Abstract
Background
Patellofemoral pain (PFP) has high recurrence rates and minimal long-term treatment success. Central sensitization refers to dysfunctional pain modulation that occurs when nociceptive neurons become hyperresponsive. Researchers in this area of PFP have been increasingly productive in the past decade.
Objective
To determine whether evidence supports manifestations of central sensitization in individuals with PFP.
Data Sources
We searched MeSH terms for quantitative sensory testing (QST) pressure pain thresholds (PPTs), conditioned pain modulation (CPM), temporal summation, sensitization, hyperalgesia, and anterior knee pain or PFP in PubMed, SPORTDiscus, CINAHL, Academic Search Complete, and EBSCOhost.
Study Selection
Peer-reviewed studies that were written in English and published between 2005 and 2020 and investigated QST or pain mapping in a sample with PFP were included in this review.
Data Extraction
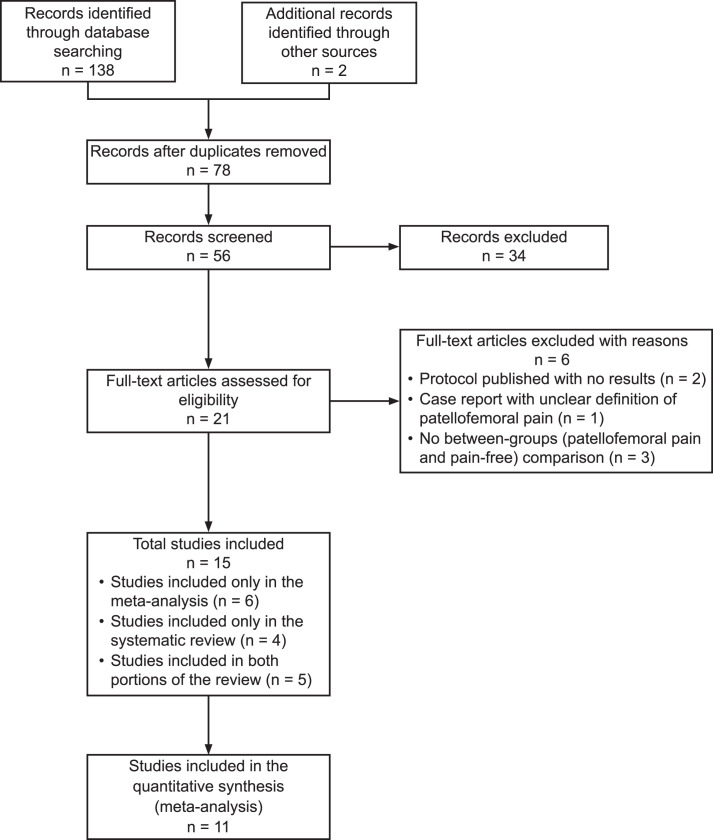
The initial search yielded 140 articles. After duplicates were removed, 78 abstracts were reviewed. The full text of 21 studies was examined, and we included 15 studies in our evaluation: 6 in the meta-analysis, 4 in the systematic review, and 5 in both the meta-analysis and systematic review.
Data Synthesis
A random-effects meta-analysis was conducted for 4 QST variables (local PPTs, remote PPTs, CPM, temporal summation). Strong evidence supported lower local and remote PPTs, impaired CPM, and facilitated temporal summation in individuals with PFP compared with pain-free individuals. Evidence for heat and cold pain thresholds was conflicting. Pain mapping demonstrated expanding pain patterns associated with long duration of PFP symptoms.
Conclusions
Signs of central sensitization were present in individuals with PFP, indicating altered pain modulation. The etiologic and treatment models of PFP should reflect the current body of evidence regarding central sensitization. Signs of central sensitization should be monitored clinically, and treatments with central effects should be considered as part of a multimodal plan of care.
Keywords: anterior knee pain, pain sensitization, hyperalgesia
Key Points
Pain persistence in patients with patellofemoral pain may be the result of central sensitization.
Individuals with patellofemoral pain demonstrated altered pressure pain thresholds, central pain inhibition, and central pain facilitation compared with pain-free individuals.
Clinicians should incorporate quantitative sensory tests into the examination process to track improvement over time.
Patellofemoral pain (PFP) is a musculoskeletal pain condition affecting an estimated 25% of the population and is >2 times more prevalent in females.1–3 A long duration of symptoms is a consistent predictor of poor treatment outcomes for individuals with PFP.4–6 Currently accepted etiologic theory suggests that pathomechanics of the hip, knee, or foot and ankle lead to elevated patellofemoral joint loading, which drives nociception and pain.7 Treatment strategies aimed at correcting observed pathomechanics or reducing patellofemoral joint loading have led to short-term pain relief; however, pain persists in >50% of patients at follow ups ranging from 1 to 8 years,8–12 and PFP is recurrent in 70% to 90% of patients.13 Whereas pathomechanics are one hypothetical factor in the development of PFP, researchers14 studying other chronic musculoskeletal conditions have demonstrated the importance of central sensitization in the development of chronic pain.
Central sensitization has been defined by the International Association for the Study of Pain as “increased responsiveness of nociceptive neurons in the central nervous system.”15 Hallmarks of central sensitization include pain in the presence of a non-noxious stimulus (allodynia), pain hypersensitivity at the affected site (primary hyperalgesia), increased receptive fields, and pain hypersensitivity in uninjured tissues beyond the affected area (secondary hyperalgesia).16 The presence of central sensitization is especially important when providing health care to patients with chronic musculoskeletal pain, as it may guide treatment selection.17
Quantitative sensory testing (QST) is a test battery for assessing the state of endogenous pain facilitation and inhibition.14,18 It has been used to demonstrate altered somatosensory function in patient populations or subgroups (eg, those with low back pain, knee osteoarthritis),19,20 predict treatment response,21–24 and guide treatment selection.16,17,25 Pressure pain thresholds (PPTs), conditioned pain modulation (CPM), temporal summation of pain, and temperature pain and detection thresholds are all forms of QST.14,18
Pain thresholds represent the minimum stimulus (pressure, thermal, or electrical) that is perceived as painful.14 Pressure pain thresholds are commonly used QST techniques and involve a mechanical stimulus (eg, pressure algometer or cuff algometer),14 whereas thermal pain thresholds involve heat and cold stimuli.26 Lower pain thresholds at the affected site (eg, the knee) indicate local pain hypersensitivity and reduced nociceptive thresholds in the peripheral nervous system. Lower pain thresholds remote to the affected site (eg, upper limb for a lower extremity condition) indicate widespread pain hypersensitivity and reduced nociceptive neuron thresholds in the central nervous system.14,18,27,28
Conditioned pain modulation is the concept that “pain inhibits pain” and assesses the integrity of central pain inhibition.14,16,18 During a CPM protocol, pain from a noxious stimulus (test stimulus) is decreased by a second noxious stimulus (conditioning stimulus).14,29 If there is minimal or no change in the perceived pain of the test stimulus with the conditioning stimulus, CPM is considered impaired. A reduced CPM response indicates less effective descending pain inhibition and is a manifestation of central sensitization.16
Temporal summation of pain assesses the efficiency of central pain facilitation.14 To assess temporal summation, changes in pain perception over time are recorded during a sustained or repeated stimulus at a constant noxious intensity.18 Increased pain reports over time indicate central sensitization.14 Temporal summation can be measured using a variety of stimuli, ranging from the application of heat or cold pain to punctate temporal summation, which uses a repetitive pinprick test or monofilament application.14,18 Facilitated temporal summation indicates enhanced central pain facilitation.16
Widespread pain is also indicative of dysfunctional peripheral or central pain modulation.16 Pain maps allow patients to self-report the pain location and provide objective measures of the pain area. Spreading of a painful area beyond the affected body part (ie, the knee) or an increased number of painful sites may indicate widespread pain.16,18
In a systematic review, De Oliveira Silva et al30 assessed the characteristics of pain sensitization in patients with chronic knee conditions. Moderate evidence supported hyperalgesia at the knee and upper limb in patients with PFP, indicating peripheral or central sensitization, respectively. Researchers in this area have been productive recently, and synthesis of these additional studies may provide further insight into central changes that occur in individuals with PFP, which may guide treatment decisions. Signs of central sensitization are neglected in current etiologic or treatment models of PFP. Treatment plans focusing on strengthening and movement quality alone may not address a key component contributing to pain persistence. Therefore, the question guiding this review was, “Do individuals with PFP exhibit signs of central sensitization compared with healthy, pain-free individuals?”
