Abstract
Background
Since the DSM‐5, adaptive functioning has taken a prominent place in the classification of intellectual disability (ID). The ADAPT was developed to assess adaptive skills in individuals with ID.
Method
A total of 2,081 ADAPTs from clients with suspected ID or borderline intellectual functioning and 129 ADAPTs from people from the general population (non‐ID) were collected, along with background characteristics.
Results
Internal consistency of the ADAPT was high (α = 0.98). ADAPT scores were positively associated with IQ, educational level and level of independent living. Furthermore, individuals without ID scored significantly higher than the clients on all of the 65 ADAPT items. Reference values were established for different IQ groups and living situations.
Conclusion
Results suggest that the ADAPT is a valid instrument for measuring adaptive skills in individuals with ID. The reference values may be used for the purpose of estimating the level of ID and the needed intensity of support.
Keywords: ADAPT, adaptive functioning, adaptive skills, borderline intellectual functioning, intellectual disability
1. INTRODUCTION
Adaptive skills are skills that are required to be able to function independently in society (Tassé et al., 2012). Such skills have become increasingly important in the classification of an intellectual disability. In the past, often only cognitive functioning in terms of IQ scores was used for determining an intellectual disability. Since the introduction of the DSM‐5 (American Psychiatric Association, 2013), however, adaptive skills play a leading role in the classification of an intellectual disability. This shift is due to the worldwide growing awareness that it is not primarily intellectual functioning but particularly adaptive functioning that determines whether someone can meet society's demands.
In practice however, many people with limitations in adaptive functioning are not recognized as such and do not receive support from organizations that specifically care for people with intellectual disabilities. This is especially true for clients in whom the intellectual disability is not noticeable at first sight, as quite often is the case in clients with borderline intellectual functioning, and to a lesser extent, in clients with a mild intellectual disability. A time‐efficient instrument to assess adaptive skills could be helpful to provide more people with deficiencies in adaptive skills the support and care they need. To give an example, intellectual disability currently still appears to be poorly recognized in general mental health care in the Netherlands. When screening for mild intellectual disabilities and borderline intellectual functioning, a prevalence of about 40% is found in samples of psychiatric patients of general mental health institutions, of which about half concerned patients with (a suspicion of) mild intellectual disability and half with (a suspicion of) borderline intellectual functioning (Nieuwenhuis et al., 2017; Seelen et al., 2019), whereas on the basis of the normal distribution one would expect about 16%. Not recognizing intellectual disabilities can be harmful to such an already vulnerable group of people with psychiatric disorders. First, clients with an intellectual disability may receive incorrect DSM classifications and treatments (including medication) when the characteristics of intellectual disability are seen as symptoms of a psychiatric disorder or because psychiatric disorders in people with an intellectual disability have different manifestations (Fletcher et al., 2016; Hurley, 2006). Second, the coping and abilities to solve everyday problems often fail in people with an intellectual disability, resulting in chronically high stress levels that can manifest themselves in, for example, acting‐out behaviour, somatic symptoms or psychotic‐type behaviour (e.g. Fletcher et al., 2016). Third, because their behaviour is misunderstood, clients with an intellectual disability are more often involuntarily admitted, hospitalization takes longer, and they are almost four times more likely to be confronted with coercive measures during psychiatric hospitalizations in general mental health care (Nieuwenhuis et al., 2017).
A clearly elevated prevalence of about 30 to 40% of mild intellectual disability and borderline intellectual functioning has also been found in Dutch prisons and forensic institutions (Kaal, 2016; Kaal et al., 2015; Nijman et al., 2017). Internationally, the prevalence of prisoners with an intellectual disability (IQ below 70) was found to be between 7 and 10% (Hellenbach et al., 2017), whereas 2.2% could be expected on the basis of the normal distribution. If intellectual disability is not recognized in detention, the prison guards may think that prisoners do not ‘want’ instead of ‘cannot’ cooperate, and they are inclined to use corrective measures more often (Kaal et al., 2011). In these cases, these prisoners may also be released from prison without adequate treatment and support, after which problems may start again. By not detecting intellectual disabilities and deficiencies in adaptive skills, the support during probation and resocialization may not be adequate for, or sensitive to, the specific needs of prisoners with intellectual disabilities. In our opinion, better recognition of intellectual disabilities could reduce the aforementioned problems, through better alignment with the needs of the client.
To measure adaptive functioning and increase the chance of correctly classifying (the severity of) an intellectual disability, a standardized instrument is needed (Schalock et al., 2010). The reason for developing the ADAPT (which is the English version of the Dutch ‘Adaptieve Vragenlijst Verstandelijke Beperking’ or AVVB in short; Jonker et al., 2016) was that no suitable and modern instruments were available in the Dutch language to measure adaptive skills in adult individuals with an intellectual disability, as well as with borderline intellectual functioning. Borderline intellectual functioning (IQ below 85) is often included in the Dutch prevalence figures, as there is a tradition in the Netherlands that clients with borderline intellectual functioning (combined with limitations in adaptive functioning) may also receive care from organizations for people with an intellectual disability. The Dutch‐language instrument called Sociale Redzaamheid Schaal – Plus (Social Selfhelp Scale – Plus; SRZ‐P; Kraijer and Kemna, 2004) was outdated with its norms dating from 1997. The Vineland‐3 (Sparrow et al., 2016) has not been translated into Dutch as far as we know, has a long completion time and is mainly used for clients with severe to mild intellectual disabilities, and to a lesser extent for clients with borderline intellectual functioning. The Adaptive Behavior Assessment System‐2 (ABAS‐II; Oakland and Harrison, 2008) was also not translated into Dutch, and the ABAS‐3 (Harrison and Oakland, 2015) did not exist at the time the ADAPT was being constructed in 2016. Finally, for the ADAPT, data on reference groups were mainly collected from the target group for whom the instrument will be used most: clients (with an intellectual disability and borderline intellectual functioning), in contrast to the ABAS‐3 that is standardized on people from the general population.
