Abstract
Objective
Narcolepsy is a rare sleep disorder in which psychotic‐like symptoms can present diagnostic and therapeutic challenges. We aimed to review the association between, and medical management of, narcolepsy and psychosis in children and adults.
Methods
We reviewed the full text of 100 papers from 187 identified by a PubMed search on narcolepsy plus any of these keywords: psychosis, schizophrenia, delusion, side effects, safety, and bipolar disorder.
Results
Three relevant groups are described. (i) In typical narcolepsy, psychotic‐like symptoms include predominantly visual hallucinations at the sleep‐wake transition (experienced as “not real”) and dissociation because of intrusion of rapid eye movement (REM) sleep phenomena into wakefulness. (ii) Atypical patients (“the psychotic form of narcolepsy”) experience more severe and vivid, apparently REM‐related hallucinations or dream/reality confusions, which patients may rationalize in a delusion‐like way. (iii) Some patients have a comorbid schizophrenia spectrum disorder with psychotic symptoms unrelated to sleep. Psychostimulants used to treat narcolepsy may trigger psychotic symptoms in all three groups. We analyzed 58 published cases from groups 2 and 3 (n = 17 and 41). Features that were reported significantly more frequently in atypical patients include visual and multimodal hallucinations, sexual and mystical delusions, and false memories. Dual diagnosis patients had more disorganized symptoms and earlier onset of narcolepsy.
Conclusion
Epidemiological studies tentatively suggest a possible association between narcolepsy and schizophrenia only for very early‐onset cases, which could be related to the partially overlapping neurodevelopmental changes observed in these disorders. We propose a clinical algorithm for the management of cases with psychotic‐like or psychotic features.
Keywords: delusion, hallucination, narcolepsy, psychosis, schizophrenia, side effects
Summations
Besides substance‐induced psychotic events, there are three main groups of patients with narcolepsy and psychotic‐like symptoms. Despite overlapping symptoms, clinical cues may help differentiate between patients with narcolepsy and atypical‐severe psychotic‐like symptoms and patients with a dual diagnosis of narcolepsy and a psychotic disorder.
Early‐onset narcolepsy or psychosis could be associated with a higher risk of co‐occurrence of both disorders.
Modafinil and pitolisant are apparently the wake‐promoting drugs with the least propensity to induce psychotic symptoms in patients with narcolepsy.
Limitations
The small number of cohort studies and the rarity of narcolepsy comorbid with schizophrenia prevent us from conducting a formal meta‐analysis.
The systematic review draws primarily on case reports and small cohort studies using diverse research designs to explore the overlap between narcolepsy and psychosis. Larger, well‐designed epidemiological and treatment studies (particularly in children) will be needed to advance our understanding in this domain.
1. INTRODUCTION
Narcolepsy is a chronic central disorder of hypersomnolence, affecting 1:5000 to 1:3300 people.1 Subtypes include Narcolepsy Type 1 (NT1, with cataplexy and/or hypocretin deficiency), and Narcolepsy Type 2 (NT2, without cataplexy or hypocretin deficiency; 15–25% of cases). Age at onset has two peaks, at ages 15 and 35. The sex ratio is ~1.2, 3 Sleep‐related daytime hallucinations are reported in 45–87% of NT1 patients and 28% of NT2 patients.4 Dissociation or delusions are less common. These symptoms may suggest a comorbid or primary diagnosis of psychotic disorder,5, 6, 7, 8 generating diagnostic, and therapeutic dilemmas. Here, we review the literature on the association between narcolepsy and psychosis, propose a framework for differential diagnosis, and suggest an approach to pharmacotherapy in patients with psychotic‐like or psychotic symptoms.
By current criteria,2 the diagnosis of NT1 and NT2 requires excessive daytime sleepiness daily for 3 months. NT1 then requires either:
low CSF hypocretin‐1 (≤110 pg/mL or 1/3 of mean values by a standard assay), or
both cataplexy and two sleep study findings: mean sleep latency ≤8 minutes; and ≥2 sleep‐onset rapid eye movement (REM) periods (SOREMPs) (either both on a Mean Sleep Latency Test [MSLT], or one on MSLT and one within 15 minutes of sleep onset on nocturnal polysomnogram).
NT2 requires the above sleep study findings, without cataplexy or low CSF hypocretin‐1 (or untested hypocretin). Other causes of daytime sleepiness should be ruled out (Table 1), especially in children. (See Ref.9 for discussion of diagnostic complexities.)
TABLE 1.
Evaluation of medical causes of secondary narcolepsy
| Type | Specific diagnoses | Evaluation |
|---|---|---|
| Neoplasm | Brain tumor (hypothalamus: eg, craniopharyngioma); lymphocytic or non‐lymphocytic acute leukemia | Brain neuroimaging, complete blood count |
| Inflammatory | Guillain Barré syndrome; acute encephalomyelitis; multiple sclerosis; neurolupus; anti‐NMDA receptor anti‐Ma2 and anti‐aquaporin‐4 encephalitis; neurosarcoidosis; post H1N1 vaccination or infection narcolepsy | Chronology, blood and/or CSF testing for antibodies or inflammatory markers |
| Infectious | Infectious encephalitis; meningoencephalitis | Lumbar puncture |
| Traumatic | Head trauma; Diffuse axonal injury | Chronology, neuroimaging |
| Iatrogenic | Cerebral irradiation | Chronology |
| Malformation | Holoprosencephaly; callosal agenesis | Imaging during pregnancy |
| Genetic | Myotonic dystrophy, Prader Willi syndrome; Coffin‐Lowry syndrome; Moebius syndrome; Hereditary Sensory and Autonomic Neuropathy Type 1E (HSAN1E); Autosomal dominant cerebellar ataxia‐deafness‐narcolepsy syndrome (ADCA‐DN); mutation of the preprohypocretin | Neurological examination, DNA testing for mutations |
| Metabolic | Niemann‐Pick type C; Rapid‐onset obesity, hypoventilation, hypothalamic dysfunction and autonomic dysfunction (ROHHAD) | Filipin staining test; clinical, hormonal explorations, methylation analysis, cytogenetic and molecular analysis |
| Neurodegenerative | Parkinson's disease | Neurological examination (parkinsonism), DAT scan |
The table summarizes the known medical causes of secondary narcolepsy and the typical clinical/laboratory evaluations for each type. Consideration should be given on a case‐by‐case basis to the possibility of any of these diagnoses and the need for evaluation, particularly in children presenting with possible narcolepsy.
CSF, cerebrospinal fluid; DAT, dopamine transporter positron emission tomography scan; NMDA, anti‐N‐methyl‐D‐aspartate.
Narcolepsy is typically caused by polygenic risk factors and environmental factors.10 HLA allele DQB1*06:02 is carried by almost all NT1 patients (except for familial cases),1, 11 and 42% of NT2 patients, vs. ~20% in the population.12 When cataplexy is unclear, genotyping may be used as a screening test before proposing lumbar puncture to assay CSF hypocretin‐1. Substantial evidence suggests that in most NT1 and some NT2 cases, HLA, and other risk loci13 produce susceptibility to an autoimmune response triggered by environmental factors (eg, streptococcus or H1N1 influenza infection or vaccination), resulting in the destruction of >90% of hypocretin‐1‐expressing neurons in NT1.14, 15 Hypocretin‐1 stimulates wake‐inducing monoamines, activating arousal systems which consolidate wakefulness into a single daily episode. NT2 has been considered a prodromal/incomplete form of NT1,16, 17 or a syndrome resembling idiopathic hypersomnia.18
Narcolepsy impacts school and work functioning, driving, interpersonal relationships, and quality of life.19 Typically, brief sleep attacks are followed by several hours of normal wakefulness. Total daily sleep time is usually normal but may be prolonged in children (rarely in adults) or around disease onset.20 Cataplexy consists of seconds to minutes of sudden, bilateral loss of muscle tone, with maintained consciousness, usually triggered by positive emotions.21 Weight gain is frequent at onset. Other symptoms include sleep‐related hallucinations,1 sleep paralysis, dyssomnia, nightmares, REM sleep behavior disorder, atypical eating disorders, attention problems, and depression. Atypical features in childhood or at onset include general weakness instead of cataplexy, avoidance behavior,22 hyperactivity,23 complex movement disorders, and loss of orofacial muscle tone.24
Psychotic disorders are characterized by delusions and hallucinations. Delusions are firm beliefs that differ from convictions based on false or incomplete information, confabulation, or dogma. True hallucinations are sensory experiences in the absence of an external stimulus, perceived as “real.” They differ from dreaming because they occur during wakefulness, and from illusions (which are misperceptions of real stimuli). Here, we use “psychotic‐like symptoms” to describe experiences of narcolepsy patients which are not classically “psychotic”: (i) “hallucinations” (usually visual) occurring at the sleep/wake boundary (hypnagogic hallucinations at sleep onset or hypnopompic at sleep offset), rapidly recognized by the patient as “not real”; (ii) delusion‐like explanations offered by some patients for their vivid hallucination‐like experiences; (iii) dissociation or derealization. Rarely, narcolepsy patients also have hallucinations when awake, for example, while driving.4, 25 Psychotic‐like symptoms are sometimes mistaken for psychotic symptoms of schizophrenia,26, 27, 28 for example, in an adolescent with sleep disturbances and “visions,” thus delaying appropriate narcolepsy therapy. But some narcolepsy patients do experience classical psychotic symptoms, apparently because of a comorbid psychotic disorder or side effects of stimulants.
