Abstract
Aim
To compare Health‐Related Quality of Life (HRQOL) of paediatric patients with newly collected HRQOL data of the general Dutch population, explore responses to individual items and investigate variables associated with HRQOL.
Methods
Children (8–12y) and adolescents (13–17y) from the general population (N = 966) and from a paediatric population (N = 1209) completed the Pediatric Quality of Life Inventory (PedsQLTM) online via the KLIK Patient‐Reported Outcome Measures portal. PedsQLTM scale scores were compared between groups with independent t tests, by age group and gender. Responses to PedsQLTM items were explored using descriptive analyses. Linear regression analyses were performed to determine which variables were associated with HRQOL.
Results
Paediatric patients reported worse HRQOL than the general population on all PedsQLTM scales (p ≤ .001, d = 0.20–1.03), except social functioning, and a high proportion reported problems on PedsQLTM items, for example, ‘I have trouble sleeping’. Younger age, female gender and school absence were negatively associated with HRQOL (β = −0.37–0.10, p ≤ .008).
Conclusion
Paediatric patients reported lower HRQOL than the general population, and school absence, female gender and younger age were associated with lower HRQOL. The results underline the importance to structurally monitor paediatric patients’ HRQOL in clinical practice to detect problems and offer the right help on time.
Keywords: clinical practice, health‐related quality of life, paediatric patients, patient‐reported outcome measures, Pediatric Quality of Life Inventory
Abbreviations
- CHC
Chronic Health Condition
- HRQOL
Health‐Related Quality of Life
- IC
Informed Consent
- PedsQLTM
Pediatric Quality of Life Inventory
- PROM
Patient‐Reported Outcome Measure
Keynotes.
Paediatric patients with various chronic health conditions (N = 1209) who complete Patient‐Reported Outcome Measures (PROMs) in clinical practice, report remarkably lower Health‐Related Quality of Life (HRQOL) compared to the general population (N = 966)
School absence, female gender and younger age are associated with lower HRQOL.
Paying attention to and monitoring HRQOL and psychosocial issues (by using PROMs) in clinical practice is thus important.
1. INTRODUCTION
Previous studies have shown that paediatric patients have more psychosocial problems and a lower Health‐Related Quality of Life (HRQOL) than their healthy peers.1, 2, 3, 4 It is therefore important to pay attention to and monitor these outcomes in daily clinical practice,5, 6 for example by systematically using Patient‐Reported Outcome Measures (PROMs). PROMs are validated questionnaires, completed by patients that measure any aspect of a patients’ health status.7, 8
A system that uses PROMs in daily clinical practice is the evidence‐based KLIK PROM portal, implemented since 2011 after two effectiveness studies.9, 10 With KLIK, paediatric patients and/or parents complete PROMs on the KLIK website (www.hetklikt.nu) at home before an outpatient visit. Answers are converted into an electronic PROfile (KLIK ePROfile) containing several ways of feedback,11 which is discussed during consultation. Currently, >1200 clinicians (e.g., paediatricians, nurses, psychologists) have been trained in using KLIK, and >18,000 patients (from >60 different patient groups) in 30 different centres use KLIK.12, 13 Of the over 300 PROMs available in KLIK, the Pediatric Quality of Life Inventory (PedsQLTM)14, 15 is the most often used PROM. The KLIK ePROfile provides feedback of the PedsQLTM to clinicians over time consisting of individual item and scale score feedback. For individual item feedback, traffic light colours are applied to response categories (never/almost never a problem = green, sometimes a problem = orange, often/almost always a problem = red) to indicate possibly concerning responses and for scale score feedback a reference line of a healthy norm group is included (Figure 1).11
FIGURE 1.
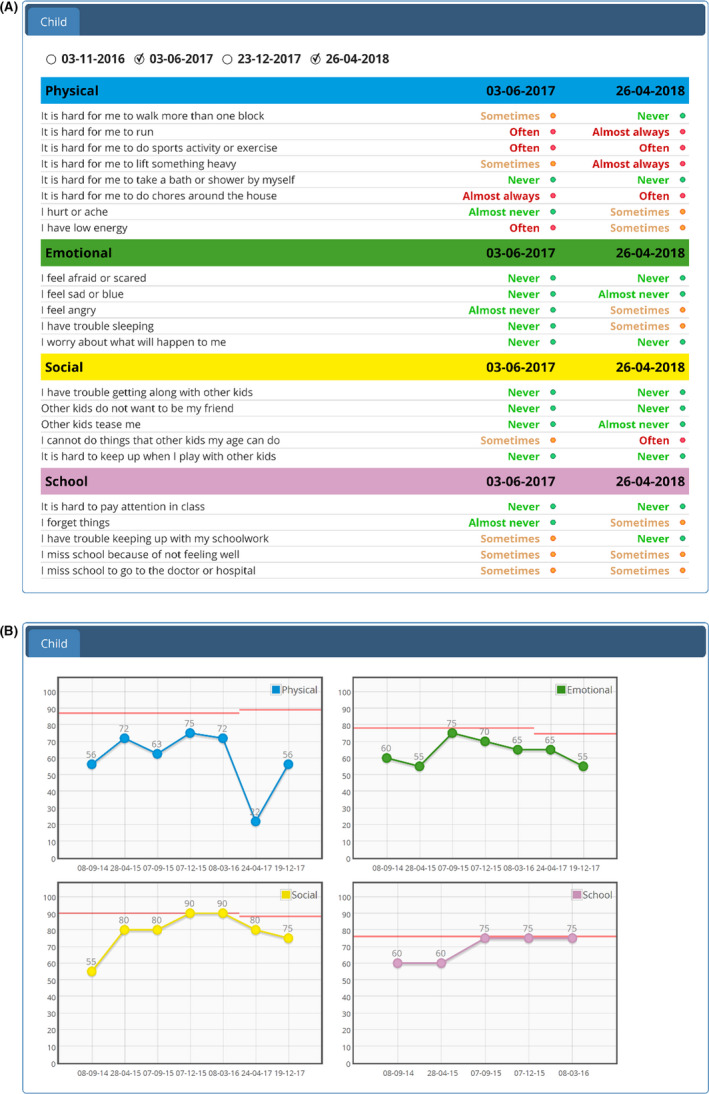
Feedback over time of the PedsQLTM in the KLIK ePROfile: (A) individual items in traffic light colours, (B) scale scores including a healthy reference line
Using the PedsQLTM in KLIK for >9 years has resulted in a large amount of HRQOL data. As previous studies have mostly focused on comparing HRQOL of paediatric patients with one specific chronic health condition (CHC) to a healthy norm group,5, 16, 17 this large group of paediatric patients with various CHCs as a group compared to a general population can give an overall picture of HRQOL of paediatric patients. This overall picture of HRQOL of a large paediatric patient group with various CHCs was also requested by clinicians in our yearly KLIK evaluation and recent focus groups (e.g., to use as comparative data for rare diseases). Furthermore, this study can provide us with more information on which HRQOL domains paediatric patients and the general population differ, as results from previous studies are inconclusive.4, 14 Additionally, no previous studies looked at individual items of the PedsQLTM, even though this might help explain the possible differences that are found on domain score level. As sociodemographic and school variables are also collected with KLIK, it is possible to investigate which variables are associated with HRQOL. Previous studies showed that older age and female gender,1, 18, 19, 20 non‐western ethnicity,21 lower parental education,22 school absence23 and repeating grades24 were associated with lower HRQOL. This information may help to target and provide interventions to children and adolescents who are most at risk for HRQOL problems. Finally, since the currently used Dutch normative data in KLIK are outdated (collected in 2006–2007) and representativeness for the general population is not optimal as data were only collected in Amsterdam and surroundings,15 we collected new normative data for the present study. The aims of this study were to (A) compare HRQOL scale scores of paediatric patients with newly collected normative data of the general population, (B) explore the responses (proportion of respondents reporting problems) to individual HRQOL items for paediatric patients and the general population, and (C) investigate which sociodemographic and school variables are associated with HRQOL.