METHODS
Search Strategy
This systematic review was registered with PROSPERO (Registration No. CRD42019127548) and was prepared according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We searched MeSH terms for studies using QST methods and pain mapping in individuals with PFP in the PubMed, SPORTDiscus, CINAHL, Academic Search Complete, and EBSCOhost databases (Supplementary Table). The search took place between November 2018 and February 2019 and was repeated in June 2020. Studies were included if they were published in English in the past 15 years, included at least 1 QST or pain mapping measure in human participants, and included a between-subjects (PFP versus pain-free control) comparison for QST (or cross-sectional data for pain mapping).
Review Process
One researcher (K.J.S.) conducted the search across databases and exported all potential studies to EndNote X8 (Clarivate Analytics) for cross-referencing. The process of article screening and review is outlined in Figure 1. Two researchers (K.J.S., J.E.E.B.) independently reviewed titles and abstracts for inclusion. No conflicts needed to be resolved at this stage. Full-text copies of the included articles were screened. Fifteen total studies were included, with 11 studies accepted for the meta-analysis and 9 for the systematic review. Two reviewers (K.J.S., M.K.H.B.) independently conducted a quality review using the modified Downs and Black checklist.31 The reviewers first discussed any scoring differences, and a plan was in place to have a third reviewer resolve any disputes. No differences required third-party resolution.
Figure 1.
Flowchart of search.
Data Extraction
We extracted the following information: publication information (author, year, study design, journal), number of participants, participant characteristics (age, sex, any grouping variables and characteristics), and outcome measures from QST variables (means and SDs or CIs). When CIs were reported instead of SDs, we converted them to SDs. Data not presented in the full text of articles or supplementary data files were requested from 2 primary authors, who provided these values or data files.
Quality Assessment
The modified Downs and Black checklist was selected for quality assessment based on the expectation that most studies would have cross-sectional designs.32 The modified Downs and Black checklist has a total of 16 scored items across 5 categories (reporting, external validity, internal validity [bias, internal validity], confounding, and power).32,33 The maximum score is 17, with 15 items scored from 0 to 1 point, and 1 item scored from 0 to 2 points, where 0 indicates lower quality and higher numbers indicate higher quality.
Risk of Bias and Publication Bias
Risk of bias was assessed using the Cochrane risk of bias tool in RevMan 5.0 (Cochrane). Publication bias was assessed using RevMan 5.0 for homogeneous groups of studies.
Data Synthesis and Analysis
A random-effects meta-analysis was conducted for QST variables with ≥3 studies (local PPTs, remote PPTs, and CPM) using RevMan 5.0. For all other variables, too few authors of studies used similar methods to pool data. A moderator analysis was conducted for local and remote PPTs. We report the standardized mean differences (SMDs) with 95% CIs, χ2 statistics, τ values, I2 values, and results for the overall effect.
Studies for which meta-analysis was not possible are described qualitatively using means and SDs or medians and interquartile ranges when appropriate. Strength of evidence is described using the criteria of van Tulder et al34 for the levels of evidence, which categorize studies based on statistical homogeneity (Table 1). Subgroup analyses were conducted after initial review of the evidence and when heterogeneity of pooled results was observed. Moderator analysis was selected because there were too few studies per outcome variable to properly power a meta-regression and allow appropriate interpretation of results.35
Table 1.
Description of Criteria of van Tulder et al34
| Criterion |
Description |
| Strong | Data pooled from ≥3 studies |
| Minimum of 2 high-quality homogeneous studies | |
| Result may be statistically significant or nonsignificant | |
| Moderate | Statistically significant pooled results from multiple heterogeneous studies |
| Includes 1 high-quality study or multiple low-quality homogeneous studies | |
| Limited | Statistically heterogeneous results from 1 high-quality study or multiple low-quality studies |
| Very limited | Results from 1 low-quality study |
| Conflicting | Pooled results that are nonsignificant |
| Results derived from multiple statistically heterogeneous studies, regardless of quality |
RESULTS
Study Characteristics
A total of 15 studies were included in this review: 6 in the meta-analysis only,37–39,41,42,44 4 in the systematic review only,45–48 and 5 in both portions of the review.27,28,36,40,43 Eleven evaluated PPTs at the knee,27,28.36–44 10 assessed PPTs at a remote site,27,28,36–41,43,44 5 assessed CPM,27,36,40,43,44 4 evaluated temporal summation36,40,43,44 3 evaluated heat and cold pain thresholds,43,45,46 and 6 used pain-mapping techniques.27,28,36,40,47,48 A total of 14 investigations were cross-sectional, and 1 was a cohort study. For the cohort study,44 only cross-sectional between-groups baseline data were extracted for data analysis, as the aim of our review was not to determine treatment effects. Study and participant characteristics are described in Table 2, and quality scores are provided in Table 3.
Table 2.
Study Characteristics Extended on Next Page
| Study |
Participants, No. (age, y, mean ± SD or median [IQR]) |
PFP Symptom Duration, mo, Mean ± SD or Median (IQR) |
Patient-Reported Outcome Score, Mean ± SD or Median |
| Boudreau et al47 (2017) | 35 with PFP (18.8 ± 1.7): 2 males, 33 females | 60 ± 33 | NR |
| Boudreau et al48 (2018) | 299 with PFP: 126 males (23.1 ± 8.2), 173 females (19.1 ± 8.2) | 24 (12–48) | NR |
| Holden et al36 (2018) | 65 females: 36 with PFP (22.8 ± 1.1), 29 CON (23.1 ± 1.2) | 96 (84–120) | KOOS-Symptoms: 71 ± 16; KOOS-Pain: 67 ± 13; KOOS-ADL: 78 ± 13; KOOS-Sport and Recreation: 48 ± 21; KOOS-Quality of Life: 51 ± 21 |
| Holden et al44 (2020) | 201 total: 151 with PFP (36 males, 115 females; 12 ± 1.2), 50 pain-free (19 males, 31 females; 12.3 ± 1.4) | 18 (9–24) | KOOS-Symptoms: 78.2 ± 12.2; KOOS-Pain: 68.5 ± 1.2; KOOS-ADL: 79 ± 14.3; KOOS-Sport and Recreation: 55.3 ± 21.2; KOOS-Quality of Life: 49.3 ± 15.5 |
| Jensen et al45 (2007) | 48 total: 25 with unilateral PFP (9 males, 16 females; 32 [19–44]), 23 healthy (11 males, 12 females; 29 [18–44]) | 74 (12–260) | NR |
| Jensen et al46 (2008) | 114 total: 91 with unilateral PFP (56 males, 35 females; 31.2), 23 healthy (11 males, 12 females; 29) | 70 (3–240) | Cincinnati Rating Scale: 66 |
| Maclachlan et al43 (2020) | 211 total: 150 with PFP (53 males, 97 females; 32.1), 61 CON (24 males, 37 females; 32.6) | <6: 7.4%; 6–12: 3.3%; 13–60: 37.3%; 60–120: 20.7%; >120: 31.3% | AKPS: 72.5 ± 12; KOOS-Symptoms: 78.4 ± 12.5; KOOS-Pain: 75.8 ± 12.9; KOOS-ADL: 85.7 ± 13.5; KOOS-Sport and Recreation: 65.8 ± 19.7; KOOS-Quality of Life: 51.9 ± 20.5; KOOS-PF: 61.8 ± 17.9 |
| Noehren et al37 (2016) | 40 females: 20 with PFP (23.2 ± 5.6), 20 CON (22.7 ± 5.0) | 40.8 ± 52.8 | NR |
| Pazzinatto et al38 (2016) | 71 female runners: 38 with PFP (21.6 ± 2.6), 33 asymptomatic CON (22.4 ± 3.5) | 62.3 ± 46.1 | NR |
| Pazzinatto et al39 (2017) | 40 female runners: 20 with PFP (25.62 ± 4.05), 20 asymptomatic CON (27 ± 5.58) | 37.7 ± 49.3 | AKPS: 80.45 |
| Rathleff et al28 (2013) | 79 female adolescents: 57 with PFP (17.13 ± 1.1), 22 CON (17.1 ± 0.9) | 34 (18–51) | KOOS-Symptoms: 97.7 ± 3; KOOS-Pain: 99.7 ± 1.2; KOOS-ADL: 99.9 ± 0.3; KOOS-Sport and Recreation: 99.5 ± 1.5; KOOS-Quality of Life: 99.1 ± 2.1 |
| Rathleff et al40 (2016) | 40 females: 20 with PFP (20 [19–21]), 20 CON (20.5 [20–21]) | 72 (4.5–7) | KOOS-Symptoms: 96 ± 5; KOOS-Pain: 99 ± 2; KOOS-ADL: 100 ± 1; KOOS-Sport and Recreation: 98 ± 3; KOOS-Quality of Life: 97 ± 7 |
| Rathleff et al27 (2017) | 65 total: 33 with PFP (10 males, 23 females; 28.5 ± 5.3), 32 CON (10 males, 23 females; 27.1 ± 5.2) | 24 (14–60) | NR |
| van der Heijden et al42 (2015) | 38 (12 males, 26 females): 22 with PFP (22 ± 5.8), 16 CON (22.5 ± 6.5) | 12 ± 6.5 | NR |
| van der Heijden et al41 (2018) | 134 adults and adolescents (60 males, 74 females): 64 with PFP (35 female, 29 males; 44 adults, 20 adolescents; 23.4 ± 7), 70 CON (41 females, 29 males; 50 adults, 20 adolescents; 23.1 ± 5.9) | Adults: 11 ± 6.4; Adolescents: 14.2 ± 8.1; Females: 13.7 ± 6.8; Males: 9.9 ± 7.1 | AKPS: 66.3 ± 11.6 |
Abbreviations: AKPS, Anterior Knee Pain Scale; CON, control; CPM, conditioned pain modulation; CPT, cold pain threshold; HPT, heat pain threshold; IPAQ, International Physical Activity Questionnaire; IQR, Interquartile range; KOOS, Knee Osteoarthritis Outcome Score; NR, not reported; NRS, numeric rating scale; PF, Patellofemoral subscale; PFP, patellofemoral pain; PM, pain mapping; PPT, pressure pain thresholds; QST, quantitative sensory testing; TSP, temporal summation of pain; VAS, visual analog scale.