We report here on a systematic review of the literature on psychotic and psychotic‐like symptoms in adults and children with narcolepsy, a topic last fully reviewed in 2003.29 Less comprehensive discussions have appeared recently in case reports or cohort studies.4, 30, 31, 32 We reviewed cohort reports, reports of cases with narcolepsy and psychotic features, and papers relevant to the treatment of cases with these features (including drug‐induced psychosis). We also report a statistical analysis of clinical differences between reported narcolepsy cases with psychosis‐like symptoms vs. those with comorbid psychotic diagnoses.
1.1. Aims of the study
The objectives are to (i) facilitate correct diagnosis by defining subgroups of cases with these features; and (ii) provide guidance for clinical management, including the safety and use of psychostimulants, and the indications and choice of antipsychotic drug treatments.
2. MATERIALS AND METHODS
2.1. Medline search
We searched pubmed.ncbi.nlm.nih.gov/on 27 April 2020 for narcolepsy[MeSH Major Topic] AND (psychosis OR schizophrenia OR delusion OR bipolar disorder OR side effect OR safety). We omitted “hallucinations” because, as a core narcolepsy symptom, it yielded hundreds of largely non‐relevant results. We examined articles in English or French since 1950, excluding those that were not about narcolepsy in humans, or did not address psychotic‐like or psychotic symptoms. We selected additional relevant papers from the references in papers reviewed in full text.
2.2. Quantitative analysis
The cohort reports were not amenable to meta‐analysis because of their variable study designs and outcome measures. We performed quantitative analyses (using SPSS 23.0) comparing 17 reported cases with psychotic‐like symptoms attributed to narcolepsy, and 41 diagnosed by the authors as narcolepsy plus a psychotic disorder. Each case was reviewed (by C.H.) with a checklist of clinical features (Table S3), rating features “present” (mentioned/strongly suggested) or “absent” (denied/not described). For ages at onset of sleep and psychotic symptoms, normality of the distribution was inspected graphically and confirmed (Kolmogorov–Smirnov test), equality of variance confirmed (Levene's test), and the groups were contrasted with Student's t tests. For dichotomous variables, χ 2 tests were performed.
3. RESULTS
3.1. Literature search
Systematic PubMed search identified 187 articles. Based on abstracts, we excluded 44 articles that were not about narcolepsy and psychotic symptoms, 4 with inaccessible full text, 12 not in English or French; 9 in a non‐narcolepsy cohort, 15 about non‐relevant outcomes, and 1 letter to the editor without additional data/hypotheses. We reviewed the full text of the remaining 100 articles, including 26 reviews, 27 case reports, 23 cohort studies, 20 clinical trials, and 4 meta‐analyses (of narcolepsy treatment trials) (Figure 1; Table S2 lists citations for each article type).
FIGURE 1.
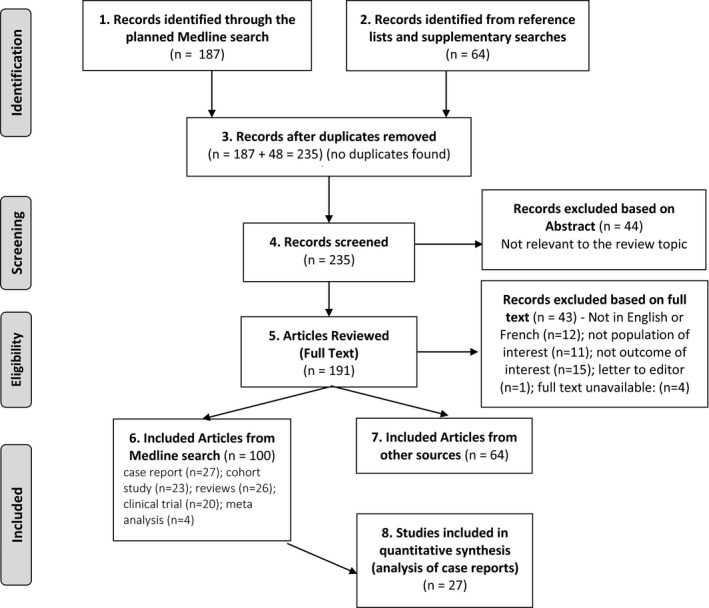
Flow chart of review process. The systematic literature search was conducted on 27 April 2020, using the following Search Builder: narcolepsy[MeSH Major Topic] AND (psychosis OR schizophrenia OR delusion OR bipolar disorder OR safety OR side effect, yielding 187 records. An additional 48 records were identified via reference lists from the 187 selected records, or from supplementary Medline searches (15 papers on mechanisms or adverse effects of drugs used to treat narcolepsy; 12 with relevance to the discussion of the relationship between narcolepsy and psychosis; and 21 with more relevance to discussion of narcolepsy or to psychosis but not their relationship). None of the additional records were cohort or case reports. We list as excluded records those that were identified by systematic search but not selected as eligible for inclusion in the qualitative or quantitative analyses for the reasons cited
3.2. Systematic review: Qualitative results
Since the first 13 cases published in 1884,33 case and cohort reports have discussed the relationship between narcolepsy and psychotic symptoms. Authors generally described three groups:27 (i) hallucinations as part of the narcolepsy process, clearly different from psychosis; (ii) patients with narcolepsy and a comorbid, independent psychotic disorder (schizophrenia, schizoaffective disorder, or more rarely a mood disorder with psychotic features); and (iii) psychotic symptoms provoked by psychostimulants treatment. Based on a larger number of reports, we suggest a modified grouping approach. Group 1 is typical narcolepsy. Group 2 (sometimes called “the psychotic form of narcolepsy”) comprises more severe and atypical psychotic‐like symptoms thought to be driven by the same mechanisms as in Group 1. Group 3 patients probably have two independent diagnoses, although an etiological relationship remains possible, especially in childhood‐onset cases. Psychostimulant‐induced psychosis can occur in each group, particularly at high dosages.
3.3. Psychotic‐like symptoms in typical narcolepsy
Hallucinations are described in 20%34 to 80%25 of NT1, and in 28.2% of NT2 patients, when falling asleep (55% of those with hallucinations), waking up (3%), or both (42%), with 18% reporting daytime hallucinations while wide awake.4 They increase when lying supine, which is not observed in psychotic disorders.
An observational study found that hallucinations (predominantly non‐verbal) were as frequent in 28 NT1 patients without psychotic diagnoses as in 21 schizophrenia patients.8 All sensorial modalities were observed in both groups. Hallucinations were predominantly sleep‐related in narcolepsy (75% vs. 4.8%, p < 0.0001) and multimodal (predominantly auditory verbal) in schizophrenia (76% vs. 3.6%, p < 0.0001). The groups had similar proportions with visual hallucinations (shadows, monsters, demons, or animals [zoopsia]).
Fortuyn et al. interviewed 60 patients with NT1, 102 with schizophrenia, and 120 healthy controls using the Schedules for Clinical Assessment in Neuropsychiatry 2.1.25 More NT1 patients than controls (83% vs. 2%, p < 0.001) reported hallucination‐like experiences that are not considered as definitely “psychotic” in psychiatric studies (presence of unseen‐unheard visitors, falling/flying sensations, out‐of‐body experiences, altered perception of time, déjà‐vu, derealization), but this percentage was not different in schizophrenia patients (70%). Compared with schizophrenia, narcolepsy patients more often reported visual hallucinations (15% for simple and 38% for complex images), non‐verbal auditory hallucinations (footsteps, slamming/creaking of doors, animal sounds – 50% vs. 15%), kinesthetic and tactile hallucinations (heat, pain, crawling under the skin or in the genital area, 48%) and less frequently olfactory hallucinations. Verbal hallucinations were less frequent (18 vs. 45%). NT1 and schizophrenia patients equally experienced multimodal hallucinations. NT1 patients had more fantastic delusions and false memories than controls. Rarely, NT1 patients reported grandiose (2%), fantastic (5%), or persecutory delusions (2%).
