician = 8.5%, neurologist's office = 8.3%).
Conclusions
Clearance to return to play after SRC was frequently provided by a medical doctor and at a PCP. The median time to return to unrestricted participation after SRC varied by HCP and medical facility. Future researchers should elucidate the reasons for these differences and determine why athletes seek care at different types of medical facilities.
Keywords: head injuries, recovery, sports, health disparity
Key Points
The initial examiner for most high school student-athletes with sport-related concussion was an athletic trainer, followed by a coach.
Approximately 20% of patients had >1 initial examiner.
The median time to authorized clearance for return to play after sport-related concussion differed by the type of medical facility.
Male athletes had an athletic trainer as an initial examiner more often than did female athletes.
Differences in the medical facility that provided clearance existed between sexes.
Sport-related concussion (SRC) is a growing health concern, particularly in younger, at-risk athletic populations. Researchers1 estimated that between 1.1 and 1.9 million sport- and recreation-related concussions occur annually in youth younger than 19 years. Currently, all states and the District of Columbia have enacted youth concussion laws. However, these laws vary in the credential requirements of the health care providers (HCPs) authorized to clear a concussed athlete to return to unrestricted activity and do not specify which medical facilities may provide clearance. Moreover, with the advances in SRC diagnosis and return-to-play (RTP) guidelines and continuous updates to consensus and position statements on concussion, RTP decisions may be a daunting responsibility for many HCPs.
The HCPs who care for athletes with SRC and authorize clearance to RTP should ensure that their decisions are guided by best practices. Current consensus and position statements2,3 suggested that concussed athletes should complete a stepwise progression before returning to participation. It is also recommended that athletes first have an initial period (24–48 hours) of relative physical and cognitive rest and progress through stages of symptom-limited activity, light aerobic exercise, sport-specific exercise, and noncontact training, with at least 24 hours between steps. After the athletes are asymptomatic and cleared by an HCP, they can continue to full practice and competition.2 However, guidelines differ as to which HCP should make the RTP decision. Valovich McLeod et al4 reported that an athletic trainer (AT) was the primary decision maker for 69.2% of concussed athletes, followed by other physician (17.3%) and team physician (8.9%); yet these data were collected before states enacted laws regarding the management of concussions in athletes. Currently, in some states, ATs are not included as HCPs responsible for authorizing medical clearance. For example, in Michigan, only medical doctors (MDs), doctors of osteopathic medicine (DOs), physician assistants (PAs), and nurse practitioners (NPs) are allowed to clear an athlete with SRC to participate in a sanctioned Michigan High School Athletic Association (MHSAA) sport or activity. Therefore, it is important to determine which HCP is making RTP decisions in Michigan, as ATs are not an option.
Although physicians can clear athletes to RTP after they sustain concussions, parents or guardians are usually responsible for bringing their children to the physician. Researchers5 have found that parents have inconsistent views on which physician or medical facility should care for their concussed children. For example, Zamarripa et al5 noted that 44% of parents would call or go to their children's regular care provider (ie, pediatrician or primary care physician [PCP]) and 42% would seek immediate care at a hospital emergency department (ED). Approximately two-thirds of parents who took their concussed children to an ED expected to be told whether their children had a concussion, 68% definitely expected to be told how long to keep the children out of school or activities, and half expected the ED physician to sign a return-to-activity form for physical education or sports.5
Despite parents' expectations of care provided to their children with SRCs by an ED physician,5 HCPs in these settings may not have the training or resources to manage the patient according to best practices, yielding variability in concussion clinical care practice.6 Stern et al6 observed that approximately one-third of ED physicians did not use any formal clinical guidelines for concussion assessment, whereas 57% of physicians used neuroimaging to guide their clinical decision, despite numerous consensus and position statements indicating the absence of structural damage during concussion diagnosis.2,3 Furthermore, only 32% of ED physicians recommended a gradual or stepwise return to participation.6 This lack of gradual or stepwise return to participation may influence the recovery time or place athletes at further risk for injury. In addition, although they regularly care for concussed patients, pediatric primary care and emergency medicine providers may not have adequate training or infrastructure to properly manage the patient.7 Lastly, when ATs and school nurses were asked about SRC management, they cited inconsistent care practices, including discordance between physician practice and regulation protocols, physicians clearing students prospectively with a note, other HCPs clearing students without documentation of physician oversight, and physicians providing premature medical clearance,8 which may reflect differences in where concussed athletes seek care.
In the past decade, emerging evidence has provided insight into recovery timelines after SRC, and improved education has aided recognition and management. Investigators have demonstrated that a typical recovery for pediatric athletes is <1 to 4 weeks9,10; however, for some, recovery requires >4 weeks.11 Physical and cognitive rest has been recommended,11 but strict rest may result in negative consequences and early exercise may improve recovery time.12–16 Furthermore, since 2015, recovery from SRC has been shown to be influenced by immediate removal from sport6,17–19 and academic accommodations,11 both of which are management practices that may vary by HCP and medical facility. Therefore, it is critical to identify who is involved in acute care, which HCPs are authorizing clearance, and where clearance is authorized to determine if any differences in concussion management exist. As such, the primary purpose of our study was to identify the initial examiner for high school athletes with SRCs, the credentials of the HCPs who authorized clearance to RTP, and the medical facility where athletes obtained the medical clearance. The secondary purpose was to determine if the time for authorized clearance was the same for concussed athletes cleared by different medical providers and medical facilities. The tertiary purpose was to compare an AT as an initial examiner and the medical facility authorizing clearance between sexes.