In sum, an instrument was lacking that encompasses contemporary adaptive skills – such as Internet banking, using email and mobile phones, and dealing with social media – and can help classify (the severity of) an intellectual disability and the DSM‐5V‐code borderline intellectual functioning.
In the development of the ADAPT, the requirements set by the American Association on Intellectual and Developmental Disabilities (AAIDD) for instruments on adaptive functioning were taken as starting points (Schalock et al., 2010). A full version of the ADAPT translated into English can be obtained from the first author.
The inter‐rater reliability of the total ADAPT scores was initially investigated in two small Dutch samples by having two caregivers fill in the ADAPT independently concerning the same clients (Kruisdijk et al., 2019; Nijman et al., 2017). The inter‐rater reliability was found to be good (n = 33, ICC of the ADAPT total scores = 0.81, and n = 44, Spearman's Rho of the ADAPT total scores = 0.77, respectively). Internal consistency of ADAPT scores was high in both studies with Cronbach's αs of 0.98 and 0.97, respectively. For the assessment of convergent validity, the ADAPT was compared with SRZ‐P total scores. Results revealed a moderate to strong positive correlation between the ADAPT and the SRZ‐P (n = 30) of r =.72 (Kruisdijk et al., 2019). The average completion time of the ADAPT was found to be 14 min (Kruisdijk et al., 2019). Although the results of these earlier, small‐scale, studies on the ADAPT were promising, further large‐scale, multicentre research was needed to further establish the psychometric characteristics of the ADAPT.
The main aim of the current study was to further evaluate psychometric properties of the ADAPT, and in particular the (convergent) validity of the instrument, and provide reference scores. More specifically, the following research questions are addressed:
Do clients with an intellectual disability who receive treatment or support have significantly lower ADAPT scores as compared to people who adaptively function independently in society?
Do people with higher IQ scores have higher ADAPT scores than people with lower IQ scores?
Do people with a higher level of education have higher ADAPT scores than people with a lower level of education?
Do people who live in protected living or are institutionalized have lower ADAPT scores than people who receive less or no living support?
Do people who have (a) psychiatric disorder(s) have lower ADAPT scores than people without psychiatric comorbidity? This was done to explore whether, and to what extent, comorbid psychiatric disorders appear to have a negative effect on the level of adaptive functioning.
With the ADAPT, we hope to be able to classify the severity of an intellectual disability, and that specific needs for support can be identified with the instrument.
2. METHODS AND MATERIAL
2.1. Setting and participants
A multicentre study was conducted between January 2018 and May 2020. Participants were 2,081 clients with an (suspected) intellectual disability receiving support or care from a wide variety of Dutch care facilities. A main inclusion criterium was that clients were sixteen or older. Clients with (comorbid) psychiatric disorder(s) were included in the study except for those with a florid psychosis. Clients with florid psychosis (or otherwise psychiatrically severely disrupted clients) were excluded because these conditions may (temporarily) impair adaptive functioning. In addition, we collected data among a comparison group consisting of 129 volunteers from the general population who function adaptively independently in society (hereafter referred to as: non‐intellectual disability group).
2.2. Procedure
Permission was requested and obtained from the Ethics Committee Social Science (ECSS) of Radboud University, Nijmegen, the Netherlands, for the collection of (anonymized) ADAPT data (ECSW‐2018‐122). Facilities providing care and treatment for clients with an intellectual disability were approached for participation. Following information meetings, conferences and a Dutch publication of a pilot study investigating the Dutch version of the ADAPT (see Kruisdijk et al., 2019), various facilities for clients with an intellectual disability, psychiatric problems and/or forensic problems were willing to participate in the study. Ultimately, more than 60 facilities located throughout the Netherlands participated. After a facility had expressed interest in participation, the first author gave verbal and written instructions about how the ADAPT should be completed. The ADAPTs were completed by proxies, such as caregivers or adult (household) family members who had detailed insight into the client's daily functioning and adaptive skills, in multiple contexts, such as home, school, work and the community. In this way, 2,081 ADAPTs were collected from clients who received some type of support or treatment. In addition, ADAPT scores were collected for 129 people from the general population. For these 129 participants in the non‐intellectual disability group, an adult family member was asked to complete the ADAPT.
2.3. The ADAPT
The ADAPT was developed to measure skills in the three domains (i.e. conceptual, social and practical) of adaptive behaviour in adults (DSM‐5; American Psychiatric Association, 2013) and consisted of 65 items. Examples of items of the ADAPT are as follows: [the client]
brushes teeth
washes and dries clothes
uses Internet banking
uses social media
starts and maintains healthy love relationships
takes initiative to have a talk and shows interest in the story of the other
thinks before acting
learns from mistakes
postpones behaviour or wishes if necessary
Each of the 65 items can be scored on a 5‐point Likert scale from 1: ‘does not perform the skill, even with help’ to 5: ‘performs the skill completely independently’. Proxies should score the items on the basis of actual behaviour of the client, and not on what a client potentially is capable of. The total ADAPT score ranges between 65 and 325. In case of a low item score (i.e. 1 or 2), caregivers or family members are asked to also indicate whether a client is judged to be able to acquire that skill, for example by training.