Leu‐Semenescu et al4 studied the characteristics of hallucinations in 100 narcolepsy patients (54 NT1, 46 NT2) and 100 Parkinson's disease patients. Among the 45% of narcolepsy patients with hallucinations (59% in NT1, 28% in NT2), 24% had auditory (changing voices, footsteps) or visual illusions (including dyschromatopsia); 15% had unformed hallucinations (presence of a person; a passing animal); 95% had formed, visual hallucinations (human, animal, or fantastic figures such as ghosts, vampires; complete or distorted, with vivid colors) with more than half of these reporting kinetic hallucinations (lateral movement in bed as if on a slippery surface, falling, being sucked into the bed, flying, levitating, out‐of‐body experiences). One‐third of patients reported tactile hallucinations (air blowing on oneself, being touched, burned, bitten, trampled, strangled, or sexually abused). Auditory hallucinations could be non‐verbal (44%, doors opening, alarm ringing, footsteps, plates breaking) or verbal (33%, being called by name, hearing conversation fragments). Hallucinations were usually multimodal (98%, primarily NT1) and sometimes holistic (42%). Hallucinations were associated with sleep paralysis and REM sleep behavior disorder but not with cataplexy, HLA positivity, or sleepiness, consistent with other studies.35
3.4. Narcolepsy with atypical psychotic‐like symptoms
The term “psychotic form of narcolepsy” has been suggested in patients with psychotic‐like features resembling more severe forms of typical narcolepsy symptoms, sometimes leading to a misdiagnosis of schizophrenia.27, 36 They had vividly realistic and emotional dreams (8% of narcolepsy patients in Leu‐Semenescu et al4) and hallucinations (which can be nightly). Episodes of dream‐reality confusion were reported by 83% of 46 NT1 patients vs. 15% of 41 healthy controls (p < 0.0001),37 lasting up to several weeks and associated with severe, frequent cataplexy, and treatment‐resistance. These symptoms may be worsened by antipsychotic drugs26, 38 and reduced by psychostimulants.39
Some patients explain these experiences with what appear to be secondary “delusional” thoughts,38 with fantastic, persecutory, sexual abuse, mystical, megalomaniacal, referential, or paranormal themes. Several case studies mentioned medico‐legal consequences after sincere but possibly false rape allegations.40, 41 Several hypotheses have been proposed. Fortuyn et al25 noted that some narcolepsy patients (otherwise mentally healthy) had difficulty in differentiating hallucinations from reality. Impaired insight was more common in narcolepsy than in Parkinson's disease.4 Memory deficits have been reported (false beliefs based on false memories).37 Narcolepsy patients often complain of memory problems and may have deficits in source memory (monitoring a memory's origin),42 but show no deficits on formal memory testing.43, 44
Children with narcolepsy have hallucinations (39–50%) and may have difficulty in distinguishing dreaming from reality.7 Clinicians sometimes misinterpret their hallucinations and behavioral changes as psychotic disorganization.45
3.5. Quantitative comparison of atypical narcolepsy and dual diagnosis cases
Comorbidity of narcolepsy with a psychotic disorder has been documented primarily in case reports or series (Table S1). A separate psychotic disorder diagnosis has usually been assigned when the symptoms met diagnostic criteria and appeared unrelated to REM intrusion. Table S1 describes 58 cases: 41 with a dual narcolepsy and psychotic disorder diagnosis (Group 3); and 17 described as “psychotic” or “delusional” narcolepsy (Group 2). Table 2 summarizes analyses of group differences (Table S4 provides details of our ratings). Dual diagnosis patients usually developed narcolepsy first, and then (6.8 years later on average) psychosis, mostly (38/41 cases) in the schizophrenia spectrum. They more often had disorganized symptoms including thought disorder (65.9% vs. 17.6%). Group 2 cases were more likely to have visual (88.2% vs. 19.5%) and multimodal hallucinations, zoopsia, sexual and mystical delusions, and false memories.
TABLE 2.
Case reports of “psychotic form of narcolepsy” vs. comorbid narcolepsy and psychotic disorder: Differences in clinical features
| All cases (n = 58) | “Psychotic form” (n = 17) | Comorbid cases (n = 41) | ||||
|---|---|---|---|---|---|---|
| Clinical feature (mean) | a | a | a | t | df | p |
| Age at onset of sleep symptoms | 19.0 | 25.3 | 16.6 | 2.40 | 46 | 0.02 |
| Age at onset of psychotic‐like symptoms | 23.5 | 23.8 | 23.4 | 0.09 | 46 | 0.93 |
| Sleep symptoms, N (%) | n = 52 | n = 15 | n = 37 | χ 2 | df | p |
| Cataplexy | 48 (92.3%) | 13 (86.7%) | 35 (94.6%) | 0.95 | 1 | 0.33 |
| Sleep‐related hallucinations | 40 (76.9%) | 13 (86.7%) | 27 (73.0%) | 1.13 | 1 | 0.29 |
| Sleep paralysis | 33 (63.5%) | 8 (53.3%) | 25 (67.6%) | 0.93 | 1 | 0.33 |
| Psychotic‐like symptoms, N (%) | n = 58 | n = 17 | n = 41 | χ 2 | df | p |
| Hallucinations | 51 (87.9%) | 17 (100%) | 34 (82.9%) | 1.27 | 1 | 0.26 |
| Auditory | 50 (86.2%) | 16 (94.1%) | 34 (82.9%) | 1.27 | 1 | 0.26 |
| Visual | 23 (39.7%) | 15 (88.2%) | 8 (19.5%) | 23.72 | 1 | 0.00 |
| Multimodal | 22 (37.9%) | 14 (82.4%) | 8 (19.5%) | 20.16 | 1 | 0.00 |
| Zoopsia | 2 (3.45%) | 2 (11.8%) | 0 (0.00%) | 5.00 | 1 | 0.03 |
| Delusional thoughts | 56 (96.6%) | 17 (100%) | 39 (95.1%) | 0.86 | 1 | 0.35 |
| Persecution | 38 (65.5%) | 11 (64.7%) | 27 (65.9%) | 0.01 | 1 | 0.93 |
| Poisoning | 1 (1.72%) | 1 (5.88%) | 0 (0.00%) | 2.45 | 1 | 0.12 |
| Sexual | 10 (17.2%) | 7 (41.2%) | 3 (7.32%) | 9.66 | 1 | 0.00 |
| Megalomaniac | 3 (5.17%) | 0 (0.00%) | 3 (7.32%) | 1.31 | 1 | 0.25 |
| Mystic | 9 (15.5%) | 6 (35.3%) | 3 (7.32%) | 7.18 | 1 | 0.01 |
| Jealousy | 4 (6.90%) | 1 (5.88%) | 3 (7.32%) | 0.04 | 1 | 0.84 |
| Hypochondriac | 2 (3.45%) | 1 (5.88%) | 1 (2.44%) | 0.43 | 1 | 0.51 |
| Fantasy | 1 (1.72%) | 1 (5.88%) | 0 (0.00%) | 2.45 | 1 | 0.12 |
| Influence | 5 (8.62%) | 2 (11.8%) | 3 (7.32%) | 0.30 | 1 | 0.58 |
| Reference | 6 (10.3%) | 3 (17.6%) | 3 (7.32%) | 1.38 | 1 | 0.24 |
| Fake memory | 5 (8.62%) | 4 (23.5%) | 1 (2.44%) | 6.79 | 1 | 0.01 |
| Disorganized symptoms | 30 (51.7%) | 3 (17.6%) | 27 (65.9%) | 11.18 | 1 | 0.00 |
| Derealization | 1 (1.72%) | 1 (5.88%) | 0 (0.00%) | 2.45 | 1 | 0.12 |
| n = 58 | n = 17 | n = 41 | χ 2 | df | p | |
| Possible drug‐induced psychosis? | 20 (34.5%) | 4 (23.5%) | 16 (39.0%) | 1.95 | 1 | 0.16 |
We classified 58 cases (reported in 27 papers, Table S2) according to the authors’ diagnostic conclusion (psychotic form of narcolepsy vs. comorbid narcolepsy and psychotic disorder). For each case, we recorded age at onset for sleep and psychotic‐like symptoms and presence/absence of the clinical features listed in the table. A feature was considered “present” if it was explicitly mentioned or very clearly suggested by the clinical description, otherwise, it was considered “absent,” that is, we attempted not to infer the presence of symptoms beyond the data in the report. P‐values less than 0.05 are bolded.
For age at onset variables (sleep problems or psychotic‐like symptoms), 10 cases were excluded from analysis because no numerical information was provided about ages. In 4 of the 48 remaining cases, onset was described as occurring “before the age of X” and we entered X into the analysis. Thus, N for these analyses was 48 and the t‐tests had 46 df).
These symptomatic differences are not a validation of these subgroupings. Rather, they quantify the clinical judgments of the various authors (and probably a consensus of the field) that Group 2 patients are experiencing a more severe form of classical narcolepsy symptoms, with the same underlying pathophysiology. No large‐scale or prospective data exist to better describe or validate these subgroups and the gray areas between them, but they have implications for treatment as discussed below.
