Abstract
Aims and objectives
To compare the washing without water method with the water and soap method regarding comfort perceptions of the bed bath.
Background
Bathing affects nurses’ and care recipients’ comfort. Bedridden care recipients can be bathed in bed with water and soap or with washing without water products. Little is known about the differences between these two bed bath methods regarding comfort perceptions among care recipients and nurses.
Design
Crossover randomised laboratory‐controlled trial, conducted from March 2018–November 2019, according to the CONSORT guidelines.
Methods
Nursing students were randomly allocated roles as a patient (who received both types of bed baths) or a nurse (who provided both types of bed baths). Also, the order in which the bed baths were received/provided was randomised. A total of 97 students were included in the analysis. Student patients filled out the Patient Evaluation of Emotional Comfort Experienced (PEECE) scale to measure emotional comfort and a single‐item question on physical comfort after each bed bath. Student nurses filled out the Physical Demands scale after each bed bath to measure their physical comfort perceptions.
Results
No differences were found between the two bed bathing methods regarding student patients’ emotional or physical comfort levels. Among student nurses, the washing without water method was less physically demanding than the water and soap method.
Conclusions
Taking into account time‐efficiency and physical comfort for nurses, washing without water seems to be a valuable alternative to water and soap from a care recipient comfort perspective, which should be assessed in a clinical setting in future research.
Relevance to clinical practice
The washing without water method is less physically demanding for nurses and takes less time. It does not have a detrimental effect on care recipients’ emotional and physical comfort. The trial is registered at www.trialregister.nl (ID = NL6787).
Keywords: bed bath, comfort, crossover randomised trial, essentials of care, multi‐actor perspective, nursing education, physical demands, time effectiveness, washing without water, water and soap
Impact statement.
What does this paper contribute to the wider global clinical community?
Bathing is an important yet often undervalued essential of nursing care, which can be performed with water and soap or by disposable washing without water products for bedridden care recipients.
The study results show that washing without water seems to be a suitable and valuable replacement for the bed bath with water and soap in terms of comfort perceptions.
Washing without water is less physically demanding for nurses and less time consuming. It could free up time for nurses to spend on other care activities with care recipients.
1. INTRODUCTION
Bathing and showering are important personal care activities that most of us are able to fulfil independently. However, when people age, independent bathing can rapidly become less self‐evident (Jagger et al., 2001). At least 15% of Europeans aged 65 or older have severe difficulties with bathing and showering (Eurostat, 2016). Within healthcare institutions, many care recipients require assistance in bathing from nursing staff; this particularly applies to immobile care recipients who often need to be bathed in bed due to cognitive and physical decline (Cohen‐Mansfield & Jensen, 2005).
Bathing is part of the essentials of care (Feo & Kitson, 2016), which embody nursing care activities that care recipients deem most vital for their well‐being (Zwakhalen et al., 2018). As an essential of care activity, bathing has a substantial impact on nurses and care recipients, as became evident in a qualitative study about experiences of the bed bath (Groven et al., 2020, unpublished). For many nurses, the daily morning activities consist for the most part of bathing care recipients. For care recipients, bathing is often one of the first activities of the day. Moreover, bathing contributes to care recipients’ well‐being by fulfilling hygiene and comfort needs (Jangland et al., 2018).
Nurses and nursing students often undervalue the impact of bathing on care recipients and perceive it as a routine nursing activity that does not require much skill (Feo & Kitson, 2016; Pipe et al., 2012). However, care recipients’ comfort is compromised if the bed bath is not provided properly (Parr et al., 2017). Comfort is a source of care recipients’ well‐being and is described as a holistic and multidimensional experience (Lorente et al., 2017; Malinowski & Stamler, 2002), including physical and emotional dimensions (Jangland et al., 2018; Williams & Irurita, 2004). Physical comfort is related to the relief of physical discomforts, including pain (Kolcaba, 1994). Emotional comfort relates to the experience of positive emotions (e.g. feeling valued and at ease) and the absence of negative emotions (e.g. feeling dependent) (Williams & Irurita, 2004).
One of the few interventions that aims to optimise bed bathing is washing without water. This intervention consists of prepacked products containing disposable nonwoven washcloth with a cleansing fluid that does not have to be rinsed (Schoonhoven et al., 2015). Evidence regarding washing without water with respect to comfort for care recipients and nurses is limited. To guide nursing practice, the current study explores differences between the traditional water and soap method and the washing without water method with respect to physical and emotional comfort among people bathed in bed, and physical comfort among people providing the bed bath. Consequently, this study adds to the limited scientific evidence on essentials of care (Richards et al., 2018), such as the bed bath (Downey & Lloyd, 2008).
2. BACKGROUND
For both care recipients and nurses, comfort in bathing is important. Because bathing is a substantial part of the morning routine, an uncomfortable bed bath could literarily mean a bad start to the day or shift. Unfortunately, many bedridden people perceive the bed bath to have a detrimental impact on their levels of physical and emotional comfort (Cohen‐Mansfield & Jensen, 2005; Lopes et al., 2012; Veje et al., 2019a). With respect to emotional comfort, bedridden care recipients can feel embarrassed and frustrated and might feel their body is violated during the bed bath (Downey & Lloyd, 2008; Morse et al., 1995). Consequently, feelings of dependency and a lack of dignity reduces bedridden care recipients’ level of emotional comfort (Johannesen et al., 2004). Physical comfort is particularly pressured when bedridden care recipients experience pain on movement (Downey & Lloyd, 2008), feel weak and tired or are cold (Rader et al., 2006). For nurses, the bed bath can be physically demanding and a source of physical complaint, which reduces their level of physical comfort (El‐Soussi & Asfour, 2016; Hoeffer et al., 2006).
The applied bed bath method can have an influence on bedridden care recipients’ levels of emotional and physical comfort and on nurses’ level of physical comfort. Traditionally, bedridden people are bathed in bed with water and soap. As an alternative, washing without water is increasingly used in health care, particularly in Europe (Schoonhoven et al., 2015; Veje et al., 2019b) and the US (Sturgeon et al., 2019). In a systematic review, washing without water has been shown to be at least as effective as water and soap with respect to hygiene, skin condition and bathing completeness (Groven et al., 2017). However, the results of this review also show that the number of studies on washing without water is low, especially with respect to users’ emotional and physical comfort perceptions.
