Abstract
Context
Considering current models that highlight the role of psychological components in pain management, mindfulness practice may be an effective strategy in the management of pain.
Objective
To examine the effects of adding an 8-week mindfulness program to exercise therapy on the perceptions of pain severity, knee function, fear of movement, and pain catastrophizing of female recreational runners with patellofemoral pain (PFP).
Design
Randomized controlled clinical trial.
Setting
University laboratory.
Patients or Other Participants
Thirty female runners (age = 28.3 ± 7.08 years) with PFP were randomly assigned to the exercise or mindfulness-exercise group.
Intervention(s)
The exercise-only group followed a protocol (18 weeks, 3 sessions/wk) that featured training modifications to help control injury-related symptoms. The mindfulness-exercise group received an 8-week mindfulness intervention in addition to the exercise protocol. The mindfulness component started 4 weeks before the exercise component; therefore, the 2 components overlapped during the first 4 weeks of the intervention.
Main Outcome Measure(s)
Usual pain, pain during stepping, and pain during running were assessed using visual analog scales. Functional limitations of the knee were assessed using the Knee Outcome Survey. Fear of movement, pain catastrophizing, and coping strategies were measured via the Tampa Scale for Kinesiophobia, the Pain Catastrophizing Scale, and the Coping Strategies Questionnaire, respectively. These outcomes were assessed at baseline, at week 9, and after 18 weeks.
Results
Pain during running, pain during stepping, and functional limitations of the knee were less for the mindfulness-exercise group than for the exercise-only group (P values < .05). The mindfulness-exercise group reported greater perceived treatment effects than the exercise-only group (P < .05). Pain catastrophizing was less and coping strategies were more favorable for mindfulness-exercise participants than for exercise-only participants (P values < .05).
Conclusions
Mindfulness practice can be an effective adjunct to exercise therapy in the rehabilitation of PFP in recreational female runners.
Keywords: sport rehabilitation, sport injuries, anterior knee pain
Key Points
Adding an 8-week mindfulness intervention to an exercise therapy program facilitated a quicker onset of perceived therapeutic effectiveness in terms of clinical and psychological outcomes in runners with patellofemoral pain.
After 18 weeks of exercise therapy, participants who received an 8-week mindfulness program showed greater improvements in clinical and psychological outcomes than those who did not receive the program, indicating better long-term effectiveness.
Adding an 8-week mindfulness practice to the patellofemoral pain exercise therapy program led to more long-lasting effects 2 months after the interventions.
Patellofemoral pain (PFP), which refers to pain around or behind the patella that is exacerbated by activities that exert load on the patellofemoral joint,1 is a common condition among runners2 and can have adverse effects on physical and occupational functioning.1 Although athletic trainers who provide treatment for patients with PFP usually target physical impairments, such as muscle weakness, muscle shortness, and poor quality of movement,3 the relationship between structural malalignment of the patellofemoral joint and pain and disability in these patients is weak.4 Researchers5–7 have suggested that psychological characteristics play a role in exacerbating and prolonging the pain and weakening the physical function of athletes with PFP. According to the biopsychosocial model, pain and disability are the result of an ongoing interaction among physiological, psychological, and social factors, which leads to a complex pattern of symptoms with potentially chronic consequences.7 Consistent with the tenets of the biopsychosocial model,5,6,8,9 investigators have supported the proposed role of psychological factors in the disability and pain of PFP. In particular, inverse relationships between maladaptive cognitions and functional status in patients with PFP5,9 indicate that co-interventions specifically targeting catastrophic thinking may enhance treatment outcomes.
Framed in a biopsychosocial perspective, the fear-avoidance model has been used to examine the role of cognitive and emotional factors in the chronicization of pain and disability in musculoskeletal conditions.8 In the fear-avoidance model, pain intensity is associated with negative appraisals of and excessive negative attitudes toward pain (catastrophic thoughts), which lead to fear of reinjury and subsequent maladaptive coping behaviors, such as escape, avoidance, and hypervigilance to certain experiences or movements that limit the person's functioning.8 Almost all of these maladaptive coping behaviors are present in individuals with PFP5–7 and have been associated with increased pain intensity, pain chronicization, and disability.5–8 Such pain may result in psychological distress, reflected in people's fear-avoidance and catastrophizing thoughts concerning their knee pain,6,9 that can interfere with involvement in physical activity.10 A deeper understanding of the negative psychological responses associated with PFP may help in relieving pain and improving knee function in these patients.
Mindfulness is a mental state that involves a deep sensory consciousness of present-moment experiences, without any revealing, responsive, and self-referential judgment of the inner experience.11 The practice of mindfulness requires deliberate, sustained attention to sensory and cognitive processes along with an unconditional acceptance of the inner experience.11 This practice requires a conscious effort to inhibit learned responses and create greater acceptance of, detachment from, and objectivity regarding each experience.11 Mindfulness practice makes it possible for participants to truly experience what is happening in the here and now through attention to and awareness of emotional states.12 As part of an injury-rehabilitation program, mindfulness can be an effective means of achieving physical and mental relaxation,13 facilitating an individual's communication with the mind and body,12 and recognizing and accepting his or her condition as an injured athlete,13 thereby promoting a more effective focus on rehabilitation.13 Mindfulness can also change several aspects of the pain-related fear-avoidance cycle, such as catastrophizing, anxiety, arousal, and avoidance behaviors,11,14–16 which may reduce the physical pain and disability associated with sport injuries. Furthermore, mindfulness can facilitate pain relief through detachment from the sensory aspects of pain and changes in the cognitive appraisals of and affective-motivational reactions to pain.14,15
Our goal in this study was to assess the effect of adding a mindfulness program to an exercise program on pain intensity, knee-related function, perceived treatment effect, fear of reinjury, and pain catastrophizing in female recreational runners with PFP. Based on the literature, we hypothesized that compared with a control group, runners with PFP who received mindfulness training in addition to the exercise treatment program would experience (1) less pain intensity, fear of reinjury, and pain catastrophizing; and (2) better knee function and more frequent use of coping strategies to manage pain.