METHODS
Research Design, Schools, and Participants
This was a prospective cohort design using data obtained from the MHSAA Head Injury Reporting System (HIRS). Data were collected during the 2015–2016 through 2018–2019 academic years and included students in 9th through 12th grades, with approximately 750 high schools participating each year. The MSHAA middle schools are not included in the HIRS; however, middle school–aged student-athletes participating in high school sports were included in the analyses. Requirements and deadlines for reporting participant and concussion data into the HIRS for all participating high schools in Michigan are reported in the current MHSAA concussion protocol.20 The MHSAA sanctions 28 sports.21 To date, data on 16 001 cases of SRC have been included in the HIRS (males: 65.5%, n = 10 483; females: 35.5%, n = 5518). The frequencies of student-athletes in each grade are shown in Table 1. The Institutional Review Board at Michigan State University determined that this study was exempt because of the use of deidentified data.
Table 1.
Characteristics of Student-Athletes With Sport-Related Concussions Recorded in the Head Injury Reporting System
| Characteristic |
No. (%) |
| Sex | |
| Male | 10 483 (65.5) |
| Female | 5518 (34.5) |
| Grade level | |
| Sixth–eightha | 166 (1.0) |
| Freshman | 4689 (29.3) |
| Sophomore | 4477 (28.0) |
| Junior | 3488 (21.8) |
| Senior | 3181 (19.9) |
| Concussion history? | |
| Yes | 2470 (15.4) |
| Initial examinerb | |
| Athletic director | 480 (3.0) |
| Athletic trainer | 11 404 (71.3) |
| Coach | 5673 (35.5) |
| Doctor of osteopathic medicine | 178 (1.1) |
| Medical doctor | 749 (4.7) |
| Nurse practitioner | 56 (0.4) |
| Physician assistant | 80 (0.5) |
| Sideline emergency personnel | 279 (1.7) |
| Other appropriate health care provider | 460 (2.9) |
| No. of initial examiners | |
| 1 | 12 990 (81.2) |
| 2 | 2716 (17.0) |
| ≥ 3 | 295 (1.8) |
Data from Michigan High School Athletic Association middle schools are not included in the Head Injury Reporting System. However, data from middle school–aged student-athletes participating in high school sports were included in the analyses.
Patients with sport-related concussion may have had >1 initial examiner, so the percentages do not total 100%.
Data Reporting and Definitions
Operational Definition of SRC
The SRCs recorded in the HIRS had to meet 3 criteria, which have been described in previous studies.22,23 An MD, DO, PA, or NP diagnosed all SRCs.
Initial Examiner
For each case of SRC, the HIRS includes the initial examiner(s) who recognized the SRC or to whom the suspected SRC was reported and who provided an initial assessment. The initial examiner options are athletic director, AT, coach, DO, MD, NP, PA, sideline emergency personnel, other appropriate HCP, or a combination of multiple examiners if > 1 initial examiner was reported.
Return-to-Play Clearance
According to the MHSAA, clearance must be unconditional and in writing. Return-to-play clearance is defined as an unrestricted return to full participation. Therefore, HCPs can only provide written authorized clearance if the concussed student-athlete is able to return to unrestricted activity.
Authorizing HCP
The MHSAA defines an authorizing HCP as an MD, DO, NP, or PA. These individuals are the only providers allowed to give written authorization for the player to return to unrestricted activity.
Medical Facility Providing Clearance
The medical facility providing clearance identifies where the concussed student-athlete obtained written authorized clearance to return to unrestricted activity. These facilities include hospital ED, neurologist's office, PCP's office, team physician, and urgent/ready care.
Procedures
Our data-collection procedures have been described in previous studies.22,23 Among the SRC injury event data that school personnel submit as part of an online report for each occurrence of SRC is the HCP or other professional providing the initial assessment, the authorizing HCP providing unrestricted written clearance, and the medical facility where clearance was authorized.
Statistical Analysis
We conducted descriptive statistics to describe frequencies, mean values, medians, and ranges. Chi-square analyses allowed us to determine if significant associations were present between the initial examiner and the medical facility providing clearance, between the authorizing HCP and the medical facility providing clearance, between sex and AT involvement as the initial examiner, and between sex and the medical facility providing clearance. The effect size was calculated using Cramér V and interpreted as small (0.1), medium (0.3), or large (0.5).24 We used Kaplan-Meier survival analyses, adjusted for concussion history and year of athletic season, to assess the median time (in days) between the date of the SRC and the date of authorized clearance to return to unrestricted activity. All survival times were truncated at 40 days, and cases of SRC were censored if the student-athlete obtained authorized clearance after the season ended. Peto tests enabled us to evaluate whether the median number of days to authorized clearance differed between the authorizing HCP and the medical facility. The statistical analysis was completed using Stata (version 16.0; StataCorp), and significance was set at P ≤ .05.
RESULTS
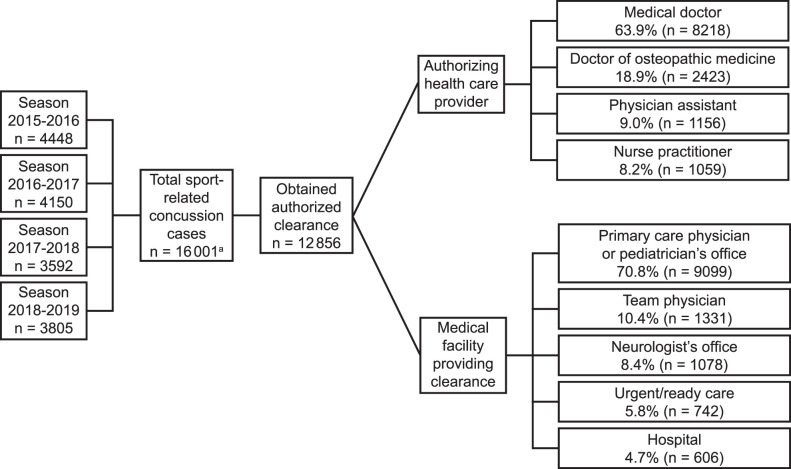
The accrued SRC cases are presented in Figure 1. A total of 16 001 SRCs occurred throughout the 4 athletic seasons. The characteristics of student-athletes with SRCs are shown in Table 1. The initial examiner was most often an AT (71.3%; n = 11 404/16 001) or a coach (35.5%; n = 5673/16 001). Each SRC could have had >1 initial examiner; however, for most SRC cases (81.2%; n = 12 990/16 001), only 1 initial examiner was involved. Authorized clearance to return to unrestricted activity was obtained in 80.3% (n = 12 856/16 001) of all SRC cases. Authorized clearance was most often obtained from an MD (63.9%; n = 8218/12 856) or DO (18.8%; n = 2423/12 856) and was typically sought at a PCP office (70.8%; n = 9099/12 856), followed by a team physician (10.4%; n = 1331/12 856) (Figure 1).