Based on extant studies, one could expect that care recipients perceive washing without water to be at least as comfortable as water and soap bed baths. A majority of care recipients have been found to perceive washing without water as a valuable alternative (Sheppard & Brenner, 2000) or replacement to the water and soap method (Schoonhoven et al., 2015). Moreover, care recipients perceive washing without water products as soft, easy to use, fast and convenient (Sheppard & Brenner, 2000; Veje et al., 2019a). In addition, most nurses perceive washing without water to be comfortable for care recipients and think that care recipients are satisfied with this type of bed bath (Larson et al., 2004; Sheppard & Brenner, 2000). However, it is unknown how these results relate to care recipients’ actual physical and emotional comfort levels.
Also with respect to physical comfort levels among nurses providing the bed bath, not much evidence is given in existing studies. Nurses have been found to perceive the washing without water method as a convenient, easy to administer and valuable alternative to the water and soap method (Larson et al., 2004; Nøddeskou et al., 2015; Schoonhoven et al., 2015; Sheppard & Brenner, 2000). However, just like much is unknown about care recipients’ emotional and physical comfort perceptions, more evidence is also needed on nurses’ physical comfort perceptions.
Based on the available evidence, we state the following two hypotheses:
The washing without water method is equal to or more physically and emotionally comfortable for care recipients as compared to the water and soap method.
The washing without water method is equal to or more physically comfortable (less physically demanding) for nurses as compared to the water and soap method.
2.1. Purpose of the study
The aim of the current study was to compare the washing without water method with the water and soap method with respect to perceived physical and emotional comfort among people bathed in bed and with respect to perceived physical comfort among people providing the bed bath.
3. METHODS
3.1. Research design
A non‐blinded crossover laboratory design was used in which participants were randomly allocated to one of two arms, each with a different order of treatments, being the bed bath with washing without water and the bed bath with water and soap. A more detailed overview of the research design is provided in the protocol, which is available online (Groven et al., 2019). The study complies with the guidelines of the Consolidated Standards of Reporting Trials (CONSORT). The CONSORT 2010 checklist of information to include when reporting a randomised trial is included in File S1.
3.2. Setting and sample
To have maximum control over the course of the trial (e.g. participants’ adherence to the order of the bed baths and the correct use of bed bath materials) and to control for confounders (e.g. people providing the bed bath, communication during the bed bath, and location of the bed bath), a controlled environment was set up in a laboratory setting (Richards & Hamers, 2009; Wilson et al., 2010). The research population consisted of first year nursing students, which was deliberately chosen for practical and theoretical reasons. Practically, it was more feasible for nursing students to participate in our laboratory setting compared with real bedridden care recipients, who would also be difficult to randomly allocate to different bed bath methods. Theoretically, nursing students do not yet have much experience with the bed bath (neither as a care recipient, nor as a nurse) and therefore are less prejudiced about the different bed bath methods. Furthermore, nursing students are likely to be more homogenous compared with real care recipients who, for example, have varying physical and cognitive conditions which cannot be controlled.
Four different groups of first year nursing students (of at least 150 students each) from two bachelor schools of nursing were informed about the research through lectures, posts on the electronic learning environments, vlogs and personal communication by teachers. In total, approximately 750 students were informed about the research. All first year nursing students were eligible if they consented to bathe or be bathed by fellow students. Because the curriculum of first year nursing students includes bed bathing training and practicing the different types of bed baths contributes to their professional development, all participants obtained study points. Altogether, the four groups of students that consented to participate consisted of 120 nursing students, of which 111 nursing students were enrolled in the study (18 to 40 participants per group).
Nursing students that were enrolled (from now on called participants) were randomly allocated to the role of a patient (from now on called ‘student patients’) or to the role of a nurse (from now on called ‘student nurses’) and simulated bed baths in the teaching rooms of their nursing school that were equipped as nursing home rooms. Each student patient was coupled randomly to a student nurse. Furthermore, each couple was randomly assigned to one of the two arms of the trial. For all allocations, randomisation was applied with a computer‐generated randomisation table containing unique identifier numbers assigned to the participants, which concealed allocation for the first researcher. Each student patient/nurse received/provided one bed bath per day with a wash‐out period of one week between the two different bed baths as shown in Figure 1.
FIGURE 1.
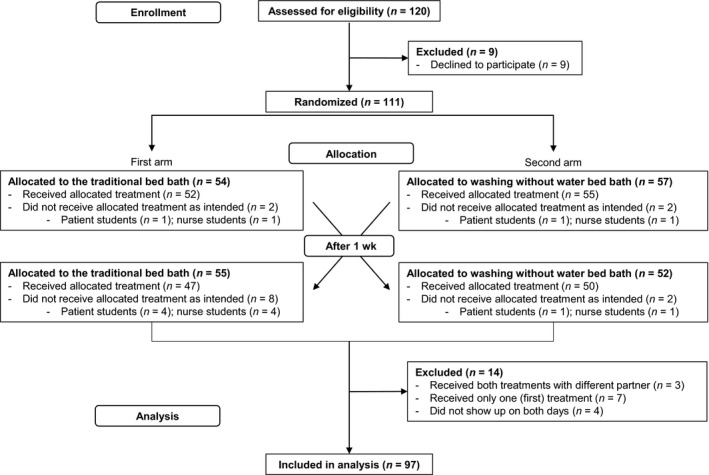
Consort diagram of the trial flow
To ensure that the bed baths were correctly executed, participants were instructed on both bed bath methods and only had materials at their disposal that were required for the type of bed bath they needed to receive or provide. Furthermore, both student patients and student nurses received a script before the start of the trial that described how to act within their role to standardise the execution of the bed baths and increase the realism of the experiment as much as possible. The script for student patients for example contained information about their physical condition and the constraints they had to imagine during the bed bath (e.g. that they had broken their leg and therefore could not turn independently). Furthermore, to control for interpersonal dynamics and communication during the bed baths that might affect participants’ comfort experiences of the bed baths, both student patients and student nurses were instructed to limit communication during the bed baths. Student nurses were only allowed to explain the different steps of the bed bath and to ask predetermined questions to student patients during the bed bath (e.g. ‘do you want me to apply deodorant or do you want to do that yourself?’). Student patients were informed about the required answers to student nurses’ questions (e.g. that they want to apply deodorant themselves). Although interpersonal dynamics and communication are important in bed baths provided in actual health care practice, these variables are controlled for in our experiment to assess the differences between the two bed bath methods.
3.3. Data collection
Data were collected between March 2018–November 2019 from the four groups of participants (recruited out of the four different groups of first year nursing students). The number of students that consented to participate was deemed sufficient to reach the required sample size of 104 participants based on a power calculation with an effect size of 0.5 on student patients’ emotional comfort, a type 1 error of 0.05 and 95% power. Before and after each bed bath, all participants filled out a questionnaire, which contained items and scales related to our primary and secondary outcomes.