2.4. Demographic and other characteristics
2.4.1. IQ
Results from IQ tests were taken from clients' case files. IQ scores were from the WAIS‐IV‐NL (Wechsler, 2012), WAIS‐III‐NL (Wechsler et al., 2005), WISC‐V‐NL (Hendriks et al., 2017), WISC‐III‐NL (Kort et al., 2005), SON‐R (Tellegen & Laros, 2011), GIT‐2 (Luteijn & Barelds, 2004) and the KAIT‐NL (Mulder et al., 2004). Reference groups were based upon the criteria of the DSM‐IV: labelling IQ scores between 40 and 54 as a moderate intellectual disability, IQ scores between 55 and 69 as a mild intellectual disability and IQ scores between 70 and 84 as borderline intellectual functioning.
In addition to the ADAPT and the results from IQ tests (if available), information on other characteristics was gathered, namely age, gender, level of education, potential DSM classification(s) determined by a qualified psychologist or psychiatrist and the current living situation. For the 129 subjects from the general population, generally no IQ scores were available.
2.5. Statistical analyses
For statistical analyses, SPSS version 25 was used. The normality of the distribution of the ADAPT scores was examined by means of the skewness and kurtosis values and visual inspection of the histogram. The internal consistency of the ADAPT was investigated by calculating Cronbach's α.
Sample characteristics were analysed and presented using descriptive statistics. Average ADAPT scores of different subgroups, such as IQ subgroups (e.g. IQ 40–54, 55–69, 70–84, 85–99), educational level, categories of type and intensity of support, were analysed by means of one‐way ANOVAs. Associations between IQ and ADAPT scores were also examined by means of a Pearson's r correlation. Differences in ADAPT scores between clients with and without psychiatric comorbidity were analysed using t‐tests. The main analyses, and the hypothesized directions, to test the (convergent) validity of the ADAPT are summarized in Table 1.
TABLE 1.
Summary of the analyses, and the hypothesized directions, to test the (convergent) validity of the ADAPT
| Hypothesis | Groups/participants used to test the hypothesis | Statistical test used |
|---|---|---|
| 1. Clients who receive care from institutions providing ID care, have significantly lower ADAPT scores compared to people from the general population who function independently in society | ADAPT scores from 2081 clients receiving care from ID institutions, versus 129 persons from the general population | t‐test |
| 2. People with higher IQ scores have higher ADAPT scores than people with lower IQ scores | 1,378 participants for whom the IQ group was reported, divided into the following groups: moderate ID (n = 261), mild ID (n = 617), borderline IF (n = 440) and zero to one SD below‐average intelligence (n = 60). |
ANOVA 95% confidence intervals Pearson's r correlation between IQ and ADAPT scores |
| 3. People with higher levels of education on average have higher ADAPT scores than people with lower levels of education | 1,894 participants for whom the educational level was known | ANOVA |
| 4. People who receive more care and live less independently on average will have lower ADAPT scores | 2,018 participants for whom the living conditions were known, categorized into: living independently without any support (n = 238); living with ambulatory support (n = 351); living in a facility with daytime support only (n = 70); living with parents (n = 334); and living in a facility with full time, 24/7, support (n = 1025) | ANOVA |
| 5. Clients who have (a) psychiatric disorder(s) on average have lower ADAPT scores than people without psychiatric comorbidity | ADAPT scores from the 2079 clients, with (n = 1017) or without (n = 1062) psychiatric comorbidity (n = 2079), split into the IQ groups of moderate ID, mild ID and borderline IF | t‐tests |
3. RESULTS
3.1. Distribution and internal consistency of ADAPT scores
As mentioned earlier, 2,210 ADAPTs were collected in total; 2,081 from clients with an (suspected) intellectual disability receiving care from of ambulant and clinical facilities, and from 129 people living independently (non‐intellectual disability group). The skewness and kurtosis of ADAPT scores in our sample of 2,081 clients from facilities were limited with values of −0.15 and −0.38, respectively. Visual inspection of the histogram showed that the distribution of ADAPT scores was very close to the normal curve, which allows the use of the parametric statistical tests mentioned in the previous statistical paragraph (i.e. ANOVAs, Pearson's correlations and t‐tests). The internal consistency of the ADAPT was high (Cronbach's alpha = 0.98).
3.2. Characteristics of the sample
In Table 2, the main characteristics of the participants of the study are summarized. As can be seen, the mean age of the total sample of 2,210 participants was 36.6 years (range: 16–83; SD = 15.26). The 2,210 participants consisted of 1,303 men (59%) and 907 women (41%). The higher number of men in our data set can be explained by the contribution of ADAPTs from forensic psychiatric institutions. Of the 2,081 clients receiving care from (intellectual disability) facilities, 1,238 were men (59%) and 843 were women (41%). There was no difference in the ADAPT scores between male and female clients (t [2,079] = 1.77, p = .077, two‐tailed).
TABLE 2.