Figure 1.
Sport-related concussion cases recorded in the Head Injury Reporting System from the 2015–2016 through 2018–2019 athletic seasons. a Six cases either did not have a date of injury or contained an incorrect date.
We observed an association between the initial examiner and the medical facility providing clearance for athletic director (χ2 = 52.6, P < .001, V = .06), AT (χ2 = 172.0, P < .001, V = .12), coach (χ2 = 161.5, P < .001, V = .11), DO (χ2 = 59.4, P < .001, V = .07), sideline emergency personnel (χ2 = 37.9, P < .001, V = .05), NP (χ2 = 10.0, P = .03, V = .12), and other appropriate HCPs (χ2 = 35.6, P < .001, V = .05; Table 2). When an AT was involved in the initial examination, a greater proportion of student-athletes received authorized clearance from a team physician, and a smaller proportion was cleared at a PCP office than when an AT was not an initial examiner. The opposite occurred when a coach was involved in the initial examination, with a greater proportion of student-athletes receiving authorized clearance from a PCP office and a smaller proportion receiving clearance from a team physician than when a coach was not an initial examiner. We demonstrated an association between the authorized medical examiner and the medical facility providing authorized clearance (χ2 = 1400, P < .001, V = .19). A DO was most often an examiner at the PCP office (62.0%, n = 1503/2423) or the team physician (26.5%, n = 642/2423), an MD was most often a medical examiner at the PCP (71.2%, n = 5893/8218) or neurologist's office (11.4%; n = 937/8218), and an NP and a PA were most often examiners at the PCP office (NP: 78.6%, n = 832/1059; PA: 75.4%, n = 871/1156) and urgent/ready care (NP: 14.8%, n = 157/1059; PA: 13.5%, n = 156/1156; Table 3).
Table 2.
Association Between Initial Examiner and Medical Facility Providing Authorized Clearance (N = 12 856)a
| Initial Examiner |
Medical Facility Cleared,b No. (%) |
χ2 Statistic |
V Coefficient |
P Value |
||||
| Hospital |
Neurologist's Office |
Primary Care Physician or Pediatrician's Office |
Team Physician |
Urgent/Ready Care |
||||
| Athletic director | 52.6 | .06 | <.001 | |||||
| Yes (n = 372) | 38 (10.2) | 16 (4.3) | 283 (76.1) | 12 (3.2) | 23 (6.2) | |||
| No (n = 12 484) | 568 (4.6) | 1062 (8.5) | 8816 (70.6) | 1319 (10.6) | 719 (5.8) | |||
| Athletic trainer | 172.0 | .12 | <.001 | |||||
| Yes (n = 9230) | 386 (4.2) | 837 (9.1) | 6341 (68.7) | 1131 (12.3) | 535 (5.8) | |||
| No (n = 3626) | 220 (6.1) | 241 (6.7) | 2758 (76.1) | 200 (5.5) | 207 (5.7) | |||
| Coach | 161.5 | .11 | <.001 | |||||
| Yes (n = 4532) | 247 (5.5) | 288 (6.4) | 3439 (75.9) | 301 (6.6) | 257 (5.7) | |||
| No (n = 8324) | 359 (4.3) | 790 (9.5) | 5660 (68.0) | 1030 (12.4) | 485 (5.8) | |||
| Doctor of osteopathic medicine | 59.4 | .07 | <.001 | |||||
| Yes (n = 150) | 14 (9.3) | 6 (4.0) | 85 (56.7) | 41 (27.3) | 4 (2.7) | |||
| No (n = 12 706) | 592 (4.6) | 1072 (8.4) | 9014 (70.9) | 1290 (10.2) | 738 (5.8) | |||
| Medical doctor | 6.1 | .02 | .19 | |||||
| Yes (n = 594) | 32 (5.4) | 47 (7.9) | 414 (69.7) | 75 (12.6) | 26 (4.4) | |||
| No (n = 12 262) | 574 (4.7) | 1031 (8.4) | 8685 (70.8) | 1256 (10.2) | 716 (5.8) | |||
| Nurse practitioner | 10.0 | .03 | .04 | |||||
| Yes (n = 44) | 3 (6.8) | 1 (2.3) | 33 (75.0) | 1 (2.3) | 6 (13.6) | |||
| No (n = 12 812) | 603 (4.7) | 1077 (8.4) | 9066 (70.8) | 1330 (10.4) | 736 (5.7) | |||
| Physician assistant | 3.3 | .02 | .51 | |||||
| Yes (n = 67) | 6 (9.0) | 6 (9.0) | 44 (65.6) | 6 (9.0) | 5 (7.4) | |||
| No (n = 12 789) | 600 (4.7) | 1072 (8.4) | 9055 (70.8) | 1325 (10.4) | 737 (5.8) | |||
| Sideline emergency personnel | 37.9 | .05 | <.001 | |||||
| Yes (n = 203) | 24 (11.8) | 9 (4.4) | 154 (75.9) | 6 (2.9) | 10 (4.9) | |||
| No (n = 12 653) | 582 (4.6) | 1069 (8.5) | 8945 (70.7) | 1325 (10.5) | 732 (5.8) | |||
| Otherc | 35.6 | .05 | <.001 | |||||
| Yes (n = 327) | 35 (10.7) | 33 (10.1) | 224 (68.5) | 17 (5.2) | 18 (5.5) | |||
| No (n = 12 529) | 571 (4.6) | 1045 (8.3) | 8875 (70.8) | 1314 (10.5) | 724 (5.8) | |||
These data include all student-athletes with sport-related concussions who obtained authorization to return to unrestricted participation.