2. METHODS
2.1. Participants and procedures
2.1.1. General population
Dutch norm data for the PedsQLTM 4.0 for children and adolescents aged 8–17 years in the general population were collected online by research agency TNS NIPO operating under the name of ‘Kantar Public ©’ between February and April 2018. The Kantar panel consists of families living across the Netherlands that provided informed consent to be approached through e‐mail for completing PROMs for a small financial compensation. To obtain at least 1000 respondents, a stratified sample of 2385 children and adolescents was drawn from the Kantar panel. A two‐step stratified random sampling technique was used to ensure that the sample was representative (with a maximum deviation of 2.5% of the distribution in the Dutch population, based on the Gold Standard 2017 – Statistics Netherlands, www.cbs.nl/en‐gb) on key demographics: sex, ethnicity, social class and educational level. Children and adolescents had to be fluent in Dutch (assessed by Kantar). E‐mails were sent to the parents of 2385 children with a login code that granted access to the KLIK research website. After logging in, parents (child 8–15 years) and adolescents (12–17 years) provided informed consent. Thereafter, they were asked to complete their questionnaires (parents – sociodemographic questionnaire, children/adolescents – PedsQLTM 4.0 and school questions) independently.
2.1.2. CHC group
For the CHC group, PedsQLTM data of paediatric patients (8–17 years) using KLIK for clinical purposes for their CHC on the outpatient clinic in the Emma Children's Hospital Amsterdam University Medical Centers (UMC) were used. Patients from the following condition groups were eligible: defecation disorders, oncology, rheumatology, endocrinology, IBD, sickle cell disease, haemophilia, cleft lip, nephrology, HIV, dermatology, craniofacial abnormalities, spherocytosis, cystic fibrosis, lysosomal storage disorders, intensive care follow‐up, Marfan syndrome, spina bifida, home parenteral nutrition, feeding disorders and muscular disorders. During registration for KLIK, patients’ (12–17 years) and parents’ (child 8–15 years) informed consent (IC) was asked to use their data for scientific purposes. Paediatric patients with IC, fluent in Dutch (assessed by clinician), with one of the above mentioned CHCs, and who completed the PedsQLTM 4.0 between June 2011 and October 2017, were eligible for inclusion in the CHC group. The first assessment of HRQOL in KLIK was used to avoid effects that KLIK could have on HRQOL outcomes (as a result of discussing HRQOL issues regularly). Additionally, as the first assessment in KLIK happens in all stages of the disease, both patients recently diagnosed as well as patients with a long disease duration were included. When patients did not have access to a computer, there was a possibility to complete the PROMs on a computer at the outpatient clinic. Patients registered for KLIK who completed questionnaires for clinical purposes, but without IC for scientific research, were considered non‐participants.
Mode of administration of the questionnaires was identical for both groups. Anonymity and data security were guaranteed by the websites, compliant with national standards, and information regarding these topics was available on the websites. Data collections were performed with approval of the medical ethics committee of the Amsterdam UMC, location AMC.
2.2. Measures
2.2.1. Sociodemographic questionnaire
Parents in both the general population as of paediatric patients using KLIK completed a similar sociodemographic questionnaire online, containing questions concerning the parent (age, country of birth, educational level) and the child (age, gender). Parental educational level was divided into three categories: low (primary education, lower vocational education, lower/middle general secondary education), intermediate (middle vocational education, higher secondary education, pre‐university education) and high (higher vocational education, university). In addition, paediatric patients completed questions regarding the following school variables: educational level, grade repetition (no/yes) and school absence (in days) in the last three months. Paediatric patients’ CHC type (initially reported by the clinician) was obtained from the KLIK website.
2.2.2. PedsQLTM 4.0
HRQOL was measured with the Dutch version of the generic PedsQLTM 4.0,14, 15 (self‐report 25) for children (8–12 years) and adolescents (13–17 years). The PedsQLTM contains 23 items in four scales: physical health (8 items), emotional functioning (5 items), social functioning (5 items) and school functioning (5 items). A psychosocial health score — combined score of the emotional, social, and school functioning subscales — and a total scale score can be computed. Items are scored on a 5‐point Likert scale from 1 ‘Never a problem’ to 5 ‘Almost always a problem’, with a one‐week recall period. Answers are transformed into a 0–100 scale, with a higher score representing a better HRQOL. Previous research has shown that reliability and validity of the PedsQLTM are good.14, 15
2.3. Statistical analyses
Descriptive analyses were used to characterise the general population and CHC group. Baseline differences in gender and age between participants and non‐participants within both groups and between participants in the general population and CHC group were analysed for children (8–12 years) and adolescents (13–17 years), using χ2 tests for dichotomous and categorical variables and independent t tests for continuous variables. Effect sizes (Cohen's d) were calculated. Since sample sizes were large in this study, parametric tests could be performed.
