Abstract
Background:
The etiology for subsequent surgeries following ACL reconstruction vary, but if risk factors for specific subsequent surgeries can be identified, we can better understand which patients are at greatest risk.
Hypothesis/Purpose:
To report the incidence and types of subsequent surgeries that occur in a cohort of patients 6 years following their index ACL reconstruction, and to identify which variables are associated with the incidence of a patient having a subsequent surgery following their index ACL reconstruction.
Study Design:
Prospective cohort study
Methods:
Patients completed a questionnaire prior to their index ACL surgery and were followed up at 2 and 6 years. Patients were contacted to determine whether any underwent additional surgeries since baseline. Operative reports were obtained, and all surgeries were categorized and recorded. Logistical regression models were constructed to predict which patient demographic and surgical variables are associated with the incidence of having a subsequent surgery following their index ACL reconstruction.
Results:
The cohort consisted of 3,276 subjects (56% male) with a median age of 23 years. Six-year follow-up was obtained on 92% (2999/3276) with regards to information on incidence and frequency of subsequent surgeries. Overall, 20% (612/2999) of the cohort was documented to have had at least one subsequent surgery on the ipsilateral knee 6 years following their index ACL reconstruction. The most common subsequent surgeries were related to meniscus (11.9%), revision ACL reconstruction (7.5%), loss of motion (7.8%), or articular cartilage (6.7%). The most significant risk factors for incurring a subsequent meniscus-related surgery were patients having a medial meniscus repair, hamstring autograft or allograft reconstruction, higher Marx activity level, and younger age. Significant predictors of having a subsequent surgery involving the articular cartilage were higher BMI, higher Marx activity level, autograft hamstring or allograft reconstruction, or grades 3/4 articular cartilage pathology classified at time of index ACL reconstruction. Risk factors for incurring a subsequent surgery for loss of motion were younger age, female sex, low baseline KOOS symptom score, and a soft-tissue allograft.
Conclusion:
These findings can be used to identify patients who are at the greatest risk of incurring a subsequent surgery following ACL reconstruction.
Keywords: anterior cruciate ligament reconstruction, subsequent surgery, meniscus, articular cartilage, loss of motion
INTRODUCTION
Anterior cruciate ligament (ACL) tears commonly have associated injuries such as meniscus tears,6 cartilage injuries,5 and additional ligament sprains.11 Patients with an ACL tear and concomitant medial meniscal and chondral injuries have poorer functional outcomes scores, decreased activity levels, and lower return to sports rates.18, 21 Associated injuries such as meniscus tears and cartilage damage contribute to post-traumatic arthritis years later, but in the short term they can lead to subsequent surgeries when the pathologies fail to heal or respond to treatments. Subsequent surgery after ACL reconstruction decreases patient outcomes scores and satisfaction.19 The reason for subsequent surgeries vary widely, and if we can identify modifiable risk factors for specific subsequent surgeries we can better understand which patients are at greatest risk. Previous studies have identified risk factors for subsequent surgeries after ACL reconstruction,1, 2, 4, 7–10, 12, 16, 17, 19 but to our knowledge only a few studies have been done to evaluate which factors increase the risk for specific procedures related to meniscus, articular cartilage, or for loss of motion.1, 2, 8
Csintalan et al. identified multiple risk factors for subsequent surgeries following ACL reconstruction.2 Meniscal repair at the time of the initial ACL reconstruction was a risk factor for having a subsequent meniscus surgery. Older age and undergoing an ACL reconstruction by a sports medicine fellowship-trained surgeon were associated with subsequent cartilage surgeries. Allografts and female gender were associated with subsequent hardware removal surgeries. Debridement for arthrofibrosis was more likely in females and patients with prior surgery. Some of these risk factors are predictable, such as meniscus repair increasing the likelihood of a subsequent meniscus surgery. Other associations are less obvious.
The purpose of this study was two-fold: 1) to report the incidence and types of subsequent surgeries that occur in a cohort of ACL reconstructed patients within 6 years following their index ACL reconstruction; and, 2) to identify and assess which variables (i.e., patient demographic and surgical) are associated with the incidence of a patient having a subsequent surgery (other than a revision ACL reconstruction) following their index ACL reconstruction.
METHODS
Study Design and Population
This was a multicenter longitudinal prospective cohort study design, consisting of 7 consortium sites [Vanderbilt University Medical Center, Nashville, TN (coordinating center); Cleveland Clinic Foundation, Cleveland, OH; Hospital for Special Surgery, New York, NY; The Ohio State University, Columbus, OH: University of Colorado, Boulder, CO; University of Iowa, Iowa City, IA; Washington University in St. Louis, MO] and 17 surgeons.
After obtaining approval from each site’s respective institutional review boards, all patients who underwent unilateral primary or revision ACL reconstruction surgery were eligible for enrollment from 2002–2008. Multi-ligamentous injuries were included. Simultaneous bilateral ACL reconstructions were excluded for this study.
Data Sources and Management
After informed consent was obtained, each participant completed a questionnaire that included baseline demographics, injury descriptors, sports participation level, comorbidities, knee surgical history, and validated patient-reported outcome measures [the International Knee Documentation Committee (IKDC), Knee injury and Osteoarthritis Outcome Score (KOOS) five subscales (symptoms, pain, activities of daily living [ADL], sports and recreation, knee-related quality of life), and Marx activity rating scale].
Following the surgery, each surgeon completed a questionnaire that documented the results of the exam under anesthesia, surgical technique, and the arthroscopic findings and treatment of any concomitant meniscal and cartilage injuries. Surgeon documentation of any articular cartilage pathology was recorded, based on the modified Outerbridge classification.3, 15 Meniscus pathology was classified by location, size, and partial versus complete tears, while treatment was recorded as not treated, repair, extent of resection, or other (i.e., transplant, etc.). Following surgery, the patients were given a uniform set of standardized evidence-based rehabilitation guidelines.
Completed data forms were mailed from each participating site to the data coordinating center and scanned into a master database using Teleform™ software (OpenText; Waterloo, Ontario, Canada). A series of logical error and quality control checks were performed as part of our regular data maintenance. Cases which failed these checks were tagged and verified against the source documents in order to resolve prior to analysis.
Follow-Up
Two- and six-year follow-up was completed by mail with re-administration of the same questionnaire that the patients completed at baseline (defined as the time of index ACL surgery). In addition, patients were also contacted to determine whether any underwent additional surgeries since baseline (e.g., revision ACL reconstruction on the ipsilateral knee, primary ACL reconstruction on the contralateral knee, and/or any arthroscopy to either knee). Every effort was made to obtain the operative note on these additional surgeries. If an operative report could not be obtained but the patient reported an ACL reconstruction, surgery for infection, or total knee arthroplasty (TKA), these were recorded as such. If the patient reported any other type of surgery, patient accuracy was assumed to be unreliable, and the surgery was recorded as “no op report/unknown.” These “unknowns” were included in counts as subsequent surgeries but excluded from categorical analyses. Operative reports were obtained and independently read by two orthopaedic surgeons, and all procedures performed during the subsequent surgery were categorized and recorded, along with the surgical date. If multiple procedures were done during a surgery, all were recorded. If the two surgeons disagreed on how to categorize any procedure, a third blinded orthopaedic surgeon was asked to read the operative report, and majority ruled. A diagram depicting the categories and subcategories of defined procedures within a subsequent surgery is shown in Figure 1.
Figure 1.