More rarely,38 narcolepsy emerges as a possible primary diagnosis in “schizophrenia” patients in whom antipsychotics were poorly tolerated or overly sedating (as discussed further below). This is a challenging clinical situation,10 because antipsychotic medications interfere with polysomnography and MSLT by reducing REM sleep time and daytime mean sleep onset latency. By contrast, antipsychotic withdrawal can produce REM sleep rebound and a false positive narcolepsy diagnosis.10 Undertaking prolonged antipsychotic washout is a difficult decision. An alternative is to measure CSF hypocretin‐1 levels, which remain in the normal range during antipsychotic treatment.113
3.6. Is there an association between narcolepsy and psychotic disorders?
Older studies suggested an increased prevalence of narcolepsy among schizophrenia patients31, 36 and (retrospectively) a greater risk of schizophrenia among narcolepsy patients vs. among controls.46 Narcolepsy was diagnosed in 7% of a schizophrenia cohort,38 but the study design was flawed (the estimation of 7% was based on 5 misdiagnosed in‐patients plus a small cohort of current out‐patients, rather than collecting an in‐patient cohort during a defined time period). A well‐designed study could not replicate this finding32: narcolepsy symptom questionnaires were administered to 366 consecutive hospitalized adults with schizophrenia spectrum disorders. Among 24 with possible narcolepsy (after sleep medicine consultations), 5 carried HLA DQB1*06:02, of whom 3 accepted lumbar puncture, but all had normal hypocretin‐1 levels, thus no NT1 cases were detected. Sleep studies were not performed because antipsychotics could not be discontinued. Further, among 548 adult NT1 patients in two large sleep centers, 1.8% had a history of schizophrenia spectrum psychoses (close to population prevalence), in whom anti‐NMDA antibodies were not detected.47 However, early‐onset NT1 (<16 years old) was more common in patients with (60%) than without (35%) a comorbid psychotic disorder.
A significant association of schizophrenia was reported in early‐onset NT1 in a prospective study of 151 narcolepsy patients in Taiwan's only child/adolescent sleep clinic.31 Ten of 102 NT1 patients (9.8%) had comorbid schizophrenia based on clinical and research interviews. Average age at onset was 11.25 for NT1 and 15.8 for schizophrenia. Compared with 37 age‐matched NT1‐only and 13 schizophrenia‐only cases, comorbid cases had poorer antipsychotic response and increased weight. However, in a population‐based study of 38 narcoleptic children in Western Sweden (most with cataplexy, sleep study abnormalities, and exposure to anti‐H1N1 vaccination, but no hypocretin deficiency), 43% had a psychiatric diagnosis, but no psychotic disorder.48 Thus, the Taiwan finding awaits replication. We note that in the largest recent series of comorbid cases, onset of sleep symptoms occurred before 16 years of age in 10/105 and 6/10 cases47 (Canellas et al5 provide a useful structured interview to evaluate such cases).
There is an ongoing discussion in the literature about possible common genetic or environmental risk factors or shared hypocretin pathophysiology49 in producing overlapping symptoms.5
3.7. Proposed mechanisms of psychotic‐like symptoms in narcolepsy
Typical hallucinations in narcolepsy are attributed to partial REM sleep intrusions while awake.4, 38, 50 Typical sleep‐related hallucinations generally improve with adequate wake‐promoting (and not with antipsychotic) treatment, and in some cases serotonergic antidepressants are added because they suppress REM activity (see discussion below), suggesting that these symptoms are directly related to narcolepsy.27, 38
Overlapping autoimmune mechanisms have been hypothesized. There is an extensive literature on infectious and autoimmune factors in schizophrenia.51 Older studies suggested an association of HLA DQB1*0602 with schizophrenia,52 but recently Sekar et al53 reported strong evidence that genetic association near the HLA region on chromosome 6 is largely explained by structural sequence variants in the complement 4 gene which has a role in synaptic pruning. There are conflicting data regarding anti‐NMDA antibodies in dual diagnosis cases.47, 54 It has been proposed that loss of hypocretin neurons (which project to the ventral tegmental area, prefrontal cortex, and nucleus accumbens) leads to impaired mesocortical‐pathway signaling and psychosis,55 possibly interacting with an independent susceptibility to psychosis.29
3.8. Medication‐induced psychosis in narcolepsy patients
All primary narcolepsy drug treatments enhance dopaminergic neurotransmission, a mechanism associated with a risk of provoking psychosis. Classical psychostimulants (methylphenidate, amphetamines, and methamphetamine–now considered second‐line narcolepsy treatments) increase synaptic dopamine primarily by noncompetitively blocking the dopamine transporter (reuptake site) without increasing presynaptic release.56 Methylphenidate57 and amphetamines are generally considered safe in narcolepsy.58 A Japanese‐language paper on a study of 329 NT1 patients59 followed up after a mean of 15.4 years (mentioned in reference27 but not accessible to us) reported a 3.2% rate of psychostimulant‐induced psychosis. An English‐language chapter by the same author about the same study60 describes the methodology as retrospective data collection by self‐report questionnaire. Another retrospective study (chart review) reported psychotic events in 5% of 58 patients on “standard” dosages of psychostimulants, primarily methylphenidate, vs. 24% of 58 patients receiving “high” dosages (>120 mg/day; odds ratio = 12.0), with additional adverse psychiatric outcomes.61
Modafinil, a first‐line treatment, indirectly reduces dopamine and norepinephrine reuptake through serotonin‐mediated inhibition of aminobutyric acid (GABA) release62 and enhances dopamine‐dependent modulation of adrenergic receptors,63 with a good safety profile in narcolepsy.64, 65, 66 Psychiatric adverse events have been reported, including rare cases of psychosis,67, 68 elated mood,69, 70, 71, 72 and switch to mania with psychosis.72, 73, 74 In a pharmacovigilance study, 2,416 modafinil prescribers reported one manic and two psychotic episodes.75 A small study of children with narcolepsy reported one case with exacerbation of a pre‐existing psychotic disorder.68 A meta‐analysis of adjunctive modafinil and its derivative armodafinil in schizophrenia showed no improvement, and no increase in psychotic symptoms.76
Sodium oxybate (gamma hydroxybutyrate, GHB) inhibits dopamine release via activation of GABA‐B circuits and the GHB receptor77, 78 which could upregulate dopamine receptors. It is generally well‐tolerated in adults and children with narcolepsy.79, 80, 81, 82, 83 Psychotic symptoms have been reported (usually shortly after starting or resuming treatment).73, 84, 85, 86, 87 Emergence or exacerbation of psychotic symptoms by sodium oxybate was retrospectively reported in 5 of 90 narcoleptic patients with no psychiatric history,87 and 1 of 63 children in a clinical trial.88 Mazindol, a sympathomimetic amine, reduces dopamine and norepinephrine reuptake. Psychotic symptoms were not reported in a retrospective study of 94 adult and child patients89 or a clinical trial (n = 37).90 Pitolisant enhances histaminergic transmission via inhibition of presynaptic uptake (inverse histamine H3 receptor agonist effect).91 It indirectly increases release of dopamine, norepinephrine, and acetylcholine.92 Anxiety and depression have been observed but not psychosis,93, 94, 95 in limited data.
3.9. An algorithm for clinical practice
Based on literature review, we suggest an algorithm for evaluating and treating narcolepsy patients with psychotic symptoms (Figure 2).
FIGURE 2.
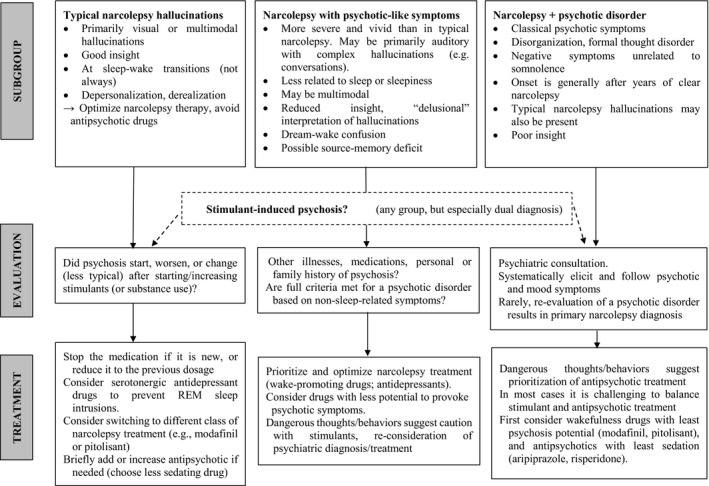
Algorithm for evaluating and treating narcolepsy patients with psychotic symptoms
Typical sleep‐related hallucinations of narcolepsy, recognized as such by the patient, and without other psychotic features (Group 1), are treated with drugs for narcolepsy, and not antipsychotics. The most common psychosis‐related complication in all groups is the onset of psychotic or worsening atypical psychotic‐like symptoms after a wake‐promoting drug has been introduced or its dosage increased. The new drug is generally stopped, or the previous dosage restored; if symptoms resolve rapidly, drug‐induced psychosis is the likely diagnosis. Brief treatment with a less sedating antipsychotic (eg, aripiprazole or risperidone) may be helpful, but further optimization of narcolepsy treatment should then be attempted. If the psychosis was provoked by classical stimulants, modafinil or pitolisant might be considered.
Both the typical wake‐state hallucinations of narcolepsy (Group 1) and their atypical variants (Group 2) are presumed to represent REM intrusions into wakefulness, with atypical patients sometimes developing delusion‐like ideas to rationalize the experiences. Antidepressants with serotonergic activity are known to suppress REM sleep,96 and in clinical practice, they are frequently prescribed for typical narcoleptic patients to control REM intrusion phenomena such as cataplexy and hallucinations.97 This is based on anecdotal observations98 and consensus guidelines99, 100 rather than controlled studies. The same strategy may be attempted in Group 2 patients, in the hope that additional treatment of REM intrusions will improve both the atypical hallucinations and the delusion‐like rationalizations. Optimizing wake‐promoting medication or adding an SSRI/SNRI is recommended to reduce psychotic‐like symptoms. Psychiatric consultation is advised for patients with dangerous impulses or behaviors.