3.3.1. Primary outcomes
Among student patients, the following primary outcomes were measured. First, emotional comfort during the bed bath among student patients was measured using the validated Patient Evaluation of Emotional Comfort Experienced (PEECE) scale for which Cronbach α values between 0.74–0.88 have been reported (Williams et al., 2017). The PEECE scale consists of 12 items, each related to a positive feeling, which needed to be answered on a 5‐point Likert scale, ranging from one (not at all experienced) to five (very much experienced) after each bed bath. The cumulative score (ranging from 12 to 60) was used for the analysis with a high score indicating a high level of emotional comfort during the bed bath. Second, to measure physical comfort among student patients, a single‐item question about the physical comfort of the bed bath had to be answered on a scale from 1 (very uncomfortable)–10 (very comfortable) after each bed bath.
Among student nurses, physical comfort was the primary outcome. To assess physical comfort, the validated 7‐item Physical Demands scale was completed after each bed bath. Previously reported Cronbach α coefficients between 0.87–0.91 indicate a high reliability of this scale (De Jonge et al., 1999; Verbeek, 2011). The items are related to physically demanding activities or postures and can be answered on a scale from 1 (not at all present during the bed bath)–5 (very much present during the bed bath). The cumulative score (ranging from 7 to 35) was used for the analysis with a low score (low physical demands) indicating a high level of physical comfort during the bed bath.
3.3.2. Secondary outcomes
Among the secondary outcomes were participants’ bed bath preferences after study completion. With respect to bed bath preferences, both student patients and student nurses were asked two questions: 1) which bed bathing method they preferred and 2) which bed bathing method they would choose for a (hypothetical) future trial. Furthermore, all participants were asked to grade each bed bath method on a scale from 1 (very bad)–10 (very good). In addition, the duration of the bed baths was measured by the research assistants who observed the bed baths. In addition to the secondary outcomes related to all participants, we asked student patients about the general importance of the bed bath from the patient perspective on a scale from 1 (not at all important)–10 (very important) both before and after the trial. Also, student nurses were asked the same questions about the general importance of the bed bath, but from the nurse perspective. Furthermore, student nurses were asked to fill out the PEECE scale and the single‐item physical comfort question on behalf of the student patient after each bed bath to measure student nurses’ perceptions of student patients’ emotional and physical comfort during the bed bath.
3.4. Data analysis
Statistical analysis was performed in IBM® SPSS® Statistics, version 25. Participants were excluded from the analysis if they did not undergo both bed baths and therefore missed one element of data collection. Two participants who were included in the analysis did not fill out all items of the scales measuring emotional comfort, for which the mean values of the total group of participants for the particular items were imputed (Tan et al., 2018). Afterwards, differences in baseline characteristics were assessed between the four groups of participants with respect to gender, age, length, weight, experience with the bed bath, bed bath method preferences and perceptions about the importance of the bed bath. Due to the limited amount of information about scale reliability in existing literature, reliability was assessed for the PEECE and the Physical Demands scales by calculating Cronbach's Alpha coefficients, which are reported in Appendix 1.
To detect possible differences between the two bed bath methods regarding our primary comfort outcomes, paired sample t tests were executed. Paired sample t tests were also performed for the secondary outcomes: grades assigned to the two bathing methods, duration of the bed bath, and emotional and physical comfort of the bed bath for student patients according to student nurses. Also, differences in perceived importance of the bed bath among student patients and student nurses before and after the trial were assessed by means of a paired sample t test. Bed bath method preferences were assessed by chi‐square goodness‐of‐fit tests, testing equal counts for the water and soap bed bath, washing without water or having no preference. Finally, additional linear mixed regression models were conducted in which the first level included the repeated measures and the second level the participants. These analyses allowed us to assess the effects of potential covariates on our continuous outcome variables. In a separate linear mixed regression, an interaction variable ‘method*order’ was included (i.e. method represents the type of bed bath received/provided, and order, whether the type of bed bath was received/provided first or second in the trial) to assess whether the effect of the bed bath method on our outcome variables depended on the order in which the two types of bed baths were received/provided.
Numbers and percentages are presented for categorical data. For continuous variables, means and standard deviations (SD) are presented. For all outcomes, p < .05 is considered as statistically significant. For every statistically significant result from the paired samples t test, the effect sizes have been determined by calculating Cohen's d using an online effect size calculator. Based on Cohen (1977), the effect size is considered to be small, medium or large at values equalling or exceeding 0.2, 0.5 and 0.8 respectively. Finally, 95% confidence intervals are reported.
3.5. Ethical approval
This study conforms to the Declaration of Helsinki, has been evaluated and waived for approval by a Dutch Medical Ethics Committee and is registered at www.trialregister.nl (ID = NL6787). Participants provided written consent before the start of the study.
4. RESULTS
4.1. Sample characteristics
Out of four different groups of first year nursing students, in total 120 nursing students gave initial consent. The four groups of participants were highly similar. Although in one of the groups, students had relatively more experience with providing a bed bath and had a relatively high preference for the washing without water method prior to the trial, these small differences did not affect the results. Out of the 120 participants, nine declined to participate before commencement of the trial. Therefore, eventually 111 nursing students were randomly allocated of which 14 participants were excluded from the analysis because they did not complete both of the bed baths that were part of the crossover trial. In total, 97 students completed both bed baths as intended and were included in the analysis.
Table 1 provides an overview of the sample's characteristics. The majority of the participants were female, had not been bed bathed before the trial, did have some experience in providing the bed bath and did not have a preference for a bed bathing method before the trial. Furthermore, participants perceived the bed bath as highly important (from the patient perspective) before the start of the trial.
TABLE 1.