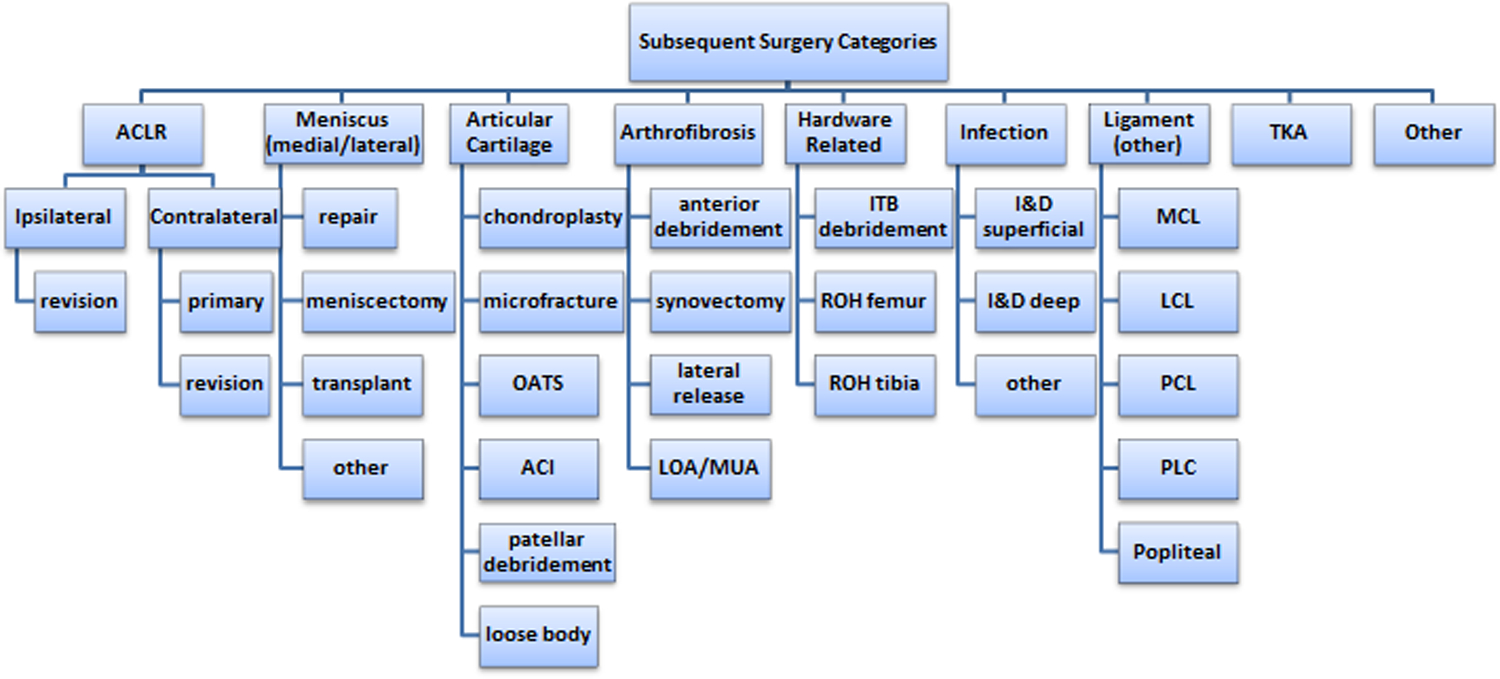
Listing of categories and subcategories used for classifying procedures within a subsequent surgery. Key: ACI=autologous chondrocyte implantation; ACLR=ACL reconstruction; I&D=infection and debridement; ITB=iliotibial band; LCL=lateral collateral ligament; LOA/MUA=lysis of adhesions/manipulation under anesthesia; MCL=medial collateral ligament; OATS=osteochondral transfer system; PCL=posterior cruciate ligament; PLC=posterolateral corner; ROH=removal of hardware; TKA=total knee arthroplasty.
Quantitative Variables and Statistical Methods
Three separate logistic regression models were constructed to predict which variables (i.e., patient demographic and surgical) are associated with the incidence of a patient having a subsequent surgery following their index ACL reconstruction: one model examined subsequent meniscus-related surgeries on the ipsilateral knee, one model examined subsequent articular cartilage-related surgeries on the ipsilateral knee, and one model examined subsequent surgeries due to loss of motion on the ipsilateral knee. Of note, no models were constructed to examine subsequent ACL reconstruction on either the ipsilateral or contralateral knees because these have previously been reported.9, 10
Risk factor variables included for each model (Table 1)
Table 1.
Risk Factor Variables Included for Each Model
| Variables | Levels | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| Meniscus-related surgery | Articular cartilage-related surgery | Loss of motion-related surgery | ||
| Age | Continuous | X | X | X |
| Sex | Male, Female | X | X | X |
| Body mass index [BMI] | Continuous | X | X | X |
| Baseline Marx activity score | 0–16 | X | X | |
| Baseline KOOS symptom subscale score | 0–100 | X | ||
| Smoking status | Never, Quit, Current | X | X | |
| Baseline knee joint effusion | Yes, No | X | ||
| Reconstruction type | Primary, Revision | X | X | |
| Graft type | Autograft bone-patellar tendon-bone [BTB], Autograft hamstring [HS], Allograft | X | X | X |
| Previous meniscal surgery on the ipsilateral knee | Yes, No | considered for removal, not removed | ultimately removed from final model | |
| Previous ACL reconstruction surgery on the contralateral knee | Yes, No | X | ultimately removed from final model | |
| Meniscal treatment (most severe in any compartment) | None, No treatment for tear, Repair, Excision, Other | X | ||
| Any concurrent meniscal repair | Yes, No | X | ||
| Current medial meniscus treatment | None, No treatment for tear, Repair, Excision, Other | X | ||
| Current lateral meniscus treatment | None, No treatment for tear, Repair, Excision, Other | X | ||
| Articular cartilage [AC] pathology (highest grade in any compartment) | Normal/grade 1, Grade 2, Grade 3/ 4 | X | ||
| AC pathology in the medial compartment (highest grade in the medial femoral condyle [MFC] or medial tibial plateau [MTP]) | Normal/grade 1, Grade 2, Grade 3/ 4 | X | ||
| AC pathology in the lateral compartment (highest grade in the lateral femoral condyle [LFC] or lateral tibial plateau [LTP]) | Normal/grade 1, Grade 2, Grade 3/ 4 | X | ||
| AC pathology in the patellofemoral compartment (highest grade in the patella or the trochlea) | Normal/grade 1, Grade 2, Grade 3/ 4 | X | ||
| Other concurrent ligament reconstruction: Lateral collateral ligament [LCL] Medial collateral ligament [MCL] Posterior collateral ligament [PCL] |
Yes, No Yes, No Yes, No |
X X X |
Key: AC=articular cartilage; ACL=anterior cruciate ligament.
The associated baseline variables were considered for each of the following outcomes on the ipsilateral knee within 6 years of index ACL reconstruction (Table 1).
Full Models
All continuous variables (age, BMI, and Marx activity level scores) were tested for non-linear relationships. All full models were run for each outcome. Non-significant (at p≥ 0.05 level) non-linear terms were tested collectively with a likelihood ratio test. The discrimination ability and overfitting metrics were computed.
Reducing over-fit models
Likelihood ratio (LR) tests, Akaike Information Criterion (AIC) values, and shrinkage estimates were obtained to test the full and reduced models to determine the optimal models.