A comorbid psychotic disorder should be considered if hallucinations and delusional ideas emerge and appear unlikely to be related to REM intrusions. We found no published clinical trials for the treatment of patients with dual diagnoses. Narcolepsy misdiagnosed as schizophrenia is probably rare in adults but might be more common in children with narcoleptic and psychotic‐like symptoms. Treatment of dual diagnosis cases is challenging because stimulants increase dopamine release which can induce psychosis, whereas antipsychotic drugs can worsen sleepiness by blocking dopamine and histamine transmission. Kishi et al 27 recommended maintaining a wake‐promoting drug (despite the small risk of psychotic exacerbation), preferably modafinil because of its predominantly non‐dopaminergic mechanism.67 Pitolisant may be useful in our experience, although there is limited evidence regarding its potential to provoke psychosis. Less sedating antipsychotics like risperidone or aripiprazole are recommended4, 5, 101, 102; aripiprazole may stabilize rather than simply block dopaminergic neurotransmission.102 In some case reports, olanzapine, clozapine, haloperidol, or quetiapine was effective.30, 47, 103, 104 The clinical management of these complex situations requires further study.
4. DISCUSSION
Most narcolepsy patients with psychotic or psychotic‐like symptoms will fit into one of three groups, and patients in any group may experience drug‐induced psychosis (especially those on high doses of psychostimulants and those with previous psychotic symptoms):
Patients with typical hallucinations of narcolepsy. The intrusion of REM sleep phenomena into wakefulness causes hallucinations (usually visual, at sleep‐wake transitions, recognized by the patient as “not real”), cataplexy, and sleep paralysis. These patients are recognized as “not psychotic” by sleep medicine specialists.
Atypical narcolepsy with psychotic‐like symptoms (“psychotic form of narcolepsy”). These patients have more severe and vivid hallucinatory, daytime dream‐like experiences and may develop delusion‐like rationalizations (analogous to severe obsessive‐compulsive disorder with delusion‐like ideas about obsessions). They may have deficits in insight and source memory. They may worsen on antipsychotic drugs and improve on psychostimulants. Misdiagnosis is more common, especially in children.
Narcolepsy with a comorbid psychotic disorder. These patients have psychotic symptoms unrelated to sleep phenomena, often including disorganized behavior and thought disorder starting years after narcolepsy onset (Table 2, Table S2). It is unlikely that narcolepsy is frequently misdiagnosed as schizophrenia in adults,32 although case reports demonstrate that it can occur. However, children and adolescents with NT1 may be at increased risk of comorbid schizophrenia spectrum disorders.31 It remains unclear whether there are shared autoimmune mechanisms.105
The possible association of NT1 with schizophrenia spectrum disorders in childhood deserves further study—a difficult challenge given that both presentations are rare in the population. Studies of children with NT1 have consistently found increases of more common psychiatric disorders,45, 106 including attention deficit‐hyperactivity disorder (ADHD), internalizing (depressive and anxiety) disorders, and learning problems.48, 107, 108, 109, 110, 111 This broad vulnerability has been attributed in part to excessive daytime sleepiness111 and impulsive/hyperactive counterstrategies to fight it,108 to persistent, frightening sleep‐related hallucinatory experiences107 and to psychological distress because of the overall disease burden. However, an additional role of organic lesions is suggested by the association of depression with severity of brain white matter structural changes observed in adult NT1 using diffusion tensor imaging.112
If the association of early‐onset NT1 with schizophrenia is confirmed in future studies, several explanations are possible. A direct effect of central Hcrt‐1 deficiency has been considered, because Hcrt‐1 influences dopaminergic neurotransmission in the midbrain and prefrontal cortex, which are involved in the pathophysiology of schizophrenia.55 However, schizophrenia is rare in adult‐onset NT1 patients despite the dramatic loss of central Hcrt‐1, and CSF Hcrt‐1 is normal in schizophrenia113, 114 (although these small studies do not exclude a low‐Hcrt‐1 subgroup). CSF Hcrt‐1 is also typically normal in adult major depression.55 It seems unlikely that reduced Hcrt‐1 directly leads to psychosis.
Narcolepsy onset in childhood is typically associated with symptoms never observed in adult‐onset cases, including complex movement disorders (lasting up to two years after onset and then disappearing), massive weight gain, and psychiatric symptoms. This suggests that there is transient inflammation in the hypothalamus that extends beyond hypocretin neurons,115 or an acute destabilization of dopaminergic‐hypocretinergic interactions.24 Furthermore, Hcrt‐1 deficiency in childhood could impair normal neurodevelopment in ways that either increase the child's risk of schizophrenia or that lead to an earlier age at onset in predisposed individuals. There is a partial overlap in the structural MRI changes observed in childhood‐onset schizophrenia116 and in childhood NT1,117 including reduced gray matter volume in prefrontal cortex and cerebellum. It is possible that these and other changes have a major impact on schizophrenia risk in a minority of children (representing a syndromic type of schizophrenia), or that they constitute an additional risk factor for schizophrenia which has a large number of interacting genetic118, 119 and environmental120 risk factors. Larger‐scale data are needed on prospective follow‐up and on structural brain changes and cognitive functioning in children and adolescents with narcolepsy. Future studies of the association of childhood narcolepsy and schizophrenia could inform our understanding of the etiopathology of both disorders.
5. PERMISSION TO REUSE AND COPYRIGHT
Figures, tables, and images will be published under a Creative Commons CC‐BY license and permission must be obtained for use of copyrighted material from other sources (including re‐published/adapted/modified/partial figures and images from the Internet). It is the responsibility of the authors to acquire the licenses, to follow any citation instructions requested by third‐party rights holders, and cover any supplementary charges.
CONFLICT OF INTEREST
During the last two years, David Cohen reported past consultation for or the receipt of honoraria from Otsuka, Shire, Lundbeck, and IntegraGen. All other authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
CH conducted the literature search, reviewed references, and wrote the first draft of the manuscript. CL and DC reviewed key papers and contributed to revisions. IA, ML, and JBM contributed to the final revision of the manuscript with their expertise in sleep medicine. All authors read and approved the final manuscript and contributed to the drafting and revising of the paper.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/acps.13300.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
CH and CLL would like to express their appreciation for the contributions and expertise of the Sleep Disorder Unit of Pitié‐Salpétrière Hospital and to the Department of Functional Exploration of Robert Debré Hospital. The authors declare that this study was conducted without funding.