Main characteristics of the participants of the study (i.e. sex, age and IQ groups)
| Variable | Clients from (ID‐) institutions | Persons from the general population | Total sample |
|---|---|---|---|
| N | 2,081 | 129 | 2,210 |
| Sex |
1,238 men (59%), 843 women (41%) |
65 men (50%), 64 women (50%) |
1,303 men (59%), 907 women (41%) |
| Age |
M = 36.5 years (range 16–83; SD = 15.19) 14 missing values |
M = 39.4 years (range 17–75; SD = 16.27) | M = 36.6 years (range 16–83; SD = 15.26) |
| IQ groups |
Moderate ID: n = 261 Mild ID: n = 617 Borderline IF; n = 440 Zero to one SD below‐average IQ; n = 60 703 missing values |
The 2,081 ADAPTs of clients consisted of 1,621 clients receiving support from intellectual disability facilities, 349 patients from general mental healthcare or addiction care facilities, and 293 patients from forensic hospitals. Some of the facilities offered combined care, such as forensic care for clients with an intellectual disability or forensic addiction health care, implying that these numbers added together exceed the total number of 2,081 ADAPTs collected. Not all clients who received care from facilities eventually turned out to have an intellectual disability if this was solely based on their IQ scores. In practice, ADAPT scores were also obtained for a number of clients with an IQ of 85 to 99 (see the paragraph ‘Relationships between IQ and ADAPT scores’).
Of the 2,081 clients for whom an ADAPT was collected, about half (51%) also had one or more comorbid psychiatric disorders. Autism spectrum disorders (17%) were most frequently mentioned, followed by diagnoses pertaining to alcohol and/or substance abuse (13%), psychotic disorders (9%), personality disorders (9%), ADHD (8%), posttraumatic stress disorder or anxiety disorders (8%), mood disorders (7%), emotion regulation disorders (2%), attachment disorders (1%), genetic disorders or syndromes (1%) and other disorders (1%).
3.3. ADAPT scores from clients compared to people from the general population (hypothesis 1)
As was anticipated, the mean ADAPT total score of the 2,081 clients who received support and/or treatment was significantly lower than that of the 129 people of the non‐intellectual disability group (t [2,208] = 22.31 p < .001, one‐tailed). The mean ADAPT score of clients was 205 (SD = 52.48), whereas the mean ADAPT score of the non‐intellectual disability group was 309 (SD = 24.23). Furthermore, significant differences between these two groups were found for all 65 individual items of the ADAPT. Clients scored significantly lower on every item of the ADAPT compared to the non‐intellectual disability group (all p‐values < .001, one‐tailed).
3.4. Relationships between IQ and ADAPT scores (hypothesis 2)
A significant positive correlation between IQ total scores and ADAPT scores was observed, but this association was modest (r = .29, p < .001, one‐tailed). Mean values for participants with a moderate intellectual disability, a mild intellectual disability, borderline intellectual functioning and zero to one SD below‐average intelligence (i.e. an IQ from 85 to 99) are shown in Figure 1 along with the 95% confidence intervals. The difference in average ADAPT scores between the IQ groups was significant (F [3, 1,374] = 36.84, p < .001). A follow‐up post hoc Tukey test showed that the difference in ADAPT total scores between clients with moderate and a mild intellectual disability was significant (p < .001), as was the difference between clients with a mild intellectual disability and borderline intellectual functioning (p = .001). However, no significant difference was observed between clients with borderline intellectual functioning and clients with below‐average intelligence (p = .348).
FIGURE 1.
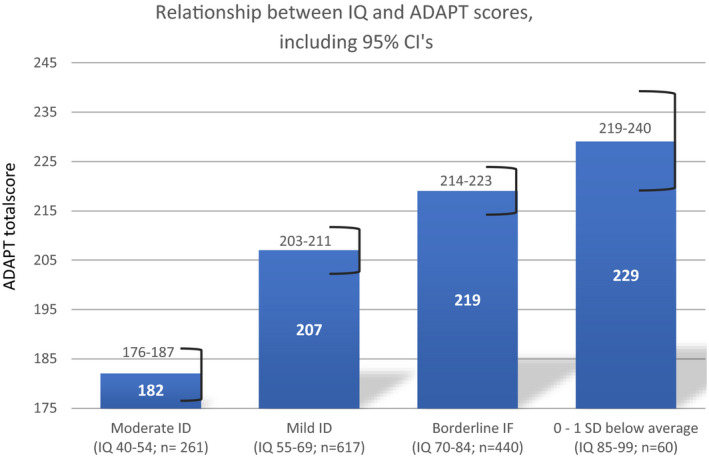
Relationship between IQ and ADAPT scores, including 95% CI's
The mean values and confidence intervals of ADAPT scores per IQ subgroup can possibly be used as reference values to compare the scores of individual clients with.
3.5. Relationships between the level of education and ADAPT scores (hypothesis 3)
Information on educational level was available for 1,894 of the total of 2,210 participants (86%). Figure 2 shows the educational levels ordered from lower levels (left) to higher levels (right). To explain the Dutch terminology of Dutch educational levels, the first three levels of education in the left of Figure 3 concern primary education up to the age of twelve. Education levels 4 and 5 concern lower secondary education until the age of about sixteen. Educations levels 1, 2 and 4 are specifically for people diagnosed with an intellectual disability. Based on the Dutch Intelligence Test for Education Level (NIO; Van Dijk, 2018), people with education level 5 function at about borderline intellectual functioning level (IQ 80–90). The educational levels 6 to 12 concern either secondary or tertiary education with increasing levels of difficulty, with the highest level (i.e. level 12) being educations at the academic/university level. In line with expectations, we found that the higher the educational level, the higher the ADAPT score on average is (F [11, 1882] = 76.47, p < .001).