METHODS
Design
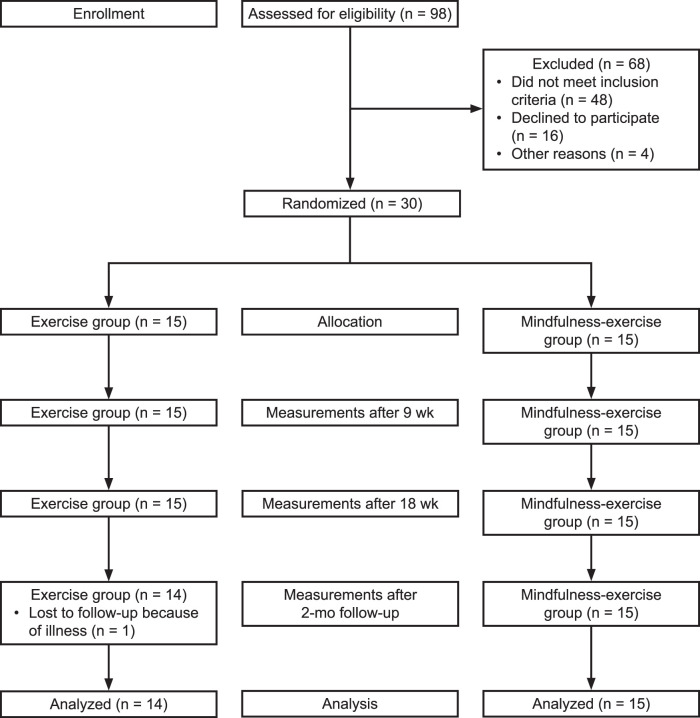
This study was an 18-week, single-blinded, parallel-group randomized controlled trial conducted at the University College of Omran and Tosseeh and University of Nahavand. Participants were assessed at baseline, week 9 after completion of the mindfulness sessions (midintervention), week 18 (end of the exercise intervention), and 2 months after the end of the intervention (follow-up; Figure).
Figure.
Flow of participants during the study.
Participants
Based on a prior study that identified an SD of 25-mm pain intensity measured on a 100-mm visual analog scale (VAS),17 we determined that 15 participants in each group would be necessary to detect a 20-mm between-groups difference in pain intensity, considering a 2-tailed significance level (α) of .05 and desired power (1 − β) of .90.
A total of 98 female recreational runners suspected of experiencing PFP were screened, and 30 met the inclusion criteria. It is well documented that females are more likely than males to experience PFP.18 To be included in the study, recreational runners had to (1) be female and between the ages of 18 and 40 years; (2) report running ≥2 times per week for >45 minutes or a minimum weekly running distance of 10 km; (3) present a history of insidious onset of signs and symptoms of PFP in 1 or both knees that was unrelated to trauma for at least 3 months before assessment; (4) score <85/100 on the Activities of Daily Living Scale of the Knee Outcome Survey (KOS-ADLS); and (5) report anterior or retropatellar knee pain of ≥3 on the 10-cm VAS during at least 3 of the following tasks: manual compression of the patella against the femur at rest; an isometric knee-extensor contraction; palpation of the posteromedial and posterolateral borders of the patella; resisted knee extension; and running, jumping, squatting, kneeling, ascending or descending stairs, or prolonged sitting.2
Recruits were excluded if they had an intra-articular condition, coexisting lower limb injury, a history of patellar dislocation or knee surgery, pain originating in the patellar tendon or menisci, Osgood-Schlatter or Sinding- Larsen-Johansson syndrome, knee joint effusion, or hip pain or if palpation of the patellar tendon, iliotibial band, or pes anserinus tendon induced pain. All assessments were conducted by a licensed physiotherapist at a university-based laboratory. If participants had bilateral knee pain, the most painful knee (as indicated on the VAS) was selected for testing. Volunteers were recruited via flyers and pamphlets posted in physiotherapy clinics and public places and emails to faculty and staff of University College of Omran and Tosseeh and University of Nahavand in January and February 2019. All participants signed an informed consent form approved by the Ethics Committee for Research on Human Subjects of University College of Omran and Tosseeh and the University of Nahavand, which also approved the study, and the trial was registered with the University Hospital Medical Information Network Clinical Trial Registry (UMIN000035347).
Randomization and Blinding
Participants were enrolled by an independent physiotherapist who was blinded to their allocation to experimental conditions. A computer-generated (version 2.0; Random Allocation Software) random allocation sequence was used to block randomize participants (block sizes of 2, 4, or 6; allocation ratio = 1:1) to the exercise-only or mindfulness-exercise group.
To control for selection bias, we used sequentially numbered, opaque, sealed envelopes to hide the group allocations from the researchers enrolling and assessing participants. The envelopes were numbered and recorded on an official trial form by an independent researcher. Corresponding envelopes were opened by a research assistant after the enrolled participants completed the baseline assessments and it was time to allocate the intervention. All clinical assessments were performed by a laboratory specialist who was not directly involved in the study and was blinded to the intervention(s) the patients received. The data analyst was also blinded to group allocation. Precautions were taken to ensure that participants were unaware of the intervention(s) applied in the other group. They were asked not to disclose the content of their program to the laboratory specialist.
Outcome Measures
Pain Intensity
Pain intensity was measured on a 100-mm VAS ranging from 0 (no pain) to 100 (worst possible pain).19 Participants rated their current, best, and worst level of pain during the last 24 hours. The average of the 3 ratings was used to estimate usual pain intensity. Pain during running and stepping was also measured.