Percentages were rounded, so totals may not equal 100%.
Other indicates another appropriate health care provider.
Table 3.
Association Between Authorized Medical Examiner and Medical Facility Providing Authorized Clearance (N = 12 856)a
| Authorized Medical Examiner |
Medical Facility Cleared, No. (%)b |
χ2 Statistic |
V Coefficient |
P Value |
||||
| Hospital |
Neurologist's Office |
Primary Care Physician or Pediatrician's Office |
Team Physician |
Urgent/Ready Care |
||||
| Doctor of osteopathic medicine (n = 2423) | 100 (4.1) | 85 (3.5) | 1503 (62.0) | 642 (26.5) | 93 (3.8) | 1400 | .19 | <.001 |
| Medical doctor (n = 8218) | 417 (5.1) | 937 (11.4) | 5893 (71.2) | 635 (7.7) | 336 (4.1) | |||
| Nurse practitioner (n = 1059) | 42 (4.0) | 26 (2.5) | 832 (78.6) | 2 (0.2) | 157 (14.8) | |||
| Physician assistant (n = 1156) | 47 (4.1) | 30 (2.6) | 871 (75.4) | 52 (4.5) | 156 (13.5) | |||
These data include all student-athletes with sport-related concussion cases who obtained authorization to return to unrestricted participation.
Percentages were rounded, so totals may not equal 100%.
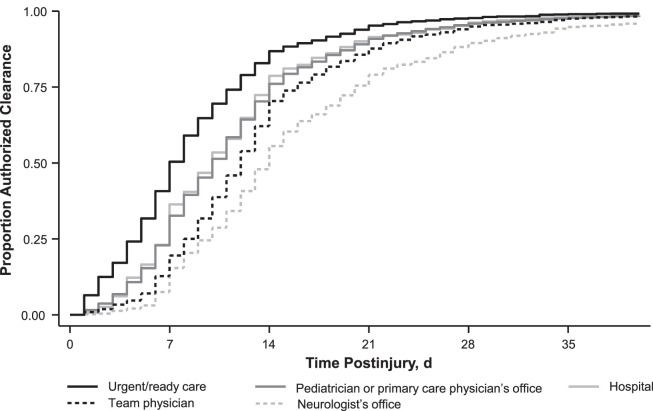
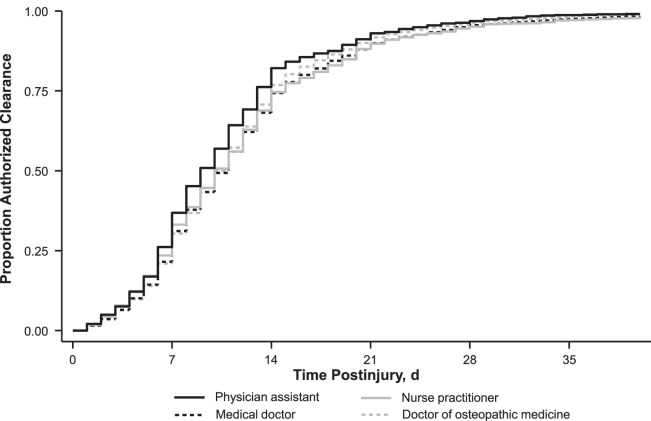
Overall, the median (interquartile range [IQR]) time between the date of injury and authorized clearance to return to unrestricted activity was 11 days (7–16 days). The median (IQR) time for authorized clearance by each medical facility was 7 days (4–11 days) for urgent/ready care, 9 days (6–14 days) for a hospital, 10 days (6–14 days) for a PCP, 12 days (8–16 days) for the team physician, and 13 days (9–20 days) for a neurologist's office (P < .001) when adjusting for concussion history and year of athletic season (Figure 2). The median (IQR) time for authorized clearance by each authorizing HCP was 9 days (5–13 days) for a PA, 10 days (6–14 days) for a DO, 10 days (6–14 days) for an MD, and 10 days (6–14 days) for an NP (P < .001) when adjusting for concussion history and year of athletic season (Figure 3).
Figure 2.
Time to authorized clearance by medical facility adjusted for concussion history and year of athletic season. Median (interquartile range) was 7 days (4–11 days) for urgent/ready care, 9 days (6–14 days) for hospital, 10 days (6–14 days) for primary care physician's or pediatrician's office, 12 days (8–16 days) for team physician, and 13 days (9–20 days) for neurologist's office.
Figure 3.
Time to authorized clearance by authorizing health care provider (HCP) adjusted for concussion history and year of season. Median (interquartile range) was 10 days (6–14 days) for medical doctor, 10 days (6–14 days) for doctor of osteopathic medicine, 9 days (5–13 days) for physician assistant, and 10 days (6–14 days) for nurse practitioner.