FIGURE 2.
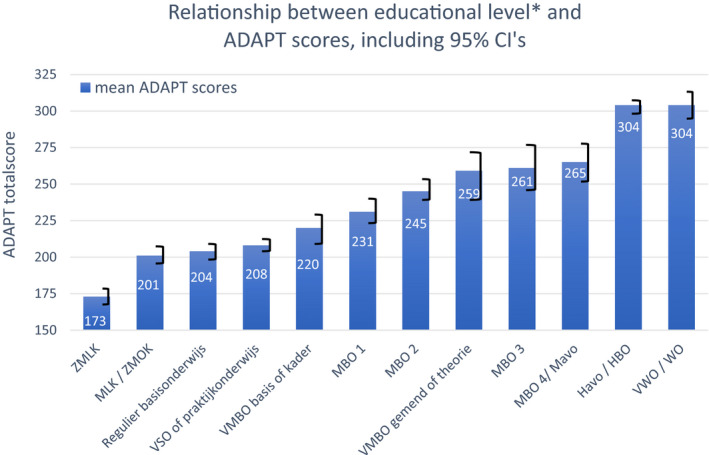
Relationship between educational level* and ADAPT scores, including 95% CI's
FIGURE 3.
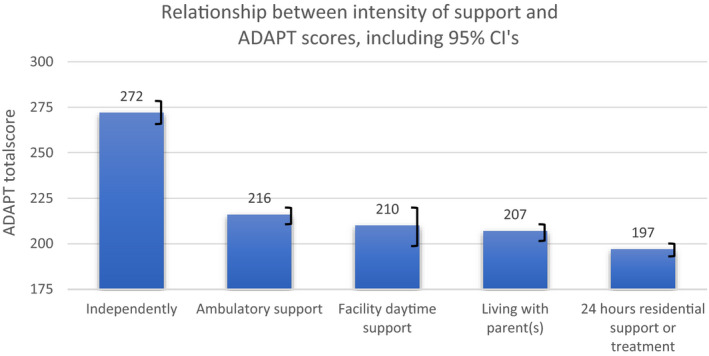
Relationship between intensity of support and ADAPT scores, including 95% CI's
3.6. Relationships between intensity of support and ADAPT scores (hypothesis 4)
Among the group of 2,210 participants, it was also investigated whether ADAPT scores are related to the extent to which they live independently or whether they are offered support to a greater or lesser extent. We assumed that the more support participants receive, the lower their ADAPT scores on average is. The living conditions were known for 2018 of the 2,210 participants (91%), and the following categories were distinguished: living independently without any support; living independently with ambulatory support; living in a facility with daytime support only; living with parents; and living in a facility with full time, 24/7, support (including staff being present at night). As can be seen in Figure 3, the ADAPT scores on average are higher for participants living independently compared to those living with various levels of support, care or supervision. In other words, the highest ADAPT scores are found for participants who live completely independently and the lowest ADAPT scores are found for participants who receive 24‐h care and support (F [4, 2013] = 101.50, p < .001). Clients receiving 24‐h care and support (n = 1,025) stayed in closed settings, partially closed or open residential and treatment settings. The degree of openness of the 24‐h care setting, however, did not make any difference in terms of total ADAPT scores (F [2, 285) = 1.28, p = .280].
3.7. ADAPT and psychiatric comorbidity (hypothesis 5)
Finally, it was examined whether there were differences in ADAPT scores between clients with or without psychiatric comorbidity (n = 2,079). We found that 62% of clients with borderline intellectual functioning had a comorbid psychiatric diagnosis, compared to 49% of clients with a mild intellectual disability and 38% with a moderate intellectual disability. When clients with a moderate intellectual disability, a mild intellectual disability and borderline intellectual functioning were analysed as separate groups for differences in ADAPT scores between clients with or without psychiatric comorbidity, significant differences were only found in the group of clients with borderline intellectual functioning (t [438] = 3.26, p = .001; two‐tailed). Clients with borderline intellectual functioning without psychiatric comorbidity on average scored fifteen points higher than clients with borderline intellectual functioning and psychiatric comorbidity (see Figure 4).
FIGURE 4.
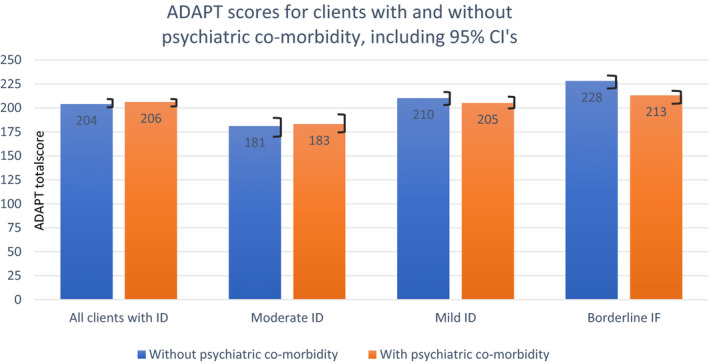
ADAPT scores for clients with and without psychiatric co‐morbidity, including 95% CI's
4. DISCUSSION AND CONCLUSIONS
The aim of the present study was to investigate the psychometric characteristics of the ADAPT, a newly developed and short instrument for measuring adaptive functioning in individuals with an intellectual disability or borderline intellectual functioning. In line with what was expected, it was found that clients receiving treatment or support scored significantly lower on both the ADAPT total score and all individual items of the instrument, as compared to people from the general population. Furthermore, the observed associations in the current study between ADAPT scores on the one hand and IQ, educational level and living situations on the other, all went in the expected directions; the higher the IQ and the educational level, the higher the ADAPT scores on average were. In addition, ADAPT scores were the lowest on average for people who received 24‐h residential support or treatment and the highest for people who lived totally independently. Finally, the assumption that clients with additional psychiatric comorbidity would have lower ADAPT scores on average than clients without psychiatric comorbidity was only confirmed for clients with borderline intellectual functioning and not for clients with a moderate or mild intellectual disability.