To assess reliability of the PedsQLTM versions (8–12 and 13–17 years) in the CHC and general population group, internal consistency estimates (Cronbach's α) were calculated. Estimates of 0.70 or greater were considered sufficient.26 Thereafter, mean PedsQLTM scale scores and standard deviations were calculated by age group and gender (as gender differences were found within the general population and CHC group). To examine differences on the PedsQLTM scales between the CHC group and general population, independent t tests were performed by age group and gender. Effect sizes (Cohen's d) were calculated by dividing the difference in mean scale scores between the general population and the CHC group by the pooled SD. Effect sizes of 0.2 were considered small, 0.5 moderate and 0.8 large.27 For individual items, PedsQLTM answer categories were recoded binary (0; never, almost never, sometimes, 1; often, almost always), in line with previous studies.17, 28 Thereafter, descriptive analyses (percentages) were performed for each item to explore the proportion of respondents in the CHC group and general population reporting to experience ‘often’ or ‘almost always’ a problem on the concerning item. These analyses were also performed by age group and gender.
Finally, to investigate which factors regarding the child (age, gender, school absence, grade retention) and the parent (country of birth, education) are associated with HRQOL in the CHC group, multiple linear regression analyses were performed for each PedsQLTM subscale score. No variables had to be excluded due to multicollinearity (no correlations >0.80). Standardised regression coefficients (β) were reported, where coefficients of 0.1 were considered small, 0.3 moderate and 0.5 large for continuous variables. For binary‐coded variables (e.g., gender), regression coefficients of 0.2 were considered small, 0.5 moderate and 0.8 large.29
The Statistical Package for Social Sciences (SPSS) version 25.0 was used for all analyses.
3. RESULTS
3.1. Sociodemographic characteristics
In Table 1, sociodemographic characteristics of participants and non‐participants of the general population and CHC group are presented.
TABLE 1.
Sociodemographic characteristics of participants and non‐participants of the general population and CHC group
| Participants | Non‐participants | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 8–12 years | 13–17 years | 8–12 years | 13–17 years | ||||||||||||||
| GP group | Child characteristics (N = 966) | N | M | SD | N | M | SD | N | M | SD | N | M | SD | ||||
| Age (years) | 475 | 10.6e | 1.5 | 491 | 15.5c, f | 1.4 | 717 | 10.2 | 1.4 | 677 | 15.0 | 1.4 | |||||
| % | % | % | % | ||||||||||||||
| Gender (female) | 231 | 48.6 | 239 | 48.7 | 331 | 46.2 | 320 | 47.3 | |||||||||
| Parent characteristics | N | M | SD | N | M | SD | |||||||||||
| Age (years) | 469 | 43.3 | 5.7 | 488 | 48.2 | 5.1 | |||||||||||
| % | % | ||||||||||||||||
| Country of birth | 469 | 488 | |||||||||||||||
| Netherlands | 421 | 89.8 | 454 | 93.0 | |||||||||||||
| Other | 48 | 10.2 | 34 | 7.0 | |||||||||||||
| Educational levela | 469 | 488 | |||||||||||||||
| Low | 53 | 11.3 | 63 | 12.9 | |||||||||||||
| Intermediate | 224 | 47.8 | 237 | 48.6 | |||||||||||||
| High | 192 | 40.9 | 188 | 38.5 | |||||||||||||
|
CHC group |
Child characteristics (N = 1209) | N | M | SD | N | M | SD | N | M | SD | N | M | SD | ||||
| Age (years) | 589 | 10.4d, e | 1.4 | 620 | 15.7c, f | 1.4 | 274 | 10.6 | 1.5 | 238 | 14.8 | 1.1 | |||||
| % | % | % | % | ||||||||||||||
| Gender (female) | 269 | 45.7 | 330 | 53.2 | 128 | 46.7 | 125 | 52.5 | |||||||||
| Clinician‐reported CHCb | |||||||||||||||||
| Defecation disorders | 110 | 18.7 | 39 | 6.3 | 38 | 13.9 | 22 | 9.2 | |||||||||
| Oncology | 98 | 16.6 | 70 | 11.3 | 11 | 4.0 | 14 | 5.9 | |||||||||
| Rheumatology | 83 | 14.1 | 149 | 24.0 | 52 | 19.0 | 61 | 25.6 | |||||||||
| Endocrinology | 56 | 9.5 | 94 | 15.2 | 27 | 9.9 | 29 | 12.2 | |||||||||
| IBD | 24 | 4.1 | 89 | 14.4 | 7 | 2.6 | 7 | 2.9 | |||||||||
| Sickle cell disease | 10 | 1.7 | 20 | 3.2 | 55 | 20.1 | 33 | 13.9 | |||||||||
| Other | 208 | 35.3 | 159 | 25.6 | 84 | 30.5 | 72 | 30.3 | |||||||||
| Parent characteristics | N | M | SD | N | M | SD | |||||||||||
| Age (years) | 564 | 42.7 | 5.3 | 449 | 47.1 | 4.9 | |||||||||||
| % | % | ||||||||||||||||
| Country of birth | 587 | 468 | |||||||||||||||
| Netherlands | 513 | 87.4 | 410 | 87.6 | |||||||||||||
| Other | 74 | 12.6 | 58 | 12.4 | |||||||||||||
| Educational levela | 578 | 468 | |||||||||||||||
| Low | 61 | 10.6 | 62 | 13.3 | |||||||||||||
| Intermediate | 244 | 42.2 | 225 | 48.3 | |||||||||||||
| High | 273 | 47.2 | 179 | 38.4 | |||||||||||||
Abbrevations: CHC, Chronic Health Condition; GP, General Population.
Highest level completed: Low: primary education, lower vocational education, lower and middle general secondary education; Intermediate: middle vocational education, higher secondary education, pre‐university education; High: higher vocational education, university.
Only most common conditions groups (>10% in one of the age groups) are reported, other: haemophilia, cleft lip, nephrology, HIV, dermatology, craniofacial abnormalities, spherocytosis, cystic fibrosis, lysosomal storage disorders, Intensive Care follow‐up, Marfan syndrome, spina bifida, home parenteral nutrition, feeding disorders and muscular disorders.
Participants differed significantly from non‐participants at p ≤ .001, range d = .28–.69.
participants differed significantly from non‐participants at p = .03, d = .16.
GP differed significantly from CHC at p = .007, d = .17.
GP differed significantly from CHC at p = .013, d = .15.
In the general population group, 966 children (8–12 years) and adolescents (13–17 years) participated (response rate = 40.5%). The sample was representative for the Dutch population (maximum deviation of 2.5% on key demographics). Baseline differences in age were found between participants and non‐participants in the general population group: participating children (M age = 10.6) were older than non‐participating children (M age = 10.2, p ≤ .001, d = −.28) and participating adolescents (M age = 15.5) were older than non‐participating adolescents (M age = 15.0, p ≤ .001, d = −.39). No baseline differences in gender were found between participants and non‐participants in the general population group.