REFERENCES
- 1.Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet Lond Engl. 2007;369(9560):499‐511. 10.1016/S0140-6736(07)60237-2. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 3.Dauvilliers Y, Montplaisir J, Molinari N, et al. Age at onset of narcolepsy in two large populations of patients in France and Quebec. Neurology. 2001;57(11):2029‐2033. [DOI] [PubMed] [Google Scholar]
- 4.Leu‐Semenescu S, De Cock VC, Le Masson VD, et al. Hallucinations in narcolepsy with and without cataplexy: contrasts with Parkinson’s disease. Sleep Med. 2011;12(5):497‐504. 10.1016/j.sleep.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Canellas F, Lin L, Julià MR, et al. Dual cases of type 1 narcolepsy with schizophrenia and other psychotic disorders. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2014;10(9):1011‐1018. 10.5664/jcsm.4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dauvilliers Y, Paquereau J, Bastuji H, Drouot X, Weil J‐S, Viot‐Blanc V. Psychological health in central hypersomnias: the French Harmony study. J Neurol Neurosurg Psychiatry. 2009;80(6):636‐641. 10.1136/jnnp.2008.161588. [DOI] [PubMed] [Google Scholar]
- 7.Jardri R, Bartels‐Velthuis AA, Debbané M, et al. From phenomenology to neurophysiological understanding of hallucinations in children and adolescents. Schizophr Bull. 2014;40(Suppl 4):S221‐232. 10.1093/schbul/sbu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plazzi G, Fabbri C, Pizza F, Serretti A. Schizophrenia‐like symptoms in narcolepsy type 1: shared and distinctive clinical characteristics. Neuropsychobiology. 2015;71(4):218‐224. 10.1159/000432400. [DOI] [PubMed] [Google Scholar]
- 9.Schneider L, Mignot E. Diagnosis and Management of Narcolepsy. Semin Neurol. 2017;37(4):446‐460. 10.1055/s-0037-1605554. [DOI] [PubMed] [Google Scholar]
- 10.Mignot E, Lammers GJ, Ripley B, et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002;59(10):1553‐1562. [DOI] [PubMed] [Google Scholar]
- 11.Aran A, Lin L, Nevsimalova S, et al. Elevated anti‐streptococcal antibodies in patients with recent narcolepsy onset. Sleep. 2009;32(8):979‐983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Capittini C, De Silvestri A, Terzaghi M, et al. Correlation between HLA‐DQB1*06:02 and narcolepsy with and without cataplexy: approving a safe and sensitive genetic test in four major ethnic groups. A systematic meta‐analysis. Sleep Med. 2018;52:150‐157. 10.1016/j.sleep.2018.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Miyagawa T, Tokunaga K. Genetics of narcolepsy. Hum Genome Var. 2019;6:4. 10.1038/s41439-018-0033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh AK, Mahlios J, Mignot E. Genetic association, seasonal infections and autoimmune basis of narcolepsy. J Autoimmun. 2013;43:26‐31. 10.1016/j.jaut.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partinen M, Kornum BR, Plazzi G, Jennum P, Julkunen I, Vaarala O. Narcolepsy as an autoimmune disease: the role of H1N1 infection and vaccination. Lancet Neurol. 2014;13(6):600‐613. 10.1016/S1474-4422(14)70075-4. [DOI] [PubMed] [Google Scholar]
- 16.Pizza F, Vandi S, Liguori R, et al. Primary progressive narcolepsy type 1: the other side of the coin. Neurology. 2014;83(23):2189‐2190. 10.1212/WNL.0000000000001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopez R, Barateau L, Evangelista E, et al. Temporal Changes in the Cerebrospinal Fluid Level of Hypocretin‐1 and Histamine in Narcolepsy. Sleep. 2017;40(1): 10.1093/sleep/zsw010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dauvilliers Y, Barateau L. Narcolepsy and other central hypersomnias. Contin Minneap Minn. 2017;23(4):989‐1004. 10.1212/CON.0000000000000492 [DOI] [PubMed] [Google Scholar]
- 19.Zeman A, Britton T, Douglas N, et al. Narcolepsy and excessive daytime sleepiness. BMJ. 2004;329(7468):724‐728. 10.1136/bmj.329.7468.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vernet C, Arnulf I. Narcolepsy with long sleep time: a specific entity? Sleep. 2009;32(9):1229‐1235. 10.1093/sleep/32.9.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anic‐Labat S, Guilleminault C, Kraemer HC, Meehan J, Arrigoni J, Mignot E. Validation of a cataplexy questionnaire in 983 sleep‐disorders patients. Sleep. 1999;22(1):77‐87. [PubMed] [Google Scholar]
- 22.Peraita‐Adrados R, del Rio‐Villegas R, Vela‐Bueno A. Environmental factors in the development of narcolepsy with cataplexy. A case‐control study. Rev Neurol. 2015;60(12):529‐534. [PubMed] [Google Scholar]
- 23.Rocca FL, Pizza F, Ricci E, Plazzi G. Narcolepsy during childhood: an update. Neuropediatrics. 2015;46(3):181‐198. 10.1055/s-0035-1550152. [DOI] [PubMed] [Google Scholar]
- 24.Plazzi G, Pizza F, Palaia V, et al. Complex movement disorders at disease onset in childhood narcolepsy with cataplexy. Brain J Neurol. 2011;134(Pt 12):3477‐3489. 10.1093/brain/awr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fortuyn HAD, Lappenschaar GA, Nienhuis FJ, et al. Psychotic symptoms in narcolepsy: phenomenology and a comparison with schizophrenia. Gen Hosp Psychiatry. 2009;31(2):146‐154. 10.1016/j.genhosppsych.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Douglass AB, Shipley JE, Haines RF, Scholten RC, Dudley E, Tapp A. Schizophrenia, narcolepsy, and HLA‐DR15, DQ6. Biol Psychiatry. 1993;34(11):773‐780. [DOI] [PubMed] [Google Scholar]
- 27.Kishi Y, Konishi S, Koizumi S, Kudo Y, Kurosawa H, Kathol RG. Schizophrenia and narcolepsy: a review with a case report. Psychiatry Clin Neurosci. 2004;58(2):117‐124. [DOI] [PubMed] [Google Scholar]
- 28.Ullman KC. Narcolepsy and schizophrenia. Am J Psychiatry. 1977;134(7):822. 10.1176/ajp.134.7.822b. [DOI] [PubMed] [Google Scholar]
- 29.Douglass AB. Narcolepsy: differential diagnosis or etiology in some cases of bipolar disorder and schizophrenia? CNS Spectr. 2003;8(2):120‐126. [DOI] [PubMed] [Google Scholar]
- 30.Cavalier Y, Kothare SV. The association of schizophrenia and narcolepsy in adolescents. Pediatr Neurol. 2018;83:56‐57. 10.1016/j.pediatrneurol.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Huang Y‐S, Guilleminault C, Chen C‐H, Lai P‐C, Hwang F‐M. Narcolepsy‐cataplexy and schizophrenia in adolescents. Sleep Med. 2014;15(1):15‐22. 10.1016/j.sleep.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Sansa G, Gavaldà A, Gaig C, et al. Exploring the presence of narcolepsy in patients with schizophrenia. BMC Psychiatry. 2016;16:177. 10.1186/s12888-016-0859-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coren HZ, Strain JJ. A case of narcolepsy with psychosis (paranoid state of narcolepsy). Compr Psychiatry. 1965;6:191‐199. [DOI] [PubMed] [Google Scholar]
- 34.Benca RM. Narcolepsy and excessive daytime sleepiness: diagnostic considerations, epidemiology, and comorbidities. J Clin Psychiatry. 2007;68(Suppl 13):5‐8. [PubMed] [Google Scholar]
- 35.Dahmen N, Kasten M, Mittag K, Müller MJ. Narcoleptic and schizophrenic hallucinations. Implications for differential diagnosis and pathophysiology. Eur J Health Econ HEPAC Health Econ Prev Care. 2002;3(Suppl 2):S94‐98. 10.1007/s10198-002-0113-x. [DOI] [PubMed] [Google Scholar]
- 36.Walterfang M, Upjohn E, Velakoulis D. Is schizophrenia associated with narcolepsy? Cogn Behav Neurol Off J Soc Behav Cogn Neurol. 2005;18(2):113‐118. [DOI] [PubMed] [Google Scholar]
- 37.Wamsley E, Donjacour CEHM, Scammell TE, Lammers GJ, Stickgold R. Delusional confusion of dreaming and reality in narcolepsy. Sleep. 2014;37(2):419‐422. 10.5665/sleep.3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Douglass AB, Hays P, Pazderka F, Russell JM. Florid refractory schizophrenias that turn out to be treatable variants of HLA‐associated narcolepsy. J Nerv Ment Dis. 1991;179(1):12‐17.discussion 18. [DOI] [PubMed] [Google Scholar]
- 39.Bhat SK, Galang R. Narcolepsy presenting as schizophrenia. Am J Psychiatry. 2002;159(7):1245. 10.1176/appi.ajp.159.7.1245. [DOI] [PubMed] [Google Scholar]
- 40.Hays P. False but sincere accusations of sexual assault made by narcoleptic [correction of narcotic] patients. Med Leg J. 1992;60(Pt 4):265‐271. 10.1177/002581729206000405. [DOI] [PubMed] [Google Scholar]
- 41.Szucs A, Janszky J, Holló A, Migléczi G, Halász P. Misleading hallucinations in unrecognized narcolepsy. Acta Psychiatr Scand. 2003;108(4):314‐316; dicussion 316–317. [DOI] [PubMed] [Google Scholar]
- 42.Hood B, Bruck D. Metamemory in narcolepsy. J Sleep Res. 1997;6(3):205‐210. [DOI] [PubMed] [Google Scholar]
- 43.Rogers AE, Rosenberg RS. Tests of memory in narcoleptics. Sleep. 1990;13(1):42‐52. [PubMed] [Google Scholar]