The modest but significant correlation (0.29) between IQ and total ADAPT scores confirmed results from previous (pilot) studies on the ADAPT. In an earlier study of Nijman, Lammers, et al., (2017), a correlation of 0.36 was found between IQ and ADAPT scores. The correlation established in the current study would possibly have been stronger if IQ scores for the independently functioning people from the general population were also obtained. The modest correlation between IQ and ADAPT scores is in line with results from previous studies. Saleem et al., (2019), for instance, recently reported a low, but significant, correlation of 0.17 (p = .03) between the scores of the Adaptive Behaviour Composite of the Vineland‐II and the full scale (WAIS) IQ.
The correlation of 0.29 we found between adaptive functioning and IQ scores is also in line with the assumption the DSM‐5 (American Psychiatric Association, 2013) makes, namely that IQ and level of adaptive skills are related, but do not necessarily strongly correspond with each other. People with a low IQ can reach a relatively high level of adaptive functioning, for instance by means of education, training and treatment, and vice versa.
The found associations between educational levels and ADAPT scores make clear that the higher the level of successfully completed education is, the higher the ADAPT scores on average are. In the Netherlands, there is focus on educating and training of practical skills such as self‐care in the more practical forms of educations, but teachers and school managers possibly could use the ADAPT to assess which specific skills in general are (still) weak in their students at the end of the education, so that learning these skills potentially could receive more attention in the curriculum. In absolute terms, the differences in ADAPT scores between the highest and the lowest level of education were greater than the differences in the scores between the IQ groups that were examined. Furthermore, the lack of differences in average ADAPT scores among people with the two highest educational levels (see Figure 2) suggests that there is a ceiling effect of ADAPT scores. Highly educated people often seem to possess and execute (almost) all the skills that are measured with the ADAPT. This ceiling effect is characteristic of instruments that measure adaptive functioning, because they are skills that most adult people possess (Tassé et al., 2012).
Furthermore, the comparison between living situation and ADAPT scores showed that persons who live independently without any support or care have higher ADAPT scores than people who receive support or live in institutions. This finding also supports the validity of the ADAPT. However, it appears the ADAPT is less sensitive to distinguish between residential facilities where care is only available during the day or 24‐h care, of within 24‐h care whether the care was provided in an open, semi‐closed or closed setting. Yet, the decision for care on a (locked) residential facility may also depend on other factors such as the severity and risks of displaying harmful and dangerous behaviour for the environment of the client involved. Besides that, it should be noted that with the current correlation research design it does not become clear what the direction of the association between living in a 24‐h setting and low ADAPT scores is. A low level of adaptive functioning may increase the need for 24‐h care and being hospitalized, but the hospitalization by itself may also have a negative influence on being able to, or having the need for, performing certain adaptive skills independently.
A significant difference in ADAPT scores between clients with and without psychiatric comorbidity was only observed in the borderline intellectual functioning group. A possible explanation of this may be that this specific group of clients with borderline intellectual functioning is found to be common in general mental healthcare institutions (see Nieuwenhuis et al., 2017; Seelen et al., 2019). In general mental healthcare institutions, there probably is a stronger, and more primary, focus on determining psychiatric diagnoses compared to institutions primarily providing care for clients with an intellectual disability in which the focus may be less on diagnosing potential psychiatric comorbidity. This is supported by the finding that clients with higher IQ levels more often received comorbid classifications in comparison with clients with lower IQ levels. However, this should be viewed with caution as we could not assess the reliability of psychiatric diagnoses or classifications. In addition, all types of psychiatric diagnoses were considered as one overall category, while the influence of psychiatric comorbidity on adaptive functioning may only apply to some disorders and not to others. The negative effect on adaptive functioning has already been demonstrated in various psychiatric disorders, such as psychosis (Matson et al., 2003), autism (Kenworthy et al., 2010) and ADHD (Stravo et al., 2006).
The current study also has a number of other limitations. Due to the absence of national population figures, we do not know whether the collected data adequately represent the situation in the Netherlands, let alone for facilities in other countries. Further, our data set has an overrepresentation of men. This overrepresentation of men may be the result from the contribution of ADAPTs to our database from forensic psychiatric hospitals in which men were overrepresented. Finally, only ADAPTs from clients who received some type of care were collected and we therefore do not know how people in the general population with a limited cognitive ability would score on the ADAPT. For example, it is estimated that only one third of (Dutch) people with an IQ between 71 and 85 actually have limitations in adaptive functioning (Woittiez et al., 2019).
However, the data set is very large and more than sixty facilities located throughout the Netherlands took part in the data collection. Besides that, our assumptions about the direction of the associations of ADAPT scores with the other variables were largely confirmed. Finally, previous small‐scale studies into the ADAPT (Kruisdijk et al., 2019; Nijman, Lammers, et al., 2017) indicated that the inter‐rater reliability was good. Taking into account these results and limitations of the current study, we conclude that the presented data are suitable as a starting point for establishing reference values for clients with an intellectual disability who receive professional care in the Netherlands.