The CHC group consisted of 1209 paediatric patients aged 8–17 years, under treatment at the Emma Children's Hospital (response rate = 70.2%). For children (8–12 years), the most often reported condition groups were defecation disorders (18.7%) and oncology (16.6%) and for adolescents (13–17 years) rheumatology (24.0%) and endocrinology (15.2%). Baseline differences in age were found between participants and non‐participants in the CHC group: participating children (M age = 10.4) were younger than non‐participating children (M age = 10.6, p = .03, d = .16) and participating adolescents (M age = 15.7) were older than non‐participating adolescents (M age = 14.8, p ≤ .001, d = −.69). No baseline differences in gender were found between participants and non‐participants in the CHC group.
Finally, baseline differences in age were found between participants in the general population and CHC group: participating children were older in the general population group (M age = 10.6) compared to the CHC group (M age = 10.4, p = .007, d = .17) and participating adolescents were younger in the general population group (M age = 15.5) compared to the CHC group (M age = 15.7, p = .013, d = −.15). No baseline differences in gender were found between the general population group and CHC group.
3.2. Reliability
All internal consistency estimates were sufficient. In the CHC group, Cronbach's alpha for the 8–12 version ranged from .70–.90 and for the 13–17 version from .75–.92. In the general population group, Cronbach's alpha ranged from .76–.91 for the 8–12 version and from .82–.93 for the 13–17 version.
3.3. PedsQLTM scale scores CHC group versus general population
In Table 2, the PedsQLTM scale scores of the general population and CHC group split by age group and gender are provided.
TABLE 2.
PedsQLTM mean scale scores of the general population versus CHC group by age group and gender
| GP group | CHC group | GP vs CHC | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PedsQLTM scale | N | M | SD | N | M | SD | p | d | |
| Age group 8–12 | Total score | 475 | 85.34 | 11.66 | 589 | 76.19 | 15.16 | .000 | .67 |
| Physical health | 475 | 92.59 | 11.17 | 589 | 78.83b | 19.94 | .000 | .83 | |
| Psychosocial health | 475 | 81.48a | 13.84 | 589 | 74.78 | 15.41 | .000 | .45 | |
| Emotional functioning | 475 | 78.17 | 17.09 | 589 | 70.90 | 19.40 | .000 | .40 | |
| Social functioning | 475 | 83.49a | 16.87 | 589 | 81.35 | 17.62 | .044 | .12 | |
| School functioning | 475 | 82.77a | 15.44 | 589 | 72.09 | 18.28 | .000 | .63 | |
| Age group 8–12 female | Total score | 231 | 86.75 | 11.11 | 269 | 75.18 | 15.14 | .000 | .87 |
| Physical health | 231 | 92.52 | 11.64 | 269 | 76.21 | 19.99 | .000 | .98 | |
| Psychosocial health | 231 | 83.67 | 12.65 | 269 | 74.63 | 15.30 | .000 | .64 | |
| Emotional functioning | 231 | 79.13 | 16.61 | 269 | 68.94 | 19.79 | .000 | .55 | |
| Social functioning | 231 | 86.19 | 15.17 | 269 | 80.99 | 17.19 | .000 | .32 | |
| School functioning | 231 | 85.69 | 14.02 | 269 | 73.96 | 17.76 | .000 | .73 | |
| Age group 8–12 male | Total score | 244 | 84.01 | 12.03 | 320 | 77.04 | 15.16 | .000 | .50 |
| Physical health | 244 | 92.65 | 10.74 | 320 | 81.04 | 19.66 | .000 | .71 | |
| Psychosocial health | 244 | 79.40 | 14.60 | 320 | 74.91 | 15.53 | .001 | .30 | |
| Emotional functioning | 244 | 77.25 | 17.52 | 320 | 72.55 | 18.94 | .003 | .26 | |
| Social functioning | 244 | 80.94 | 18.01 | 320 | 81.66 | 17.98 | .641 | –.04 | |
| School functioning | 244 | 80.00 | 16.22 | 320 | 70.52 | 18.59 | .000 | .54 | |
| Age group 13–17 | Total score | 491 | 84.51c | 13.49 | 620 | 74.99d | 16.22 | .000 | .63 |
| Physical health | 491 | 90.66c | 13.35 | 620 | 73.62d | 22.89 | .000 | .88 | |
| Psychosocial health | 491 | 81.24 | 15.48 | 620 | 75.72d | 15.22 | .000 | .36 | |
| Emotional functioning | 491 | 80.37c | 19.45 | 620 | 76.54d | 19.25 | .001 | .20 | |
| Social functioning | 491 | 85.22 | 16.99 | 620 | 83.41d | 16.87 | .077 | .11 | |
| School functioning | 491 | 78.12 | 17.76 | 620 | 67.20 | 19.17 | .000 | .59 | |
| Age group 13–17 female | Total score | 239 | 82.74 | 14.67 | 330 | 71.10 | 16.73 | .000 | .73 |
| Physical health | 239 | 88.51 | 14.92 | 330 | 67.64 | 23.44 | .000 | 1.03 | |
| Psychosocial health | 239 | 79.67 | 16.63 | 330 | 72.94 | 16.08 | .000 | .41 | |
| Emotional functioning | 239 | 76.97 | 21.23 | 330 | 72.83 | 19.71 | .017 | .20 | |
| Social functioning | 239 | 83.31 | 17.99 | 330 | 80.50 | 17.90 | .066 | .16 | |
| School functioning | 239 | 78.72 | 17.74 | 330 | 65.48 | 20.15 | .000 | .69 | |
| Age group 13–17 male | Total score | 252 | 86.19 | 12.05 | 290 | 79.42 | 14.42 | .000 | .51 |
| Physical health | 252 | 92.70 | 11.33 | 290 | 80.43 | 20.24 | .000 | .73 | |
| Psychosocial health | 252 | 82.72 | 14.18 | 290 | 78.88 | 13.53 | .001 | .28 | |
| Emotional functioning | 252 | 83.59 | 17.03 | 290 | 80.76 | 17.84 | .060 | .16 | |
| Social functioning | 252 | 87.04 | 15.82 | 290 | 86.72 | 14.97 | .809 | .02 | |
| School functioning | 252 | 77.54 | 17.79 | 290 | 69.16 | 17.82 | .000 | .47 | |
A higher score (0–100) indicates a better HRQOL. Differences at p ≤ .008 are considered significant, Bonferroni corrected for multiple testing by dividing .05 by the amount of tests.6 Significant p‐values for the general population group versus the CHC group are shown in bold.
Abbrevations: CHC, Chronic Health Condition; d, effect size; GP, General Population.
Females scored significantly higher than males within the age group 8–12 of the GP.
Females scored significantly lower than males within the age group 8–12 of the CHC group.
Females scored significantly lower than males within the age group 13–17 of the GP.
Females scored significantly lower than males within the age group 13–17 of the CHC group.