Pain intensity was measured on either a 10-cm VAS or an NRS with a maximum score of 10.
Table 2.
Extended From Previous Page
| Body Mass Index, Mean |
Physical Activity Level |
Pain Intensity, Mean ± SD or Median (IQR)a |
Type of QST |
Summary of Findings |
| NR | NR | VAS current: 4.8 ± 2.7 | PM | PM: Most patients reported peripatellar pain, less than half reported combined retropatellar and peripatellar pain, and 1 reported retropatellar pain. Patients with symptoms >5 y demonstrated larger pain area than did those with symptoms of <5 y. Most patients reported symmetric bilateral pain. Longer symptom duration was related to spreading of pain up the thigh and down the leg. |
| NR | NR | VAS worst: 5.0 (3.3–7.0) | PM | PM: No sex differences in pain clusters or distributions. Longer symptom duration was associated with bilateral PFP. Longer symptom durations were related to larger pain area and specific pain patterns, including pain up the thigh and down the lower leg. Pain intensity was not related to pain area. |
| PFP group: 24.1; CON group: 22.7 | NR | NRS current: 2.0 ± 2.0; NRS worst previous 4 wk: 7.0 ± 2.0; NRS average previous 4 wk: 4.0 ± 1.0 | PPTs, TSP, CPM, PM | Local PPTs: PFP group < CON group (center of patella). Remote PPT: PFP group < CON group (elbow). TSP: PFP group > CON group (cuff algometry). CPM: PFP group = CON group (cuff algometry). PM: Most of PFP group reported pain in an area in addition to the knee, and 21% of PFP group met American College of Rheumatology criteria for widespread pain. |
| NR | NR | NRS worst previous wk: 6.6 ± 2.2 | PPTs, CPM, TSP | Local PPTs: PFP group < CON group (center of patella). Remote PPTs: PFP group < CON group (elbow). CPM: PFP group < CON group (cuff algometry). TSP: PFP group > CON group (cuff algometry). |
| PFP group: 23.8; CON group: 23.4 | NR | VAS current: 2.4 (SD NR); VAS worst: 5.5 (SD NR) | HPT, CPT | HPT: PFP group = CON group. CPT: PFP group = CON group. |
| PFP group: 23.4; CON group: 23.1 | NR | NR | HPT, CPT | HPT: PFP group = CON group. CPT: PFP group = CON group. Other: 32% of participants with PFP did not achieve CPT before cold limit (1°C). 15 With PFP reported heat sensation with CPT testing. |
| PFP group: 25.2; CON group: 24.0 | Weekly activity level (IPAQ): PFP group, 4849.2; CON group, 3191.7 | VAS worst: 5.4 ± 1.6 | PPTs, TSP, CPM, HPT, CPT | Local PPTs: PFP group < CON group (center of patella). Remote PPTs: PFP group < CON group (elbow). TSP: PFP group > CON group (pinprick test). CPM: PFP group = CON group (cold pressor test). HPT: PFP group < CON group. CPT: PFP group < CON group. |
| NR | NR | NRS current: 5.8 ± 2.0 | PPTs | Local PPTs: PFP group < CON group (patellar tendon). Remote PPTs: PFP group < CON group (elbow). |
| NR | NR | NR | PPTs | Local PPTs: PFP group < CON group (lateral to the patella). Remote PPTs: PFP group < CON group (elbow). |
| NR | Distance run per week: PFP group, 19.75 km; CON group, 20.75 km | VAS current: 1.2 ± 1.5; VAS worst previous mo: 4.8 ± 1.5 | PPTs | Local PPTs: PFP group < CON group (center of patella). Remote PPTs: PFP group < CON group (elbow). |
| PFP group: 20.5; CON group: 21.4 | NR | VAS worst: 5.0 (3.8–6.8); VAS current: 1.3 (0.3–2.7) | PPTs, PM | Local PPTs: PFP group < CON group (center of patella). Remote PPTs: PFP group < CON group (tibialis anterior). PM: Majority of PFP group reported bilateral pain that was peripatellar and diffuse. |
| NR | Sport participation: PFP group, 80%; CON group, 75% | NR | PPTs, TSP, CPM, PM | Local PPTs: PFP group < CON group (center of patella). Remote PPTs: PFP group < CON group (elbow). TSP: PFP group = CON group (cuff algometry). CPM: PFP group < CON group (cuff algometry). PM: Most participants with PFP reported peripatellar pain that included spreading pain up the thigh. |
| PFP group: 24.2; CON group: 21.9 | NR | NRS worst previous wk: 5.0 (3.0–7.0) | PPTs, CPM, PM | Local PPTs: No difference between PFP and CON groups (center of patella). Remote PPTs: No difference between PFP and CON groups (elbow). CPM: PFP = CON group (cold-pressor test). PM: Most participants with PFP reported retropatellar pain and combined retropatellar and peripatellar pain. One reported only peripatellar pain. |
| PFP group: 23.9; CON group: 23.3 | Sport participation: PFP group, 54.5%; CON group, 81.3% | NRS current: 4.7 ± 2.3 | PPTs | Local PPTs: PFP group < CON group (center of patella). |
| PFP group: 23.6; CON group: 22.3 | Sport participation: PFP group, 38%; CON group, 55% | NRS current: 4.7 (SD NR) | PPT | Local PPTs: PFP group < CON group (most painful location). Remote PPTs: PFP group < CON group (forearm). Other: age did not affect PPTs. Lower PPTs for females versus males for bilateral knees and the contralateral arm. Sex modified effect size between PFP and CON groups. |
Table 3.