Variable Importance
To assess the relative importance of the variables contained in each model, the AIC metric was used, which quantifies the trade-off between how well the model fits the data and how complex the model is (i.e., how many degrees of freedom are used). The difference in AIC was computed between the full model and after removing each variable from the full model. A variable causing the largest increase in AIC is deemed most important, whereas a decrease in AIC upon removal actually means the model is better without the variable (statistically).
Missing Data
Missing data were imputed using Multiple Imputation by Chained Equations (MICE) via the R package mice. The final models for each outcome were run on the un-imputed data as a sensitivity analysis to check for any drastic changes in model coefficients or other metrics. Statistical analysis was performed with free open-source R statistical software (www.r-project.org).
RESULTS
Study Population
Table 2 provides a univariate summary of the cohort, displaying medians with (25th, 75th) percentiles for numeric variables, and frequencies with percentages for categorical variables.
Table 2.
Descriptive Summaries of Baseline Characteristics and 6-year Outcomes
| Variable | Summary | Variable | Summary | ||
|---|---|---|---|---|---|
| Age | 23 (17,35) | AC Pathology (Medial) | |||
| Sex | Normal/Grade 1 | 2485 (75.9%) | |||
| Female | 1433 (43.7%) | Grade 2 | 466 (14.2%) | ||
| Male | 1843 (56.3%) | Grades 3/4 | 325 (9.9%) | ||
| BMI | 24.9 (22.3,28) | AC Pathology (Lateral) | |||
| <NA> | 48 (1.5%) | Normal/Grade 1 | 2558 (78.1%) | ||
| Baseline MARX | 12 (8,16) | Grade 2 | 502 (15.3%) | ||
| <NA> | 31 (0.9%) | Grades 3/4 | 216 (6.6%) | ||
| Smoking status | AC Pathology (Patellofemoral) | ||||
| Never | 2601 (79.4%) | Normal/Grade 1 | 2556 (78.0%) | ||
| Quit | 334 (10.2%) | Grade 2 | 417 (12.7%) | ||
| Current | 302 (9.2%) | Grades 3/4 | 303 (9.2%) | ||
| NA | 39 (1.2%) | AC Pathology (highest grade in any compartment) | |||
| Reconstruction type | Normal/Grade 1 | 1833 (56.0%) | |||
| Primary | 3059 (93.4%) | Grade 2 | 830 (25.3%) | ||
| Revision | 217 (6.6%) | Grade 3 | 479 (14.6%) | ||
| Graft type | Grade 4 | 134 (4.1%) | |||
| Autograft BTB | 1408 (43.0%) | Other concurrent ligament reconstruction | |||
| Autograft HS | 1106 (33.8%) | No | 3178 (97.0%) | ||
| Allograft | 762 (23.3%) | Yes | 98 (3.0%) | ||
| Medial Meniscus Treatment | Previous Meniscal surgery (ipsilateral knee) | ||||
| Normal | 2014 (61.5%) | No | 2980 (91.0%) | ||
| No tx for tear | 146 (4.5%) | Yes | 296 (9.0%) | ||
| Repair | 472 (14.4%) | Previous ACL reconstruction surgery (on contralateral knee) | |||
| Excision | 599 (18.3%) | No | 2979 (90.9%) | ||
| Other | 45 (1.4%) | Yes | 297 (9.1%) | ||
| Lateral Meniscus Treatment | Number of patients incurring at least 1 subsequent surgery on the ipsilateral knee | ||||
| Normal | 1746 (53.3%) | No | 2387 (79.6%) | ||
| No tx. for tear | 328 (10%) | Yes | 612 (20.4%) | ||
| Repair | 223 (6.8%) | Number of patients incurring at least 1 meniscal-related subsequent surgery on the ipsilateral knee | |||
| Excision | 951 (29%) | No | 2728 (91.0%) | ||
| Other | 28 (0.9%) | Yes | 271 (9.0%) | ||
| Meniscus Treatment (most severe) | Number of patients incurring at least 1 articular cartilage-related subsequent surgery on the ipsilateral knee | ||||
| Normal | 1090 (33.3%) | No | 2855 (95.2%) | ||
| No tx. for tear | 289 (8.8%) | Yes | 144 (4.8%) | ||
| Repair | 472 (14.4%) | Number of patients incurring at least 1 arthrofibrosis-related subsequent surgery on the ipsilateral knee | |||
| Excision | 1369 (41.8%) | No | 2764 (92.2%) | ||
| Other | 56 (1.7%) | Yes | 235 (7.8%) | ||
| Number of patients incurring at least 1 subsequent surgery due to loss of motion on the ipsilateral knee | |||||
| No | 2915 (97.2%) | ||||
| Yes | 84 (2.8%) | ||||
Key: AC=articular cartilage; BMI=body mass index; BTB=bone-patellar tendon-bone; HS=hamstring; tx=treatment.
The cohort consisted of 3,276 subjects (56% male) with a median age of 23 years at the time of enrollment. Primary ACL reconstructions comprised 93% of the group, and most subjects underwent bone-patellar tendon-bone (BTB) autograft reconstructions (43%), while 34% underwent hamstring autograft and 23% had allograft reconstructions.
Follow-up
Overall, we were able to obtain 92% (2999/3276) follow-up with regards to information on incidence and frequency of subsequent surgeries on the cohort.
Incidence of Subsequent Surgery
Overall, 20% (612/2999) of the cohort was documented to have had at least one subsequent surgery on the ipsilateral knee 6 years following their index ACL reconstruction (Table 2). These 612 subjects encompassed 1,272 categorical procedures (Table 3).
Table 3.