3.3.1. Children (8–12 years)
Children with CHCs reported significantly lower HRQOL on five out of six PedsQLTM scales than the general population (p ≤ .001, range d = .40–.83). Boys and girls with CHCs reported significantly lower HRQOL on five out of six and six out of six PedsQLTM scales than boys and girls in the general population (p ≤ .003 range d = .26–.98).
3.3.2. Adolescents (13–17 years)
Adolescents with CHCs reported significantly lower HRQOL on five out of six PedsQLTM scales than the general population (p ≤ .001, range d = .20–.88). Boys and girls with CHCs reported significantly lower HRQOL on four out of six PedsQLTM scales than boys and girls in the general population (p ≤ .001, range d = .28–1.03).
3.4. PedsQLTM item scores CHC group and general population
In Table 3, the proportion of respondents reporting problems on PedsQLTM items in the general population and CHC group split by age group and gender are provided.
TABLE 3.
Proportion of children and adolescents reporting ‘often a problem’ or ‘almost always a problem’ on the PedsQLTM items in the general population and the CHC group by age group and gender
| PedsQLTM scale | Items | 8–12 years | 13–17 years | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | ||||||||
| GP N = 475 | CHC N = 589 | GP N = 231 | CHC N = 269 | GP N = 244 | CHC N = 320 | GP N = 491 | CHC N = 620 | GP N = 239 | CHC N = 330 | GP N = 252 | CHC N = 290 | ||
| % | % | % | % | % | % | % | % | % | % | % | % | ||
|
Physical health |
It is hard for me to walk more than one block | 0.8 | 5.9 | 1.3 | 7.4 | 0.4 | 4.7 | 0.6 | 7.3 | 0.4 | 7.9 | 0.8 | 6.6 |
| It is hard for me to run | 1.7 | 11.7 | 2.2 | 12.6 | 1.2 | 10.9 | 4.5 | 22.4 | 6.3 | 30.9 | 2.8 | 12.8 | |
| It is hard for me to do sports activity or exercise | 1.9 | 12.6 | 2.2 | 13.8 | 1.6 | 11.6 | 3.5 | 19.7 | 5.0 | 27.3 | 2.0 | 11.0 | |
| It is hard for me to lift something heavy | 1.5 | 9.5 | 1.7 | 11.2 | 1.2 | 8.1 | 1.8 | 13.9 | 2.5 | 19.4 | 1.2 | 7.6 | |
| It is hard for me to take a bath or shower by myself | 1.9 | 5.9 | 2.2 | 4.5 | 1.6 | 7.2 | 1.4 | 3.4 | 1.3 | 3.3 | 1.6 | 3.4 | |
| It is hard for me to do chores around the house | 1.9 | 6.6 | 1.7 | 6.7 | 2.0 | 6.6 | 3.3 | 8.4 | 4.2 | 8.5 | 2.4 | 8.3 | |
| I hurt or ache | 5.1 | 19.4 | 5.6 | 25.7 | 4.5 | 14.1 | 5.1 | 23.1 | 7.1 | 30.9 | 3.2 | 14.1 | |
| I have low energy | 1.1 | 15.8 | 0.9 | 19.3 | 1.2 | 12.8 | 6.5 | 26.0 | 10.0 | 33.6 | 3.2 | 17.2 | |
|
Emotional functioning |
I feel afraid or scared | 2.9 | 6.1 | 2.6 | 6.3 | 3.3 | 5.9 | 4.1 | 2.4 | 6.3 | 3.6 | 2.0 | 1.0 |
| I feel sad or blue | 3.4 | 7.3 | 3.9 | 8.6 | 2.9 | 6.3 | 6.3 | 6.9 | 9.2 | 9.7 | 3.6 | 3.8 | |
| I feel angry | 5.1 | 10.5 | 2.2 | 8.9 | 7.8 | 11.9 | 4.3 | 6.0 | 5.9 | 6.1 | 2.8 | 5.9 | |
| I have trouble sleeping | 7.2 | 23.3 | 7.4 | 25.3 | 7.0 | 21.6 | 10.4 | 16.8 | 14.2 | 20.3 | 6.7 | 12.8 | |
| I worry about what will happen to me | 4.8 | 13.8 | 5.2 | 17.5 | 4.5 | 10.6 | 6.9 | 7.7 | 9.6 | 8.5 | 4.4 | 6.9 | |
|
Social functioning |
I have trouble getting along with other kids/teens | 3.4 | 4.9 | 1.7 | 4.5 | 4.9 | 5.3 | 4.1 | 2.3 | 5.9 | 2.4 | 2.4 | 2.1 |
| Other kids/teens do not want to be my friend | 7.4 | 4.9 | 6.5 | 4.8 | 8.2 | 5.0 | 5.5 | 2.4 | 7.9 | 2.4 | 3.2 | 2.4 | |
| Other kids/teens tease me | 2.7 | 4.4 | 2.2 | 4.5 | 3.3 | 4.4 | 1.8 | 1.1 | 2.1 | 1.2 | 1.6 | 1.0 | |
| I cannot do things that other kids/teens my age can do | 3.4 | 13.6 | 3.5 | 11.2 | 3.3 | 15.6 | 5.5 | 18.7 | 6.3 | 22.4 | 4.8 | 14.5 | |
| It is hard for me to keep up when I play with other kids/It is hard for me to keep up with my peers | 2.7 | 6.1 | 0.9 | 7.4 | 4.5 | 5.0 | 3.5 | 11.3 | 4.2 | 15.8 | 2.8 | 6.2 | |
| School functioning | It is hard to pay attention in class | 6.7 | 13.1 | 4.8 | 10.0 | 8.6 | 15.6 | 9.8 | 12.4 | 10.9 | 13.9 | 8.7 | 10.7 |
| I forget things | 6.1 | 12.9 | 3.9 | 9.7 | 8.2 | 15.6 | 10.2 | 17.9 | 9.6 | 20.6 | 10.7 | 14.8 | |
| I have trouble keeping up with my schoolwork | 7.2 | 12.6 | 4.3 | 8.2 | 9.8 | 16.3 | 10.0 | 15.2 | 8.8 | 15.5 | 11.1 | 14.8 | |
| I miss school because of not feeling well | 0.8 | 7.1 | 0.4 | 7.1 | 1.2 | 7.2 | 1.6 | 11.5 | 2.1 | 14.5 | 1.2 | 7.9 | |
| I miss school to go to the doctor or hospital | 0.4 | 13.8 | 0.4 | 14.5 | 0.4 | 13.1 | 2.0 | 14.8 | 3.8 | 16.1 | 0.4 | 13.4 | |
Abbrevations: CHC, Chronic Health Condition; GP, General Population.