Quality Review Based on Modified Downs and Black Scores33
| Study |
Score (No./17) |
Quality |
| Boudreau et al47 (2017) | 13 | High |
| Boudreau et al48 (2018) | 14 | High |
| Holden et al36 (2018) | 14 | High |
| Holden et al44 (2020) | 16 | High |
| Jensen et al45 (2007) | 9 | Low |
| Jensen et al46 (2008) | 8 | Low |
| Maclachlan et al43 (2020) | 14 | High |
| Noehren et al37 (2016) | 12 | Moderate |
| Pazzinatto et al38 (2016) | 12 | Moderate |
| Pazzinatto et al39 (2017) | 10 | Moderate |
| Rathleff et al28 (2013) | 13 | High |
| Rathleff et al40 (2016) | 13 | High |
| Rathleff et al27 (2017) | 15 | High |
| van der Heijden et al42 (2015) | 10 | Moderate |
| van der Heijden et al41 (2018) | 12 | Moderate |
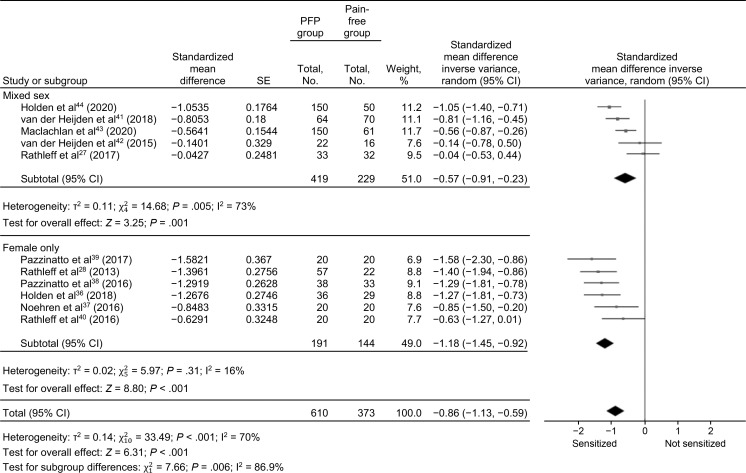
Strong evidence (n = 983) from 6 high-quality27,28,36,40,43,44 and 5 moderate-quality37–39,41,42 studies supported a large SMD (−0.86; 95% CI = −1.13, −0.59; Figure 2) that was different in local (knee) PPTs between individuals with PFP and healthy, pain-free control individuals. A post hoc subgroup analysis was conducted to explore the effect of sex (female-only studies versus mixed-sex studies) on local PPTs. Subgroup analysis demonstrated maintained heterogeneity (I2 = 73% and 16%, respectively; Figure 2) and differences (P ≤ .001 for each subgroup).
Figure 2.
Meta-analysis results of local pressure pain thresholds. a Abbreviation: PFP, patellofemoral pain.
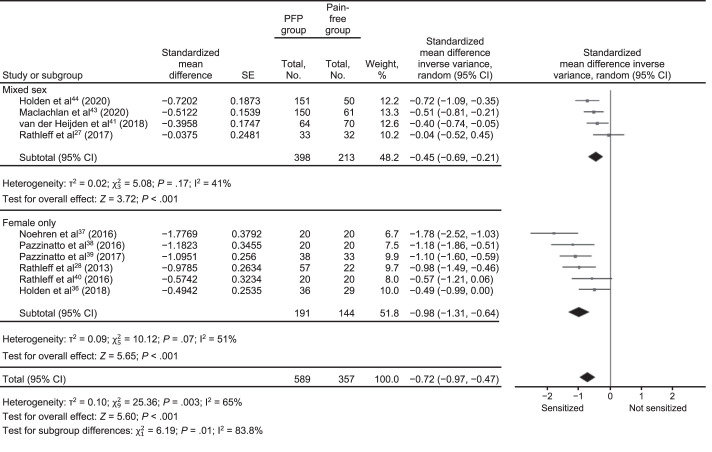
Strong evidence (n = 946) from 6 high-quality27,28,36,40,43,44 and 4 moderate-quality37–39,41 studies was observed for a moderate SMD that was different in remote (upper limb) PPTs between individuals with PFP and the healthy, pain-free control group (SMD = −0.72 [−0.97, −0.47]; Figure 3). We conducted a post hoc subgroup analysis to explore the effect of sex on remote PPTs. This analysis demonstrated maintained heterogeneity in mixed-sex (I2 = 41%) and female-only (I2 = 51%) cohorts and differences (P < .001 for mixed-sex and female-only studies).
Figure 3.
Meta-analysis results of remote pressure pain thresholds. a Abbreviation: PFP, patellofemoral pain.
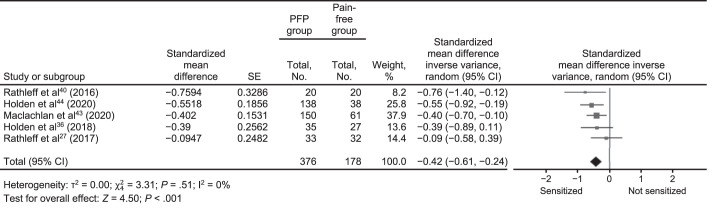
Strong evidence (n = 554) from 5 high-quality studies27,36,40,43,44 supported a small SMD (−0.42 [−0.61, −0.24]; P < .001) that was different for the CPM response between individuals with PFP and healthy, pain-free control individuals (Figure 4). Subgroup analysis (for sex or other variables) was not conducted for CPM, as no heterogeneity was present (I2 = 0%).
Figure 4.
Meta-analysis results of conditioned pain modulation. a Abbreviation: PFP, patellofemoral pain.
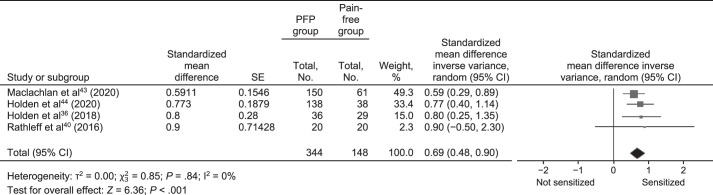
Strong evidence (n = 492) from 4 high-quality studies27,36,43,44 supported a moderate SMD (0.69 [0.48, 0.90]) that was different for the temporal summation responses between those with PFP and pain-free control individuals (Figure 5). Subgroup analysis was not conducted for CPM, as no heterogeneity existed (I2 = 0%).
Figure 5.
Meta-analysis results of remote temporal summation of pain. a Abbreviation: PFP, patellofemoral pain.
Systematic Review
We conducted a systematic review of the data that could not be pooled because of a low number of total studies or differences in methods that did not allow for pooled results. Nine studies were included in the systematic review: 3 assessed thermal pain thresholds,43,45,46 and 6 assessed pain mapping.27,28,36,40,47,48
Thermal Pain Thresholds
Conflicting evidence has been reported for heat and cold pain thresholds for participants with PFP.43,45,46 The SMDs could not be calculated because the data were not normally distributed in 1 study.46 One group43 reported a large effect size (1.2; 95% CI = 0.8, 1.63), demonstrating lower heat pain thresholds at the knee in the PFP group than in the pain-free group (n = 211), whereas another45 reported no differences between groups (n = 48).
Pain Mapping
Six high-quality studies27,28,36,40,47,48 (n = 583) provided evidence that could not be pooled because of variations in methods and reporting. Three studies27,28,40 used pain-mapping information to characterize and group the location of pain into retropatellar, peripatellar, or both, and total pain-area data were not reported. One group of researchers36 identified a higher number of painful sites with increased symptom duration in the PFP group relative to a pain-free group. Two studies47,48 demonstrated increased pain area (pixels) using a digital knee map. Distinct pain patterns associated with spreading of pain up the thigh and down the lower leg were also associated with longer symptom durations. These findings lend support for central sensitization but warrant further examination.
Risk of Bias and Publication Bias
The risk-of-bias assessment indicated that allocation concealment and adequate expression of group differences may be threats to study validity (Table 4). Only 3 investigations27,36,40 concealed group allocation from the researcher, which could have introduced researcher bias. Unpublished work in this area was not sought. This may have led to an increased risk of publication bias, regardless of our findings. A funnel plot for published studies of CPM (Figure 6) showed some asymmetry, likely due to the low number of studies (k = 5)27,36,40,43,44 and small sample sizes in each study. A funnel plot for temporal summation produced a nearly vertical line with most results on the sensitized portion of the graph, indicating the likelihood that studies with results that were different may be published more frequently (Figure 7). This bias is difficult to confirm with no data from unpublished studies, a low number of studies (k = 4),36,40,43,44 and small sample sizes. We could not assess publication bias for PPTs because of the heterogeneity observed in all meta-analysis results.35
Table 4.