The reference values given in this article can potentially be used as follows. First, as mentioned earlier, the assessed level of adaptive functioning has become an important factor in the DSM‐5 to classify the presence and severity of an intellectual disability (American Psychiatric Association, 2013). Second, ADAPT scores can be helpful to assess whether a client's adaptive skills are relatively strong or weak compared to his or her intelligence level (as determined by an IQ test), or compared to their educational level. In case of lower ADAPT scores that can be expected compared to the IQ and educational level of a client, one can wonder: Did the client never have the opportunity to learn certain skills? And if so, can these skills still be trained and learned by this client? Is the client (currently) unable to show certain skills? The latter could be due for instance to a current (comorbid) psychiatric condition, a living context in which the client is over demanded, or a very restricted (locked) living situation which precludes the performance of certain skills. In a scenario that ADAPT scores are relatively high compared to the IQ and educational level, the living context and support for the client may be optimal, but one still should be cautious that a transferral to a more demanding and independent living situation may potentially lead to a reduction of adaptive functioning when too much strain and demands are put on the client. It should be noted in a general sense that the ADAPT measures skills that someone actually shows. This does not always say anything about a person's potential. For example, it is our clinical experience that clients with an intellectual disability in a structured setting often show more skills than when they are not offered structure from their environment or when too high demands are placed on the client. The context must therefore always be taken into account when estimating how independently someone functions or can function.
5. CONCLUSION
In sum, the main results of the current study on the (convergent) validity of the ADAPT showed that volunteers from the general population had higher ADAPT scores than the clients receiving help from institutions for people with an intellectual disability, and that higher IQs of the studied participants on average were associated with higher ADAPT scores. Furthermore, ADAPT scores increased as the educational level of the studied person was higher, and people who lived on a ward or in a sheltered home with care being present around the clock had lower ADAPT scores than people who lived independently or received less intensive care. Taken together, these results indicate that the ADAPT seems to be a valid instrument for assessing (deficiencies in) adaptive skills.
CONFLICT OF INTEREST
The (Dutch version of the) ADAPT may be published by Hogrefe publishers in the future.
ACKNOWLEDGMENTS
The study was (financially) supported by De Borg and Kwaliteit Forensische Zorg (KFZ). We would also like to thank all facilities and organizations who participated in the collection of the data.
REFERENCES
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Fletcher, R. J., Barnhill, J., & Cooper, S.‐A. (Eds.) (2016). Diagnostic manual – Intellectual disability (DMID‐2): A textbook of diagnosis of mental disorders in persons with intellectual disability. NADD Press. [DOI] [PubMed] [Google Scholar]
- Harrison, P., & Oakland, T. (2015). Adaptive Behavior Assessment System, Third Edition (ABAS‐3). Western Psychological Services. [Google Scholar]
- Hellenbach, M., Karatzias, T., & Brown, M. (2017). Intellectual disabilities among prisoners: prevalence and mental and physical health comorbidities. Journal of Applied Research in Intellectual Disabilities, 30, 230–241. 10.1111/jar.12234 [DOI] [PubMed] [Google Scholar]
- Hendriks, M. P. H., Ruiter, S. V., Schittekatte, M., & Bos, A. (2017). Wechsler Intelligence Scale for Children‐V (WISC‐V‐NL). Pearson Assessment B.V. [Google Scholar]
- Hurley, A. D. (2006). Mood disorders in intellectual disability. Current Opinion in Psychiatry, 19, 65–469. [DOI] [PubMed] [Google Scholar]
- Jonker, F., Kruisdijk, S., Goedhard, L., & Nijman, H. (2016). Adaptieve Vragenlijst Verstandelijk Beperking (AVVB). Wier. [Google Scholar]
- Kaal, H. L. (2016). Prevalentie licht verstandelijke beperking in het justitiedomein. (Prevalence of mild intellectual disability in the justice domain). Hogeschool Leiden. [Google Scholar]
- Kaal, H. L., Negenman, A. M., Roeleveld, E., & Embregts, P. J. C. M. (2011). De problematiek van gedetineerden met een lichte verstandelijke beperking in het gevangeniswezen. (Problems of detainees with a mild intellectual disability in prison). Primaprint. [Google Scholar]
- Kaal, H. L., Nijman, H. L. I., & Moonen, X. M. H. (2015). Identifying offenders with an intellectual disability in detention in the Netherlands. Journal of Intellectual Disabilities and Offending Behavior, 6, 94–101. 10.1108/JIDOB-04-2015-0008 [DOI] [Google Scholar]