Sample characteristics
| Variables | Total (n = 97) | Student patients (n = 48) | Student nurses (n = 49) |
|---|---|---|---|
| Treatment order | |||
| Water and soap bed bath first | 50 (52%) | 25 (52%) | 25 (51%) |
| Washing without water bed bath first | 47 (48%) | 23 (48%) | 24 (49%) |
| Gender | |||
| Female | 83 (86%) | 43 (90%) | 40 (82%) |
| Male | 14 (14%) | 5 (10%) | 9 (18%) |
| Age in years—mean (SD) | 19.2 (1.8) | 19 (2) | 19 (2) |
| Length in cm—mean (SD) | 171.1 (7.2) | 171 (6) | 172 (8) |
| Weight in kg—mean (SD) | 65.9 (13.2) | 65.4 (10.8) | 66.4 (15.3) |
| Has the student been bed bathed before? | |||
| Yes | 25 (26%) | 7 (15%) | 18 (37%) |
| No | 72 (74%) | 41 (85%) | 31 (63%) |
| Has the student provided a bed bath before? | |||
| Yes | 67 (69%) | 35 (73%) | 32 (65%) |
| No | 30 (31%) | 13 (27%) | 17 (35%) |
| Preference for bed bathing method | |||
| Water and soap bed bath | 28 (29%) | 15 (31%) | 13 (27%) |
| Washing without water bed bath | 14 (14%) | 3 (6%) | 11 (22%) |
| No preference | 55 (57%) | 30 (63%) | 25 (51%) |
| Perceived importance of the bed bath on a scale from 1–10—mean (SD) | 8.7 (1.2) | 8.7 (1.1) | 8.7 (1.3) |
4.2. Primary outcomes
Emotional and physical comfort of the bed bath was the primary outcomes related to people receiving a bed bath. No statistically significant difference was found between the water and soap method and the washing without water method in the emotional and physical comfort scores among student patients. For those providing the bed bath, only physical comfort was assessed by measuring how physically demanding the bed bath was perceived to be among student nurses. The cumulative physical demands score was statistically significantly lower (p = .001) for the washing without water method (M = 13.24) compared with the water and soap method (M = 14.76), which indicates slightly higher physical comfort levels for the washing without water method among student nurses. These results are presented in Table 2 and support our hypotheses.
TABLE 2.
Differences in comfort levels between water and soap bed bath and washing without water
| Variable | Bed bath method | Mean (SD) | p a | 95% CI | Effect size (Cohen's d) |
|---|---|---|---|---|---|
| Emotional comfort student patientsb (n = 48) | Water and soap bed bath | 45.90 (5.72) | .847 | [−1.89, 1.56] | ‐ |
| Washing without water | 46.06 (6.48) | ||||
| Physical comfort student patientsc (n = 48) | Water and soap bed bath | 7.54 (1.15) | .828 | [−0.34, 0.43] | ‐ |
| Washing without water | 7.50 (1.17) | ||||
| Physical demands student nursesd (n = 48) | Water and soap bed bath | 14.76 (3.65) | .001 | [0.67, 2.35] | Small (0.4) |
| Washing without water | 13.24 (3.86) |
Paired samples t test; bPossible range: 12–60; cPossible range: 1–10; dPossible range: 7–35.
Additional linear mixed model regressions showed that the order in which the two different bed baths were provided did not have an effect on our primary outcome variables. Furthermore, several covariates were included in the regressions analysis, which did not yield important confounding effects (File S2 for results).
4.3. Secondary outcomes
With respect to the secondary outcomes of this study, statistically significant differences between the two bed bath methods were found on two variables as shown in Table 3. First, student nurses gave a higher general grade (p = .005) to the washing without water method (M = 7.9) than to the water and soap method (M = 7.2). Second, a difference was found in bed bath duration (p < .001), with the washing without water method taking less time (M = 15 min) than the water and soap method (M = 24 min). No statistically significant difference between the two bed bath methods was found with respect to general grades given by student patients, nor with respect to emotional or physical comfort of the bed bath for student patients according to student nurses.
TABLE 3.
Results of continuous secondary outcomes
| Variable | Bed bath method | Mean (SD) | p a | 95% CI | Effect size (Cohen's d) |
|---|---|---|---|---|---|
| General grades given by student patients to bed bath methodb (n = 48) | Water and soap bed bath | 7.63 (1.21) | .308 | [−.24, .74] | ‐ |
| Washing without water | 7.38 (1.18) | ||||
| General grades given by student nurses to bed bath methodb (n = 49) | Water and soap bed bath | 7.18 (1.29) | .005 | [−1.13, −0.22] | Medium (0.54) |
| Washing without water | 7.86 (1.21) | ||||
| Emotional comfort for student patients according to student nursesc (n = 49) | Water and soap bed bath | 42.67 (5.70) | .592 | [−1.74, 1] | ‐ |
| Washing without water | 43.04 (5.65) | ||||
| Physical comfort for student patients according to student nursesb (n = 49) | Water and soap bed bath | 7.04 (1.19) | .05 | [−0.78, 0] | |
| Washing without water | 7.43 (1.17) | ||||
| Bed bath duration (n = 49) | Water and soap bed bath | 23.65 (5.27) | <.001 | [7.03, 10.15] | Large (1.88) |
| Washing without water | 15.06 (3.76) |
Paired samples t test; bPossible range: 1–10; cPossible range: 12–60.
With respect to preferences among student patients and student nurses, the results in Table 4 reveal that most student patients (48%) preferred the water and soap method (p = .028) when asked about their general preference. They did not have a statistically significant preference when asked how they wanted to be bathed in a (hypothetical) future trial. The majority of student nurses (63%) preferred the washing without water method (p < .001) and also chose this bed bath method (70%) when they were asked which bed bath they would choose if they had to provide a bed bath again in a future (hypothetical) trial (p < .001). Finally, with respect to the perceived importance of the bed bath, a statistically significant difference between the pre‐trial and post‐trial scores was only found among student patients (p = .03) as shown in Table 5. Student patients perceived the bed bath as slightly more important after the trial (M = 9.0) compared with their perception about its importance before the trial (M = 8.7).
TABLE 4.
Preferences among student patients and student nurses for bed bath methods
| Variable | Preference | n (%) | p a | Chi‐square (df) |
|---|---|---|---|---|
| Preference student patients (n = 48) | No preference | 8 (17%) | .028 | 7.13 (2) |
| Water and soap bed bath | 23 (48%) | |||
| Washing without water | 17 (35%) | |||
| Preference student nurses (n = 49) | No preference | 8 (16%) | <.001 | 19.88 (2) |
| Water and soap bed bath | 10 (21%) | |||
| Washing without water | 31 (63%) | |||
| Student patients’ bed bath of choice for future bed bath (n = 48) | No preference | 13 (27%) | .570 | 1.13 (2) |
| Water and soap bed bath | 19 (40%) | |||
| Washing without water | 16 (33%) | |||
| Student nurses’ bed bath of choice for future bed bath (n = 49) | No preference | 7 (14%) | <.001 | 28.69 (2) |
| Water and soap bed bath | 8 (16%) | |||
| Washing without water | 34 (70%) |
Chi‐square goodness‐of‐fit test assuming equal counts.
TABLE 5.
Differences in perceived importance of the bed bath before and after the trial
| Variable (secondary) | Before/after trial | Mean (SD) | p a | 95% CI | Effect size (Cohen's d) |
|---|---|---|---|---|---|
|
Perceived importance of the bed bath among student patientsb (n = 48) |
Before the trial | 8.67 (1.14) | .032 | [−0.72, −0.03] | Small (0.35) |
| After the trial | 9.04 (0.97) | ||||
| Perceived importance of the bed bath among student nursesb (n = 49) | Before the trial | 8.78 (0.90) | .471 | [−0.31, 0.14] | ‐ |
| After the trial | 8.86 (1.04) |
Paired samples t test; bPossible range: 1–10.