Subsequent Procedures Stratified to 2- and 6-Year Follow-up
| Overall (n=1272 procedures) N (% follow-up cohort) |
0–2 years (n=731 procedures) N |
2–6 years (n=541 procedures) N |
Median (months) | |
|---|---|---|---|---|
|
Revision ACL Reconstruction
|
226 (7.5) | 126 | 100 | 21.1 |
| Meniscus | 357 (11.9) | 21.8 | ||
| Medial repair | 51 (1.7) | 30 | 21 | 20.7 |
| Medial meniscectomy | 170 (5.7) | 90 | 80 | 23.0 |
| Lateral repair | 7 (<1) | 3 | 4 | 24.4 |
| Lateral meniscectomy | 122 (4.1) | 73 | 49 | 20.1 |
| Transplant | 1 (<1) | 1 | 0 | 11.0 |
| Other / unknown | 6 (<1) | 2 | 4 | 24.5 |
| Articular Cartilage | 201 (6.7) | 25.9 | ||
| Chondroplasty | 99 (3.3) | 52 | 47 | 21.8 |
| Microfracture | 30 (1.0) | 9 | 21 | 42.6 |
| OATS | 4 (<1) | 1 | 3 | 34.3 |
| ACI | 1 (<1) | 1 | 0 | 19.7 |
| Patellar debridement | 49 (1.6) | 22 | 27 | 25.8 |
| Loose body | 18 (<1) | 5 | 13 | 38.4 |
| Arthrofibrosis | 235 (7.8) | 14.3 | ||
| Anterior debridement | 139 (4.6) | 98 | 41 | 14.3 |
| Synovectomy | 64 (2.1) | 38 | 26 | 19.8 |
| Lateral release | 7 (<1) | 5 | 2 | 15.0 |
| LOA/MUA | 25 (<1) | 25 | 0 | 7.3 |
| Hardware | 87 (2.9) | 16.1 | ||
| ITB debridement | 19 (<1) | 18 | 1 | 6.0 |
| ROH femur | 9 (<1) | 5 | 4 | 22.6 |
| ROH tibia | 58 (1.9) | 33 | 25 | 20.6 |
| Unknown | 1 (<1) | 0 | 1 | 54.4 |
| Infection | 35 (1.2) | 1.2 | ||
| I&D superficial | 11 (<1) | 10 | 1 | 1.1 |
| I&D deep | 19 (<1) | 19 | 0 | 1.2 |
| Other | 5 (<1) | 4 | 1 | 1.9 |
| Ligament (Other) | 5 (<1) | 6.0 | ||
| MCL | 1 (<1) | 1 | 0 | 12.0 |
| LCL | 2 (<1) | 2 | 0 | 6.0 |
| PCL | 0 | 0 | 0 | -- |
| PLC | 2 (<1) | 1 | 1 | 28.9 |
| Popliteal | 0 | 0 | 0 | -- |
| Other | 39 (1.3) | 29 | 10 | 14.3 |
| TKA | 19 (0.6) | 5 | 14 | 45.3 |
| No Operative Report | 68 (2.3) | 23 | 45 | 38.3 |
Key: ACI=Autologous Chondrocyte Implantation; ACL=anterior cruciate ligament; I&D=irrigation and debridement; ITB=iliotibial band; LCL=lateral collateral ligament; LOA/MUA= lysis of adhesions / manipulation under anesthesia; MCL=medial collateral ligament; OATS=Osteochondral autograft Transfer System; PCL=posterior cruciate ligament; PLC=posterolateral corner; ROH=removal of hardware; TKA=total knee arthroplasty
The majority of subsequent surgical procedures involved the meniscus (n=357; 11.9%), with medial meniscus repairs and/or meniscectomies occurring almost twice as frequently as on the lateral meniscus (7.4% vs. 4.2%). The most common subsequent surgery that occurred in our cohort was having a revision ACL reconstruction of the index knee, which occurred in 7.5% of the cohort (Table 2).
Predictors of Subsequent Meniscal Surgeries
The variables that were found to be significant predictors of having a subsequent meniscal surgery on the ipsilateral knee were patients with lower age, higher baseline Marx activity level, patients who had quit smoking (compared to non-smokers), having a hamstring autograft or allograft (compared to a BTB autograft), or having a medial meniscus repair or a medial meniscus tear that was not treated at the time of index surgery (Table 4).
Table 4.
Odds ratios (OR), 95% confidence intervals (CI), and associated p-values for variables in the meniscal and articular cartilage subsequent surgery models.
| Variable | Ipsilateral Knee | ||||||
|---|---|---|---|---|---|---|---|
| Meniscus | Articular cartilage | ||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Age | 0.97 | (0.95,0.99) | 0.001 | 0.99 | (0.97,1.01) | 0.167 | |
| Sex | |||||||
| Female | - | - | - | - | - | - | |
| Male | 0.98 | (0.74,1.28) | 0.867 | 0.86 | (0.6,1.21) | 0.383 | |
| BMI | 1.03 | (1,1.06) | 0.068 | 1.05 | (1.01,1.08) | 0.006 | |
| Baseline Marx activity score | Non-linear | <0.001 | 1.05 | (1.01,1.09) | 0.012 | ||
| Baseline KOOS Symptom score | |||||||
| Smoking status | |||||||
| Never | - | - | - | - | - | - | |
| Quit | 1.65 | (1.04,2.62) | 0.034 | 1.56 | (0.91,2.68) | 0.109 | |
| Current | 0.77 | (0.44,1.37) | 0.379 | 1.38 | (0.79,2.4) | 0.26 | |
| Reconstruction type | |||||||
| Primary | - | - | - | - | - | ||
| Revision | 0.94 | (0.52,1.7) | 0.842 | 1.67 | (0.95,2.93) | ||
| Graft type | |||||||
| Autograft BTB | - | - | - | - | - | - | |
| Autograft Hamstring | 1.75 | (1.29,2.39) | <0.001 | 1.84 | (1.20,2.81) | 0.005 | |
| Allograft | 3.23 | (2.21,4.72) | <0.001 | 2.44 | (1.51,3.94) | <0.001 | |
| Previous meniscal surgery | |||||||
| No | - | - | - | ||||
| Yes | 1.52 | (0.9,2.59) | 0.121 | ||||
| Previous ACL reconstruction surgery (contralateral knee) | |||||||
| No | - | - | - | ||||
| Yes | 0.44 | (0.24,0.8) | 0.007 | ||||
| Medial meniscus treatment | |||||||
| Normal | - | - | - | ||||
| No tx for tear | 1.87 | (1.06,3.28) | 0.03 | ||||
| Repair | 4.38 | (3.22,5.96) | <0.001 | ||||
| Excision | 0.75 | (0.46,1.20) | 0.228 | ||||
| Other | 1.02 | (0.30,3.44) | 0.979 | ||||
| Lateral meniscus treatment | |||||||
| Normal | - | - | - | ||||
| No tx for tear | 1.02 | (0.65,1.61) | 0.923 | ||||
| Repair | 1.52 | (0.96,2.42) | 0.077 | ||||
| Excision | 1.21 | (0.89,1.66) | 0.222 | ||||
| Other | 1.37 | (0.37,5.11) | 0.643 | ||||
| Meniscus treatment (most severe) | |||||||
| Normal | - | - | - | ||||
| No tx for tear | 1.17 | (0.57,2.40) | 0.67 | ||||
| Repair | 2.17 | (1.31,3.59) | 0.003 | ||||
| Excision | 1.23 | (0.80,1.88) | 0.339 | ||||
| Other | 0.83 | (0.19,3.65) | 0.804 | ||||
| AC pathology - medial | |||||||
| Grade 1 | - | - | - | ||||
| Grade 2 | 0.81 | (0.52,1.26) | 0.352 | ||||
| Grade 3 or 4 | 0.92 | (0.52,1.63) | 0.776 | ||||
| AC pathology - lateral | |||||||
| Grade 1 | - | - | - | ||||
| Grade 2 | 0.52 | (0.33,0.83) | 0.006 | ||||
| Grade 3 or 4 | 1.04 | (0.59,1.83) | 0.898 | ||||
| AC pathology - patellofemoral | |||||||
| Grade 1 | - | - | - | ||||
| Grade 2 | 0.78 | (0.48,1.27) | 0.321 | ||||
| Grade 3 or 4 | 0.81 | (0.44,1.49) | 0.505 | ||||
| AC pathology (highest grade in any compartment) | |||||||
| Grade 1 | - | - | - | ||||
| Grade 2 | 0.95 | (0.6,1.5) | 0.818 | ||||
| Grade 3 | 1.68 | (1.03,2.76) | 0.039 | ||||
| Grade 4 | 3.21 | (1.67,6.2) | <0.001 | ||||
| Concurrent ligament reconstruction | |||||||
| No | - | - | |||||
| Yes | 0.47 | (0.18,1.23) | 0.124 | ||||
Key: Since non-linear terms do not have a single odds ratio, those were omitted from the table, though p-values from a likelihood ratio test were included to display significance. P-values bolded were statistically significant at the 0.05 level. AC=articular cartilage; BTB=bone-patellar tendon-bone;Tx=treatment.