Knee Symptoms and Function
During daily living and sport, knee symptoms and function were assessed with the KOS, which consists of the following 2 subscales: the KOS-ADLS and the KOS-Sports Activities Scale (KOS-SAS). The KOS-ADLS contains 14 items that evaluate knee injury-related symptoms and functional limitations during daily living. The KOS-SAS contains 11 items related to symptoms and functional limitations during sport activities. Responses are rated on a 6-point Likert scale from 0 (unable to perform) to 5 (no difficulty). Scores are calculated by summing the item scores for each subscale and normalizing them to a 0 to 100 score, with 0 indicating extreme knee problems and 100 indicating no knee problems.20
Perceived Treatment Effect
The treatment effect was measured using the global rating of change scale.21 Participants rated the perceived effect of treatment on a 15-point, single-item scale ranging from −7 (a very great deal worse) to +7 (a very great deal better), with 0 representing about the same. Participant scores and the number of participants who scored +4 (moderately better) or higher, indicating successful treatment, are reported.17
Fear of Movement and Reinjury
Fear of movement and reinjury was assessed using the Tampa Scale of Kinesiophobia. The Tampa Scale of Kinesiophobia is a 17-item questionnaire in which participants rate their agreement with each item (eg, “I'm afraid that I might injure myself if I exercise”) on a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree). A total sum is calculated, and higher scores reflect more pain-related fear.22
Pain Catastrophizing
We assessed this factor using the Pain Catastrophizing Scale, which consists of 13 items describing the pain experience (eg, “If I am in pain, I am afraid the pain will get worse”). The Pain Catastrophizing Scale measures the 3 dimensions of catastrophizing: rumination, magnification, and helplessness. Rumination refers to a patient's incapacity to stop thinking of attending to the pain. Magnification represents an exaggerated appraisal of pain as a threat. Helplessness describes a state of despair that is brought about by the perception that one is incapable of exerting any control over the experience of pain. Participants rate their agreement with each item using a 5-point Likert scale from 0 (not at all) to 4 (always). Higher total and subscale scores indicate more frequent pain catastrophizing.23
Coping Strategies
The frequency of each participant's use of pain-coping strategies was assessed on the 27-item Coping Strategies Questionnaire. Coping strategies are categorized into 6 domains: distraction (5 items), catastrophizing (6 items), ignoring pain sensations (5 items), distracting from pain (4 items), coping self-statements (4 items), and praying and hoping (3 items). Each domain is scored separately; higher scores indicate a greater use of strategies.24 Respondents rate how often they use each strategy to cope with pain on a Likert scale ranging from 0 (never do that) to 6 (always do that).24
A survey was used to gather information on age, weight, height, pain medication use, and running habits.
Interventions
Exercise Intervention
Participants in both groups received an exercise protocol that consisted of 13 exercises (6 stretching exercises, 7 strength and balance exercises) for three 60- to 90-minute sessions per week over 18 weeks.17,25 The exercise protocol was preceded with a 10-minute warm-up and ended with a 10-minute cool-down, including jogging and general and dynamic exercises. Rest intervals between sets and exercises were 30 and 90 seconds, respectively. The initial intensity of most strength-training exercises was a maximum of 10 repetitions, which produced VAS pain ratings of >3. We chose 10 repetitions maximum (approximately 75% of a maximal repetition) according to the Baechle and Earle guidelines for strength training.26 If participants did all the exercises without (1) aggravating their knee pain, (2) excessive fatigue, or (3) local muscle pain 48 hours after the training session, the training load was increased (Supplement Table 1).
Participants were also given instructions on how to manage their training load and modify their running according to their symptoms. We first asked them to increase their weekly exercise frequency and to reduce the duration and speed of each training session. Because some individuals had difficulties running downstairs and downhill, they were advised to avoid such activities and engage in run-walk intervals instead. We recommended they keep the PFP intensity to ≤3 of 10 on the VAS while running. If the pain did not return to the pre-exercise levels within 60 minutes postexercise or if symptoms were increased the following morning, the training load and intensity of the running program were modified. Runners were advised against increasing the step rate by more than 7.5% to 10% per week27 and using a non–rearfoot-strike pattern.28
At the end of each week, each person had a 10-minute treadmill session and received feedback from the physiotherapist on running technique. The weekly program was individually tailored and continuously modified by a physiotherapist depending on the participant's symptoms. All exercises were supervised by a researcher and a physiotherapist. None of the participants pursued any other training programs during the study, and all were asked not to attempt physical activities that would induce knee pain.
Mindfulness Training
During the 8 weeks of mindfulness-based stress reduction,29 the mindfulness-exercise group received instruction on mindfulness meditation practices, such as breathing meditation, body scan meditation, gentle yoga, sitting meditation, and walking meditation. This instruction was expected to increase the awareness of thoughts, bodily sensations, and emotions, with an attitude of curiosity, openness, and acceptance12,14 (Supplemental Table 2).
The mindfulness component started 4 weeks before the exercise component; therefore, these components overlapped during the first 4 weeks of the exercise intervention. To optimize skill learning, mindfulness sessions were conducted by a trained sport psychologist and delivered in 2 sessions involving 7 and 8 participants. We did not administer 1-on-1 training sessions, but when a participant had difficulty learning any skill, the sport psychologist spent more time with that person at the end of the session as needed. Participants were asked to practice the skills at home for up to 45 minutes daily. This regimen was listed on a preprinted form that was used to monitor participant adherence. Researchers provided training manuals and CDs with instructions for practice during the intervention and follow-up periods.
Attendance
Attendance rates for the exercise component of the programs for the exercise-only group and mindfulness-exercise group were 87.7% (range = 81.5%–100%) and 92.3% (range = 85.2%–100%), respectively. Time limitations, family problems, fatigue, and disease were the main reasons cited for nonattendance. The attendance rate for the mindfulness component was 100%.
Safety
Participants were asked to report any adverse events experienced during the study, regardless of perceived severity (eg, mild pain). An adverse event was defined as any unfavorable or unintended medical occurrence (ie, abnormal laboratory finding, symptom, or disease) temporally associated with the study, whether it was related to the interventions or not. Any individual reporting an adverse event was referred to an independent physician for clinical assessment and initiation of the appropriate course of action. Five participants (16.7%, 3 from the exercise-only group and 2 from the mindfulness-exercise group) described at least 1 adverse event, but no serious adverse events were identified. The adverse events consisted of temporary pain and resolved within 12 to 48 hours after the end of the exercise training session.
Data Analysis
Descriptive statistics were computed for all variables. Normality and homogeneity of variances were tested with the Shapiro-Wilk and Levene tests, respectively. A series of 2 (exercise-only group and mindfulness-exercise group) × 4 (baseline, week 9, week 18, and follow-up) mixed-model analyses of variance were used to test the main and interaction effects of group (independent factor) and time (repeated-measures factor) on the dependent variables. For significant interactions, we performed pairwise comparisons with Bonferroni correction, for which multiplicity-adjusted P values are reported. The Cohen d effect size (ES) and difference between the exercise-only group and mindfulness-exercise group (Dif) were calculated for all continuous variables. Values are presented as mean ± SD and 95% CIs. All statistical analyses were conducted at an α level of .05 using SPSS statistical software (version 18.0; SPSS Inc).
RESULTS
At baseline, the mindfulness-exercise group was similar to the exercise-only group in terms of demographic and pain characteristics (P > .05). The session, duration, and distance of running were similar for both groups (P values > .05). Fourteen participants (9 from the exercise-only group, 5 from the mindfulness-exercise group) reported using medication for pain during the study (Table 1).