Risk of Biasa
| Study |
Clear Purpose and Aim? |
Allocation Concealed? |
Unreported or Loss of Participant Data (>2 cases) |
Group Differences Reported (Mean ± SD or 95% CI) |
| Boudreau et al47 (2017) | + | NS | + | + |
| Boudreau et al48 (2018) | + | NS | − | + |
| Holden et al36 (2018) | + | + | + | + |
| Holden et al44 (2020) | + | NS | + | + |
| Jensen et al45 (2007) | + | − | − | + |
| Jensen et al46 (2008) | + | − | + | + |
| Maclachlan et al43 (2020) | + | NS | + | + |
| Noehren et al37 (2016) | + | − | + | + |
| Pazzinatto et al38 (2016) | + | − | − | + |
| Pazzinatto et al39 (2017) | + | − | − | + |
| Rathleff et al28 (2013) | + | − | − | + |
| Rathleff et al40 (2016) | + | + | + | + |
| Rathleff et al27 (2017) | + | + | − | − |
| van der Heijden et al42 (2015) | + | − | + | + |
| van der Heijden et al41 (2018) | + | − | + | + |
Abbreviation: NS, not specified.
+ Indicates no risk of bias and − indicates risk of bias in this category.
Figure 6.
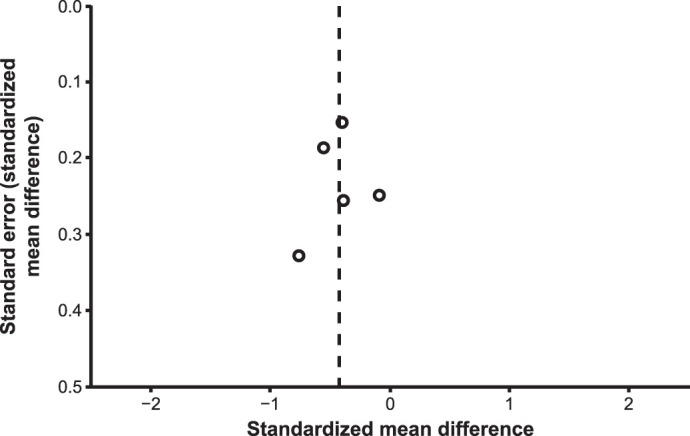
Funnel plot of results from published conditioned pain modulation studies.
Figure 7.
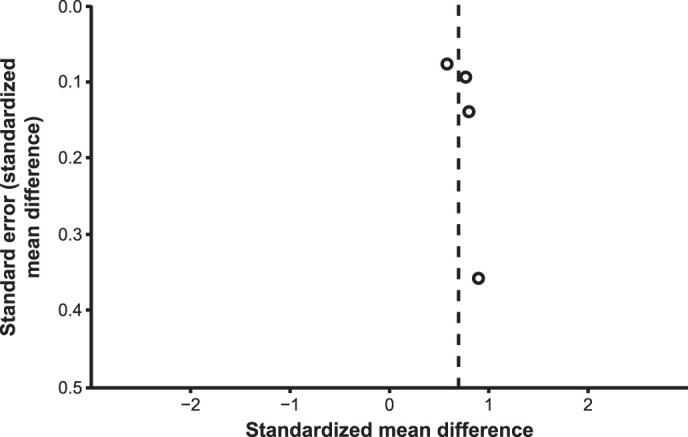
Funnel plot of results from published temporal summation of pain studies.
DISCUSSION
The purpose of our review was to determine whether the current literature supports central sensitization in individuals with PFP compared with pain-free control individuals. Our findings supplied strong support for signs of central sensitization, including lower local and remote PPTs, impaired CPM, and facilitated temporal summation in those with PFP. The evidence was conflicting regarding altered heat and cold pain thresholds in individuals with PFP. Signs of central sensitization demonstrated ineffective pain modulation in the central nervous system. Although muscle weakness and altered biomechanics may be key components of PFP development, they may not be the only sources of pain persistence. Signs of central sensitization should be monitored clinically, and treatments with central effects should be considered part of a multimodal plan of care.
Potential Mechanisms of Central Sensitization in Patients With PFP
The cause of PFP is hypothesized to be pathomechanical. Motor and biomechanical dysfunction of the hip, knee, and foot or ankle have been proposed to lead to increased patellofemoral joint loading.7 Treatments that align with this theory include movement retraining, hip and thigh strengthening, and use of corrective orthoses. Despite the efficacy of these treatments, PFP has high rates of recurrence9,12,49,50 and persistence.13 With a centrally sensitized nervous system, a pain response to subsequent patellofemoral joint loading may reflect the functional state of central neurons16 rather than the state of the kinetic chain and patellofemoral joint loading. This means that clinicians may treat the underlying movement factors but still neglect a key mechanism of pain persistence. Treating a patient with signs of central sensitization requires a multimodal treatment plan that affects central pain-modulation mechanisms.17 Clinicians would best serve patients with PFP by obtaining and tracking signs of sensitization to monitor progress.17
Participant Characteristics
Several interpersonal factors can affect central sensitization and pain perceptions.43,51 Subjective clinical measures of pain intensity, age, sex, body mass index, physical activity level, perceptions of knee function, and symptom duration may play roles in QST responses. A breakdown of consistently reported participant characteristics is given in Table 2.
Symptom duration had a wide range (3.4 months to >10 years); however, authors of 13 of the 15 studies included in the review noted mean or median symptom durations of 18 months or longer.27,28,36–40,43–48 Physical activity level was described in different units (mean weekly metabolic minutes of physical activity, kilometers of running per week, and percentage of sport participation) in 5 studies.39–43 The PFP groups reported more metabolic minutes than did the pain-free groups,43 PFP and healthy groups reported similar weekly running distances,39 and comparisons of sport participation varied by study.40,41,42 In 1 study,43 49% of the PFP group (PFP group: n = 150) indicated they stopped normal activity because of their knee pain. Body mass index was provided in 8 studies27,28,36,41–43,45,46 and was higher in the PFP group in only 1 study.41 Six investigations assessed females only,28,36–40 9 assessed mixed-sex cohorts,27,41–48 and none assessed males only.
Measures of function and pain intensity were more commonly collected (Table 2). Whereas specific scores on the Knee Osteoarthritis Outcome Score and Anterior Knee Pain Scale are not indicative of categorical function or ability, scores closer to 0 represent greater problems, and a score of 100 indicates no problems. The range of scores for the included studies was 63 to 100, which may suggest a moderate to low level of disability. Little evidence to date aligns relationships between central sensitization and perceptions of function. Researchers in 12 studies27,28,36,37,39,41–45,47,48 reported pain intensity at the time of the study (current), worst pain, or pain in the past week or month using numeric rating scales or visual analog scales.
Patellofemoral pain is a condition affecting a wide age range, from adolescents to older adults.52 Only 2 studies28,44 involved participants with a mean age of <18 years; the mean age of participants was >25 years in 5 studies.27,39,43,45,46 Some authors50,52 have contended that PFP may be a different experience for adolescents than adults and that onset in adolescence may result in persistence or recurrence in adulthood. The effect of age on QST results should continue to be explored among individuals with PFP.
Pressure and Thermal Pain Thresholds
Strong evidence supported reduced local and remote PPTs in individuals with PFP. Nine of the included studies assessed pressure algometry,27,28,36–40,43,44 and 2 studies assessed a handheld dynamometer method.41,42 We observed group differences in all but 1 investigation,27 and it may be worth noting that the mean age was older than that reported in most investigations (28.5 years). Based on our subgroup analyses, both female-only and mixed-sex studies maintained statistical heterogeneity. Sex should still be considered during analysis, as females experienced a variety of PFP symptoms and factors differently than did males,36,40,53,54 but sex alone may not be enough to explain the observed differences in PPTs.