- 44.Aguirre M, Broughton R, Stuss D. Does memory impairment exist in narcolepsy‐cataplexy? J Clin Exp Neuropsychol. 1985;7(1):14‐24. 10.1080/01688638508401239. [DOI] [PubMed] [Google Scholar]
- 45.Postiglione E, Antelmi E, Pizza F, Lecendreux M, Dauvilliers Y, Plazzi G. The clinical spectrum of childhood narcolepsy. Sleep Med Rev. 2018;38:70‐85. 10.1016/j.smrv.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 46.Wilcox J. Psychopathology and narcolepsy. Neuropsychobiology. 1985;14(4):170‐172. 10.1159/000118223. [DOI] [PubMed] [Google Scholar]
- 47.Dauvilliers Y, Gaig C, Barateau L, et al. Absence of NMDA receptor antibodies in the rare association between Type 1 Narcolepsy and Psychosis. Sci Rep. 2016;6:25230. 10.1038/srep25230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Szakács A, Hallböök T, Tideman P, Darin N, Wentz E. Psychiatric comorbidity and cognitive profile in children with narcolepsy with or without association to the H1N1 influenza vaccination. Sleep. 2015;38(4):615‐621. 10.5665/sleep.4582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deutch AY, Bubser M. The orexins/hypocretins and schizophrenia. Schizophr Bull. 2007;33(6):1277‐1283. 10.1093/schbul/sbm096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saucerman SA. Dissociation of W/REM/NREM states may cause psychotic symptoms. Schizophr Res. 1997;25(3):261‐263. [DOI] [PubMed] [Google Scholar]
- 51.Müller N. Inflammation in Schizophrenia: pathogenetic aspects and therapeutic considerations. Schizophr Bull. 2018;44(5):973‐982. 10.1093/schbul/sby024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grosskopf A, Müller N, Malo A, Wank R. Potential role for the narcolepsy‐ and multiple sclerosis‐associated HLA allele DQB1*0602 in schizophrenia subtypes. Schizophr Res. 1998;30(2):187‐189. [DOI] [PubMed] [Google Scholar]
- 53.Sekar A, Bialas AR, de Rivera H, et al. Schizophrenia risk from complex variation of complement component 4. Nature. 2016;530(7589):177‐183. 10.1038/nature16549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tsutsui K, Kanbayashi T, Tanaka K, et al. Anti‐NMDA‐receptor antibody detected in encephalitis, schizophrenia, and narcolepsy with psychotic features. BMC Psychiatry. 2012;12:37. 10.1186/1471-244X-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pizza F, Magnani M, Indrio C, Plazzi G. The hypocretin system and psychiatric disorders. Curr Psychiatry Rep. 2014;16(2):433. 10.1007/s11920-013-0433-9. [DOI] [PubMed] [Google Scholar]
- 56.Spensley J, Rockwell DA. Psychosis during methylphenidate abuse. N Engl J Med. 1972;286(16):880‐881. 10.1056/NEJM197204202861607. [DOI] [PubMed] [Google Scholar]
- 57.Pawluk LK, Hurwitz TD, Schluter JL, Ullevig C, Mahowald MW. Psychiatric morbidity in narcoleptics on chronic high dose methylphenidate therapy. J Nerv Ment Dis. 1995;183(1):45‐48. [DOI] [PubMed] [Google Scholar]
- 58.Mitler MM, Hajdukovic R, Erman MK. Treatment of narcolepsy with methamphetamine. Sleep. 1993;16(4):306‐317. [PMC free article] [PubMed] [Google Scholar]
- 59.Honda Y. Experience of long‐term treatment of narcolepsy with psychostimulants: effectiveness and problems. Annual Report of the Pharmacopsychiatry Research foundation [Japanese Language]. 1997;28:54‐59. [Google Scholar]
- 60.Honda YA. 10–40 Year Follow‐Up Study of Narcolepsy. In: Meier‐Ewert K, Okawa M, ed. Sleep—Wake Disorders. Boston, MA: Springer US; 1997: 105‐114. 10.1007/978-1-4899-0245-0_11 [DOI] [Google Scholar]
- 61.Auger RR, Goodman SH, Silber MH, Krahn LE, Pankratz VS, Slocumb NL. Risks of high‐dose stimulants in the treatment of disorders of excessive somnolence: a case‐control study. Sleep. 2005;28(6):667‐672. [DOI] [PubMed] [Google Scholar]
- 62.Volkow ND, Fowler JS, Logan J, et al. Effects of modafinil on dopamine and dopamine transporters in the male human brain: clinical implications. JAMA. 2009;301(11):1148‐1154. 10.1001/jama.2009.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wisor JP, Eriksson KS. Dopaminergic‐adrenergic interactions in the wake promoting mechanism of modafinil. Neuroscience. 2005;132(4):1027‐1034. 10.1016/j.neuroscience.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 64.Besset A, Chetrit M, Carlander B, Billiard M. Use of modafinil in the treatment of narcolepsy: a long term follow‐up study. Neurophysiol Clin Clin Neurophysiol. 1996;26(1):60‐66. 10.1016/0987-7053(96)81535-8. [DOI] [PubMed] [Google Scholar]
- 65.Schwartz JRL, Feldman NT, Fry JM, Harsh J. Efficacy and safety of modafinil for improving daytime wakefulness in patients treated previously with psychostimulants. Sleep Med. 2003;4(1):43‐49. 10.1016/s1389-9457(02)00240-x. [DOI] [PubMed] [Google Scholar]
- 66.Golicki D, Bala MM, Niewada M, Wierzbicka A. Modafinil for narcolepsy: systematic review and meta‐analysis. Med Sci Monit Int Med J Exp. Clin Res. 2010;16(8):RA177‐186. [PubMed] [Google Scholar]
- 67.Narendran R, Young CM, Valenti AM, Nickolova MK, Pristach CA. Is psychosis exacerbated by modafinil? Arch Gen Psychiatry. 2002;59(3):292‐293. [DOI] [PubMed] [Google Scholar]
- 68.Ivanenko A, Tauman R, Gozal D. Modafinil in the treatment of excessive daytime sleepiness in children. Sleep Med. 2003;4(6):579‐582. [DOI] [PubMed] [Google Scholar]
- 69.Becker PM, Schwartz JRL, Feldman NT, Hughes RJ. Effect of modafinil on fatigue, mood, and health‐related quality of life in patients with narcolepsy. Psychopharmacology. 2004;171(2):133‐139. 10.1007/s00213-003-1508-9. [DOI] [PubMed] [Google Scholar]
- 70.Kumar R. Approved and investigational uses of modafinil: an evidence‐based review. Drugs. 2008;68(13):1803‐1839. 10.2165/00003495-200868130-00003. [DOI] [PubMed] [Google Scholar]
- 71.Leong GB, Shaner AL, Silva JA. Narcolepsy, paranoid psychosis, and analeptic abuse. Psychiatr J Univ Ott Rev Psychiatr Univ Ott. 1989;14(3):481‐483. [PubMed] [Google Scholar]
- 72.Vorspan F, Warot D, Consoli A, Cohen D, Mazet P. Mania in a boy treated with modafinil for narcolepsy. Am J Psychiatry. 2005;162(4):813‐814. 10.1176/appi.ajp.162.4.813-a. [DOI] [PubMed] [Google Scholar]
- 73.Crosby MI, Bradshaw DA, McLay RN. Severe mania complicating treatment of narcolepsy with cataplexy. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2011;7(2):214‐216. [PMC free article] [PubMed] [Google Scholar]
- 74.Kondziella D, Arlien‐Soborg P. Diagnostic and therapeutic challenges in narcolepsy‐related psychosis. J Clin Psychiatry. 2006;67(11):1817‐1819. [DOI] [PubMed] [Google Scholar]
- 75.Davies M, Wilton L, Shakir S. Safety profile of modafinil across a range of prescribing indications, including off‐label use, in a primary care setting in England: results of a modified prescription‐event monitoring study. Drug Saf. 2013;36(4):237‐246. 10.1007/s40264-013-0025-y. [DOI] [PubMed] [Google Scholar]
- 76.Andrade C, Kisely S, Monteiro I, Rao S. Antipsychotic augmentation with modafinil or armodafinil for negative symptoms of schizophrenia: systematic review and meta‐analysis of randomized controlled trials. J Psychiatr Res. 2015;60:14‐21. 10.1016/j.jpsychires.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 77.Tarabar AF, Nelson LS. The gamma‐hydroxybutyrate withdrawal syndrome. Toxicol Rev. 2004;23(1):45‐49. [DOI] [PubMed] [Google Scholar]
- 78.Huang Y‐S, Guilleminault C. Narcolepsy: action of two gamma‐aminobutyric acid type B agonists, baclofen and sodium oxybate. Pediatr Neurol. 2009;41(1):9‐16. 10.1016/j.pediatrneurol.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 79.Mayer G, Plazzi G, Iranzo Á, et al. Long‐term compliance, safety, and tolerability of sodium oxybate treatment in patients with narcolepsy type 1: a postauthorization, noninterventional surveillance study. Sleep. 2018;41(9): 10.1093/sleep/zsy128. [DOI] [PubMed] [Google Scholar]
- 80.Murali H, Kotagal S. Off‐label treatment of severe childhood narcolepsy‐cataplexy with sodium oxybate. Sleep. 2006;29(8):1025‐1029. 10.1093/sleep/29.8.1025. [DOI] [PubMed] [Google Scholar]
- 81.Lecendreux M, Poli F, Oudiette D, et al. Tolerance and efficacy of sodium oxybate in childhood narcolepsy with cataplexy: a retrospective study. Sleep. 2012;35(5):709‐711. 10.5665/sleep.1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mamelak M, Swick T, Emsellem H, Montplaisir J, Lai C, Black J. A 12‐week open‐label, multicenter study evaluating the safety and patient‐reported efficacy of sodium oxybate in patients with narcolepsy and cataplexy. Sleep Med. 2015;16(1):52‐58. 10.1016/j.sleep.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 83.Moresco M, Pizza F, Antelmi E, Plazzi G. Sodium oxybate treatment in pediatric type 1 narcolepsy. Curr Drug Metab. 2018;19(13):1073‐1079. 10.2174/1389200219666180305153134. [DOI] [PubMed] [Google Scholar]