Table 1.
Participants' Baseline Demographic Characteristics, Biomedical Information, and Sport Function by Treatment Groupa
| Variables |
Groupb |
Mean Difference (95% CI) |
P Value |
|
| Mindfulness-Exercise (n = 15) |
Exercise (n = 14) |
|||
| Age, y | 27.9 ± 7.5 | 28.8 ± 6.8 | −0.9 (−6.12, 4.65) | .78 |
| Body mass index, m/kg2 | 23.7 ± 2.3 | 23.2 ± 2.6 | 0.5 (−1.30, 2.39) | .55 |
| Affected knee, n (left/right/bilateral) | 1/8/6 | 0/6/9 | .77 | |
| Target knee, n (dominant/ nondominant) | 13/2 | 13/2 | ||
| Injury history, wk | 27.9 ± 12.7 | 24.1 ± 10.7 | 3.8 (−5.10 to 12.55) | .4 |
| Sessions run/wk, No. | 3.5 ± 1.1 | 3.7 ± 0.8 | −0.2 (−0.93 to 0.53) | .6 |
| Duration run/wk, min | 101.0 ± 31.2 | 97.5 ± 22.5 | 3.5 (−16.67 to 24.01) | .7 |
| Distance run/wk, km | 13.4 ± 3.3 | 14.4 ± 2.6 | −1.0 (−3.27 to 1.14) | .3 |
| Any pain medication intake, No. (%) | 5 (33) | 9 (60) | .14 | |
Chi-square tests.
Mean ± SD except where indicated otherwise.
Pain Intensity
Significant time × treatment interaction effects were present for usual pain, pain during running, and pain during stepping (P values < .01; Table 2). Usual pain (P < .001, ES = 1.14), pain during running (P < .001, ES = 2.12), and pain during stepping (P < .001, ES = 1.16) decreased from baseline to week 9 for the mindfulness-exercise group. Pain during stepping decreased more for participants in the mindfulness-exercise group than for those in the exercise-only group at week 9 (P = .03; Dif = 13.1%; 95% CI = 7.3%, 18.9%), week 18 (P < .01; Dif = 12.3%; 95% CI = 2.9%, 21.7%), and follow-up (P < .01; Dif = 17%; 95% CI = 8.2%, 25.8%). Pain during running decreased more for individuals in the mindfulness-exercise group than for those in the exercise-only group at week 18 (P < .01; Dif = 15.8%; 95% CI = 11.0%, 20.6%) and follow-up (P < .01; Dif = 21.2%; 95% CI = 14.6%, 27.8%). In addition, usual pain decreased more for participants in the mindfulness-exercise group than for those in the exercise-only group at follow-up (P < .01; Dif = 21.9%; 95% CI = 14.1%, 29.7%).
Table 2.
Pain and Disability by Treatment Groups
| Variables |
Group, Mean ± SD |
Mean Difference (95% CI) |
Time |
Group |
Time × Group Interaction |
||||
| Mindfulness-Exercise (n = 15) |
Exercise (n = 14) |
||||||||
|
P Value |
ηp2 |
P Value |
ηp2 |
P Value |
ηp2 |
||||
| Usual pain | |||||||||
| Baseline | 32.9 ± 8.2a,b,c | 32.5 ± 8.8b,c | 0.4 (−5.9 to 6.7) | .001 | 0.94 | .23 | 0.05 | .001 | 0.34 |
| Week 9 | 29.9 ± 7.6 | 31.2 ± 7.3 | −1.3 (−7.1 to 4.5) | ||||||
| Week 18 | 11.6 ± 5.4 | 15.8 ± 5.1 | −4.2 (−8.1 to −0.3) | ||||||
| Follow-up | 12.9 ± 5.8 | 19.4 ± 5.9 | −6.5 (−10.9 to −2.1)d | ||||||
| Pain during running | |||||||||
| Baseline | 46.9 ± 11.0a,b,c | 45.1 ± 11.4b,c | 1.8 (−6.57 to 10.17) | .001 | 0.92 | .32 | 0.04 | .01 | 0.20 |
| Week 9 | 39.1 ± 10.1 | 43.1 ± 10.9 | −4.0 (−11.85 to 3.85) | ||||||
| Week 18 | 18.3 ± 6.4 | 23.7 ± 9.9 | −5.4 (−11.7 to 0.9)d | ||||||
| Follow-up | 21.3 ± 7.2 | 27.1 ± 10.0 | −5.8 (−12.7 to 0.8)d | ||||||
| Pain during stepping | |||||||||
| Baseline | 50.1 ± 13.5a,b,c | 49.7 ± 12.1b,c | 0.4 (−9.2 to 9.9) | .001 | 0.94 | .20 | 0.06 | .004 | 0.25 |
| Week 9 | 40.5 ± 10.2 | 46.3 ± 9.6 | −6.2 (−16.4 to 4.0)d | ||||||
| Week 18 | 20.1 ± 8.0 | 26.0 ± 7.7 | −5.9 (−11.8 to −0.1)d | ||||||
| Follow-up | 21.9 ± 10.3 | 30.1 ± 11.0 | −8.2 (−16.2 to −0.3)d | ||||||
| Knee-related function | |||||||||
| Baseline | 64.9 ± 9.1a,b,c | 62.6 ± 11.2a,b,c | 2.3 (−5.4 to 9.9) | .001 | 0.88 | .02 | 0.17 | .007 | 0.23 |
| Week 9 | 71.2 ± 9.2 | 68.8 ± 9.9 | 2.4 (−4.8 to 9.6) | ||||||
| Week 18 | 90.2 ± 8.1 | 81.8 ± 4.7 | 8.4 (3.4 to 13.4)d | ||||||
| Follow-up | 84.9 ± 8.2 | 71.9 ± 5.9 | 13.0 (7.7 to 18.3)d | ||||||
| Perceived treatment effect | |||||||||
| Week 9 | 3.5 ± 3.18a,b,c | 1.5 ± 2.41a,b,c | 2.0 (−0.1 to 4.1)d | .001 | 0.44 | .04 | 0.13 | .41 | 0.03 |
| Week 18 | 5.4 ± 1.76 | 3.9 ± 1.94 | 1.5 (−0.08 to 2.9)d | ||||||
| Follow-up | 4.4 ± 1.94 | 3.3 ± 2.02 | 1.1 (−0.4 to 2.6) | ||||||
| Fear of movement | |||||||||
| Baseline | 45.7 ± 6.7a,b,c | 46.5 ± 5.8a,b | −0.8 (−5.5 to 3.8) | .001 | 0.75 | .001 | 0.33 | .001 | 0.37 |
| Week 9 | 32.5 ± 5.7 | 40.4 ± 4.4 | −7.9 (−11.6 to −4.1)d | ||||||
| Week 18 | 27.5 ± 5.5 | 38.3 ± 6.9 | −10.8 (−15.4 to −6.1)d | ||||||
| Follow-up | 30.9 ± 4.9 | 42.3 ± 7.8 | −11.4 (−16.3 to −6.5)d | ||||||
Within-group difference between baseline and week 9.