We observed differences in the initial examiner between sexes for SRC cases. The frequencies of each initial examiner stratified by sex for all SRC cases (n = 16 001) are provided in Table 4. A greater proportion of males (74.1%; n = 7772/10 483) had an AT as their initial examiner compared with females (65.8%; n = 3632/5518; χ2 = 122.2, P < .001, V = .08). In addition, for cases in which authorized clearance was obtained, we found an association between sex and the medical facility where the student-athlete was cleared (Table 5). A greater proportion of males (11.3%; n = 957/8459) than females (8.5%, n = 374/4397) received authorized clearance through a team physician, whereas a greater proportion of females (73.6%; n = 3235/4397) than males (69.3%; n = 5864/8459) received clearance from a PCP.
Table 4.
Initial Examiner for Sport-Related Concussion Stratified by Sex (N = 16 001), No. (%)a
| Initial Examinerb |
Males (n = 10 483) |
Females (n = 5518) |
| Athletic director | 317 (3.02) | 163 (2.95) |
| Athletic trainer | 7772 (74.14) | 3632 (65.82) |
| Coach | 3287 (31.36) | 2386 (43.24) |
| Doctor of osteopathic medicine | 150 (1.43) | 28 (0.51) |
| Medical doctor | 572 (5.46) | 177 (3.21) |
| Nurse practitioner | 41 (0.39) | 15 (0.27) |
| Physician assistant | 61 (0.58) | 19 (0.34) |
| Sideline emergency personnel | 232 (2.21) | 47 (0.85) |
| Other appropriate health care provider | 333 (3.18) | 127 (2.30) |
These data include all student-athletes with sport-related concussion included in the Head Injury Reporting System.
Sport-related concussion cases may have had >1 initial examiner, so percentages do not equal 100%.
Table 5.
Association Between Sex and Medical Facility Providing Authorized Clearance (N = 12 856)a
| Sex |
Medical Facility Cleared, No. (%) |
χ2 Statistic |
V Coefficient |
P Value |
||||
| Hospital |
Neurologist's Office |
Primary Care Physician or Pediatrician's Office |
Team Physician |
Urgent/Ready Care |
||||
| Male (n = 8459) | 417 (4.9) | 712 (8.4) | 5864 (69.3) | 957 (11.3) | 509 (6.0) | 34.4 | .05 | <.001 |
| Female (n = 4397) | 189 (4.3) | 366 (8.3) | 3235 (73.6) | 374 (8.5) | 233 (5.3) | |||
These data include all student-athletes with sport-related concussion cases who obtained authorization to return to unrestricted participation.
DISCUSSION
We sought to identify the personnel involved in the initial SRC examination and compare the time to authorized clearance to return to unrestricted activity between the HCP (DO, MD, NP, PA) and medical facilities authorizing clearance using the largest sample to date of SRC injury surveillance in the high school athletic setting. The MHSAA mandates that athletes obtain written authorized clearance before returning to full participation; however, athletes with an SRC seek care from a variety of medical providers and medical facilities. An AT was at least 1 of the initial examiners in 71% of SRC cases. We found that in 19.7% of SRC cases, athletes did not obtain authorized clearance to return, which may be because of many different factors (eg, end of the season, return occurred after the season, not given authorization to return, did not seek authorization, or quit sport) and warrants further exploration. Athletes most often obtained authorized clearance to return to unrestricted activity from a PCP. When comparing the time to authorized clearance, athletes obtained clearance a median of 5 or 6 days sooner from an urgent/ready care facility than from a team physician or neurologist's office, respectively. This difference may be perceived as small, yet for a student-athlete, it could be the difference between playing in a game versus sitting out. Furthermore, serious consequences (ie, subsequent concussion, prolonged recovery) may occur if student-athletes are returned too soon. These results may also be clinically useful in conversations between ATs and key stakeholders (ie, athletes, coaches, parents) to explain anticipated return outcomes, which vary among medical settings. Our findings may exemplify more conservative management practices based on medical facilities and, therefore, can be used to direct future research questions based on medical facility and provider RTP management practices.
As initial examiners, ATs play a major role in identifying and managing athletes with SRC. In a recent study of Wisconsin high schools, McGuine et al25 noted that AT availability was positively associated with the reported incidence of SRC and proper management practices, including the use of an RTP protocol. That being said, 34% of public and private high schools across the United States with athletic programs did not have access to athletic training services; in Michigan, 48% had no access.26 Our results indicated that 29% of SRC cases did not have an AT involved in the initial examination. Post et al27 reported that coaches (66.8%) were most often responsible for immediate medical care during practices, whereas ATs (57.9%) were most often responsible for immediate medical care during competitions, as ATs' presence at practices and competitions is variable. Appropriate medical coverage is often prioritized based on the risk involved in the sport, and some high school sports (eg, football, basketball, soccer, track) require more athletic training services than do others.28 This creates disparities in medical coverage for athletes who participate in other sports in an athletics program without access to athletic training services. In our sample, a greater proportion of males (74.1%) had an AT listed as an initial examiner than females (65.8%). These findings suggest a possible disparity in athletic training coverage for high school female athletes that may influence acute SRC management, referral, and where female athletes seek further care, warranting more study in this area. In addition, the clinical implications of these results provide a rationale for increasing AT access for all athletes, including female athletes, and ensuring that coaches are trained to properly identify and acutely manage SRCs in the absence of an AT because of their involvement in the initial evaluation of males (31.4%) and females (43.2%). Early access to appropriate medical care has been demonstrated to influence length of recovery from SRC29,30; therefore, future work should address disparities in AT coverage that may facilitate seeking proper care and management of SRC.