3.4.1. Children (8–12 years)
The items ‘I hurt or ache’, ‘I have low energy’ and ‘I have trouble sleeping’ were the most reported problems by children with CHCs (15.8%–23.3%), especially by girls with CHCs (19.3%–25.7%). The items ‘I worry about what will happen to me’, ‘I cannot do things that other kids my age can do’ and ‘I miss school to go to the doctor or hospital’ were other often reported problems by children with CHCs (13.6%–13.8%). Children in the general population rated these items less often to be a problem (0.4%–7.2%).
3.4.2. Adolescents (13–17 years)
The items ‘I have low energy’, ‘I hurt or ache’, ‘It is hard for me to run’ and ‘It is hard for me to do sports activity or exercise’ were the most reported problems by adolescents with CHCs (19.7%–26%), especially by girls with CHCs (27.3%–33.6%). Additionally, the items ‘I have trouble sleeping’, ‘I cannot do things that other teens my age can do’, ‘I forget things’ and ‘I miss school to go to the doctor or hospital’ were other often reported problems by adolescents with CHCs in all three groups (14.8%–18.7%). Adolescents in the general population rated these items less often to be a problem (2%–10.4%).
3.5. Variables associated with PedsQLTM scale scores within the CHC group 8–17 years
In Table 4, the regression analyses outcomes are presented regarding the variables associated with the PedsQLTM scales in the CHC group. Higher age was significantly associated with higher scores for psychosocial health, emotional functioning and social functioning (β‐range: 0.12–0.20, p ≤ .001). Being a boy was significantly associated with higher scale scores (β‐range: 0.10–0.19, p≤ .008), except for school functioning. More school absence was significantly associated with lower scores on all scales (β‐range:−0.37–0.20, p ≤ .001). Grade retention was significantly associated with a lower score on school functioning (β = −0.09, p ≤ .008).
TABLE 4.
Standardised regression coefficients (β) of variables associated with PedsQLTM scales in the CHC group (N = 1209)
| Total score | Physical health | Psychosocial health | Emotional functioning | Social functioning | School functioning | |
|---|---|---|---|---|---|---|
| Predictors | β | β | β | β | β | β |
| Age | 0.05 | −0.06 | 0.12b | 0.22b | 0.13b | −0.07 |
| Gender (boy) | 0.16b | 0.19b | 0.10a | 0.15b | 0.10a | 0.00 |
| Parental country of birth (foreign country) | 0.04 | 0.04 | 0.04 | 0.05 | −0.02 | 0.06 |
| Parental education (high) | 0.07 | 0.08 | 0.06 | 0.05 | 0.05 | 0.05 |
| School absence | −0.37b | −0.37b | −0.31b | −0.22b | −0.20b | −0.35b |
| Grade retention (yes) | −0.05 | −0.01 | −0.08 | −0.07 | −0.04 | −0.09a |
| R2 | .17 | .19 | .12 | .11 | .06 | .15 |
| F Test | 27.14b | 31.49b | 17.93b | 15.94b | 8.67b | 23.28b |
Abbreviations: CHC, Chronic Health Condition; F test, Statistic of Multiple Linear Regression analysis; R 2, Explained variance.
Differences at p ≤ .008 are considered significant, Bonferroni corrected for multiple testing by dividing.05 by the amount of tests.6
Difference at p ≤ .001.
4. DISCUSSION
In this study, PedsQLTM data of paediatric patients with CHCs, collected with KLIK in clinical practice, were compared to newly collected normative PedsQLTM data of the general Dutch population. Paediatric patients reported worse HRQOL on nearly all PedsQLTM scales, especially on physical health, compared to the general population, with moderate to large effect sizes. Additionally, a high proportion of paediatric patients reported problems on the PedsQLTM items. School absence, younger age and being a girl were negatively associated with the HRQOL scales, with small to moderate regression coefficients.
Our results regarding the lower PedsQLTM scores for the CHC group are in accordance with previous literature.1, 2, 4, 30 In contrast with earlier studies,1, 4 no differences were found between the CHC group and general population on the social functioning scale. However, paediatric patients in our sample did report quite some problems on individual item level for social functioning. Paediatric patients reported difficulties on items with a physical component (e.g., I cannot do things that other kids/teens my age can do). This implicates that paediatric patients perceive difficulty to participate in the same activities as their peers. Not many problems were reported on items regarding social acceptance (e.g., Other kids/teens do not want to be my friend), which matches the outcome of a large meta‐analysis where no differences were found on the social acceptance scale as well.4 It is known that social acceptance problems (e.g., being bullied) are more often reported by patients that have external visible CHCs like craniofacial disorders, osteogenesis imperfecta and spina bifida.19, 31 Many of the CHCs in our heterogeneous sample were not visibly present, which might explain why not many problems were reported on these items. In contrast to the social functioning scale, this study showed differences on the emotional functioning scale, while previous studies did not report this difference.5, 15, 17 When looking at the individual items of this scale, the difference might be explained by the higher proportion of paediatric patients reporting to have sleep and worrying problems. Another interesting finding was found in the regression analyses, where higher age was associated with better HRQOL. While this finding is in contrast with previous studies showing that higher age was associated with lower HRQOL in two general population groups 18, 20 and a chronic conditions group (gastrointestinal disorders),1 a recent large meta‐analysis in children with CHCs did not find an effect of age on HRQOL at all.19 A possible explanation for the positive association found in the current study could be the differences in CHCs between the younger (e.g., defecation disorders and cancer) and older patients (e.g., rheumatology and endocrinology). However, the study by Pinquart 19 displayed that these particular patient groups show similar declines in HRQOL compared to the general population. It would be interesting to further investigate how the increase in HRQOL over age can be explained.
The results of this study however underline that HRQOL of paediatric patients is affected and that they need support in adapting to their CHC using a multidisciplinary approach. Clinicians should thus monitor and discuss HRQOL in clinical practice. One way to do this, is by using PROMs. From our experience with implementing PROMs in clinical practice and annual evaluation meetings with clinicians, we know that clinicians can be reluctant to ask paediatric patients to complete PROMs in clinical practice as they doubt if children will report problems. However, this study indicated that paediatric patients do report HRQOL problems when completing PROMs in clinical practice and this information can thus be used during a doctor's visit. Discussion of both HRQOL scales and items is suggested as problems were reported on both levels. Clinicians can use the individual items as a conversation tool, as items provide concrete examples about which the clinician can ask questions. In addition, clinicians should be informed that patients with female gender, younger age and more school absence might be more vulnerable for having HRQOL problems. This might help clinicians in judging which patients need extra attention.