Conversely, having a previous ACL reconstruction surgery on the contralateral knee prior to the index surgery or having grade 2 articular cartilage pathology on the lateral compartment at the time of index surgery were significant predictors of not having any subsequent surgery related to the meniscus 6 years following an ACL reconstruction (Table 4).
Figure 2 shows the relative comparison of significance between the variables. Variables with the highest increase in AIC are deemed the most significant. Our statistical model found that after adjusting for all other covariates, medial meniscus treatment and graft type were the two most significant variables which contributed towards the likelihood of having a subsequent meniscal-related surgery by 6 years. Specifically, patients who had an initial medial meniscus repair were 4.4 times more likely to undergo a subsequent meniscal-related surgery, compared with patients with no initial meniscal pathology (p<0.001; Table 4), and medial meniscal tears which were left untreated were 1.9 times more likely to incur a subsequent surgery (p=0.03; Table 4). Similarly, patients who had an initial allograft reconstruction were over 3 times more likely to incur a subsequent meniscal-related surgery by 6 years, and patients who had an initial hamstring autograft reconstruction were 1.8 times more likely to incur a subsequent meniscal-related surgery (p<0.001; Table 4).
Figure 2.
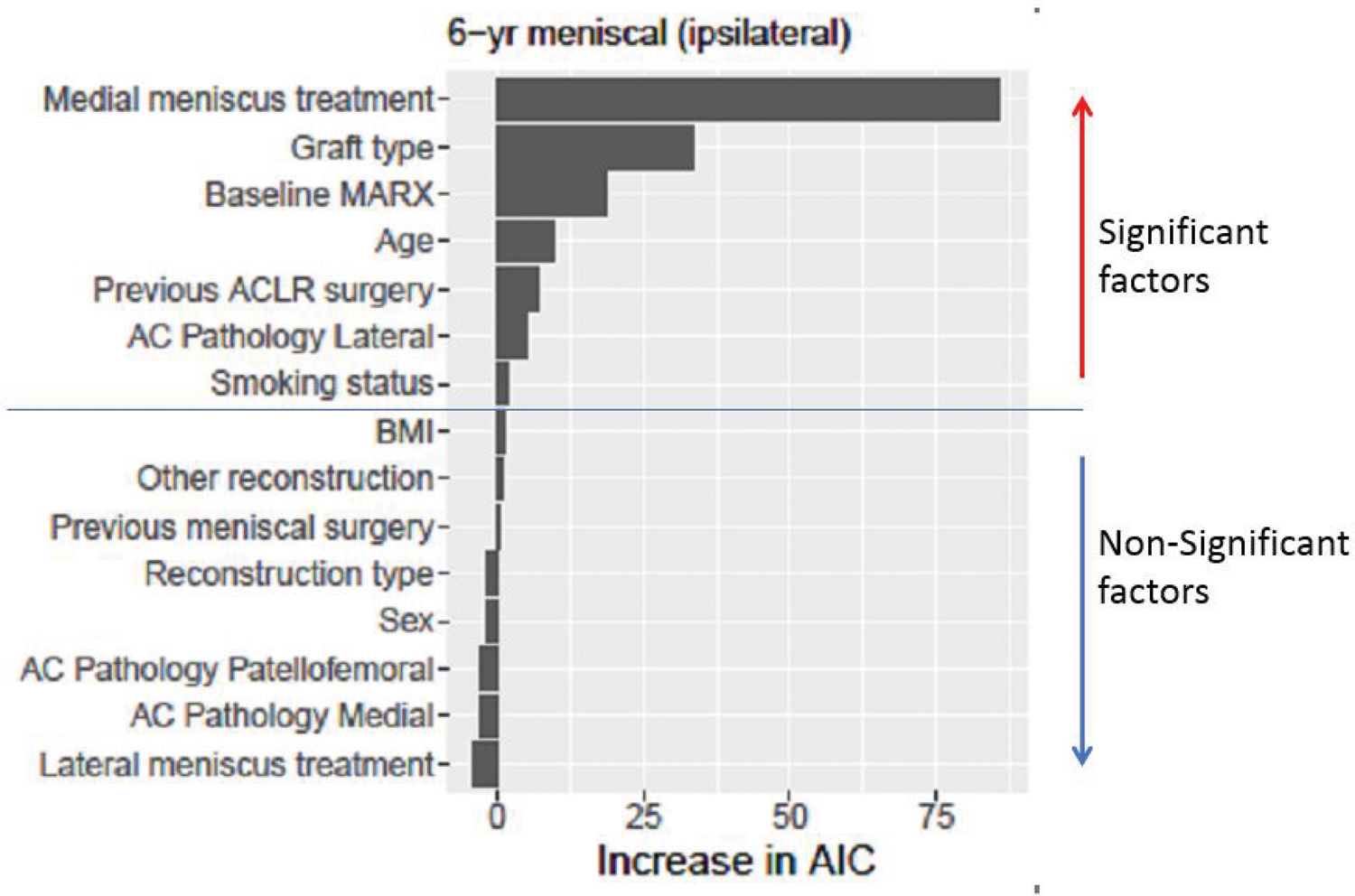
Relative variable importance by increase in AIC in the meniscal-related subsequent surgery model. AC=articular cartilage; ACLR=anterior cruciate ligament reconstruction; AIC=Akaike Information Criterion; BMI=body mass index.
Predictors of Subsequent Articular Cartilage Surgeries
The variables that were found to be significant predictors of having a subsequent surgery involving the articular cartilage (AC) on the ipsilateral knee were patients with higher BMI, higher baseline Marx activity level, having a hamstring autograft or allograft (compared to a BTB autograft), having a meniscus repair at the time of index surgery, or having grade 3 or 4 AC pathology in any compartment (Table 4). Specifically, if a patient has grade 4 changes in any compartment at the time of their index reconstruction, they are over 3 times more likely to have a subsequent AC-related surgery by 6 years, after controlling for all covariates (p<0.001; Table 3). If a patient has an initial allograft reconstruction, they are over 2 times more likely to have a subsequent AC-related surgery by 6 years (p<0.001; Table 4).
Figure 3 shows the relative comparison of significance between the variables and shows that graft type and AC pathology were the top 2 positive predictors. Age was not a significant predictor of having a subsequent AC surgery in this cohort.
Figure 3.