Within-group difference between baseline and week 18.
Within-group difference between baseline and follow-up.
Between-groups difference.
A significant positive relationship was demonstrated between pain intensity before the intervention(s) and the amount of pain reduction after the 18-week intervention(s) for usual pain (r = 0.54, P < .001), pain during running (r = 0.63, P < .001), and pain during stepping (r = 0.43, P < .001). These results suggest that the pain reduction was greater for participants who reported higher levels of pain before the interventions.
Knee-Related Function
A significant time × treatment interaction effect was found for knee function (P < .01; Table 2). Knee function for the exercise and mindfulness-exercise groups improved from baseline to week 9 (P < .001, ES = 1.28 and P < .001, ES = 1.40, respectively). This improvement was similar for both groups at week 9 (P > .05), but knee function improved more for the mindfulness-exercise group than for the exercise-only group at week 18 (P < .01; Dif = 8.2%; 95% CI = 3.3%, 13.1%) and follow-up (P < .01; Dif = 14.8%; 95% CI = 6.6%, 23.0%).
Perceived Treatment Effect
Time and treatment effects were evident for the perceived treatment effect (P < .01; Table 2). Follow-up comparisons showed that the perceived treatment effect improved more for the mindfulness-exercise group than for the exercise-only group at week 9 (P < .01; Dif = 28.5%, 95% CI = 19.9%, 37.1%) and week 18 (P < .01; Dif = 20.8%, 95% CI = 15.3%, 26.3%) but not at follow-up (P > .05). By week 9, 60% of the mindfulness-exercise group reported that treatment was successful, compared with 27% of the exercise-only group (χ2 = 6.42, P = .02). By week 18, 73% of the mindfulness-exercise group and 60% of the exercise-only group noted that treatment was successful, whereas at follow-up, these numbers were 67% for the mindfulness-exercise group and 60% for the exercise-only group; none of these differences were significant (χ2 = 2.73, P = .21, and χ2 = 0.23, P = .57, respectively).
Fear of Movement
A significant time × treatment interaction effect was observed for fear of movement (P < .01; Table 2). Fear of movement decreased from baseline to week 9 for participants in the mindfulness-exercise group (P < .001, ES = 2.76) but not for those in the exercise-only group (P > .05). Fear of movement decreased more in the mindfulness-exercise group than in the exercise-only group at week 9 (P < .001; Dif = 20.6%; 95% CI = 13.0%, 28.2%), week 18 (P = .001; Dif = 22.1%; 95% CI = 14.6%, 29.6%), and follow-up (P < .01; Dif = 23.4%; 95% CI = 11.9%, 34.9%).
Pain Catastrophizing
A significant time × treatment interaction effect was present for pain catastrophizing (P < .01; Table 3). Pain catastrophizing decreased in the mindfulness-exercise group from baseline to week 9 (P < .01, ES = 0.80) but not in the exercise-only group (P > .05). Pain catastrophizing decreased more in the mindfulness-exercise group than in the exercise-only group at week 9 (P < .01; Dif = 30.8%; 95% CI = 21.8%, 39.8%), week 18 (P = .01; Dif = 40.9%; 95% CI = 29.6%, 52.2%), and follow-up (P < .02; Dif = 28.4%; 95% CI = 18.7%, 38.1%).
Table 3.
Pain-Catastrophizing Variables by Treatment Groups
| Variables |
Group, Mean ± SD |
Mean Difference (95% CI) |
Time |
Group |
Time × Group Interaction |
||||
| Mindfulness-Exercise (n = 15) |
Exercise (n = 14) |
||||||||
|
P Value |
η
p
2
|
P Value |
η
p
2
|
P Value |
η
p
2
|
||||
| Pain catastrophizing | |||||||||
| Baseline | 21.2 ± 4.4a,b,c | 22.1 ± 4.9a,b | −0.9 (−3.7 to 1.9) | .001 | 0.77 | .001 | 0.49 | .001 | 0.45 |
| Week 9 | 10.5 ± 2.0 | 17.8 ± 3.5 | −7.3 (−9.1 to −5.5)d | ||||||
| Week 18 | 9.3 ± 2.1 | 18.4 ± 3.3 | −9.1 (−11.1 to −7.1)d | ||||||
| Follow-up | 12.4 ± 2.2 | 19.2 ± 5.1 | −6.8 (−9.7 to −3.9)d | ||||||
| Rumination | |||||||||
| Baseline | 9.5 ± 3.3a,b,c | 8.0 ± 3.6b | 1.5 (−1.0 to 4.1) | .001 | 0.76 | .14 | 0.08 | .001 | 0.44 |
| Week 9 | 3.7 ± 1.5 | 6.1 ± 2.7 | −2.4 (−4.0 to −0.8)d | ||||||
| Week 18 | 3.3 ± 1.4 | 5.9 ± 2.6 | −2.6 (−4.1 to −1.1)d | ||||||
| Follow-up | 4.4 ± 1.7 | 6.2 ± 2.8 | −1.8 (−3.4 to −0.2)d | ||||||
| Magnification | |||||||||
| Baseline | 5.7 ± 3.5a,b,c | 7.3 ± 1.7a,b | −1.6 (−3.7 to 0.5) | .001 | 0.45 | .002 | 0.29 | .06 | 0.10 |
| Week 9 | 3.5 ± 1.6 | 5.7 ± 1.8 | −2.2 (−3.4 to −1.0)d | ||||||
| Week 18 | 2.9 ± 1.3 | 5.9 ± 1.7 | −3.0 (−4.2 to −1.8)d | ||||||
| Follow-up | 4.2 ± 1.9 | 6.5 ± 1.8 | −2.3 (−3.7 to −0.9)d | ||||||
| Hopelessness | |||||||||
| Baseline | 5.9 ± 2.5a,b,c | 6.8 ± 2.3 | −0.9 (−2.9 to 1.1) | .001 | 0.33 | .003 | 0.27 | .01 | 0.12 |
| Week 9 | 3.4 ± 1.7 | 6.1 ± 2.2 | −2.7 (−4.2 to −1.2)d | ||||||
| Week 18 | 3.1 ± 1.8 | 5.8 ± 2.0 | −2.7 (−4.1 to −1.3)d | ||||||
| Follow-up | 3.8 ± 1.6 | 6.5 ± 3.0 | −2.7 (−4.5 to −0.9)d | ||||||
Within-group difference between baseline and week 9.