5. DISCUSSION
Our findings indicate that the washing without water method and the water and soap method do not differ in terms of perceived emotional and physical comfort for the person being bathed in bed. A small but statistically significant difference in favour of washing without water was found in perceived physical demands for nurses providing the bed bath. Furthermore, a large difference was found in the duration of the bed bath, which was 36% shorter for the washing without water method. In addition to emotional and physical comfort, our crossover design made it possible to assess participants’ preferences for bed bath methods (i.e. all participants experienced both bed baths), which might relate to perceived comfort levels. Especially among participants that provided the bed baths, a strong preference was detected for the washing without water method, while participants that were bathed slightly preferred water and soap.
Previous studies have reported care recipients’ perceptions about the washing without water concept being soft and convenient (Sheppard & Brenner, 2000; Veje et al., 2019a), which is positively related to physical comfort. However, our results indicate that there is no difference in physical (nor emotional) comfort between the bed bathing methods for people being bathed. Furthermore, while Schoonhoven et al. (2015) reported that most care recipients within a nursing home setting would replace water and soap with washing without water, our results show a slight preference for the water and soap method among people being bathed. A possible explanation for this finding might be offered by Veje et al. (2019a) who reported a preference for the water and soap method among care recipients who believed it to be more effective in cleaning the skin. Although scientific evidence shows that both methods are equally effective in removing micro‐organisms from the skin (Larson et al., 2004; Veje et al., 2019b), this trial's participants might also perceive washing without water as less hygienically effective. Such perceptions might have affected the preferences of the nursing students who participated in this trial as it will be their future responsibility to meet care recipients’ hygiene needs.
Our results with respect to users’ preferences and perceived physical demand levels are in line with previous research that reported nurses’ preferences for the washing without water method for convenience, among other reasons (Larson et al., 2004; Nøddeskou et al., 2015; Sheppard & Brenner, 2000) related to physical comfort. Also the users in our study mainly preferred the washing without water method and perceived this bed bath as less physically demanding than the water and soap method. Probably, these results are partly explained by the big difference in bed bath duration between the two bed bath methods. We found that the average duration of the bed bath with the washing without water method accounted for less than two‐thirds of the duration of a bed bath with water and soap, which is in line with previous research (Nøddeskou et al., 2015, 2018).
Overall, evidence on washing without water indicates that this bed bath method outperforms or equals the water and soap method with respect to hygiene, skin condition and bathing completeness, among other areas (Groven et al., 2017). The bed bath method should be selected according to care recipients’ preferences but our results indicate that washing without water could especially be valuable for certain groups of care recipients. Washing without water seems highly suitable for patients that would benefit from shorter bed baths, such as people suffering from COPD or people receiving palliative care. Furthermore, people with dementia that show resistance during the bed bath (e.g. because they are afraid of water) could experience more physical and emotional comfort when bathed using the washing without water method (Cohen‐Mansfield & Jensen, 2005). For nurses, bathing people with dementia can be a struggle (Conroy, 2017), which also makes washing without water a valuable alternative for them because it takes less time and physical effort. In addition, washing without water can be valuable for healthcare institutions, especially in times of crises, such as the COVID‐19 pandemic, when the need for hygienic and comfortable personal care is high but time is limited. Also when time constraints are less pressing, washing without water could free up time for nurses to spend on other care activities with care recipients. Furthermore, as the technical execution of the bed bath takes less time with the washing without water method, nurses could spend more time and attention on the interpersonal aspects of the bed bath (e.g. communication with the patient), which we controlled for in our study but can be essential for a comfortable bed bath.
Apart from our results with respect to the bed bath methods, a somewhat remarkable finding can be reported regarding the bed bath in general. Although bathing is reported to be commonly undervalued among nurses and nursing students (Meehan et al., 2018), the nursing students that participated in our study assigned high grades to its importance. This might be explained by an above‐average interest among this study's participants compared with the much bigger group of nursing students that declined to participate.
Less than 20% of nursing students were willing to participate in the trial. Possibly, being accustomed to the use of mannequins in practicing healthcare activities (Wolf, 1997) increases students’ emotional distress when they personally have to experience the bed bath (Gul & Ali, 2010). The common practice of using mannequins could not only have negatively influenced students’ willingness to participate in the trial, but in general also deprives students of the possibility to personally experience what it means to be bathed. Therefore, we would like to encourage nursing educators to reintroduce the practice of essential care activities, such as the bed bath, on fellow students. In doing so, we would like to stress the importance of interpersonal factors, such as communication (Conroy, 2017), with respect to how the bed bath (method) is experienced. In our trial, the person providing the bed bath and communication during the bed bath were potential confounders, which we controlled for by making fixed student couples and by instructing participants to confine communication during the bed baths. However, in actual healthcare settings, these interpersonal factors influence healthcare actors’ experiences, including comfort perceptions (Conroy, 2017; Miranda et al., 2017). Therefore, nursing educators should also pay attention to such factors to offer valuable learning experiences to students. If students obtain personal and more realistic experience with the bed bath, they will likely possess more knowledge and confidence (El‐Soussi & Asfour, 2016; Lopes et al., 2019) and struggle less in properly carrying out bed baths on real patients (Feo & Kitson, 2016; Feo et al., 2018; Zwakhalen et al., 2018). Moreover, practicing on real people and personally experiencing the bed bath as a patient adds to students’ understanding about the importance of this essential care activity.
Bathing people (i.e. instead of mannequins) in different ways also supports students to form better informed judgements with respect to bathing interventions, such as washing without water. Generally, there is a lack of evidence on essential care interventions that could support nurses to deliver optimal care (Zwakhalen et al., 2018). Our study contributes to the limited scientific evidence on bathing, which hopefully supports the re‐evaluation of its importance. Moreover, our results add to the evidence base regarding washing without water and justify its use in healthcare practice from a comfort perspective.
5.1. Limitations and recommendations for future research
To our knowledge, our study is the first to assess differences between the water and soap method and the washing without water method with respect to comfort, which is one of the foremost goals of bed bathing (Veje et al., 2019a). Although this study has been carried out carefully, some limitations need to be mentioned that should be taken into account in future research.