Identifying the personnel involved in the initial SRC examination is also important because these professionals may influence where a student-athlete goes to receive further medical care and obtain authorized clearance. In a study of RTP compliance, Haarbauer-Krupa et al31 found that high school students followed guidelines more consistently when their care was managed by an interdisciplinary team (ie, AT and physician). O'Keefe et al32 observed that athletes were more likely to present to a sports medicine clinic than an ED if they were initially examined by an AT. These results are consistent with ours, supporting the benefit of having an AT involved in the acute phase of SRC management, as an association was present between the initial examiner of the SRC and where the student-athlete ultimately sought authorized clearance to return to unrestricted activity; however, the effect sizes were small. Specifically, a greater percentage of student-athletes with an AT as an initial examiner obtained clearance from a team physician or neurologist's office, and a smaller percentage obtained clearance from a PCP compared with student-athletes without an AT involved in their initial examination. In contrast, a smaller percentage of student-athletes obtained clearance from a team physician if a coach or athletic director was an initial examiner than if a coach or athletic director was not the initial examiner. This could have a number of explanations. As an HCP, an AT is more qualified to ascertain the severity and specificity of concussion symptoms than is a coach or athletic director and, thus, may be able to refer a student-athlete to a more specialized care facility, such as a neurologist's office. Furthermore, if a coach or athletic director is the initial examiner, this may indicate a lack of sports medicine resources and access to athletic training services for that team and may suggest less collaboration with a sports medicine or team physician in SRC management. Although we did not have specific information regarding health care access in this study, further investigation of this factor in Michigan high schools is warranted.
We also noted a difference in the median time to clearance from a medical facility. Student-athletes with an SRC returned to unrestricted activity 5 or 6 days sooner if they obtained authorized clearance in an urgent/ready care facility compared with a team physician or neurologist's office, respectively. The median number of days for clearance authorized at an urgent/ready care was 7 days when adjusted for concussion history and year of academic season, whereas the time to authorized clearance increased with specialized care. Adherence to an RTP progression likely influences these differences in time to authorized clearance. Also, urgent/ready care facilities are often available for immediate access versus appointments being needed for more specialized care. However, if an athlete is progressing through an RTP progression as expected, appointments for clearance are probably made in a timely fashion. Wallace et al33 determined that 84% of ATs reported following a gradual stepwise progression during SRC management; the most commonly used RTP guidelines were the National Athletic Trainers' Association 2014 position statement and the International Conference on Concussion in Sport consensus statement.2,34,35 Wallace et al33 also stated that an interdisciplinary approach (eg, ATs and team physician or ATs and PCP) for final RTP decisions was used 28% of the time, and a PCP made the final RTP decisions alone 22% of the time. Yet in a recent report, Lempke et al34 identified team physicians (41.3%), ATs (37.1%), and PCP (14.5%) as the final decision makers, with ATs collaboratively involved in most decisions (93.8%). Importantly, the aforementioned studies involved ATs practicing in a variety of states and work settings, whereas the MHSAA requires clearance to be authorized by a DO, MD, NP, or PA.
Our results suggested that when student-athletes obtained clearance from an urgent/ready care facility, the gradual stepwise progression may have been accelerated, not monitored properly, or not incorporated, resulting in the earlier clearance time. The SRC management practices among other HCPs in these settings are discouraging, as parents often seek immediate care from an emergency setting and an HCP who may lack adequate training or resources.5 For example, in EDs, 94% of HCPs routinely supplied formal written discharge recommendations; however, in 1 study,6 35% did not use formal clinical guidelines, and only 13% or 19% recommended a gradual or stepwise progression, respectively. When asked about referral practices, ED providers indicated referral to a PCP (57%) most often, followed by a neurologist (46%), sports medicine specialist (20%), neuropsychologist (7%), or concussion clinic (6%); 25% indicated making no referrals.6 Similarly, 20% and 21% of pediatric emergency medicine providers cited inadequate training and time, respectively, as barriers to educating families about SRC.7 In previous research,7,36 PCPs described being uncomfortable with SRC management or uncertain about best SRC management practices and lacking adequate training to prescribe an RTP protocol. These outcomes may partially explain why 87% of PCPs stated that they referred patients with SRC to another provider, most often a concussion clinic (57%) or pediatric neurologist (31%).7,36 However, other factors (eg, state practice acts) should undoubtedly also be considered. In addition, school professionals who are commonly involved in managing student-athletes with SRCs (eg, ATs and school nurses) have commented that physicians often lack adequate training in concussion diagnosis and treatment and are inconsistent in their practices. This creates confusion among parents and athletes because of discordance between practice and regulations.8 However, educational interventions and in-depth training in SRC management have yielded favorable SRC management practices and behavioral changes among pediatric providers, including increased knowledge and comfort, implementation of RTP and return-to-learn guidelines, and development of individualized treatment and return plans.36–38 Importantly, ATs can use our findings in clinical practice to address anticipated returns based on the medical facility where an athletic receives clearance to athletes, coaches, and parents and the potential for more conservative concussion-management strategies.
No meaningful difference in the time to clearance by authorized HCPs was evident. Student-athletes who sought care from an NP received authorized clearance in a median of 9 days compared with 10 days for those who sought care from an MD or DO. Note that, whereas the test for equivalence of these times to clearance revealed a difference, we attribute that to the large sample size. Overall, the type of medical facility appeared to be more important than the authorizing HCP with respect to time to clearance.