Within-group difference between baseline and week 18.
Within-group difference between baseline and follow-up.
Between-groups difference.
Coping Strategies
Significant time × treatment interaction effects were demonstrated for ignoring pain sensations and distracting from pain (P < .01) (Table 4). Ignoring pain sensations and distracting from pain strategies were increased in the mindfulness-exercise group from baseline to week 9 (P < .001, ES = 0.73 and P < .001, ES = 1.1, respectively) but not in the exercise-only group (P > .05). Furthermore, both strategies were used more often in the mindfulness-exercise group than in the exercise-only group at week 9 (P < .001; Dif = 18.4%; 95% CI = 8.3%, 28.5% and P < .001; Dif = 32.3%; 95% CI = 17.9%, 46.7%, respectively), week 18 (P < .001; Dif = 39.7%; 95% CI = 30.1%, 49.3% and P < .01; Dif = 30.7%; 95% CI = 23.4%, 38.0%, respectively), and follow-up (P < .001; Dif = 30.6%; 95% CI = 24.7%, 36.5% and P < .001; Dif = 27.4%; 95% CI = 22.5%, 32.3%, respectively).
Table 4.
Coping Strategies by Treatment Group
| Variables |
Group, Mean ± SD |
Mean Difference (95% CI) |
Time |
Group |
Time × Group Interaction |
||||
| Mindfulness-Exercise (n = 15) |
Exercise (n = 14) |
||||||||
|
P Value |
ηp2 |
P Value |
ηp2 |
P Value |
ηp2 |
||||
| Distraction | |||||||||
| Baseline | 17.1 ± 5.9a,b,c | 17.2 ± 5.3 | −0.1 (−4.3 to 4.1) | .001 | 0.31 | .36 | 0.03 | .08 | 0.09 |
| Week 9 | 20.1 ± 6.1 | 18.5 ± 6.1 | 1.6 (−3.0 to 6.2) | ||||||
| Week 18 | 22.3 ± 5.8 | 19.1 ± 5.1 | 3.2 (−0.9 to 7.3)d | ||||||
| Follow-up | 20.4 ± 4.8 | 18.3 ± 4.6 | 2.1 (−1.4 to 5.6) | ||||||
| Catastrophizing | |||||||||
| Baseline | 18.4 ± 6.9a,b,c | 19.5 ± 7.4 | −1.1 (−4.3 to 6.5) | .001 | 0.31 | .08 | 0.11 | .02 | 0.14 |
| Week 9 | 14.4 ± 5.2 | 18.3 ± 5.1 | −3.9 (−7.8 to −0.1)d | ||||||
| Week 18 | 13.2 ± 4.2 | 17.5 ± 4.8 | −4.3 (−7.7 to −0.9)d | ||||||
| Follow-up | 13.9 ± 4.5 | 17.8 ± 4.7 | −3.9 (−7.3 to −0.5)d | ||||||
| Ignoring pain sensations | |||||||||
| Baseline | 15.7 ± 5.9a,b,c | 16.6 ± 6.4 | −0.9 (−5.5 to 3.8) | .001 | 0.68 | .17 | 0.07 | .001 | 0.57 |
| Week 9 | 20.0 ± 5.4 | 17.3 ± 6.4 | 2.7 (−1.7 to 7.1)d | ||||||
| Week 18 | 22.4 ± 5.7 | 17.2 ± 5.9 | 5.2 (0.9 to 9.5)d | ||||||
| Follow-up | 21.0 ± 4.8 | 17.1 ± 6.1 | 3.9 (−0.2 to 8.0)d | ||||||
| Distancing from pain | |||||||||
| Baseline | 14.1 ± 4.9a,b,c | 15.6 ± 5.9 | −1.5 (−5.6 to 2.6) | .001 | 0.46 | .36 | 0.03 | .001 | 0.23 |
| Week 9 | 19.1 ± 4.4 | 16.1 ± 6.1 | 3.0 (1.0 to 7.0)d | ||||||
| Week 18 | 20.5 ± 5.3 | 17.9 ± 5.2 | 2.6 (−1.3 to 6.5)d | ||||||
| Follow-up | 19.1 ± 4.3 | 16.7 ± 5.3 | 2.4 (−1.2 to 6.0)d | ||||||
| Coping self-statement | |||||||||
| Baseline | 14.3 ± 3.9a,b | 14.5 ± 3.9 | −0.2 (−2.7 to 3.1) | .06 | 0.09 | .41 | 0.02 | .13 | 0.06 |
| Week 9 | 16.1 ± 4.9 | 14.2 ± 4.9 | 1.9 (−1.8 to 5.6) | ||||||
| Week 18 | 17.1 ± 4.8 | 14.8 ± 4.7 | 2.3 (−1.3 to 5.8)d | ||||||
| Follow-up | 15.8 ± 3.9 | 14.9 ± 4.8 | 0.9 (−2.4 to 4.2) | ||||||
| Praying and hoping | |||||||||
| Baseline | 7.4 ± 2.9b,c | 8.8 ± 2.1 | −1.4 (−3.3 to 0.5) | .16 | 0.06 | .09 | 0.01 | .12 | 0.07 |
| Week 9 | 8.2 ± 3.4 | 8.5 ± 3.2 | −0.3 (−2.8 to 2.2) | ||||||
| Week 18 | 9.8 ± 2.4 | 8.7 ± 2.2 | 1.1 (−0.6 to 2.8) | ||||||
| Follow-up | 9.1 ± 2.1 | 8.1 ± 2.1 | 1.0 (−1.3 to 3.3) | ||||||
Within-group difference between baseline and week 9.
Within-group difference between baseline and week 18.
Within-group difference between baseline and follow-up.
Between-groups difference.