Three limitations are related to our sample. First, 93% of the calculated sample size was reached, which was partly due to the study design. Only participants that completed both treatments were included in the analysis. Because couples of students were created, this meant that both students had to be excluded from the analyses if one of the two did not show up on the second day of the trial. However, the attrition rate in our study (13%) was below 20%, which is argued to be the level at which bias in the results can be expected (Gul & Ali, 2010). Still, our study might be underpowered, especially because participants were eventually recruited from four clusters of nursing students of two nursing schools, which was needed due to the low participation rate. The low participation rate implies a second limitation as it could have caused participation bias because the participating students might have different perceptions about the bed bath compared with the students who declined to participate in the trial. Third, while this study's laboratory setting is suitable for having a first check on causality and, therefore, has a positive effect on the internal validity of our findings (Hooghe et al., 2010; Wilson et al., 2010), the chosen setting and study subjects (i.e. nursing students) have implications for our findings’ external validity. Students differ in many ways from actual bedridden care recipients and form a much more homogenous group (Andersen et al., 2010). Furthermore, because interpersonal factors (e.g. communication) that could influence comfort experiences were controlled for in the current trial, our results related to student patients’ comfort perceptions and preferences should cautiously be generalised to actual bedridden care recipients. Therefore, future research should assess comfort perceptions in real‐life healthcare settings with actual bedridden care recipients, such as nursing home residents or hospital patients (Andersen et al., 2010), taking into account interpersonal factors.
Yet, our results with respect to student nurses’ perceptions and preferences can be generalised to actual nurses providing real bed baths. Wilson et al. (2010) argue that experiments that score high on experimental and mundane realism can still have high external validity. Experimental realism is the extent to which the experiment is involving for the participants and has an impact on them, whereas mundane realism is the extent to which the experimental situation is likely to occur in the participants’ real lives. For the student patients in our study, experimental realism was likely high, but mundane realism rather low as they did not need to be bathed by others in real life. However, for student nurses, both types of realism are likely to be high, because these students will provide bed baths to actual bedridden people in the near future.
Another limitation relates to the measurement of physical comfort for which we found a surprisingly limited number of validated scales. Although it is a rather general construct, we mainly found scales related to pain or broad comfort scales that do not measure physical comfort specifically (Kolcaba et al., 2006; Leonardsen et al., 2017). Consequently, we measured physical comfort among student patients with a single‐item question and used the Physical Demands scale as a proxy for physical comfort among student nurses. While high reliability has been reported for the Physical Demands scale (De Jonge et al., 1999; Verbeek, 2011), its reliability turned out to be rather low in the current study (Cronbach α coefficients of 0.58 for the water and soap method and .72 for the washing without water method). Conversely, the reliability of the PEECE scale, which was used to measure emotional comfort, was high (Cronbach α coefficients of 0.87 and 0.89). These results should be taken into account in the selection of scales to measure comfort in future research. Furthermore, we focused on emotional and physical comfort, but comfort is often described as a holistic construct including physical, psychospiritual, environmental and social dimensions (Kolcaba, 1992). Therefore, future research could study differences in other comfort dimensions between the different bed bath methods.
6. CONCLUSION
Based on our results, washing without water seems to be a suitable alternative for the traditional bed bath with water and soap from the care recipients’ comfort perspective. Moreover, washing without water is more time‐efficient and is less physically demanding for those providing the bed bath. Therefore, its use in health care practice is encouraged.
7. RELEVANCE TO CLINICAL PRACTICE
To follow the daily natural routine, bed baths are mainly provided in the morning, which puts time constraints on to nursing staff. Our study results show that washing without water is less physically demanding for nurses, which is related to nurses’ physical comfort. In addition, the washing without water concept saves time without having a detrimental effect on care recipients’ emotional and physical comfort. Nurses could spend the time saved on other care activities with the care recipient. Finally, our results inform healthcare practice and educators about the perceptions regarding bed bath methods among nursing students, who will soon have to carry out these bed baths themselves.
CONFLICT OF INTEREST
The first author is a doctoral candidate at Maastricht University who is working on research which is partially funded by Arion Holding B.V. Employees of this holding were not involved in the collection, analysis, or interpretation of the data. Hence, the authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
Conception and design of the study; collection, analysis and interpretation of the results: FMVG and SMGZ. Conception and design of the study; analysis and interpretation of the results: GO and JPHH. Data analysis and interpretation; study design: FT. Drafting and revising the manuscript; reading and approval of the final manuscript; accountable for all aspects of the work: All authors.
Supporting information
Supplementary Material
Supplementary Material
ACKNOWLEDGEMENTS
We would like to express our gratitude to our contacts at the bachelor schools of nursing who participated in this trial, in particular to Marijke van Hommerich‐Cronenberg for her enthusiasm, willingness and commitment in setting up the research and recruiting participants. Furthermore, we would like to thank all research assistants who completed the observations of the bed baths.
APPENDIX 1. Cronbach's Alpha coefficients PEECE scale and Physical Demands scale
| Scale | Cronbach's Alpha values (mean inter‐item correlation) | |
|---|---|---|
| Traditional bed bath | Washing without water | |
| PEECE measuring emotional comfort of patients during the bed bath (12 items) | 0.874 | 0.886 |
| Physical Demands measuring physical demands of the bed bath among nurses (7 items) | 0.581 (0.152) | 0.719 (0.298) |
Funding information
This study is partially funded by Arion Holding B.V. (Rutherford 11, 6422 RE Heerlen (NL); info@arion-group.com). Employees of this holding were not involved in the collection, analysis, or interpretation of the data, or the decision to submit results.
REFERENCES
- Andersen, S., Harrison, G. W., Lau, M. I., & Rutström, E. E. (2010). Preference heterogeneity in experiments: Comparing the field and laboratory. Journal of Economic Behavior & Organization, 73(2), 209–224. 10.1016/j.jebo.2009.09.006. [DOI] [Google Scholar]
- Cohen, J. (1977). Statistical power analysis for the behavioral sciences. Academic Press. [Google Scholar]
- Cohen‐Mansfield, J., & Jensen, B. (2005). The preference and importance of bathing, toileting and mouth care habits in older persons. Gerontology, 51(6), 375–385. 10.1159/000088701. [DOI] [PubMed] [Google Scholar]
- Conroy, T. (2017). Factors influencing the delivery of the fundamentals of care: Perceptions of nurses, nursing leaders and healthcare consumers. Journal of Clinical Nursing, 27(11–12), 2373–2386. 10.1111/jocn.14183. [DOI] [PubMed] [Google Scholar]
- De Jonge, J., Mulder, M. J. G. P., & Nijhuis, F. J. N. (1999). The incorporation of different demand concepts in the job demand‐control model: Effects on health care professionals. Social Science & Medicine, 48(9), 1149–1160. [DOI] [PubMed] [Google Scholar]
- Downey, L., & Lloyd, H. (2008). Bed bathing patients in hospital. Nursing Standard, 22(34), 35–40. 10.7748/ns2008.04.22.34.35.c6531. [DOI] [PubMed] [Google Scholar]
- El‐Soussi, A. H., & Asfour, H. I. (2016). Examining bed‐bath practices of critically ill patients. Journal of Nursing Education and Practice, 6(12), 1–11. 10.5430/jnep.v6n12p1.29142615 [DOI] [Google Scholar]
- Eurostat (2016). Disability statistics prevalence and demographics. Retrieved from https://ec.europa.eu/eurostat/statistics‐explained/pdfscache/34409.pdf.