Our study had limitations. First, some high schools that contributed data to the HIRS did not have licensed HCPs available at sponsored athletic events; therefore, the coaches or athletic administrators reported the SRCs. A weakness of the database is the inability to address who entered SRCs in the HIRS. Nonmedical personnel may lack the training necessary to appropriately identify SRCs and refer student-athletes to the proper resource. However, all student-athletes were required to seek care from an HCP to receive an official diagnosis of SRC. Second, the RTP protocol used for each student-athlete at each facility and whether an AT was involved in the RTP progression beyond the initial evaluation were unknown, which may have influenced the time to authorized clearance. Nevertheless, the athletic association mandates that authorized clearance requires an unconditional return, so this timing includes an RTP progression. From the HIRS database, we were able to determine the presence of an AT only during the initial evaluation but not at other stages of the SRC management process. Therefore, analyses to determine whether an AT's presence throughout SRC recovery influences return outcomes were not possible. Specific data regarding the RTP progression or criteria used for RTP at each facility or by providers were not recorded for each SRC case in the database. Future researchers should focus on elucidating why differences existed across medical facilities. Similarly, we did not account for the number of patient encounters with an HCP or referrals between HCPs and medical facilities. The number of times a patient sees an HCP during recovery from an SRC may influence the timing of return to activity, so this information should be included in the interpretation of findings and incorporated into future studies. Reasons why an athlete did not obtain clearance to return were also not recorded for each case, which may include but are not limited to the end of the season, return occurring after the season, not being given authorization to return, not seeking authorization, or quitting the sport. Third, although the sample size was one of the biggest strengths of our work, the sample consisted only of high school student-athletes in Michigan, and the complexity of their injuries was unknown. Thus, these factors have unknown effects on the generalizability of the results, particularly in areas of the United States that lack a concussion-reporting system.
CONCLUSIONS
This is the largest investigation to date examining differences in time to authorized clearance after SRC by HCPs and medical facilities among a high school student-athlete population. Athletic trainers, followed by coaches, were most often the first point of contact after SRC. Our results also revealed where student-athletes sought authorized clearance and when they obtained authorized clearance to return to unrestricted activity. We observed differences between sexes in the initial examiner for SRC cases, as a greater proportion of males (74.1%, n = 7772) had an AT involved in their initial examination than did females (65.8%, n = 3632). For cases in which authorized clearance was obtained, we also found an association between sex and the medical facility where the student-athlete was cleared. Ultimately, we demonstrated an association between the personnel involved in the initial SRC examinations and where a student-athlete obtained authorized clearance to return to unrestricted activity; student-athletes were most frequently cleared to return to full unrestricted activity by a PCP or team physician. Student-athletes were authorized to return to full, unrestricted activity 5 to 6 days sooner if they sought care at an urgent/ready care facility versus more specialized medical facilities (eg, team physician, neurologist's office). These findings provide meaningful data for ATs to use when directing clearance for return to full participation and describing anticipated recovery outcomes based on clearance by medical facilities. Future researchers should explore why these differences in authorized clearance time exist and why athletes seek care at different medical facilities.
REFERENCES
- 1.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F; Seattle Sports Concussion Research Collaborative. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138(1) doi: 10.1542/peds.2015-4635. e20154635. [DOI] [PubMed] [Google Scholar]
- 2.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–847. doi: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 3.Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213–225. doi: 10.1136/bjsports-2018-100338. [DOI] [PubMed] [Google Scholar]
- 4.Valovich McLeod TC, Kostishak NII, Anderson BE, Welch Bacon CE, Lam KC. Patient, injury, assessment, and treatment characteristics and return-to-play timelines after sport-related concussion: an investigation from the Athletic Training Practice-Based Research Network. Clin J Sport Med. 2019;29(4):298–305. doi: 10.1097/JSM.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 5.Zamarripa A, Clark SJ, Rogers AJ, Wang-Flores H, Stanley RM. Pediatric concussion management in the emergency department: a national survey of parents. J Pediatr. 2017;181:229–234. doi: 10.1016/j.jpeds.2016.10.071. [DOI] [PubMed] [Google Scholar]
- 6.Stern RA, Seichepine D, Tschoe C, et al. Concussion care practices and utilization of evidence-based guidelines in the evaluation and management of concussion: a survey of New England emergency departments. J Neurotrauma. 2017;34(4):861–868. doi: 10.1089/neu.2016.4475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zonfrillo MR, Master CL, Grady MF, Winston FK, Callahan JM, Arbogast KB. Pediatric providers' self-reported knowledge, practices, and attitudes about concussion. Pediatrics. 2012;130(6):1120–1125. doi: 10.1542/peds.2012-1431. [DOI] [PubMed] [Google Scholar]
- 8.Howland J, Hackman H, Taylor A, et al. Evaluation of implementation of Massachusetts sports concussion regulations: results of focus groups with school nurses and athletic trainers. J Sch Nurs. 2018;34(5):344–349. doi: 10.1177/1059840517702697. [DOI] [PubMed] [Google Scholar]
- 9.Nelson LD, Guskiewicz KM, Barr WB, et al. Age differences in recovery after sport-related concussion: a comparison of high school and collegiate athletes. J Athl Train. 2016;51(2):142–152. doi: 10.4085/1062-6050-51.4.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams RM, Puetz TW, Giza CC, Broglio SP. Concussion recovery time among high school and collegiate athletes: a systematic review and meta-analysis. Sports Med. 2015;45(6):893–903. doi: 10.1007/s40279-015-0325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halstead ME, Walter KD, Moffatt K; Council on Sports Medicine and Fitness. Sport-related concussion in children and adolescents. Pediatrics. 2018;142(6):e20183074. doi: 10.1542/peds.2018-3074. [DOI] [PubMed] [Google Scholar]
- 12.Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250–259. doi: 10.1097/HTR.0b013e31825ad658. [DOI] [PubMed] [Google Scholar]
- 13.Buckley TA, Munkasy BA, Clouse BP. Acute cognitive and physical rest may not improve concussion recovery time. J Head Trauma Rehabil. 2016;31(4):233–241. doi: 10.1097/HTR.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grool AM, Aglipay M, Momoli F, et al. Pediatric Emergency Research Canada (PERC) Concussion Team. Association between early participation in physical activity following acute concussion and persistent postconcussive symptoms in children and adolescents. JAMA. 2016;316(23):2504–2514. doi: 10.1001/jama.2016.17396. [DOI] [PubMed] [Google Scholar]
- 15.Leddy JJ, Haider MN, Ellis MJ, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173(4):319–325. doi: 10.1001/jamapediatrics.2018.4397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas DG, Apps JN, Hoffmann RG, McCrea M, Hammeke T. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics. 2015;135(2):213–223. doi: 10.1542/peds.2014-0966. [DOI] [PubMed] [Google Scholar]
- 17.Asken BM, Bauer RM, Guskiewicz KM, et al. CARE Consortium Investigators. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate student-athletes. Am J Sports Med. 2018;46(6):1465–1474. doi: 10.1177/0363546518757984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51(4):329–335. doi: 10.4085/1062-6050-51.5.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elbin RJ, Sufrinko A, Schatz P, et al. Removal from play after concussion and recovery time. Pediatrics. 2016;138(3):e20160910. doi: 10.1542/peds.2016-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sports. Michigan High School Athletic Association. 2021 Accessed June 14. https://www.mhsaa.com/sports.