Some limitations to this study should be mentioned. First, differences in age were found between several groups. However, these differences were very small and analyses were therefore conducted in two age groups. Second, the representativeness of the CHC group cannot be guaranteed (e.g., due to regional data collection and disproportionate distribution of CHCs) and information about non‐participants with a CHC was lacking because only patients who completed questionnaires on the KLIK website and gave permission to use their data for scientific purposes were included. Third, an online, unsupervised data collection method was used for both the general population and CHC group, by which we cannot guarantee that children and adolescents completed the questionnaires themselves. Fourth, the data collections were performed on different time scales, namely six years (in all four seasons) for the CHC group and three months (in Spring only) for the general population. Therefore, it could be that seasonal variations in HRQOL might partly account for the lower HRQOL scores that were found in the CHC group.32 Fifth, only a limited number of variables was included in the regression model, even though previous research showed that factors like pain,5 fatigue 33 and disease duration 19 are also associated with HRQOL. Additionally, in the regression analyses some variables might have been prone to bias when reported by the child. For example, school absence (days missed) is a variable that children may not keep track of. Finally, no analyses could be performed on disease‐specific functioning of patient groups, as the sample sizes of individual CHC subgroups were too small.
4.1. Clinical implications
As a result of this study, new normative data have become available. We therefore updated the KLIK ePROfile (Figure 2) by replacing the reference line based on outdated HRQOL data of the healthy Dutch population by the reference line based on the newly collected PedsQLTM data of the general population, and by adding a reference line representing the PedsQLTM scale scores of the CHC group to the graphs. Gender (and age)‐specific reference lines are shown, since differences in HRQOL scores were found between boys and girls. Finally, information about school absence (days missed) was added as this factor was negatively associated with HRQOL outcomes. In line with these updates, the KLIK training for clinicians was updated with information on which PedsQLTM scales and items most problems are reported and which factors are associated with HRQOL. This may help clinicians in discussing a HRQOL PROM during the consultation.
FIGURE 2.
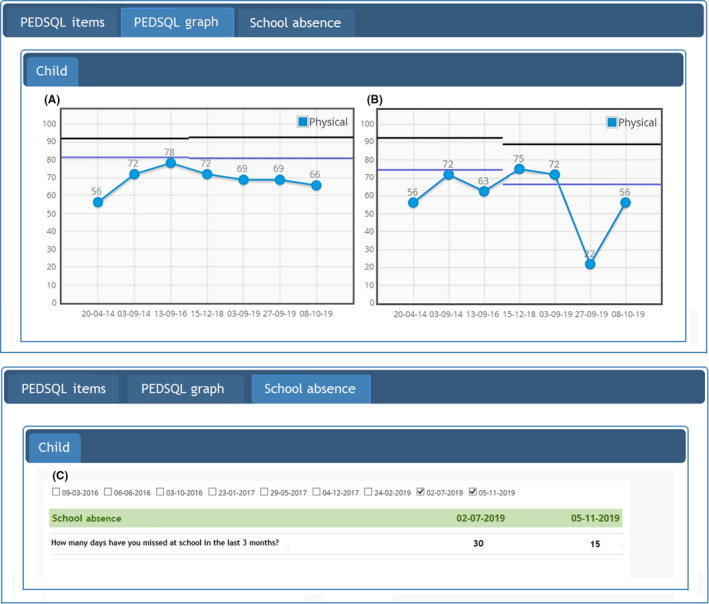
Updated feedback of the PedsQLTM over time in the KLIK ePROfile by providing reference lines of the general population (upper line) and CHC group (lower line) for boys (A) and girls (B) separately and per age group (shown by shift of reference line) and information about school absence of the patient (C)
5. CONCLUSIONS
This study showed that paediatric patients, who complete PROMs in daily clinical practice, experience more difficulties than the general population in HRQOL. School absence, female gender and younger age were negatively associated with HRQOL. It is therefore important to structurally monitor HRQOL by using and discussing PROMs in daily clinical practice (e.g., by using the updated KLIK PROM portal) and to take into account the associated factors, to detect problems and offer the right help on time.
CONFLICTS OF INTEREST
All authors have no financial or other conflicts of interest to disclose.
ACKNOWLEDGEMENTS
We would like to acknowledge the Dutch National Health Care Institute for their funding. We also thank the following clinicians of the Emma Children’s Hospital of the KLIK collaborator group for their support with the data collection: Benninga, M. A., van den Berg, J. M., Bouts, A. H. M., Breugem, C. C., Fijnvandraat, C. J., Groothoff, J. W., van der Horst, C. M., Jaeger, B., Kindermann, A., Knoester, H., Koot, B. G. P., Menke, L. A., Middelkamp Hup, M. A., Peters, M., van Rossum, M. A. J., Rutjes, N. W. P., Scherpbier, H. J., Schouten, A. Y. N., Stoelinga, F., Tabbers, M. M., Trotsenburg, A. S. P., Wijburg, F. A.
Funding Information
The data collection in this study was supported by the Dutch National Health Care Institute.
Contributor Information
Maud M. van Muilekom, Email: m.m.vanmuilekom@amsterdamumc.nl.
the KLIK collaborator group:
Benninga M. A., van den Berg J. M., Bouts A. H. M., Breugem C. C., Fijnvandraat C. J., Groothoff J. W., van der Horst C. M., Jaeger B., Kindermann A., Knoester H., Koot B. J. P., Menke L. A., Middelkamp Hup M. A., Peters M., van Rossum M. A. J., Rutjes N. W. P., Scherpbier H. J., Schouten A. Y. N., Stoelinga F., Tabbers M. M., Trotsenburg A. S. P., and Wijburg F. A.
DATA AVAILABILITY STATEMENT
Data are available upon reasonable request.