When considered alone, lower local (knee) PPTs are manifestations of peripheral sensitization; however, when considered concurrently with reduced remote PPTs, they indicate central excitability.16,55 Some authors55 have proposed a mechanism by which local joint nociceptors may maintain central sensitization. This hypothesis offers potential explanations for findings of local and widespread hyperalgesia in patients with chronic musculoskeletal conditions.55 The authors postulated that peripheral sensitization spreads to extraterritorial regions by stimulating adjacent neurons in the dorsal horn of the spinal cord. Other researchers16,18 have supported the idea that if the central nervous system is sensitized, peripheral nociceptors will also demonstrate increased excitability due to dysfunctional descending pain modulation. Without longitudinal evidence, it is impossible to make the distinction. Regardless of the mechanism, clinical manifestations of PFP include local and remote hyperalgesia. Assessing and tracking PPTs using a handheld pressure algometer (a quick, inexpensive, and easy-to-learn option for clinicians) would help clinicians monitor progress by providing an objective measure of pain hypersensitivity.
Three studies43,45,46 assessed thermal pain thresholds, but we could not pool those data. Two groups45,46 reported no differences between heat and cold pain thresholds between groups, whereas 1 group43 observed lower thresholds for both modalities in the individuals with PFP. Remote assessment was also conducted at the elbow in 1 investigation43 and demonstrated lower thresholds for both (heat and cold) modalities in the patients with PFP. Jensen et al46 noted that 32% of participants with PFP did not achieve cold pain thresholds before reaching the maximum temperature limit. Whereas we could not include these data in the final analysis, increased cold pain thresholds may be inferred due to the lower temperatures that would have been needed to sense pain.46 This finding may also be a sign of hypoesthesia, or loss of sensation, which can manifest because of dysfunctional peripheral or central pain modulation.
Researchers37,45,46 have hypothesized that nociception may be prioritized over touch and temperature information in individuals with PFP. Hypoesthesia, or impaired tactile sensation, was seen in 3 studies37,45,46 and increased vibration thresholds in 1 study,46 supporting this notion. When assessed concurrently with central sensitization, these data may support inhibition of non-noxious sensory information while nociceptive neurons are activated to subthreshold levels. Further examination is needed to better understand the role of thermal pain findings in this population.
Conditioned Pain Modulation
A key finding in this review was strong support for impaired CPM in individuals with PFP relative to pain-free individuals.36,40,43,44 Impaired CPM represents inefficient central pain inhibition.14 The CPM paradigms can be assessed using a variety of protocols.29 Three studies included in this review used cuff algometry,36,40,44 and 2 studies assessed the cold-pressor test.27,43 Authors of 240,44 of the 3 studies that used cuff algometry reported impaired CPM in the PFP group, whereas neither of the 2 studies27,43 that used the cold-pressor test demonstrated inefficient CPM in the PFP group. This could indicate that the type of conditioning stimulus affects the results even if the measurement unit (pressure in kilopascals) is the same. In addition, the pooled data did not reflect any heterogeneity, and both investigations that used the cold-pressor test involved mixed-sex cohorts, whereas 236,40 of the 3 studies assessing cuff algometry involved only females. The SMD was small but different for impaired CPM between groups, and 327,43,44 of 5 studies involved mixed-sex samples. We recommend that sex should continue to be considered a subgrouping variable in order to better understand whether sex differences exist.
The CPM responses exist on a continuum and are associated with wide interpersonal differences.14 For this reason, identifying and tracking within-patient CPM responses can test and ensure restoration of efficient central pain modulation pathways. In other chronic musculoskeletal pain conditions, impaired CPM has been hypothesized to affect a subgroup of the overall patient population, and the same should be expected in PFP.14,18 Clinical assessment of CPM would be useful for determining individual responses and can be used to monitor descending central pain modulation.
Temporal Summation of Pain
Another key finding from this review was strong evidence36,40,43,44 for enhanced temporal summation in individuals with PFP. Enhanced temporal summation represents increased central pain facilitation. Three groups of researchers36,40,44 used cuff algometry, and 1 group43 used the pinprick test to assess temporal summation. Two sets of authors36,40 included only females with PFP, and 2 sets of authors43,44 included both males and females. All studies36,40,43,44 examined individuals with longstanding PFP symptoms (range = 4.5 months to >10 years).
Analyses of temporal summation responses differed across studies, which may have resulted in different outcomes. Rathleff et al40 used normalized visual analog scale scores from each of the 10 consecutive test intervals, Holden et al36 assessed the difference in visual analog scale averages from the last 3 intervals and the second through fourth intervals, and Maclachlan et al43 measured the maximum possible effect as a percentage between the first and worst numeric rating scale. Interestingly, Holden et al36 also observed a lower temporal summation response for individuals who had recovered from PFP compared with those who were currently symptomatic. Both PFP groups reported enhanced pain facilitation relative to the pain-free group.36 Temporal summation responses may be restored among patients with PFP, supporting the clinical relevance of these findings.17
Pain Mapping
Pain mapping can provide evidence of widespread pain. Unfortunately, only 2 pain-mapping studies47,48 involved the same methods or reported outcomes, making an analysis of pooled information difficult. Five27,28,40,47,48 of the 6 studies27,28,36,40,47,48 in this area only assessed a knee pain map, which differed among investigations, and 136 assessed pain maps for a number of painful sites. Other painful locations were the hip, pelvis, back, and neck.36,47,48 However, we were able to determine from the existing evidence that individuals with PFP may have an increased pain area or number of painful sites as symptoms persist over time.27,28,36,47,48 In fact, Boudreau et al47,48 suggested that specific pain patterns may extend beyond the knee with increased symptom duration. The observed patterns represented a broader pain area around the knee in addition to pain spreading up the thigh and down the lower leg.47,48 These results are supported by Rathleff et al,28 who noted that diffuse pain was experienced by 54% of the sample, regional pain by 30%, and local pain by only 16%. Bilateral PFP28,47,48 was more common than unilateral PFP. Bilateral PFP was also associated with longer symptom durations (median = 24 months; interquartile range = 12–60 months), and patients with bilateral pain described mirror-image pain in 56% of cases.48 Both neural and immune factors have been hypothesized to cause mirror-image pain patterns, and this finding is commonly attributed to central sensitization, especially if the original pain was unilateral.56 In the data presented, whether the original onset of pain was bilateral, mirror image, or unilateral was not indicated, but this aspect would be an interesting addition to the pain-mapping research in patients with PFP.
Although pain maps limited to the knee can provide useful information on localized pain, widespread pain may be better portrayed on bilateral lower extremity or whole-body maps. To improve our understanding of the effect that expanding pain areas have on individuals with PFP, consistency in analyzing and reporting these data is important. Pain spreading beyond the knee and mirror-image bilateral pain offer support for central sensitization.
Risk of Bias and Publication Bias
Our assessment of the risk of bias suggested that more studies in which group allocation is concealed from the researcher are needed. We could not properly evaluate publication bias because of the lack of homogeneity in results and a lack of data regarding unpublished or prepublication studies. This information may be useful in drawing meaningful conclusions and extrapolating the results of this review to the population with PFP.
Clinical Relevance
Although exploration of treatment effects was beyond the scope of our review, central pain modulation has been effectively restored using interventions with known central effects. These treatment options include transcutaneous electrical nerve stimulation, manual therapy, pain education, and exercise therapy. Thus far, few researchers have explored the effectiveness of these interventions in patients with PFP. Given the hypothesized pathomechanical cause of the condition, it is necessary to determine whether central sensitization has any effect on or relation to observed movement or motor dysfunction. Without that information, a multimodal patient-centered treatment approach may offer the best opportunity for long-term symptom relief. If restoration of central pain modulation, pain control, or coping can occur, then movement retraining and exercise therapy may be more effective than using any of the aforementioned interventions alone.
Central sensitization mechanisms may reflect a subgroup of patients with PFP. In this case, it would be important to screen patients individually in order to select a treatment program that accounts for central changes. In addition, QST can be tracked over time to determine whether selected treatment approaches effectively restore normal central pain modulation.
A variety of QST protocols and methods can be applied clinically. One example is handheld algometers, which are an affordable clinical alternative to computerized algometers, although they cannot standardize the pressure delivered over time. Similarly, PPTs can be used to determine the magnitude of CPM. In this test, the CPM response is calculated by comparing PPTs before and during the application of another noxious stimulus (ie, ice immersion of an extremity). Temporal summation can be assessed via the change in reported pain intensity with repetitive application of a monofilament.