DISCUSSION
Overall, adding an 8-week mindfulness intervention to exercise therapy led to decreased pain intensity, fear of reinjury, and pain catastrophizing and increased knee function and coping strategies to manage knee pain in recreational runners with PFP. These findings are consistent with those of researchers30 who showed that mindfulness training enhanced the responses to nonpharmacologic interventions for knee osteoarthritis.
Mindfulness practice modified pain-associated cognitions (ie, fear of pain and pain catastrophizing) so that runners were less fearful of reinjury when performing rehabilitation movements and reported fewer pain-catastrophizing thoughts. These results augment those of previous studies in which adding cognitive-behavioral treatment to routine biomedical therapy for chronic low back pain was associated with decreased fear-of-movement beliefs29 and alterations in fear-avoidance beliefs about physical activity were the strongest predictor of functional improvement and postrehabilitation pain reduction in patients with anterior knee pain.9 Other authors5,6 have also shown that changes in catastrophizing and kinesiophobia after exercise therapy can predict changes in disability and pain intensity in patients with anterior knee pain. The precise mechanisms by which catastrophizing can affect pain and disability are not well understood. It appears that people who are prone to catastrophizing have difficulty moving their focus away from painful or threatening stimuli, thereby exacerbating pain-related fear.31 Catastrophizing is also associated with an excessive emotional evaluation of pain, which facilitates pain perception.31,32 Among our participants, mindfulness may have disrupted the fear-avoidance cycle by attenuating pain catastrophizing. In other words, mindfulness may act as a moderator of the relationship between pain intensity and pain catastrophizing.16
According to the fear-avoidance model of pain,32 pain-related fear leads to avoidance behaviors. Therefore, informing runners of the negative effects of ruminative thinking concerning their pain may lead to less fear of pain. In turn, less avoidant behavior can reduce the risk of functional disability after PFP. Overall, our results suggested that reductions in fear of pain and pain catastrophizing mediated the effects of mindfulness on pain and rehabilitation outcomes.
Mindfulness may help runners experience pain relief by enabling them to detach themselves from the sensory dimension of pain.14,15 Such detachment can lead to a decrease in the primary sensory component of pain through descending inhibitory signals.15 Higher scores in ignoring pain sensations and distracting from pain dimensions in the mindfulness-exercise group than those in the exercise-only group may represent this detachment from the sensory dimension of pain. Mindfulness is associated with shifting attention from ruminative thoughts to the present moment.12 This shift can lead to a lower level of negative affect, detachment from the sensory dimension of pain, and less cognitive disruption during the therapeutic exercise program, all of which could help improve the performance outcomes of runners with PFP.
Our study had several limitations. Because participants were exclusively recreational female runners with PFP, the results cannot be generalized to other populations or sport activities. In addition, we focused only on chronic PFP. Nevertheless, our participants had similar characteristics as patients who typically seek clinical care. Although we reported pain medication use, we did not directly measure pain medication use before and during the investigation. In future work, researchers should control for pain medication use because it may affect study outcomes. Indeed, evidence indicated that patients who suffered from depression and anxiety reported more intense pain and that these relationships were bidirectional.33,34 Patients with depression and anxiety have the tendency to engage in catastrophizing. Pain-based catastrophizing has prospectively predicted pain, pain acceptance has predicted less pain-related distress, and engagement in activity predicted less depression.35 Thus, an exercise therapy program that integrates mindfulness is likely to affect catastrophizing and pain perception, and the patient's mental health should be considered to achieve a more effective recovery. At the beginning of the study, no participants described receiving regular meditation or yoga training. However, we did not request information about their history of engagement in such programs. Future researchers should examine any history of participation in meditation and yoga as an inclusion or exclusion criterion. According to the sport psychologist, almost all participants were satisfied and eager to participate in mindfulness training. Yet we did not directly measure participant satisfaction with the class; this factor should be addressed by future authors. Previous investigators36 suggested that as the amount of contact or social support available from health professionals or other exercise participants in a group-based intervention increases, so do the beneficial effects of the intervention. Accordingly, we administered both interventions (ie, exercise training and mindfulness training) in a group setting. Therefore, participants in both experimental groups received social support. Nevertheless, 1 group received only 1 intervention, whereas the other group received both interventions. Hence, the extent to which participants received different amounts of social support might have influenced the results; this limitation can be overcome in subsequent studies by including a placebo intervention in a group approach. Another limitation of our evaluation was that the exercise sessions were long and so not easily applied to most clinical practice settings in which recreational runners are treated for injuries. Programs that are more easily translated into practice settings should be considered in future work. We excluded a large number of volunteers (n = 98), potentially raising concerns about selection bias. Still, this concern was attenuated by the fact that participants were screened and enrolled by an independent physiotherapist who was blinded to their allocation to the experimental conditions and the research goals.
CONCLUSIONS
Adding mindfulness practice to exercise therapy might reduce knee pain intensity, fear of movement, and pain catastrophizing and improve knee function in runners with PFP. Moreover, it might result in pain relief, quicker onset of therapeutic effects, and longer-lasting effects than exercise therapy alone and without the harmful side effects associated with current pharmacologic treatments. Therefore, we recommend that mindfulness practice be used as an adjunct to exercise therapy in PFP rehabilitation programs.