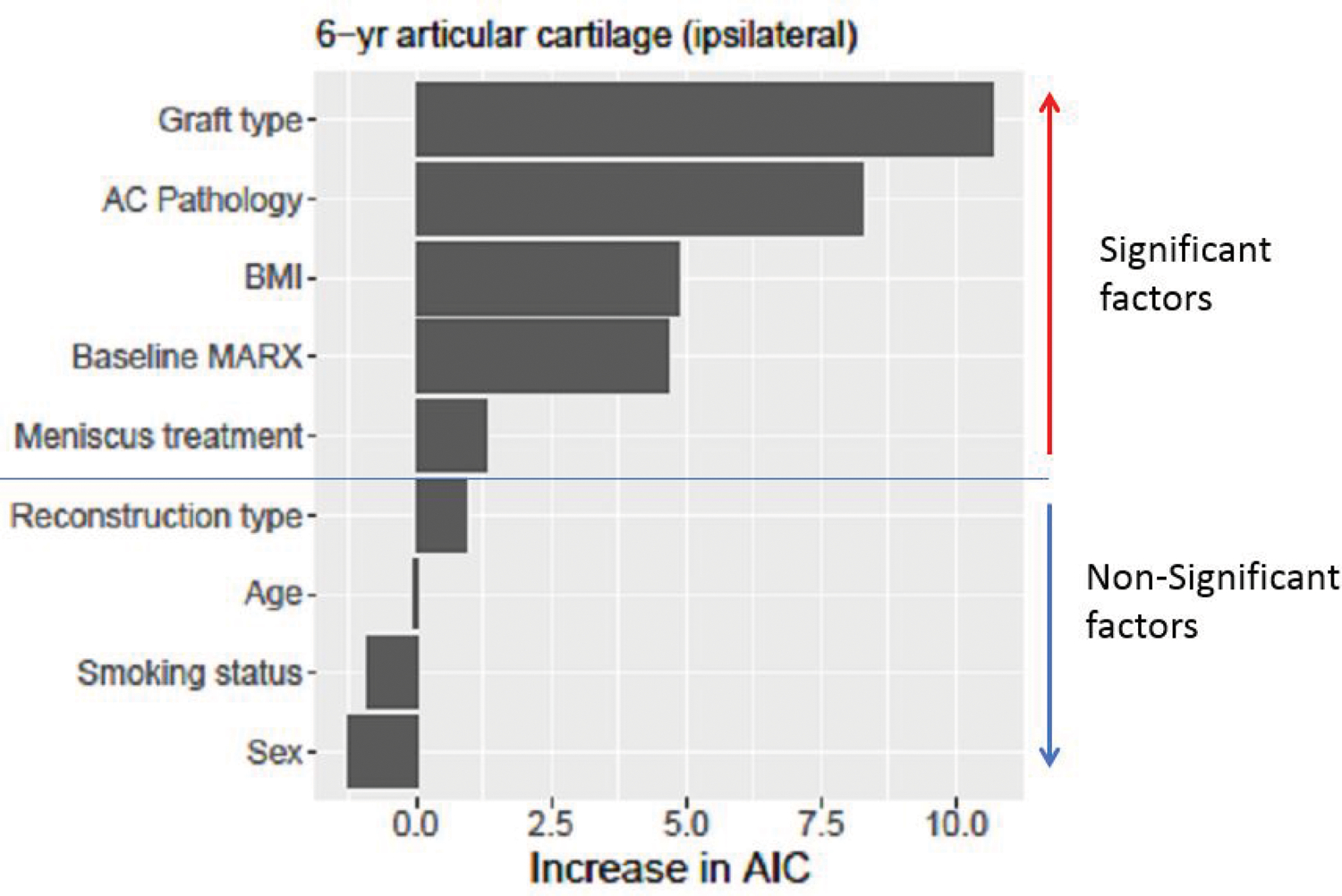
Relative variable importance by increase in AIC in the articular cartilage-related subsequent surgery model. AC=articular cartilage; AIC=Akaike Information Criterion; BMI=body mass index.
Predictors of Subsequent Surgeries for Loss of Motion
Although there were 235 cases for arthrofibrosis-related subsequent surgeries, we were interested in which cases were driven by a loss of motion. The operative reports that mentioned a pre-operative symptom of the patient having loss of motion were tagged. A total of 84 surgical cases involved patients who required surgery for loss of motion. The variables that were found to be significant predictors of having a subsequent surgery related to loss of motion were patients who were female, younger, had lower baseline KOOS symptom subscores, or patients having a soft tissue allograft (compared to a BTB autograft; Table 5). For example, females were 2.5 times more likely to have a subsequent surgery involving loss of motion, compared to their male counterparts (p<0.001).
Table 5.
Odds ratios (OR), 95% confidence intervals (CI), and associated p-values for variables in the loss of motion-related subsequent surgery model.
| Variable | Level | OR (95% CI) | P-value |
|---|---|---|---|
| Sex | Male (reference) | - | |
| Female | 2.49 (1.55,4.02) | <0.001 | |
| Age (years) | 0.60 (0.39,0.92) | 0.02 | |
| BMI | 0.96 (0.73,1.25) | 0.75 | |
| Baseline KOOS Symptom score | 0.54 (0.39,0.76) | <0.001 | |
| Knee Effusion | No (reference) | - | |
| Yes | 1.35 (0.86,2.12) | 0.19 | |
| Concurrent meniscal repair? | No (reference) | - | |
| Yes | 0.74 (0.41,1.33) | 0.31 | |
| Graft type | Autograft - BTB (reference) | - | |
| Autograft - hamstring | 1.08 (0.64,1.84) | 0.77 | |
| Allograft - BTB | 0.83 (0.28,2.48) | 0.75 | |
| Allograft - soft tissue | 1.93 (1.05,3.56) | 0.03 |
Key: P-values less than 0.05 are bolded; Numeric variables compare the 25th and 75th percentiles. Key: BMI=body mass index; BTB = bone-patellar tendon-bone; KOOS=Knee injury and Osteoarthritis Outcome Score.
Figure 4 shows the relative comparison of significance between the variables and shows that sex and baseline KOOS symptom scores were the top 2 predictors; whereas BMI and having a concurrent meniscal repair were the least important. Knee effusion at the time of surgery was not a significant predictor of having a subsequent surgery related to loss of motion in this cohort.
Figure 4.
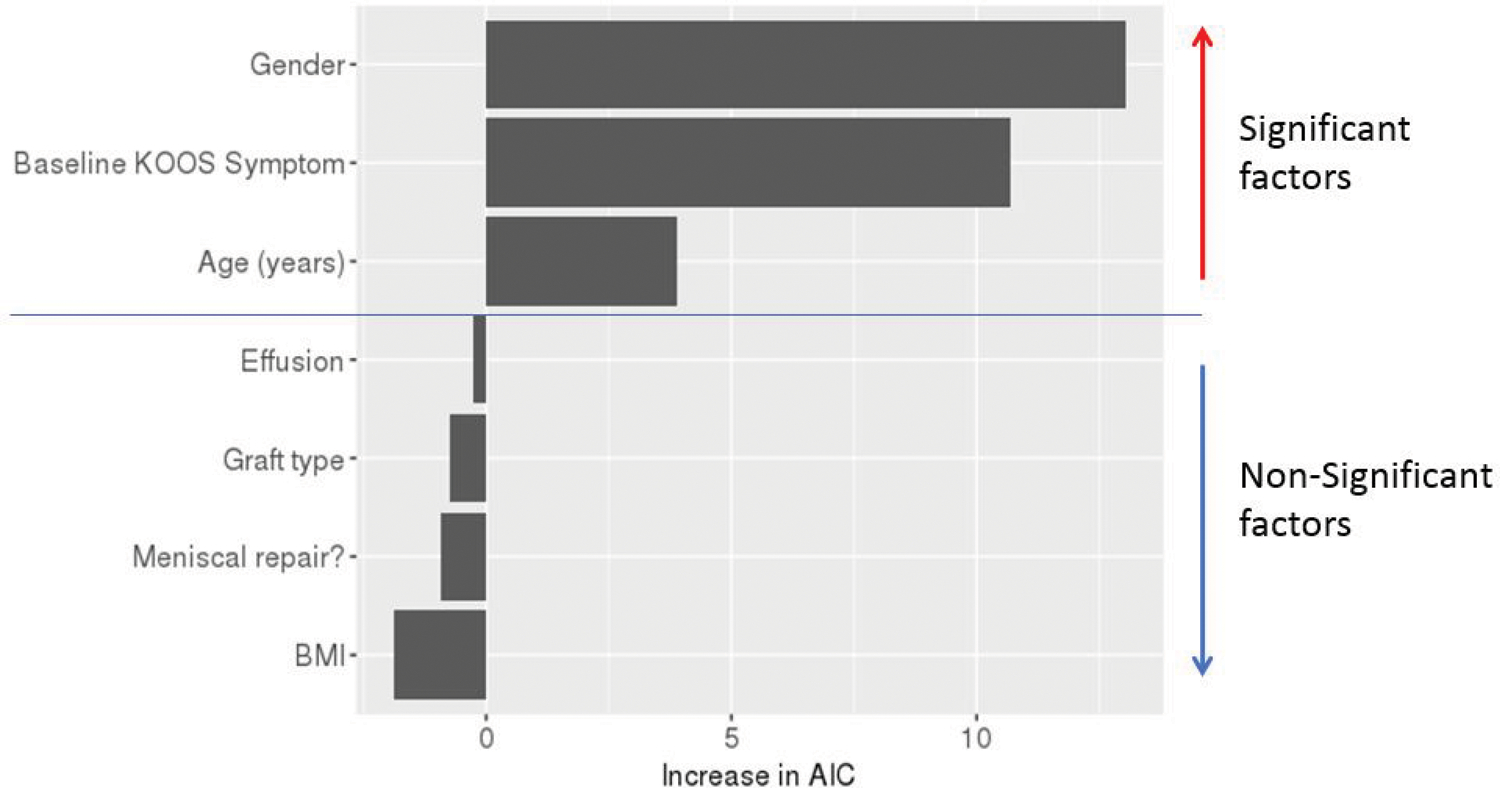
Relative variable importance by increase in AIC in the subsequent surgery model related to loss of motion. AIC=Akaike Information Criterion; BMI=body mass index; KOOS=Knee injury and Osteoarthritis Outcome Score.