- Feo, R., & Kitson, A. (2016). Promoting patient‐centred fundamental care in acute healthcare systems. International Journal of Nursing Studies, 57, 1–11. 10.1016/j.ijnurstu.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Feo, R., Kitson, A., & Conroy, T. (2018). How fundamental aspects of nursing care are defined in the literature: A scoping review. Journal of Clinical Nursing, 27(11–12), 2189–2229. 10.1111/jocn.14313. [DOI] [PubMed] [Google Scholar]
- Groven, F. M. V., Odekerken‐Schröder, G., Zwakhalen, S., & Hamers, J. P. H. (2020). Network Well‐Being from a Balanced Centricity Perspective. Manuscript submitted for publication.
- Groven, F. M. V., Zwakhalen, S., Odekerken‐Schröder, G., Joosten, E. J. T., & Hamers, J. P. H. (2017). How does washing without water perform compared to the traditional bed bath: A systematic review. BMC Geriatrics, 17(1), 31. 10.1186/s12877-017-0425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groven, F. M. V., Zwakhalen, S. M. G., Odekerken‐Schröder, G., Tan, F., & Hamers, J. P. H. (2019). The effects of washing without water versus the traditonal bed bath with water and soap on comfort and physical demands: protocol of a cross‐over randomized trial. https://assets.researchsquare.com/files/rs‐7409/v1/manuscript.pdf.
- Gul, R. B., & Ali, P. A. (2010). Clinical trials: The challenge of recruitment and retention of participants. Journal of Clinical Nursing, 19(1–2), 227–233. 10.1111/j.1365-2702.2009.03041.x. [DOI] [PubMed] [Google Scholar]
- Hoeffer, B., Talerico, K. A., Rasin, J., Mitchell, C. M., Stewart, B. J., McKenzie, D., Barrick, A. L., Rader, J., & Sloane, P. D. (2006). Assisting cognitively impaired nursing home residents with bathing: effects of two bathing interventions on caregiving. Gerontologist, 46(4), 524–532. [DOI] [PubMed] [Google Scholar]
- Hooghe, M., Stolle, D., Mahéo, V., & Vissers, S. (2010). Why can’t a student be more like an average person? Sampling and attrition effects in social science field and laboratory experiments. The Annals of the American Academy, 628(1), 85–96. 10.1177/0002716209351516. [DOI] [Google Scholar]
- Jagger, C., Arthur, A. J., Spiers, N. A., & Clarke, M. (2001). Patterns of onset of disability in activities of daily living with age. Journal of the American Geriatrics Society, 49(4), 404–409. [DOI] [PubMed] [Google Scholar]
- Jangland, E., Mirza, N., Conroy, T., Merriman, C., Suzui, E., Nishimura, A., & Ewens, A. (2018). Nursing students’ understanding of the Fundamentals of Care: A cross‐sectional study in five countries. Journal of Clinical Nursing, 27(11–12), 2460–2472. 10.1111/jocn.14352. [DOI] [PubMed] [Google Scholar]
- Johannesen, A., Petersen, J., & Avlund, K. (2004). Satisfaction in everyday life for frail 85‐year‐old adults: a Danish population study. Scandinavian Journal of Occupational Therapy, 11(1), 3–11. 10.1080/11038120410019045. [DOI] [Google Scholar]
- Kolcaba, K. (1992). Holistic comfort: Operationalizing the construct as a nurse‐sensitive outcome. Advances in Nursing Science, 15(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Kolcaba, K. (1994). A theory of holistic comfort for nursing. Journal of Advanced Nursing, 19(6), 1178–1184. [DOI] [PubMed] [Google Scholar]
- Kolcaba, K., Schirm, V., & Steiner, R. (2006). Effects of hand massage on comfort of nursing home residents. Geriatric Nursing, 27(2), 85–91. [DOI] [PubMed] [Google Scholar]
- Larson, E. L., Ciliberti, T., Chantler, C., Abraham, J., Lazaro, E. M., Venturanza, M., & Pancholi, P. (2004). Comparison of traditional and disposable bed baths in critically ill patients. American Journal of Critical Care, 13(3), 235–241. [PubMed] [Google Scholar]
- Leonardsen, A.‐C., Grøndahl, V. A., Ghanima, W., Storeheier, E., Schönbeck, A., Løken, T.‐A., Bakken, N. C. M., Letting, G. S., Holst, R., & Jelsness‐Jørgensen, L.‐P. (2017). Evaluating patient experiences in decentralised acute care using the Picker Patient Experience Questionnaire; methodological and clinical findings. BMC Health Services Research, 17(1), 658. 10.1186/s12913-017-2614-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes, J. L., Baptista, R. C. N., Lopes, C. T., Rossi, M. B., Swanson, E. A., & Barros, A. L. B. L. (2019). Efficacy of a video during bed bath simulation on improving the performance or psychomotor skills of nursing undergraduates: A randomized clinical trial. International Journal of Nursing Studies, 99, 7–12. 10.1016/j.ijnurstu.2019.04.001. [DOI] [PubMed] [Google Scholar]
- Lopes, J. L., Nogueira‐Martins, L. A., & de Barros, A. L. B. L. (2012). Bed and shower baths: comparing the perceptions of patients with acute myocardial infarction. Journal of Clinical Nursing, 22(5–6), 733–740. 10.1111/j.1365-2702.2012.04320.x. [DOI] [PubMed] [Google Scholar]
- Lorente, S., Losilla, J. M., & Vives, J. (2017). Instruments to assess patient comfort during hospitalization: A psychometric review. Journal of Advanced Nursing, 74(5), 1001–1015. 10.1111/jan.13495. [DOI] [PubMed] [Google Scholar]
- Malinowski, A., & Stamler, L. L. (2002). Comfort: exploration of the concept in nursing. Journal of Advanced Nursing, 39(6), 599–606. [DOI] [PubMed] [Google Scholar]
- Meehan, T. C., Timmins, F., & Burke, J. (2018). Fundamental care guided by the Careful Nursing Philosophy and Professional Practice Model©. Journal of Clinical Nursing, 27(11–12), 2260–2273. 10.1111/jocn.14303. [DOI] [PubMed] [Google Scholar]