Supplementary Material
REFERENCES
- 1.Lopes AD, Hespanhol LC, Yeung SS, Costa LOP. What are the main running-related musculoskeletal injuries? Sports Med. 2012;42(10):891–905. doi: 10.1007/BF03262301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839–843. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Witvrouw E, Callaghan MJ, Stefanik JJ, et al. Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013. Br J Sports Med. 2014;48(6):411–414. doi: 10.1136/bjsports-2014-093450. [DOI] [PubMed] [Google Scholar]
- 4.Thomeé R, Renström P, Karlsson J, Grimby G. Patellofemoral pain syndrome in young women: I. A clinical analysis of alignment, pain parameters, common symptoms and functional activity level. Scand J Med Sci Sports. 1995;5(4):237–244. [PubMed] [Google Scholar]
- 5.Doménech J, Sanchis-Alfonso V, Espejo B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2295–2300. doi: 10.1007/s00167-014-2968-7. [DOI] [PubMed] [Google Scholar]
- 6.Domenech J, Sanchis-Alfonso V, López L, Espejo B. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1562–1568. doi: 10.1007/s00167-012-2238-5. [DOI] [PubMed] [Google Scholar]
- 7.Mansfield CB, Selhorst M. The effects of fear-avoidance beliefs on anterior knee pain and physical therapy visit count for young individuals: a retrospective study. Phys Ther Sport. 2018;34:187–191. doi: 10.1016/j.ptsp.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Smith BE, Moffatt F, Hendrick P, et al. The experience of living with patellofemoral pain–loss, confusion and fear-avoidance: a UK qualitative study. BMJ Open. 2018;8(1):e018624. doi: 10.1136/bmjopen-2017-018624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piva SR, Fitzgerald GK, Wisniewski S, Delitto A. Predictors of pain and function outcome after rehabilitation in patients with patellofemoral pain syndrome. J Rehabil Med. 2009;41(8):604–612. doi: 10.2340/16501977-0372. [DOI] [PubMed] [Google Scholar]
- 10.Rathleff MS, Rasmussen S, Olesen JL. Unsatisfactory long-term prognosis of conservative treatment of patellofemoral pain syndrome [in Danish] Ugeskr Laeger. 2012;174(15):1008–1013. [PubMed] [Google Scholar]
- 11.Desbordes G, Gard T, Hoge EA, et al. Moving beyond mindfulness: defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness (N Y) 2015;6(2):356–372. doi: 10.1007/s12671-013-0269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stahl B, Goldstein E. A MindfulnessBased Stress Reduction Workbook. New Harbinger Publications; 2010. [Google Scholar]
- 13.Arvinen-Barrow M, Walker N. The Psychology of Sport Injury and Rehabilitation. Routledge; 2013. [Google Scholar]
- 14.Garland E, Gaylord S, Park J. The role of mindfulness in positive reappraisal. Explore (NY) 2009;5(1):37–44. doi: 10.1016/j.explore.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lange K, Gorbunova A, Christ O. The influence of mindfulness on different aspects of pain perception and affective reactivity to pain-feasibility of a multimethodical approach. Mindfulness (N Y) 2012;3(3):209–217. doi: 10.1007/s12671-012-0113-6. [DOI] [Google Scholar]
- 16.Schütze R, Rees C, Preece M, Schütze M. Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain. 2010;148(1):120–127. doi: 10.1016/j.pain.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 17.Baldon Rde M, Serrão FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(4):240–251. doi: 10.2519/jospt.2014.4940. [DOI] [PubMed] [Google Scholar]
- 18.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chesworth BM, Culham E, Tata GE, Peat M. Validation of outcome measures in patients with patellofemoral syndrome. J Orthop Sports Phys Ther. 1989;10(8):302–308. doi: 10.2519/jospt.1989.10.8.302. [DOI] [PubMed] [Google Scholar]
- 20.Salavati M, Mazaheri M, Negahban H, et al. Validation of a Persian-version of Knee injury and Osteoarthritis Outcome Score (KOOS) in Iranians with knee injuries. Osteoarthritis Cartilage. 2008;16(10):1178–1182. doi: 10.1016/j.joca.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 22.French DJ, France CR, Vigneau F, French JA, Evans RT. Fear of movement/(re) injury in chronic pain: a psychometric assessment of the original English version of the Tampa scale for kinesiophobia (TSK) Pain. 2007;127(1–2):42–51. doi: 10.1016/j.pain.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–532. doi: 10.1037/1040-3590.7.4.524. [DOI] [Google Scholar]
- 24.Robinson ME, Riley JL, III, Myers CD, et al. The coping strategies questionnaire: a large sample, item level factor analysis. Clin J Pain. 1997;13(1):43–49. doi: 10.1097/00002508-199703000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Esculier JF, Bouyer LJ, Dubois B, et al. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain? A randomised clinical trial. Br J Sports Med. 2018;52(10):659–666. doi: 10.1136/bjsports-2016-096988. [DOI] [PubMed] [Google Scholar]
- 26.Baechle TR, Earle RW. Essentials of Strength Training and Conditioning. Human Kinetics; 2008. 3rd ed. [Google Scholar]
- 27.Willy RW, Meardon SA, Schmidt A, Blaylock NR, Hadding SA, Willson JD. Changes in tibiofemoral contact forces during running in response to in-field gait retraining. J Sports Sci. 2016;34(17):1602–1611. doi: 10.1080/02640414.2015.1125517. [DOI] [PubMed] [Google Scholar]
- 28.Roper JL, Harding EM, Doerfler D, et al. The effects of gait retraining in runners with patellofemoral pain: a randomized trial. Clin Biomech (Bristol Avon) 2016;35:14–22. doi: 10.1016/j.clinbiomech.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 29.Kabat-Zinn J. Mindfulness-based stress reduction (MBSR) Constructivism Human Sci. 2003;8(2):73–107. [Google Scholar]
- 30.Lee AC, Harvey WF, Price LL, Morgan LPK, Morgan NL, Wang C. Mindfulness is associated with psychological health and moderates pain in knee osteoarthritis. Osteoarthritis Cartilage. 2017;25(6):824–831. doi: 10.1016/j.joca.2016.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rainville J, Smeets RJ, Bendix T, Tveito TH, Poiraudeau S, Indahl AJ. Fear-avoidance beliefs and pain avoidance in low back pain—translating research into clinical practice. Spine J. 2011;11(9):895–903. doi: 10.1016/j.spinee.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Vlaeyen JWS, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016;157(8):1588–1589. doi: 10.1097/j.pain.0000000000000574. [DOI] [PubMed] [Google Scholar]
- 33.Michaelides A, Zis P. Depression, anxiety and acute pain: links and management challenges. Postgrad Med. 2019;131(7):438–444. doi: 10.1080/00325481.2019.1663705. [DOI] [PubMed] [Google Scholar]
- 34.Woo AK. Depression and anxiety in pain. Rev Pain. 2010;4(1):8–12. doi: 10.1177/204946371000400103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Noyman-Veksler G, Lerman SF, Joiner TE, et al. Role of pain-based catastrophizing in pain, disability, distress, and suicidal ideation. Psychiatry. 2017;80(2):155–170. doi: 10.1080/00332747.2016.1230984. [DOI] [PubMed] [Google Scholar]
- 36.Burke SM, Carron AV, Eys MA, Ntoumanis N, Estabrooks PA. Group versus individual approach? A meta-analysis of the effectiveness of interventions to promote physical activity. Sport Exerc Psychol Rev. 2006;2(1):19–35. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.