- 21.MHSAA protocol for implementation of national federation sports playing rules for concussions. Michigan High School Athletic Association. 2021 Accessed June 14. https://www.mhsaa.com/portals/0/documents/health%20safety/concussionprotocol.pdf.
- 22.Bretzin AC, Covassin T, Fox ME, et al. Sex differences in the clinical incidence of concussions, missed school days, and time loss in high school student-athletes, part 1. Am J Sports Med. 2018;46(9):2263–2269. doi: 10.1177/0363546518778251. [DOI] [PubMed] [Google Scholar]
- 23.Covassin T, Petit KM, Savage JL, et al. Sports-related concussion occurrence at various time points during high school athletic events, part 2. Am J Sports Med. 2018;46(9):2270–2276. doi: 10.1177/0363546518780225. [DOI] [PubMed] [Google Scholar]
- 24.Gravetter FJ, Wallnau LB, Forzano LAB, Witnauer JE. Essentials of Statistics for the Behavioral Sciences. Cengage Learning; 2020. 9th ed. [Google Scholar]
- 25.McGuine TA, Pfaller AY, Post EG, Hetzel SJ, Brooks A, Broglio SP. The influence of athletic trainers on the incidence and management of concussions in high school athletes. J Athl Train. 2018;53(11):1017–1024. doi: 10.4085/1062-6050-209-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huggins RA, Coleman KA, Attanasio SM, et al. Athletic trainer services in the secondary school setting: the Athletic Training Locations and Services Project. J Athl Train. 2019;54(11):1129–1139. doi: 10.4085/1062-6050-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Post EG, Schaefer DA, Biese KM, et al. A comparison of emergency preparedness between high school coaches and club sport coaches. J Athl Train. 2019;54(10):1074–1082. doi: 10.4085/1062-6050-207-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lam KC, Valier AR, Anderson BE, McLeod TC. Athletic training services during daily patient encounters: a report from the Athletic Training Practice-Based Research Network. J Athl Train. 2016;51(6):435–441. doi: 10.4085/1062-6050-51.8.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Desai N, Wiebe DJ, Corwin DJ, Lockyer JE, Grady MF, Master CL. Factors affecting recovery trajectories in pediatric female concussion. Clin J Sport Med. 2019;29(5):361–367. doi: 10.1097/JSM.0000000000000646. [DOI] [PubMed] [Google Scholar]
- 30.Kontos AP, Jorgensen-Wagers K, Trbovich AM, et al. Association of time since injury to the first clinic visit with recovery following concussion. JAMA Neurol. 2020;7(4):435–440. doi: 10.1001/jamaneurol.2019.4552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haarbauer-Krupa JK, Comstock RD, Lionbarger M, Hirsch S, Kavee A, Lowe B. Healthcare professional involvement and RTP compliance in high school athletes with concussion. Brain Inj. 2018;32(11):1337–1344. doi: 10.1080/02699052.2018.1482426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Keefe KA, Beamon B, Brewer KL, Niceler B. Sports-related concussions in children: differences in care and expectations when seen in an emergency department versus a sports medicine clinic. Pediatr Emerg Care. 2018;34(5):322–324. doi: 10.1097/PEC.0000000000001476. [DOI] [PubMed] [Google Scholar]
- 33.Wallace J, Covassin T, Lafevor M. Use of the stepwise progression return-to-play protocol following concussion among practicing athletic trainers. J Sport Health Sci. 2018;7(2):204–209. doi: 10.1016/j.jshs.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lempke LB, Schmidt JD, Lynall RC. Athletic trainers' concussion-assessment and concussion-management practices: an update. J Athl Train. 2020;55(1):17–26. doi: 10.4085/1062-6050-322-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers' Association. National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flaherty MR, Raybould T, Jamal-Allial A, et al. Impact of a state law on physician practice in sports-related concussions. J Pediatr. 2016;178:268–274. doi: 10.1016/j.jpeds.2016.08.025. [DOI] [PubMed] [Google Scholar]
- 37.Arbogast KB, Curry AE, Metzger KB, et al. Improving primary care provider practices in youth concussion management. Clin Pediatr (Phila) 2017;56(9):854–865. doi: 10.1177/0009922817709555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reisner A, Burns TG, Hall LB, et al. Quality improvement in concussion care: influence of guideline-based education. J Pediatr. 2017;184:26–31. doi: 10.1016/j.jpeds.2017.01.045. [DOI] [PubMed] [Google Scholar]