DISCUSSION
There are limited data available about subsequent surgeries (non-revision ACL reconstruction) after ACL reconstruction and the risk factors for subsequent surgeries. This was a multicenter longitudinal prospective cohort study that evaluated 3,276 patients undergoing ACL reconstruction for concomitant injuries and subsequent surgeries at 2- and 6-year follow up. This study identified the incidence and risk factors associated with subsequent meniscus, articular cartilage, and surgeries for loss of motion over a 6-year follow-up period. There was a 20% incidence of subsequent surgeries on the ipsilateral knee 6 years following a patient’s index ACL reconstruction. The results of this study fit within the range of subsequent surgery rates after ACL reconstruction reported for mid- to long-term outcomes (4% - 28%).2, 4, 7, 8, 12, 16, 19
Our study includes data from 980 patients reported by Hettrich et al. in 2013,7 and expanded upon it in order to evaluate correlations between index surgery pathologies and subsequent surgeries. Expanding the data had no effect on the overall subsequent surgery rates, but it allowed us to run predictive models on the most common subsequent surgeries. Our models corroborated their findings that younger age and allografts were predictive of any subsequent surgeries. No additional risk factors were identified in that study; whereas this study identified risk factors for specific subsequent surgeries related to the meniscus, articular cartilage, and loss of motion.
There is significant interest in understanding factors associated with subsequent surgery rates after ACL reconstruction in order to try to better identify who is at risk. Predictors of subsequent meniscal surgery in our cohort included patients with lower age, higher baseline Marx activity level, patients who had quit smoking (compared to non-smokers), having an autograft hamstring or allograft reconstruction (compared to an autograft BTB), or having a medial meniscus repair or an untreated medial meniscus tear at the time of the index surgery. In particular, medial meniscal treatment was a strong predictor of future subsequent surgery in our cohort. At the time of index surgery, 14% of the cohort had a concomitant medial meniscal repair and 4.5% had a medial meniscal tear which was left untreated (Table 1). By 6 years, 7.4% of the cohort required a subsequent medial meniscal repair or meniscectomy (Table 2). Patients who had an initial medial meniscus repair were 4.4 times more likely to have a subsequent meniscal-related subsequent surgery, compared with patients with no initial meniscal pathology (p<0.001; Table 3). Similarly, medial meniscal tears that were left untreated were 1.9 times more likely to incur a subsequent surgery (p=0.03; Table 3). Although this 7.4% subsequent surgery rate is consistent with other literature,4 we feel this is an area which can be improved upon. Conversely, lateral meniscus treatment at the time of index ACL reconstruction was relatively insignificant in predicting subsequent meniscal-related surgeries (Table 3; Figure 2). At the time of index surgery, 6.8% of the cohort had a concomitant lateral meniscal repair and 10% had a lateral meniscal tear which was left untreated (Table 1). By 6 years, 4.3% (129/2999) of the cohort required a subsequent medial meniscal repair or meniscectomy (Table 2). Patients with a lateral meniscal repair or a lateral repair left untreated were no more likely to have a subsequent meniscal-related surgery at 6 years compared with patients with no lateral meniscal pathology (Table 3).
Medial meniscus treatment was a strong predictor of subsequent surgery whereas lateral meniscus treatment was not. This may be caused by more stress to the medial meniscus due to less mobility than the lateral meniscus. Repairing smaller tears may decrease subsequent surgery rates. Less traumatizing methods of repair to the meniscus structure on larger tears may also decrease subsequent surgery rates. Multiple inside-out sutures are significantly less traumatic to the meniscus tissue than a smaller number of all-inside sutures that have a much larger diameter needle that punctures through the meniscus. Studies evaluating the subsequent surgery rates of all-inside vs inside-out repairs on the medial meniscus would help clarify which type of repair decreases subsequent surgery rates. Strategies to preserve the meniscus will decrease articular cartilage degeneration at longer-term outcomes.
The variables that were found to be significant predictors of having a subsequent surgery involving the articular cartilage on the ipsilateral knee were patients with higher BMI, higher baseline Marx activity level, having an autograft hamstring or allograft reconstruction (compared to an autograft BTB), having a medial meniscus repair at the time of the index surgery, or having grade 3 or 4 AC pathology in any compartment. Grade 3 and 4 articular cartilage damage can cause additional surgeries because of pain, recurrent effusions, or mechanical symptoms that can all result in worse function. There are likely additional stresses on the meniscus from increased friction due to the articular cartilage damage. Articular cartilage pathology management could potentially decrease subsequent surgery rates. Although this was identified as a risk factor for subsequent surgery, we do not know how management of these defects affects subsequent surgery rates. Future studies looking at the management of concomitant cartilage defects at the time of ACL reconstruction comparing techniques such as chondroplasty, microfracture, osteochondral autograft transfers, or osteochondral allograft transfers could help identify how to decrease this risk.
Loss of motion was another predictor of subsequent surgery after ACL reconstruction. Variables that were predictive of a subsequent surgery were patients who were female, younger, had lower baseline KOOS symptom sub-scores, or patients that had a soft tissue allograft ACL reconstruction. Patients who undergo subsequent surgery for loss of motion have been shown to return to sport at similar times as case-matched controls, but have displayed a lower single leg hop test and lower self-reported function.22 Based upon our data, avoiding allograft reconstructions could decrease subsequent surgeries related to loss of motion. In a study of adolescent patients who had undergone ACL reconstruction, Nwachukwu et al. reported that female sex, older adolescents, concurrent meniscal repair, and reconstruction with a patella tendon autograft were risk factors for arthrofibrosis.14 Additional studies to evaluate risk factors and causes for loss of motion would help guide future preventative treatment and improve outcomes.