As our understanding of PFP evolves, the use of QST in the clinical environment becomes more imperative. In knee osteoarthritis (among other conditions), QST has helped to identify dysfunctional pain processing resulting from and contributing to pain perceptions.57 The QST responses also predicted analgesic responses, operative and nonoperative treatment responses in individuals with knee osteoarthritis,57 and chronic pain development.14,16,18 The outcomes of QST can guide treatment selection among options with known peripheral or central effects.17 Similar findings have not yet been reported for PFP; however, our review provides support for these endeavors.
Limitations
The main limitations of this review were the small number of studies for each QST variable and population differences among them. As discussed, personal factors (ie, age, sex, activity level) may play a role in pain perceptions during QST assessment. We were unable to identify the role of potential subgroups because of limited consistency in reported participant characteristics and inclusion of a wide variety of characteristics (ie, participants from adolescent through adulthood, both sexes). For example, we identified statistical heterogeneity for PPTs, but sex alone was not a factor that explained this finding.
Authors should continue to explore how these biopsychosocial factors influence QST to better interpret and apply these findings. The main risk of bias across studies was the lack of allocation concealment. Future investigators should blind researchers to group allocation whenever possible. Exploring treatment types that restore effective pain modulation in patients with PFP, as well as factors influencing QST in this population, will also be helpful.
CONCLUSIONS
Our findings support signs of central sensitization in patients with PFP compared with pain-free control individuals. For individuals with PFP who demonstrate signs of central sensitization, clinicians should structure a multimodal care plan that addresses both movement and pain, as these factors may contribute to pain persistence. Tracking these outcomes during rehabilitation can demonstrate restoration of effective central pain modulation, which may be critical for long-term treatment success.
Supplementary Material
REFERENCES
- 1.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi: 10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nimon G, Murray D, Sandow M, Goodfellow J. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop. 1998;18(1):118–122. [PubMed] [Google Scholar]
- 3.Smith BE, Selfe J, Thacker D, et al. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS One. 2018;13(1):e0190892. doi: 10.1371/journal.pone.0190892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins NJ, Crossley KM, Darnell R, Vicenzino B. Predictors of short and long term outcome in patellofemoral pain syndrome: a prospective longitudinal study. BMC Musculoskelet Disord. 2010;11:11. doi: 10.1186/1471-2474-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lack S, Barton C, Vicenzino B, Morrissey D. Outcome predictors for conservative patellofemoral pain management: a systematic review and meta-analysis. Sports Med. 2014;44(12):1703–1716. doi: 10.1007/s40279-014-0231-5. [DOI] [PubMed] [Google Scholar]
- 6.Mallen CD, Peat G, Thomas E, Dunn KM, Croft PR. Prognostic factors for musculoskeletal pain in primary care: a systematic review. Br J Gen Pract. 2007;57(541):655–661. [PMC free article] [PubMed] [Google Scholar]
- 7.Powers CM, Witvrouw E, Davis IS, Crossley KM. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK, part 3. Br J Sports Med. 2017;51(24):1713–1723. doi: 10.1136/bjsports-2017-098717. [DOI] [PubMed] [Google Scholar]
- 8.Lankhorst NE, Damen J, Oei EH, et al. Incidence, prevalence, natural course and prognosis of patellofemoral osteoarthritis: the Cohort Hip and Cohort Knee study. Osteoarthritis Cartilage. 2017;25(5):647–653. doi: 10.1016/j.joca.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Lankhorst NE, van Middelkoop M, Crossley KM, et al. Factors that predict a poor outcome 5-8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2016;50(14):881–886. doi: 10.1136/bjsports-2015-094664. [DOI] [PubMed] [Google Scholar]
- 10.Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is knee pain during adolescence a self-limiting condition? Prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med. 2016;44(5):1165–1171. doi: 10.1177/0363546515622456. [DOI] [PubMed] [Google Scholar]
- 11.Matthews M, Rathleff MS, Claus A, et al. Can we predict the outcome for people with patellofemoral pain? A systematic review on prognostic factors and treatment effect modifiers. Br J Sports Med. 2017;51(23):1650–1660. doi: 10.1136/bjsports-2016-096545. [DOI] [PubMed] [Google Scholar]
- 12.Rathleff CR, Olesen JL, Roos EM, Rasmussen S, Rathleff MS. Half of 12–15-year-olds with knee pain still have pain after one year. Dan Med J. 2013;60(11):A4725. [PubMed] [Google Scholar]
- 13.Stathopulu E, Baildam E. Anterior knee pain: a long-term follow-up. Rheumatology (Oxford) 2003;42(2):380–382. doi: 10.1093/rheumatology/keg093. [DOI] [PubMed] [Google Scholar]
- 14.Arendt-Nielsen L, Morlion B, Perrot S, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain. 2018;22(2):216–241. doi: 10.1002/ejp.1140. [DOI] [PubMed] [Google Scholar]
- 15.IASP terminology. International Association for the Study of Pain Web site. https://www.iasp-pain.org/terminology Updated December 14, 2017. Accessed April 7, 2018.
- 16.Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 suppl):S2–S15. doi: 10.1016/j.pain.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chimenti RL, Frey-Law LA, Sluka KA. A mechanism-based approach to physical therapist management of pain. Phys Ther. 2018;98(5):302–314. doi: 10.1093/ptj/pzy030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Staud R. Abnormal endogenous pain modulation is a shared characteristic of many chronic pain conditions. Expert Rev Neurother. 2012;12(5):577–585. doi: 10.1586/ern.12.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dell'Isola A, Allan R, Smith SL, Marreiros SS, Steultjens M. Identification of clinical phenotypes in knee osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord. 2016;17(1):425. doi: 10.1186/s12891-016-1286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright A, Benson HAE, Will R, Moss P. Cold pain threshold identifies a subgroup of individuals with knee osteoarthritis that present with multimodality hyperalgesia and elevated pain levels. Clin J Pain. 2017;33(9):793–803. doi: 10.1097/AJP.0000000000000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baert IA, Lluch E, Mulder T, Nijs J, Noten S, Meeus M. Does pre-surgical central modulation of pain influence outcome after total knee replacement? A systematic review. Osteoarthritis Cartilage. 2016;24(2):213–223. doi: 10.1016/j.joca.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Kurien T, Arendt-Nielsen L, Petersen KK, Graven-Nielsen T, Scammell BE. Preoperative neuropathic pain-like symptoms and central pain mechanisms in knee osteoarthritis predicts poor outcome 6 months after total knee replacement surgery. J Pain. 2018;19(11):1329–1341. doi: 10.1016/j.jpain.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Edwards RR, Dolman AJ, Martel MO, et al. Variability in conditioned pain modulation predicts response to NSAID treatment in patients with knee osteoarthritis. BMC Musculoskelet Disord. 2016;17:284. doi: 10.1186/s12891-016-1124-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim SH, Yoon KB, Yoon DM, Yoo JH, Ahn KR. Influence of centrally mediated symptoms on postoperative pain in osteoarthritis patients undergoing total knee arthroplasty: a prospective observational evaluation. Pain Pract. 2015;15(6):E46–E53. doi: 10.1111/papr.12311. [DOI] [PubMed] [Google Scholar]
- 25.Lluch Girbes E, Nijs J, Torres-Cueco R, Lopez Cubas C. Pain treatment for patients with osteoarthritis and central sensitization. Phys Ther. 2013;93(6):842–851. doi: 10.2522/ptj.20120253. [DOI] [PubMed] [Google Scholar]