REFERENCES
- 1.Varni JW, Limbers CA, Burwinkle TM. Impaired health‐related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinquart M, Teubert D. Academic, physical, and social functioning of children and adolescents with chronic physical illness: a meta‐analysis. J Pediatr Psychol. 2011;37(4):376‐389. [DOI] [PubMed] [Google Scholar]
- 3.Moreira H, Carona C, Silva N, Frontini R, Bullinger M, Canavarro MC. Psychological and quality of life outcomes in pediatric populations: a parent‐child perspective. J Pediatr. 2013;163(5):1471‐1478. [DOI] [PubMed] [Google Scholar]
- 4.Silva N, Pereira M, Otto C, Ravens‐Sieberer U, Canavarro MC, Bullinger M. Do 8‐to 18‐year‐old children/adolescents with chronic physical health conditions have worse health‐related quality of life than their healthy peers? a meta‐analysis of studies using the KIDSCREEN questionnaires. Qual Life Res. 2019;28:1‐26. [DOI] [PubMed] [Google Scholar]
- 5.Haverman L, Grootenhuis MA, van den Berg JM, et al. Predictors of health‐related quality of life in children and adolescents with juvenile idiopathic arthritis: Results from a web‐based survey. Arthritis Care Res (Hoboken). 2012;64(5):694‐703. [DOI] [PubMed] [Google Scholar]
- 6.Reeve BB, Wyrwich KW, Wu AW, et al. ISOQOL recommends minimum standards for patient‐reported outcome measures used in patient‐centered outcomes and comparative effectiveness research. Qual Life Res. 2013;22(8):1889‐1905. [DOI] [PubMed] [Google Scholar]
- 7.Foster A, Croot L, Brazier J, Harris J, O’Cathain A. The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: a systematic review of reviews. J Patient Rep Outcomes. 2018;2(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotronoulas G, Kearney N, Maguire R, et al. What is the value of the routine use of patient‐reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol. 2014;32(14):1480‐1510. [DOI] [PubMed] [Google Scholar]
- 9.Engelen V, Detmar S, Koopman H, et al. Reporting health‐related quality of life scores to physicians during routine follow‐up visits of pediatric oncology patients: is it effective? Pediatr Blood Cancer. 2012;58(5):766‐774. [DOI] [PubMed] [Google Scholar]
- 10.Haverman L, van Rossum MA, van Veenendaal M, et al. Effectiveness of a web‐based application to monitor health‐related quality of life. Pediatrics. 2013;131(2):e533‐e543. [DOI] [PubMed] [Google Scholar]
- 11.Haverman L, van Oers HA, van Muilekom MM, Grootenhuis MA. Options for the Interpretation of and Recommendations for Acting on Different PROMs in Daily Clinical Practice using KLIK. Med Care. 2019;57:S52‐S58. [DOI] [PubMed] [Google Scholar]
- 12.Haverman L, van Oers HA, Limperg PF, et al. Implementation of electronic patient reported outcomes in pediatric daily clinical practice: the KLIK experience. Clin Pract Pediatr Psychol. 2014;2(1):50‐67. [Google Scholar]
- 13.Santana MJ, Haverman L, Absolom K, et al. Training clinicians in how to use patient‐reported outcome measures in routine clinical practice. Qual Life Res. 2015;24(7):1707‐1718. [DOI] [PubMed] [Google Scholar]
- 14.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329‐341. [DOI] [PubMed] [Google Scholar]
- 15.Engelen V, Haentjens MM, Detmar SB, Koopman HM, Grootenhuis MA. Health related quality of life of dutch children: psychometric properties of the PedsQL in the Netherlands. BMC Pediatr. 2009;9:68‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diederen K, Haverman L, Grootenhuis MA, Benninga MA, Kindermann A. Parental distress and quality of life in pediatric inflammatory bowel disease: implications for the outpatient clinic. J Pediatr Gastroenterol Nutr. 2018;66(4):630‐636. [DOI] [PubMed] [Google Scholar]
- 17.Splinter A, Tjaden LA, Haverman L, et al. Children on dialysis as well as renal transplanted children report severely impaired health‐related quality of life. Qual Life Res. 2018;27(6):1445‐1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michel G, Bisegger C, Fuhr DC, Abel T, The KIDSCREEN group . Age and gender differences in health‐related quality of life of children and adolescents in Europe: a multilevel analysis. Qual Life Res. 2009;18(9):1147‐1157. [DOI] [PubMed] [Google Scholar]
- 19.Pinquart M. Health‐related quality of life of young people with and without chronic conditions. J Pediatr Psychol. 2020;45(7):780‐792. [DOI] [PubMed] [Google Scholar]
- 20.Bisegger C, Cloetta B, von Bisegger U, Abel T, Ravens‐Sieberer U, the European Kidscreen group . Health‐related quality of life: gender differences in childhood and adolescence. Sozial‐ und Präventivmedizin. 2005;50(5):281‐291. [DOI] [PubMed] [Google Scholar]
- 21.Houben‐van Herten M, Bai G, Hafkamp E, Landgraf JM, Raat H. Determinants of health‐related quality of life in school‐aged children: a general population study in the Netherlands. PLoS One. 2015;10(5):e0125083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Didsbury MS, Kim S, Medway MM, et al. Socio‐economic status and quality of life in children with chronic disease: a systematic review. J Paediatr Child Health. 2016;52(12):1062‐1069. [DOI] [PubMed] [Google Scholar]
- 23.af Sandeberg M, Johansson E, Björk O, Wettergren L. Health‐related quality of life relates to school attendance in children on treatment for cancer. J Pediatr Oncol Nurs. 2008;25(5):265‐274. [DOI] [PubMed] [Google Scholar]
- 24.Mackner LM, Bickmeier RM, Crandall WV. Academic achievement, attendance, and school‐related quality of life in pediatric inflammatory bowel disease. J Dev Behav Pediatr. 2012;33(2):106‐111. [DOI] [PubMed] [Google Scholar]
- 25.Varni J, Limbers C, Burwinkle T. How young can children reliably and validly self‐report their health‐related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQLTM 4.0 generic core scales. Health Qual Life Outcomes. 2007;5(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nunnally JC, Bernstein IR. Psychometric Theory, 3rd edn. New York: McGraw‐Hill; 1994. [Google Scholar]
- 27.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: L. Lawrence Earlbaum Associates; 1988:2. [Google Scholar]
- 28.Engelen V, Haverman L, Koopman H, et al. Development and implementation of a patient reported outcome intervention (QLIC‐ON PROfile) in clinical paediatric oncology practice. Patient Educ Couns. 2010;81(2):235‐244. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J. The statistical power of abnormal‐social psychological research: a review. J Abnorm Soc Psychol. 1962;65(3):145. [DOI] [PubMed] [Google Scholar]
- 30.Sawyer MG, Reynolds KE, Couper JJ, et al. Health‐related quality of life of children and adolescents with chronic illness–a two year prospective study. Qual Life Res. 2004;13(7):1309‐1319. [DOI] [PubMed] [Google Scholar]
- 31.Pinquart M. Systematic review: bullying involvement of children with and without chronic physical illness and/or physical/sensory disability—a meta‐analytic comparison with healthy/nondisabled peers. J Pediatr Psychol. 2017;42(3):245‐259. [DOI] [PubMed] [Google Scholar]
- 32.Jia H, Lubetkin EI. Time trends and seasonal patterns of health‐related quality of life among US adults. Public Health Rep. 2009;124(5):692‐701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eddy L, Cruz M. The relationship between fatigue and quality of life in children with chronic health problems: a systematic review. J Spec Pediatr Nurs. 2007;12(2):105‐114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.