- Kenworthy, L., Case, L., Harms, M., Martin, A., & Wallace, G. (2010). Adaptive behavior ratings correlate with symptomatology and IQ among individuals with high‐functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 40, 416–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kort, W., Schittekatte, M., Bosmans, M., Compaan, E. L., Dekker, P. H., Vermeir, G., & Verhaeghe, P. (2005). Wechsler Intelligence Scale for Children‐III (WISC‐III‐NL). Nederlandse bewerking. Pearson Assessment B.V; [Google Scholar]
- Kraijer, D. W., & Kemna, G. N. (2004). Sociale Redzaamheidsschaal‐Z voor hoger niveau. SRZ‐P. Handleiding. Vierde, uitgebreide uitgave. (Social Selfhelp Scale‐Plus. Manual. 4th expanded edition). Harcourt Assessment. [Google Scholar]
- Kruisdijk, S., Jonker, F., Goedhard, L., & Nijman, H. (2019). Licht verstandelijke beperking in de DSM‐5: het belang van adaptief functioneren. Ontwikkeling en onderzoek van de Adaptieve Vragenlijst Verstandelijke Beperking (AVVB). (Mild intellectual disability in the DSM‐5: the importance of adaptive functioning. Developmental and research with the ADAPT). De Psycholoog, 54, 34–42. [Google Scholar]
- Luteijn, F., & Barelds, D. P. F. (2004). Groninger Intelligentie Test 2 (GIT‐2). (Groningen Intelligence Test 2). Harcourt Assessment B.V. [Google Scholar]
- Matson, J., Mayville, E., Lott, J., Bielecki, J., & Logan, R. (2003). A comparison of social and adaptive functioning in persons with psychosis, autism, and severe or profound mental retardation. Journal of Developmental and Physical Disabilities, 15, 57–65. [Google Scholar]
- Mulder, J. L., Dekker, R., & Dekker, P. H. (2004). Kaufman – Intelligentietest voor Adolescenten en Volwassenen (KAIT‐NL). PITS Testuitgeverij. [Google Scholar]
- Nieuwenhuis, J. G., Noorthoorn, E. O., Nijman, H. L. I., Naarding, P., & Mulder, C. L. (2017). A blind spot? Screening for mild intellectual disability and borderline intellectual functioning in admitted psychiatric patients: prevalence and associations with coercive measures. PLoS One, 2, e0168847. 10.1371/journal.pone.0168847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijman, H., Didden, R., & Hesper, B. (2017). Handreiking Risicomanagement LVB. (Guideline Risk Management Mild ID). Expertisecentrum Forensische Psychiatrie. [Google Scholar]
- Nijman, H., Lammers, S., Vrinten, M., & Bulten, E. (2017). (Te) lang in tbs? Een onderzoek naar patiënten die meer dan 15 jaar in tbs‐behandeling zijn. (Too long in tbs? A study on patients who have been in tbs‐treatment for at least 15 years. Tijdschrift Voor Psychiatrie, 59(1), 9–19. [PubMed] [Google Scholar]
- Oakland, T., & Harrison, P. L. (2008). Adaptive Behavior Assessment System (2nd ed.). Elsevier. [Google Scholar]
- Saleem, M., Beail, N., & Roache, S. (2019). Relationship between the Vineland Adaptive Behaviour Scales and the Wechsler Adult Intelligence Scale IV in adults with intellectual disabilities. Journal of Intellectual Disability Research, 63, 1158–1162. [DOI] [PubMed] [Google Scholar]
- Schalock, R. L., Borthwick‐Duffy, S. A., Bradley, V. J., Buntinx, W. H. E., Coulter, D. L., Craig, E. M., & Yaeger, M. H. (2010). Intellectual Disability: Definition, Classification, and Systems of Supports. AAIDD. [Google Scholar]
- Seelen, B., Smits, H., Penterman, B., Noorthoorn, E., Nieuwenhuis, J., & Nijman, H. (2019). Screening for intellectual disabilities and borderline intelligence in Dutch outpatients with severe mental illness. Journal of Applied Research in Intellectual Disabilities, 32, 1096–1102. [DOI] [PubMed] [Google Scholar]
- Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland Adaptive Behavior Scales, third edition (Vineland‐3). Pearson. [Google Scholar]
- Stravo, G., Ettenhofer, M., & Nigg, J. (2006). Executive functions and adaptive functioning in young adult attention‐deficit/hyperactivity disorder. Journal of the International Neuropsychological Society, 13, 324–334. [DOI] [PubMed] [Google Scholar]
- Tassé, M. J., Schalock, R. L., Balboni, G., Bersani, H.Jr, Borthwick‐Duffy, S. A., Spreat, S., Thissen, D., Widaman, K. F., & Zhang, D. (2012). The construct of adaptive behavior: its conceptualization, measurement, and use in the field of intellectual disability. American Journal on Intellectual and Developmental Disabilities, 117, 291–303. 10.1352/1944-7558-117.4.291 [DOI] [PubMed] [Google Scholar]
- Tellegen, P., & Laros, J. (2011). Snijders‐Oomen Niet‐verbale Intelligentietest 6–40 (SON‐R 6–40). (Snijders‐Oomen Non‐Verbal Intelligence Test (pp. 6–40). Hogrefe Uitgevers BV. [Google Scholar]
- van Dijk, H. (2018). Nederlandse Intelligentietest voor Onderwijsniveau (NIO‐2). Boom Uitgevers. [Google Scholar]
- Wechsler, D. (2012). Wechsler Adult Intelligence Scale IV‐NL (WAIS‐IV‐NL). Pearson Assessment B.V. [Google Scholar]
- Wechsler, D., Van der Steene, G., & Vertommen, H. (2005). WAIS III‐NL: Wechsler Adult Intelligence Scale III‐NL. Harcourt Test Publishers. [Google Scholar]
- Woittiez, I., Eggink, E., & Ras, M. (2019). Het aantal mensen met een licht verstandelijke beperking: een schatting. [The number of people with mild intellectual disabilities: an estimate]. Notitie ten behoeve van het IBO‐LVB. Sociaal en Cultureel Planbureau. [Google Scholar]