- 26.Defrin R, Shachal-Shiffer M, Hadgadg M, Peretz C. Quantitative somatosensory testing of warm and heat-pain thresholds: the effect of body region and testing method. Clin J Pain. 2006;22(2):130–136. doi: 10.1097/01.ajp.0000154048.68273.d8. [DOI] [PubMed] [Google Scholar]
- 27.Rathleff MS, Rathleff CR, Stephenson A, et al. Adults with patellofemoral pain do not exhibit manifestations of peripheral and central sensitization when compared to healthy pain-free age and sex matched controls—an assessor blinded cross-sectional study. PLoS One. 2017;12(12):e0188930. doi: 10.1371/journal.pone.0188930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rathleff MS, Roos EM, Olesen JL, Rasmussen S, Arendt-Nielsen L. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2013;43(6):414–421. doi: 10.2519/jospt.2013.4383. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy DL, Kemp HI, Ridout D, Yarnitsky D, Rice AS. Reliability of conditioned pain modulation: a systematic review. Pain. 2016;157(11):2410–2419. doi: 10.1097/j.pain.0000000000000689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Oliveira Silva D, Rathleff MS, Petersen K, Azevedo FM, Barton CJ. Manifestations of pain sensitization across different painful knee disorders: a systematic review including meta-analysis and metaregression. Pain Med. 2019;20(2):335–358. doi: 10.1093/pm/pny177. [DOI] [PubMed] [Google Scholar]
- 31.Zadro J, Shirley D, Ferreira M, et al. Mapping the association between vitamin D and low back pain: a systematic review and meta-analysis of observational studies. Pain Physician. 2017;20(7):611–640. [PubMed] [Google Scholar]
- 32.Barton JL, Criswell LA, Kaiser R, Chen YH, Schillinger D. Systematic review and meta-analysis of patient self-report versus trained assessor joint counts in rheumatoid arthritis. J Rheumatol. 2009;36(12):2635–2641. doi: 10.3899/jrheum.090569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Tulder M, Furlan A, Bombardier C, Bouter L; Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 35.Field AP, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63(pt 3):665–694. doi: 10.1348/000711010X502733. [DOI] [PubMed] [Google Scholar]
- 36.Holden S, Straszek CL, Rathleff MS, Petersen KK, Roos EM, Graven-Nielsen T. Young females with long-standing patellofemoral pain display impaired conditioned pain modulation, increased temporal summation of pain, and widespread hyperalgesia. Pain. 2018;159(12):2530–2537. doi: 10.1097/j.pain.000000000000135. [DOI] [PubMed] [Google Scholar]
- 37.Noehren B, Shuping L, Jones A, Akers DA, Bush HM, Sluka KA. Somatosensory and biomechanical abnormalities in females with patellofemoral pain. Clin J Pain. 2016;32(10):915–919. doi: 10.1097/AJP.0000000000000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pazzinatto MF, de Oliveira Silva D, Barton C, Rathleff MS, Briani RV, de Azevedo FM. Female adults with patellofemoral pain are characterized by widespread hyperalgesia, which is not affected immediately by patellofemoral joint loading. Pain Med. 2016;17(10):1953–1961. doi: 10.1093/pm/pnw068. [DOI] [PubMed] [Google Scholar]
- 39.Pazzinatto MF, de Oliveira Silva D, Pradela J, Coura MB, Barton C, de Azevedo FM. Local and widespread hyperalgesia in female runners with patellofemoral pain are influenced by running volume. J Sci Med Sport. 2017;20(4):362–367. doi: 10.1016/j.jsams.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 40.Rathleff MS, Petersen KK, Arendt-Nielsen L, Thorborg K, Graven-Nielsen T. Impaired conditioned pain modulation in young female adults with long-standing patellofemoral pain: a single blinded cross-sectional study. Pain Med. 2016;17(5):980–988. doi: 10.1093/pm/pnv017. [DOI] [PubMed] [Google Scholar]
- 41.van der Heijden RA, Rijndertse MM, Bierma-Zeinstra SMA, van Middelkoop M. Lower pressure pain thresholds in patellofemoral pain patients, especially in female patients: a cross-sectional case-control study. Pain Med. 2018;19(1):184–192. doi: 10.1093/pm/pnx059. [DOI] [PubMed] [Google Scholar]
- 42.van der Heijden RA, Vollebregt T, Bierma-Zeinstra SM, van Middelkoop M. Strength and pain threshold handheld dynamometry test reliability in patellofemoral pain. Int J Sports Med. 2015;36(14):1201–1205. doi: 10.1055/s-0035-1555855. [DOI] [PubMed] [Google Scholar]
- 43.Maclachlan LR, Collins NJ, Hodges PW, Vicenzino B. Psychological and pain profiles in persons with patellofemoral pain as the primary symptom. Eur J Pain. 2020;24(6):1182–1196. doi: 10.1002/ejp.1563. [DOI] [PubMed] [Google Scholar]
- 44.Holden S, Rathleff MS, Thorborg K, Holmich P, Graven-Nielsen T. Mechanistic pain profiling in young adolescents with patellofemoral pain before and after treatment: a prospective cohort study. Pain. 2020;161(5):1065–1071. doi: 10.1097/j.pain.0000000000001796. [DOI] [PubMed] [Google Scholar]
- 45.Jensen R, Hystad T, Kvale A, Baerheim A. Quantitative sensory testing of patients with long lasting patellofemoral pain syndrome. Eur J Pain. 2007;11(6):665–676. doi: 10.1016/j.ejpain.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 46.Jensen R, Kvale A, Baerheim A. Is pain in patellofemoral pain syndrome neuropathic? Clin J Pain. 2008;24(5):384–394. doi: 10.1097/AJP.0b013e3181658170. [DOI] [PubMed] [Google Scholar]
- 47.Boudreau SA, Kamavuako EN, Rathleff MS. Distribution and symmetrical patellofemoral pain patterns as revealed by high-resolution 3D body mapping: a cross-sectional study. BMC Musculoskelet Disord. 2017;18(1):160. doi: 10.1186/s12891-017-1521-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boudreau SA, Royo AC, Matthews M, et al. Distinct patterns of variation in the distribution of knee pain. Sci Rep. 2018;8(1):16522. doi: 10.1038/s41598-018-34950-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rathleff MS, Graven-Nielsen T, Holmich P, et al. Activity modification and load management of adolescents with patellofemoral pain: a prospective intervention study including 151 adolescents. Am J Sports Med. 2019;47(7):1629–1637. doi: 10.1177/0363546519843915. [DOI] [PubMed] [Google Scholar]
- 50.Rathleff MS, Holden S, Straszek CL, Olesen JL, Jensen MB, Roos EM. Five-year prognosis and impact of adolescent knee pain: a prospective population-based cohort study of 504 adolescents in Denmark. BMJ Open. 2019;9(5):e024113. doi: 10.1136/bmjopen-2018-024113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maclachlan LR, Matthews M, Hodges PW, Collins NJ, Vicenzino B. The psychological features of patellofemoral pain: a cross-sectional study. Scand J Pain. 2018;18(2):261–271. doi: 10.1515/sjpain-2018-0025. [DOI] [PubMed] [Google Scholar]
- 52.Rathleff MS, Vicenzino B, Middelkoop M, et al. Patellofemoral pain in adolescence and adulthood: same same, but different? Sports Med. 2015;45(11):1489–1495. doi: 10.1007/s40279-015-0364-1. [DOI] [PubMed] [Google Scholar]
- 53.Willy RW, Manal KT, Witvrouw EE, Davis IS. Are mechanics different between male and female runners with patellofemoral pain? Med Sci Sports Exerc. 2012;44(11):2165–2171. doi: 10.1249/MSS.0b013e3182629215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Willy RW, Hoglund LT, Barton CJ, et al. Patellofemoral pain. J Orthop Sports Phys Ther. 2019;49(9):CPG1–CPG95. doi: 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
- 55.Arendt-Nielsen L, Skou ST, Nielsen TA, Petersen KK. Altered central sensitization and pain modulation in the CNS in chronic joint pain. Curr Osteoporos Rep. 2015;13(4):225–234. doi: 10.1007/s11914-015-0276-x. [DOI] [PubMed] [Google Scholar]
- 56.Huang D, Yu B. The mirror-image pain: an unclered phenomenon and its possible mechanism. Neurosci Biobehav Rev. 2010;34(4):528–532. doi: 10.1016/j.neubiorev.2009. [DOI] [PubMed] [Google Scholar]
- 57.Cruz-Almeida Y, Fillingim RB. Can quantitative sensory testing move us closer to mechanism-based pain management? Pain Med. 2014;15(1):61–72. doi: 10.1111/pme.12230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.