- 84.Sarkanen T, Niemelä V, Landtblom A‐M, Partinen M. Psychosis in patients with narcolepsy as an adverse effect of sodium oxybate. Front Neurol. 2014;5:136. 10.3389/fneur.2014.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Langford J, Gross WL. Psychosis in the context of sodium oxybate therapy. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2011;7(6):665‐666. 10.5664/jcsm.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chien J, Ostermann G, Turkel SB. Sodium oxybate‐induced psychosis and suicide attempt in an 18‐year‐old girl. J Child Adolesc Psychopharmacol. 2013;23(4):300‐301. 10.1089/cap.2012.0130. [DOI] [PubMed] [Google Scholar]
- 87.Drakatos P, Lykouras D, D’Ancona G, et al. Safety and efficacy of long‐term use of sodium oxybate for narcolepsy with cataplexy in routine clinical practice. Sleep Med. 2017;35:80‐84. 10.1016/j.sleep.2017.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Plazzi G, Ruoff C, Lecendreux M, et al. Treatment of paediatric narcolepsy with sodium oxybate: a double‐blind, placebo‐controlled, randomised‐withdrawal multicentre study and open‐label investigation. Lancet Child Adolesc Health. 2018;2(7):483‐494. 10.1016/S2352-4642(18)30133-0. [DOI] [PubMed] [Google Scholar]
- 89.Nittur N, Konofal E, Dauvilliers Y, et al. Mazindol in narcolepsy and idiopathic and symptomatic hypersomnia refractory to stimulants: a long‐term chart review. Sleep Med. 2013;14(1):30‐36. 10.1016/j.sleep.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 90.Parkes JD, Schachter M. Mazindol in the treatment of narcolepsy. Acta Neurol Scand. 1979;60(4):250‐254. 10.1111/j.1600-0404.1979.tb02976.x. [DOI] [PubMed] [Google Scholar]
- 91.Baumann CR. Wide implications of a trial on pitolisant for cataplexy. Lancet Neurol. 2017;16(3):173‐174. 10.1016/S1474-4422(16)30398-2. [DOI] [PubMed] [Google Scholar]
- 92.Kollb‐Sielecka M, Demolis P, Emmerich J, Markey G, Salmonson T, Haas M. The European Medicines Agency review of pitolisant for treatment of narcolepsy: summary of the scientific assessment by the Committee for Medicinal Products for Human Use. Sleep Med. 2017;33:125‐129. 10.1016/j.sleep.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 93.Dauvilliers Y, Bassetti C, Lammers GJ, et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double‐blind, randomised trial. Lancet Neurol. 2013;12(11):1068‐1075. 10.1016/S1474-4422(13)70225-4. [DOI] [PubMed] [Google Scholar]
- 94.Dauvilliers Y, Arnulf I, Szakacs A, et al. Long‐term use of pitolisant to treat patients with narcolepsy: Harmony III Study. Sleep. 2019;42(11): 10.1093/sleep/zsz174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Szakacs Z, Dauvilliers Y, Mikhaylov V, et al. Safety and efficacy of pitolisant on cataplexy in patients with narcolepsy: a randomised, double‐blind, placebo‐controlled trial. Lancet Neurol. 2017;16(3):200‐207. 10.1016/S1474-4422(16)30333-7. [DOI] [PubMed] [Google Scholar]
- 96.Wang Y‐Q, Li R, Zhang M‐Q, Zhang Z, Qu W‐M, Huang Z‐L. The neurobiological mechanisms and treatments of REM sleep disturbances in depression. Curr Neuropharmacol. 2015;13(4):543‐553. 10.2174/1570159x13666150310002540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Abad VC, Guilleminault C. New developments in the management of narcolepsy. Nat Sci Sleep. 2017;9:39‐57. 10.2147/NSS.S103467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Møller LR, Østergaard JR. Treatment with venlafaxine in six cases of children with narcolepsy and with cataplexy and hypnagogic hallucinations. J Child Adolesc Psychopharmacol. 2009;19(2):197‐201. 10.1089/cap.2008.036. [DOI] [PubMed] [Google Scholar]
- 99.Lopez R, Arnulf I, Drouot X, Lecendreux M, Dauvilliers Y. Consensus. Prise en charge thérapeutique des patients hypersomniaques: quelle stratégie ? Médecine Sommeil. 2017;14(3):138‐150. 10.1016/j.msom.2017.07.005. [DOI] [Google Scholar]
- 100.Morgenthaler TI, Kapur VK, Brown T, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1705‐1711. 10.1093/sleep/30.12.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Melamed Y, Daliahu Y, Paleacu D. Narcolepsy and psychotic states–a case report. Isr J Psychiatry Relat Sci. 2009;46(1):70‐73. [PubMed] [Google Scholar]
- 102.Undurraga J, Garrido J, Santamaría J, Parellada E. Treatment of narcolepsy complicated by psychotic symptoms. Psychosomatics. 2009;50(4):427‐428. 10.1176/appi.psy.50.4.427. [DOI] [PubMed] [Google Scholar]
- 103.Canellas‐Dols F, Delgado C, Arango‐Lopez C, Peraita‐Adrados R. Narcolepsy‐cataplexy and psychosis: a case study. Rev Neurol. 2017;65(2):70‐74. [PubMed] [Google Scholar]
- 104.Chen M‐H, Bai Y‐M, Chen Y‐S, Huang K‐L, Hsu J‐W, Su T‐P. Comorbidity of narcolepsy and schizophrenia in an adolescent patient. J Chin Med Assoc JCMA. 2014;77(11):598‐600. 10.1016/j.jcma.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 105.Mohammadi S, Mayeli M, Saghazadeh A, Rezaei N. Cytokines in narcolepsy: A systematic review and meta‐analysis. Cytokine. 2020;131:155103. 10.1016/j.cyto.2020.155103. [DOI] [PubMed] [Google Scholar]
- 106.Prihodova I, Dudova I, Mohaplova M, Hrdlicka M, Nevsimalova S. Childhood narcolepsy and autism spectrum disorders: four case reports. Sleep Med. 2018;51:167‐170. 10.1016/j.sleep.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 107.Dorris L, Zuberi SM, Scott N, Moffat C, McArthur I. Psychosocial and intellectual functioning in childhood narcolepsy. Dev Neurorehabilitation. 2008;11(3):187‐194. 10.1080/17518420802011493. [DOI] [PubMed] [Google Scholar]
- 108.Lecendreux M, Lavault S, Lopez R, et al. Attention‐Deficit/Hyperactivity Disorder (ADHD) symptoms in pediatric narcolepsy: a cross‐sectional study. Sleep. 2015;38(8):1285‐1295. 10.5665/sleep.4910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Posar A, Pizza F, Parmeggiani A, Plazzi G. Neuropsychological findings in childhood narcolepsy. J Child Neurol. 2014;29(10):1370‐1376. 10.1177/0883073813508315. [DOI] [PubMed] [Google Scholar]
- 110.Rocca FL, Finotti E, Pizza F, et al. Psychosocial profile and quality of life in children with type 1 narcolepsy: a case‐control study. Sleep. 2016;39(7):1389‐1398. 10.5665/sleep.5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Stores G, Montgomery P, Wiggs L. The psychosocial problems of children with narcolepsy and those with excessive daytime sleepiness of uncertain origin. Pediatrics. 2006;118(4):e1116‐1123. 10.1542/peds.2006-0647. [DOI] [PubMed] [Google Scholar]
- 112.Park YK, Kwon O‐H, Joo EY, et al. White matter alterations in narcolepsy patients with cataplexy: tract‐based spatial statistics. J Sleep Res. 2016;25(2):181‐189. 10.1111/jsr.12366. [DOI] [PubMed] [Google Scholar]
- 113.Dalal MA, Schuld A, Pollmächer T. Lower CSF orexin A (hypocretin‐1) levels in patients with schizophrenia treated with haloperidol compared to unmedicated subjects. Mol Psychiatry. 2003;8(10):836‐837. 10.1038/sj.mp.4001363. [DOI] [PubMed] [Google Scholar]
- 114.Nishino S, Ripley B, Mignot E, Benson KL, Zarcone VP. CSF hypocretin‐1 levels in schizophrenics and controls: relationship to sleep architecture. Psychiatry Res. 2002;110(1):1‐7. 10.1016/s0165-1781(02)00032-x. [DOI] [PubMed] [Google Scholar]
- 115.Bernard‐Valnet R, Yshii L, Quériault C, et al. CD8 T cell‐mediated killing of orexinergic neurons induces a narcolepsy‐like phenotype in mice. Proc Natl Acad Sci U S A. 2016;113(39):10956‐10961. 10.1073/pnas.1603325113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ordóñez AE, Luscher ZI, Gogtay N. Neuroimaging findings from childhood onset schizophrenia patients and their non‐psychotic siblings. Schizophr Res. 2016;173(3):124‐131. 10.1016/j.schres.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tondelli M, Pizza F, Vaudano AE, Plazzi G, Meletti S. Cortical and subcortical brain changes in children and adolescents with narcolepsy type 1. Sleep. 2018;41(2): 10.1093/sleep/zsx192. [DOI] [PubMed] [Google Scholar]
- 118.Marshall CR, Howrigan DP, Merico D, et al. Contribution of copy number variants to schizophrenia from a genome‐wide study of 41,321 subjects. Nat Genet. 2017;49(1):27‐35. 10.1038/ng.3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Schizophrenia Working Group of the Psychiatric Genomics Consortium . Biological insights from 108 schizophrenia‐associated genetic loci. Nature. 2014;511(7510):421‐427. 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jaaro‐Peled H, Sawa A. Neurodevelopmental Factors in Schizophrenia. Psychiatr Clin North Am. 2020;43(2):263‐274. 10.1016/j.psc.2020.02.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