Risk factors associated with subsequent surgeries identified in previous studies include younger age at the time of the index surgery,4, 7, 10, 12, 13, 16, 20 female gender,2, 12, 16 higher BMI,17 use of allografts,2, 4, 7, 10, 16 concomitant medial meniscus repair,2 surgeon factors,2, 12 and older age specifically for subsequent cartilage surgeries.2 Our findings are consistent with findings with regards to age, sex, use of allografts, and medial meniscal repair. Since all surgeons in the current study were fellowship-trained in sports medicine, the level of specialized training as an associated variable was not examined.
Limitations of this study include patients lost to follow up (8%) and the inability to obtain operative notes for all subsequent surgeries in a minority of patients (2.1% of the surgeries reported by patients). The rates and types of subsequent surgeries also underestimate the rates of re-injury since some patients may elect to treat additional injuries non-operatively. Surgical techniques and skill levels change over the course of the study, which also can affect the subsequent surgery rates. While this study identified risk factors that predict subsequent surgeries for ipsilateral meniscus tears, cartilage procedures, and loss-of-motion procedures, there were other procedures that we were unable to statistically analyze because of their relative rarity. Future studies could help evaluate risk factors for other specific surgeries such as hardware removal or total knee arthroplasty. These findings can be used to educate physicians and patients about risk factors for a subsequent surgery following ACL reconstruction. Additional research that focuses on techniques that reduce subsequent surgery related to meniscus repair techniques, articular cartilage management techniques, and reducing loss of motion could improve clinical outcomes.
CONCLUSIONS
Subsequent surgery on the ipsilateral knee occurred in 20% of this cohort 6 years following their index ACL reconstruction. The most common subsequent surgery on the ipsilateral knee were related to meniscus (11.9%), revision ACL reconstruction (7.5%), loss of motion (7.8%), or articular cartilage (6.7%). Risk factors for incurring a subsequent meniscus-related surgery on the ipsilateral knee were prior medial meniscus repair, hamstring autograft or allograft reconstruction, increased baseline Marx activity level, younger age, previous ACL reconstruction on the contralateral knee, lateral articular cartilage pathology, and cessation of smoking. The variables that were found to be significant predictors of having a subsequent surgery involving the articular cartilage were patients with higher BMI, higher baseline Marx activity level, autograft hamstring or allograft reconstruction (compared to an autograft BTB), meniscus repair at the time of the index surgery, or grade 3 or 4 articular cartilage pathology in any compartment. Risk factors for incurring a subsequent surgery for loss of motion were young age, female sex, low baseline KOOS symptom subscale score, and a soft-tissue allograft reconstruction. Modifiable risk factors should be changed to improve clinical outcomes. Non-modifiable risk factors can be used to counsel patients regarding risks for subsequent surgery.
What is known about the subject:
Subsequent surgery after ACL reconstruction decreases patient outcomes scores and satisfaction.
What this study adds to existing knowledge:
There are limited data available about subsequent surgeries (non-revision ACL reconstruction) after ACL reconstruction and the risk factors for subsequent surgeries. This study identified the incidence and risk factors associated with subsequent meniscus, articular cartilage, and loss of motion surgeries over a 6-year follow-up period.
References
- 1.Bodendorfer BM, Keeling LE, Michaelson EM, et al. Predictors of Knee Arthrofibrosis and Outcomes after Arthroscopic Lysis of Adhesions following Ligamentous Reconstruction: A Retrospective Case-Control Study with Over Two Years’ Average Follow-Up. J Knee Surg 2019;32(6):536–543. [DOI] [PubMed] [Google Scholar]
- 2.Csintalan RP, Inacio MC, Funahashi TT, Maletis GB. Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med 2014;42(3):619–625. [DOI] [PubMed] [Google Scholar]
- 3.Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 1997;13(4):456–460. [DOI] [PubMed] [Google Scholar]
- 4.Ding DY, Zhang AL, Allen CR, et al. Subsequent Surgery After Revision Anterior Cruciate Ligament Reconstruction: Rates and Risk Factors From a Multicenter Cohort. Am J Sports Med 2017;45(9):2068–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop 2012;83(6):577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagino T, Ochiai S, Senga S, et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg 2015;135(12):1701–1706. [DOI] [PubMed] [Google Scholar]
- 7.Hettrich CM, Dunn WR, Reinke EK, Group M, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med 2013;41(7):1534–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huleatt J, Gottschalk M, Fraser K, et al. Risk Factors for Manipulation Under Anesthesia and/or Lysis of Adhesions After Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med 2018;6(9):2325967118794490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaeding CC, Aros B, Pedroza A, et al. Allograft Versus Autograft Anterior Cruciate Ligament Reconstruction: Predictors of Failure From a MOON Prospective Longitudinal Cohort. Sports Health 2011;3(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee RJ, Margalit A, Nduaguba A, Gunderson MA, Ganley TJ. Risk Factors for Concomitant Collateral Ligament Injuries in Children and Adolescents With Anterior Cruciate Ligament Tears. Orthop J Sports Med 2018;6(11):2325967118810389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am 2009;91(10):2321–2328. [DOI] [PubMed] [Google Scholar]
- 13.Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-Year Survival of Endoscopic Anterior Cruciate Ligament Reconstruction in Patients Aged 18 Years and Younger. Am J Sports Med 2016;44(2):384–392. [DOI] [PubMed] [Google Scholar]
- 14.Nwachukwu BU, McFeely ED, Nasreddine A, et al. Arthrofibrosis after anterior cruciate ligament reconstruction in children and adolescents. J Pediatr Orthop 2011;31(8):811–817. [DOI] [PubMed] [Google Scholar]
- 15.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br 1961;43-b:752–757. [DOI] [PubMed] [Google Scholar]
- 16.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 17.Traven SA, Reeves RA, Xerogeanes JW, Slone HS. Higher BMI predicts additional surgery at the time of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27(8):2552–2557. [DOI] [PubMed] [Google Scholar]
- 18.Ulstein S, Aroen A, Engebretsen L, Forssblad M, Lygre SHL, Rotterud JH. Effect of Concomitant Cartilage Lesions on Patient-Reported Outcomes After Anterior Cruciate Ligament Reconstruction: A Nationwide Cohort Study From Norway and Sweden of 8470 Patients With 5-Year Follow-up. Orthop J Sports Med 2018;6(7):2325967118786219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Dijck RA, Saris DB, Willems JW, Fievez AW. Additional surgery after anterior cruciate ligament reconstruction: can we improve technical aspects of the initial procedure? Arthroscopy 2008;24(1):88–95. [DOI] [PubMed] [Google Scholar]
- 20.Webster KE, Feller JA. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. The American Journal of Sports Medicine 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 21.Webster KE, Feller JA, Kimp A, Devitt BM. Medial meniscal and chondral pathology at the time of revision anterior cruciate ligament reconstruction results in inferior mid-term patient-reported outcomes. Knee Surg Sports Traumatol Arthrosc 2018;26(4):1059–1064. [DOI] [PubMed] [Google Scholar]
- 22.Worsham J, Lowe WR, Copa D, et al. Subsequent Surgery for Loss of Motion After Anterior Cruciate Ligament Reconstruction Does Not Influence Function at 2 Years: A Matched Case-Control Analysis. Am J Sports Med 2019;47(11):2550–2556. [DOI] [PubMed] [Google Scholar]