- Miranda, R. P. R., de Cássia Lopes Chaves, É., Silva Lima, R., Braga, C. G., Simões, I. A. R., Fava, S. M. C. L., & Iunes, D. H. (2017). The effectiveness of a simulated scenario to teach nursing students how to perform a bed bath ‐ a randomized clinical trial. Nurse Education Today, 57, 17–23. 10.1016/j.nedt.2017.06.008. [DOI] [PubMed] [Google Scholar]
- Morse, J. M., Bottorff, J. L., & Hutchinson, S. (1995). The paradox of comfort. Nursing Research, 44(1), 14–19. [PubMed] [Google Scholar]
- Nøddeskou, L. H., Hemmingsen, L. E., & Hørdam, B. (2015). Elderly patients’ and nurses’ assessment of traditional bed bath compared to prepacked single units ‐ randomised controlled trial. Scandinavian Journal of Caring Sciences, 29(2), 347–352. 10.1111/scs.12170. [DOI] [PubMed] [Google Scholar]
- Nøddeskou, L. H., Túgvustein, N., Marjunardóttir, A., Gaardbo, I., Hemmingsen, L., & Hørdam, B. (2018). Assessment of bed bathing methods in the Faroe Islands. The American Journal of Nursing Science, 7(3), 109–114. 10.11648/j.ajns.20180703.15. [DOI] [Google Scholar]
- Parr, J. M., Bell, J., & Koziol‐McLain, J. (2017). Evaluating fundamentals of care: The development of a unit‐level quality measurement and improvement programme. Journal of Clinical Nursing, 27(11–12), 2360–2372. 10.1111/jocn.14250. [DOI] [PubMed] [Google Scholar]
- Pipe, T. B., Connolly, T., Spahr, N., Lendzion, N., Buchda, V., Jury, R., & Cisar, N. (2012). Bringing back the basics of nursing: Defining patient care essentials. Nursing Administration Quarterly, 36(3), 225–233. 10.1097/NAQ.0b013e31825afb3c. [DOI] [PubMed] [Google Scholar]
- Rader, J., Barrick, A. L., Hoeffer, B., Sloane, P. D., McKenzie, D., Talerico, K. A., & Glover, J. U. (2006). The bathing of older adults with dementia: easing the unnecessarily unpleasant aspects of assisted bathing. AJN, American Journal of Nursing, 106(4), 40–49. [DOI] [PubMed] [Google Scholar]
- Richards, D. A., & Hamers, J. P. H. (2009). RCTs in complex nursing interventions and laboratory experimental studies. International Journal of Nursing Studies, 46(4), 588–592. 10.1016/j.ijnurstu.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Richards, D. A., Hilli, A., Pentecost, C., Goodwin, V. A., & Frost, J. (2018). Fundamental nursing care: A systematic review of the evidence on the effect of nursing care interventions for nutrition, elimination, mobility and hygiene. Journal of Clinical Nursing, 27(11–12), 2179–2188. 10.1111/jocn.14150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoonhoven, L., van Gaal, B. G. I., Teerenstra, S., Adang, E., van der Vleuten, C., & van Achterberg, T. (2015). Cost‐consequence analysis of "washing without water" for nursing home residents: a cluster randomized trial. International Journal of Nursing Studies, 52(1), 112–120. 10.1016/j.ijnurstu.2014.08.001. [DOI] [PubMed] [Google Scholar]
- Sheppard, C. M., & Brenner, P. S. (2000). The effects of bathing and skin care practices on skin quality and satisfaction with an innovative product. Journal of Gerontological Nursing, 26(10), 36–45, quiz 55–36. [DOI] [PubMed] [Google Scholar]
- Sturgeon, L. P., Garrett‐Wright, D., Lartey, G., Jones, M. S., Bormann, L., & House, S. (2019). A descriptive study of bathing practices in acute care facilities in the United States. American Journal of Infection Control, 47(1), 23–26. 10.1016/j.ajic.2018.07.007. [DOI] [PubMed] [Google Scholar]
- Tan, F. E. S., Jolani, S., & Verbeek, H. (2018). Guidelines for multiple imputations in repeated measurements with time‐dependent covariates: A case study. Journal of Clinical Epidemiology, 102, 107–114. 10.1016/j.jclinepi.2018.06.006. [DOI] [PubMed] [Google Scholar]
- Veje, P. L., Chen, M., Jensen, C. S., Sørensen, J., & Primdahl, J. (2019a). Bed bath with soap and water or disposable wet wipes: Patients’ experiences and preferences. Journal of Clinical Nursing, 28(11–12), 2235–2244. 10.1111/jocn.14825. [DOI] [PubMed] [Google Scholar]
- Veje, P. L., Chen, M., Jensen, C. S., Sørensen, J., & Primdahl, J. (2019b). Effectiveness of two bed bath methods in removing microorganisms from hospitalized patients: A prospective randomized crossover study. American Journal of Infection Control, 48(6), 638–643. 10.1016/j.ajic.2019.10.011. [DOI] [PubMed] [Google Scholar]
- Verbeek, H. (2011). Redesigning dementia care ‐ An evaluation of small‐scale, homelike care environments. (Doctoral dissertation).
- Williams, A. M., & Irurita, V. F. (2004). Therapeutic and non‐therapeutic interpersonal interactions: The patient’s perspective. Journal of Clinical Nursing, 13(7), 806–815. [DOI] [PubMed] [Google Scholar]
- Williams, A. M., Lester, L., Bulsara, C., Petterson, A., Bennett, K., Allen, E., & Joske, D. (2017). Patient Evaluation of Emotional Comfort Experienced (PEECE): developing and testing a measurement instrument. British Medical Journal Open, 7(7), e012999. 10.1136/bmjopen-2016-012999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, T. D., Aronson, E., & Carlsmith, K. (2010). The art of laboratory experimentation. In Fiske S. T., Gilbert D. T., & Lindzey G. (Eds.), Handbook of social psychology, Vol. one (pp. 51–81). John Wiley & Sons. [Google Scholar]
- Wolf, Z. R. (1997). Nursing students’ experience bathing patients for the first time. Nurse Educator, 22(2), 41–46. [DOI] [PubMed] [Google Scholar]
- Zwakhalen, S. M. G., Hamers, J. P. H., Metzelthin, S. F., Ettema, R., Heinen, M., de Man‐Van Ginkel, J. M., Vermeulen, H., Huisman‐de Waal, G., & Schuurmans, M. J. (2018). Basic nursing care: The most provided, the least evidence based. A discussion paper. Journal of Clinical Nursing, 27(11–12), 2496–2505. 10.1111/jocn.14296. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material


